Abstract
Aims
In Portugal, in the last 5 years, no study has published recent data regarding outcomes of patients with acute decompensated heart failure (ADHF). We aimed to determine the characteristics and outcomes of a large contemporaneous Portuguese cohort of ADHF patients admitted to our emergency department (ED).
Methods and results
We conducted a retrospective, study of all 1024 patients admitted to our ED with a discharge diagnosis of ADHF from November 2016 to December 2017. Baseline clinical data and outcomes {in‐hospital, 30 day, and follow‐up all‐cause mortality, and readmissions; median follow‐up, 5 months; interquartile range [(IQR), 3–11 months]} were determined. Mean age was 78 ± 10 years, and 53% were male; of the 1024 patients, 554 (54%) were hospitalized. The median hospitalization length was 9 (IQR, 5–15) days, and in‐hospital mortality was 12.7%. Hospitalized patients were predominantly men (56% vs. 47%; P < 0.001), younger (77 ± 9 vs. 79 ± 11 years; P = 0.002) and had higher creatinine values and B‐type natriuretic peptide values (P < 0.001) than discharged patients. Patients with prior hospitalization had lower 30 day readmission rate (8% vs. 14%; P = 0.01), same overall readmission rate (30% vs. 32%), and higher 30 day (13% vs. 5%; P < 0.001) and overall mortality rates (28% vs. 15%; P < 0.001).
Conclusions
Approximately half of the patients admitted to the ED were hospitalized. Of these, only 8% were readmitted in the ED within 30 days. The clinical and analytical status in the ED are important predictors of hospitalization.
Keywords: Acute heart failure, Emergency department, Epidemiology, Mortality, In‐hospital mortality, Readmission rates, Hospitalization, Predictors of prognosis
Introduction
Heart failure (HF) is a clinical syndrome characterized by typical symptoms (e.g. breathlessness) and signs (e.g. pulmonary crackles, peripheral edema) caused by a structural or functional cardiac abnormality, resulting in reduced cardiac output and elevated intracardiac pressures at rest or during stress.1 The prevalence of HF is approximately 1% to 2% and increases to more than 10% in persons older than 70 years.2 In Portugal, the global prevalence of HF is 4.36%, with a prevalence of 12.7% in persons older than 70 years and 16.1% in those older than 80 years.3
Acute decompensated HF (ADHF) represents a broad spectrum of disease states commonly characterized by either a rapid onset or a progressive worsening of signs and symptoms, requiring immediate treatment and leading to urgent hospitalization.1 ADHF is the leading cause of hospitalization in patients older than 65 years and has substantial health economic impacts.2, 4 Patients with ADHF often present to the emergency department (ED) and, in some cases, are hospitalized based not only on symptoms but also on the unknown risk of clinical instability or social issues.5
Although acute management of ADHF has remained essentially the same6 over the recent decades, advances in the treatment of chronic HF have improved global survival rates and reduced hospitalization rates. However, outcomes remain unsatisfactory.1, 7 The most recent European data demonstrate that 12 month all‐cause mortality rates for hospitalized and stable/ambulatory HF patients were 17% and 7%, respectively, and the 12 month hospitalization rates were 44% and 32%, respectively.8 In another study, the 30 day mortality for HF was 11.1%, and the 30 day readmission was approximately 24%.9 More recently published data indicate a 30 day readmission rate of 37% and a 30 day mortality rate of 9%.10 In Portugal, the last estimated in‐hospital mortality was 12.5% in 2014.11 In patients with HF (both hospitalized and ambulatory), most deaths were due to cardiovascular causes, mainly sudden death and worsening HF.8 Hospitalizations are often due to non‐cardiovascular causes, particularly in patients with HF with preserved left ventricular ejection fraction (LVEF). There has been a slight decline in hospitalizations for HF in recent decades; however, ED visits for this condition have not decreased significantly.12 In Portugal, thus far, no study has published recent data regarding outcomes of patients with ADHF, in terms of hospitalization, in‐hospital mortality, readmission rates, and overall mortality.3, 11 Furthermore, little is known about predictors of early discharge versus hospitalization or outcomes of patients with ADHF that are discharged from the ED after a short course of intravenous diuretics and an adjustment of oral medication.11
In this study, we aimed to describe the demographic and clinical characteristics of patients who were observed to have ADHF in a large ED, characterize the initial ED evaluation and subsequent management of patients with ADHF, and assess the short‐term and medium‐term outcomes of patients discharged from the ED or hospitalized with ADHF.
Methods
Study design and population
We conducted a retrospective study of all consecutive patients admitted to the ED of Centro Hospitalar e Universitário de Coimbra with an electronically coded discharge diagnosis of ADHF. Patients were identified for inclusion in the registry if given a discharge diagnosis of HF based on International Classification of Diseases, Ninth Revision (ICD‐9) coding (ICD‐9 codes in Supporting Information, Table A1 ). Patients were enrolled from November 2016 to December 2017. The lists of patients with these codes were obtained from hospital electronic records (Alert®; ALERT Life Sciences Computing, S.A. Vila Nova de Gaia, Portugal). Eligibility was not contingent on the use of any particular therapy. The registry accumulated data on individual hospitalizations, not individual patients, and it is possible that some patients were enrolled in the registry more than once.
Patients that did not receive a diagnosis based on the ICD‐9 coding were not included in the analysis. At patients' discharge or hospitalization, not all physicians codify the diagnosis of HF by the ICD‐9 system. Some physicians confine their diagnosis to just ‘dyspnea’, ‘fatigue’, or even abbreviators, such as ‘HF’. These inappropriately codified diagnoses may lead to a lower than expected inclusion of ADHF patients. To estimate an approximate percentage of the included patients in regard to all patients admitted with ADHF, we reviewed ED admissions over the year of 2017 during 12 random days of each month, as described in Supporting Information, Table A2 .
Inclusion and exclusion criteria
The inclusion criteria were age of at least 18 years at the time of hospitalization and signs or symptoms of ADHF, which, in addition to the discharge HF ICD‐9 coding, met one at least one of the following criteria: (i) lung congestion, assessed by clinical examination or chest X‐ray and (ii) objective findings of left ventricular systolic dysfunction or structural heart disease, in addition to B‐type natriuretic peptide (BNP) levels >100 pg/mL.
Patients that did not meet the abovementioned criteria, had BNP levels <100 pg/mL, were excluded.
Data collection
Data were collected by retrospective chart review. We collected information regarding demographics, clinical, and laboratory parameters at presentation. The acute management of ADHF patients in the ED was assessed, including drug administration, time to intravenous diuretics (‘door‐to‐furosemide’ time), and noninvasive ventilation. We also characterized the route of patients in the ED (discharged versus hospitalization).
Outcomes and follow‐up
The patients were followed‐up for a median period of 5 months {interquartile range [(IQR), 3–11 months]}. All patients had at least a 30 day follow‐up. Outcomes included all‐cause in‐hospital mortality, all‐cause 30 day mortality, all‐cause follow‐up mortality, 30 day readmission, and follow‐up all‐cause readmissions.
Ethical compliance
Patient confidentiality was preserved because direct patient identifiers, such as social security number or hospital record number, were not collected. Only data available from existing medical records were accessed, and data were reported only in aggregate format. The study was approved by the scientific and bioethical committees of Centro Hospitalar e Universitário de Coimbra (Coimbra, Portugal) and was performed in accordance with the Declaration of Helsinki.
Statistical analysis
Normality of continuous variables was assessed by histogram observation and the Kolmogorov–Smirnov test. Continuous variables were expressed as mean ± standard deviation and categorical variables as percentages. Student's t‐test or analysis of variance was used for group comparisons. Individual variables were assessed for homogeneity of variance using Levene's test. For categorical variables, chi‐square or Fisher's exact test was used, as appropriate. Fractional polynomial regression and locally weighted scatterplot smoothing was used to accomplish modulation of readmission rate versus hospitalization time and in‐hospital mortality versus ‘door‐to‐furosemide time’. Univariate and multivariate Cox's proportional hazards analyses were used to assess predictors of outcomes. A P value (two‐sided) <0.05 was considered statistically significant. STATA IC for Windows version 13 (StataCorp, Lakeway Drive, TX, USA) was used for statistical analysis.
Results
Study population
From a total of 96 000 ED admissions during the study period, a total of 1024 (1.1%) patients diagnosed with ADHF (by ICD‐9 coding) were included in our study. This group of codified ADHF diagnosis represented a mean of 58.25% (between 42% and 100%) of all ADHF diagnosis (codified and not codified) made in the ED.
The mean age was 78 ± 10 years; there was a roughly equal distribution between male (53%) and female (47%) patients. Coronary artery disease was present in 29% cases, valvular heart disease in 42%, and atrial fibrillation in 67%. Approximately 74% patients underwent echocardiography, and they have mean LVEF of 43 ± 13%, mean serum creatinine of 1.3 ± 0.7 mg/dL, mean C‐reactive protein (CRP) of 3.3 ± 2.1 mg/dL, and median BNP of 545 pg/mL (IQR, 296–1131 pg/mL).
Regarding the therapeutic management in the ED, 92% of the patients received intravenous diuretics, 5% received intravenous vasodilators (mostly dinitrate isosorbide), 5% underwent noninvasive ventilation, and 1% received inotropic support. Median ‘door‐to‐furosemide’ time was 90 min (IQR, 40–230 min). Of the 1024 patients, 46% were directly discharged from the ED, and 54% were hospitalized. The clinical and analytical characteristics according to this criterion are described in Table 1.
Table 1.
Clinical, analytical, and outcome data of the study population
| Variables | Discharged | Hospitalized | P value |
|---|---|---|---|
| Age (years) | 78 ± 10 | 75 ± 12 | 0.002* |
| Male (%) | 48 | 57 | <0.001* |
| LVEF (%) | 46 ± 10 | 41 ± 12 | <0.001* |
| CAD (%) | 24 | 33 | 0.002* |
| VHD (%) | 40 | 44 | 0.180 |
| AF (%) | 64 | 69 | 0.093 |
| Creatinine (mg/dL) | 1.20 ± 0.7 | 1.45 ± 0.8 | <0.001* |
| CRP (mg/dL) | 1.75 ± 2.7 | 2.5 ± 3.7 | <0.001* |
| BNP (pg/mL) | 385 [218–701] | 740 [384–1480] | <0.001* |
| 30 day readmission rate (%) | 14 | 9 | 0.015* |
| Follow‐up readmission rate (%) | 33 | 33 | 0.927 |
| 30 day mortality rate (%) | 5 | 13 | <0.001* |
| Follow‐up mortality rate (%) | 15 | 28 | <0.001* |
Values are presented as mean ± standard deviation, %, or median [interquartile range].
AF, atrial fibrillation; BNP, B‐type natriuretic peptide; CAD, coronary artery disease; CRP, C‐reactive protein; LVEF, left ventricular ejection fraction; VHD, valvular heart disease.
Statistically significant P value.
Clinical outcomes
Table 1 shows the prevalence of all clinical outcomes.
Patients with a prior ADHF hospitalization had a lower 30 day readmission rate (8% vs. 14%; P = 0.01), same overall readmission rate (30% vs. 32%), and higher 30 day (13% vs. 5%; P < 0.001) and overall mortality (28% vs. 15%; p<0.001) than those of discharged patients (Table 1).
There were seven deaths that occurred within 24 h of admission in the ED. Of those, two deaths occurred while patients were staying in the ED.
Predictors of clinical outcomes
Table 2 shows the predictors of the clinical outcomes, derived from univariate analysis.
Table 2.
Predictors of clinical outcomes derived from univariate analysis
| Outcomes | Predictors | HR (95% CI) | P value |
|---|---|---|---|
| 30 day readmission (discharged and hospitalized patients) | BNP | 1.6 (1.1–1.9) | 0.016* |
| CRP | 1.5 (1.1–1.7) | 0.014* | |
| Follow‐up readmission (hospitalized and discharged patients) | LVEF | 0.91 (0.90–0.94) | 0.039* |
| 30 day mortality (hospitalized patients) | Age | 1.4 (1.2–1.7) | <0.001* |
| Creatinine | 2.3 (1.4–5.3) | 0.043* | |
| 30 day mortality (discharged patients) | Creatinine | 2.3 (1.1–4.6) | 0.041* |
| Follow‐up mortality (hospitalized patients) | Age | 1.4 (1.3–1.7) | <0.001* |
| Creatinine | 1.6 (1.1–1.9) | <0.001* | |
| Follow‐up mortality (discharged patients) | BNP | 1.2 (1.1–1.5) | <0.001* |
| CRP | 1.1 (1.0–1.3) | <0.001* |
BNP, B‐type natriuretic peptide; CRP, reactive C‐protein; LVEF, left ventricular ejection fraction.
Statistically significant P value.
Hospitalization
Patients who were hospitalized (54%) were predominantly men, younger, and with higher creatinine, BNP, and CRP levels (Table 1). Male sex [odds ratio (OR), 1.59; 95% confidence interval (CI), 1.3–1.9; P = 0.016], BNP levels (OR, 1.80; 95% CI, 1.50–2.1; P < 0.001), and LVEF (OR, 0.97; 95% CI, 0.95–0.98; P < 0.001) were significant predictors of hospitalization versus discharge. The mean hospitalization length was 9 days (IQR 5–15), and in‐hospital all‐cause mortality was 13%.
Thirty day and follow‐up readmission rate
Among the 54% hospitalized patients, the 30 day all‐cause readmission rate was 8%. We found an interaction between prior hospitalization for ADHF length of stay and 30 day readmission rate. The 30 day readmission rate was higher with a prior hospitalization length less than 5 days, lower with 5–10 days, and higher with lengths for more than 10 days (Figures 1 and 2 , Table 3). Of the 46% patients who were directly discharged from the ED with a diagnosis of ADHF, 14% were readmitted at 30 days. Independent predictors for 30 day readmission were a higher BNP [hazards ratio (HR), 1.5; 95% CI, 1.1–1.8; P = 0.02] and CRP (HR 1.7; 95% CI, 1.2–1.8; P = 0.01).
Figure 1.
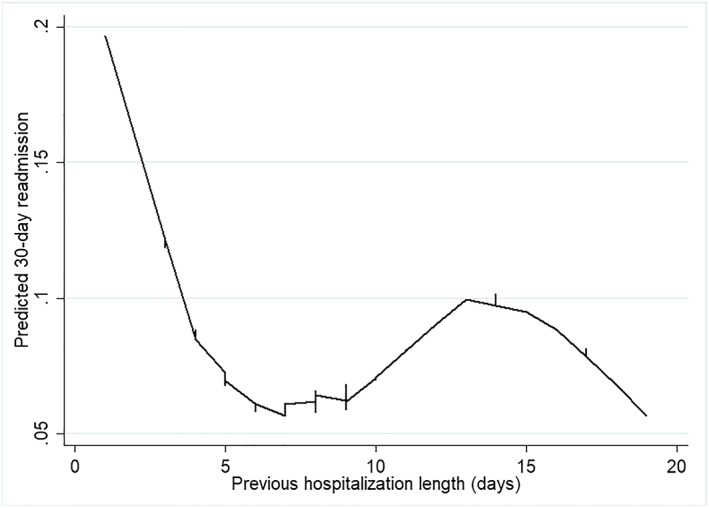
Predicted 30 day readmission in previously hospitalized patients, according to previous hospitalization length.
Figure 2.
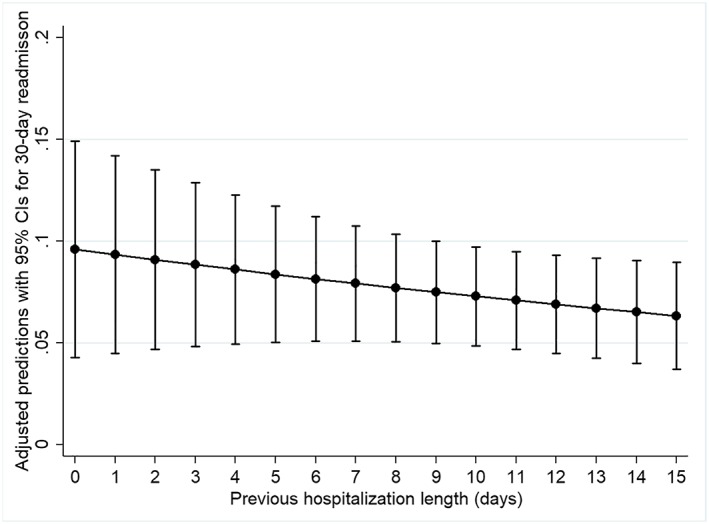
Adjusted predictions (odds ratio with 95% confidence interval) for 30 day readmission in previously hospitalized patients, according to previous hospitalization length.
Table 3.
Thirty day readmission according to previous hospitalization length in days
| Hospitalization length (days) | 30 day readmission (%) |
|---|---|
| 0–5 | 9.5 |
| 5–10 | 4.2 |
| >10 | 10.9 |
Thirty day readmission was lower in patients with a previous hospitalization length of 5–10 days (P = 0.05).
Follow‐up (median, 5 months) readmission rate for previously hospitalized patients was 30%, and its only independent predictor was LVEF (HR, 0.93; 95% CI, 0.91–0.96; P = 0.05). In patients directly discharged from the ED with ADHF, follow‐up all‐cause readmission was 32% and was predicted by LVEF (HR, 0.91; 95% CI, 0.90–0.93; P < 0.01).
Thirty‐day and follow‐up all‐cause mortality
In hospitalized patients, all‐cause mortality at 30 days was 15%, with age (HR, 1.4; 95% CI, 1.1–1.9; P = 0.04) and creatinine (HR, 2.3; 95% CI, 1.3–5.3; P = 0.04) being positive predictors. In patients directly discharged from the ED, the 30 day mortality was 4.6% and was only predicted by creatinine (HR, 2.5; 95% CI, 1.1–4.8; P = 0.04).
In hospitalized patients, follow‐up all‐cause mortality was 28% and was predicted by age (HR, 1.4; 95% CI, 1.2–1.7; P < 0.01) and creatinine (HR, 1.5; 95% CI, 1.1–1.9; P < 0.01). In directly discharged patients from the ED, all‐cause mortality was 15% and was predicted by CRP (HR, 1.15; 95% CI, 1.0–1.3; P < 0.01) and BNP (HR, 1.3; 95% CI, 1.1–1.5; P < 0.01).
Door‐to‐furosemide time
About 92% of the patients received intravenous diuretics, and median ‘door‐to‐furosemide’ time was 90 min (IQR, 40–230 min). The administration time of intravenous furosemide was not associated with any of the defined outcomes. As described in Figure 3 , the majority of patients received intravenous furosemide in the first 200 to 300 min of admission (Figure 3 , bottom); however, it did not affect the defined outcome (in‐hospital mortality), as the curve of probability does not change in regard to the minutes of furosemide administration (Figure 3 , top).
Figure 3.
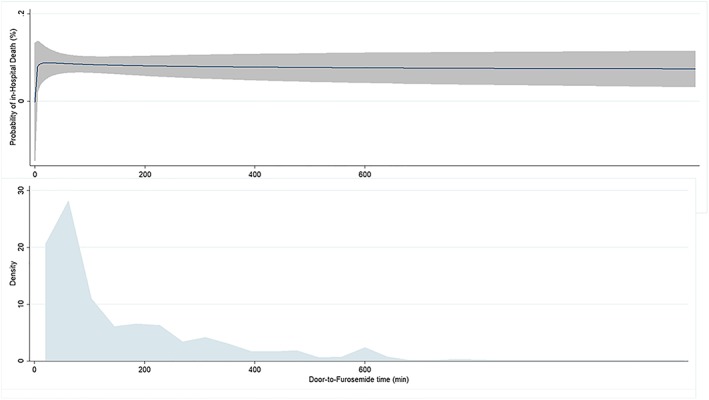
Up—probability of in‐hospital mortality according to the time of furosemide administration; the solid blue line represents the estimated probability of in‐hospital mortality, and the shaded area is the 95% confidence interval. Bottom—density plot showing the distribution of observed door‐to‐furosemide time.
Seasonality of acute decompensated heart failure incidence and hospitalizations
It is a well‐known fact that the seasons of the year have different impact on visits to the emergency departments, but the variation in ADHF incidence throughout the year in Portugal is unknown. In Figure 4 , we depict the distribution of ED recurrences according to months, divided into hospitalized and discharged patients. Recurrences were higher during the winter season, with more than twice the visits in January (10.4% of all admissions), compared with June (3.7%), July (5%), and August (4.7%).
Figure 4.
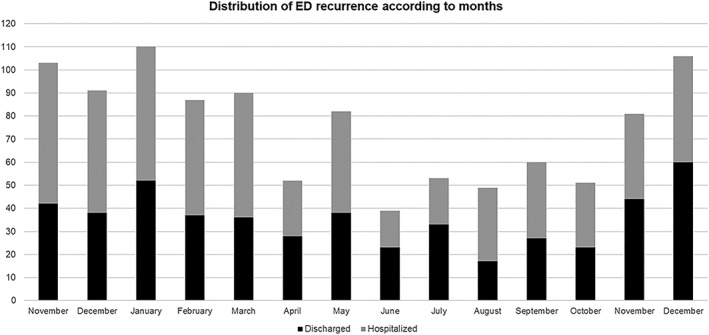
Distribution of emergency department recurrence according to months, divided into hospitalization and discharge.
Discussion
For the first time in Portugal, we performed a short‐term and mid‐term outcomes analysis of 1024 patients admitted to the ED with ADHF. Here, we found a high discharge rate in the acute setting (around 50%), but with low 30 day readmission rates (under 10%). In‐hospital mortality was high but did not vary from the previous estimate in 2014 in a Portuguese population (13% vs. 12.5%).13 Compared with recently published data, we report lower 30 day readmission (8% and 14% vs. 37%) and similar 30 day mortality rates (13% and 5% vs. 9%).11, 14
Our high in‐hospital mortality probably reflects a selection of only the most severe patients being hospitalized, and this is supported by the high proportion of patients discharged from the hospital. In fact, this can be associated with a smaller number of patients that reach the threshold of hospitalization, resulting in the healthiest portion to be managed in the ED and leaving an increasingly higher risk population to be managed in the inpatient setting. In our cohort, hospitalized patients had higher BNP and creatinine values (Table 1). Compared with other registries,15 our cohort had similar creatinine (1.4 vs. 1.2–1.4 mg/dL) and BNP values (739 vs. 493–1719 pg/mL). Our patients were somewhat younger than previously reported (mean age of 77 vs. 81 years).14
The ED is a common entry point for treatment of patients with ADHF. The decision to hospitalize or discharge the patient is very important. Patients hospitalized with ADHF are medically fit for discharge when hemodynamically stable, euvolemic, established on evidence‐based oral medication, and with stable renal function for at least 24 h before discharge.1 It was previously reported that physicians tend to overestimate the risk of ambulatory patients with advanced, chronic HF and are unable to differentiate survival of perceived low‐risk versus high‐risk patients in the clinical setting.16 These inaccuracies in prognostication could potentially lead to low‐risk hospitalizations and high‐risk hospital discharges that could lead to post‐discharge mortality.17 In our study, hospitalized patients had higher 30 day and overall mortality rates, with no differences in overall readmission.
We also found that both short (<5 days) or prolonged (>10 days) hospitalizations are associated with a higher 30 day readmission rate. In fact, we demonstrated that the optimal hospitalization length (at least, from a 30 day readmission point of view) is between 5 and 10 days (Figures 1 and 2 , Table 3). Hypothetically, short hospitalizations can be associated with faster withdrawal of intravenous diuretics and vasodilators in the earlier stages of decompensation, which prevents sustained improvement and may lead to the discharge of a patient who is still congestive. Meanwhile, prolonged hospitalizations are normally associated with several comorbidities, hospital‐acquired infections, and social issues that prevent earlier discharge and rehabilitation.
The acute pharmacological management in the ED was also assessed. Although a paradigm shift has occurred regarding the ambulatory treatment of chronic systolic HF, the management of ADHF has not changed for several decades, and most clinical studies investigating several drugs targeting this population have failed to demonstrate a favourable prognostic impact.1 It has been demonstrated that early administration of furosemide can be independently associated with a better in‐hospital outcome.18 In our cohort, ADHF management in the ED was suboptimal, with a very low usage of intravenous vasodilators (5.1%, compared with previous reported rates of 21.2%15) and delayed administration of loop diuretics [median time until administration of 90 (IQR 48–230) min compared with previous reported 90 (IQR 36–186) min18]. Also, in our cohort, door‐to‐furosemide time was not a predictor of outcomes (Figure 3 ). It remains controversial whether ADHF can have acute harmful effects that are worth addressing early with diuretics and vasodilators. Lee et al.19 also demonstrated that in‐hospital timely initiation of diuretics did not improve survival. Therefore, these controversial findings suggest that the length of door‐to‐diuretic time on clinical outcomes in patients with ADHF has a limited role for in‐hospital and post‐discharge outcomes.
Clinical and analytical statuses in the ED were important predictors of hospitalization and also 30 day and follow‐up outcomes of discharged and hospitalized patients, in line with what has been previously reported.10, 14, 15
The main limitation of our study is the low percentage of patients included (1%) in terms of overall ED admissions. This might be related to diagnosis codification. Sometimes, the attending physician is not sure of the final diagnosis and inserts only ‘dyspnea’ or other presenting symptoms. The group of codified patients represented a mean of 58.25% of the total HF diagnosis made in the ED. With a low proportion of overall ED admissions, our study might be underpowered. Nonetheless, it represents a noteworthy portion (above half) of our ADHF population, in which a direct analysis of outcomes can possibly change the clinical approach and improve management of these patients. Also, this was a single centre study. A multicenter study would provide much more data regarding ADHF patients, with an overall review of outcomes on a national scale.
Conclusions
Our study provides important contemporary information regarding ADHF patients admitted to the ED. The clinical and analytical status in the ED were predictors of hospitalization and follow‐up outcomes. Acute pharmacological management in the ED was suboptimal. Approximately half of the patients were hospitalized, and of these, only 8% were readmitted within 30 days. Among patients discharged directly from the ED, only one in seven were readmitted at 30 days. We also report a very high seasonality of ADHF admission rate. The present findings may have implications for the many patients who present to EDs worldwide because estimation of prognosis underlies many clinical decisions. Furthermore, our contemporaneous study reflects a suboptimal acute management of ADHF, which, if improved, could lead to better outcomes.
Conflict of interest
None declared.
Funding
The study was fundedby grant number poci‐01‐0145‐feder‐032414 from the Portuguese ScienceFoundation (Fundação para a Ciência e Tecnologia).
Supporting information
Data S1. Supporting information.
Marques‐Alves, P. , Marinho, A. V. , Almeida, J. P. , Gonçalves, T. , Costa, M. , Ferreira, M. , Baptista, R. , Costa, S. , Franco, F. , Fonseca, I. , and Gonçalves, L. (2020) Real‐world analysis of acute decompensated heart failure outcomes in Portugal. ESC Heart Failure, 7: 551–558. 10.1002/ehf2.12599.
References
- 1. Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, Volkmar F, González‐Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GMC, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P, ESC Scientific Document Group . 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) Developed with the special contribution. Eur Heart J 2016; 37: 2129–2200. [DOI] [PubMed] [Google Scholar]
- 2. Kurmani S, Squire I. Acute heart failure: definition, classification and epidemiology. Curr Heart Fail Rep 2017; 14: 385–392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ceia F, Fonseca C, Mota T, Morais H, Matias F, Sousa D. Prevalence of chronic heart failure in Southwestern Europe: the EPICA study. Eur Heart J 2002; 4: 531–539. [DOI] [PubMed] [Google Scholar]
- 4. Choi KH, Lee GY, Choi J, Jeon E, Lee H, Cho H, Lee SE, Kim MS, Kim JJ, Hwang KK, Chae SC. Outcomes of de novo and acute decompensated heart failure patients according to ejection fraction. Heart 2018; 104: 525–532. [DOI] [PubMed] [Google Scholar]
- 5. Pang P, Schuur JD. Emergency departments, acute heart failure, and admissions one size does not fit all *. JACC Heart Failure 2014; 2: 278–280. [DOI] [PubMed] [Google Scholar]
- 6. Shah P, Pellicori P, Cuthbert J, Clark AL. Pharmacological and non‐pharmacological treatment for decompensated heart failure: what is new? Curr Heart Fail Rep 2017; 14: 147–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. VanRiet EES, Hoes AW, Wagenaar KP, Limburg A, Landman MAJ, Rutten FH. Epidemiology of heart failure: the prevalence of heart failure and ventricular dysfunction in older adults over time. A systematic review. Eur J Heart Fail 2016; 18: 242–252. [DOI] [PubMed] [Google Scholar]
- 8. Maggioni AP, Filippatos G, Chioncel O, Leiro MC, Drozdz J, Fruhwald F, Gullestad L, Logeart D, Fabbri G, Urso R. EUR Observational Research Programme: regional differences and 1‐year follow‐up results of the Heart Failure Pilot Survey (ESC‐HF Pilot). Eur J Heart Fail 2013; 15: 808–817. [DOI] [PubMed] [Google Scholar]
- 9. Krumholz HM, Merrill AR, Schone EM, Schreiner G, Chen J, Bradley E, Wang Y, Wang Y, Lin Z, Straube BM, Rapp MT. Patterns of hospital performance in acute myocardial infarction and heart failure 30‐day mortality and readmission. Circ Cardiovasc Qual Outcomes 2009; 2: 407–413. [DOI] [PubMed] [Google Scholar]
- 10. Shen C, Yeh RW. Association of the hospital readmissions reduction program with mortality among medicare beneficiaries hospitalized for heart failure, Acute Myocardial Infarction, and Pneumonia. JAMA 2018; 320: 2542–2552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fonseca C, Brás D, Araújo I, Ceia F. Insuficiência cardíaca em números: estimativas para o século XXI em Portugal. Rev Port Cardiol 2018; 37: 97–104. [DOI] [PubMed] [Google Scholar]
- 12. Blecker S, Ladapo JA, Doran KM, Goldfeld KS. Emergency department visits for heart failure and subsequent hospitalization or observation unit admission. Am Heart J 2010; 168: 901–908.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Direção Geral da Saúde . Portugal: doenças cérebro–cardiovasculares em números ‐ 2015 [Internet]. Saúde em Números. 2015. p. 92.https://www.dgs.pt/em-destaque/portugal-doencas-cerebro-cardiovasculares-em-numeros‐201511.aspx.https://www.dgs.pt/em-destaque/portugal-doencas-cerebro-cardiovasculares-em-numeros-201511.aspx
- 14. Mcleod SL, Dreyer JF, Sabbah S, Stukel TA, Austin PC, Tu J V. Prospective validation of the emergency heart failure mortality risk grad for acute heart failure: the acute congestive heart failure urgent care evaluation (ACUTE) Study. Circulation 2019; 139: 1146–1156. [DOI] [PubMed] [Google Scholar]
- 15. Chioncel O, Mebazaa A, Harjola V, Coats A, Piepoli M, Crespo‐leiro MG, Laroche C, Seferovic PM, Anker SD, Ferrari R, Ruschitzka F. Clinical phenotypes and outcome of patients hospitalized for acute heart failure: the ESC Heart Failure Long‐Term Registry. Eur J Heart Fail 2017; 19: 1242–1254. [DOI] [PubMed] [Google Scholar]
- 16. Ambardekar A, Thibodeau J, DeVore A, Kittleson M, Forde‐McLean R, Palardy M, Mountis MM, Cadaret L, Teuteberg JJ, Pamboukian SV, Xie R, Stevenson LW, Stewart GC. Discordant perceptions of prognosis and treatment options between physicians and patients with advanced heart failure HHS Public Access. JACC Heart Fail 2017; 5: 663–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lee DS, Schull MJ, Alter DA, Austin P, LAupacis A, Chong A, Tu JV, Stukel TA. Early deaths in patients with heart failure discharged from the emergency department a population‐based analysis. Circ Heart Fail 2010; 3: 228–235. [DOI] [PubMed] [Google Scholar]
- 18. Matsue Y, Damman K, Voors AA, Kagiyama N, Yamaguchi T, Kuroda S, Okumura T, Kida K, Mizuno A, Oishi S, Inuzuka Y, Akiyama E, Matsukawa R, Kato K, Suzuki S, Naruke T, Yoshioka K, Miyoshi T, Baba Y, Yamamoto M, Murai K, Mizutani K, Yoshida K, Kitai T. Time‐to‐furosemide treatment and mortality in patients hospitalized with acute heart failure. J Am Coll Cardiol 2017; 69: 3042–3051. [DOI] [PubMed] [Google Scholar]
- 19. Lee SE, Lee HY, Cho HJ, Choe WS, Kim H, Choi JO, Jeon ES, Kim MS, Kim JJ, Hwang KK, Chae SC, Baek SH, Kang SM, Choi DJ, Yoo BS, Kim KH, Park HY, Cho MC, Oh BH. Clinical characteristics and outcome of acute heart failure in Korea: results from the Korean acute heart failure registry (KorAHF). Korean Circ J 2017; 47: 341–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Supporting information.


