Abstract
A 25-year-old man with a venous malformation (VM) along the anterior and posterolateral aspects of the right chest wall presented with progressive enlargement of VM, chest wall pain, and physical disfigurement. Because of the complexity and size of the VM, a staged multidisciplinary team approach (ie, percutaneous embolization) followed by surgical resection and tissue-skin grafting was used. The percutaneous embolization was achieved with a combination of liquid embolic agents including n-butyl cyanoacrylate for the superficial cutaneous component and ethylene vinyl alcohol copolymer for the deeper subcutaneous component of the VM. Such a combination can achieve safe occlusion of the VM, facilitate surgical resection without blood loss, and contribute to a cosmetically desirable result.
Keywords: Venous malformation, Complex venous malformations, Preoperative embolization, Liquid embolic agent, Ethylene vinyl alcohol copolymer, EVOH, Onyx, n-Butyl cyanoacrylate, NBCA
Venous malformations (VMs) are the most common symptomatic vascular malformations.1 VMs typically grow in proportion to growth of the body, but accelerated progression can be seen with trauma or hormonal changes.2 Surgical excision has been the most effective treatment of localized VMs. Percutaneous embolization (PE) has been used to control symptoms and to reduce preoperative size of the VM. Based on a systematic review, various treatment options with variable success have been employed: ethanol, 74%; gelified ethanol, 89%; bleomycin, 88%; polidocanol, 90%; sodium tetradecyl sulfate, 86%; Ethibloc (Ethicon, Somerville, NJ), 65%; surgery, 90%; and laser therapy, 94%.3 To our knowledge, use of percutaneously (transcutaneously) injected liquid embolic agents such as ethylene vinyl alcohol copolymer (EVOH) for embolization of VMs has not been reported. We report a multidisciplinary team approach including PE with a combination of liquid embolic agents followed by surgical resection and tissue-skin grafting for the treatment of a large, complex VM for which previous PE with a gel sclerosant agent had failed because of inadvertent nontarget embolization. The patient consented to publication.
Case report
The patient is a 25-year-old man with progressive enlargement of a congenital VM along the anterior and posterolateral aspects of the right chest wall. He presented with complaints of new onset of right chest wall, axillary, and back pain associated with soft tissue disfigurement (Fig 1). The patient admitted that he was self-conscious about removing his shirt and was reluctant to do so even in the initial clinical visit. The patient had undergone a trial of percutaneous injection of a gel sclerosant agent in Europe. However, PE with the gel sclerosant agent was aborted because of the fluoroscopic movement of the agent into central veins.
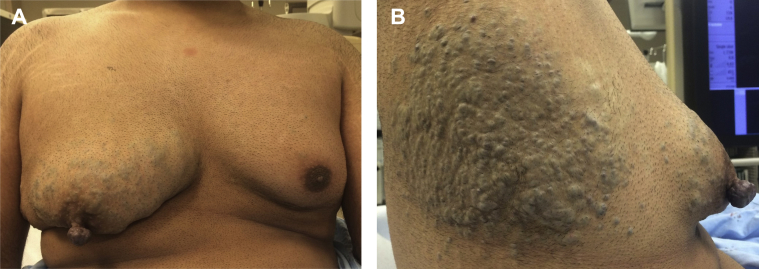
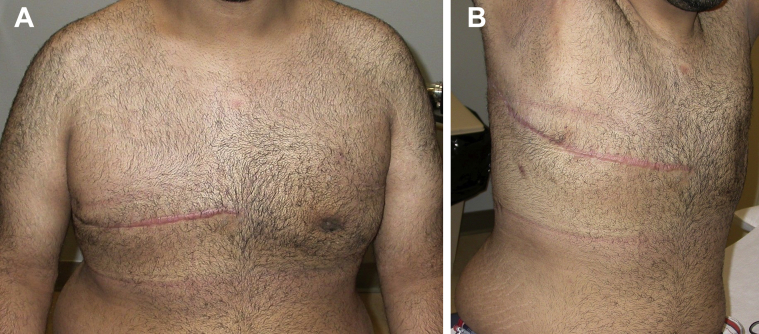
Fig 1.
Frontal (A) and side view (B) clinical photographs of the patient with a large venous malformation (VM) within the anterior and posterolateral aspects of right chest wall.
Because of the complexity and large size of this VM, a multidisciplinary team approach for treatment was used. This approach included PE of the VM in two stages using a combination of embolic agents, surgical resection on two occasions, and tissue and skin grafting as the final stage. The PE was carried out under monitored anesthesia care. Under ultrasound and fluoroscopy guidance, a 21-gauge micropuncture or butterfly needle was used to puncture the VM at multiple locations. A total of 10 mL of n-butyl cyanoacrylate (NBCA) 'glue' and ethiodized oil (Lipiodol; Guerbet, Princeton, NJ) in a 1:3 mixture was percutaneously injected into nine superficial sites within the VM around the nipple and retroareolar region. Deeper parts of the VM were then percutaneously embolized with 1.2 mL of EVOH (Onyx 34; Medtronic, Irvine, Calif; Fig 2). Before each injection, venograms were obtained to confirm an intravascular location of the needle tip. After injection, hemostasis was achieved with manual compression. A pressure dressing was then applied to compress the VM. On the next day, the patient underwent complete resection of the anterior component of the VM overlying the pectoralis muscle with minimal blood loss (Figs 3 and 4). The preoperative embolization allowed the identification of the extent of the VM.
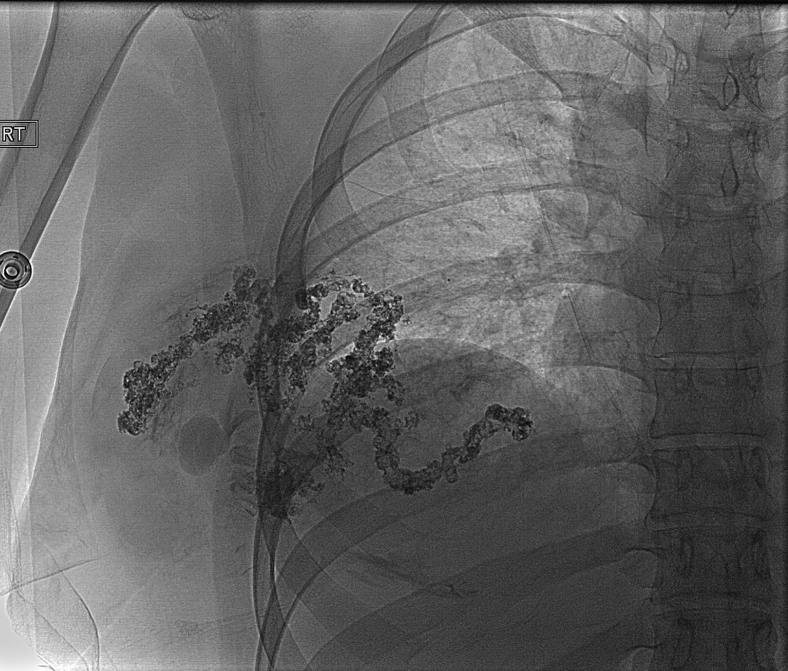
Fig 2.
Fluoroscopy image after embolization showing embolic agents (ie, n-butyl cyanoacrylate [NBCA] and ethylene vinyl alcohol copolymer [EVOH]) forming the venous lakes and cast of vessels within right anterior chest venous malformation (VM).
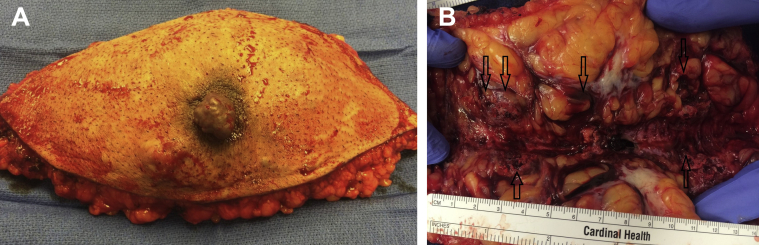
Fig 3.
A, Superficial aspect of mastectomy specimen showing absence of skin or superficial tissue discoloration or “tattooing” due to use of n-butyl cyanoacrylate (NBCA). B, Posterior aspect of mastectomy specimen showing black discoloration due to ethylene vinyl alcohol copolymer (EVOH) injection (arrows).
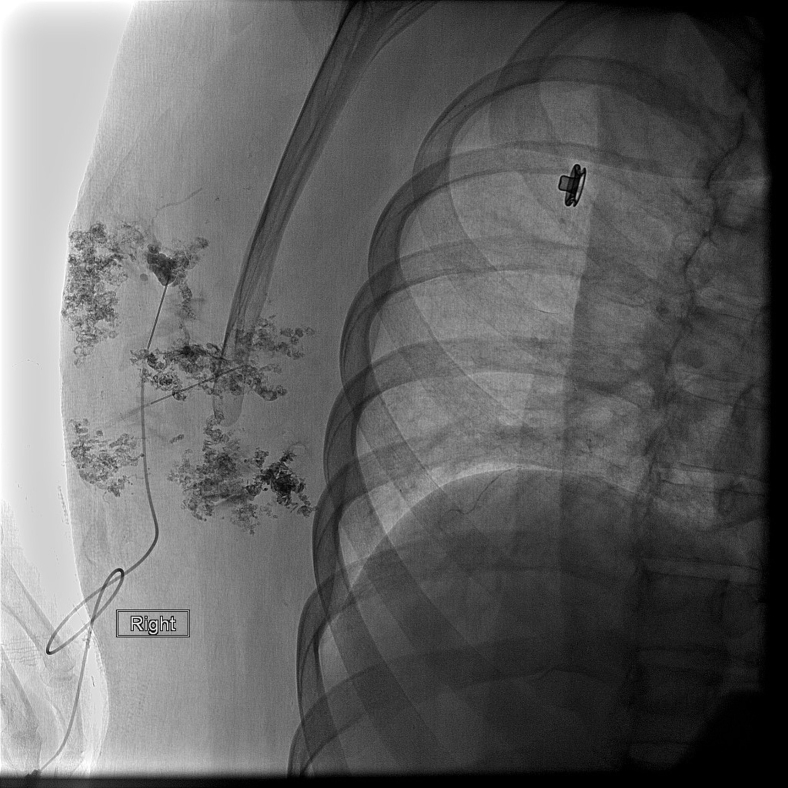
Fig 4.
Digital fluoroscopy spot image after percutaneous embolization (PE) of right posterolateral venous malformation (VM) demonstrating filling of venous lakes in the VM by embolic material.
Four months later, the patient presented for PE of the VM in the right axilla and the posterolateral chest wall. Similar to the earlier procedure, 10 mL of NBCA and Lipiodol (1:3) mixture was percutaneously injected into 15 superficial sites within the VM. Three deeper locations within the VM were embolized with 3 mL of EVOH (Onyx 18). Venography was performed before each injection to confirm the intravascular position of the needle tip. Venography performed after embolization confirmed the absence of contrast material filling the VM (Fig 4). On the next day, the patient underwent resection of the VM overlying the latissimus dorsi muscle. The large elliptical wound was primarily closed. The patient then underwent liposuction and glandular excision of the gynecomastia on the contralateral left side to preserve the symmetry of the chest wall. The patient tolerated the procedures well. On the 3-month follow-up clinical visit, the patient reported resolution of chest wall pain and was satisfied with the cosmetically desirable results (Fig 5).
Fig 5.
A and B, Frontal view clinical photographs of the patient's healed chest wall 3 months after second-stage venous malformation (VM) resection with liposuction-glandular excision of the gynecomastia on the left side and before reconstruction of the right nipple.
Discussion
In approaching the management of a large complex VM, PE with a combination of liquid embolic agents has been shown to be safe and effective in achieving occlusion of most VMs. The important parameters in the management of VM are its size, depth, and extent. The superficial simple VMs can be effectively excised. However, in performing surgical resection of deep complex VMs, ligation of vessels can be difficult. This can result in incomplete resection, inadequate hemostasis, and unwanted scarring. Hence, preoperative embolization is preferred to ease the surgical resection. To achieve safe and effective preoperative embolization, selection of an appropriate embolic agent is paramount. For PE of the superficial component of the VM, NBCA was chosen. NBCA was rendered radiopaque on fluoroscopy by the addition of Lipiodol. This allowed the operator to target the precise intravascular deposition of NBCA under fluoroscopy guidance. NBCA is a colorless, nonabsorbable liquid embolic agent that rapidly polymerizes on contact with blood and forms a mold of the vascular lumen, causing complete and irreversible occlusion. Because of its rapid polymerization, NBCA reduces the risk of nontarget embolization and also does not cause skin discoloration (“tattooing”), which would be cosmetically undesirable. The rationale for using NBCA over EVOH for PE of the superficial component of the VM was to prevent tattooing of superficial skin and tissue from the black pigment (tantalum powder) of EVOH. In the event that the VM could not have been completely resected and if EVOH were used for embolization of the superficial component, the residual skin and tissues would have been tattooed black.
For embolization of the deeper component of the VM, EVOH (Onyx) was used. Onyx is a nonabsorbable liquid embolic agent that is available as a combination of EVOH, dimethyl sulfoxide, and micronized tantalum powder. On contact with the blood, its slow solidification in a centripetal fashion allows slow, progressive, and controlled deployment within vessels of various sizes and shapes, resulting in occlusion. In addition, being a nonabsorbable agent, it also causes an irreversible occlusion of vessels.4, 5 The use of EVOH for PE of deeper components of the VM had the following advantages. Unlike NBCA, EVOH is a nonadhesive agent. It does not attach to vascular endothelium or the micropuncture needle tip, which allows its precise delivery within the deeper parts of the VM. After intravascular precipitation of EVOH, the deeper aspects of the VM retain soft sponge-like consistency. The use of EVOH embolization was shown to be superior for surgical resection of VMs compared with NBCA embolization.6 EVOH was shown to incur minimal intravascular or perivascular inflammatory reaction compared with NBCA.7,8 This facilitates safe surgical resection in the deeper planes. In this case, the black staining from EVOH delineated the junction between the VM and normal tissue, allowing surgeons to clearly identify the plane of resection. To avoid nontarget embolization, appropriate viscosity of EVOH was chosen. Onyx 34 (ie, more viscous EVOH) was used for PE of the deeper aspects of the anterior VM. This was done to avoid nontarget embolization to the central veins because during venography of the deeper anterior VM, contrast material was seen draining into central veins. Venography identified fewer draining veins of the posterolateral VM. Thus, less viscous EVOH (Onyx 18) was used to facilitate a thorough and deeper penetration of the VM.
Conclusions
PE with a combination of controllable liquid embolic agents, such as NBCA for the superficial component and EVOH for the deeper component of the VM, can be safe and effective to achieve occlusion of the VM. This in turn facilitates surgical resection with minimal blood loss and subsequent skin and tissue transfers, giving a more cosmetically desirable result.
Footnotes
Author conflict of interest: none.
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Enjolras O., Wassef M., Chapot R. Color atlas of vascular tumors and vascular malformations. Cambridge University Press; Cambridge: 2007. Introduction: ISSVA classification; pp. 1–12. [Google Scholar]
- 2.Hassanein A.H., Mulliken J.B., Fishman S.J., Alomari A.I., Zurakowski D., Greene A.K. Venous malformation: risk of progression during childhood and adolescence. Ann Plast Surg. 2011;68:98–201. doi: 10.1097/SAP.0b013e31821453c8. [DOI] [PubMed] [Google Scholar]
- 3.van der Vleuten C.J., Kater A., Wijnen M.H., Schultze Kool L.J., Rovers M.M. Effectiveness of sclerotherapy, surgery, and laser therapy in patients with venous malformations: a systematic review. Cardiovasc Intervent Radiol. 2014;37:977–989. doi: 10.1007/s00270-013-0764-2. [DOI] [PubMed] [Google Scholar]
- 4.Guimaraes M., Wooster M. Onyx (ethylene-vinyl alcohol copolymer) in peripheral applications. Semin Intervent Radiol. 2011;28:350–356. doi: 10.1055/s-0031-1284462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saeed Kilani M., Izaaryene J., Cohen F., Varoquaux A., Gaubert J.Y., Louis G. Ethylene vinyl alcohol copolymer (Onyx) in peripheral interventional radiology: indications, advantages and limitations. Diagn Interv Imaging. 2015;96:319–326. doi: 10.1016/j.diii.2014.11.030. [DOI] [PubMed] [Google Scholar]
- 6.Akin E.D., Perkins E., Ross I.B. Surgical handling characteristics of an ethylene vinyl alcohol copolymer compared with n-butyl cyanoacrylate used for embolization of vessels in an arteriovenous malformation resection model in swine. J Neurosurg. 2003;98:366–370. doi: 10.3171/jns.2003.98.2.0366. [DOI] [PubMed] [Google Scholar]
- 7.Murayama Y., Viñuela F., Ulhoa A., Akiba Y., Duckwiler G.R., Gobin Y.P. Nonadhesive liquid embolic agent for cerebral arteriovenous malformations: preliminary histopathological studies in swine rete mirabile. Neurosurgery. 1998;43:1164–1175. doi: 10.1097/00006123-199811000-00081. [DOI] [PubMed] [Google Scholar]
- 8.Duffner F., Ritz R., Bornemann A., Freudenstein D., Wiendl H., Siekmann R. Combined therapy of cerebral arteriovenous malformations: histological differences between a non-adhesive liquid embolic agent and n-butyl 2-cyanoacrylate (NBCA) Clin Neuropathol. 2002;21:13–17. [PubMed] [Google Scholar]