Abstract
Background & Aims
Inflammation plays an important role in the pathogenesis of cholestatic liver injury, but it is unclear whether the inflammasome is involved and is the objective of this study.
Methods
Gene expression was analyzed in the livers of patients with primary biliary cholangitis (n = 15) and primary sclerosing cholangitis (n = 15). Bile duct ligation (BDL) or sham operation was performed in wild-type (WT) and Caspase-1–/– (Casp1–/–) mice for 7 days. Mouse hepatocytes and macrophages were treated with bile acids.
Results
Caspase-1, NLRP1, NLRP3 and IL-1β were significantly increased in the livers of cholestatic patients when compared to healthy control subjects (n = 9). Significantly higher levels of plasma IL-1β (826 vs 345 pg/ml), ALT (674 vs 482 U/L) and ALP (900 vs 622 U/L) were seen in WT BDL mice compared to Casp1–/– BDL mice. Caspase-1 cleavage was found only in WT BDL livers. Assessment of liver histology indicated more fibrosis in Casp1–/– BDL mice than in WT BDL mice, confirmed by analyses of liver hydroxyproline content and the expression of fibrotic genes. Profiling of immune cells revealed that there were more macrophages in Casp1–/– BDL livers than in WT BDL livers. Further macrophage phenotype characterization indicated that Casp1–/– BDL livers had more M2 anti-inflammatory macrophages evidenced by more CD206 positive cells and higher expression of IL-4, CD163, Fizz1 and IL-33. When mouse hepatocytes and peritoneal macrophages were exposed to cholestatic levels of major endogenous bile acids (300μM TCA), neither IL-1β induction nor procaspase-1 cleavage were detected.
Conclusions
The inflammasome exacerbates cholestatic liver injury, but bile acids do not directly activate the inflammasome.
Keywords: Cholestasis, Bile Acids, Inflammation, Liver Injury
Abbreviations used in this paper: ALP, alkaline phosphatase; ALT, alanine aminotransferase; ATP, adenosine triphosphate; BDL, bile duct ligated/ligation; LPS, lipopolysaccharide; mRNA, messenger RNA; NASH, nonalcoholic steatohepatitis; PBC, primary biliary cholangitis; PSC, primary sclerosing cholangitis; TCA, taurocholic acid; WT, wild-type
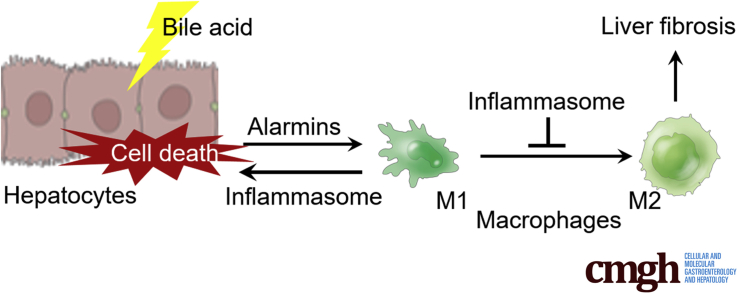
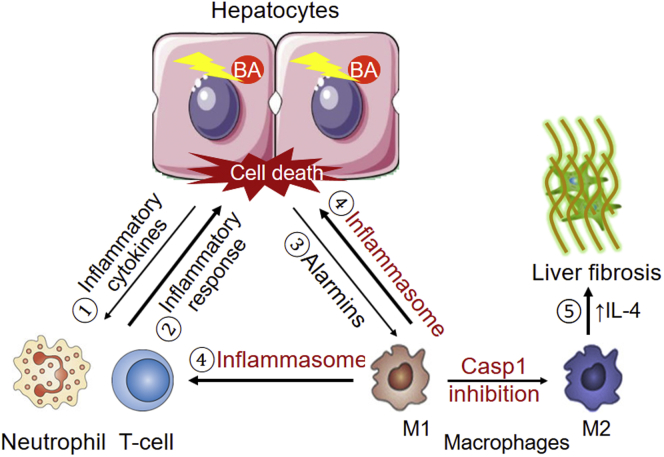
Graphical abstract
Summary.
The inflammasome exacerbates cholestatic liver injury independent of the effects of bile acids. Blocking the inflammasome (presumably in macrophages) paradoxically increases fibrosis in cholestatic mouse liver by promoting an anti-inflammatory M2 phenotype.
Cholestasis is a syndrome in which bile flow is impaired, leading to the accumulation of bile acid and numerous other endogenous and exogenous metabolites and toxins in the liver, as well as systemic circulation, and results in liver injury. Recent studies indicate that inflammation plays an important role in the pathogenesis of cholestatic liver injury, in which bile acid–induced production of inflammatory cytokines in hepatocytes may initiate this event.1,2 However, it is not clear whether the inflammasome plays a role in this process. The inflammasome is a cytosolic protein complex that senses intracellular danger stimuli. When activated, a nod-like receptor (e.g. NLRP3) activates caspase-1 by cleaving pro-caspase-1 protein. Activated caspase-1 then cleaves pro-IL-1β and pro-IL-18, releasing these cytokines from the cell and amplifying the inflammatory response.3 Proteins that comprise the inflammasome are prominently expressed in macrophages or Kupffer cells but are less abundant in liver parenchymal cells. Recent studies indicate that the inflammasome is involved in the pathogenesis of alcoholic hepatitis, nonalcoholic steatohepatitis (NASH), hepatitis C virus infection, and acetaminophen toxicity.4,5 However, the literature is conflicted as to whether bile acids can activate the inflammasome, and it is not known whether the inflammasome plays any role in cholestatic liver injury. Using mouse macrophages, Guo et al6 found that bile acids inhibited Nlrp3 inflammasome activation, whereas another report indicated that bile acids activated Nlrp3 inflammasome in mouse macrophages.7 However, it must be stressed that the cells in all of these studies were treated with bile acids that either were not the major endogenous bile acid in mouse or used concentrations that were not physiologically or pathophysiologically relevant. Nevertheless, the Nlrp3 inflammasome could be activated in liver tissue in a mouse model of lithocholic acid induced cholestasis,8 while elevated messenger RNA (mRNA) expression of IL1R1, NLRP3, and caspase-1 was also observed in the liver of patients with biliary atresia.9 Loss of Il-1r1 or Nlrp3, but not of the Caspase-1 gene, reduced bile duct injury in a mouse model of biliary atresia induced by rotavirus infection.9 However, none of these studies addressed the role of bile acids in inflammasome activation under cholestatic conditions. Therefore, it remains uncertain whether bile acids directly activate the inflammasome or whether the inflammasome is associated with other forms of cholestatic liver diseases, such as primary biliary cholangitis (PBC) and primary sclerosing cholangitis (PSC).
In this report, we analyzed the expression of inflammasome genes in the livers of patients with PBC and PSC, and examined the functional role of the inflammasome in cholestatic liver injury in vivo using bile duct–ligated (BDL) wild-type (WT) and Caspase-1–/– (Casp1–/–) mice and in vitro in primary mouse hepatocyte and macrophage cultures. Our results support a role for the inflammasome in cholestatic liver injury (most likely from macrophages but not from hepatocytes) but suggest that endogenous bile acids do not directly activate the inflammasome. Inflammasome deficiency (Casp1–/– mice) reduced hepatocyte injury after BDL by promoting anti-inflammatory M2 macrophages in the liver, where liver fibrosis was increased.
Results
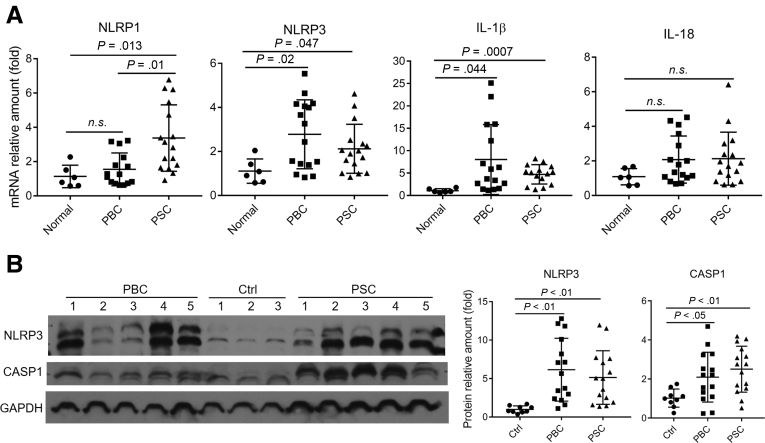
Hepatic Expression of Inflammasome Genes Is Increased in Patients With PBC and PSC
As demonstrated in Figure 1A, hepatic levels of both NLRP3 and IL-1β mRNA were significantly higher in PBC and PSC than in healthy control subjects. Hepatic NLRP1 mRNA was also increased in PSC but not PBC patients, whereas no significant difference was seen in IL-18 mRNA expression for either patient group. Western blot analysis further confirmed that the protein expression of NLRP3 and caspase-1 was increased in these cholestatic liver tissues when compared with the healthy control subjects (Figure 1B). Previous reports have shown that serum IL-1β levels are increased in patients with PBC and PSC.10,11 Together, these findings suggest that the inflammasome plays a role in the pathogenesis of human cholestatic liver injury.
Figure 1.
Elevated expression of inflammasome genes in the livers of patients with cholestatic liver diseases. (A) Hepatic mRNA expression of NLRP1, NLRP3, IL-1β, and IL-18. (B) Quantitative analysis of NLRP3 and caspase-1 protein expression by Western blots. For PBC, n = 15; for PSC, n = 15; for healthy controls (Ctrl), n = 6–9. n.s., not significant.
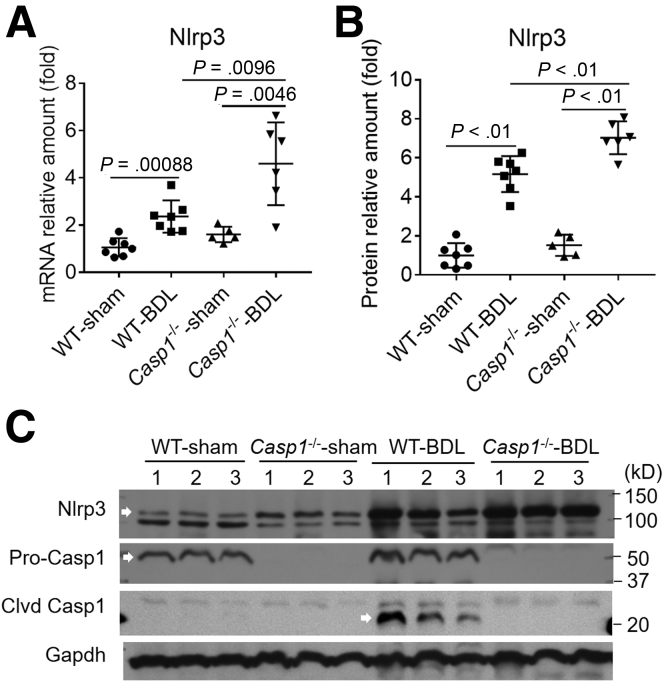
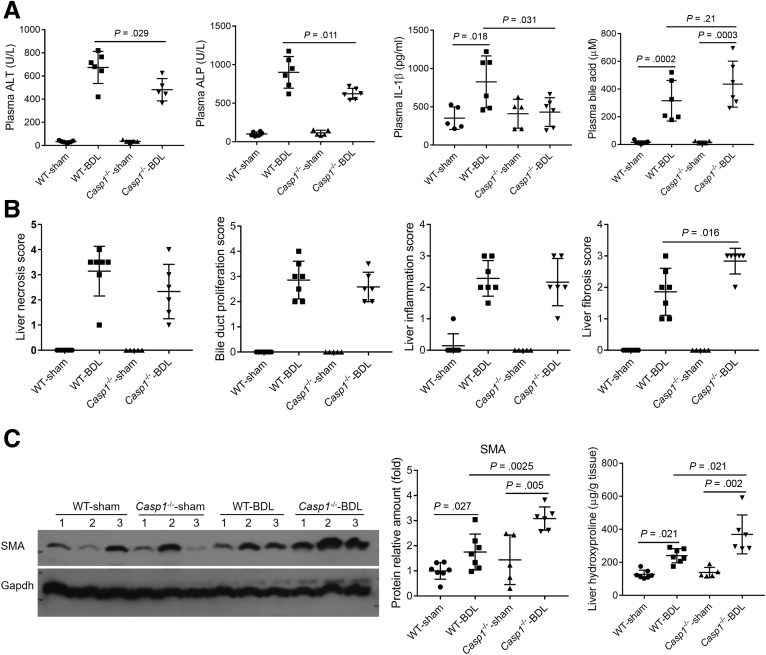
Absence of the Inflammasome Diminishes Hepatic Injury but Promotes Liver Fibrosis in BDL Mice
To examine the functional role of the inflammasome in cholestatic liver injury, we performed BDL in both WT and Casp1–/– mice for 7 days. As demonstrated in Figure 2A, Nlrp3 RNA expression was increased in both WT and Casp1–/– BDL livers when compared with the sham control subjects. However, cleaved caspase-1 (20 kD) was found only in WT BDL livers (Figure 2B), indicating that the inflammasome was activated only in the WT cholestatic mice. Deficiency of Caspase-1 protein (both pro and cleaved forms) in Casp1–/– livers confirmed that the inflammasome was not activated in these mice. After BDL for 7 days, plasma levels of liver enzymes alanine aminotransferase (ALT) and alkaline phosphatase (ALP) were significantly lower in the Casp1–/– mice than in the WT BDL group (Figure 3A). Plasma IL-1β was elevated in WT mice but not in Casp1–/– mice after BDL. In contrast, bile acid levels in both plasma (Figure 3A) and liver, while elevated after BDL compared with the sham control subjects, were not different between the Casp1–/– and WT mice 7 days after BDL (data not shown).
Figure 2.
Increased (A) mRNA and (B) protein expression of Nlrp3 in the livers of both WT and Casp1–/–mice, and (C) cleavage of caspase-1 (arrow) in WT BDL livers. Both mRNA and protein expression levels were normalized to GAPDH, data are presented as mean ± SD. Clvd, cleaved.
Figure 3.
Deficiency of caspase-1 improved liver function tests but increased liver fibrosis after 7 days of BDL in mice (WT sham, n = 7; WT BDL, n = 7; Casp1–/–sham, n = 5; Casp1–/–BDL, n = 6). (A) Plasma levels of ALT, ALP, IL-1β, and bile acid, and bile acid levels in livers. (B) Hematoxylin and eosin histology assessment (scores) of liver necrosis, fibrosis, inflammation, and bile duct proliferation. (C) Biochemical analysis of liver hydroxyproline content and Western blot analysis of smooth muscle actin (SMA) protein expression. GAPDH was used as loading control and data normalization, data presented as mean ± SD.
Blinded assessment of liver hematoxylin and eosin histology did not reveal significant differences in necrosis, bile duct proliferation, or inflammatory infiltrates between the 2 groups 7 days after BDL, while paradoxically, hepatic fibrosis was increased in the Casp1–/– mice (Figure 3B). This later finding was confirmed by Sirius staining of liver sections, measurements of hepatic hydroxyproline content and Western blot of smooth muscle actin protein in the Casp1–/– liver after BDL (Figure 3C). Together, these findings indicate that while the inflammasome may be activated in cholestatic liver, its absence reduced hepatic injury to some degree but increased liver fibrosis.
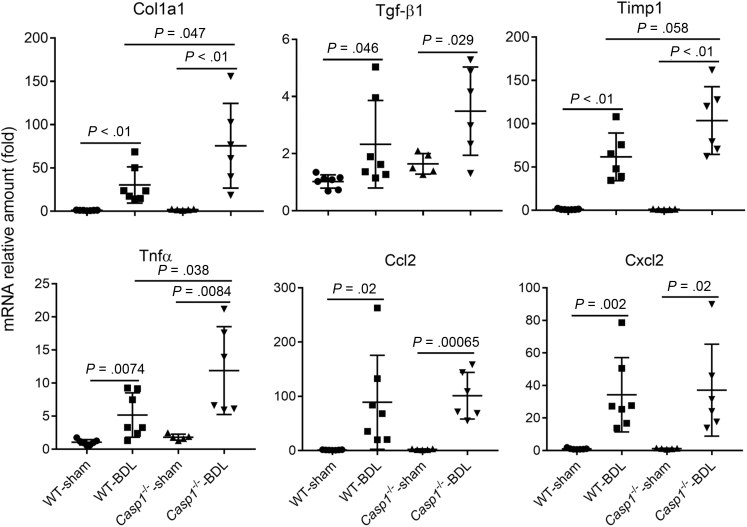
Loss of Inflammasome Activity Promotes the M2 Phenotype of Macrophages in the Cholestatic Liver
To gain insights into the nature of the pathogenic role of the inflammasome in cholestatic liver, we analyzed the hepatic expression of additional genes involved in inflammation, fibrosis, and bile acid homeostasis. As shown in Figure 4, while BDL led to marked increases of Col1a1, Tgf-β1, and Timp1 mRNA expression in both WT and Casp1–/– livers, the increases of Col1a1 and Tnfα in Casp1–/– mice were significantly higher than in WT BDL group, confirming an increase in fibrotic activity in Casp1–/– BDL liver. However, hepatic mRNA expression of genes involved in maintaining bile acid homeostasis were not substantially different between WT and Casp1–/– groups after BDL. These include the nuclear receptors Fxr/Nr1h4 and Shp/Nr0b2; bile acid transporters Ntcp/Slc10a1, Ostα/Slc51a, Bsep/Abcb11, and Mrp2/Abcc2; and the bile acid synthesis enzyme Cyp7a1. Also no differences were seen in the mRNA level of Il-1β, Ccl2, and Cxcl2 mRNA between these 2 groups, either (Figure 4 and data not shown).
Figure 4.
Increased hepatic mRNA expression of Col1a1, Tgf-β1, Timp1, and Tnfα in Casp1–/–mouse livers after 7 days of BDL (WT sham, n = 7; WT BDL, n = 7; Casp1–/–sham, n = 5; Casp1–/–BDL, n = 6). Data presented as mean ± SD. No differences were seen for Ccl2 and Cxcl2 expression between the 2 groups.
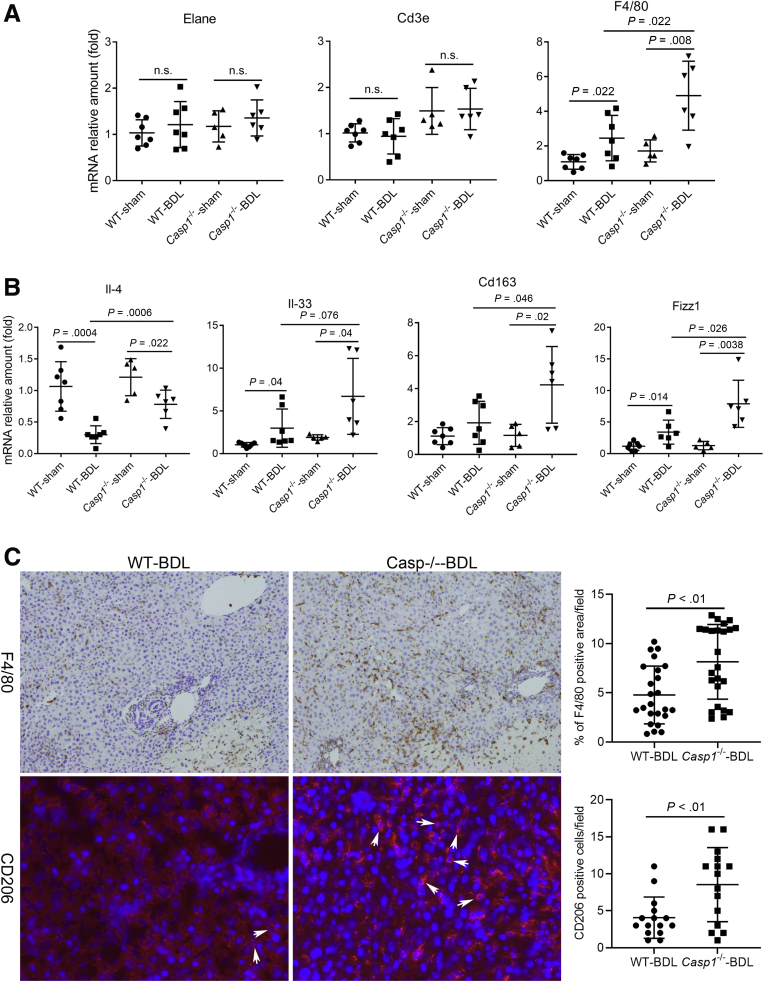
To determine whether loss of the inflammasome altered the profile of hepatic immune cells, we first measured the mRNA expression of cell type–specific marker genes (ie, Elane for neutrophil, Cd3e for T cells, and F4/80 for macrophages). While there were no differences in Elane and Cd3e expression between WT and Casp1–/– groups after 7 days BDL, Casp1–/– BDL livers had significantly higher amounts of F4/80 than was detected in the WT BDL livers (Figure 5A), indicating that there were more macrophage/Kupffer cells in the absence of inflammasome activation. To confirm this observation, we performed immunohistochemistry of liver sections from WT and Casp1–/– BDL livers. As shown in Figure 5B, there were more F4/80 positive areas in Casp1–/– livers than WT livers after BDL. To further characterize the hepatic macrophage or Kupffer cell phenotype in these mice, we analyzed the mRNA expression of markers that differentiate between pro- and anti-inflammatory types (ie, M1 and M2, respectively), including Arginase 1, Il-4, Il-33, Cd163, Fizz1, and Ym-1. We found that BDL resulted in a significant decrease in expression of the anti-inflammatory cytokine Il-4. However, this decrease was significantly less in Casp1–/– BDL liver than in WT BDL livers (Figure 5A), suggesting there were more anti-inflammatory M2-type macrophages in the Casp1–/– BDL livers. Higher expression levels of other M2-type macrophage markers (ie, Cd163, Il-33, and Fizz1) were also found in Casp1–/– BDL livers than in WT BDL livers, consistent with a higher number of M2 macrophages in the former (Figure 5A). There were no differences in arginase-1 mRNA expression among the 4 groups, presumably because arginase-1 is normally abundantly expressed in hepatocytes. Immunofluorescent labeling of hepatic CD206 (another M2 macrophage marker) further confirmed that there were more M2 macrophages in Casp1–/– BDL livers than in WT BDL livers (Figure 5B). Together, these findings suggest that the normal function of inflammasome activation is proinflammatory (as seen in WT BDL mice) but that in the absence of inflammasome activation, there is a partial conversion from a proinflammatory to an anti-inflammatory environment with respect to the macrophage phenotype (as seen in the Casp1–/– BDL livers).
Figure 5.
M2 macrophages were increased in Casp1–/–BDL mouse livers. (A) Cell type–specific gene mRNA expression. Elane for neutrophils, Cd3e for T cells, F4/80 for macrophages. (B) mRNA expression of macrophages M1 and M2 phenotype gene markers (WT sham, n = 7; WT BDL, n = 7; Casp1–/– sham, n = 5; Casp1–/– BDL, n = 6). Data presented as mean ± SD. (C) Representative images of immunohistochemistry staining of F4/80 (top, 100×) and immunofluorescent labeling of CD206 (bottom, 200×) of liver sections from BDL WT and Casp1–/– mice and their quantitative assessments of randomly selected microscopic fields. For F4/80, 6 images/section were acquired from randomly selected 4 animals in each group. For CD206, 5 images/section were acquired from randomly selected 3 animals in each group. The typical CD206/positive cells were indicated by the white arrows. n.s., not significant.
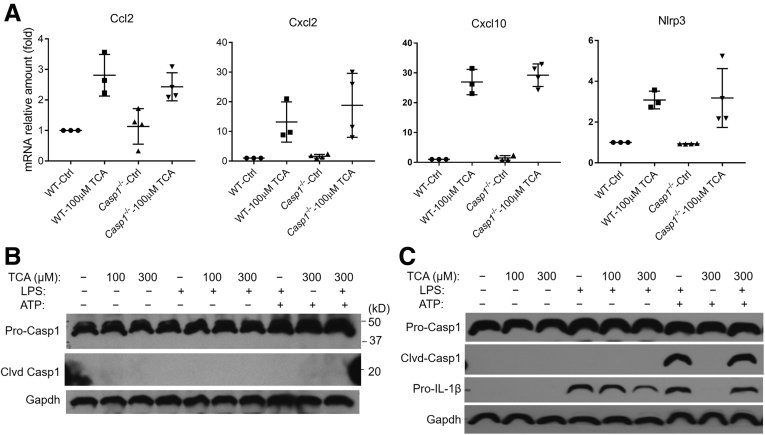
Bile Acids Do Not Activate the Inflammasome in Hepatocytes or in Macrophages
To investigate whether bile acids can activate the inflammasome, we isolated hepatic parenchymal cells and peritoneal macrophages from the mice. When hepatocytes were treated with 100 μM taurocholic acid (TCA) (the major endogenous bile acid in mice) for 24 hours, mRNA expression of chemokines Ccl2, Cxcl2, and Cxcl10 was markedly increased, as previously reported (Figure 6A),1,2 but Il-1β mRNA expression remained undetectable in these cells. Deficiency of caspase-1 did not alter TCA induction of Ccl2, Cxcl2, Cxcl10, and Nlrp3 in these mouse hepatocytes (Figure 6A). In addition, Western blot analysis did not detect any cleavage of caspase-1 when WT mouse hepatocytes were exposed to TCA (up to 300 μM, the high end of pathophysiologically relevant concentrations) or lipopolysaccharide (LPS) and adenosine triphosphate (ATP) for 16 hours (Figure 6B), indicating that the inflammasome was not activated in hepatocytes by these measures. Furthermore, glycocholic acid 50 μM, another major endogenous bile acid- and tauroursodeoxycholic acid (100 μM) treatments also did not cause pro-caspase-1 cleavage in these mouse hepatocytes. In contrast, increased pro-Il-1β protein expression and pro-caspase-1 cleavage were found in mouse macrophage cultures that were exposed to LPS and ATP, an indication of inflammasome activation in these cells (as a positive control). However, TCA treatment alone or in combination with LPS and ATP increased neither pro-Il-1β protein expression nor caspase-1 cleavage (Figure 6C).
Figure 6.
Bile acids did not activate the inflammasome in cultured mouse primary cells of either hepatocytes or peritoneal macrophages. (A) Bile acids increased mRNA expression of Nlrp3 and inflammatory chemokines Ccl2, Cxcl2, and Cxcl10 independent of the inflammasome in mouse hepatocytes (24-hour treatment) (n = 3–4). (B) Western blot analysis demonstrates that bile acids did not cause pro-caspase 1 cleavage/activation in mouse primary hepatocytes. (C) Western blot detected inflammasome activation in mouse macrophages (pro-caspase-1 cleavage and increased pro-IL-1β protein expression) after LPS + ATP treatment, but bile acids did not have such an effect. Of note, both hepatocytes and macrophages were treated with culture (Ctrl) medium, TCA, or LPS (1 μg/mL) for 16 hours, and were chased with ATP (5 mM) for 30 minutes. Clvd, cleaved.
Discussion
In this report, we examined the role of the inflammasome in cholestatic liver injury in humans and mice and determined whether bile acids can activate the inflammasome in hepatocytes and macrophages under cholestatic conditions. We found that (1) hepatic expression of the inflammasome genes NLRP1, NLPR3, caspase-1, and IL-1β (mRNA and or protein) were increased in cholestatic patients with PBC or PSC (Figure 1); (2) increased expression and activation of inflammasome genes were also seen in cholestatic mouse livers after BDL (Figure 2); (3) lack of inflammasome activation in mice reduced markers of cholestatic hepatic injury (ALT and ALP) but increased liver fibrosis after BDL (Figures 3 and 4); (4) deficiency of caspase-1 in mice also promoted an increase of the M2 macrophages phenotype in the liver after BDL, thus presumably partially converting a proinflammatory phenotype to an anti-inflammatory state (Figure 5); and (5) at pathophysiological concentrations, the major endogenous bile acid TCA did not activate the inflammasome in mouse hepatocytes or macrophages (Figure 6). Therefore, we conclude that while the inflammasome is activated in cholestatic liver and contributes to the injury, this activation does not appear to occur through the direct action of bile acids. It is likely that this activation involves the macrophage rather than the hepatocyte in the liver.
The role of the inflammasome in the pathogenesis of different diseases has often been conflicting. Inflammasome signaling has been reported to protect the liver from hepatic tumor growth, virus infection and to increase survival rates in response to a hepatic parasitic load (Trypanosoma cruzi) in mice.5,12, 13, 14 In contrast, the inflammasome contributes to the pathogenesis of alcoholic liver disease and NASH.4,15 In the present study, we found that the inflammasome is indeed activated in cholestatic livers and that loss of inflammasome activation in mice reduces acute manifestations of hepatic injury (ALT and ALP) without significant alterations in liver necrosis, bile duct proliferation, or gross estimates of inflammation, while paradoxically enhancing liver fibrosis. If fibrogenesis is considered as part of the process of tissue healing following an inflammatory injury, we may conclude that deactivation of the inflammasome in cholestasis blocks its proinflammatory properties, suggesting that when active, its role would be more consistent with that seen in other liver disorders such as alcoholic liver disease and NASH.4 This hypothesis is consistent with the increase of the M2-type macrophages in the liver of the Casp1–/– BDL mice, as reflected by the higher expression of its marker genes such as Il-4, Il-33, Cd163, Fizz1, and CD206 (Figure 5). The increase in Il-4 is known to lead to stimulation of Tgf-β1 expression, a classic profibrotic cytokine.16, 17, 18 This would explain why fibrosis was increased in Casp1–/– BDL livers, as illustrated in Figure 7. The reduced hepatic injury seen in Casp1–/– BDL mice (absence of the inflammasome) is also consistent with several earlier reports in which depletion of macrophages attenuated liver injury in rodent models of cholestasis.19, 20, 21, 22
Figure 7.
A proposed functional role of macrophages/Kupffer cells mediated activation of the inflammasome in cholestatic liver injury. ① Bile acid (BA) stressed hepatocytes produce inflammatory cytokines that ② trigger neutrophil and T cell–mediated inflammatory response and result in hepatocyte death (previous studies). ③ Dead hepatocytes release alarmins that activate the inflammasome in macrophages/Kupffer cells, orchestrating an immune response that ④ contributes further to the hepatocyte injury. Inactivation of the inflammasome promotes anti-inflammatory M2 macrophage and ⑤ stimulate IL-4 expression, which results in increased fibrosis.
Recent studies indicate that elevated hepatic levels of bile acids can initiate an inflammatory response by stimulating cytokine expression in hepatocytes.1,2 Thus, it is reasonable to speculate that bile acids might activate the inflammasome in the cholestatic liver. However, our findings do not support this hypothesis and indicate that bile acids do not directly activate the inflammasome in hepatocytes or macrophages or Kupffer cells at concentrations that are pathophysiologically relevant. Previous studies that have supported this hypothesis have used hydrophobic bile acid species such as chenodeoxycholic acid and lithocholic acid at high concentrations that are not seen in cholestatic patients or animal models and thus are likely to be artifacts of these in vitro conditions.7,8,23 The major species of endogenous bile acids are conjugated bile acids that require bile acid transport proteins to enter cells. These transporters are only seen in hepatic parenchymal cells and are absent in macrophages and other hepatic cells. Unconjugated bile acids can diffuse into cells but never reach pathophysiologic levels.24 While the mechanism by which the inflammasome is activated in cholestatic liver remains to be determined, we speculate that it is related to the well-described inflammatory response generated from the hepatocyte that is induced by the hepatic retention of bile acids.1,2,25 When hepatic parenchymal cells undergo necrosis during cholestasis, alarmins (eg, ATP and other damage-associated molecular patterns) are released from the dying cells and would trigger the activation of the inflammasome in hepatic macrophages or Kupffer cells and orchestrate an immune response that contributes to liver injury,22 as shown in Figure 7.
In summary, we found that inflammasome plays a role in cholestatic liver injury but that bile acids do not directly activate the inflammasome. Based on these findings, we speculate that the activation of the inflammasome in cholestasis is secondary to bile acid–induced inflammatory injury and that the site of this activation is the macrophage.
Materials and Methods
Materials
Chemicals were purchased from Sigma-Aldrich (St. Louis, MO), except where otherwise specified. Cell culture media (Williams’ E and Dulbecco’s modified Eagle medium), heat-inactivated fetal bovine serum, penicillin or streptomycin, trypsin, phosphate-buffered saline, and enhanced chemiluminescence reagents were obtained from ThermoFisher Scientific (Waltham, MA). Mouse IL-1β protein quantification enzyme-linked immunosorbent assay (ELISA) kits were purchased from R&D Systems (Minneapolis, MN).
Animals
All animal studies were reviewed and approved by the board of the Institutional Animal Care and Use Committee of Yale University. Whole-body gene knockout of Casp1–/– mice was on a C57Bl/6 background and described in previous publications.26,27 Wild-type C57Bl/6 mice were purchased from the Jackson Laboratory (Bar Harbor, ME). The animals were kept in a pathogen-free environment on a controlled 12-hour light/dark regime in the animal facility of Yale University. Bile duct ligation or sham operation were performed in 8- to 10-week-old mice for 7 days as previously described.2 After overnight fasting, mice were sacrificed. Plasma and liver were collected. For biochemical and molecular biology analyses, the tissues were snap-frozen in liquid nitrogen and stored at –80°C. For histological assessment, liver sections were fixed in 4% formalin and embedded in paraffin.
Mouse Hepatocyte and Macrophage Preparation and Treatment
Both hepatocytes and nonparenchymal cells were isolated from 10- to 20-week-old mice using collagenase perfusion as described.28 Hepatocytes were maintained in collagen sandwich culture to closely resemble in vivo conditions. Mouse peritoneal macrophages were isolated as previously described16 and maintained in Dulbecco’s modified Eagle medium containing 10% fetal bovine serum. All cell cultures were treated with indicated chemicals and collected within 96 hours after isolation.
Human Liver Tissue
Liver specimens were acquired from the Liver Tissue Cell Distribution System at the University of Minnesota (funded by National Institutes of Health Contract # HSN276201200017C). This included 9 normal healthy control subjects (deceased donors whose liver was not suitable for transplant), and 15 PBC and 15 PSC patients who underwent liver transplant.
Tissue Biochemistry, Liver Histology, Immunohistochemistry and Immunofluorescent Labeling
Plasma levels of liver enzymes, IL-1β and bile acids were assayed as described.29 Formalin-fixed liver tissue (the 3- to 4-mm-thick middle portion of the largest lobe in each animal) was paraffin embedded and sections were stained with hematoxylin and eosin. Liver sections were also stained with Sirius Red for fibrosis evaluation. Liver histology was blindly assessed for, necrosis, bile duct proliferation, fibrosis and inflammation on a 1 to 4+ scale. Immunohistochemistry staining and immunofluorescent labeling of liver sections were performed as previously described.30 Specifically, for immunohistochemistry staining of F4/80, a monoclonal antibody against mouse F4/80 (Cat# 70076, from Cell Signaling Technology [Danvers, MA], 1:200 dilution) was used to probe deparaffined sections from 4 randomly selected animals in each BDL group. Six images were randomly taken across the section under 100× magnification using an Olympus (Olympus Corp, Japan) BX51 microscope. ImageJ 1.51n software (National Institutes of Health, Bethesda, MD) was used to calculate the positive-signal area. For immunofluorescent labeling of CD206, a monoclonal antibody (Cat# MCA2235T, from Bio-Rad [Hercules, CA], 1:100 dilution) was incubated with frozen liver section from 3 randomly selected animals in each BDL groups. Five images were randomly taken across the section under 200× magnification using an Zeiss (Carl Zeiss Microscopy, LLC, White Plains, NY) Fluorescent microscope. The count of CD206 positive cells in each image field was assessed in a blinded fashion. Liver hydroxyproline content was assayed as previously described.30
mRNA and Protein Expression
Tissue RNA and protein were extracted and assayed as described.2 The primer or probe sets for TaqMan assay were purchased from ThermoFisher Scientific. Antibodies against α-Sma and GAPDH for Western blotting were from Sigma-Aldrich. Antibodies against mouse caspase-1 (AdipoGen Life Sciences [San Diego, CA], Cat# AG-20B-0042-C100), NLRP3 (AdipoGen Life Sciences, Cat# AG-20B-0014-C100), IL-1β (R&D Systems, Cat# MAB401), and human caspase-1 (Cell Signaling Technology, Cat# 3866) were purchased from indicated vendors and used at 1:1000 dilution in 4% bovine serum albumin. Both quantitative polymerase chain reaction and Western blot data were normalized to the corresponding levels of GAPDH.
Statistical Analysis
Data are presented as means ± SD. Differences between experimental groups were assessed for significance using 1-way analysis of variance. Two-tailed Student t test was used to calculate the P value. A P value of <.05 was considered statistically significant.
Acknowledgments
The authors are grateful to Kathy Harry and Dr. Paula Vieira Teixeira Vidigal for excellent technical support.
Footnotes
Author contributions Study concept and design: SYC, JLB, XO; Acquisition of data: SYC, MG, AM, JLB; Analysis and interpretation of data: SYC, JLB, XO; Drafting of the manuscript: SYC, JLB; Material support: RH.
Conflicts of interest The authors disclose no conflicts.
Funding This study was supported by National Institutes of Health Grant No. DK34989 (Yale Liver Center), Grant No. DK25636 (to James L. Boyer), and Pilot Grant No. P30 DK-034989 (to Xinshou Ouyang).
Contributor Information
Shi-Ying Cai, Email: shi-ying.cai@yale.edu.
James L. Boyer, Email: james.boyer@yale.edu.
References
- 1.Allen K., Jaeschke H., Copple B.L. Bile acids induce inflammatory genes in hepatocytes: a novel mechanism of inflammation during obstructive cholestasis. Am J Pathol. 2011;178:175–186. doi: 10.1016/j.ajpath.2010.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cai S.Y., Ouyang X., Chen Y., Soroka C.J., Wang J., Mennone A., Wang Y., Mehal W.Z., Jain D., Boyer J.L. Bile acids initiate cholestatic liver injury by triggering a hepatocyte-specific inflammatory response. JCI Insight. 2017;2 doi: 10.1172/jci.insight.90780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Horvath G.L., Schrum J.E., De Nardo C.M., Latz E. Intracellular sensing of microbes and danger signals by the inflammasomes. Immunol Rev. 2011;243:119–135. doi: 10.1111/j.1600-065X.2011.01050.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Szabo G., Petrasek J. Inflammasome activation and function in liver disease. Nat Rev Gastroenterol Hepatol. 2015;12:387–400. doi: 10.1038/nrgastro.2015.94. [DOI] [PubMed] [Google Scholar]
- 5.Luan J., Ju D. Inflammasome: a double-edged sword in liver diseases. Front Immunol. 2018;9:2201. doi: 10.3389/fimmu.2018.02201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guo C., Xie S., Chi Z., Zhang J., Liu Y., Zhang L., Zheng M., Zhang X., Xia D., Ke Y., Lu L., Wang D. Bile acids control inflammation and metabolic disorder through inhibition of NLRP3 inflammasome. Immunity. 2016;45:802–816. doi: 10.1016/j.immuni.2016.09.008. [DOI] [PubMed] [Google Scholar]
- 7.Hao H., Cao L., Jiang C., Che Y., Zhang S., Takahashi S., Wang G., Gonzalez F.J. Farnesoid X receptor regulation of the NLRP3 inflammasome underlies cholestasis-associated sepsis. Cell Metab. 2017;25:856–867. doi: 10.1016/j.cmet.2017.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.El-Agamy D.S., Almaramhy H.H., Ahmed N., Bojan B., Alrohily W.D., Elkablawy M.A. Anti-inflammatory effects of vardenafil against cholestatic liver damage in mice: a mechanistic study. Cell Physiol Biochem. 2018;47:523–534. doi: 10.1159/000489986. [DOI] [PubMed] [Google Scholar]
- 9.Yang L., Mizuochi T., Shivakumar P., Mourya R., Luo Z., Gutta S., Bezerra J.A. Regulation of epithelial injury and bile duct obstruction by NLRP3, IL-1R1 in experimental biliary atresia. J Hepatol. 2018;69:1136–1144. doi: 10.1016/j.jhep.2018.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barak V., Selmi C., Schlesinger M., Blank M., Agmon-Levin N., Kalickman I., Gershwin M.E., Shoenfeld Y. Serum inflammatory cytokines, complement components, and soluble interleukin 2 receptor in primary biliary cirrhosis. J Autoimmun. 2009;33:178–182. doi: 10.1016/j.jaut.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 11.Lisboa L.F., Asthana S., Kremer A., Swain M., Bagshaw S.M., Gibney N., Karvellas C.J. Blood cytokine, chemokine and gene expression in cholestasis patients with intractable pruritis treated with a molecular adsorbent recirculating system: a case series. Can J Gastroenterol. 2012;26:799–805. doi: 10.1155/2012/623862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goncalves V.M., Matteucci K.C., Buzzo C.L., Miollo B.H., Ferrante D., Torrecilhas A.C., Rodrigues M.M., Alvarez J.M., Bortoluci K.R. NLRP3 controls Trypanosoma cruzi infection through a caspase-1-dependent IL-1R-independent NO production. PLoS Negl Trop Dis. 2013;7:e2469. doi: 10.1371/journal.pntd.0002469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Paroli A.F., Gonzalez P.V., Diaz-Lujan C., Onofrio L.I., Arocena A., Cano R.C., Carrera-Silva E.A., Gea S. NLRP3 inflammasome and Caspase-1/11 pathway orchestrate different outcomes in the host protection against Trypanosoma cruzi acute infection. Front Immunol. 2018;9:913. doi: 10.3389/fimmu.2018.00913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zalinger Z.B., Elliott R., Weiss S.R. Role of the inflammasome-related cytokines Il-1 and Il-18 during infection with murine coronavirus. J Neurovirol. 2017;23:845–854. doi: 10.1007/s13365-017-0574-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thomas H. NAFLD: A critical role for the NLRP3 inflammasome in NASH. Nat Rev Gastroenterol Hepatol. 2017;14:197. doi: 10.1038/nrgastro.2017.21. [DOI] [PubMed] [Google Scholar]
- 16.Ouyang X., Ghani A., Mehal W.Z. Inflammasome biology in fibrogenesis. Biochim Biophys Acta. 2013;1832:979–988. doi: 10.1016/j.bbadis.2013.03.020. [DOI] [PubMed] [Google Scholar]
- 17.Gao B., Radaeva S. Natural killer and natural killer T cells in liver fibrosis. Biochim Biophys Acta. 2013;1832:1061–1069. doi: 10.1016/j.bbadis.2012.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grabarz F., Aguiar C.F., Correa-Costa M., Braga T.T., Hyane M.I., Andrade-Oliveira V., Landgraf M.A., Camara N.O.S. Protective role of NKT cells and macrophage M2-driven phenotype in bleomycin-induced pulmonary fibrosis. Inflammopharmacology. 2018;26:491–504. doi: 10.1007/s10787-017-0383-7. [DOI] [PubMed] [Google Scholar]
- 19.Abraham S., Szabo A., Kaszaki J., Varga R., Eder K., Duda E., Lazar G., Tiszlavicz L., Boros M., Lazar G., Jr. Kupffer cell blockade improves the endotoxin-induced microcirculatory inflammatory response in obstructive jaundice. Shock. 2008;30:69–74. doi: 10.1097/SHK.0b013e31815dceea. [DOI] [PubMed] [Google Scholar]
- 20.Zandieh A., Payabvash S., Pasalar P., Morteza A., Zandieh B., Tavangar S.M., Dehpour A.R. Gadolinium chloride, a Kupffer cell inhibitor, attenuates hepatic injury in a rat model of chronic cholestasis. Hum Exp Toxicol. 2011;30:1804–1810. doi: 10.1177/0960327111400106. [DOI] [PubMed] [Google Scholar]
- 21.Jones C., Badger S.A., Hoper M., Parks R.W., Diamond T., Taylor M.A. Hepatic cytokine response can be modulated using the Kupffer cell blocker gadolinium chloride in obstructive jaundice. Int J Surg. 2013;11:46–51. doi: 10.1016/j.ijsu.2012.11.008. [DOI] [PubMed] [Google Scholar]
- 22.Sato K., Hall C., Glaser S., Francis H., Meng F., Alpini G. Pathogenesis of Kupffer cells in cholestatic liver injury. Am J Pathol. 2016;186:2238–2247. doi: 10.1016/j.ajpath.2016.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gong Z., Zhou J., Zhao S., Tian C., Wang P., Xu C., Chen Y., Cai W., Wu J. Chenodeoxycholic acid activates NLRP3 inflammasome and contributes to cholestatic liver fibrosis. Oncotarget. 2016;7:83951–83963. doi: 10.18632/oncotarget.13796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Woolbright B.L., Jaeschke H. Novel insight into mechanisms of cholestatic liver injury. World J Gastroenterol. 2012;18:4985–4993. doi: 10.3748/wjg.v18.i36.4985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang Y., Hong J.Y., Rockwell C.E., Copple B.L., Jaeschke H., Klaassen C.D. Effect of bile duct ligation on bile acid composition in mouse serum and liver. Liver Int. 2012;32:58–69. doi: 10.1111/j.1478-3231.2011.02662.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kuida K., Lippke J.A., Ku G., Harding M.W., Livingston D.J., Su M.S., Flavell R.A. Altered cytokine export and apoptosis in mice deficient in interleukin-1 beta converting enzyme. Science. 1995;267:2000–2003. doi: 10.1126/science.7535475. [DOI] [PubMed] [Google Scholar]
- 27.Cerqueira D.M., Pereira M.S., Silva A.L., Cunha L.D., Zamboni D.S. Caspase-1 but not Caspase-11 is required for NLRC4-mediated pyroptosis and restriction of infection by flagellated legionella species in mouse macrophages and in vivo. J Immunol. 2015;195:2303–2311. doi: 10.4049/jimmunol.1501223. [DOI] [PubMed] [Google Scholar]
- 28.Cai S.Y., Gautam S., Nguyen T., Soroka C.J., Rahner C., Boyer J.L. ATP8B1 deficiency disrupts the bile canalicular membrane bilayer structure in hepatocytes, but FXR expression and activity are maintained. Gastroenterology. 2009;136:1060–1069. doi: 10.1053/j.gastro.2008.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ouyang X., Ghani A., Malik A., Wilder T., Colegio O.R., Flavell R.A., Cronstein B.N., Mehal W.Z. Adenosine is required for sustained inflammasome activation via the A(2)A receptor and the HIF-1alpha pathway. Nat Commun. 2013;4:2909. doi: 10.1038/ncomms3909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cai S.Y., Mennone A., Soroka C.J., Boyer J.L. All-trans-retinoic acid improves cholestasis in alpha-naphthylisothiocyanate-treated rats and Mdr2–/– mice. J Pharmacol Exp Ther. 2014;349:94–98. doi: 10.1124/jpet.113.209353. [DOI] [PMC free article] [PubMed] [Google Scholar]