Abstract
Background
Spreading of the COVID-19 pandemic in Italy forced health facilities to drastically change their organization to face the overwhelming number of infected patients needing hospitalization. The aim of this paper is to share with all the vascular community the protocol developed by the USL (Unità Sanitaria Locale) Toscana Centro for the reorganization of the Vascular Surgery Unit during the COVID-19 emergency, hoping to help other institutions to face the emergency during the hard weeks coming.
Methods
The USL Toscana Centro is a public Italian health care institution including four districts (Empoli, Florence, Pistoia, Prato) with 13 different hospitals, serving more than 1,500,000 people in a 5000 km2 area. The USL adopted a protocol of reorganization of the Vascular Surgery Unit during the first difficult weeks of the epidemic, consisting in the creation of a Vascular Hub for urgent cases, with a profound reorganization of activities, wards, surgical operators, operating blocks, and intensive care unit (ICU) beds.
Results
All 13 hospitals are now COVID-19 as the first days of April passed. The San Giovanni di Dio Hospital (Florence) has more than 80 COVID-19 patients in different settings (ICU, medical and surgical ward), which at the time of writing is almost one-third of the total hospital capacity (80/260 beds). It has been identified as the Surgical Hub for urgent vascular COVID-19 cases. Therefore, the elective surgical and office activities were reduced by 30% and 80%, respectively, and reserved to priority cases. A corner of the whole operating block, well separate from the remaining operating rooms, was rapidly converted into one operating room and six ICU beds dedicated to COVID patients. The COVID-19 surgical path now includes an emergency room for suspected COVID-19 patients directly connected to an elevator for the transfer of COVID patients in the COVID operating block and dedicated COVID-19 ward and ICU beds.
Conclusions
Rapid modification of hospital settings, a certain “flexibility” of the medical personnel, a stepwise shutdown of vascular surgical and office activity, and the necessity of a strong leadership are mandatory to cope with the tsunami of the COVID-19 outbreak.
The recent spread of the COVID-19 pandemic in Italy led to the urgency of finding sustainable models to face the rapid increase of symptomatic hospitalized patients while protecting noninfected patients and health care workers from the contagion. A fair number of reports have already described the efforts of health care institutions from different countries to relocate wards, intensive care units (ICUs), and operating rooms (ORs) to avoid the rapid collapse of the hospital facilities.1, 2, 3, 4, 5 Herein, we would like to share the protocol developed by the USL (Unità Sanitaria Locale) Toscana Centro for the reorganization of the Vascular Surgery Unit during the COVID-19 emergency.
The USL Toscana Centro is a public Italian health care institution including four districts (Empoli, Florence, Pistoia, and Prato) with 13 different hospitals, serving more than 1,500,000 people in a 5000 km2 area. The aim of a health regional service should be to create a non-COVID-19 hospital (if possible) where elective critical surgical activity should be spared, and this model was followed also in the USL Toscana Centro during the first weeks of the epidemic. COVID-19 patients were first admitted in those hospitals where ICU units or infectious disease wards were present. However, because of the outbreak and the overwhelming amount of COVID-19 patients needing hospitalization during the following weeks, it was not possible in our region to preserve one or more hospitals from the disease (Fig 1 ), and all 13 hospitals are now COVID-19 as the first days of April have passed (lockdown in Italy started March 9, with no COVID-19 patients in our hospital). Our hospital in Florence (San Giovanni di Dio Hospital) has more than 80 COVID-19 patients in different settings (ICU, medical and surgical wards) at the time of writing, almost a third of the total hospital capacity (80/260 beds). Since the beginning of the epidemic, the scenario has been completely different each new week, and it was not possible to plan elective activity even day by day.
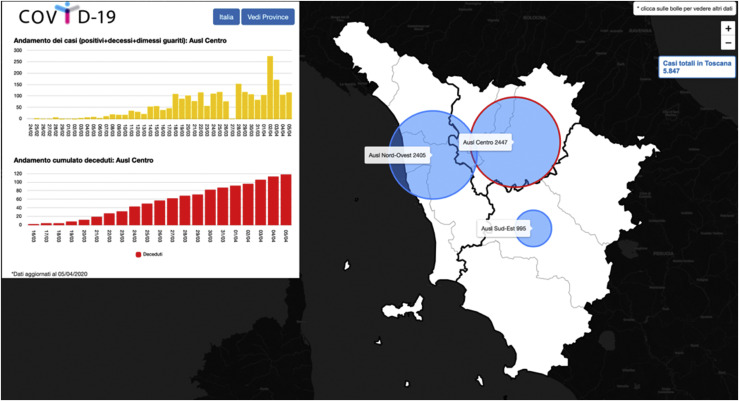
Fig 1.
Number of COVID-19 cases in Tuscany, Italy, updated to April 5, 2020.
What to do therefore? Areas previously dedicated to different activities were converted to COVID-19 wards and adjunctive ICUs, and medical staff from other specialties was converted to COVID staff to ensure 24/7 patient assistance. The elective surgical and office activity was dramatically reduced in all of the centers and reserved for priority cases. In our hospital, only 4 of 11 ORs are now usable: 1 for urgency/emergency, 1 for only COVID patients, 1 hybrid room, 1 for elective cases. This reduced number of ORs should accommodate five different specialties at the same time: urology, general surgery, orthopedics, gynecology, and finally vascular surgery. Regarding vascular surgery reorganization, we decided to cut all varicose vein surgery and all office activities (apart from urgencies). Aneurysm, symptomatic carotid lesions, critical limb-threatening ischemia (CLTI), and hemodialysis arteriovenous access operations were centralized in our hospital, collecting those cases from peripheral hospitals that were overwhelmed by COVID-19 patients. Endovascular treatment of CLTI was preferred to bypass surgery to eliminate the presence of anesthetists in the OR because of their shortage (many patients to be followed up in ICUs and some anesthetists are at the time of writing unfortunately infected). Asymptomatic carotid lesions evaluated at high risk of stroke were started to be operated on by our vascular staff in a private hospital that began to cooperate with the National Health System to help in this emergency situation. The drop of elective vascular surgical repair was around 34% if we compare March 2019 to March 2020. In the same way, the number of office visits dropped off around 80%.
Urgent cases of hemodynamically stable patients confirmed to have or suspected of having COVID-19 from peripheral hospitals were centralized in the dedicated COVID-19 surgical hub of the operating block of the San Giovanni di Dio Hospital (Florence). A corner of the whole operating block, well separate from the remaining ORs, was rapidly converted into one OR and six ICU beds dedicated to COVID patients (Fig 2 ). The COVID-19 surgical path now includes an emergency room for patients suspected of having COVID-19 directly connected to an elevator for the transfer of COVID patients in the COVID operating block. Surgical operators access a dressing room first, where they dress up with the obligatory personal protective equipment, including N95 mask, goggles, face shield, splash-resistant gown, boot covers, and two pairs of surgical gloves. Then, the operators transfer to the COVID-19 area and into the OR. The application of an alcohol solution on the second pair of gloves, followed by a sterile gown and an extra pair of sterile surgical gloves, completes the surgical dressing. After the intervention, the surgical operators transfer to the undressing room located beside the OR and execute the undressing procedure supervised by a trained operator. All the surfaces of the OR are decontaminated after the intervention.
Fig 2.
Operating room (OR) converted into two intensive care unit (ICU) beds.
Postoperative care of treated COVID patients is a further challenge for health personnel because of the high risk of cross-contagion. To decrease this risk, it is advisable to have two physicians visiting COVID patients: one “uncontaminated” waiting outside a closed room where patients are, and one “contaminated” physician wearing all the personal protective equipment visiting the patients. A clear line on the floor should be drawn to separate the clean from the contaminated field (Fig 3 ). We would like to report as an example of management of COVID-19 surgical patients two cases, a ruptured abdominal aortic aneurysm (AAA) and a ruptured thoracoabdominal aortic aneurysm (TAAA), occurring in a peripheral COVID hospital that was completely overwhelmed by COVID-19 patients with no bed left in the ICU. The AAA patient was hemodynamically unstable, so the patient was treated in the peripheral hospital and then transferred to the hub ICU and then successfully discharged to a standard surgical ward. The patient with a hemodynamically stable covered rupture of a type II TAAA was transferred to the hub hospital and treated by endovascular means as a COVID patient while waiting for the results of the COVID-19 test. The patient was kept isolated in the OR until the negative response of testing and was then transferred to the surgical ward.
Fig 3.
Two operators interacting in a COVID-19 ward of the San Giovanni di Dio Hospital (Florence, Tuscany, Italy).
In our experience until now testing the COVID-19 surgical hub, the most crucial point of the creation of a well-working model is the support and the correct use of the telemedicine infrastructure. During the last decade, one of the main goals of the USL was to implement an organization chart encouraging the sharing of health care professionals between all the facilities of the territorial network. Well-established telemedicine and surgical centralization protocols were already implemented before the outbreak of the COVID-19 epidemic, allowing a fast response of the USL to the massive modification of the infrastructural needs required to face the disease. The communication between the accepting hospital and the hub center has to be as fast as possible, with rapid sharing of the clinical status and of the vascular imaging of the patient (when available) to reduce the time for decision-making and to plan the most efficacious treatment option for the patient.
Another key point is to provide turnover for the exhausted medical personnel. Regarding our unit, some surgeons, because of a certain “unit hypertrophy” of the vascular staff related to the current reduced vascular activity, have been temporally assigned to help anesthetists in the ICUs or internist physicians in medical wards. Surgeons have also been placed at home for some days alternatively to preserve a pool of noninfected operators that could be used in any moment in case of necessity and kept healthy on the other hand to replace infected colleagues of any specialty because of the high contagiousness of the virus.
Another scenario, in case of an uncontrolled outbreak, would be to close all elective cases and take care of urgent and emergent cases only as a hub-and-spoke service.
In the last step, when the outbreak will finally come to an end and the number of patients hospitalized will be reduced, the goal will be to gradually reopen activities. In our opinion, first of all, a clear separation between COVID and non-COVID hospitals should be realized. For that purpose, testing of all admitted patients should be mandatory. Elective surgery should favor AAAs or TAAAs >7 cm, symptomatic or vulnerable carotid lesions, arteriovenous fistulas, and CLTI. During this outbreak, we also recruited angiologists to help us in office duties to preserve surgeons from the contagion, as previously described, but also to help us with the overwhelming number of visits postponed when this crisis will come to an end.
In conclusion, rapid decision, rapid modification of hospital settings transforming a surgical ward into a medical one and ORs and medical wards into ICUs, a certain “flexibility” of the medical personnel, a stepwise shutdown of vascular surgical and office activity, and the necessity of a strong leadership are mandatory to cope with the tsunami of the COVID-19 outbreak.
Author contributions
Conception and design: EC, FM, SM
Analysis and interpretation: EC, FM
Data collection: EC, FM
Writing the article: EC, FM
Critical revision of the article: EC, FM, SM
Final approval of the article: EC, FM, SM
Statistical analysis: EC, FM
Obtained funding: Not applicable
Overall responsibility: FM
EC and FM share the first authorship.
Footnotes
Author conflict of interest: none.
The editors and reviewers of this article have no relevant financial relationships to disclose per the JVS policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Lu K.L., Chen S., Leung L.P. Initial experience of an emergency department in Shenzhen in responding to the emerging Wuhan coronavirus pneumonia. Ann Emerg Med. 2020;75:556. doi: 10.1016/j.annemergmed.2020.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cao Y., Li Q., Chen J., Guo X., Miao C., Yang H., et al. Hospital emergency management plan during the COVID-19 epidemic. Acad Emerg Med. 2020;27:309–311. doi: 10.1111/acem.13951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ross S.W., Lauer C.W., Miles W.S., Green J.M., Christmas A.B., May A.K., et al. Maximizing the calm before the storm: tiered surgical response plan for novel coronavirus (COVID-19) J Am Coll Surg. 2020;230:1080–1091.e3. doi: 10.1016/j.jamcollsurg.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zangrillo A, Beretta L, Silvani P, Colombo S, Scandroglio AM, Dell’Acqua A, et al. Fast reshaping of intensive care unit facilities in a large metropolitan hospital in Milan, Italy: facing the COVID-19 pandemic emergency [published online ahead of print April 1, 2020]. Crit Care Resusc PMID: 32227819. [DOI] [PMC free article] [PubMed]
- 5.Asperges E, Novati S, Muzzi A, Biscarini S, Sciarra M, Lupi M, et al; COVID-19 IRCCS San Matteo Pavia Task Force. Rapid response to COVID-19 outbreak in northern Italy: how to convert a classic infectious disease ward into a COVID-19 response centre [published online ahead of print March 20, 2020]. J Hosp Infect doi: 10.1016/j.jhin.2020.03.020. [DOI] [PMC free article] [PubMed]