Key Points
Question
Is the repeated use of a decision aid by heart teams associated with greater shared decision-making and improved clinicians’ attitudes toward use of decision aids?
Findings
In this mixed-methods pilot study including 6 clinicians and 35 patients with aortic stenosis, multiple uses of a decision aid were associated with improved shared decision-making and increased patient knowledge and satisfaction without a change in decisional conflict. Clinicians believed that they performed shared decision-making without the decision aid and that their elderly patients did not benefit from the decision aid.
Meaning
Multiple uses of a decision aid were associated with improvements in shared decision-making and patient-centered outcomes, suggesting a learning curve; however, clinicians perceived a lack of benefit, clarifying new research directions for shared decision-making in heart teams.
Abstract
Importance
Shared decision-making (SDM) is widely advocated for patients with valvular heart disease yet is not integrated into the heart team model for patients with symptomatic aortic stenosis. Decision aids (DAs) have been shown to improve patient-centered outcomes and may facilitate SDM.
Objective
To determine whether the repeated use of a DA by heart teams is associated with greater SDM, along with improved patient-centered outcomes and clinician attitudes about DAs.
Design, Setting, and Participants
This mixed-methods study included a nonrandomized pre-post intervention and clinician interviews. It was conducted between April 30, 2015, and December 7, 2017, with quantitative analysis performed between January 12, 2017, and May 26, 2017, within 2 academic medical centers in northern New England among 35 patients with symptomatic aortic stenosis who were at high to prohibitive risk for surgery. The qualitative analysis was performed between August 6, 2018, and May 7, 2019. The Severe Aortic Stenosis Decision Aid was delivered by 6 clinicians, with patients choosing between transcatheter aortic valve replacement and medical management.
Main Outcomes and Measures
Clinician SDM performance was measured using the Observer OPTION5 scale with dual-independent coding of audiotaped clinic visits. Previsit and postvisit surveys measured the patient’s knowledge, satisfaction, and decisional conflict. Audiotaped clinician interviews were coded, and qualitative thematic analysis was performed.
Results
Six male clinicians and 35 patients (19 of 34 women [55.9%; 1 survey was missing]; mean [SD] age, 85.8 [7.8] years) participated in the study. Shared decision-making increased stepwise with repeated use of the DA (mean [SD] Observer OPTION5 scores: usual care, 17.9 [7.6]; first use of a DA, 60.5 [30.9]; fifth use of a DA, 79.0 [8.4]; P < .001 for comparison between usual care and fifth use of DA). Multiple uses of the DA were associated with increased patient knowledge (mean difference, 18.0%; 95% CI, 1.2%-34.8%; P = .04) and satisfaction (mean difference, 6.7%; 95% CI, 2.5%-10.8%; P = .01) but not decisional conflict (mean [SD]: usual care, 96.0% [9.4%]; first use of DA, 93.8% [12.5%]; fifth use of DA, 95.0% [11.2%]; P = .60). Qualitative analysis of clinicians’ interviews revealed that clinicians perceived that they used an SDM approach without DAs and that the DA was not well understood by elderly patients. There was infrequent values clarification or discussion of stroke risk.
Conclusion and Relevance
In a mixed-methods pilot study, use of a DA for severe aortic stenosis by heart team clinicians was associated with improved SDM and patient-centered outcomes. However, in qualitative interviews, heart team clinicians did not perceive a significant benefit of the DA, and therefore sustained implementation is unlikely. This pilot study of SDM clarifies new research directions for heart teams.
This mixed-methods pilot study examines whether the repeated use of a decision aid by heart teams was associated with greater shared decision-making, along with improved patient-centered outcomes and clinicians’ attitudes about decision aids.
Introduction
Aortic stenosis (AS) is increasingly prevalent as the population ages, with 12.4% of elderly patients affected.1 Options for treatment of symptomatic AS include surgical aortic valve replacement, transcatheter aortic valve replacement (TAVR), and medical management. Professional guidelines recommend a shared decision-making (SDM) approach for patients considering treatment of AS,2 yet, to our knowledge, there is little research describing real-world heart teams using tools that lead to SDM, such as patient decision aids (DAs). Decision aids are designed to help patients make informed choices about health care options based on their values and preferences.3 The underuse of DAs is often due to implementation barriers at the clinician level. Thus, many DAs “work around” clinicians and focus on patient education before the clinical encounter.4
Shared decision-making is a bidirectional exchange of information between clinicians and patients, distinct from the 1-way stream of information in patient education or informed consent.5 Prior trials suggest that DAs alone are not enough for SDM; improved clinician skill sets and attitudes are also needed.6 This mixed-methods pilot study assesses the association of a DA for severe AS delivered by heart team clinicians with SDM and patient-centered outcomes, including knowledge, satisfaction, and decisional conflict. A temporal study design examines the learning curve of DA use with a rigorous qualitative review of clinician interviews clarifying implementation barriers and guiding future research.
Methods
Intervention
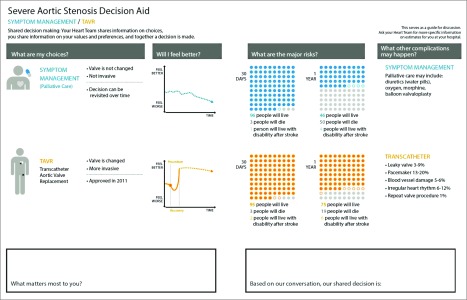
The Severe Aortic Stenosis Decision Aid is a paper-based DA used by clinicians during the clinic visit when patients at high to prohibitive surgical risk are choosing between TAVR and medical management; an iterative design was tested and was performed at 9 TAVR centers with key stakeholders (ie, patients, families, and clinicians) (Figure 1; eAppendix 1 and eFigure 1 in the Supplement). Informed written consent was obtained from patients and families, and verbal consent was obtained from physicians; the study was approved by the Dartmouth-Hitchcock Medical Center and University of Vermont Medical Center Institutional Review Boards.
Figure 1. Severe Aortic Stenosis Decision Aid.
This patient decision aid is used during a clinical visit for patients with symptomatic aortic stenosis who are at high to prohibitive risk for surgery and is delivered by heart team clinicians.
Setting and Recruitment
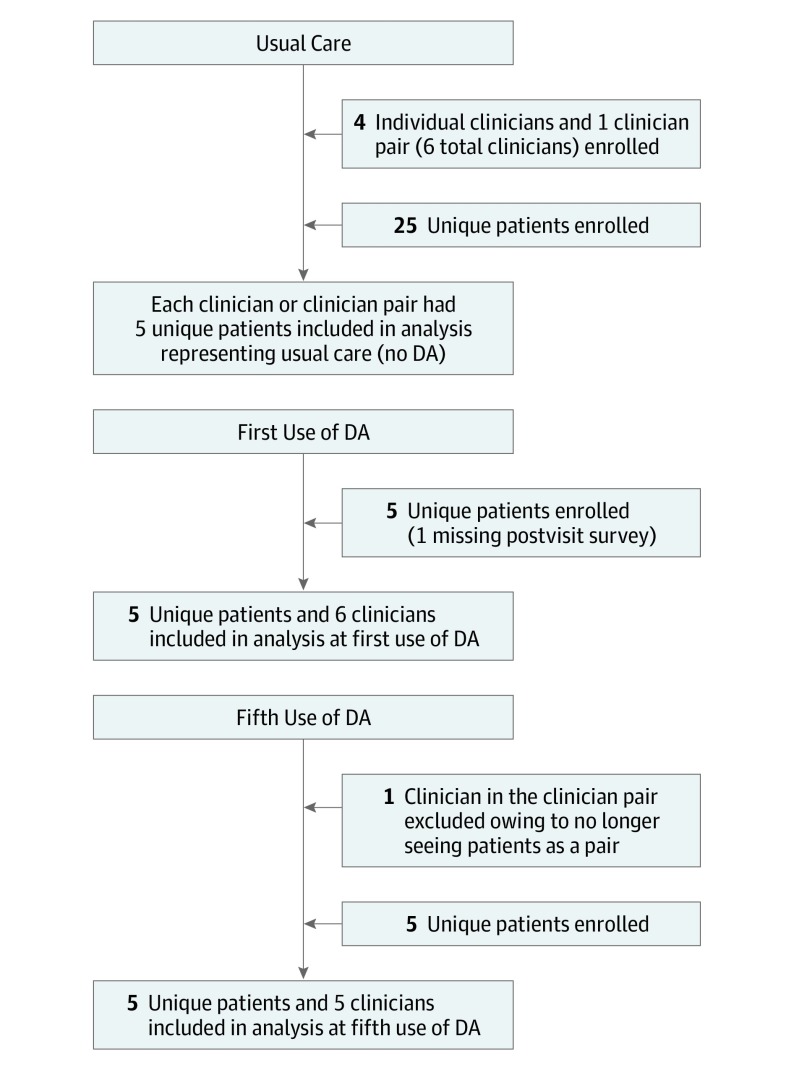
Clinicians (interventional cardiologists and cardiac surgeons; H.L.D.) and patients with severe AS were recruited at 2 TAVR centers in northern New England (Figure 2). This mixed-methods study including a nonrandomized pre-post intervention and clinician interviews was conducted between April 30, 2015, and December 7, 2017, with quantitative analysis performed between January 12, 2017, and May 26, 2017. The qualitative analysis was performed between August 6, 2018, and May 7, 2019. Clinicians were introduced to the DA with one-on-one instruction, a training video, and how-to guides (shared decision checklist) (Video; eFigure 2 in the Supplement). Patient inclusion criteria were high to prohibitive surgical risk, clinician agreement of a choice between TAVR and medical therapy, and no major barriers to providing informed consent, participating in SDM, or completing surveys.
Figure 2. CONSORT Flow Diagram.
Flow diagram of patient and clinician recruitment and data analysis. DA indicates decision aid.
Video. Shared Decision-making Training Video.
Data Collection
Usual care (UC) included baseline visits without a DA and served as the control; each clinician, or clinician pair, saw 5 patients (25 patients total). Given the temporal study design to assess a learning curve, 1 visit per clinician was recorded at the first use of the DA and 1 visit at the fifth use of the DA (10 patients total). Thus, the total number of clinicians determined the number of patients at the first use and the fifth use of the DA. Previsit and postvisit surveys were completed by patients (eAppendix 2 in the Supplement), and visits were audiorecorded with consent. A formal, validated measure assessed SDM via independent coder review of audiorecordings (Observer OPTION5 scale; eTable 1 in the Supplement). Clinician semistructured interviews were performed for each point. The postvisit questionnaire used the Consumer Assessment of Healthcare Providers and Systems survey for patient satisfaction7 and SURE (Sure of myself; Understand information; Risk-benefit ratio; Encouragement), a validated test for decisional conflict.8 Less decisional conflict indicated that patients’ choices aligned with their values.
Quantitative Data Analysis
Means and standard deviations were summarized for continuous variables, including age and knowledge. Frequencies and proportions were computed to describe the distribution of categorical variables. The characteristics of patients across visits were compared using paired t tests for continuous variables. The Fisher exact test was used for categorical variables (sex and educational level) to make comparisons between UC and the fifth use of the DA.
Changes in measures of SDM, patient knowledge, and patient satisfaction were examined graphically for comparison. Formal statistical comparisons were performed between UC and the fifth use of the DA (by a paired t test) to assess for the learning curve. The paired t test treated each clinician as an individual participant, with repeated measures (UC and the first and fifth uses of the DA). The mean of paired differences and 95% CIs were computed. Data analysis was conducted in R, version 3.4.1 (R Foundation for Statistical Computing). All P values were from 2-sided tests, and the results were deemed statistically significant at P < .05. The agreement of each rater pair for Observer OPTION5 was assessed by using the concordance correlation coefficient of Lin9 and plots by Bland and Altman.10
Qualitative Analysis of Clinician Interviews
Recorded clinician interview data were analyzed using a hybrid approach, including elements of framework and thematic analysis.11 RE-AIM (Reach, Effectiveness, Adoption, Implementation, and Maintenance), a 5-step guide for translating research effectively into practice, provided an initial framework for analysis.12,13,14,15 The Adoption category was not included because all clinicians adopted the DA for the purpose of this study. Qualitative interviews were transcribed by a third party. Two coders (S.E.D. and N.K.S.) independently reviewed and coded transcripts according to the modified RE-AIM framework, using ATLAS.ti qualitative software (ATLAS.ti Scientific Software Development GmbH). Coders met regularly with 2 additional researchers (C.H.S. and S.L.S.) to build a shared codebook based on the data. A code hierarchy was developed with categories informed by RE-AIM. Subcategories were informed by the timing of DA use. Once coding was complete, the 4-person team (S.E.D., N.K.S., C.H.S., and S.L.S.) met to analyze the data, identifying themes, resolving disagreements through consensus, and summarizing findings. CORE-Q (Consolidated Criteria for Reporting Qualitative Research), a 32-item checklist,16 was used for reporting qualitative data, and SUNDAE (Standards for Universal Reporting of Patient Decision Aid Evaluations) ensured that the DA analysis and evaluation were understandable, transparent, and high quality.17
Results
Participants
Six heart team clinicians and 35 patients participated at 2 academic medical centers that perform TAVR. Four study clinicians saw patients on their own, and 2 saw patients together. Clinicians included 2 interventional cardiologists and 4 cardiac surgeons; all were men. One cardiac surgeon in the clinician pair dropped out of the study and 1 patient had a missing survey at the first use of DA.
Patients were a mean (SD) age of 85.8 (7.8) years, 19 of 34 (55.9%) were female, and 27 of 34 (79.4%) had educational attainment of high school or greater. Most patients agreed that they were informed about treatment choices prior to the visit (28 of 34 [82.4%]). Patients at fifth use of the DA were significantly older than those at UC (mean difference, 7.7 years [95% CI, 1.5-13.9 years]; P = .03) (Table).
Table. Patient Characteristics and Outcomesa.
| Characteristic or Outcome | Usual Care | First Use of Decision Aidb | Fifth Use of Decision Aid | P Valuec |
|---|---|---|---|---|
| Age, mean (SD), y | 85.1 (7.5) | 81.5 (10.5) | 92.8 (2.7) | .03 |
| Educational level of high school or greater, No./total No. (%) | 19/25 (76.0) | 4/4 (100) | 4/5 (80) | .40 |
| Previsit knowledge, mean (SD), % | 32.0 (23.4) | 18.8 (23.9) | 30.0 (44.7) | .90 |
| Postvisit knowledge, mean (SD), % | 62.0 (17.9) | 75.0 (35.4) | 80.0 (20.9) | .04 |
| Shared decision-making, mean (SD) | 17.9 (7.6) | 60.5 (30.9) | 79.0 (8.4) | <.001 |
| Patient satisfaction, mean (SD), % | 93.9 (13.6) | 100 (0) | 100 (0) | .01 |
| Decisional conflict, mean (SD), % | 96.0 (9.4) | 93.8 (12.5) | 95.0 (11.2) | .60 |
A formal, validated measure assessed shared decision-making via independent coder review of audiorecordings (Observer OPTION5 scale). Clinician semistructured interviews were performed for each point. The postvisit questionnaire used the Consumer Assessment of Healthcare Providers and Systems survey for patient satisfaction7 and SURE (Sure of myself; Understand information; Risk-benefit ratio; Encouragement), a validated test for decisional conflict.8 Less decisional conflict indicated that patients’ choices aligned with their values.
One missing survey.
Computed from paired t tests of continuous variables and Fisher exact tests of categorical variables; comparisons were made only between usual care and fifth use of decision aid.
Shared Decision-making
After multiple uses of the DA, there were significantly greater levels of SDM compared with UC (mean difference in Observer OPTION5 score, 61.1 [95% CI, 51.3-70.9]; P < .001) (eFigure 3A in the Supplement). Mean (SD) scores increased stepwise from UC to the first use of DA to the fifth use of DA (UC, 17.9 [7.6]; first use of DA, 60.5 [30.9]; fifth use of DA, 79.0 [8.4]). Rater agreement was limited in the setting of a small sample size (eTable 2 in the Supplement).
Patient Knowledge, Patient Satisfaction, and Decisional Conflict
Previsit patient knowledge was comparable (mean [SD]: usual care, 32.0% [23.4%]; first use of DA, 18.8% [23.9%]; fifth use of DA, 30.0% [44.7%]; P = .93). Patient postvisit knowledge increased stepwise with increasing clinician experience using the DA (mean difference between UC and fifth use, 18.0% [95% CI, 1.2%-34.8%]; P = .04) (eFigure 3B in the Supplement; Table). Improved patient satisfaction was associated with use of the DA compared with UC (mean difference, 6.7% [95% CI, 2.5%-10.8%]; P = .01) (eFigure 3C in the Supplement). Decisional conflict did not differ (mean [SD]: usual care, 96.0% [9.4%]; first use of DA, 93.8% [12.5%]; fifth use of DA, 95.0% [11.2%]; P = .60). Elicitation of patient values and preferences was not different between the first use and the fifth use of DA; clinicians asked patients “What matters most?” or similar questions to elicit patient goals and preferences 41% of the time, and rarely mentioned stroke risk.
Qualitative Clinician Interviews
Six clinicians underwent semistructured interviews at UC. One cardiac surgeon left the study; thus, 5 clinicians completed interviews after the first and fifth uses of DA (Figure 2).
Usual Care
Qualitative analysis demonstrated that, prior to use of the DA, nearly all clinicians believed that they already performed SDM, naming the use of visual aids to communicate key concepts with patients to depict the disease process. (“The visual cues are typically drawings,” [clinician 2] and “I do a visual with my hands” [clinician 5].)
Clinicians were confident that patients were most interested in hearing about serious outcomes of valve replacement. (“No one cares about bleeding or pacemaker or length of stay. They care about stroke and death” [clinician 1].)
Using a DA was seen by clinicians to replicate what was already being done. Strategies for values clarification, or finding out what mattered most to patients, were not well described. One clinician contrasted SDM with informed consent. (“I think many surgeons feel that shared decision-making is something that we do every time we consent someone for surgery … [but] it isn’t necessarily part of the consent process” [clinician 4].)
First Use of the DA
After the initial use of the DA, clinicians confirmed that it replicated what they were already doing. They found the DA awkward to incorporate into their usual routine. (“I purposely made it clunky so I didn’t miss anything … whereas [otherwise] I think we organically hit the 5 points [of shared decision-making]” [clinician 2], and “It’s like when I get into my car: I know I have to put my seat belt on … I don’t have a checklist to tell me to do [it] … I’d like to think that the same conversations happen whether the tool is there or not” [clinician 3].)
Clinicians stated that elderly patients were less likely to understand the DA and that patient review before the visit may be helpful. They believed that younger family members benefited more from the DA than did their frail parents. One clinician highlighted that patients were not prepared to discuss values and preferences. Some felt that values did not need to be explicitly verbalized, and others appreciated a reminder. (“I didn’t get into … what his values and preferences were because … I feel that is going into his decision-making” [clinician 4], and “I think it’s great to have a stopping point that says, ‘What matters most?’ as a reminder to physicians to elicit that conversation” [clinician 5].)
Fifth Use of the DA
After 5 uses of the DA, clinicians reported greater ease implementing the DA but still felt that it was poorly understood by patients. This perception appeared in part to be due to a greater number of questions from patients as conversations expanded. (“The questions I got back from patients implied to me that they weren’t necessarily grasping everything … To be honest, the people who really liked it were the family members that were with the patients” [clinician 3].)
Summary of Qualitative Analysis
The in-depth qualitative analysis revealed a consistent perception from clinicians that SDM occurs in their normal routine (eTable 3 in the Supplement); a formal SDM measurement with a third-party review did not support this perception. Most notable was an impression of poor patient understanding of the DA, even while SDM and patient knowledge and satisfaction improved. A minor theme was that clinicians thought that younger family members were more likely than the older patients to benefit from the DA.
Discussion
The recently revised Centers for Medicare & Medicaid Services National Coverage Determination for TAVR18 stopped short of mandating SDM, explaining that they “support patient shared decision-making in aortic valve replacement, but there is not a fully developed tool at this time.” To our knowledge, this study represents the first association of a DA for severe AS with increased SDM, improved patient knowledge, and improved patient satisfaction; there was no association between the DA and decisional conflict. Although clinicians thought that they already performed SDM, a formal measurement did not support this belief. Clinicians had limited insight that the quality of clinical encounters was improving, perceiving that patients had a poor understanding of the DA. As a result, clinicians’ attitudes toward SDM and DAs underwent little transformation, and implementation is unlikely. This is a critical finding, challenging the simplistic framing that once fully developed tools are available, sustained use of a DA will occur, leading to SDM. This exploratory study helps clarify new directions in SDM research for heart teams (Box).
Box. Future SDM Research Questions for Heart Teams.
Patient Preparation Before Heart Team Visit
Is patient engagement needed prior to the heart team physician visit, and could other multidisciplinary team members lead this patient engagement?
What strategies may improve the inclusion of patient values and preferences in the heart team visit? What other patient engagement activities prior to the physician visit could be performed? Which team members would be most well suited to perform these activities? Could supportive team members be trained in discrete tasks (ie, values clarification by medical assistants)?
Can dividing tasks of SDM among team members create a more efficient visit for physicians, with dual benefit of greater levels of SDM? Are there benefits such as cost savings or reductions in reported physician burnout?
Heart Team Visit
What are the benefits and unintended consequences of having cardiac surgeons and interventional cardiologists meet simultaneously with the patient and family? Do the benefits differ from a physician perspective vs a patient and family perspective?
Do younger family members influence how clinicians perceive elderly patient understanding or benefit of DAs?
Would providing feedback to clinicians on improved patient-centered outcomes (ie, patient satisfaction) with the use of a DA lead to greater sustained use of DAs?
Outcome Measures of SDM in Heart Teams
What is the most accurate measure of an SDM process? Can new measures be created for heart teams that replicate more intensive measures (ie, Observer OPTION5)?
How do DAs influence patient choice? How does this influence differ between older patients with multiple comorbidities and younger, healthier patients with heart valve disease?
Prior literature shows that DAs were associated with improved patient-centered outcomes and may increase use of an SDM process.3 Most DAs are used outside the clinical encounter, largely owing to barriers surrounding clinician engagement.19 Clinicians are concerned that SDM is too time-intensive, and they also simultaneously believe that SDM is already happening at each visit—attitudes that are common challenges to real-world use of DAs.6 Research suggests that clinicians poorly predict patients’ desired role in decision-making,20 make inaccurate self-assessments of their communication skills,21 and fail to innovate in how time is allocated for care.22
Clinicians paradoxically perceived the frail elderly to not benefit even as SDM and patient knowledge improved. Decision aids are efficacious across a broad range of diverse demographics, including individuals with low health literacy.23 The National Quality Forum highlights SDM as a potential way to address health disparities. A recent National Quality Partners Playbook, “Shared Decision Making in Healthcare,” describes how health care systems can encourage SDM among clinicians, including educating patients and families about what to expect from clinicians, advancing team knowledge and skill sets in SDM, integrating SDM into the clinical workflow, and holding health care teams accountable for SDM engagement.5
Strengths and Limitations
This study has several unique strengths. Prior research in SDM skill sets has been limited by a lack of DA delivery by clinicians, highlighting the importance of studying the use of DAs by heart teams. Visits in this study were audiorecorded, allowing for in-depth analysis of the clinician-patient interactions. Qualitative review of interviews at 3 time points with clinicians provided further understanding, leveraging validated outcome measures and frameworks (RE-AIM, CORE-Q, and SUNDAE).
Our conclusions also have some limitations. This was a small sample size of clinicians, and the focus on discrete time points (ie, isolating first use) led to a small sample of patients. Patients in the fifth use group were significantly older. Given the small sample size, there was poor concordance between reviewers for Observer OPTION5, reducing certainty of SDM outcomes. All clinicians were men, which is reflective of the marked gender disparities in interventional cardiology and cardiac surgery, where women make up less than 5% of the workforce.24,25
Conclusions
In a mixed-methods pilot study, the use of a DA for severe AS by heart team clinicians was associated with improved SDM and patient-centered outcomes. However, in qualitative interviews, heart team clinicians did not perceive a significant benefit, and therefore sustained implementation is unlikely. This pilot study of SDM clarifies new research directions for heart teams.
eAppendix 1. Development of Severe Aortic Stenosis Decision Aid
eAppendix 2. Patient Surveys
eFigure 1. Prior Version of Severe Aortic Stenosis Decision Aid
eFigure 2. Shared Decision-Making Checklist for Severe Aortic Stenosis Choice
eFigure 3. Changes in Decisional Quality Outcomes With Multiple Uses of Patient Decision Aid
eTable 1. Shared Decision-Making (Observer OPTION5) Score Scale
eTable 2. Raters’ Agreement for Observer OPTION5
eTable 3. Themes Generated From Qualitative Analysis of Clinician Semi-Structured Interviews, With Supportive Quotes
eReferences
Footnotes
Abbreviations: DA, decision aid; SDM, shared decision-making.
References
- 1.Osnabrugge RL, Mylotte D, Head SJ, et al. Aortic stenosis in the elderly: disease prevalence and number of candidates for transcatheter aortic valve replacement: a meta-analysis and modeling study. J Am Coll Cardiol. 2013;62(11):1002-1012. doi: 10.1016/j.jacc.2013.05.015 [DOI] [PubMed] [Google Scholar]
- 2.Bavaria JE, Tommaso CL, Brindis RG, et al. 2018 AATS/ACC/SCAI/STS Expert Consensus Systems of Care document: operator and institutional recommendations and requirements for transcatheter aortic valve replacement: a joint report of the American Association for Thoracic Surgery, American College of Cardiology, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2019;73(3):340-374. doi: 10.1016/j.jacc.2018.07.002 [DOI] [PubMed] [Google Scholar]
- 3.Stacey D, Légaré F, Lewis K, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2017;4:CD001431. doi: 10.1002/14651858.CD001431.pub5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Elwyn G, Scholl I, Tietbohl C, et al. “Many miles to go …”: a systematic review of the implementation of patient decision support interventions into routine clinical practice. BMC Med Inform Decis Mak. 2013;13(suppl 2):S14. doi: 10.1186/1472-6947-13-S2-S14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Quality Forum National Quality Partners playbook: shared decision making in healthcare. Washington, DC: National Quality Forum; 2018. [Google Scholar]
- 6.Joseph-Williams N, Lloyd A, Edwards A, et al. Implementing shared decision making in the NHS: lessons from the MAGIC Programme. BMJ. 2017;357:j1744. doi: 10.1136/bmj.j1744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Agency for Healthcare Research and Quality CAHPS Clinician & Group Survey. https://www.cahps.ahrq.gov/. Accessed July 5, 2019.
- 8.Ferron Parayre A, Labrecque M, Rousseau M, Turcotte S, Légaré F. Validation of SURE, a four-item clinical checklist for detecting decisional conflict in patients. Med Decis Making. 2014;34(1):54-62. doi: 10.1177/0272989X13491463 [DOI] [PubMed] [Google Scholar]
- 9.Lin LI. A concordance correlation coefficient to evaluate reproducibility. Biometrics. 1989;45(1):255-268. doi: 10.2307/2532051 [DOI] [PubMed] [Google Scholar]
- 10.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Int J Nurs Stud. 2010;47(8):931-936. doi: 10.1016/j.ijnurstu.2009.10.001 [DOI] [PubMed] [Google Scholar]
- 11.Ritchie J, Spencer L. Qualitative data analysis for applied policy research In: Bryman A, Burgess RG, eds. Analyzing Qualitative Data. London, UK: Routledge; 2002:173-194. [Google Scholar]
- 12.Pope C, Ziebland S, Mays N. Qualitative research in health care: analysing qualitative data. BMJ. 2000;320(7227):114-116. doi: 10.1136/bmj.320.7227.114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13:117. doi: 10.1186/1471-2288-13-117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77-101. doi: 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 15.Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999;89(9):1322-1327. doi: 10.2105/AJPH.89.9.1322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349-357. doi: 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- 17.Sepucha KR, Abhyankar P, Hoffman AS, et al. Standards for universal reporting of patient decision aid evaluation studies: the development of SUNDAE Checklist. BMJ Qual Saf. 2018;27(5):380-388. doi: 10.1136/bmjqs-2017-006986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Medicare & Medicaid Services. Decision memo for transcatheter aortic valve replacement (TAVR) (CAG-00430R). https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=293. Accessed December 15, 2019.
- 19.Hess EP, Coylewright M, Frosch DL, Shah ND. Implementation of shared decision making in cardiovascular care: past, present, and future. Circ Cardiovasc Qual Outcomes. 2014;7(5):797-803. doi: 10.1161/CIRCOUTCOMES.113.000351 [DOI] [PubMed] [Google Scholar]
- 20.Elkin EB, Kim SHM, Casper ES, Kissane DW, Schrag D. Desire for information and involvement in treatment decisions: elderly cancer patients’ preferences and their physicians’ perceptions. J Clin Oncol. 2007;25(33):5275-5280. doi: 10.1200/JCO.2007.11.1922 [DOI] [PubMed] [Google Scholar]
- 21.Davis DA, Mazmanian PE, Fordis M, Van Harrison R, Thorpe KE, Perrier L. Accuracy of physician self-assessment compared with observed measures of competence: a systematic review. JAMA. 2006;296(9):1094-1102. doi: 10.1001/jama.296.9.1094 [DOI] [PubMed] [Google Scholar]
- 22.Pieterse AH, Stiggelbout AM, Montori VM. Shared decision making and the importance of time. JAMA. 2019;322(1):25-26. doi: 10.1001/jama.2019.3785 [DOI] [PubMed] [Google Scholar]
- 23.Coylewright M, Branda M, Inselman JW, et al. Impact of sociodemographic patient characteristics on the efficacy of decision aids: a patient-level meta-analysis of 7 randomized trials. Circ Cardiovasc Qual Outcomes. 2014;7(3):360-367. doi: 10.1161/HCQ.0000000000000006 [DOI] [PubMed] [Google Scholar]
- 24.Wang TY, Grines C, Ortega R, et al. Women in interventional cardiology: update in percutaneous coronary intervention practice patterns and outcomes of female operators from the National Cardiovascular Data Registry. Catheter Cardiovasc Interv. 2016;87(4):663-668. doi: 10.1002/ccd.26118 [DOI] [PubMed] [Google Scholar]
- 25.Antonoff MB, David EA, Donington JS, et al. Women in thoracic surgery: 30 years of history. Ann Thorac Surg. 2016;101(1):399-409. doi: 10.1016/j.athoracsur.2015.11.014 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix 1. Development of Severe Aortic Stenosis Decision Aid
eAppendix 2. Patient Surveys
eFigure 1. Prior Version of Severe Aortic Stenosis Decision Aid
eFigure 2. Shared Decision-Making Checklist for Severe Aortic Stenosis Choice
eFigure 3. Changes in Decisional Quality Outcomes With Multiple Uses of Patient Decision Aid
eTable 1. Shared Decision-Making (Observer OPTION5) Score Scale
eTable 2. Raters’ Agreement for Observer OPTION5
eTable 3. Themes Generated From Qualitative Analysis of Clinician Semi-Structured Interviews, With Supportive Quotes
eReferences