Abstract
This cross-sectional study compares health care spending among high-deductible health plan vs traditional plan enrollees with substance use and mental health disorders.
High-deductible health plans (HDHPs) have proliferated in the US in recent years.1 Such plans are heterogenous and sometimes paired with savings accounts or transparency tools. Cost savings may come at a price if increased financial strain associated with high deductibles leads to poorer health outcomes. Little is known about health care spending among HDHP enrollees with substance use and mental health (SU/MH) disorders. These conditions are highly prevalent,2 undertreated,3 and high cost,4 which may exacerbate the effects of HDHPs.
Methods
Using the Truven Health MarketScan database (January 1, 2011, to December 31, 2016), we identified enrollees who were continuously enrolled in HDHPs and traditional plans for at least 12 months. HDHPs were defined in MarketScan as a statutory HDHP, meaning they had a sufficiently large deductible coupled with a tax-advantaged health savings account. Traditional plans included a mix of lower-deductible plans, such as preferred provider organizations and health maintenance organizations. This study was approved and found to be exempt from informed consent by the Johns Hopkins Bloomberg School of Public Health institutional review board. For these reasons, patient consent was also waived.
We identified plan enrollees with at least 2 uniquely dated SU/MH claims using a standard set of International Classification of Diseases, Ninth Revision codes5,6 and hand verifying a Centers for Medicare & Medicaid Services International Statistical Classification of Diseases and Related Health Problems, Tenth Revision crosswalk. Enrollees were classified as having 1 or more disorders: opioid use, alcohol use, other substance use, anxiety or posttraumatic stress, adjustment, depressive, schizophrenia, bipolar, or other mental health disorders. We selected a 20% random sample of enrollees without SU/MH disorders for comparison.
Spending categories included total health care spending defined as both plan spending and out-of-pocket (OOP) spending (ie, deductibles, cost sharing), OOP spending alone, and the share of total spending paid OOP. We also examined inpatient, outpatient, and pharmaceutical spending separately.
Unadjusted outcomes were compared for enrollees with and without an SU/MH disorder by health care plan type using 2-sided difference of mean significance tests and a significance threshold of .01. We repeated this analysis for each of the SU/MH disorder categories. Analyses were performed using Stata version 14.2 (StataCorp). Analysis began October 2019.
Results
In all, our analysis included 52 230 886 person-years of data with a mean (SD) age of 34.75 (17.73) years; 28 815 776 (55.17%) were female. Overall spending was higher for those in traditional plans than those in HDHPs, with a greater difference among those with an SU/MH disorder ($912) than those without ($667) (Table). Although overall spending was higher in traditional plans than HDHPs for both populations, OOP spending was substantially higher for those in HDHPs compared with traditional plans, especially for those with SU/MH disorders ($573 vs $280).
Table. Annual Mean Total and OOP Spending Comparing Traditional and HDHP Enrollees With and Without SU/MH Disorder, 2011-2016a.
| Variable | Enrollees with an SU/MH disorder | Enrollees without an SU/MH disorder | With vs without an SU/MH disorder | ||||
|---|---|---|---|---|---|---|---|
| Traditional (n = 27 485 702) | HDHP (n = 1 624 961) | Difference | Traditional (n = 21 564 925) | HDHP (n = 1 555 298) | Difference | ||
| Overall health care spending, mean (SD), $ | |||||||
| Total | 7924 (15 971) | 7012 (15 285) | −912b | 3447 (9924) | 2781 (8814) | −667b | −246c |
| OOP | 1034 (1387) | 1607 (1807) | 573b | 511 (953) | 791 (1317) | 280b | 293c |
| Inpatient spending, mean (SD), $ | |||||||
| Total | 1618 (8631) | 1320 (7743) | −298b | 650 (5271) | 505 (4577) | −146b | −153c |
| OOP | 87 (509) | 118 (675) | 31b | 42 (349) | 59 (477) | 17b | 14c |
| Outpatient spending, mean (SD), $ | |||||||
| Total | 4692 (9556) | 4372 (9546) | −320b | 2155 (6141) | 1821 (5521) | −334b | 14 |
| OOP | 719 (1070) | 1165 (1479) | 446b | 369 (746) | 608 (1078) | 238b | 207c |
| Pharmaceutical spending, mean (SD), $ | |||||||
| Total Rx spending | 1614 (5255) | 1320 (5057) | −294b | 642 (3415) | 455 (3107) | −187b | −107c |
| OOP Rx spending | 228 (441) | 324 (646) | 95b | 100 (286) | 124 (409) | 25b | 72c |
Abbreviations: HDHP, high-deductible health plan; OOP, out-of-pocket; Rx, prescription; SU/MH, substance use and mental health.
Study sample includes person-years continuously enrolled for at least 12 calendar months without switching plans with and without an SU/MH disorder. HDHP by definition had a minimum statutory deductible ($1200 for 2011-2012, $1250 for 2013-2014, $1300 for 2015-2016) and a health savings account.
Traditional vs HDHP difference significantly different from 0 at the P < .01 level.
Enrollees with and without an SU/MH disorder significantly different from 0 at the P < .01 level.
Larger differentials in total and OOP spending in HDHPs compared with traditional plans were detected for the group with SU/MH disorders within subcategories of inpatient and pharmaceutical spending. There was no significant difference in total outpatient spending in HDHPs compared with traditional plans between the group with SU/MH disorders compared with those without ($320 vs $334). However, the outpatient OOP spending difference between HDHPs and traditional plans was almost double in the SU/MH group compared with the group without these disorders ($446 vs $238).
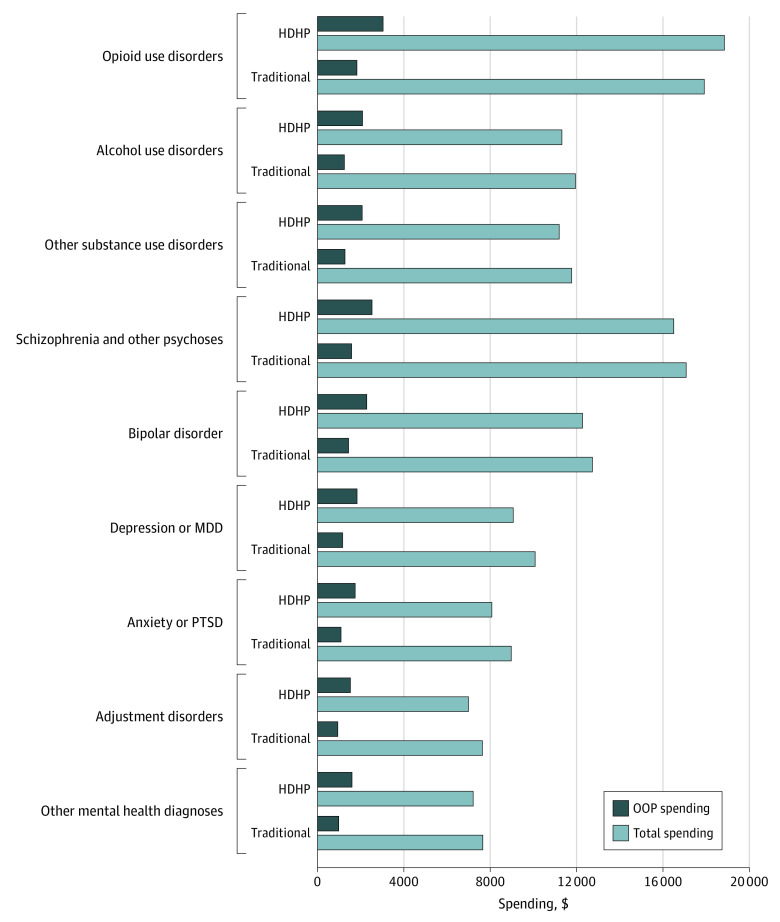
The Figure presents spending differences by SU/MH diagnosis. Across all categories, HDHP enrollees had significantly higher OOP spending compared with traditional plan enrollees.
Figure. Annual Mean Total and OOP Spending Comparing Traditional and HDHP Enrollees With an SU/MH Disorder, 2011-2016.
HDHP indicates high-deductible health plans; MDD, major depressive disorder; OOP, out-of-pocket; PTSD, posttraumatic stress disorder; SU/MH, substance use and mental health.
Study sample includes person-years continuously enrolled for at least 12 calendar months without switching plans and with an SU/MH disorder. All HDHP vs traditional plan differences are significant at the P < .01 level. HDHP by definition had a minimum statutory deductible ($1200 for 2011-2012, $1250 for 2013-2014, $1300 for 2015-2016) and a health savings account. Our sample included 744 662; 1 663 664; 927 951; 789 035; 1 913 966; 12 136 751; 14 691 013; 7 225 202; 10 511 968 person-years of data for the opioid use disorder, alcohol use disorder, other substance use disorder, schizophrenia, bipolar, depression, anxiety, adjustment, and other mental health categories, respectively. Note that some individuals may have had multiple conditions.
Discussion
Commercially insured HDHP enrollees with SU/MH disorder diagnoses had 12% less in overall health care spending than traditional plan enrollees. However, OOP spending was 55% higher in the HDHP group and the share of spending paid OOP was 23 percentage points higher in the HDHP group. This suggests that HDHPs might be posing differential barriers for enrollees with SU/MH disorders compared with enrollees with other conditions. Because baseline spending among those with SU/MH disorders is much higher than the general population, financial strain associated with OOP spending in HDHPs may hit those with SU/MH disorders significantly harder. This study did not examine selection into different plan types or differences in networks across plans. Future research is needed to understand the causes of the differences observed in this study.
References
- 1.Kaiser Family Foundation Percentage of covered workers enrolled in an HDHP/HRA or HSA-qualified HDHP, 2006-2018. Accessed May 1, 2019. https://www.kff.org/report-section/2018-employer-health-benefits-survey-section-8-high-deductible-health-plans-with-savings-option/attachment/figure-8-5/
- 2.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617-627. doi: 10.1001/archpsyc.62.6.617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stephenson J. Mental disorders undertreated. JAMA. 2000;283(3):325."https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=10647784&dopt=Abstract" . doi: 10.1001/jama.283.3.325-JHA90011-2-110647784 [DOI] [Google Scholar]
- 4.Roehrig C. Mental disorders top the list of the most costly conditions in the United States: $201 billion. Health Aff (Millwood). 2016;35(6):1130-1135. doi: 10.1377/hlthaff.2015.1659 [DOI] [PubMed] [Google Scholar]
- 5.Stuart EA, Barry CL, Donohue JM, et al. Effects of accountable care and payment reform on substance use disorder treatment: evidence from the initial 3 years of the alternative quality contract. Addiction. 2017;112(1):124-133. doi: 10.1111/add.13555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kennedy-Hendricks A, Epstein AJ, Stuart EA, et al. Federal parity and spending for mental illness. Pediatrics. 2018;142(2):e20172618. doi: 10.1542/peds.2017-2618 [DOI] [PMC free article] [PubMed] [Google Scholar]