Key Points
Question
Is there an association between visit-to-visit blood pressure variability in early adulthood and myocardial structure and function in middle age?
Findings
In this cohort study including 2400 participants, greater visit-to-visit variability in systolic and diastolic blood pressure in young adulthood was associated with higher left-ventricular mass, higher left-ventricular filling pressures, impaired left-ventricular relaxation, and greater global longitudinal strain.
Meaning
Greater visit-to-visit systolic and diastolic blood pressure variability in early adulthood appears to be associated with adverse alterations in cardiac structure as well as systolic and diastolic function in middle age.
Abstract
Importance
Long-term blood pressure (BP) variability has emerged as a reproducible measure that is associated with heart failure independent of systemic BP. Visit-to-visit BP variability may be associated with the risk of heart failure early in the life course and thus may be reflected in subclinical alterations in cardiac structure and function.
Objective
To evaluate the association between visit-to-visit BP variability in early adulthood and myocardial structure and function in middle age.
Design, Setting, and Participants
This cohort study used data from the Coronary Artery Risk Development in Young Adults (CARDIA) study, a community-based cohort study of 5115 participants aged 18 to 30 years at baseline (year 0; March 25, 1985, to June 7, 1986) and followed up over a 30-year interval. A total of 2400 CARDIA study participants underwent evaluation at 4 field sites (Birmingham, Alabama; Oakland, California; Chicago, Illinois; and Minneapolis, Minnesota). Blood pressure was measured at 8 visits over a 25-year interval and participants received echocardiograms at year 25 (June 1, 2010, to August 31, 2011). Data analysis was conducted from June 7, 1986, to August 31, 2011.
Exposures
Visit-to-visit systolic and diastolic BP variability measures included SD, average real variability, and variability independent of the mean.
Main Outcomes and Measures
Echocardiographic indices of myocardial structure, systolic function, and diastolic function at the year 25 examination.
Results
Of the 2400 participants, 1024 were men (42.7%) and 976 were African American (40.7%); mean (SD) age at the year 25 examination was 50.4 (3.6) years. Per 1-SD increment, greater visit-to-visit systolic BP variability independent of the mean was associated with higher left-ventricular (LV) mass index (β [SE], 2.66 [0.4] g/m2, P < .001), worse diastolic function (early peak diastolic mitral annular velocity [é]) (β [SE], −0.40 [0.1] cm/s, P < .001), higher LV filling pressures (mitral inflow velocity to early diastolic mitral annular velocity [E/é]) β [SE], 0.37 [0.1] cm/s, P < .001), and worse global longitudinal strain (β [SE], 0.17 [0.1], P = .002). Similarly, greater visit-to-visit diastolic BP variability was associated with higher LV mass index (β [SE], 3.21 [0.5] g/m2, P < .001), worse diastolic function (é: β [SE], −0.24 [0.1] cm/s [P < .001]; E/é: β [SE], 0.23 [0.1] cm/s [P < .001]), and worse global longitudinal strain (β [SE], 0.13 [0.1], P = .02). The findings remained consistent when other BP variability measures were used (SD and average real variability).
Conclusions and Relevance
In this cohort study using data from the CARDIA study, greater visit-to-visit systolic and diastolic BP variability have been associated with adverse alterations in cardiac structure as well as systolic and diastolic function independent of mean BP levels.
This cohort study examines the association between blood pressure variability in early adulthood and myocardial structure and function in middle age.
Introduction
Blood pressure (BP) is an inherently dynamic physiologic measure that can fluctuate over time. Rather than representing measurement error in the assessment of an individual’s true BP, long-term visit-to-visit BP variability has emerged as a risk measure that can be reliably reproduced.1
Evidence suggests that, independent of systemic BP levels, greater visit-to-visit BP variability is associated with an increased risk of heart failure.2,3 The underlying mechanisms that support observed associations between long-term BP variability and heart failure are, however, incompletely understood. In this context, it is established that cardiac remodeling precedes the onset of cardiovascular disease, such as heart failure.4 Potential associations between visit-to-visit BP variability and alterations in myocardial structure and function may therefore further elucidate reported associations with cardiovascular disease outcomes, particularly heart failure. We therefore investigated the association between visit-to-visit systolic and diastolic BP variability and echocardiographic features associated with heart failure.
Methods
Study Design and Participants
This cohort study used data from the Coronary Artery Risk Development in Young Adults (CARDIA) study; the design and participant selection of that study has been previously published.5 In summary, the CARDIA study is a community-based cohort study that recruited 5115 white and African American men and women participants from 4 US field sites (Birmingham, Alabama; Oakland, California; Chicago, Illinois; and Minneapolis, Minnesota). The study was approved by the institutional review boards at each site, and all participants provided written informed consent. Participants did not receive financial compensation.
Participants were aged 18 to 30 years at the baseline examination from March 25, 1985, to June 7, 1986 (year 0). Follow-up examinations were conducted at year 2 (response rate, 91%), year 5 (86%), year 7 (81%), year 10 (79%), year 15 (74%), year 20 (72%), year 25 (72%), and year 30 (71%). Among the 3498 participants who attended the CARDIA year 25 examination (June 1, 2010, to August 31, 2011), we included persons with documented systolic and diastolic BP measurements in 8 examinations who were free of cardiovascular disease, resulting in an analytic sample of 2400 participants. In an additional sensitivity analysis to further test the robustness of the findings, we examined a subset of participants (n = 1698) who never used BP-lowering medications and had a mean BP level of less than 130/80 mm Hg.
Visit-to-Visit BP Variability
Blood pressure was measured using standardized protocols across all study examinations. Participants were asked to fast and abstain from heavy physical activity for at least 12 hours before evaluation. Participants were then seated in a quiet room for 5 minutes, and trained staff obtained 3 readings from the brachial artery. The mean of the second and third BP readings was used. In the years 0 to 15 examinations, a random zero sphygmomanometer was used. However, for the years 20 and 25 examinations, because of concerns about mercury contained in the apparatus, automated oscillometric BP monitors were used. A calibration study was performed, and values standardized to the sphygmomanometric measures were used for CARDIA study years 20 and 25 BP measurements to limit measurement bias.6 Visit-to-visit systolic and diastolic BP variability from years 0 to 25 was the exposure of interest in the present study. Variability measures used were SD, average real variability (ARV), and variability independent of the mean (VIM).
Average real variability was calculated using the following formula:
 , ,
|
where N denotes the number of BP measurements in the analytic data set (N = 8) and ARV represents the absolute difference between successive BP measurements. In contrast to SD, ARV takes the order of BP measurements into account when quantifying BP variability. Because both SD and ARV are partly dependent on changes in systemic BP levels, biases from systemic changes in BP levels may be present even after adjustments in regression models.7 We therefore also determined the VIM,8 which was calculated as the SD divided by the within-individual mean to the power p and multiplied by the mean value of the systolic or diastolic BP in the cohort to the power p.
Covariates
The CARDIA study risk factor assessments have been described previously.9,10 In summary, covariates were obtained using a combination of self-reported standardized questionnaires, clinical data, and laboratory data. Weight and height were measured with standardized procedures and used to calculate body mass index (BMI) (calculated as weight in kilograms divided by height in meters squared). Smoking status was self-reported using standardized questions and documented as never, former, or current smokers. Antihypertensive medication use was assessed by self-report and review of medical records. A modified version of the Minnesota Leisure Time Physical Activity questionnaire was used to capture moderate to vigorous physical activity. Fasting samples were collected using standardized protocols. Plasma cholesterol levels were assessed using enzymatic assays by Northwest Lipids Research Laboratory.
Echocardiographic Evaluation
The year 25 examination echocardiographic protocol has been reported previously.11,12 In brief, the year 25 examination followed guidelines of the American Society of Echocardiography.13 Trained sonographers used a commercially available ultrasonographic system (Artida; Toshiba Medical Systems) with a 1.8- to 4.2-MHz phased-array transducer to acquire images from all field sites, and experienced readers at a core reading center interpreted digitized images. Left-ventricular (LV) mass was derived from the Devereux formula. Left-atrial and LV volumes were estimated from apical views. Left-ventricular ejection fraction (LVEF) was calculated from LV end-diastolic and end-systolic volumes. Tissue Doppler was used to assess the peak early diastolic velocity (E) and early peak diastolic mitral annular velocity (é). The mean of the septal and lateral mitral annular velocities was used. A more positive E/é (mitral inflow velocity to early diastolic mitral annular velocity) represents higher LV filling pressures, and a more negative é denotes impaired LV relaxation. Higher LV filling pressures and impairments in LV relaxation are representative of worse diastolic function. Speckle tracking echocardiography was performed (Advanced Cardiology Package 2D Wall Motion Tracking, version 3.0; Toshiba Medical Systems Co). Global longitudinal strain was defined as the peak systolic change in the segment length relative to the length at end-diastole and was represented as a percentage. Global longitudinal strain has increased prognostic value over LVEF, and a more positive global longitudinal strain represents worse myocardial deformation (systolic function).14 The year 25 echocardiographic examination had excellent reproducibility.11
Statistical Analysis
Data analysis was conducted from June 7, 1986, to August 31, 2011. Continuous variables are presented as mean (SD). Categorical variables are reported as frequency and proportion. Pearson correlation coefficients were computed for BP variability measures. The primary goal of the analysis was to assess the association between visit-to-visit BP variability measures and echocardiographic outcomes. We therefore used multivariable linear regression models to assess visit-to-visit variability in systolic and diastolic BP (explanatory variables) and echocardiographic outcomes (dependent variable separate models for each: LV mass, left-atrial volume, LVEF, global longitudinal strain, E/é, and é). Models were adjusted for year 25 covariates: age, sex, race, educational level, BMI, smoking status, fasting glucose level, high-density lipoprotein cholesterol level, total cholesterol level, physical activity, and antihypertensive medication use (year 0 to year 25). In models assessing BP variability using SD and ARV, we additionally adjusted for mean BP level. To examine the possibility that BP-lowering medications and hypertension can have residual effects even after statistical adjustment, we carried out a sensitivity analysis in a subset of study participants who had a mean BP level less than 130/80 mm Hg and never used any BP medications in any study visit. Racial or sex differences in the association between BP variability and echocardiographic outcomes were assessed. Collinearity was not detected based on a variance inflation factor of less than 2.5. A 2-tailed P value <.05 was considered to be statistically significant. All analysis was performed using Stata, version 15.1 (StataCorp).
Results
Population characteristics are presented in Table 1. Mean (SD) age at the year 25 examination was 50.4 (3.6) years; 1024 participants were men (42.7%), and 976 were African American (40.7%). At the year 25 examination, the mean (SD) BMI was 29.9 (7.1) and 319 participants (13.3%) were current smokers. Mean (SD) systolic BP was 117.9 (15.3) mm Hg and mean (SD) diastolic BP was 73.3 (10.9) mm Hg. Mean (SD) visit-to-visit systolic BP VIM was 8.4 (3.4), whereas mean (SD) diastolic BP VIM was 7.2 (2.8). The distribution of systolic and diastolic BP is illustrated in a histogram (eFigure in the Supplement). Systolic BP SD and ARV were moderately correlated (Pearson r = 0.59). Both systolic BP VIM and mean systolic BP (Pearson r = 0.03) and diastolic BP VIM and mean diastolic BP (Pearson r = 0.002) were poorly correlated. Compared with the excluded participants in the overall cohort, the analytic sample was more likely to be men, to be African American, and to have lower systolic BP, and there was no statistically significant difference in diastolic BP (eTable 1 in the Supplement).
Table 1. Population Characteristicsa.
| Characteristic | CARDIA study year 25 examination (n = 2400) |
|---|---|
| Age, y | 50.4 (3.6) |
| Sex, No. (%) | |
| Women | 1376 (57.3) |
| Men | 1024 (42.7) |
| African American, No. (%) | 976 (40.7) |
| BMI | 29.9 (7.1) |
| Antihypertensive medication use, No. (%) | 587 (24.5) |
| Current smoking, No. (%) | 319 (13.3) |
| Physical activity, EU | 345.0 (276.5) |
| Fasting plasma glucose level, mg/dL | 98.7 (26.4) |
| Total cholesterol level, mg/dL | 193.1 (36.4) |
| Blood pressure parameters, mm Hg | |
| Systolic | 117.9 (15.3) |
| Diastolic | 73.3 (10.9) |
| Visit-to-visit, mm Hg | |
| Systolic ARV | 1.16 (2.2) |
| Diastolic ARV | 0.7 (1.8) |
| Systolic SD | 8.5 (4.1) |
| Diastolic SD | 7.1 (2.9) |
| Systolic VIM | 8.4 (3.4) |
| Diastolic VIM | 7.2 (2.8) |
| Echocardiographic measures | |
| LV mass, g | 167.2 (51.4) |
| LA volume, mL | 49.5 (15.5) |
| LV ejection fraction, % | 61.7 (6.9) |
| Global longitudinal strain, % | −15.2 (2.4) |
| E/é | 7.7 (2.2) |
| é, cm/s | 10.6 (2.3) |
Abbreviations: ARV, average real variability; BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); CARDIA, Coronary Artery Risk Development in Young Adults; E, peak early diastolic velocity; é, early peak diastolic mitral annular velocity; E/é, mitral inflow velocity to early diastolic mitral annular velocity; EU, exercise units; LA, left atrial; LV, left ventricular; VIM, variability independent of the mean.
SI unit conversion: To convert glucose to millimoles per liter, multiply by 0.0555; total cholesterol to millimoles per liter, multiply by 0.0259.
Data are presented as mean (SD) unless otherwise indicated.
In the Figure, linear prediction plots with 95% CIs show the association between visit-to-visit systolic BP variability and echocardiographic measures. As given in Table 2, per 1-SD increment, greater visit-to-visit systolic BP VIM was associated with higher LV mass index (β [SE], 2.66 [0.4]; P < .001), worse diastolic function (é) (β [SE], −0.40 [0.1]; P < .001), higher LV filling pressures (E/é) (β [SE], 0.37 [0.1]; P < .001), and worse global longitudinal strain (β [SE], 0.17 [0.1]; P = .002). Similarly, as reported in Table 3, greater visit-to-visit diastolic BP VIM was associated with higher LV mass index (β [SE], 3.21 [0.5]; P < .001), worse diastolic function (é: β [SE], −0.24 [0.1]; P < .001; E/é: β [SE], 0.23 [0.1]; P < .001), and worse global longitudinal strain (β [SE], 0.13 [0.1]; P = .02). We did not observe any association between visit-to-visit BP variability and either LVEF or left atrial volume. The findings remained consistent when 2 other BP variability measures were used (SD and ARV). There were no statistically significant racial or sex differences in the associations between BP variability and echocardiographic outcomes. We conducted a sensitivity analysis in a subset of participants who never used BP medications and had a mean BP level less than 130/80 mm Hg (n = 1698) (eTable 2 and eTable 3 in the Supplement). In this subset, the magnitude of associations between visit-to-visit systolic and diastolic BP variability and echocardiographic outcomes was attenuated, but the findings were consistent overall. In a sensitivity analysis, visit-to-visit systolic and diastolic BP variability was also associated with LV hypertrophy and diastolic dysfunction (eTable 4 in the Supplement).
Figure. Linear Plots for the Association Between Systolic Blood Pressure (BP) Variability and Echocardiographic Outcomes.
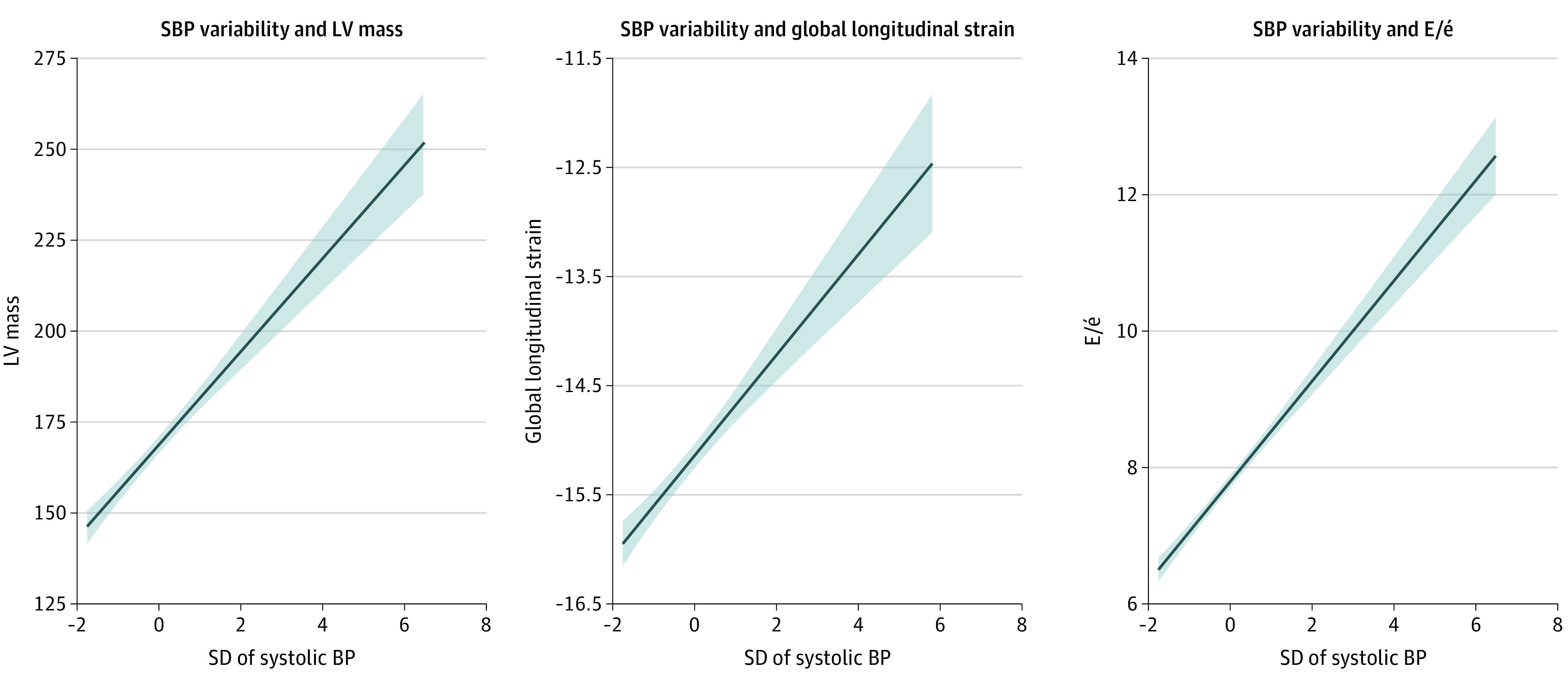
Linear prediction plots and 95% CIs for the association between systolic BP variability (SD) and echocardiographic outcomes: left-ventricular (LV) mass, global longitudinal strain, and higher mitral inflow velocity to early diastolic mitral annular velocity (E/é).
Table 2. Association Between Visit-to-Visit Systolic Blood Pressure Variability and Cardiac Structure and Functiona.
| Characteristic | Systolic VIM | Systolic SD | Systolic ARV | |||
|---|---|---|---|---|---|---|
| Unadjusted β (SE) | Adjusted β (SE) | Unadjusted β (SE) | Adjusted β (SE) | Unadjusted β (SE) | Adjusted β (SE) | |
| LVMi | 1.85 (0.5) | 2.66 (0.4) | 5.19 (0.5) | 3.47 (0.5) | 2.67 (0.5) | 2.54 (0.4) |
| P value | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 |
| LAVi | 0.33 (0.2) | 0.20 (0.2) | 0.78 (0.15) | 0.32 (0.2) | 0.45 (0.2) | 0.24 (0.2) |
| P value | .02 | .19 | <.001 | .07 | .004 | .13 |
| LVEF | 0.33 (0.1) | 0.14 (0.2) | 0.19 (0.2) | 0.12 (0.2) | 0.07 (0.2) | −0.04 (0.2) |
| P value | .03 | .38 | .22 | .51 | .62 | .80 |
| GLS | 0.19 (0.1) | 0.17 (0.1) | 0.44 (0.1) | 0.18 (0.1) | 0.32 (0.1) | 0.22 (0.1) |
| P value | <.001 | .002 | <.001 | .004 | <.001 | <.001 |
| E/é | 0.55 (0.1) | 0.37 (0.1) | 0.70 (0.1) | 0.45 (0.1) | 0.66 (0.1) | 0.52 (0.1) |
| P value | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 |
| é | −0.51 (0.1) | −0.40 (0.1) | −0.73 (0.1) | −0.47 (0.1) | −0.64 (0.1) | −0.55 (0.1) |
| P value | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 |
Abbreviations: ARV, average real variability; é, early peak diastolic mitral annular velocity; E/é, mitral inflow velocity to early diastolic mitral annular velocity; GLS, global longitudinal strain; LAVi, left-atrial volume index; LV, left-ventricular; LVEF, LV ejection fraction; LVMi, LV mass index; VIM, variability independent of the mean.
Dependent variables were LVMi, LAVi, LVEF, GLS, E/é (more positive values represent worse diastolic function), and é (more negative values denote worse LV relaxation). Independent variables were measures of systolic blood pressure variability: VIM, SD, and ARV. β Represents regression coefficient per SD increments in exposures. Models were adjusted for year 25 covariates: age, sex, race, educational level, body mass index, smoking status, physical activity, fasting glucose level, total cholesterol level, high-density lipoprotein cholesterol level, antihypertensive medication use (year 0 to year 25), and mean systolic blood pressure.
Table 3. Association Between Visit-to-Visit Diastolic Blood Pressure Variability and Cardiac Structure and Functiona.
| Characteristic | Diastolic VIM | Diastolic SD | Diastolic ARV | |||
|---|---|---|---|---|---|---|
| Unadjusted β (SE) | Adjusted β (SE) | Unadjusted β (SE) | Adjusted β (SE) | Unadjusted β (SE) | Adjusted β (SE) | |
| LVMi | 3.33 (0.4) | 3.21 (0.5) | 5.0 (0.4) | 3.57 (0.5) | 2.66 (0.5) | 2.39 (0.5) |
| P value | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 |
| LAVi | 0.59 (0.1) | 0.38 (0.2) | 0.61 (0.2) | 0.43 (0.2) | 0.29 (0.2) | 0.17 (0.2) |
| P value | <.001 | .02 | <.001 | .009 | .05 | .29 |
| LVEF | 0.04 (0.2) | 0.04 (0.2) | −0.05 (0.2) | 0.01 (0.2) | 0.05 (0.1) | 0.14 (0.2) |
| P value | .80 | .80 | .73 | .97 | .74 | .39 |
| GLS | 0.18 (0.1) | 0.13 (0.1) | 0.38 (0.1) | 0.14 (0.1) | 0.35 (0.1) | 0.21 (0.1) |
| P value | .001 | .02 | <.001 | .02 | <.001 | <.001 |
| E/é | 0.36 (0.1) | 0.23 (0.1) | 0.48 (0.1) | 0.26 (0.1) | 0.48 (0.1) | 0.36 (0.1) |
| P value | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 |
| é | −0.30 (0.1) | −0.24 (0.1) | −0.51 (0.1) | −0.27 (0.1) | −0.54 (0.1) | −0.47 (0.1) |
| P value | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 |
Abbreviations: ARV, average real variability; é, early peak diastolic mitral annular velocity; E/é, mitral inflow velocity to early diastolic mitral annular velocity; GLS, global longitudinal strain; LAVi, left-atrial volume index; LV, left-ventricular; LVEF, LV ejection fraction; LVMi, LV mass index; VIM, variability independent of the mean.
Dependent variables were LVMi, LAVi, LVEF, GLS, E/é (more positive values represent worse diastolic function), and é (more negative values denote worse LV relaxation). Independent variables were measures of systolic blood pressure variability: VIM, SD, and ARV. β Represents regression coefficient per SD increments in exposures. Models were adjusted for year 25 covariates: age, sex, race, educational level, body mass index, smoking status, physical activity, fasting glucose level, total cholesterol level, high-density lipoprotein cholesterol level, antihypertensive medication use (year 0 to year 25), and mean systolic blood pressure.
Discussion
In this community-based sample of young adults followed up for 25 years, greater visit-to-visit systolic and diastolic BP variability was associated with unfavorable alteration in myocardial structure and function independent of the mean BP levels. Our findings remained consistent even among a subset of participants who had a mean BP level less than 130/80 mm Hg and had never used BP-lowering medications. Our results are relevant from a public health perspective because even modest population-level increases in echocardiographic indices may have prognostic value for adverse outcomes.4,15 Our study observations lend support to a distinct association of visit-to-visit BP variability with risk of heart failure because of the associations with adverse cardiac remodeling.
To our knowledge, this study is the first to comprehensively investigate the association between long-term BP variability and cardiac remodeling. In 3 small studies that focused on short-term systolic BP variability (≤24 hours), higher systolic BP variability was associated with adverse LV alterations.16,17,18 Taking this finding a step further, Sega et al19 showed that the noncyclical (ie, erratic) component of 24-hour BP variability, but not the routine cyclical BP component, was associated with LV mass. It is plausible that the erratic component of 24-hour BP variability is more closely aligned with long-term BP variability than routine cyclical changes in BP. Our observations add to the scientific literature by providing data on long-term BP variability in a community-based sample with detailed assessment of cardiac structure and function. In the present study, we noted associations of visit-to-visit systolic and diastolic BP variability with higher global longitudinal strain but not with LVEF. Global longitudinal strain is a marker of systolic function that reflects longitudinal myocardial deformation and has been established to provide incremental prognostic value for outcomes compared with LVEF.14,20,21 In our analysis, we found no association between visit-to-visit systolic BP variability and left atrial volume. However, we noted associations between greater visit-to-visit systolic and diastolic BP variability and impaired LV relaxation and higher LV filling pressures, which may precede LA remodeling. Our study observations are notable because cardiac structural and functional alterations can antedate the risk of heart failure22,23 and other cardiovascular disease outcomes in general.15,20,24,25
There is accumulating evidence of pathophysiologic pathways that link greater BP variability with cardiac remodeling. Long-term, visit-to-visit BP variability is associated with factors that are also involved in cardiac remodeling, such as environmental, neurohormonal, and genetic factors, and cardiovascular disease risk burden.26,27,28,29 Studies have shown that BP variability is associated with endothelial dysfunction, coronary atheroma progression,30,31 and arterial remodeling,32,33,34,35 all of which are implicated in cardiac remodeling. In a murine study, mice that had no hypertension but had spontaneous variations in BP were reported to have desensitization of the β2-adrenoceptor, which is important for β-adrenoceptor agonist–induced relaxation in the large arteries.36 By exerting cyclical mechanical stress on the arterial wall, BP variability may facilitate vascular smooth muscle cell proliferation, extracellular matrix deposition, fibrotic changes, and microvascular alterations.37,38 In addition, there is increasing evidence of a possible bidirectional positive feedback loop wherein arterial stiffness indicates the probability of BP variability and increased BP variability can lead to greater arterial stiffness.33,34 Changes in arterial material properties exert a pressure load on the LV that may induce compensatory LV remodeling to normalize wall tension.9,39,40 Blood pressure variability may also have direct effects on cardiac structure and function.41 In another experimental study that performed sinoatrial denervation to produce increases in the variability of BP without changes in mean BP, greater BP variability was associated with perivascular macrophage infiltration, myocardial fibrosis, cardiac hypertrophy, and LV systolic dysfunction.41 Collectively, these reports are supportive of a potential association between BP variability and cardiac structure and function.
Strengths and Limitations
Our study results are strengthened by the use of standardized BP protocols and contemporary echocardiographic assessment in a large, biracial community-based sample; long-term study follow-up with good cohort retention; and the ability to account for a broad range of confounding factors.
Limitations of the study include the possibility of additional variability in periods between study visits. The optimal number of visits to assess BP variability is uncertain; however, it has been reported that at least 6 visits may be sufficient to estimate the cardiovascular disease risk associated with long-term BP variability.1 Ambulatory BP readings were not investigated in the present study; thus, our findings may not be generalizable to this context. Antihypertension medication use, drug dose or type, and medication nonadherence may be associated with BP variability; however, our findings remained consistent even among a subset of participants who never used BP-lowering medications. Because this was an observational study and our analysis did not examine change in echocardiographic indices over time, reverse causation and causal inferences cannot be determined. We attempted to account for confounding factors, but residual confounding from measured or unmeasured variables remains a possibility. Owing to the limited mid-life heart failure events from year 25 in this young cohort, we were not able to assess associations with heart failure. Although excluded CARDIA study participants had a higher comorbidity burden, the analytic sample in the present study represented a diverse cohort with a wide spectrum of cardiovascular risk factors. To the extent that the exclusion of high-risk participants likely biases toward the null, associations between BP variability and myocardial structure and function may be underestimated.
Conclusions
Greater visit-to-visit systolic and diastolic BP variability in young adulthood appears to be associated with unfavorable subclinical alterations in myocardial structure and function by middle age independent of the association with mean BP levels. Our study observations support a distinct association of long-term BP variability with risk of heart failure because of the association of subclinical echocardiographic features with heart failure.
eTable 1. Characteristics of CARDIA Participants at the Year-0 (1985-1986) by Inclusion in Blood Pressure Variability Analysis
eTable 2. Association Between Visit-to-Visit Systolic Blood Pressure Variability and Cardiac Structure and Function Among Participants Who Never Used Anti-Hypertensive Medication and Had Average Blood Pressure <130/80 mm Hg
eTable 3. Association Between Visit-to-Visit Diastolic Blood Pressure Variability and Cardiac Structure and Function Among Participants Who Never Used Anti-Hypertensive Medication and Had Average Blood Pressure <130/80 mm Hg
eTable 4. Sensitivity Analysis Showing the Association Between Systolic Diastolic Blood Pressure Variability and Cardiac Target Organ Damage Phenotypes (Left Ventricular Hypertrophy, Diastolic Dysfunction, and Left Atrial Enlargement)
eFigure. Histogram Showing the Distribution of Systolic and Diastolic Blood Pressure Variability in Analytic Sample
References
- 1.Lim HM, Chia YC, Ching SM, Chinna K. Number of blood pressure measurements needed to estimate long-term visit-to-visit systolic blood pressure variability for predicting cardiovascular risk: a 10-year retrospective cohort study in a primary care clinic in Malaysia. BMJ Open. 2019;9(4):e025322. doi: 10.1136/bmjopen-2018-025322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kwon S, Lee SR, Choi EK, et al. Visit-to-visit variability of metabolic parameters and risk of heart failure: a nationwide population-based study. Int J Cardiol. 2019;293:153-158. doi: 10.1016/j.ijcard.2019.06.035 [DOI] [PubMed] [Google Scholar]
- 3.Muntner P, Whittle J, Lynch AI, et al. Visit-to-visit variability of blood pressure and coronary heart disease, stroke, heart failure, and mortality: a cohort study. Ann Intern Med. 2015;163(5):329-338. doi: 10.7326/M14-2803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nwabuo CC, Moreira HT, Vasconcellos HD, et al. Left ventricular global function index predicts incident heart failure and cardiovascular disease in young adults: the Coronary Artery Risk Development in Young Adults (CARDIA) study. Eur Heart J Cardiovasc Imaging. 2019;20(5):533-540. doi: 10.1093/ehjci/jey123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Friedman GD, Cutter GR, Donahue RP, et al. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol. 1988;41(11):1105-1116. doi: 10.1016/0895-4356(88)90080-7 [DOI] [PubMed] [Google Scholar]
- 6.Yano Y, Reis JP, Levine DA, et al. Visit-to-visit blood pressure variability in young adulthood and hippocampal volume and integrity at middle age: the CARDIA study (Coronary Artery Risk Development in Young Adults). Hypertension. 2017;70(6):1091-1098. doi: 10.1161/HYPERTENSIONAHA.117.10144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rothwell PM. Limitations of the usual blood-pressure hypothesis and importance of variability, instability, and episodic hypertension. Lancet. 2010;375(9718):938-948. doi: 10.1016/S0140-6736(10)60309-1 [DOI] [PubMed] [Google Scholar]
- 8.Yano Y. Visit-to-visit blood pressure variability—what is the current challenge? Am J Hypertens. 2017;30(2):112-114. doi: 10.1093/ajh/hpw124 [DOI] [PubMed] [Google Scholar]
- 9.Nwabuo CC, Moreira HT, Vasconcellos HD, et al. Association of aortic root dilation from early adulthood to middle age with cardiac structure and function: the CARDIA study. J Am Soc Echocardiogr. 2017;30(12):1172-1179. doi: 10.1016/j.echo.2017.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vasconcellos HD, Moreira HT, Ciuffo L, et al. Cumulative blood pressure from early adulthood to middle age is associated with left atrial remodelling and subclinical dysfunction assessed by three-dimensional echocardiography: a prospective post hoc analysis from the coronary artery risk development in young adults study. Eur Heart J Cardiovasc Imaging. 2018;19(9):977-984. doi: 10.1093/ehjci/jey086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Armstrong AC, Ricketts EP, Cox C, et al. Quality control and reproducibility in M-Mode, two-dimensional, and speckle tracking echocardiography acquisition and analysis: the CARDIA study, year 25 examination experience. Echocardiography. 2015;32(8):1233-1240. doi: 10.1111/echo.12832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moreira HT, Nwabuo CC, Armstrong AC, et al. Reference ranges and regional patterns of left ventricular strain and strain rate using two-dimensional speckle-tracking echocardiography in a healthy middle-aged black and white population: the CARDIA study. J Am Soc Echocardiogr. 2017;30(7):647-658.e2. doi: 10.1016/j.echo.2017.03.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28(1):1-39.e14. doi: 10.1016/j.echo.2014.10.003 [DOI] [PubMed] [Google Scholar]
- 14.Russo C, Jin Z, Elkind MS, et al. Prevalence and prognostic value of subclinical left ventricular systolic dysfunction by global longitudinal strain in a community-based cohort. Eur J Heart Fail. 2014;16(12):1301-1309. doi: 10.1002/ejhf.154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Armstrong AC, Jacobs DR Jr, Gidding SS, et al. Framingham score and LV mass predict events in young adults: CARDIA study. Int J Cardiol. 2014;172(2):350-355. doi: 10.1016/j.ijcard.2014.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li CL, Liu R, Wang JR, Yang J. Relationship between blood pressure variability and target organ damage in elderly patients. Eur Rev Med Pharmacol Sci. 2017;21(23):5451-5455. [DOI] [PubMed] [Google Scholar]
- 17.Okada R, Okada A, Okada T, Nanasato M, Wakai K. Visit-to-visit blood pressure variability is a marker of cardiac diastolic function and carotid atherosclerosis. BMC Cardiovasc Disord. 2014;14:188. doi: 10.1186/1471-2261-14-188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shin SH, Jang JH, Baek YS, et al. Relation of blood pressure variability to left ventricular function and arterial stiffness in hypertensive patients. Singapore Med J. 2019;60(8):427-431. doi: 10.11622/smedj.2019030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sega R, Corrao G, Bombelli M, et al. Blood pressure variability and organ damage in a general population: results from the PAMELA study (Pressioni Arteriose Monitorate E Loro Associazioni). Hypertension. 2002;39(2 Pt 2):710-714. doi: 10.1161/hy0202.104376 [DOI] [PubMed] [Google Scholar]
- 20.Cheng S, McCabe EL, Larson MG, et al. Distinct aspects of left ventricular mechanical function are differentially associated with cardiovascular outcomes and all-cause mortality in the community. J Am Heart Assoc. 2015;4(10):e002071. doi: 10.1161/JAHA.115.002071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Biering-Sørensen T, Biering-Sørensen SR, Olsen FJ, et al. Global longitudinal strain by echocardiography predicts long-term risk of cardiovascular morbidity and mortality in a low-risk general population: the Copenhagen City Heart study. Circ Cardiovasc Imaging. 2017;10(3):e005521. doi: 10.1161/CIRCIMAGING.116.005521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Velagaleti RS, Gona P, Pencina MJ, et al. Left ventricular hypertrophy patterns and incidence of heart failure with preserved versus reduced ejection fraction. Am J Cardiol. 2014;113(1):117-122. doi: 10.1016/j.amjcard.2013.09.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yeboah J, Rodriguez CJ, Stacey B, et al. Prognosis of individuals with asymptomatic left ventricular systolic dysfunction in the Multi-Ethnic Study of Atherosclerosis (MESA). Circulation. 2012;126(23):2713-2719. doi: 10.1161/CIRCULATIONAHA.112.112201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bluemke DA, Kronmal RA, Lima JA, et al. The relationship of left ventricular mass and geometry to incident cardiovascular events: the MESA (Multi-Ethnic Study of Atherosclerosis) study. J Am Coll Cardiol. 2008;52(25):2148-2155. doi: 10.1016/j.jacc.2008.09.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Armstrong AC, Liu K, Lewis CE, et al. Left atrial dimension and traditional cardiovascular risk factors predict 20-year clinical cardiovascular events in young healthy adults: the CARDIA study. Eur Heart J Cardiovasc Imaging. 2014;15(8):893-899. doi: 10.1093/ehjci/jeu018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sasaki N, Ozono R, Fujiwara S, Maeda R, Kihara Y. Impaired glucose metabolism is associated with visit-to-visit blood pressure variability in participants without cardiovascular disease. Int J Hypertens. 2018;2018:5126270. doi: 10.1155/2018/5126270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Xu X, Ding X, Zhang X, et al. Genetic and environmental influences on blood pressure variability: a study in twins. J Hypertens. 2013;31(4):690-697. doi: 10.1097/HJH.0b013e32835e2a4a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Spallone V. Blood pressure variability and autonomic dysfunction. Curr Diab Rep. 2018;18(12):137. doi: 10.1007/s11892-018-1108-z [DOI] [PubMed] [Google Scholar]
- 29.Chen H, Zhang R, Zheng Q, Yan X, Wu S, Chen Y. Impact of body mass index on long-term blood pressure variability: a cross-sectional study in a cohort of Chinese adults. BMC Public Health. 2018;18(1):1193. doi: 10.1186/s12889-018-6083-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Eto M, Toba K, Akishita M, et al. Reduced endothelial vasomotor function and enhanced neointimal formation after vascular injury in a rat model of blood pressure lability. Hypertens Res. 2003;26(12):991-998. doi: 10.1291/hypres.26.991 [DOI] [PubMed] [Google Scholar]
- 31.Clark D III, Nicholls SJ, St John J, et al. Visit-to-visit blood pressure variability, coronary atheroma progression, and clinical outcomes. JAMA Cardiol. 2019;4(5):437-443. doi: 10.1001/jamacardio.2019.0751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhou TL, Henry RMA, Stehouwer CDA, van Sloten TT, Reesink KD, Kroon AA. Blood pressure variability, arterial stiffness, and arterial remodeling. Hypertension. 2018;72(4):1002-1010. doi: 10.1161/HYPERTENSIONAHA.118.11325 [DOI] [PubMed] [Google Scholar]
- 33.Miyauchi S, Nagai M, Dote K, et al. Visit-to-visit blood pressure variability and arterial stiffness: which came first: the chicken or the egg? Curr Pharm Des. 2019;25(6):685-692. doi: 10.2174/1381612825666190329122024 [DOI] [PubMed] [Google Scholar]
- 34.Shimbo D, Shea S, McClelland RL, et al. Associations of aortic distensibility and arterial elasticity with long-term visit-to-visit blood pressure variability: the Multi-Ethnic Study of Atherosclerosis (MESA). Am J Hypertens. 2013;26(7):896-902. doi: 10.1093/ajh/hpt040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Boardman H, Lewandowski AJ, Lazdam M, et al. Aortic stiffness and blood pressure variability in young people: a multimodality investigation of central and peripheral vasculature. J Hypertens. 2017;35(3):513-522. doi: 10.1097/HJH.0000000000001192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rocha ML, Silva BR, Lunardi CN, Ramalho LN, Bendhack LM. Blood pressure variability provokes vascular β-adrenoceptor desensitization in rats. Vascul Pharmacol. 2016;82:82-89. doi: 10.1016/j.vph.2016.05.007 [DOI] [PubMed] [Google Scholar]
- 37.Aoki Y, Kai H, Kajimoto H, et al. Large blood pressure variability aggravates arteriolosclerosis and cortical sclerotic changes in the kidney in hypertensive rats. Circ J. 2014;78(9):2284-2291. doi: 10.1253/circj.CJ-14-0027 [DOI] [PubMed] [Google Scholar]
- 38.Hata J, Arima H, Rothwell PM, et al. ; ADVANCE Collaborative Group . Effects of visit-to-visit variability in systolic blood pressure on macrovascular and microvascular complications in patients with type 2 diabetes mellitus: the ADVANCE trial. Circulation. 2013;128(12):1325-1334. doi: 10.1161/CIRCULATIONAHA.113.002717 [DOI] [PubMed] [Google Scholar]
- 39.Ohyama Y, Ambale-Venkatesh B, Noda C, et al. Association of aortic stiffness with left ventricular remodeling and reduced left ventricular function measured by magnetic resonance imaging: the Multi-Ethnic Study of Atherosclerosis. Circ Cardiovasc Imaging. 2016;9(7):e004426. doi: 10.1161/CIRCIMAGING.115.004426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bell V, McCabe EL, Larson MG, et al. Relations between aortic stiffness and left ventricular mechanical function in the community. J Am Heart Assoc. 2017;6(1):e004903. doi: 10.1161/JAHA.116.004903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yasuoka S, Kai H, Kajimoto H, et al. Blood pressure variability activates cardiac mineralocorticoid receptor and induces cardiac remodeling in hypertensive rats. Circ J. 2013;77(6):1474-1481. doi: 10.1253/circj.CJ-12-1253 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Characteristics of CARDIA Participants at the Year-0 (1985-1986) by Inclusion in Blood Pressure Variability Analysis
eTable 2. Association Between Visit-to-Visit Systolic Blood Pressure Variability and Cardiac Structure and Function Among Participants Who Never Used Anti-Hypertensive Medication and Had Average Blood Pressure <130/80 mm Hg
eTable 3. Association Between Visit-to-Visit Diastolic Blood Pressure Variability and Cardiac Structure and Function Among Participants Who Never Used Anti-Hypertensive Medication and Had Average Blood Pressure <130/80 mm Hg
eTable 4. Sensitivity Analysis Showing the Association Between Systolic Diastolic Blood Pressure Variability and Cardiac Target Organ Damage Phenotypes (Left Ventricular Hypertrophy, Diastolic Dysfunction, and Left Atrial Enlargement)
eFigure. Histogram Showing the Distribution of Systolic and Diastolic Blood Pressure Variability in Analytic Sample


