Abstract
Background:
Bone bruises observed on magnetic resonance imaging (MRI) after an anterior cruciate ligament (ACL) injury could provide significant information about ACL injury mechanisms.
Purpose/Hypothesis:
The purpose of this study was to investigate common bone bruise patterns after an ACL injury. It was hypothesized that the most common bone bruise distribution pattern would be only the lateral side of both the femur and tibia.
Study Design:
Cross-sectional study; Level of evidence, 3.
Methods:
Knee MRI scans of patients who underwent acute ACL reconstruction from August 2016 to August 2018 at our institution were selected. Imaging sequences in the sagittal and coronal planes were used for determining the bone bruise location in the lateral-medial and anterior-posterior directions, respectively. The presence, location, and intensity of bone bruises within specific compartments of the tibia and femur were documented. The relative bone bruise patterns of the tibia and femur were classified and analyzed.
Results:
A total of 207 patients (165 men, 42 women) met the inclusion criteria from a total of 4209 ACL reconstruction cases. The most common relative bone bruise pattern was located on only the lateral side of both the femur and the tibia (44.4%), followed by the lateral and medial sides of both the femur and tibia (29.0%). For the pattern found on the lateral and medial sides of both the femur and tibia, the bone bruises on only the lateral side of both the tibia and femur were more severe (P < .001 and P < .001, respectively) and more anterior (P < .001 and P < .001, respectively) than those on only the medial side.
Conclusion:
The most common relative bone bruise pattern observed was on only the lateral side of both the tibia and femur. Bone bruises on the lateral side were more severe than those on the medial side in patients with bone bruises on the lateral and medial sides of both the femur and tibia. Anterior translation of the tibia relative to the femur occurred during an ACL injury based on the location of bone bruises in the anterior-posterior direction.
Keywords: anterior cruciate ligament, magnetic resonance imaging, mechanism, bone bruise
An anterior cruciate ligament (ACL) rupture is one of the most common and devastating injuries in sports.27 The surgical reconstruction cost, length of rehabilitation time, and risk of long-term disability have generated a significant interest in preventing ACL injuries.5,17,35 Understanding ACL loading mechanisms and risk factors for the injury is critical for improving prevention strategies.
Femoral and tibial bone bruises are thought to represent a footprint of impact at the time of the injury, offering insight into the mechanisms of an ACL injury.29,32,33 Previous studies have reported that the most common patterns observed in an ACL injury were bone bruises in the lateral compartment,23,29 which indicated that the valgus load was the primary mechanism of an ACL injury.20 Other studies reported that anterior tibial translation with a small knee flexion angle may be the primary mechanism of an ACL injury based on the observed bone bruises on the posterior tibia and anterior femur.2,34,36,38
Although many studies have been conducted on the bone bruise locations of the femur and tibia in patients with ACL ruptures, these studies separately reported the frequency and location of tibial and femoral bone bruises in patients with ACL injuries,34,36 and little is known regarding the relative bone bruise locations of the tibia and femur. The relative bone bruise locations of the tibia and femur could help us better understand loading patterns during an ACL injury. Additionally, most studies have focused on the lateral-medial direction of bone bruise locations, with little attention to the anterior-posterior direction.1,2,10,19,23,28,31 Further, 2 recent systematic reviews concluded that further studies on bone bruise distribution patterns should be conducted to improve the accuracy of the bone bruise pattern.25,38
Therefore, the purpose of this study was to investigate the common bone bruise patterns after an ACL injury. We hypothesized that the most common bone bruise distribution pattern would be only the lateral side of both the femur and tibia. We also hypothesized that there would be anterior translation of the tibia relative to the femur during an ACL injury based on the location of bone bruises in the anterior-posterior direction.
Methods
Patient Selection
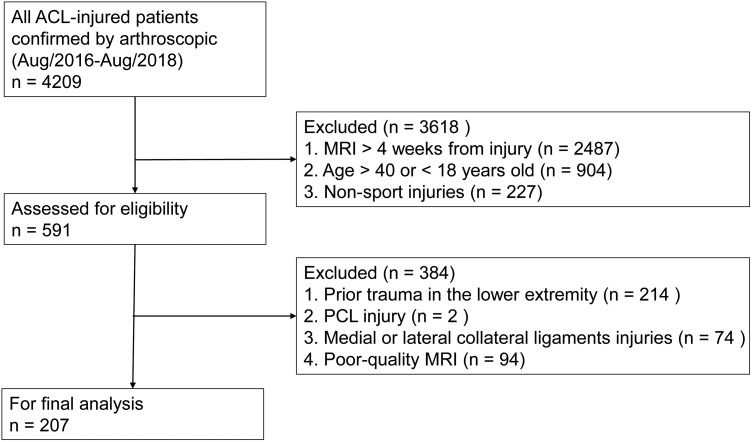
A total of 4209 ACL reconstruction procedures were performed at our institution from August 2016 to August 2018. Of these, 207 patients met the inclusion criteria and were entered into the study. The inclusion criteria were as follows: (1) an ACL rupture confirmed by arthroscopic examination, (2) magnetic resonance imaging (MRI) performed within 4 weeks of the injury, (3) injury sustained during sports activities, and (4) patient age 18 to 40 years. The time from injury to MRI was determined by reviewing the collected clinical notes, which included the date of injury as reported by the patient. Contact or noncontact injury information was also collected routinely through a personal interview during hospitalization. Although a 6-week threshold has commonly been used in the literature, the 4-week threshold was selected to further minimize timing errors12 and preserve the signal characteristics of bone bruises. Given that skeletally immature patients demonstrate unique bone bruise patterns,23 and bone mineral density decreases gradually in patients aged >40 years,13 which could affect the signal characteristics of a bone bruise, only those aged 18 to 40 years were selected. The exclusion criteria included (1) previous trauma to the affected knee, (2) posterior cruciate ligament injuries, (3) medial or lateral collateral ligament injuries, and (4) absent or poor-quality MRI scans (Figure 1). Clinical notes, operative reports, and MRI scans were reviewed to provide detailed injury information. Meniscal and ligamentous injuries were confirmed by MRI, performed by an experienced radiologist, as well as arthroscopic surgery, performed by sports medicine orthopaedic surgeons.
Figure 1.
Flowchart of patient selection. ACL, anterior cruciate ligament; MRI, magnetic resonance imaging; PCL, posterior cruciate ligament.
Institutional review board approval was obtained before proceeding with this study, and the requirement for obtaining informed consent from the patients was waived.
MRI and Determination of Bone Bruise Location
All patients underwent MRI of the injured knee using our standard protocol. Scans were acquired on a 1.5-T scanner (SIGNA; GE Healthcare) with a 3.5-mm slice space and 512 × 512 matrix in the sagittal, coronal, and axial planes. Imaging sequences in the sagittal and coronal planes were used for determining the bone bruise location in the lateral-medial and anterior-posterior directions, respectively.
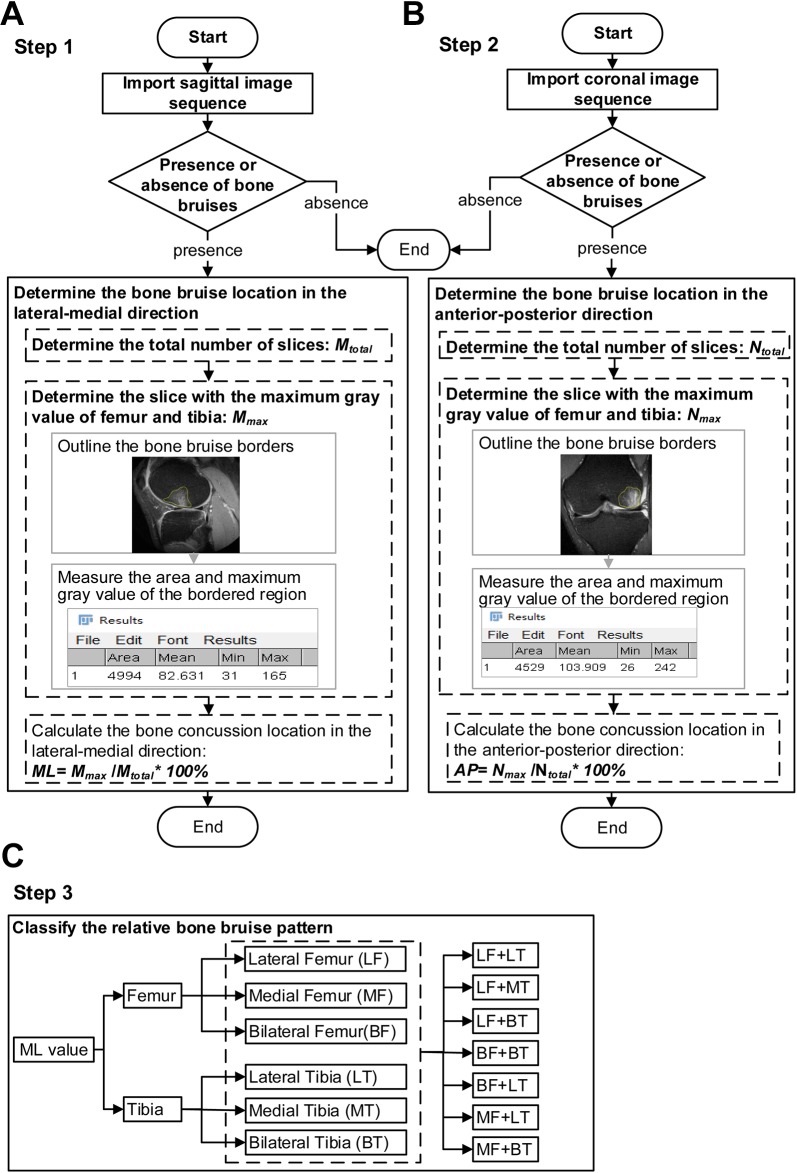
A bone bruise was defined as a traumatically involved, geographic, and nonlinear area of decreased signal intensity on T1-weighted scans and increased signal intensity on T2-weighted scans.21 Participants were first classified according to the presence or absence of bone bruises. For participants with bone bruises, the bone bruise borders were traced using the freehand region-of-interest function of ImageJ software (National Institutes of Health). The gray values recorded based on imaging pixels range from 0 to 255.18 The maximum gray value of the pixel and area of the bordered region were measured using functions in ImageJ. As the gray value of a pixel is determined by the intensity of the MRI signal of the voxel represented,8 the signal intensity on MRI could indicate impact on the bone.4 The gray value was used to evaluate the severity of bone bruises within 1 imaging sequence in the present study, and a greater gray value represented a larger signal intensity and thus more severe bone impact. The slice that showed the maximum gray value was considered where the bone impacted. In case the different slices of 1 bone bruise showed the same maximum gray value, the areas of bone bruises were used to further determine the slice where the bone impacted. The bone bruise location in the lateral-medial direction was first determined using the sagittal imaging sequence (Figure 2A), and the location in the anterior-posterior direction was then determined using the coronal imaging sequence (Figure 2B).
Figure 2.
Protocol of determining the bone bruise location. (A) Determine the bone bruise location in the lateral-medial direction using the sagittal imaging sequence. (B) Determine the bone bruise location in the anterior-posterior direction using the coronal imaging sequence. (C) Classify the relative bone bruise pattern.
The bone bruise locations in the lateral-medial and anterior-posterior directions of the tibia and femur were recorded separately. The precise bone bruise location in the lateral-medial direction was determined using the following formula:
where Mmax is the number of the slice at which the gray value is maximum among all the slices in the order of lateral to medial sides in the sagittal plane, and Mtotal is the total number of slices in the sagittal plane based on the presence of bone segments. ML is a measure of the location in the lateral-medial direction, and it ranges in value from 0% (closer to the lateral side of the bone) to 100% (closer to the medial side of the bone).
The precise bone bruise location in the anterior-posterior direction was determined using the following formula:
where Nmax is the number of the slice at which the gray value is maximum among all the slices in the order of anterior to posterior sides in the coronal plane, and Ntotal is the total number of slices in the coronal plane based on the presence of bone segments. AP is a measure of the location in the anterior-posterior direction, and it ranges in value from 0% (closer to the anterior side of the bone) to 100% (closer to the posterior side of the bone).
The relative bone bruise patterns of the tibia and femur were further classified based on the documented location in the lateral-medial direction after the abovementioned determination of the bone bruise (Figure 2C). For the femur and tibia, the classification of the bone bruise location was the (1) lateral (only 1 measure of the location in the lateral-medial direction [ML value] <50%), (2) medial (only 1 ML value ≥50%), or (3) lateral and medial (1 ML value <50% and another value ≥50%) parts of the bone. The 7 relative bone bruise patterns in this study include bone bruises located on (1) the lateral and medial sides of both the femur and the tibia (BF + BT), (2) the lateral and medial sides of the femur and the lateral side only of the tibia (BF + LT), (3) only the lateral side of both the femur and the tibia (LF + LT), (4) only the lateral side of the femur and the lateral and medial sides of the tibia (LF + BT), (5) only the lateral side of the femur and only the medial side of the tibia (LF + MT), (6) only the medial side of the femur and the lateral and medial sides of the tibia (MF + BT), and (7) only the medial side of the femur and only the lateral side of the tibia (MF + LT). Other bone bruise patterns, such as only the medial side of both the femur and tibia (MF + MT) as well as the lateral and medial sides of the femur and only the medial side of the tibia (BF + MT), may also occur. This study found only the initial 7 relative bone bruise patterns above.
MRI scans were read by 2 orthopaedic researchers (1 sports medicine doctor [Z.L.] and 1 physical therapist [H.S.]). To assess the interrater reliability of bone bruise assessments, intraclass correlation coefficients (ICCs) were calculated by randomly selecting 20 sets of MRI scans. The 2 MRI observers separately defined the presence or absence of bone bruises and the location of femoral bone bruises in the lateral-medial and anterior-posterior directions. The interrater ICCs were 1.00 (P < .001) for the presence or absence of bone bruises. The interrater ICCs also showed excellent reliability for the location of femoral bone bruises in the lateral-medial (ICC, 0.954; P < .001) and anterior-posterior directions (ICC, 0.961; P < .001).
Statistical Analysis
Demographic characteristics of the patients involving categorical variables were summarized using counts and percentages. Continuous variables were reported as means ± SDs. Paired t tests were used to compare the location in the anterior-posterior direction between the lateral and medial compartments. Given the discrepancy between the MRI scans in pixel size at acquisition as well as the fact that the signal intensity varied widely among patients, we compared the severity of lateral and medial bone bruises based on signal intensity only within the same imaging sequence in the same participant. Paired t tests were used to compare the maximum gray value of bone bruises between the lateral and medial sides in patients with BF + BT and LF + BT patterns. The chi-square test was used to compare the incidence of meniscal injuries between patients with and without bone bruises. A type I error rate of 0.05 was selected as the indication for statistical significance. All statistical analyses were performed using SPSS (Version 16; IBM).
Results
Demographics and Characteristics
Among the 207 patients, 165 were male and 42 were female. Overall, 169 (81.6%) of the 207 patients had bone bruises identified on MRI (Table 1). The most common sport associated with an ACL injury was basketball (n = 101; 48.8%). Other common sports related to the ACL injury were soccer (n = 60; 29.0%), skiing (n = 20; 9.7%), and badminton (n = 15; 7.2%). Statistical analysis showed that patients without bone bruises had a higher percentage of meniscal injuries than patients with bone bruises (P = .009).
Table 1.
Patient Demographics (N = 207)a
| With Bone Bruise (n = 169) | Without Bone Bruise (n = 38) | |
|---|---|---|
| Age, mean ± SD, y | 28.7 ± 6.3 | 27.2 ± 6.6 |
| Noncontact/contact injury, n | 151/18 | 33/5 |
| Most common sport of injury | Basketball | Basketball |
| Time from injury to MRI, mean (range), d | 17.4 (2-28) | 16.3 (0-28) |
| Meniscal injury, n | ||
| No injury | 71 | 7 |
| Medial only | 25 | 21 |
| Lateral only | 53 | 5 |
| Both medial and lateral | 20 | 5 |
aMRI, magnetic resonance imaging.
Bone Bruise Patterns
Table 2 presents the bone bruise distribution patterns of our patients. The most common bone bruise pattern observed among the patients was LF + LT, followed by BF + BT and LF + BT (Table 2).
Table 2.
Bone Bruise Patternsa
| n (%) | |
|---|---|
| LF + LT | 75 (44.4) |
| BF + BT | 49 (29.0) |
| BF + LT | 5 (3.0) |
| LF + BT | 26 (15.4) |
| LF + MT | 1 (0.6) |
| MF + BT | 4 (2.4) |
| MF + LT | 7 (4.1) |
| Bruising on only the tibia | 2 (1.2) |
aBF + BT, lateral and medial sides of both the femur and the tibia; BF + LT, lateral and medial sides of the femur and lateral side only of the tibia; LF + BT, lateral side only of the femur and lateral and medial sides of the tibia; LF + LT, lateral side only of both the femur and the tibia; LF + MT, lateral side only of the femur and medial side only of the tibia; MF + BT, medial side only of the femur and lateral and medial sides of the tibia; MF + LT, medial side only of the femur and lateral side only of the tibia.
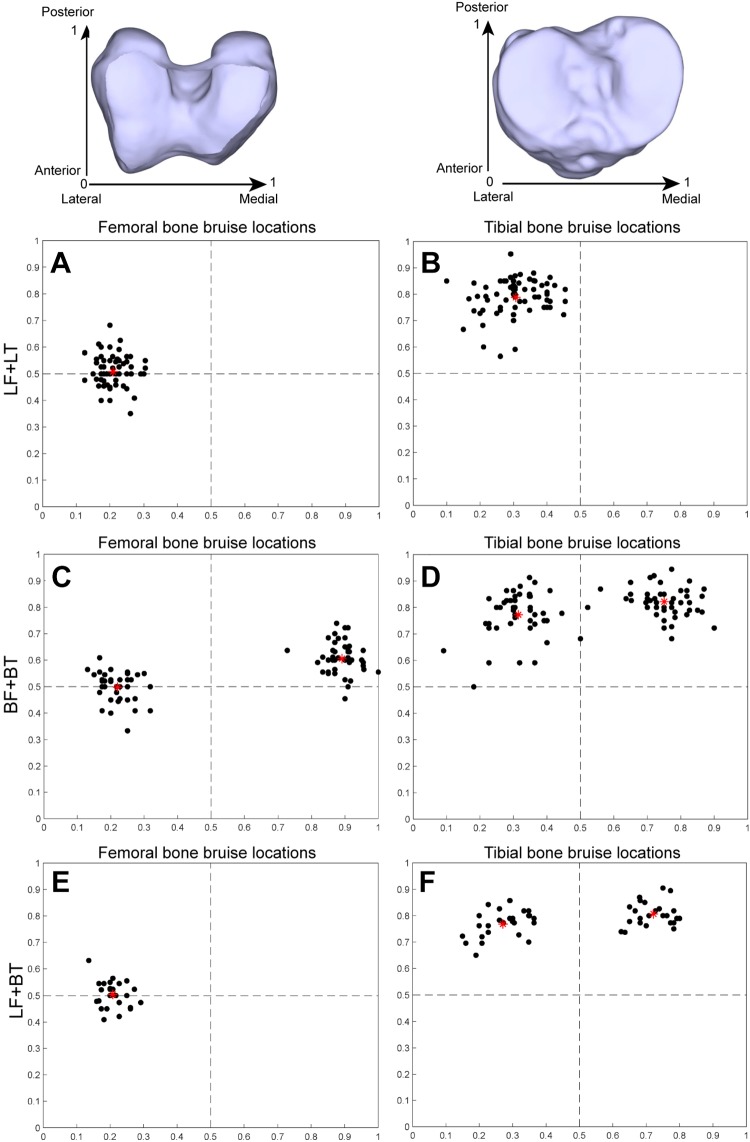
The overall bone bruise distribution patterns of the tibia and femur are shown in the lateral-medial and anterior-posterior directions (Figure 3). The maximum gray values on the lateral side of both the tibia (158.73 ± 36.97) and the femur (161.71 ± 33.03) were significantly greater than those on the medial side of both the tibia (137.91 ± 33.42) and femur (139.51 ± 37.47) in patients with the BF + BT pattern (P < .001 and P < .001, respectively). Paired t tests showed that the bone bruise locations on the lateral side (femur: 49.8% ± 5.3%; tibia: 77.2% ± 8.4%) of both the femur and the tibia were more anterior than those on the medial side (femur: 60.5% ± 5.9%; tibia: 82.2% ± 5.3%) in patients with the BF + BT pattern (P < .001 and P < .001, respectively). No significant difference in the maximum gray value between the lateral (146.58 ± 39.76) and medial sides (138.69 ± 46.64) of the tibia was observed in patients with the LF + BT pattern (P = .074). The bone bruises on the lateral tibial plateau (76.8% ± 5.0%) were more anterior than those on the medial tibial plateau (80.6% ± 4.4%) in patients with the LF + BT pattern (P = .001).
Figure 3.
Bone bruise distribution patterns of the femur and tibia. The dots represent different patients, and the red star in each subfigure represents the mean bone bruise location of those patients. (A) Femoral bone bruise locations of the LF + LT pattern. (B) Tibial bone bruise locations of the LF + LT pattern. (C) Femoral bone bruise locations of the BF + BT pattern. (D) Tibial bone bruise locations of the BF + BT pattern. (E) Femoral bone bruise locations of the LF + BT pattern. (F) Tibial bone bruise locations of the LF + BT pattern. BF, bilateral femur; BT, bilateral tibia; LF, lateral femur; LT, lateral tibia.
Discussion
The results of the present study provide new information regarding bone bruise locations within specific compartments of the tibia and femur. Our results show that the most common relative bone bruise pattern was located on the lateral side only of both the femur and the tibia, which could help us better understand the loading patterns during an ACL injury.
Bone Bruise Patterns
The results of this study support our hypothesis that the most common bone bruise distribution pattern was the lateral side only of both the femur and the tibia, which was consistent with the findings of previous investigators who reported that the proportion of bone bruises in the lateral compartment was higher than that in the medial compartment.22,34,37 The results indicate that impact forces occurred on the lateral side of both the tibia and the femur during an ACL injury in patients with the LF + LT pattern. The results of this study also show that the second most common bone bruise pattern was BF + BT, and the gray values on the lateral side of both the femur and the tibia were greater than those on the medial side. Similarly, previous investigators have demonstrated that the volume of lateral compartment bone bruises was larger than that of the corresponding medial compartment bone bruises.14 Wittstein et al36 also reported that tibial bone bruises on the lateral side were more severe than those on the medial side in the majority of women and men. The more severe bone bruises on the lateral side suggested that impact on the lateral side was more severe than that on the medial side. This pattern may have resulted from the contrecoup forces on the medial compartment at the resolution of valgus forces.14 These results combined together indicate that knee lateral compression accompanied bone bruise occurrence during ACL injuries and that valgus loading in the coronal plane could be an important contributor to some ACL injuries. Recent studies using cadaveric impact-simulated landing showed that ACL strain increased with greater dynamic knee abduction moment.3,30 Reducing high abduction loads during sports activities should be emphasized in ACL injury prevention programs.
The relative bone bruise patterns of the tibia and femur in this study are critical for understanding the causes of ACL injuries, with the assumption that bone bruises are the result of impact between the femur and tibia at the event of an ACL injury. If we assume that medial bone bruises are contrecoup injuries, the LF + LT pattern is the direct and accurate footprint left behind from the injury and could provide more valuable clues to the ACL injury mechanism compared with other bone bruise patterns. Future studies about the ACL injury mechanism based on the bone bruise location, such as simulation and position prediction, should focus more on MRI scans with only 1 bone bruise on the tibia and femur.
The results of this study support our second hypothesis that anterior translation of the tibia relative to the femur also occurs during an ACL injury based on the incidence and location of bone bruises. Our results demonstrate that for all of the most common bone bruise patterns in the current study, tibial bone bruises occurred in the posterior section, whereas femoral bone bruises occurred in the central section and were consistent with the findings of previous studies investigating bone bruise patterns using MRI.6,34 These results suggest that during an injury, the central or anterior section of the femoral condyle impacted the posterior section of the tibial plateau, which indicated that a substantial anterior tibial translation relative to the femur must have occurred during the ACL injury.15,22 Moreover, 2 recent studies demonstrated that a large anterior tibial translation was measured in patients at the predicted position of injury.16,24 Given that the ACL is a primary restraint to anterior shear loading, a large anterior tibial translation could produce large anterior tibial shear forces and cause an ACL injury.38 Therefore, these results combined together suggest that anterior tibial shear force in the sagittal plane could also be a key risk factor for ACL injuries.
The most common bone bruise distribution pattern indicated that knee abduction and anterior tibial translation could both be important contributors to the injury mechanism. The findings of this study also demonstrate that the bone bruise locations on the lateral side of both the femur and the tibia are significantly more anterior than those on the medial side for the second most common pattern. Although it is difficult to infer whether the tibia is internal or external relative to the femur at the time of injury based on the location of bone bruises, the asymmetric positions in the anterior-posterior direction between the lateral and medial sides indicated that tibial rotation in the axial plane occurred during the ACL injury. The results of this study demonstrate that the ACL injury pattern was complex and that the ACL injury mechanism involved a multiplanar loading pattern rather than a uniplanar loading pattern. Quatman et al28 also reported that tibial abduction rotation combined with anterior tibial translation or external or internal tibial rotation is the major ACL injury mechanism. These results together suggest that the loading patterns involve multiplanar loading during an ACL injury and that ACL ruptures may not be the result of uniplanar loading.
In addition to bone bruise patterns, our study also found that patients without bone bruises had a greater percentage of meniscal injuries than patients with bone bruises. Similarly, Pezeshki et al26 showed that the existence of bone bruises on knee MRI was negatively associated with medial meniscal injuries. In addition to decreasing contact stress at the articular surface,7 the menisci are important in shock absorption. The meniscal collagen ultrastructure is oriented circumferentially in the deeper layers with radial linking fibers, which is ideal for transferring a vertical compressive load into circumferential “hoop” stress.9 A greater percentage of meniscal injuries in patients without bone bruises may imply that impact forces are absorbed by the menisci rather than the bone.
This study has some limitations. First, although the current study had a large screening sample (4209 patients with ACL ruptures confirmed by an arthroscopic examination), the number of female patients was still too small to compare the sex-specific difference in bone bruise patterns because of the low proportion of women among the overall patient cohort. Further studies should include more female patients to investigate the sex-associated differences in the ACL injury mechanism based on the bone bruise distribution pattern. Second, bone bruise patterns at the time of injury seen on MRI may reflect the forces applied to the knee by specific sports activities, and the activities leading to an ACL injury are associated with certain injury patterns.11 Future studies are needed to fully understand the sports-specific injury patterns based on the bone bruise patterns. Third, as the bone bruises were more severe in patients with noncontact injuries than in patients with contact injuries,34 further studies are needed to compare bone bruise patterns between noncontact and contact groups. Finally, the medial tibial condyle is concave and longer in the anterior-posterior direction, whereas the lateral tibial plateau is smaller and more convex. The lateral bone bruise location was based on the total anterior-posterior depth of the tibia, not the lateral side. Thus, the method used in the present study may bias lateral tibial bone bruises to appear more anterior than they really are.
Conclusion
The most common relative bone bruise pattern was observed on only the lateral side of both the tibia and the femur. Bone bruises on the lateral side were more severe than those on the medial side in patients with bone bruises on the lateral and medial sides of both the femur and the tibia. There was anterior translation of the tibia relative to the femur during an ACL injury based on the location of bone bruises in the anterior-posterior direction.
Footnotes
Final revision submitted December 3, 2019; accepted December 23, 2019.
One or more of the authors has declared the following potential conflict of interest or source of funding: This work was supported in part by the National Natural Science Foundation of China (81330040) and the Beijing Municipal Natural Science Fund (7171014). AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Peking University Third Hospital Medical Ethics Committee.
References
- 1. Ali AM, Pillai JK, Gulati V, Gibbons CER, Roberton BJ. Hyperextension injuries of the knee: do patterns of bone bruising predict soft tissue injury? Skeletal Radiol. 2018;47(2):173–179. [DOI] [PubMed] [Google Scholar]
- 2. Aravindh P, Wu T, Chan CX, Wong KL, Krishna L. Association of compartmental bone bruise distribution with concomitant intra-articular and extra-articular injuries in acute anterior cruciate ligament tears after noncontact sports trauma. Orthop J Sports Med. 2018;6(4):2325967118767625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bates NA, Schilaty ND, Nagelli CV, Krych AJ, Hewett TE. Multiplanar loading of the knee and its influence on anterior cruciate ligament and medial collateral ligament strain during simulated landings and noncontact tears. Am J Sports Med. 2019;47(8):1844–1853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Blankenbaker DG, De Smet AA, Vanderby R, McCabe RP, Koplin SA. MRI of acute bone bruises: timing of the appearance of findings in a swine model. Am J Roentgenol. 2008;190(1):W1–W7. [DOI] [PubMed] [Google Scholar]
- 5. Brophy RH, Wright RW, Matava MJ. Cost analysis of converting from single-bundle to double-bundle anterior cruciate ligament reconstruction. Am J Sports Med. 2009;37(4):683–687. [DOI] [PubMed] [Google Scholar]
- 6. Fayad LM, Parellada JA, Parker L, Schweitzer ME. MR imaging of anterior cruciate ligament tears: is there a gender gap? Skeletal Radiol. 2003;32(11):639–646. [DOI] [PubMed] [Google Scholar]
- 7. Fukubayashi T, Kurosawa H. The contact area and pressure distribution pattern of the knee: a study of normal and osteoarthrotic knee joints. Acta Orthop Scand. 1980;51(6):871–879. [DOI] [PubMed] [Google Scholar]
- 8. Fullerton GD. Magnetic resonance imaging signal concepts. Radiographics. 1987;7(3):579–596. [DOI] [PubMed] [Google Scholar]
- 9. Ghosh P, Ingman AM, Taylor TK. Variations in collagen, non-collagenous proteins, and hexosamine in menisci derived from osteoarthritic and rheumatoid arthritic knee joints. J Rheumatol. 1975;2(1):100–107. [PubMed] [Google Scholar]
- 10. Graf BK, Cook DA, De Smet AA, Keene JS. “Bone bruises” on magnetic resonance imaging evaluation of anterior cruciate ligament injuries. Am J Sports Med. 1993;21(2):220–223. [DOI] [PubMed] [Google Scholar]
- 11. Granan L-P, Inacio MCS, Maletis GB, Funahashi TT, Engebretsen L. Sport-specific injury pattern recorded during anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41(12):2814–2818. [DOI] [PubMed] [Google Scholar]
- 12. Hewett TE, Schilaty ND. Determination of the position of the knee at the time of an anterior cruciate ligament rupture for male versus female patients by an analysis of bone bruises: letter to the editor. Am J Sports Med. 2018;46(11):NP47–NP48. [DOI] [PubMed] [Google Scholar]
- 13. Huang JY, Song WZ, Huang M. Effectiveness of osteoporosis self-assessment tool for Asians in screening for osteoporosis in healthy males over 40 years old in China. J Clin Densitom. 2017;20(2):153–159. [DOI] [PubMed] [Google Scholar]
- 14. Kaplan PA, Gehl RH, Dussault RG, Anderson MW, Diduch DR. Bone contusions of the posterior lip of the medial tibial plateau (contrecoup injury) and associated internal derangements of the knee at MR imaging. Radiology. 1999;211(3):747–753. [DOI] [PubMed] [Google Scholar]
- 15. Kaplan PA, Walker CW, Kilcoyne RF, Brown DE, Tusek D, Dussault RG. Occult fracture patterns of the knee associated with anterior cruciate ligament tears: assessment with MR imaging. Radiology. 1992;183(3):835–838. [DOI] [PubMed] [Google Scholar]
- 16. Kim SY, Spritzer CE, Utturkar GM, Toth AP, Garrett WE, DeFrate LE. Knee kinematics during noncontact anterior cruciate ligament injury as determined from bone bruise location. Am J Sports Med. 2015;43(10):2515–2521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kostogiannis I, Ageberg E, Neuman P, Dahlberg L, Friden T, Roos H. Activity level and subjective knee function 15 years after anterior cruciate ligament injury: a prospective, longitudinal study of nonreconstructed patients. Am J Sports Med. 2007;35(7):1135–1143. [DOI] [PubMed] [Google Scholar]
- 18. Mahmood N, Shah A, Waqas A, Abubakar A, Kamran S, Zaidi SB. Image segmentation methods and edge detection: an application to knee joint articular cartilage edge detection. J Theor Appl Inf Technol. 2015;71(1):87–96. [Google Scholar]
- 19. Matsumoto H. Mechanism of the pivot shift. J Bone Joint Surg Br. 1990;72(5):816–821. [DOI] [PubMed] [Google Scholar]
- 20. Mazzocca AD, Nissen CW, Geary M, Adams DJ. Valgus medial collateral ligament rupture causes concomitant loading and damage of the anterior cruciate ligament. J Knee Surg. 2003;16(3):148–151. [PubMed] [Google Scholar]
- 21. Mink JH, Deutsch AL. Occult cartilage and bone injuries of the knee: detection, classification, and assessment with MR imaging. Radiology. 1989;170(3)(pt 1):823–829. [DOI] [PubMed] [Google Scholar]
- 22. Murphy B, Smith R, Uribe J, Janecki C, Hechtman K, Mangasarian R. Bone signal abnormalities in the posterolateral tibia and lateral femoral condyle in complete tears of the anterior cruciate ligament: a specific sign? Radiology. 1992;182(1):221–224. [DOI] [PubMed] [Google Scholar]
- 23. Novaretti JV, Shin JJ, Albers M, et al. Bone bruise patterns in skeletally immature patients with anterior cruciate ligament injury: shock-absorbing function of the physis. Am J Sports Med. 2018;46(9):2128–2132. [DOI] [PubMed] [Google Scholar]
- 24. Owusu-Akyaw KA, Kim SY, Spritzer CE, et al. Determination of the position of the knee at the time of an anterior cruciate ligament rupture for male versus female patients by an analysis of bone bruises: response. Am J Sports Med. 2018;46(11):NP48–NP51. [DOI] [PubMed] [Google Scholar]
- 25. Patel SA, Hageman J, Quatman CE, Wordeman SC, Hewett TE. Prevalence and location of bone bruises associated with anterior cruciate ligament injury and implications for mechanism of injury: a systematic review. Sports Med. 2014;44(2):281–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Pezeshki S, Vogl TJ, Pezeshki MZ, Daghighi MH, Pourisa M. Association of the type of trauma, occurrence of bone bruise, fracture and joint effusion with the injury to the menisci and ligaments in MRI of knee trauma. Muscles Ligaments Tendons J. 2016;6(1):161–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Prodromos CC, Han Y, Rogowski J, Joyce B, Shi K. A meta-analysis of the incidence of anterior cruciate ligament tears as a function of gender, sport, and a knee injury-reduction regimen. Arthroscopy. 2007;23(12):1320–1325.e6. [DOI] [PubMed] [Google Scholar]
- 28. Quatman CE, Kiapour A, Myer GD, et al. Cartilage pressure distributions provide a footprint to define female anterior cruciate ligament injury mechanisms. Am J Sports Med. 2011;39(8):1706–1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Sanders TG, Medynski MA, Feller JF, Lawhorn KW. Bone contusion patterns of the knee at MR imaging: footprint of the mechanism of injury. Radiographics. 2000;20(suppl 1):S135–S151. [DOI] [PubMed] [Google Scholar]
- 30. Schilaty ND, Bates NA, Krych AJ, Hewett TE. Frontal plane loading characteristics of medial collateral ligament strain concurrent with anterior cruciate ligament failure. Am J Sports Med. 2019;47(9):2143–2150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Song GY, Zhang H, Wang QQ, Zhang J, Li Y, Feng H. Bone contusions after acute noncontact anterior cruciate ligament injury are associated with knee joint laxity, concomitant meniscal lesions, and anterolateral ligament abnormality. Arthroscopy. 2016;32(11):2331–2341. [DOI] [PubMed] [Google Scholar]
- 32. Speer KP, Warren RF, Wickiewicz TL, Horowitz L, Henderson L. Observations on the injury mechanism of anterior cruciate ligament tears in skiers. Am J Sports Med. 1995;23(1):77–81. [DOI] [PubMed] [Google Scholar]
- 33. Spindler KP, Schils JP, Bergfeld JA, et al. Prospective study of osseous, articular, and meniscal lesions in recent anterior cruciate ligament tears by magnetic resonance imaging and arthroscopy. Am J Sports Med. 1993;21(4):551–557. [DOI] [PubMed] [Google Scholar]
- 34. Viskontas DG, Giuffre BM, Duggal N, Graham D, Parker D, Coolican M. Bone bruises associated with ACL rupture: correlation with injury mechanism. Am J Sports Med. 2008;36(5):927–933. [DOI] [PubMed] [Google Scholar]
- 35. von Porat A, Roos EM, Roos H. High prevalence of osteoarthritis 14 years after an anterior cruciate ligament tear in male soccer players: a study of radiographic and patient relevant outcomes. Ann Rheum Dis. 2004;63(3):269–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Wittstein J, Vinson E, Garrett W. Comparison between sexes of bone contusions and meniscal tear patterns in noncontact anterior cruciate ligament injuries. Am J Sports Med. 2014;42(6):1401–1407. [DOI] [PubMed] [Google Scholar]
- 37. Yoon KH, Yoo JH, Kim KI. Bone contusion and associated meniscal and medial collateral ligament injury in patients with anterior cruciate ligament rupture. J Bone Joint Surg Am. 2011;93(16):1510–1518. [DOI] [PubMed] [Google Scholar]
- 38. Zhang L, Hacke JD, Garrett WE, Liu H, Yu B. Bone bruises associated with anterior cruciate ligament injury as indicators of injury mechanism: a systematic review. Sports Med. 2019;49(3):453–462. [DOI] [PubMed] [Google Scholar]