Abstract
Study Design:
Systematic review and meta-analysis.
Objectives:
This study aims to evaluate the effects of anterior cervical decompression and fusion (ACDF) on axial neck pain in adult patients receiving surgery for myelopathy, radiculopathy, or a combination of both.
Methods:
Two independent reviewers completed a librarian-assisted search of 4 databases. Visual Analogue Scale (VAS) and Neck Disability Index (NDI) scores were extracted preoperatively and at 3, 6, 12, 24, 36, 48, and 48+ months postoperatively for ACDF groups and pooled using a random-effects model.
Results:
Of 17 850 eligible studies, 37 were included for analysis, totaling 2138 patients analyzed with VAS and 2477 with NDI score. Individual VAS mean differences were reduced at 6 weeks (−2.5 [95% confidence interval (CI): −3.5 to −1.6]), 3 months (−2.9 [−3.7 to −2.2]), 6 months (−3.2 [−3.9 to −2.6]), 12 months (−3.7 [−4.3 to −3.1]), 24 months (−4.0 [−4.4 to −3.5]), 48 months (−4.6 [−5.5 to −3.8]), and >48 months (−4.7 [−5.8 to −3.6]) follow-up (P < .0001 for all endpoints). Individual NDI mean differences were reduced at 6 weeks (−26.7 [−30.9 to −22.6]), 3 months (−29.8 [−32.7 to −26.8]), 6 months (−31.2 [−35.5 to −26.8)], 12 months (−29.3 [−33.2 to −25.4]), 24 months (−28.9 [−32.6 to −25.2]), 48 months (−33.1 [−37.4 to −28.7]), and >48 months (−37.6 [−45.9 to −29.3]) follow-up (P < .0001 for all endpoints).
Conclusions:
ACDF is associated with a significant reduction in axial neck pain compared with preoperative values in patients being treated specifically for myelopathy or radiculopathy. This influences the preoperative discussions surgeons may have with patients regarding their expectations for surgery. The effects seen are stable over time and represent a clinically significant reduction in axial neck pain.
Keywords: ACDF, anterior cervical decompression and fusion, axial neck pain, Visual Analogue Scale, Neck Disability Index
Introduction
Degenerative cervical disc disease may result in disc herniations, which compress nerve roots causing radiculopathy or compress the spinal cord causing myelopathy.1 Patients with degenerative cervical disc disease classically have a significant degree of axial neck pain.1 The source of axial neck pain, whether it be discogenic, osseous, muscular, or alignment related, is generally difficult to elucidate on history and physical examination. For this reason, surgeons rely on neurological signs and symptoms to guide treatment.
Anterior cervical discectomy and fusion (ACDF) is a procedure that may be performed for patients with degenerative spondylitic myelopathy or radiculopathy. While the specific indications for surgery vary depending on patient symptoms and anatomic considerations such as previous surgery or deformity, there are well-recognized guidelines for treatment.1 Myelopathy guidelines generally recommend decompression for moderate or severe patient symptoms, and the literature suggests surgical decompression for radiculopathy when it is unresponsive to a minimum of 6 weeks of conservative therapy or symptoms are progressive.1 Accurate patient understanding of the expected surgical outcomes may improve the perceived success of the surgery and reduce medicolegal litigation.12 This involves accurately addressing both patient and surgeon expectations of the procedure preoperatively. While myelopathy may improve with surgery, the results are variable so the general goals of the procedure are to halt progression.15,16 Radiculopathy, however, tends to improve more reliably so patients anticipate reliable reductions in arm pain.2,3
While axial neck pain symptoms are particularly troubling to many patients, the effects of ACDF on axial neck pain are more poorly understood. Whereas several studies report a reduction in axial neck pain following ACDF, there have been no meta-analyses to date examining the effects of ACDF on cervical spondylitic myelopathy and/or radiculopathy. Accordingly, preoperative discussions may lack clarity regarding the outcomes of surgery with regard to the prognosis of axial neck pain. Therefore, the purpose of this meta-analysis is to examine all randomized controlled trials and prospective cohort studies that recorded preoperative and postoperative axial neck pain scores in order to examine the effect of single-level ACDF on axial neck pain in patients with myelopathy and/or radiculopathy.
Methods
Eligibility Criteria
This systematic review included adult patients receiving ACDF. The inclusion criteria for this review were the following: (1) published online and in the English language; (2) randomized controlled trial or cohort study; (3) included preoperative and postoperative data on subjective midline axial neck pain scores (either Visual Analog Scale [VAS] or Neck Disability Index [NDI] scores); (4) single-level pathology. All studies involving corpectomy or multilevel anterior decompressions, as well as posterior decompressive procedures, were excluded. In multiple cases there were studies published with what, in the authors’ best judgement, appeared to be the same ACDF data as a previously published control arm for disc arthroplasty versus ACDF trials. In these cases, the most recent data was utilized and the earlier studies by these authors were not included.
Search Strategy
Two independent authors searched MEDLINE, EMBASE, PubMed, and Cochrane databases with the guidance of a professional librarian using the following terms: “anterior cervical decompression and fusion” OR “ACDF,” OR “cervical decompression” AND “axial neck pain” OR “midline neck pain” to broaden the number of studies retrieved. Initial search results were vetted for duplicates and a title screen was performed for relevance. Reference lists of eligible studies were screened for additional studies meeting eligibility criteria. Discrepancy was resolved with discussion and consultation with the senior supervising author.
Risk of Bias
The risk of bias of included studies was assessed by using the Methodological Index for Non-Randomized Studies (MINORS) scale. The MINORS scale scores vary from 0 to 24 for risk of bias. The use of this scale is appropriate because the randomization process of the trials did not apply to this review as only data from the ACDF trial arms were extracted.
Data Abstraction
Two independent reviewers collected data into Excel spreadsheets. Demographics, type and study risk of bias, mean preoperative and postoperative VAS and/or NDI scores were recorded at multiple points in time (preoperatively, and postoperatively at 6 weeks, 3, 6, 12, 24, 36, and 48 months). Research ethics board approval is not required as it examines data from published studies. Therefore, there are no concerns regarding patient privacy or participant ethics.
Statistical Analysis
Demographic data is pooled for age, gender, smoking status, and NDI and VAS scores. The pooled proportions and pooled mean with standard deviation are reported. Some studies utilized a 100-point VAS neck pain scale while others utilized the more traditional 10-point scale. These scores are documented in the tables as reported by authors; however, the 10-point scale was selected for formal analyses and the 100-point scores were therefore divided by 10 to standardize the pain score from 0 and 10. In order to evaluate the mean change in pain scores, the mean pain scores from the preoperative assessment and at each follow-up visit were pooled from 32 included studies. The pooled means were compared to preoperative pooled means at each follow-up visit by use of a random-effects model with inverse variance. Between-study heterogeneity was tested using χ2 test and quantified by I2 statistics. The overall pooled mean change in pain scores with 95% confidence intervals (CIs) over 24 months and heterogeneity are reported. Comprehensive Meta-Analysis version 3.3.070 (Biostat, Inc, Englewood, NJ) was used for meta-analysis.
Results
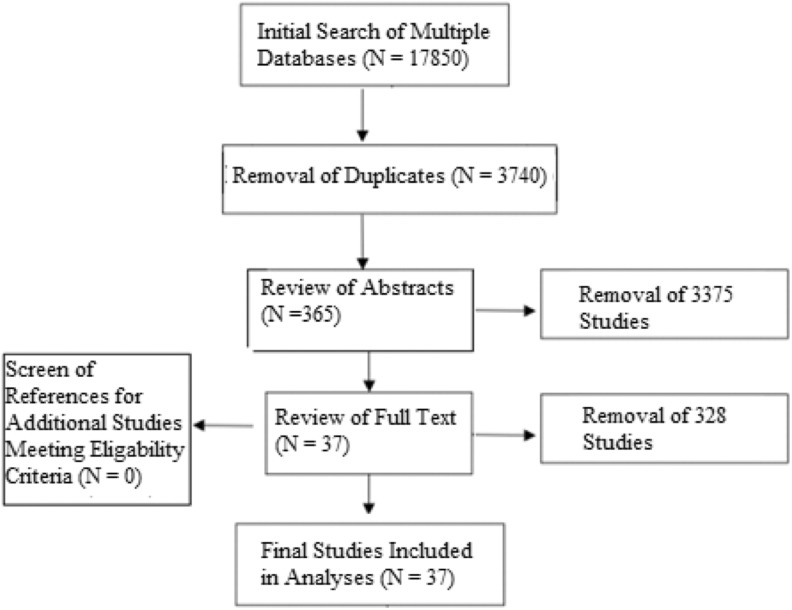
Initial librarian-assisted search revealed 17 850 studies, which after deletion of duplicates and initial title screen for relevance left 3740 studies for abstract review (Figure 1). Following abstract review, 3375 studies were removed for failure to meet eligibility criteria. The remaining 365 studies were examined via full text review. Discrepancies were resolved between authors and 37 studies were included in final analyses.4-40 Individual studies are presented in Table 1. Detailed information regarding studies and collected data is available in the appendix, available online.
Figure 1.
Flow diagram of search strategy with included studies.
Table 1.
A List of Studies Included in the Analyses.
| Study | Year | VAS | NDI | Study | Year | VAS | NDI |
|---|---|---|---|---|---|---|---|
| Zoëga et al Group 14 | 1998 | X | Maldonado et al22 | 2011 | X | X | |
| Zoëga et al Group 24 | 1998 | X | Zhang et al23 | 2012 | X | X | |
| Porchet et al 20 045 | 2004 | X | X | Coric et al24 | 2013 | X | X |
| Chen et al6 | 2005 | X | Ha et al Group 125 | 2013 | X | X | |
| Schils et al Group 17 | 2006 | X | Ha et al Group 225 | 2013 | X | X | |
| Schils et al Group 27 | 2006 | X | Chen et al26 | 2013 | X | X | |
| Bindal et al8 | 2007 | X | Kasliwal et al Group 127 | 2013 | X | X | |
| Mummaneni et al9 | 2007 | X | Kasliwal et al Group 227 | 2013 | X | X | |
| Nabhan et al10 | 2007 | X | Kasliwal et al Group 327 | 2013 | X | X | |
| Oktenoglu et al11 | 2007 | X | Phillips et al28 | 2013 | X | X | |
| Cosar et al12 | 2008 | X | Zigler et al29 | 2013 | X | X | |
| Fernández-Fairen et al Group 113 | 2008 | X | X | Janssen et al30 | 2015 | X | |
| Fernández-Fairen et al Group 213 | 2008 | X | X | Skeppholm et al31 | 2015 | X | X |
| Bhadra et al Group 114 | 2009 | X | Arnold et al Group 132 | 2016 | X | X | |
| Bhadra et al Group 214 | 2009 | X | Arnold et al Group 232 | 2016 | X | X | |
| Bhadra et al Group 314 | 2009 | X | Hisey et al33 | 2016 | X | X | |
| Heller et al15 | 2009 | X | Loumeau et al34 | 2016 | X | X | |
| Murrey et al16 | 2009 | X | Richter et al35 | 2016 | X | ||
| Nabhan et al Group 117 | 2009 | X | X | Burkus et al36 | 2017 | ||
| Nabhan et al Group 217 | 2009 | X | X | Pandey et al37 | 2017 | X | X |
| Burkus et al18 | 2010 | X | X | Razankovic et al38 | 2017 | X | |
| Delamarter et al19 | 2010 | X | X | Sasso et al 201 739 | 2017 | X | X |
| Garrido et al20 | 2010 | X | X | Arts et al Group 140 | 2017 | X | |
| Löfgren et al Group 121 | 2010 | X | X | Arts et al Group 240 | 2017 | X | |
| Löfgren et al Group 221 | 2010 | X | X |
Abbreviations: VAS, Visual Analogue Scale; NDI, Neck Disability Index.
Studies range in year from 1998 to 2017. A total of 2138 patients are analyzed with regard to VAS scores and 2477 patients with regard to NDI scores. Fifty-three percent of participants were male. Average time to final follow-up ranged from 6 months to 120 months for VAS (mean 33.1 ± 23.9 months) and NDI data (mean 34.5 ± 23.8 months).
Risk of Bias
Each of the 37 studies underwent risk of bias by MINORS scale. The mean MINORS score was 19.9 (±2.2) and ranged from 13 to 23 indicating that the risk of bias was overall acceptable for most of the included studies. Table 2 presents each study along with its MINORS score.
Table 2.
A List of Studies Included Along With Respective MINORS Scores for Quality Assessment.
| Study | MINORS Score | Study | MINORS Score |
|---|---|---|---|
| Zoëga et al4 | 15 | Zhang et al23 | 20 |
| Porchet et al5 | 20 | Coric et al24 | 22 |
| Chen et al6 | 21 | Ha et al25 | 21 |
| Schils et al7 | 19 | Chen et al26 | 20 |
| Bindal et al8 | 14 | Kasliwal et al27 | 22 |
| Mummaneni et al9 | 21 | Phillips et al28 | 21 |
| Nabhan et al10 | 22 | Zigler et al29 | 22 |
| Oktenoglu et al11 | 13 | Janssen et al30 | 21 |
| Cosar et al12 | 19 | Skeppholm et al31 | 20 |
| Fernández-Fairen et al13 | 22 | Arnold et al32 | 22 |
| Bhadra et al14 | 18 | Hisey et al33 | 18 |
| Heller et al15 | 20 | Loumeau et al34 | 20 |
| Murrey et al16 | 20 | Richter et al35 | 20 |
| Nabhan et al17 | 20 | Burkus et al36 | 19 |
| Burkus et al18 | 22 | Pandey et al37 | 18 |
| Delamarter et al19 | 23 | Razankovic et al38 | 20 |
| Garrido et al20 | 21 | Sasso et al39 | 19 |
| Löfgren et al21 | 23 | Arts et al40 | 18 |
| Maldonado et al22 | 21 | Mean ± SD | 19.9 ± 2.2 |
Abbreviation: MINORS, Methodological Index for Non-Randomized Studies.
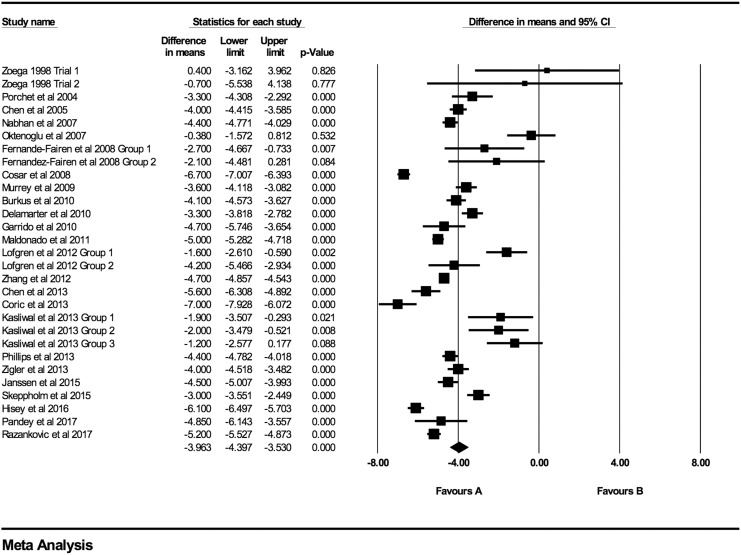
Axial Neck Pain
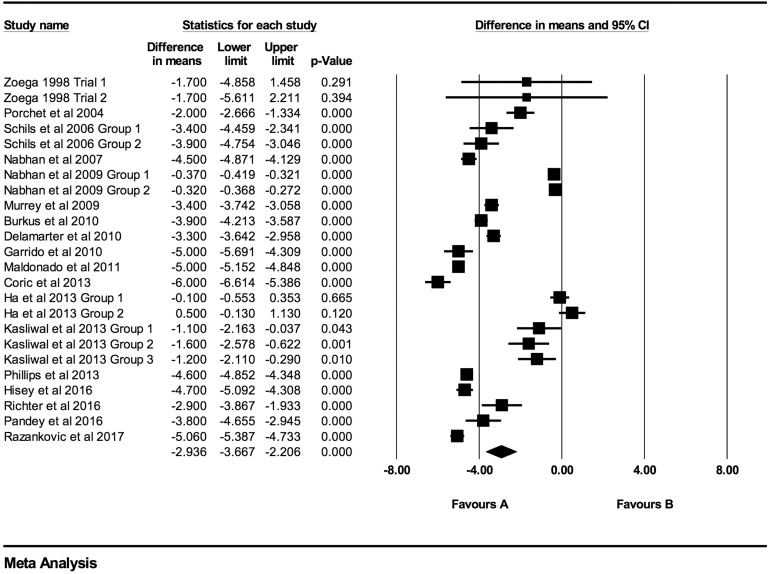
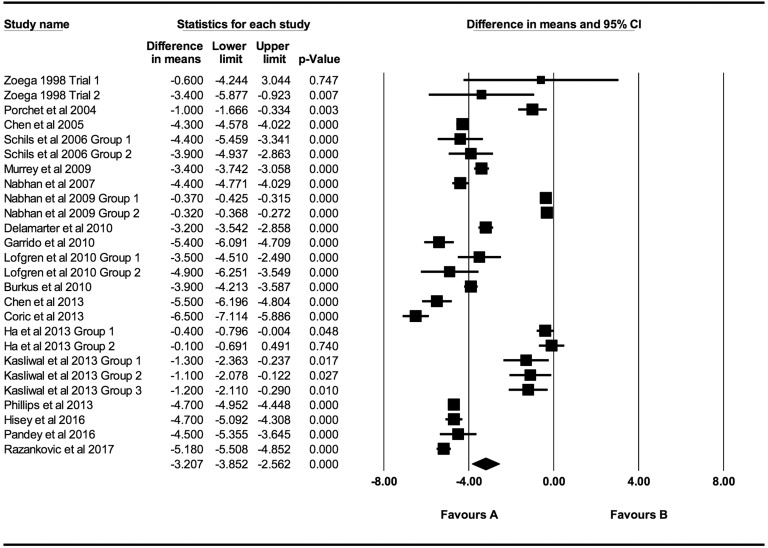
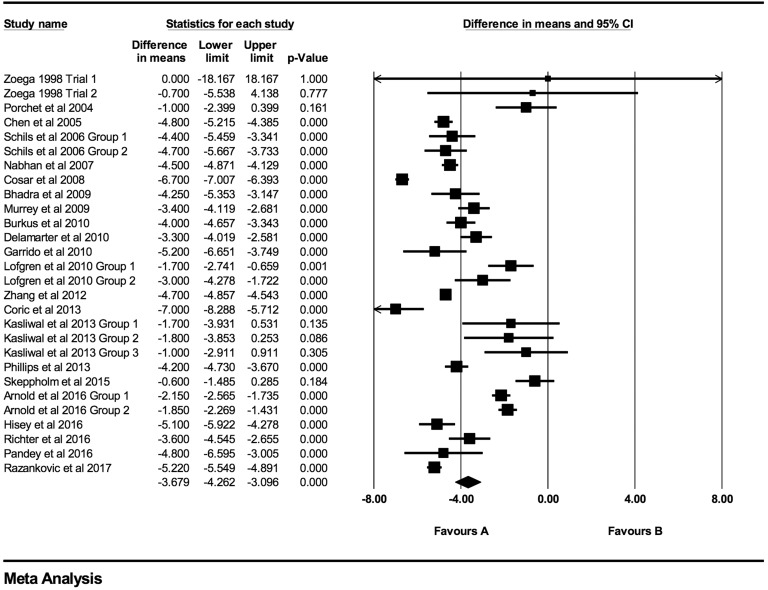
At every time point there was a statistically significant decrease in both VAS and NDI scores. Individual VAS mean differences are reduced compared postoperative scores at 6 weeks, 3 months, 6 months, 12 months, 24 months, 48 months, and >48 months follow-up were −2.52 (95% CI: −3.46 to −1.59; P < .0001; I2 = 99.9%; Figure A1), −2.94 (95% CI: −3.67 to −2.21; P < .0001; I2 = 99.7%; Figure 2), −3.21 (95% CI: −3.85 to −2.56; P < .0001; I2 = 99.5%; Figure 3), −3.68 (95% CI: −4.26 to −3.10; P < .0001; I2 = 98%; Figure 4), −3.96 (95% CI: −4.40 to −3.53; P < .0001; 94.7%; Figure 5), −4.65 (95% CI: −5.51 to −3.79; P < .0001; 90.9%; Figure 6), −4.71 (95% CI: −5.83 to −3.58; P < .0001; I2 = 93.0%; Figure A2), respectively.
Figure 2.
VAS baseline scores compared to 3-month follow-up (−2.94 [95% CI: −3.67 to −2.21]; heterogeneity: I2 = 99.7%, P < .001).
Figure 3.
VAS baseline scores compared to 6-month follow-up (−3.21 [95% CI: −3.85 to −2.56]; heterogeneity: I2 = 99.5%, P < .001).
Figure 4.
VAS baseline scores compared to 12-month follow-up (−3.68 [95% CI: −4.26 to −3.10]; heterogeneity: I2 = 98.1%, P < .001).
Figure 5.
VAS baseline scores compared to 24-month follow-up (−3.96 [95% CI: −4.40 to −3.53]; heterogeneity: I2 = 94.7%, P < .001).
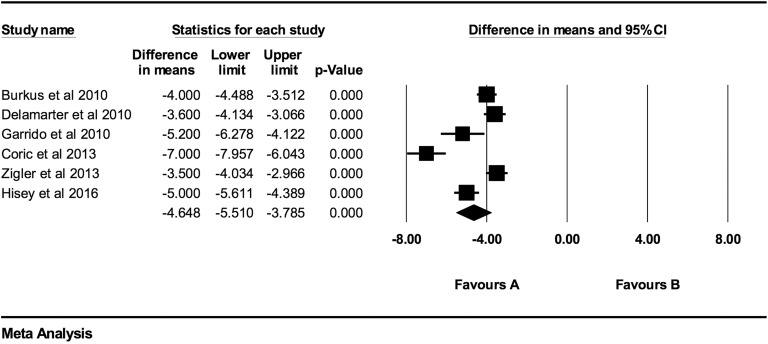
Figure 6.
VAS baseline scores compared to 48-month follow-up (−4.65 [95% CI: −5.51 to −3.79]; heterogeneity: I2 = 90.9%, P < .001).
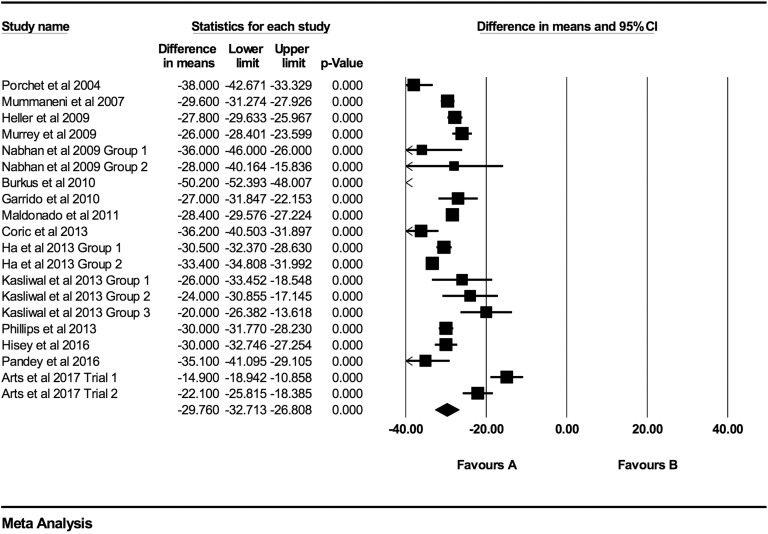
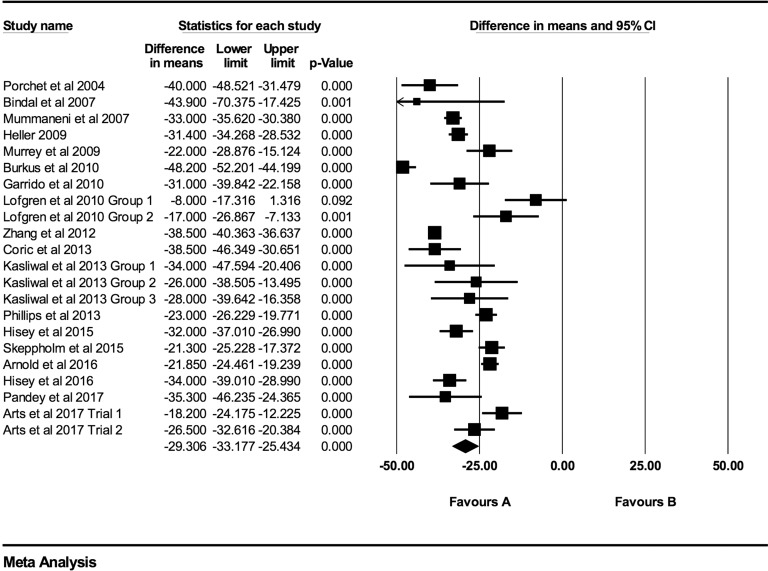
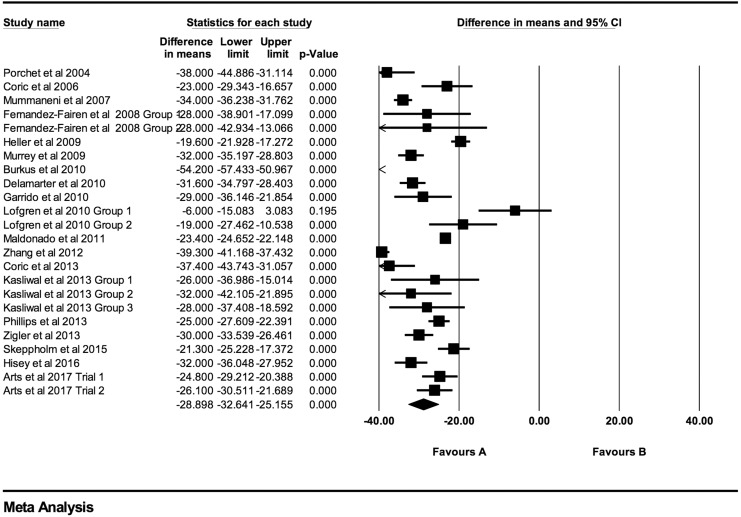
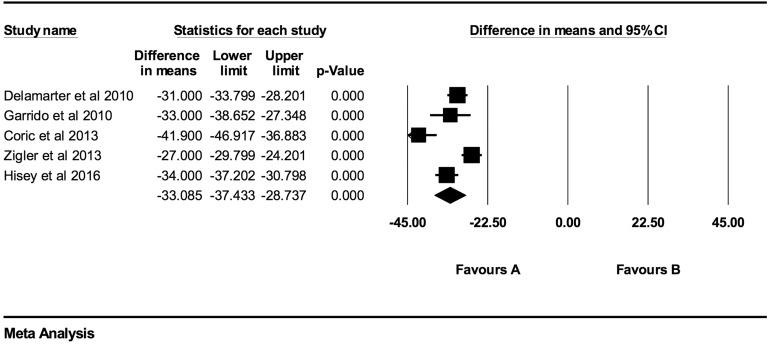
Individual NDI mean differences at 6 weeks, 3 months, 6 months, 12 months, 24 months, 48 months, and >48 months follow-up were −26.73 (95% CI: −30.88 to −22.59; P < .0001; I2 = 97.0%; Figure A3), −29.76 (95% CI: −32.71 to −26.81; P < .0001; I2 = 96.0%; Figure 7), −31.17 (95% CI: −35.49 to −26.84; P < .0001; I2 = 98.1%; Figure 8), −29.31 (95% CI: −33.18 to −25.43; P < .0001; I2 = 93.0%; Figure 9), −28.90 (95% CI: −32.64 to −25.16; P < .0001; I2 = 96.1%; Figure 10), −33.09 (95% CI: −37.43 to −28.74; P < .0001; I2 = 86.3%; Figure 11), and −37.61 (95% CI: −45.88 to −29.34; P < .0001; I2 = 91.0%; Figure A4), respectively.
Figure 7.
NDI baseline scores compared to 3-month follow-up (−29.76 [95% CI: −32.71 to −26.81]; heterogeneity: I2 = 96.0%, P < .001).
Figure 8.
NDI baseline scores compared to 6-month follow-up (−31.17 [95% CI: −35.49 to −26.84]; heterogeneity: I2 = 98.1%, P < .001).
Figure 9.
NDI baseline scores compared to 12-month follow-up (−29.31 [95% CI: −33.18 to −25.43]; heterogeneity: I2 = 93.0%, P < .001).
Figure 10.
NDI baseline scores compared to 24-month follow-up (−28.90 [95% CI: −32.64 to −25.16]; heterogeneity: I2 = 96.12%, P < .001).
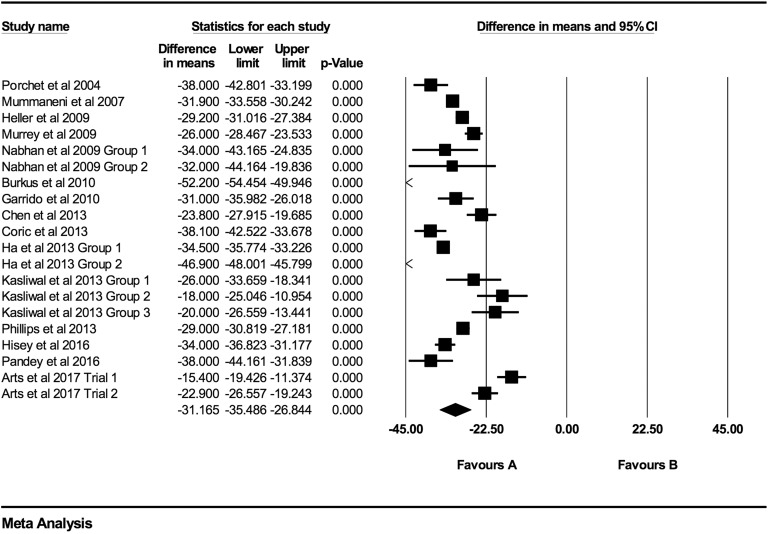
Figure 11.
NDI baseline scores compared to 48-month follow-up (−33.09 [95% CI: −37.43 to −28.74]; heterogeneity: I2 = 86.3%, P < .001).
Discussion
Axial neck pain is a multifactorial problem associated with muscular, ligamentous, discogenic, and degenerative bony spinal anatomy. This meta-analysis demonstrates that in patients with myelopathy or radiculopathy resulting from single-level disc disease, there are consistent reductions in axial neck pain following ACDF. It is likely that the disc itself is the main neck pain generator in these patients as pain is relieved following discectomy and fusion, and motion-preserving disc arthroplasty. For ACDF, the effect is stable over time with similar mean reductions in VAS and NDI at all time points postoperatively. These results will help guide preoperative discussions with patients, and may accurately address patient expectations.
Minimally important differences (MIDs) are the smallest effects that a patient would consider beneficial to justify a procedure41 and have been studied for multiple different scales within the field of spinal surgery. The MID for the VAS is found to be 2.5 points for extremity,42 and 3.5 points for VAS axial pain.42 The MID for NDI is determined to be 7.5 points.43 While the NDI data suggest a clinically significant reduction in axial neck pain at all time points, the VAS data presented here exceed the MID 12 months following ACDF. Our study finds a 28.8-point decrease in NDI at 24 months as well as a 4.1-point decrease in VAS for neck pain. The precise estimates and large number of included studies suggest a comprehensive evaluation of the current evidence of ACDF on the outcome of neck pain.
While this study reports clinically meaningful and statistically significant reductions in neck pain following ACDF, we do not recommend ACDF for neck pain in the absence of currently accepted indications for surgery. Selection bias is present as included patients were enrolled due to the presence of cervical myelopathy or radiculopathy. Accordingly, interpreting a causal relationship between ACDF and neck pain in the absence of neural compression warrants caution. One group of surgeons from Washington University report a systematic review on 3 case series utilizing ACDF for the purpose of mechanical/axial neck pain in patients without radiculopathy or any other standard indications for the procedure. They were criticized by editorial staff for presenting limited data to produce a meaningful analysis; however, they are commended for venturing beyond the accepted standards for this procedure. The 3 studies they reported44-46 included a total of 166 patients showing a 50% to 60% decrease in axial neck pain at 4-year follow-up and patient satisfaction rates ranging from 56% to 79%.3 Functional outcomes were improved between 32% and 52% from baseline.3
Future research may attempt to understand the direct relationship between ACDF and axial neck pain in patients with single-level disc disease. It is unethical to randomize patients to surgical treatment for neck pain, as ACDF is not accepted as a treatment for this condition. However, the current treatment guidelines for myelopathy suggest that mild myelopathy may be treated conservatively or surgically. Therefore, clinical equipoise exists to design a study examining patients with mild myelopathy, with and without axial neck pain, to determine the treatment effects of ACDF on axial neck pain directly. The degree to which axial neck pain is affected by other treatments for myelopathy (eg, laminectomy, laminoplasty, anterior corpectomy, and fusion) remains to be determined. It would be useful for future research to fully characterize the effects of these procedures on axial neck pain.
There are multiple strengths in this meta-analysis. A thorough search strategy is used with various keywords and a comprehensive search of multiple databases is undertaken. There are multiple reviewers involved in the process of article retrieval, risk of bias assessment, and data abstraction to ensure accuracy and minimize bias. The included studies are multicenter trials, including multiple implant products and surgeons, which increases the generalizability of our results. While we demonstrate high levels of heterogeneity in our outcomes at several time points, a large majority of studies were in favor for ACDF for a reduction in axial neck pain. Accordingly, we do not consider this inconsistency in treatment effect to weaken our study’s conclusion.
Conclusions
Our results indicate that ACDF is associated with a significant reduction in axial neck pain compared to preoperative values in patients being treated for myelopathy or radiculopathy. These effects meet clinically significant MIDs and may influence patients’ expectations for surgery. These results may help clarify expected surgical outcomes in preoperative discussions.
Supplemental Material
ACDF_Supplementary_Files for The Role of Anterior Cervical Discectomy and Fusion on Relieving Axial Neck Pain in Patients With Single-Level Disease: A Systematic Review and Meta-Analysis by Colby Oitment, Tracy Watson, Victor Lam, Mohammed Aref, Alex Koziarz, Edward Kachur, Jetan H. Badhiwala, Saleh A. Almenawer and Aleksa Cenic in Global Spine Journal
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Supplemental Material: The supplemental material is available in the online version of the article.
References
- 1. Albert TJ, Murrell SE. Surgical management of cervical radiculopathy. J Am Acad Orthop Surg. 1999;7:368–376. [DOI] [PubMed] [Google Scholar]
- 2. Robinson RA, Smith GW. Anterolateral cervical disc removal and interbody fusion for cervical disc syndrome. Bull Johns Hopkins Hosp. 1955;96:223–224. [Google Scholar]
- 3. Riew KD, Ecker E, Dettori JR. Anterior cervical discectomy and fusion for the management of axial neck pain in the absence of radiculopathy or myelopathy. Evid Based Spine Care J. 2010;1:45–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zoëga B, Kärrholm J, Lind B. One-level cervical spine fusion. A randomized study with or without plate fixation, using radiostereometry in 27 patients. Acta Orthop Scand. 1998;69:363–368. [DOI] [PubMed] [Google Scholar]
- 5. Porchet F, Metcalf NH. Clinical outcomes with the Prestige II cervical disc: preliminary results from a prospective randomized clinical trial. Neurosurg Focus. 2004;17:E6. [DOI] [PubMed] [Google Scholar]
- 6. Chen JF, Wu CT, Lee SC, Lee ST. Use of a polymethylmethacrylate cervical cage in the treatment of single-level cervical disc disease. J Neurosurg Spine. 2005;3:24–28. [DOI] [PubMed] [Google Scholar]
- 7. Schils F, Rilliet B, Payer M. Implantation of an empty carbon fiber cage or a tricortical iliac crest autograft after cervical discectomy for single-level disc herniation: a prospective comparative study. J Neurosurg Spine. 2006;4:292–299. [DOI] [PubMed] [Google Scholar]
- 8. Bindal RK, Ghosh S, Foldi B. Resorbable anterior cervical plates for single-level degenerative disc disease. Operative Neurosurg. 2007;61(5 suppl 2):305–310. [DOI] [PubMed] [Google Scholar]
- 9. Mummaneni PV, Burkus JK, Haid RW, Traynelis VC, Zdeblick TA. Clinical and radiographic analysis of cervical disc arthroplasty compared with allograft fusion: a randomized controlled clinical trial. J Neurosurg Spine. 2007;6:198–209. [DOI] [PubMed] [Google Scholar]
- 10. Nabhan A, Ahlhelm F, Pitzen T, et al. Disc replacement using Pro-Disc C versus fusion: a prospective randomized and controlled radiographic clinical study. Eur Spine J. 2007;16:423–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Oktenoglu T, Cosar M, Ozer AF, et al. Anterior cervical microdiscectomy with or without fusion. J Spinal Disord Tech. 2007;20:361–368. [DOI] [PubMed] [Google Scholar]
- 12. Cosar M, Ozer AF, Iplikkcioglu AC, et al. The results of beta-tricalcium phosphate coated hydroxyapatite (beta TCP/HA) grafts for interbody fusion after anterior cervical discectomy. J Spinal Disorder Tech. 2008;21:436–441. [DOI] [PubMed] [Google Scholar]
- 13. Fernández-Fairen M, Sala P, Dufoo M, Jr, Ballester J, Murcia A, Merzthal L. Anterior cervical fusion with tantalum implant. A prospective randomized controlled study. Spine (Phila Pa 1976). 2008;33:465–472. [DOI] [PubMed] [Google Scholar]
- 14. Bhadra AK, Raman AS, Casey ATH, Crawford RJ. Single-level cervical radiculopathy: clinical outcome and cost-effectiveness of four techniques of anterior cervical discectomy and fusion and disc arthroplasty. Eur Spine J. 2009;18:232–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Heller JG, Sasso RC, Papadopoulos SM, et al. Comparison of BRYAN cervical disc arthroplasty with anterior cervical decompression and fusion: clinical and radiographic results of a randomized, controlled, clinical trial. Spine (Phila Pa 1976). 2009;34:101–107. [DOI] [PubMed] [Google Scholar]
- 16. Murrey DB, Janssen ME, Odum SM, et al. Two-year results of a randomized controlled clinical trial comparing ProDisc-C and anterior cervical discectomy and fusion. SAS J. 2009;2:76–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Nabhan A, Ishak B, Steimer O, et al. Comparison of bioresorbable and titanium plates in cervical spinal fusion: early radiologic and clinical results. J Spinal Disord Tech. 2009;22:155–161. [DOI] [PubMed] [Google Scholar]
- 18. Burkus JK, Haid RW, Traynelis VC, Mummaneni PV. Long-term clinical and radiographic outcomes of cervical disc replacement with the Prestige disc: results from a prospective randomized controlled clinical trial. J Neurosurg Spine. 2010;13:308–318. [DOI] [PubMed] [Google Scholar]
- 19. Delamarter RB, Murrey D, Janssen ME, et al. Results at 24 months from the prospective, randomized, multicenter investigational device exemption trial of ProDisc-C versus anterior cervical discectomy and fusion with 4-year follow-up and continued access patients. SAS J. 2010;4:122–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Garrido BJ, Taha TA, Sasso RC. Clinical outcomes of Bryan cervical disc arthroplasty: a prospective randomized, controlled, single site trial with 48-month follow-up. J Spinal Disord Tech. 2010;23:367–371. [DOI] [PubMed] [Google Scholar]
- 21. Löfgren H, Engquist M, Hoffmann P, Sigstedt B, Vavruch L. Clinical and radiological evaluation of trabecular metal and the Smith-Robinson technique in anterior cervical fusion for degenerative disease: a prospective, randomized, controlled study with 2-year follow-up. Eur Spine J. 2010;19:464–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Maldonado CV, Paz RDR, Martin CB, Adjacent level degeneration after cervical disc arthroplasty versus fusion. Eur Spine J. 2011;20(suppl 3):2403–2407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Zhang X, Zhang X, Chen C, et al. Randomized, controlled, multicenter, clinical trial comparing BRYAN cervical disc arthroplasty with anterior cervical decompression and fusion in China. Spine (Phila Pa 1976). 2012;37:433–438. [DOI] [PubMed] [Google Scholar]
- 24. Coric D, Kim PK, Clemente JD, Boltes MO, Nussbaum M, James S. Prospective randomized study of cervical arthroplasty and anterior cervical discectomy and fusion with long-term follow-up: results in 74 patients from a single site. J Neurosurg Spine. 2013;18:36–42. [DOI] [PubMed] [Google Scholar]
- 25. Ha SM, Kim JH, Oh SH, Song JH, Kim HI, Shin DA. Vertebral distraction during anterior cervical discectomy and fusion causes postoperative neck pain. J Korean Neurosurg Soc. 2013;53:288–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Chen Y, Wang X, Lu X, Yang H, Chen D. Cervical disk arthroplasty versus ACDF for preoperative reducible kyphosis. Orthopedics. 2013;36:e958–e965. [DOI] [PubMed] [Google Scholar]
- 27. Kasliwal MK, Baskin DS, Traynelis VC. Failure of porous tantalum cervical interbody fusion devices: two-year results from a prospective, randomized, multicenter clinical study. J Spinal Disord Tech. 2013;26:239–245. [DOI] [PubMed] [Google Scholar]
- 28. Phillips FM, Lee JYB, Geisler FH, et al. A prospective, randomized, controlled clinical investigation comparing PCM cervical disc arthroplasty with anterior cervical discectomy and fusion: 2-year results from the US FDA IDE clinical trial. Spine (Phila Pa 1976). 2013;38:E907–E918. [DOI] [PubMed] [Google Scholar]
- 29. Zigler JE, Delamarter R, Murrey D, Spivak J, Janssen M. ProDisc-C and anterior cervical discectomy and fusion as surgical treatment for single-level cervical symptomatic degenerative disc disease: five-year results of a Food and Drug Administration study. Spine (Phila Pa 1976). 2013;38:203–209. [DOI] [PubMed] [Google Scholar]
- 30. Janssen ME, Zigler JE, Spivak JM Delamareter RB, Darden BV, 2nd, Kopjar B. ProDisc-C total disc replacement versus anterior cervical discectomy and fusion for single-level symptomatic cervical disc disease: seven-year follow-up of the prospective randomized US Food and Drug Administration Investigational Device Exemption Study. J Bone Joint Surg. 2015:97;1738–1747. [DOI] [PubMed] [Google Scholar]
- 31. Skeppholm M, Lindgren L, Henriques T, Vavruch L, Löfgren H, Olerud C. The discover artificial disc replacement versus fusion in cervical radiculopathy—a randomized controlled outcome trial with 2-year follow-up. Spine J. 2015;15:1284–1294. [DOI] [PubMed] [Google Scholar]
- 32. Arnold PM, Sasso RC, Janssen ME, et al. Efficacy of I-factor bone graft versus autograft in anterior cervical discectomy and fusion. Results of the prospective randomized, single-blinded Food and Drug Administration Investigational Device Exemption Study. Spine (Phila Pa 1976). 2016;41:1075–1083. [DOI] [PubMed] [Google Scholar]
- 33. Hisey MS, Zigler JE, Jackson R, et al. Prospective, randomized comparison of one-level Mobi-C cervical total disc replacement vs anterior cervical discectomy and fusion: results at 5-year follow-up. Int J Spine Surg. 2016;10:10 doi:10.14444/3010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Loumeau TP, Darden BV, Kesman TJ, et al. A RCT comparing 7-year clinical outcomes of one level symptomatic cervical disc disease (SCDD) following ProDisc-C total disc arthroplasty (TDA) versus anterior cervical discectomy and fusion (ACDF). Eur Spine J. 2016;25:2263–2270. [DOI] [PubMed] [Google Scholar]
- 35. Richter H, Seule M, Hildebrandt G, Fournier JY. Dynamic cervical implant versus anterior cervical diskectomy and fusion: a prospective study of clinical and radiographic outcome. J Neurol Surg A Cent Eur Neurosurg. 2016;77:300–307. [DOI] [PubMed] [Google Scholar]
- 36. Burkus JK, Dryer RF, Arnold PM, Foley KT. Clinical and radiographic outcomes in patients undergoing single-level anterior cervical arthrodesis: a prospective trial comparing allograft to a reduced dose of rhBMP-2. Clin Spine Surg. 2017;30:E1321–E1332. [DOI] [PubMed] [Google Scholar]
- 37. Pandey PK, Pawar I, Gupta J, Verma RR. Comparison of outcomes of single-level anterior cervical discectomy with fusion and single-level artificial cervical disc replacement for single-level cervical degenerative disc disease. Spine (Phila Pa 1976). 2017;42:E41–E49. [DOI] [PubMed] [Google Scholar]
- 38. Razankovic M, Marasanov M, Vukic M. Cervical disk replacement with discover versus fusion in single-level cervical disk disease. A prospective single-centre randomized trial with a minimum 2-year follow-up. Clin Spine Surg. 2017;30:E515–E522. [DOI] [PubMed] [Google Scholar]
- 39. Sasso WR, Smucker JD, Sasso MP, Sasso RC. Long term clinical outcomes of cervical disc arthroplasty. a prospective randomized controlled trial. Spine (Phila Pa 1976). 2017;42:209–216. [DOI] [PubMed] [Google Scholar]
- 40. Arts MP, Wolfs JFC, Corbin TP. Porous silicon nitride spacers versus PEEK cages for anterior cervical discectomy and fusion: clinical and radiological results of a single-blinded randomized controlled trial. Eur Spine J. 2017;26:2372–2379. [DOI] [PubMed] [Google Scholar]
- 41. Evaniew N, Khan M, Drew B, Kwok D, Bhandari M, Ghert M. Minimally invasive versus open surgery for cervical and lumbar discectomy: a systematic review and meta-analysis. CMAJ Open. 2014;2:E295–E305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Solberg T, Johnsen LG, Nygaard ØP, Grotle M. Can we define success criteria for lumbar disc surgery? Estimates for a substantial amount of improvement in core outcome measures. Acta Orthop. 2013;84:196–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Carreon LY, Glassman SD, Campbell MJ, Anderson PA. Neck disability index, short form-36 physical component summary, and pain scales for neck and arm pain: the minimum clinically important difference and substantial clinical benefit after cervical spine fusion. Spine J. 2010;10:469–474. [DOI] [PubMed] [Google Scholar]
- 44. Eck JC, Humphreys SC, Hodges SD, Levi P. A comparison of outcomes of anterior cervical discectomy and fusion in patients with and without radicular symptoms. J Surg Orthop Adv. 2006;15:24–26. [PubMed] [Google Scholar]
- 45. Garvey TA, Transfedlt EE, Malcolm JR, Kos P. Outcome of anterior cervical discectomy and fusion as perceived by patients treated for dominant axial-mechanical cervical spine pain. Spine (Phila Pa 1976). 2002;27:1887–1895. [DOI] [PubMed] [Google Scholar]
- 46. Palit M, Schoffermann J, Goldthwaite N, et al. Anterior discectomy and fusion for the management of neck pain. Spine (Phila Pa 1976). 1999;24:2224–2228. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
ACDF_Supplementary_Files for The Role of Anterior Cervical Discectomy and Fusion on Relieving Axial Neck Pain in Patients With Single-Level Disease: A Systematic Review and Meta-Analysis by Colby Oitment, Tracy Watson, Victor Lam, Mohammed Aref, Alex Koziarz, Edward Kachur, Jetan H. Badhiwala, Saleh A. Almenawer and Aleksa Cenic in Global Spine Journal