Abstract
Purpose:
We tested the hypothesis that individual- and neighborhood-level measures of socioeconomic status (SES) are more concordant in urban than rural areas, and we used the previously established association between obesity and self-rated health to illustrate the effect of residual confounding by individual-level SES when only neighborhood-level SES is considered.
Methods:
Using data from two population-based surveys, we calculated Spearman’s rank correlations between household income and neighborhood socioeconomic advantage across eight Pennsylvania counties. We applied multivariable Poisson regression models with robust variance estimates to each county to estimate the degree that individual SES confounds the association between obesity and self-rated health when the analysis accounts for neighborhood SES only and examined how this confounding varied by county urbanicity.
Results:
Concordance between household income and neighborhood advantage increased with county urbanicity (ρ = 0.16–0.26 vs. 0.31–0.45 vs. 0.47 in medium metro/micropolitan, suburban, and large metro counties, respectively). Conversely, confounding by individual SES on the obesity and self-rated health association decreased with urbanicity (15–22% vs. 6–13% vs. 3% in medium metro/micropolitan, suburban, and large metro counties, respectively).
Conclusion:
Individual- and neighborhood-level SES measures are poorly correlated outside of urban areas, suggesting that neighborhood-level measures inadequately account for individual SES in rural settings.
Keywords: socioeconomic status, urban-rural, neighborhood characteristics, research methods, confounding
Introduction
The socioeconomic status (SES) of individuals and their neighborhood environments are important social determinants of health that impact many health indicators and outcomes.1–5 Low SES has been associated with increased exposure to environmental hazards, pollutants and allergens, as well as negative life events and chronic stress.6–8 As a result, SES can confound exposure-outcome relationships, and SES-related measures are included as covariates in many epidemiological studies.
The use of SES measures is often limited by data availability, and multilevel analyses that incorporate both individual- and neighborhood-level indicators are not always possible. For example, individual-level SES is seldom documented in large health datasets, including disease registries, claims databases, and electronic health records. A common approach for overcoming these data limitations is to use neighborhood-level measures to capture SES when individual-level measures are unavailable.9–11 However, because individual- and neighborhood-level SES are distinct constructs with independent effects on health,3–5 use of neighborhood-level measures may not capture all relevant aspects of SES confounding exposure-outcome relationships. Figure 1 contains path diagrams illustrating possible relationships that individual and neighborhood SES may have with an exposure and an outcome. Adjusting for only neighborhood SES is appropriate when individual SES does not act as a confounder (Fig. 1b). However, when individual SES does act as a confounder (Fig. 1a and 1c), adjusting only for neighborhood SES leaves residual confounding by individual SES – especially absent a strong correlation between these variables.
Fig. 1.
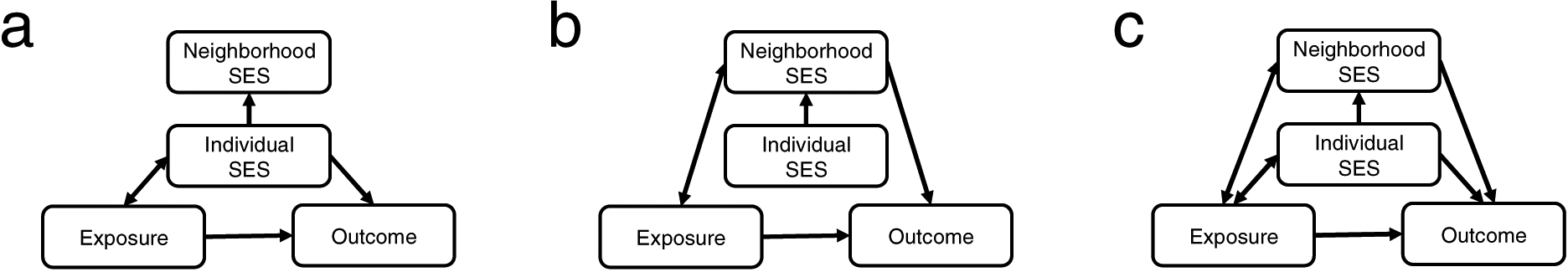
Path diagrams illustrating hypothetical situations where an exposure-outcome relationship is confounded by individual-level SES only (a), neighborhood-level SES only (b), or both individual- and neighborhood-level SES (c).
Although many studies use neighborhood-level measures of SES as the sole SES measure in analyses, the relationship between individual- and neighborhood-level SES is not always clear. Reported agreement between individual- and neighborhood-level SES measures has varied. Research in the U.S. found that agreement between individual- and neighborhood-level measures of SES was lower in a mixed urban-rural county in Minnesota than in an urban county in Missouri (Cohen’s κ = 0.15–0.22 vs. 0.26–0.36).12,13 Similarly, a study assessing the association between self-reported income and an area-based measure of income in a patient cohort from Alberta, Canada found little concordance (κ = 0.07) in this rural area,14 while agreement was higher in studies conducted in metropolitan Vancouver (Spearman’s ρ = 0.23–0.35)15 and Montreal (ρ = 0.31–0.39).16 Analysis of a pediatric asthma cohort in Rome, Italy found moderate agreement between parental education and neighborhood SES (ρ = 0.47–0.48).17
While these previous results suggest that neighborhood-level measures of SES are more correlated with individual-level measures in urban versus rural areas, the association between individual and neighborhood SES agreement and regional urbanicity has not been formally investigated. Here, we measured the correlation between individual- and neighborhood-level SES measures across eight counties in Pennsylvania with varying degrees of urbanization and determined whether the correlation between these measures increased with county urbanicity. We then assessed the extent to which the use of neighborhood-level SES measures results in residual confounding by individual-level SES, using the association between obesity and self-rated health as an illustrative example.
Materials and Methods
Study population and survey implementation
We obtained data from two population-based community health surveys administered by the Public Health Management Corporation (PHMC) in eight contiguous counties of Southeastern Pennsylvania: Southeastern Pennsylvania Household Health Survey (SEPA-HHS) and Berks-Lancaster-Schuylkill Household Health Survey (BLS-HHS). SEPA-HHS and BLS-HHS were approved by the PHMC Institutional Review Board, and PHMC obtained informed consent from all participating individuals. SEPA-HHS was administered in 2010 and 2012 to residents of urban Philadelphia County, which is coterminous with the City of Philadelphia, as well as residents of the neighboring suburban counties of Bucks, Chester, Delaware, and Montgomery (Supplemental Fig. 1). BLS-HHS was administered to residents of these eponymous outlying counties in 2011. SEPA-HHS and BLS-HHS were administered using similar survey instruments and procedures.18–20 Both surveys aimed to capture the health status and personal health behaviors of local residents through telephone interviews with people 18 years or older. Sampling in all cycles was stratified by geographic subareas (54 for SEPA-HHS and 13 for BLS-HHS), and balancing weights were provided to account for differences in response rates and ensure respondents were demographically representative of their areas of residence.
To understand the demographic and socioeconomic characteristics of the eight counties surveyed, we obtained county-aggregated summary measures from the American Community Survey 5-year estimates for 2009–2013.21 The level of urbanization for each county was determined using the 2006 National Center for Health Statistics (NHCS) Urban-Rural Classification Scheme for Counties, which divides U.S. counties into six classes: large central metro (1), large fringe metro (2), medium metro (3), small metro (4), micropolitan (5), and noncore (6).22 The eight surveyed counties fell into NCHS classes 1, 2, 3 and 5, which we’ve labeled large metro, suburban, medium metro and micropolitan, respectively.
Individual-level SES measures
Individual-level SES measures captured by the surveys included self-reported household income and educational attainment. Household income was an ordinal variable with 24–29 levels (i.e., income categories), which we transformed to a continuous variable by averaging upper and lower bounds for middle income categories and assigning the single boundary value for highest and lowest income categories. Educational attainment was an ordinal variable with the following levels: less than high school (equivalent to 0–11 years of education), high school graduate (12 years), some college (13–15 years), and college graduate or higher (≥16 years). We excluded respondents less than 25 years old to reduce the risk of exposure misclassification, as individuals in this age group were least likely to have completed their education.
Unadjusted household income may be an unreliable measure of SES because a family’s financial resource requirements vary substantially by household size and composition. To allow income to be more readily compared between households, we determined the household-specific poverty threshold for each respondent based on: (1) the number of related adults and children reported to be living in the household by the respondent and (2) federal poverty threshold tables released by the U.S. Census Bureau corresponding to the years of survey administration.23 We then calculated each household’s relative income by dividing unadjusted income by the household-specific poverty threshold.
Neighborhood-level SES measure
The Area Deprivation Index (ADI) is a composite measure of neighborhood socioeconomic disadvantage that captures multiple socioeconomic domains, including education, income, employment, and housing quality (Supplemental Table 1). First formulated by Singh in 2003,24 the ADI has been validated for detecting socioeconomic disparities in a number of health outcomes, including all-cause, cardiovascular, cancer, and childhood mortality,24–28 hospital readmission risk29,30 and cytomegalovirus seropositivity during pregnancy.31 We sourced 2013 ADI (calculated using variables from the American Community Survey 5-year estimates for 2009–2013) for all block groups in our study area from the Neighborhood Atlas online portal.32,33 Because the surveys reported residence at the level of census tracts, rather than block groups, we derived census tract-level ADI as the median ADI of nested block groups and assigned values to respondents according to their residential census tracts. To facilitate comparison with relative income and education, where higher values represent greater advantage, we transformed ADI (reported as a percentile ranking taking integer values 1–100) by subtracting it from 101 to derive a measure of neighborhood advantage.
Evaluating agreement between individual- and neighborhood-level SES measures
We calculated Spearman’s rank correlation coefficients (ρ) between individual-level SES measures (i.e., relative income and education) and neighborhood advantage, while stratifying respondents by their county of residence. To evaluate whether individual and neighborhood SES agreement differed according to regional urbanicity, we plotted county-wide agreement (ρ) against log-transformed county population density (a proxy for urbanicity) and computed Spearman’s rank correlation coefficients. We similarly assessed trends in correlation between individual and neighborhood SES versus NCHS class. Weighted correlations were obtained with the wCorr R package using survey weights provided by PHMC, and statistical significance was assessed via permutation tests.34
Residual confounding by individual-level SES after adjustment for neighborhood-level SES
To illustrate residual confounding by individual-level SES that may remain when only neighborhood-level SES is accounted for, we estimated the degree to which individual SES confounded the relationship between obesity and self-rated health. We chose self-rated health as our outcome variable because it is a validated measure of general health status35–37 and has been shown to be independently associated with both obesity and individual SES.38–42 Given the evidence linking low income and educational attainment to obesity,43–45 we reasoned that individual SES is likely to confound the association between obesity and self-rated health. SEPA-HHS and BLS-HHS asked respondents to rate their health as excellent, good, fair, or poor, and we dichotomized this variable as excellent/good or fair/poor. Body mass index (BMI) was calculated using self-reported height and weight measures and dichotomized as obese or not obese, where obesity was defined as BMI ≥ 30.
Confounding of the association between obesity and self-rated health by individual SES was assessed as follows. First, we determined whether individual-level SES was independently associated with both obesity and self-rated health in each county: after stratifying respondents by county of residence, we used multivariable Poisson regression models with robust variance estimates46 to estimate the relative risk of fair/poor health associated with education and relative income, while adjusting for age, sex, race/ethnicity and neighborhood advantage. Relative income and neighborhood advantage were categorized by quartiles, and age was categorized to seven ordinal levels (25–34, 35–44, 45–54, …, ≥85). We repeated this analysis with obesity as the dependent variable. Only counties for which individual-level SES was independently associated with obesity and self-rated health (according to two-sided alpha = 0.05 level) were included in the next step, as absence of these associations indicated that individual SES did not confound the obesity/self-rated health association. Second, we created multivariable Poisson regression models with robust variance estimates to estimate the relative risk of fair/poor health associated with obesity, stratified by county. Two relative risk estimates were derived for each county: model 1 included covariate adjustment for demographic variables (i.e., age, sex, race/ethnicity) and neighborhood-level SES (i.e. neighborhood advantage), while model 2 additionally included adjustment for two individual-level SES variables (i.e. relative income and respondent education). The magnitude of residual confounding by individual-level SES was quantified for each county as the percentage difference between the two relative risk estimates for the obesity/self-rated health association: 100*(RR1 − RR2)/RR2, where RR1 and RR2 were the relative risks estimated from models 1 and 2, respectively.
Results
Characteristics of counties based on ACS 5-year estimates for 2009–2013 are provided in Table 1. Philadelphia was a large metro characterized by high population density and roughly equal proportions of black and white residents. Compared to Philadelphia, the neighboring suburban counties of Bucks, Chester, Delaware, and Montgomery were less populated, predominantly white, and more socioeconomically affluent. The medium metro/micropolitan counties of Berks, Lancaster, and Schuylkill were predominantly white, more sparsely populated than the suburban counties, and had median income and poverty rates between those of the suburban counties and Philadelphia.
Table 1.
Characteristics of counties included in the Southeastern Pennsylvania Household Health Survey and Berks-Lancaster-Schuylkill Household Health Survey
| County | Survey region | Population densitya,b | NCHS classc | Percentage whiteb | Percentage blackb | Median incomed | Poverty rated |
|---|---|---|---|---|---|---|---|
| Philadelphia | SEPA | 4,393.6 | 1 | 41.0 | 43.4 | 37,192 | 26.5 |
| Bucks | SEPA | 399.5 | 2 | 89.2 | 3.6 | 76,555 | 5.4 |
| Chester | SEPA | 256.6 | 2 | 85.5 | 6.1 | 86,050 | 6.9 |
| Delaware | SEPA | 1,173.9 | 2 | 72.5 | 19.7 | 64,041 | 10.3 |
| Montgomery | SEPA | 639.3 | 2 | 81.1 | 8.7 | 79,183 | 6.1 |
| Berks | BLS | 185.5 | 3 | 83.2 | 4.9 | 55,170 | 13.9 |
| Lancaster | BLS | 212.5 | 3 | 88.6 | 3.7 | 56,483 | 10.5 |
| Schuylkill | BLS | 73.5 | 5 | 94.4 | 2.7 | 45,012 | 12.8 |
| Pennsylvania | -- | 109.6 | -- | 81.9 | 10.8 | 52,548 | 13.3 |
| United States | -- | 33.7 | -- | 72.4 | 12.6 | 53,046 | 15.4 |
Population density is expressed as population per square kilometer of land area;
County-, state- and national-level population density and racial composition are taken from the 2010 Decennial Census;
2013 National Center for Health Statistics (NCHS) Urban-Rural Classification Scheme for Counties categories are: 1 - large central metro, 2 - large fringe metro, 3 - medium metro, 4 - small metro, 5 - micropolitan, and 6 - noncore;
County-, state- and national-level median income, expressed in 2013 inflation-adjusted dollars, and poverty rate, expressed as the percent population below poverty level, are taken from the 2013 ACS 5-year estimates.
A total of 23,024 respondents were surveyed by SEPA-HHS and BLS-HHS in 2010–2012. Of these, 1,289 (5.6%) respondents were excluded for being less than 25 years old, 4,764 (21.9%) were excluded for missing income information, 1,690 (10.0%) were excluded for missing address or geocode information, and 147 (0.6%) were excluded for other missingness, leaving 15,134 (65.7%) complete cases for assessing individual and neighborhood SES agreement. Respondents who were excluded due to missing income were generally older and less educated but did not differ substantially by race/ethnicity compared to those with complete variable information (Supplemental Table 1), while respondents who were excluded due to incomplete address information did not differ substantially from those with complete variable information (Supplemental Table 2).
Characteristics of the 15,134 respondents included in analyses are provided in Table 2. Respondent characteristics generally reflected county characteristics although females were over-represented. Respondents from Philadelphia were more likely to be black and low-income than those of other counties, while respondents from suburban counties tended to have higher levels of educational attainment and higher household incomes. The medium metro/micropolitan counties had similarly high proportions of white respondents as suburban counties, although the average educational attainment of these respondents was lower and followed distributions similar to those of Philadelphia.
Table 2.
Characteristics of respondents with non-missing data by county residence, the Southeastern Pennsylvania Household Health Survey 2010, 2012 (SEPA-HHS) and Berks-Lancaster-Schuylkill Household Health Survey 2011 (N = 15,134)
| Survey cycle(s) | SEPA-HHS 2010 & 2012 | BLS-HHS 2011 | ||||||
|---|---|---|---|---|---|---|---|---|
| County | Philadelphia (n = 5,212) | Bucks (n = 1,656) | Chester (n = 1,792) | Delaware (n = 1,937) | Montgomery (n = 2,387) | Berks (n = 704) | Lancaster (n = 705) | Schuylkill (n = 741) |
| Age, median (IQR), y | 53 (42–63) | 52 (44–62) | 52 (43–61) | 53 (43–62) | 52 (43–62) | 54 (45–63) | 52 (42–63) | 54 (44–64) |
| Female, No. (%) | 3,483 (66.8) | 1,009 (60.9) | 1,069 (59.7) | 1,233 (63.7) | 1,471 (61.6) | 389 (55.3) | 347 (49.2) | 413 (55.7) |
| Race/ethnicity, No. (%) | ||||||||
| Non-Hispanic white | 2,326 (44.6) | 1,543 (93.2) | 1,593 (88.9) | 1,530 (79.0) | 2,087 (87.4) | 628 (89.2) | 631 (89.5) | 715 (96.5) |
| Non-Hispanic black | 2,253 (43.2) | 36 (2.2) | 99 (5.5) | 299 (15.4) | 166 (7.0) | 21 (3.0) | 15 (2.1) | 4 (0.5) |
| Hispanic | 405 (7.8) | 31 (1.9) | 39 (2.2) | 35 (1.8) | 40 (1.7) | 44 (6.2) | 41 (5.8) | 9 (1.2) |
| Other | 228 (4.4) | 46 (2.8) | 61 (3.4) | 73 (3.8) | 94 (3.9) | 11 (1.6) | 18 (2.6) | 13 (1.8) |
| Rel. incomea, No. (%) | ||||||||
| High (>5) | 1,027 (19.7) | 698 (42.1) | 885 (49.4) | 671 (34.6) | 1,001 (41.9) | 159 (22.6) | 150 (21.3) | 103 (13.9) |
| Middle (2–5) | 1,928 (37.0) | 670 (40.5) | 645 (36.0) | 814 (42.0) | 1,039 (43.5) | 354 (50.3) | 371 (52.6) | 363 (49.0) |
| Low (<2) | 2,257 (43.3) | 288 (17.4) | 262 (14.6) | 452 (23.2) | 347 (14.5) | 191 (27.1) | 184 (26.1) | 275 (37.1) |
| Educationb, No. (%) | ||||||||
| College + | 1,619 (31.1) | 754 (45.5) | 1,038 (57.9) | 856 (44.2) | 1,295 (54.3) | 202 (28.7) | 216 (30.6) | 136 (18.4) |
| Some college | 1,168 (22.4) | 390 (23.6) | 308 (17.2) | 429 (22.1) | 454 (19.0) | 146 (20.7) | 122 (17.3) | 168 (22.7) |
| High school | 1,862 (35.7) | 458 (27.7) | 386 (21.5) | 585 (30.2) | 562 (23.5) | 275 (39.1) | 279 (39.6) | 368 (49.7) |
| < High school | 563 (10.8) | 54 (3.3) | 60 (3.3) | 67 (3.5) | 76 (3.2) | 81 (11.5) | 88 (12.5) | 69 (9.3) |
Rel. Income (relative income) refers to the factor by which reported household income is above or below the federal poverty line determined for that household;
Education refers to the respondent’s educational attainment
Spearman’s rank correlations between individual-level SES measures and neighborhood advantage are provided in Table 3. Agreement (ρ) between household income and neighborhood advantage generally increased with county urbanicity (Fig. 2). Agreement was low in micropolitan Schuylkill county (ρ = 0.26) and medium metro Berks and Lancaster counties (ρ = 0.16–0.31), low to moderate in suburban Bucks, Chester, Delaware, and Montgomery counties (ρ = 0.33–0.45), and moderate in the large metro of Philadelphia (ρ = 0.47). The correlation between relative income-neighborhood advantage agreement and county urbanicity was high, whether urbanization was represented by county population density (Spearman’s ρ = 0.86) or NCHS class (ρ = −0.89). The correlations between respondent education-neighborhood advantage agreement and county urbanicity were similar to those obtained for relative income (Supplemental Fig. 2; ρ = 0.83 for county population density and ρ = −0.89 for NCHS class). However, the magnitude of the agreement between individual-level SES and neighborhood advantage was lower for all counties when education, rather than income, served as the individual-level SES indicator (ρ = 0.05–0.39 vs. 0.16–0.47; Table 3). With the exception of the correlation between education and neighborhood advantage in Lancaster (p = 0.16), all correlations were significant with p < 0.001.
Table 3.
Agreement (ρ) between individual SES indicators (indicated by column name) and neighborhood advantage for counties surveyed by SEPA-HHS and BLS-HHS. Bolded values are significant with p < 0.001.
| County | Urbanicity (NCHS classa) | Rel. incomeb | Education |
|---|---|---|---|
| Philadelphia | Large metro (1) | 0.472 | 0.385 |
| Bucks | Suburban (2) | 0.332 | 0.311 |
| Chester | Suburban (2) | 0.390 | 0.320 |
| Delaware | Suburban (2) | 0.447 | 0.354 |
| Montgomery | Suburban (2) | 0.356 | 0.283 |
| Berks | Medium metro (3) | 0.308 | 0.239 |
| Lancaster | Medium metro (3) | 0.156 | 0.045c |
| Schuylkill | Micropolitan (5) | 0.256 | 0.154 |
2013 National Center for Health Statistics (NCHS) Urban-Rural Classification Scheme for Counties categories are: 1 - large central metro, 2 - large fringe metro, 3 - medium metro, 4 - small metro, 5 - micropolitan, and 6 - noncore;
Rel. income (relative income) refers to the factor by which reported household income is above or below the federal poverty line determined for that household;
Not significant at alpha = 0.05 level
Fig. 2.
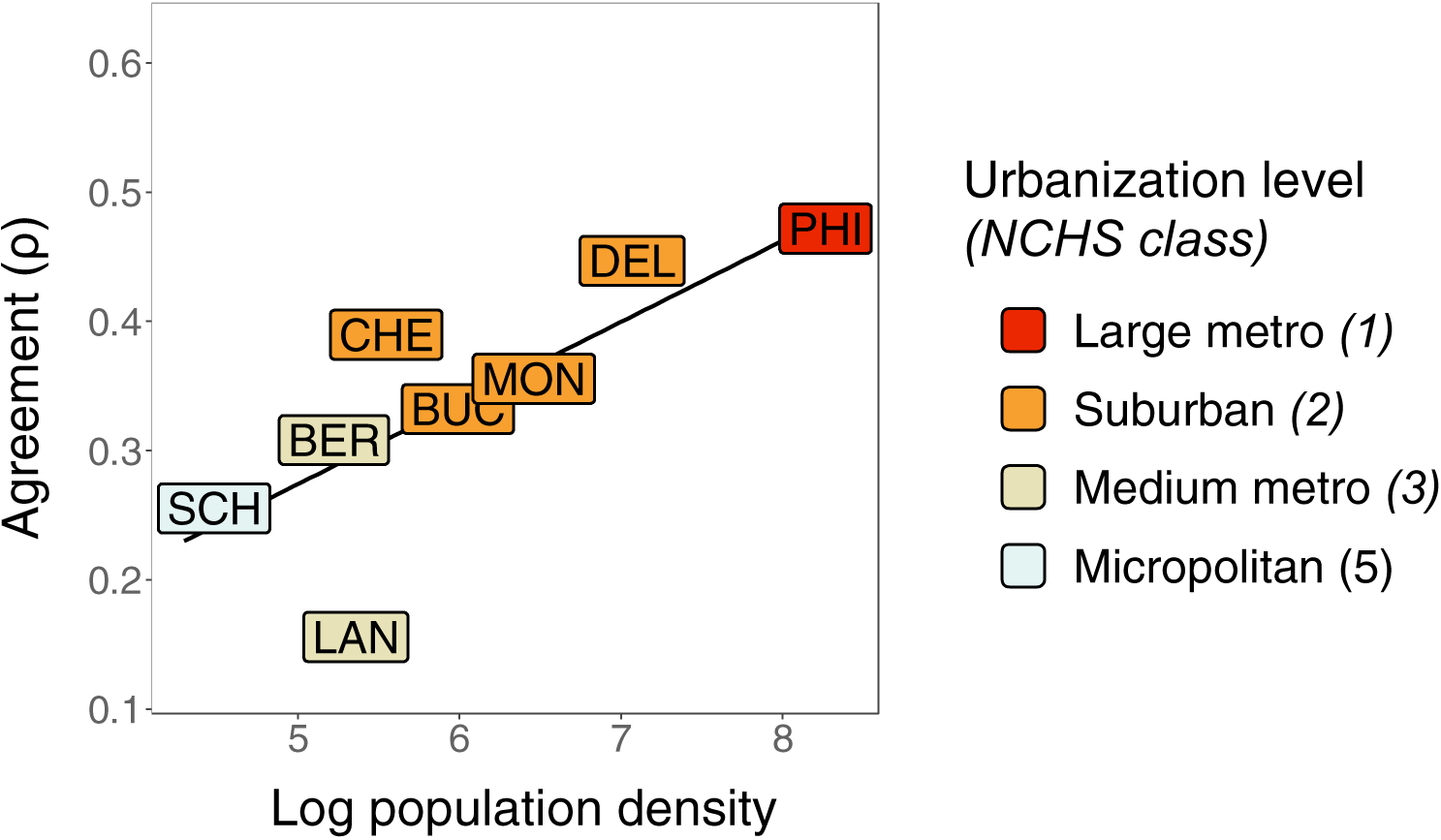
County-level agreement (Spearman’s ρ) between respondents’ relative household income and neighborhood advantage. PHI = Philadelphia, BUC = Bucks, CHE = Chester, DEL = Delaware, MON = Montgomery, BER = Berks, LAN = Lancaster, and SCH = Schuylkill.
Individual-level SES measures (relative income and education) were associated with fair/poor health and obesity in all counties (p < 0.05), with the exception of Schuylkill county, where individual-level SES measures were not associated with obesity (Supplemental Table 3 and Supplemental Table 4). Schuylkill county residents were thus excluded from the analysis of residual confounding. Fair/poor health was significantly associated with obesity in all models for the remaining counties (p<0.05), and point estimates from models that only adjusted for neighborhood-level SES were larger than those that additionally adjusted for individual-level SES (RR1 > RR2; Fig. 3a and Supplemental Table 5). Furthermore, the estimated magnitude of residual confounding by individual-level SES decreased with county urbanicity: it was highest in the medium metro counties (15–22%), intermediate in the suburban counties (6–13%), and lowest in Philadelphia (3%; Fig. 3b).
Fig. 3.
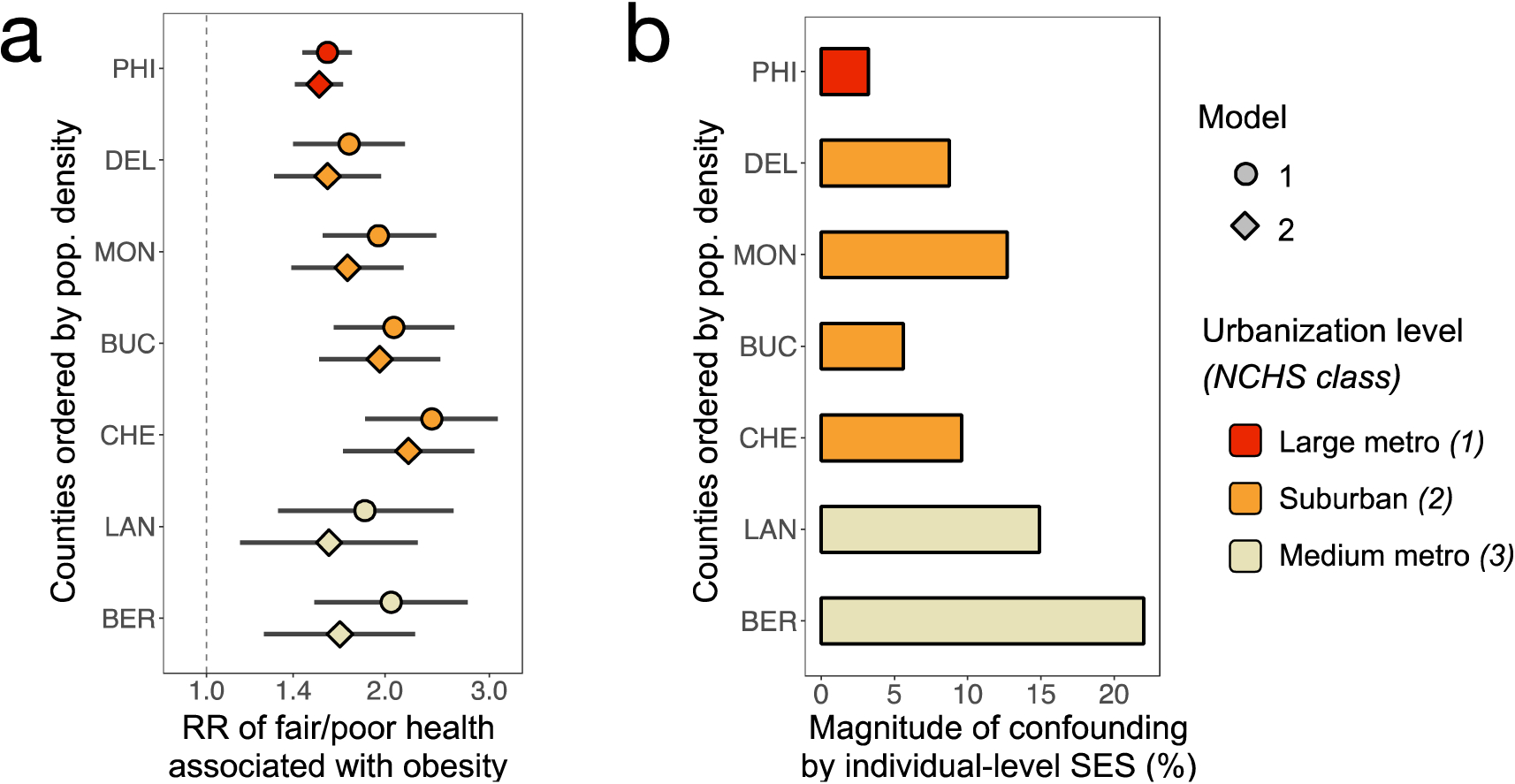
Estimated magnitude of residual confounding by individual-level SES when only neighborhood-level SES was accounted for. Fig. 3a shows the relative risk (RR) of self-rated fair/poor health associated with obesity according to multivariable Poisson regression estimated using model 1, which included demographic variables and neighborhood advantage and model 2, which included demographic variables, neighborhood advantage, relative household income and respondent education. Fig. 3b shows the magnitude of confounding by individual-level SES estimated as 100*(RR1 − RR2)/RR2, where RR1 and RR2 were estimated using models 1 and 2, respectively. PHI = Philadelphia, BUC = Bucks, CHE = Chester, DEL = Delaware, MON = Montgomery, BER = Berks, LAN = Lancaster, and SCH = Schuylkill.
Discussion
When individual-level measures of SES are unavailable for the secondary analysis of health datasets (such as data derived from administrative databases9,10 or electronic health records11), a common approach is to use neighborhood-level measures alone to represent SES. Our results suggest that when individual SES acts as a confounder, adjusting only for neighborhood-level SES can lead to significant residual confounding by individual-level SES, particularly outside of urban areas where correlations between individual- and neighborhood-level SES tend to be low.
The greater agreement between individual and neighborhood SES measures in urban areas may be expected, as Census tracts drawn by the U.S. Census Bureau, which aim to capture ~4,000 inhabitants that are “as homogeneous as possible” with respect to demographic and socioeconomic characteristics,47 tend to be smaller and more uniform in urban areas. Summary measures of neighborhood environments are relatively good proxies for individual-level measures in urban areas, and thus neighborhood-level SES measures may be able to account for the confounding effects of individual SES in urban centers like Philadelphia. In less urbanized areas, however, the use of neighborhood-level measures to represent individual SES is likely to result in considerable measurement error. Because controlling for mis-measured variables results in incomplete covariate adjustment,48 adjusting only for neighborhood-level SES measures may result in significant residual confounding by individual SES when individual- and neighborhood-level measures are weakly correlated.
These findings carry implications for multi-site studies or analyses of state- or nation-wide databases that encompass multiple areas spanning the urban-rural spectrum. If individual SES confounds the exposure-outcome relationship under study, adjustment for neighborhood-level SES measures only will result in varying degrees of residual confounding by individual SES, with rural areas generally exhibiting more confounding. If this residual confounding biases results in a systematic way (e.g., away from the null as in the present analysis), then stratified analyses may spuriously demonstrate effect modification by regional urbanicity. Using the present study as an example, one might conclude from analyses using only neighborhood-level SES measures that the link between obesity and fair/poor health weakens with increased urbanization when this trend can be attributed to the greater effects of residual confounding in rural areas.
Our results are subject to limitations. The analysis was restricted to eight counties in Southeastern Pennsylvania, and the extent that results can be generalized to other regions of the United States is unknown. The surveys captured only one rural (i.e., non-metro) county, and the trend between urbanicity grade and individual-neighborhood SES agreement was determined across mostly metro areas rather than areas ranging the full urban-rural spectrum. However, agreement is likely minimal in very remote areas, where census tract boundaries encompass large, disparate areas; thus, we expect the trend between urbanicity and individual-neighborhood SES agreement to be even more pronounced across a full urban-rural spectrum. Neighborhood SES was derived at the census tract level, and our results are likely to depend on the choice of neighborhood aggregation boundary (an issue known as the modifiable areal unit problem49). Nevertheless, the urban-rural gradient in individual vs. neighborhood SES agreement was still evident in analyses where Zip Code Tabulation Areas formed the geographic unit used to derive neighborhood SES (Supplemental Table 7, Supplemental Fig. 3), suggesting this trend was not solely driven by the use of census tracts as the neighborhood aggregation boundary. Income was subject to self-reporting bias and missing for 22% of respondents, consistent with income nonresponse rates noted in other health surveys.50,51 Respondents excluded for income nonresponse were generally older and had less education than those who reported their income, and this selective nonresponse may have biased our results.
In conclusion, neighborhood-level measures of SES were poorly correlated with individual-level measures outside of large metro or suburban areas, suggesting that analyses that include only neighborhood-level measures may result in significant residual confounding by individual-level SES in less urban settings. When SES is suspected to confound an exposure-outcome relationship, the results of regression models that include covariate adjustment for neighborhood-, but not individual-, level SES measures should be interpreted cautiously, particularly for studies of rural populations or analyses of state-or nation-wide databases that cover a spectrum of rural and urban environments.
Supplementary Material
Acknowledgements:
We would like to thank Gary Klein, Senior Data Analyst at PHMC, for helping us obtain and understand data from the SEPA-HHS and BLS-HHS. This work was supported by National Institutes of Health grants F31-HL142153 (SX), R21-CA227613 (RAH), R01-HL133433 (BEH), and R01-HL141992 (BEH). Additionally, this work was supported in part by the National Institute of Environmental Health Sciences under award number P30ES013508.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Braveman P, Egerter S, Williams DR. The social determinants of health: coming of age. Annu Rev Public Health 2011;32:381–98. [DOI] [PubMed] [Google Scholar]
- 2.Kozyrskyj AL, Kendall GE, Jacoby P, Sly PD, Zubrick SR. Association between socioeconomic status and the development of asthma: analyses of income trajectories. Am J Public Health 2010;100(3):540–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Diez Roux AV, Mair C. Neighborhoods and health. Annals of the New York Academy of Sciences 2010;1186(1):125–145. [DOI] [PubMed] [Google Scholar]
- 4.Ludwig J, Duncan GJ, Gennetian LA, Katz LF, Kessler RC, Kling JR, Sanbonmatsu L. Neighborhood effects on the long-term well-being of low-income adults. Science 2012;337(6101):1505–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ludwig J, Sanbonmatsu L, Gennetian L, Adam E, Duncan GJ, Katz LF, Kessler RC, Kling JR, Lindau ST, Whitaker RC, McDade TW. Neighborhoods, obesity, and diabetes--a randomized social experiment. N Engl J Med 2011;365(16):1509–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Havard S, Deguen S, Zmirou-Navier D, Schillinger C, Bard D. Traffic-related air pollution and socioeconomic status: a spatial autocorrelation study to assess environmental equity on a small-area scale. Epidemiology 2009;20(2):223–30. [DOI] [PubMed] [Google Scholar]
- 7.Evans GW, Kantrowitz E. Socioeconomic status and health: the potential role of environmental risk exposure. Annu Rev Public Health 2002;23:303–31. [DOI] [PubMed] [Google Scholar]
- 8.Chen E, Hanson MD, Paterson LQ, Griffin MJ, Walker HA, Miller GE. Socioeconomic status and inflammatory processes in childhood asthma: the role of psychological stress. J Allergy Clin Immunol 2006;117(5):1014–20. [DOI] [PubMed] [Google Scholar]
- 9.Bai L, Chen H, Hatzopoulou M, Jerrett M, Kwong JC, Burnett RT, van Donkelaar A, Copes R, Martin RV, Van Ryswyk K, Lu H, Kopp A, Weichenthal S. Exposure to Ambient Ultrafine Particles and Nitrogen Dioxide and Incident Hypertension and Diabetes. Epidemiology 2018;29(3):323–332. [DOI] [PubMed] [Google Scholar]
- 10.Fell DB, Platt RW, Basso O, Wilson K, Kaufman JS, Buckeridge DL, Kwong JC. The Relationship Between 2009 Pandemic H1N1 Influenza During Pregnancy and Preterm Birth: A Population-based Cohort Study. Epidemiology 2018;29(1):107–116. [DOI] [PubMed] [Google Scholar]
- 11.Reilly JP, Zhao Z, Shashaty MGS, Koyama T, Christie JD, Lanken PN, Wang C, Balmes JR, Matthay MA, Calfee CS, Ware LB. Low to Moderate Air Pollutant Exposure and Acute Respiratory Distress Syndrome after Severe Trauma. Am J Respir Crit Care Med 2019;199(1):62–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pardo-Crespo MR, Narla NP, Williams AR, Beebe TJ, Sloan J, Yawn BP, Wheeler PH, Juhn YJ. Comparison of individual-level versus area-level socioeconomic measures in assessing health outcomes of children in Olmsted County, Minnesota. J Epidemiol Community Health 2013;67(4):305–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Narla NP, Pardo-Crespo MR, Beebe TJ, Sloan J, Yawn B, Williams AR, Juhn YJ. Concordance between Individual vs. Area-Level Socioeconomic Measures in an Urban Setting. J Health Care Poor Underserved 2015;26(4):1157–72. [DOI] [PubMed] [Google Scholar]
- 14.Southern DA, McLaren L, Hawe P, Knudtson ML, Ghali WA, Investigators A. Individual-level and neighborhood-level income measures: agreement and association with outcomes in a cardiac disease cohort. Med Care 2005;43(11):1116–22. [DOI] [PubMed] [Google Scholar]
- 15.Marra CA, Lynd LD, Harvard SS, Grubisic M. Agreement between aggregate and individual-level measures of income and education: a comparison across three patient groups. BMC Health Serv Res 2011;11:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Demissie K, Hanley JA, Menzies D, Joseph L, Ernst P. Agreement in measuring socioeconomic status: area-based versus individual measures. Chronic Dis Can 2000;21(1):1–7. [PubMed] [Google Scholar]
- 17.Cesaroni G, Farchi S, Davoli M, Forastiere F, Perucci CA. Individual and area-based indicators of socioeconomic status and childhood asthma. Eur Respir J 2003;22(4):619–24. [DOI] [PubMed] [Google Scholar]
- 18.Public Health Management Corporation. 2012 Southeastern Pennsylvania Household Health Survey Documentation. Philadelphia: Public Health Management Corporation, 2012. [Google Scholar]
- 19.Public Health Management Corporation. 2010 Southeastern Pennsylvania Household Health Survey Documentation. Philadelphia: Public Health Management Corporation, 2010. [Google Scholar]
- 20.Public Health Management Corporation. Berks-Lancaster-Schuylkill Household Health Survey Documentation. Philadelphia: Public Health Management Corporation, 2011. [Google Scholar]
- 21.United States Census Bureau; American Community Survey. American Community Survey 5-Year Estimates for 2009–2013; using American FactFinder; <http://factfinder.census.gov>. 2013.
- 22.Ingram DD, Franco SJ. 2013. NCHS Urban-Rural Classification Scheme for Counties. Vital Health Stat 2 2014(166):1–73. [PubMed] [Google Scholar]
- 23.United States Census Bureau. Poverty thresholds by size of family and number of children. 2017. [Google Scholar]
- 24.Singh GK. Area deprivation and widening inequalities in US mortality, 1969–1998. Am J Public Health 2003;93(7):1137–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Singh GK, Azuine RE, Siahpush M, Kogan MD. All-cause and cause-specific mortality among US youth: socioeconomic and rural-urban disparities and international patterns. J Urban Health 2013;90(3):388–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Singh GK, Miller BA, Hankey BF. Changing area socioeconomic patterns in U.S. cancer mortality, 1950–1998: Part II--Lung and colorectal cancers. J Natl Cancer Inst 2002;94(12):916–25. [DOI] [PubMed] [Google Scholar]
- 27.Singh GK, Miller BA, Hankey BF, Feuer EJ, Pickle LW. Changing area socioeconomic patterns in U.S. cancer mortality, 1950–1998: Part I--All cancers among men. J Natl Cancer Inst 2002;94(12):904–15. [DOI] [PubMed] [Google Scholar]
- 28.Singh GK, Williams SD, Siahpush M, Mulhollen A. Socioeconomic, Rural-Urban, and Racial Inequalities in US Cancer Mortality: Part I-All Cancers and Lung Cancer and Part II-Colorectal, Prostate, Breast, and Cervical Cancers. J Cancer Epidemiol 2011;2011:107497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hu J, Kind AJH, Nerenz D. Area Deprivation Index Predicts Readmission Risk at an Urban Teaching Hospital. Am J Med Qual 2018;33(5):493–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kind AJ, Jencks S, Brock J, Yu M, Bartels C, Ehlenbach W, Greenberg C, Smith M. Neighborhood socioeconomic disadvantage and 30-day rehospitalization: a retrospective cohort study. Ann Intern Med 2014;161(11):765–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lantos PM, Hoffman K, Permar SR, Jackson P, Hughes BL, Kind A, Swamy G. Neighborhood Disadvantage is Associated with High Cytomegalovirus Seroprevalence in Pregnancy. J Racial Ethn Health Disparities 2018;5(4):782–786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kind AJH, Buckingham WR. Making Neighborhood-Disadvantage Metrics Accessible - The Neighborhood Atlas. N Engl J Med 2018;378(26):2456–2458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.University of Wisconsin School of Medicine and Public Health. 2013 Area Deprivation Index. 2018. [Google Scholar]
- 34.Emad AB P. wCorr: Weighted Correlations.—R package ver. 1.9.1 2017.
- 35.Lima-Costa MF, Cesar CC, Chor D, Proietti FA. Self-rated health compared with objectively measured health status as a tool for mortality risk screening in older adults: 10-year follow-up of the Bambui Cohort Study of Aging. Am J Epidemiol 2012;175(3):228–35. [DOI] [PubMed] [Google Scholar]
- 36.Miilunpalo S, Vuori I, Oja P, Pasanen M, Urponen H. Self-rated health status as a health measure: the predictive value of self-reported health status on the use of physician services and on mortality in the working-age population. J Clin Epidemiol 1997;50(5):517–28. [DOI] [PubMed] [Google Scholar]
- 37.Wu S, Wang R, Zhao Y, Ma X, Wu M, Yan X, He J. The relationship between self-rated health and objective health status: a population-based study. BMC Public Health 2013;13:320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Månsson N-O, Råstam L. Self-rated health as a predictor of disability pension and death—a prospective study of middle-aged men. Scandinavian journal of public health 2001;29(2):151–158. [PubMed] [Google Scholar]
- 39.Molarius A, Berglund K, Eriksson C, Lambe M, Nordstrom E, Eriksson HG, Feldman I. Socioeconomic conditions, lifestyle factors, and self-rated health among men and women in Sweden. Eur J Public Health 2007;17(2):125–33. [DOI] [PubMed] [Google Scholar]
- 40.Phillips LJ, Hammock RL, Blanton JM. Predictors of Self-rated Health Status Among Texas Residents. Preventing Chronic Disease 2005;2(4). [PMC free article] [PubMed] [Google Scholar]
- 41.Vingilis ER, Wade TJ, Seeley JS. Predictors of adolescent self-rated health. Analysis of the National Population Health Survey. Can J Public Health 2002;93(3):193–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Foraker RE, Rose KM, Chang PP, McNeill AM, Suchindran CM, Selvin E, Rosamond WD. Socioeconomic status and the trajectory of self-rated health. Age and ageing 2011;40(6):706–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McLaren L. Socioeconomic status and obesity. Epidemiol Rev 2007;29:29–48. [DOI] [PubMed] [Google Scholar]
- 44.Ogden CL, Lamb MM, Carroll MD, Flegal KM. Obesity and socioeconomic status in adults: United States, 2005–2008. NCHS Data Brief 2010(50):1–8. [PubMed] [Google Scholar]
- 45.Baltrus PT, Lynch JW, Everson-Rose S, Raghunathan TE, Kaplan GA. Race/ethnicity, life-course socioeconomic position, and body weight trajectories over 34 years: the Alameda County Study. Am J Public Health 2005;95(9):1595–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol 2004;159(7):702–6. [DOI] [PubMed] [Google Scholar]
- 47.U.S. Bureau of the Census. Census Tracts and Block Numbering Areas. In: Torrieri NK, ed. Geographic Areas Reference Manual. Washington, DC: US Department of Commerce, 1994. [Google Scholar]
- 48.Greenland S, Robins JM. Confounding and misclassification. Am J Epidemiol 1985;122(3):495–506. [DOI] [PubMed] [Google Scholar]
- 49.Openshaw S, Taylor P. A million or so correlation coefficients: three experiments on the modifiable areal unit problem In: Wrigley N, ed. Statistical Applications in the Spatial Sciences. London: Pion, 1979;127–144. [Google Scholar]
- 50.Shavers VL. Measurement of socioeconomic status in health disparities research. J Natl Med Assoc 2007;99(9):1013–23. [PMC free article] [PubMed] [Google Scholar]
- 51.Schenker N, Raghunathan TE, Chiu P-L, Makuc DM, Zhang G, Cohen AJ. Multiple Imputation of Missing Income Data in the National Health Interview Survey. Journal of the American Statistical Association 2006;101(475):924–933. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


