Abstract
Background
Dietary fatty acid (FA) content has been shown to influence the development of post-traumatic osteoarthritis (PTOA) in obesity. We used the fat-1 transgenic mouse to examine the hypothesis that endogenous reduction of ω-6 to ω-3 FA ratio, under the same dietary conditions, would mitigate metabolic inflammation and the pathogenesis of PTOA in obese male and female mice.
Methods
Male and female fat-1 and wild-type littermates were fed either a control diet or an ω-6 FA-rich high-fat diet and underwent destabilization of the medial meniscus (DMM) surgery to induce PTOA. OA severity, synovitis, and osteophyte formation were determined histologically, while biomarker and lipidomic analyses were performed to evaluate levels of adipokines, insulin, pro-/anti-inflammatory cytokines, and FAs in serum and joint synovial fluid. Multivariable models were performed to elucidate the associations of dietary, metabolic, and mechanical factors with PTOA.
Results
We found that elevated serum levels of ω-3 FAs in fat-1 mice as compared to wild-type controls fed the same diet resulted in reduced OA and synovitis in a sex- and diet-dependent manner, despite comparable body weights. The fat-1 mice showed trends toward decreased serum pro-inflammatory cytokines and increased anti-inflammatory cytokines. Multivariable analysis for variables predicting OA severity in mice resulted in correlations with serum FA levels, but not with body weight.
Conclusions
This study provides further evidence that circulating FA composition and systemic metabolic inflammation, rather than body weight, may be the major risk factor for obesity-associated OA. We also demonstrate the potential genetic use of ω-3 FA desaturase in mitigating PTOA in obese patients following injury.
Keywords: Metabolic syndrome, Diabetes, Adipocytokine, Cartilage, Arthritis
Introduction
Post-traumatic osteoarthritis (PTOA) is a debilitating joint disease that develops following trauma to the joint [1]. It is estimated that of the 27 million patients with osteoarthritis (OA), approximately 12% are due to trauma. Currently, there are no disease-modifying drugs available for this condition. While the main risk factors for OA include joint injury, age, sex, and genetics, the primary preventable risk factors for this disease are obesity and obesity-associated effects such as metabolic syndrome [2, 3].
The mechanisms relating diet-induced obesity and OA are not fully understood [4], but may involve several factors such as altered joint loading, systemic inflammation, and/or dietary fatty acid (FA) content. Obesity-associated inflammation is characterized by elevated serum levels of pro-inflammatory cytokines such as interleukin-1 (IL-1), IL-6, and tumor necrosis factor alpha (TNF-α) [5], as well as altered levels of adipokines such as leptin and adiponectin [6]. Furthermore, these same cytokines are also upregulated following joint injury and with PTOA [7–10]. In humans, switching to an ω-3 FA-rich diet reduces the serum levels of IL-1β and TNF-α, and increasing evidence suggests that dietary supplementation with ω-3 polyunsaturated fatty acids (PUFAs) can ameliorate metabolic syndrome and modulate circulating levels of leptin and adiponectin [11–13]. These data provide the rationale for this study aimed at genetically altering the ratio of ω-6 FAs to ω-3 FAs via an ω-3 FA desaturase in the context of a PTOA model system.
The fat-1 gene encodes an ω-3 FA desaturase that was originally identified in Caenorhabditis elegans and is not found in mammalian cells. This desaturase dehydrogenates ω-6 FAs to ω-3 FAs by adding a double bond at the third carbon from the methyl terminus [14]. Kang et al. produced a transgenic mouse model that constitutively expresses the fat-1 gene–encoded ω-3 FA desaturase throughout the body of the animal. Conventionally, to investigate the effect of dietary FAs on disease progression, animals need to be fed different diets with specific FA compositions. The fat-1 transgenic mouse provides a unique model to study the role of ω-3 FAs in OA pathogenesis without the confounding factors introduced by diet intervention because both wild-type (WT) and fat-1 animals can be fed the same diet, relying on ω-3 FA desaturase to increase endogenous ω-3 FA levels. Recently, Cai et al. showed that fat-1 mice and WT littermates exhibited comparable idiopathic OA scores when fed a lean diet rich in ω-6 FAs [15]. In a PTOA model, female fat-1 mice showed reduced OA scores and increased levels of ω-3 FAs in the serum and cartilage compared to the WT mice [16]. Although both studies provide important insights into how the ω-6/ω-3 FA ratio may affect the development of PTOA in lean animals, the influence of endogenous ω-3 FAs on PTOA progression in obesity and the effects of sex as a variable remain unknown.
In this study, we hypothesized that obese fat-1 mice fed a diet rich in ω-6 FAs will exhibit reduced PTOA-related joint degeneration compared to WT mice in a sex-dependent manner. Biomarker and lipidomic analyses were also performed to evaluate levels of adipokines, insulin, cytokines, and FAs in serum and joint synovial fluid.
Methods
Detailed methods are provided in online supplementary documents.
Animals
All animal procedures were approved by the Duke University Institutional Animal Care and Use Committee. fat-1 mice and littermate wild-type (WT) controls were bred for this study. Mice were placed on either a control diet (“lean” group) or an ω-6 FA-rich high-fat diet (HFD or “obese” group) starting at 5 weeks of age (Fig. 1a). Dual-energy X-ray absorptiometry (DXA) was used to assess bone mineral density (BMD) and percent body fat at 10, 14, and 28 weeks of age.
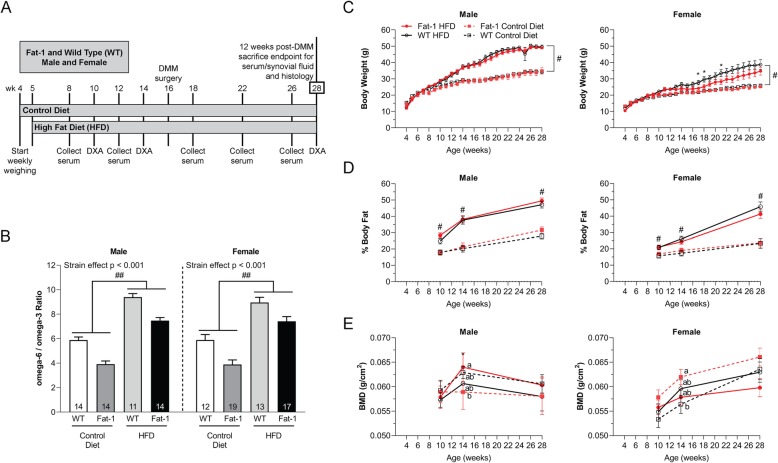
Fig. 1.
a The experimental design. Control and HFD treatment started at 5 weeks of age for both WT and fat-1 mice. DMM was performed at 16 weeks of age, and animals were sacrificed 12 weeks post-DMM surgery to evaluate OA and joint synovitis. b Serum ω-6/ω-3 FA ratio. Two-way ANOVA within the same sex. p < 0.001, WT vs. fat-1 strain effect. ##p < 0.001, HFD vs. control diet. The number (n) of the mice used in each group is indicated on plots. Data presented as mean ± SEM. c Body weight and d percent body fat over time. Two-way repeated measures ANOVA followed by Fisher’s LSD post hoc. #p < 0.05, HFD vs. control diet. *p < 0.05, WT female mice treated with HFD vs. fat-1 female mice treated with HFD. Data presented as mean ± SEM. e Whole-body BMD. Two-way repeated measures ANOVA followed by Fisher’s LSD post hoc. Groups not sharing the same letter are significantly different, p < 0.05, at 14 weeks of age. Data presented as mean ± SEM. For BMD and percent fat: male control diet WT n = 16, fat-1 n = 13; male HFD WT n = 12, fat-1 n = 15; female control diet WT n = 12, fat-1 n = 17; and female HFD WT n = 13, fat-1 n = 16. For body weight: male control diet WT n = 16, fat-1 n = 8; male HFD WT n = 7, fat-1 n = 15; female control diet WT n = 12, fat-1 n = 17; and female HFD WT n = 8, fat-1 n = 11
Destabilization of the medial meniscus (DMM) model
At 16 weeks of age, mice underwent DMM surgery in the left hind limb to induce PTOA [17]. The right hind limb remained non-operated as a contralateral control. At sacrifice 12 weeks post-DMM, both hind limbs from each mouse were harvested and processed into sections for the assessment of articular cartilage degeneration, synovitis, and osteophyte formation.
Serum and synovial fluid biomarker assays
Serial serum was collected at 8, 12, 18, 22, and 26 weeks of age. At sacrifice 12 weeks post-DMM, serum and synovial fluid were collected for biomarker and lipidomic analyses.
Statistical analysis
All results were analyzed using the SPSS Software Package (IBM, Armonk NY, USA), with significance reported at the 95% confidence level.
Results
Decreased serum ω-6/ω-3 FA ratio in fat-1 mice compared to WT mice
High-fat feeding of both male and female mice increased the serum ω-6/ω-3 FA ratio (Fig. 1b) at 28 weeks of age. However, this ratio was significantly decreased in fat-1 mice compared to WT mice. Indeed, fat-1 mice, independent of sex and diet treatments, demonstrated lower serum ω-6 FA levels (although the statistical significance was only observed in male mice fed the control diet), suggesting endogenous conversion of ω-6 FAs into ω-3 FAs (see supplementary Fig. S1A-B). Additionally, both WT and fat-1 mice also exhibited similar serum levels of saturated fatty acids (SFAs) and monounsaturated fatty acids (MUFAs) (see supplementary Fig. S1C-D).
Comparable body weight and percent body fat in fat-1 and WT mice under the same diet
Mice fed the HFD exhibited increased body weight in comparison with the mice treated with the control diet (Fig. 1c). In addition, male mice had relatively higher body weight than female mice regardless of the strain or diet treatment. However, independent of sex and diet, fat-1 mice had similar body weights to those of the WT mice under the same diet at 28 weeks of age; in contrast, obese fat-1 female mice had significantly decreased body weight compared to obese WT female mice at 17, 18, and 21 weeks of age.
At all measured time points, independent of sex, obese mice had significantly increased percent body fat compared to the mice treated with the control diet (Fig. 1d). Both male and female fat-1 mice had percent body fat comparable to WT mice of the same sex under the same diet treatment.
Sex- and diet-dependent effect of decreased serum ω-6/ω-3 FA ratio on whole-body BMD
Male fat-1 mice fed the control diet had lower whole-body bone mineral density (BMD) compared to male WT mice under the same diet at 14 and 28 weeks of age (Fig. 1e). Once again, this trend was opposite for females; the female fat-1 mice fed the control diet had significantly higher whole-body BMD compared to female WT mice under the same diet at 14 weeks of age.
Obese male fat-1 mice had a trend toward increased whole-body BMD compared to male obese WT mice at 14 and 28 weeks of age (Fig. 1e). This trend once again was opposite for females, as female obese fat-1 mice trended toward having lower whole-body BMD compared to obese WT mice at 14 and 28 weeks of age.
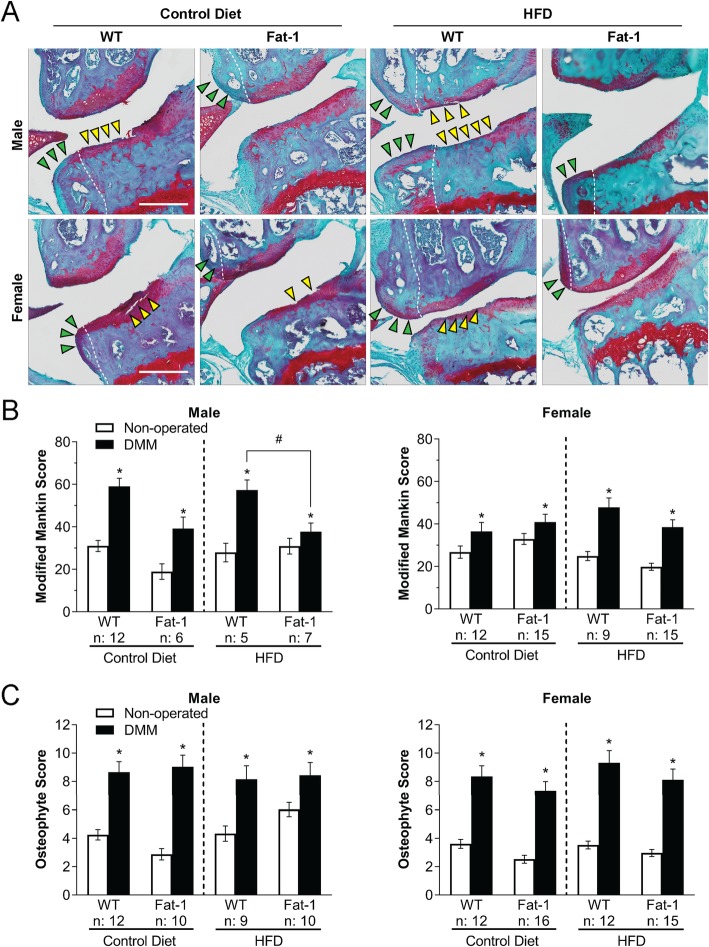
Reduced injury-induced OA in obese fat-1 mice in a sex-dependent and diet-dependent manner
DMM surgery resulted in a significant joint degeneration at 12 weeks post-surgery (Fig. 2a, b). OA scores were higher in WT male compared to those in WT female mice. Despite obesity, male and female fat-1 mice exhibited decreased OA in the DMM-operated joints as compared to obese WT littermates, although statistical significance was only observed in male mice (Fig. 2b). Lean male fat-1 mice fed the control diet, but not lean female fat-1 mice, also showed a similar trend toward lower OA scores in the DMM-operated joints versus their corresponding lean WT littermates.
Fig. 2.
a Safranin-O– and Fast Green–stained DMM-operated joints. Yellow arrowheads: severe cartilage loss and damage. Green arrowheads: osteophytes. White dashed lines: boundary between bone and osteophyte. Scale bar = 1 mm. b Modified Mankin score and c osteophyte scores for total joints. Two-way repeated measures ANOVA within the same sex followed by Fisher’s LSD post hoc. *p < 0.05, DMM-operated vs. non-operated joints. #p < 0.05, HFD fat-1 vs. WT DMM-operated joints. The number (n) of the mice used in each group is indicated on plots. Data presented as mean ± SEM
Similar osteophyte scores in fat-1 mice compared to their WT littermates
DMM surgery led to osteophyte formation in the operated joints (Fig. 2c). However, fat-1 mice, regardless of sex or diet, did not show altered osteophyte scores compared to their corresponding WT littermates.
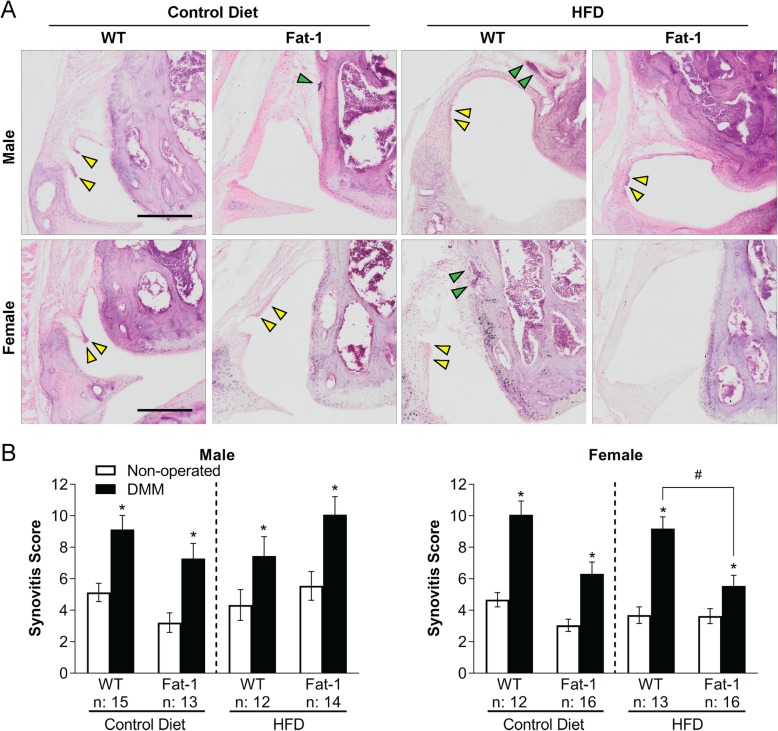
Reduced synovitis trends for fat-1 mice in a sex-dependent manner
In all groups, DMM surgery increased joint synovial inflammation in mice, accounting for diet treatment, strain, and sex (Fig. 3a, b). Obese female fat-1 mice on the HFD had statistically significant decreased synovitis scores in the DMM-operated joints compared to obese female WT mice, with control diet female mice showing a similar trend. Male fat-1 mice did not have attenuated synovial inflammation in the DMM-operated joints regardless of strain or diet treatments.
Fig. 3.
a Hematoxylin and eosin (H&E) staining of the medial femoral condyle in DMM-operated joints. Yellow arrowheads: formation of pannus and infiltration of cells in the synovial layer. Green arrowheads: inflammatory aggregates of immune cells in the synovium. Scale bar = 250 μm. b Total joint synovitis score. Two-way repeated measures ANOVA within the same sex followed by Fisher’s LSD post hoc. *p < 0.05, DMM-operated vs. non-operated joints. #p < 0.05, HFD fat-1 vs. WT DMM-operated joints. The number (n) of the mice used in each group is indicated on plots. Data presented as mean ± SEM
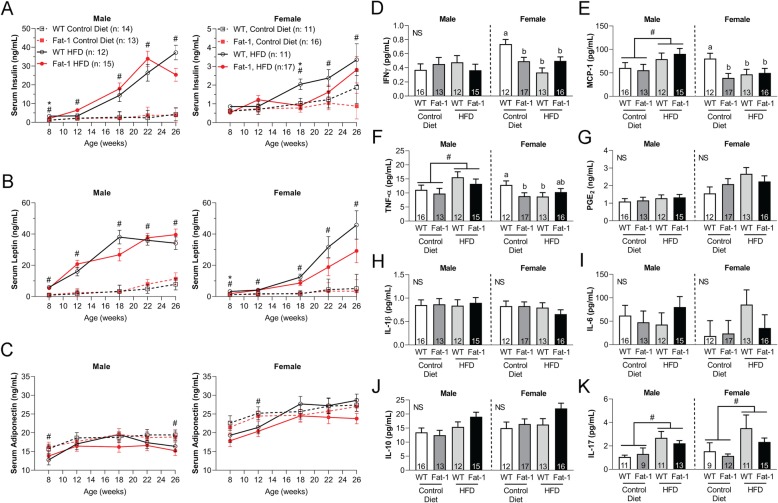
Obesity and decreased ω-6/ω-3 FA ratio affected serum insulin and leptin levels in a sex-dependent manner
Male obese mice exhibited significantly higher serum insulin and leptin levels compared to lean male mice at 26 weeks of age regardless of the strain (Fig. 4a, b). Similar trends of increased serum insulin and leptin levels were also observed for obese female mice, although female obese fat-1 mice showed relatively lower levels of insulin and leptin compared to female WT mice. Insulin levels for fat-1 and WT male obese mice at later time points reached levels an order of magnitude above those of their lean male and both female counterparts. Obesity resulted in a moderate but significant decrease in serum adiponectin levels in male, but not female, mice at 26 weeks of age (Fig. 4c).
Fig. 4.
Serum levels of a insulin, b leptin, and c adiponectin over time. Serum cytokine levels at 28 weeks of age for d IFN-γ, e MCP-1, f TNF-α, g PGE2, h IL-1β, i IL-6, j IL-10, and k IL-17. #p < 0.05, mice treated with HFD vs. mice treated with control diet within a specific time point. Two-way ANOVA within the same sex followed by Fisher’s LSD post hoc. NS, interaction term not significant (> 0.05). #p < 0.05, diet effect. Groups not sharing the same letter are significantly different, p < 0.05. The number (n) of the mice used in each group is indicated on plots. Data presented as mean ± SEM
Trends toward decreased pro-inflammatory cytokines and increased anti-inflammatory cytokines in fat-1 transgenic mice
Serum cytokines were collected at 28 weeks of age (i.e., 12 weeks post-DMM surgery) and evaluated using a multiplex kit. Serum concentrations of pro-inflammatory cytokines including interferon-γ (IFN-γ), monocyte chemoattractant protein-1 (MCP-1), TNF-α, and IL-12p70 were either significantly decreased or trended lower in the female fat-1 mice fed the control diet compared to female WT mice under the same diet (Fig. 4d–f; see supplementary Fig. S2). Obese female mice, regardless of strain, showed significantly lower serum levels of IFN-γ, MCP-1, and TNF-α compared to female WT fed the control diet. Male obese fat-1 mice trended toward lower serum concentrations of IFN-γ and TNF-α versus male obese WT mice. Obese female fat-1 mice also showed reduced serum prostaglandin E2 (PGE2), IL-1β, and IL-6 levels compared to obese female WT mice (Fig. 4g–i). Both male and female obese fat-1 mice trended toward increased serum IL-10, but decreased serum IL-17 compared to the corresponding obese WT mice (Fig. 4j, k). Statistically significant increases in MCP-1 and TNF-α levels were seen in male obese mice as compared to their lean counterparts on control diet, and a similar increase in IL-17 levels was seen in both male and female mice. Synovial fluid from DMM-operated limbs showed statistically significant increases in IL-8 levels, as compared to non-operated contralateral control levels, in every group regardless of diet treatment, strain, or sex (see supplementary Fig. S3).
Bivariate regression analysis between serum FAs, OA severity, and joint synovitis in fat-1 mice and WT littermates demonstrated sex-dependent correlations
To evaluate the association between various lipid species with disease markers (i.e., OA and synovitis scores), WT and fat-1 data for both HFD and control diets were pooled, but still separated by sex. Bivariate regression analysis was performed using lipid species as predictors. Correlation values for OA (modified Mankin scores) and synovitis scores show distinctly different results for male and for female mice (Table 1). Two ω-6 FAs (γ-linolenic acid and osbond acid) were positively associated with OA; docosanoic acid, a SFA, was positively associated with synovitis in male mice. Furthermore, eicosapentaenoic acid (EPA), an ω-3 FA, was negatively associated with OA severity. We also observed that nervonic acid, a MUFA, and all-cis-7,10,13,16,19-docosapentaenoic acid (DPA), an ω-3 FA, were both negatively associated with synovitis in male mice. Except for EPA (negatively associated with synovitis) for female mice, there were no statistically significant associations of FAs and OA or FAs and synovitis.
Table 1.
Correlations between the normalized concentration (Mol%) of serum lipid species with OA severity and synovitis
| Male | Female | ||||
|---|---|---|---|---|---|
| Predictor variables | OA | Synovitis | OA | Synovitis | |
| r | r | r | r | ||
| SFAs | Myristic acid | − 0.20 | − 0.23 | 0.13 | 0.17 |
| Pentadecylic acid | − 0.09 | − 0.18 | 0.12 | 0.11 | |
| Palmitic acid | 0.18 | − 0.01 | − 0.10 | 0.09 | |
| Stearic acid | − 0.25 | − 0.02 | − 0.06 | − 0.16 | |
| Docosanoic acid | 0.00 | 0.45* | 0.22 | 0.02 | |
| MUFAs | Myristoleic acid | − 0.21 | − 0.30 | 0.08 | 0.14 |
| Palmitoleic acid | 0.19 | − 0.15 | − 0.04 | 0.18 | |
| Oleic acid | 0.10 | − 0.14 | − 0.03 | 0.15 | |
| Eicosenoic acid | − 0.16 | − 0.07 | − 0.09 | 0.15 | |
| Nervonic acid | 0.02 | − 0.41* | 0.09 | − 0.02 | |
| ω-6 FAs | Linoleic acid | − 0.27 | 0.14 | 0.14 | − 0.16 |
| γ-Linolenic acid | 0.51** | 0.18 | 0.04 | − 0.27 | |
| Eicosadienoic acid | 0.11 | 0.23 | 0.12 | 0.01 | |
| Arachidonic acid | 0.12 | 0.07 | − 0.02 | 0.02 | |
| Osbond acid | 0.56** | − 0.09 | − 0.08 | 0.22 | |
| ω-3 FAs | α-Linolenic acid | − 0.13 | − 0.22 | 0.05 | − 0.06 |
| Stearidonic acid | − 0.14 | − 0.29 | − 0.12 | − 0.01 | |
| ETA | − 0.11 | 0.20 | 0.10 | 0.13 | |
| EPA | − 0.39* | − 0.12 | − 0.03 | − 0.32* | |
| DPA | − 0.09 | − 0.42* | − 0.15 | − 0.20 | |
| DHA | − 0.06 | 0.04 | − 0.02 | − 0.10 | |
| ω-6/ω-3 FA ratio | 0.09 | 0.14 | 0.12 | 0.1 | |
ETA eicosatetraenoic acid, EPA eicosapentaenoic acid, DPA all-cis-7,10,13,16,19-docosapentaenoic acid, DHA docosahexaenoic acid. p values less than 0.05 are shown in bold. *p < 0.05; **p < 0.01
Multivariable regression analysis for variables predicting OA severity in male mice resulted in correlations with biochemical factors
To assess the relative contribution of biochemical and biomechanical factors (e.g., body weight) on OA severity, we constructed multivariate generalized linear models to identify which variables remained independently associated with the OA. Specifically, biochemical factors such as serum ω-3 FA (i.e., EPA), ω-6 FA (i.e., osbond acid), and leptin, along with biomechanical factors (i.e., body weight), were used to predict OA severity in male mice. Multivariable regression analysis was restricted to male mice due to general sex dependence of the associations between lipid species and OA. Biochemical factors, particularly serum EPA levels, but not body weight, were significantly associated with OA in male mice (Table 2).
Table 2.
Multivariate regression analyses for variables predicting OA severity
| Parameters | Model 1 | Model 2 |
|---|---|---|
| β | β | |
| Biochemical | ||
| ω-6 FA (osbond acid) | 0.36 (p < 0.08) | |
| ω-3 FA (EPA) | − 0.44* | |
| Leptin | − 0.24 | |
| Biomechanical | ||
| Weight | − 0.15 | − 0.06 |
| Whole model (r2) | 0.47** | 0.01 |
β standardized coefficient, EPA eicosapentaenoic acid. p values less than 0.05 are shown in bold. *p < 0.05; **p < 0.01
Discussion
The findings of this study demonstrated that fat-1 mice had decreased PTOA and joint synovial inflammation in a sex- and diet-dependent manner compared to WT mice, specifically with male fat-1 mice showing a reduced Mankin OA score and female fat-1 mice showing reduced synovitis relative to WT controls. The fat-1 mice also had reduced serum ω-6/ω-3 FA ratios compared to their littermate WT mice. As all mice were fed the same diets in their specific diet groups, the difference in OA severity and synovitis between fat-1 and WT mice can be mainly attributed to the increased levels of endogenous serum ω-3 FAs in fat-1 mice.
While obese fat-1 mice had decreased OA severity and decreased synovitis (female mice only) compared to the obese WT mice (sex-dependent significance), both groups had comparable body weight and percent body fat. These results indicate that altering circulating serum levels of pro- and anti-inflammatory FAs was sufficient to decrease obesity-associated OA, despite the fact that the body weight remained unchanged. Using multivariable regression analysis, we further demonstrated that OA severity was independent of body weight while exhibiting a negative correlation to serum levels of EPA in male mice. This observation is consistent with the results of our recent study showing that a “metabolic” factor such as systemic inflammation, rather than a “mechanical” factor such as body weight, is the main contributor of obesity-related OA following joint injury [17]. These findings are also in line with previous studies showing that leptin-deficient (ob/ob) and leptin receptor–deficient (db/db) transgenic mice, which naturally become obese on control chow diets, do not develop knee OA, further suggesting that body weight by itself may not be a risk factor for joint degeneration in obesity under a control diet [18].
In the present study, we observed that lean female fat-1 mice had comparable OA severity compared to lean female WT mice post-DMM surgery. Malfait et al. showed sex-dependent differences in C57BL/6 mice 8 weeks following surgery, with female mice demonstrating reduced arthritic changes compared to male mice [19]. However, with obesity, female mice demonstrated increased OA [20]. In this study, we observed trends toward mitigated OA scores in obese female fat-1 mice. It has been recently reported that when fed a control diet, fat-1 mice showed no differences in idiopathic OA compared to WT mice [15]. These results imply that the beneficial effects of ω-3 FAs for preventing OA may be accentuated in trauma- and/or diet-induced obesity. Nonetheless, Huang et al. reported that lean female fat-1 mice had significantly lower OA scores compared to lean female WT mice following joint injury [16]. The discrepancy between their study and ours may result from the different time points when the joints were harvested: while the authors of the previous study harvested the joints at 8 weeks following DMM surgery, we sacrificed the mice 12 weeks post-injury. Collectively, these results suggest that increased levels of serum ω-3 FAs delayed OA onset in lean female mice at early time points. However, the severity of cartilage degradation likely reached the same levels at later time points for both female fat-1 and WT mice, supporting the notion that anti-catabolic effects of ω-3 FA on PTOA is more prominent in obesity.
Adipokines, such as leptin and adiponectin, as well as other circulating factors such as insulin are associated with “metabolic syndrome” and have been extensively studied in obesity-linked OA [17, 21]. For example, leptin and insulin levels were elevated in mice on an ω-6 FA-rich HFD compared to those on an ω-3 FA-rich HFD, and leptin had a positive association with OA severity [17]. In the current study, a significantly lower serum leptin concentration was observed in obese female fat-1 mice at 26 weeks of age compared to obese WT mice, which is consistent with previous studies showing that fat-1 mice on a HFD had significantly lower levels of leptin compared to their WT littermates [22]. Although a number of serum and synovial fluid cytokines analyzed did not reach statistical significance by diet or strain, we did observe that lean female fat-1 mice exhibited decreases in serum pro-inflammatory cytokines, including IFN-γ, TNF-α, and MCP-1, compared to lean female WT mice, providing a potential mechanism for the reduction in joint synovitis. Our observation of decreased serum IFN-γ and MCP-1 levels in lean female fat-1 mice is in line with the results of a recent study showing that fat-1 mice exhibit lower gene expression of these two inflammatory molecules in the ankle tissues compared to WT mice after induction of rheumatoid arthritis [23].
Several putative mechanisms through which ω-6 and ω-3 FAs modulate inflammation have been proposed [24–26]. For example, arachidonic acid, an ω-6 FA, can be converted into PGE2, which may play a role in enhancing IL-1β–associated cartilage degradation [27]. On the contrary, ω-3 FAs can enhance insulin sensitivity through G protein–coupled receptor 120 (GPR120) [28], while GRP120 knock-out mice showed accelerated cartilage degeneration compared to WT mice [29]. In the current study, serum ω-6 FAs, particularly γ-linolenic acid and osbond acid, were positively associated with OA in male mice, while serum ω-3 FAs, such as EPA and DPA, were negatively associated with OA and synovitis, respectively. These results corroborate our previous studies showing that obesity-associated OA had opposite associations to serum levels of γ-linolenic acid and EPA in mice. Moreover, serum ω-6 FAs were positively associated with knee synovitis in humans [30]. Growing evidence suggests that dietary FAs can significantly influence circulating levels of various cytokines and adipokines associated with obesity and metabolic syndrome [11–13]. Collectively, our findings provide further evidence that ω-6 FAs play a role as pro-inflammatory mediators, whereas ω-3 FAs may act in an anti-inflammatory manner in obesity and obesity-associated OA.
Both WT and fat-1 mice exhibited similar serum levels of SFAs and MUFAs in molar percentage (mole %), although obese mice fed HFD had decreased serum levels of MUFAs compared to lean mice receiving the control diet. This result indicates that altering ω-6/ω-3 FA ratios has a minimal effect, if any, on the metabolic processes of other types of FAs. Additionally, we found that serum levels of docosanoic acid had a positive correlation with synovitis in male mice. Despite this positive association, it remains unclear how docosanoic acid modulates joint synovitis, although exposure of oligodendrocytes and astrocytes to docosanoic acids led to cell death by inducing mitochondrial depolarization [31]. The observation of the negative association between serum levels of nervonic acid with synovitis in male mice is consistent with our previous findings showing that obese male mice fed ω-3 FA-rich HFD exhibited decreased synovitis and had higher levels of serum nervonic acid compared to the obese mice treated with HFD rich in ω-6 FA or SFA [32], implying a potential anti-inflammatory effect of nervonic acid on synovial inflammation.
We did not observe strong correlations between FAs and OA in female mice; however, serum EPA concentration was negatively associated with joint synovitis. This may be attributed to the generally lower OA scores in female mice compared to male mice, suggesting sex-dependent cartilage degeneration in response to HFD and injury. This result is consistent with a study showing that sex hormones play a critical role in the pathogenesis of injury-induced OA as male mice had more severe OA than females following DMM surgery, while female mice with ovariectomy had exacerbated OA progression due to loss of sex hormones [33]. We also observed that serum insulin concentrations were 10-fold lower in female mice compared to males and that female mice had less weight gain versus male mice under high-fat feeding. In our previous study, female C57BL/6J mice also showed variation in susceptibility to diet-induced obesity [34]. Recently, it has been reported that increases in a regulatory T cell population, instead of inflammatory macrophages, in the adipose tissue upon HFD may help female mice resist obesity-associated inflammation [35], providing a plausible explanation for the observation of low OA in female mice in our study. Additionally, previous findings indicate that estrogen levels are linked to joint homeostasis [36], and estrogen may regulate leptin secretion [37], suggesting potential mechanisms for the sex differences observed in the current study. Nevertheless, future studies are required to elucidate the mechanisms behind the sex differences in obesity-related inflammation and OA development.
Conclusions
In summary, we demonstrated that fat-1 mice exhibited decreased serum ω-6/ω-3 FA ratios, resulting in a mitigation of OA severity despite exhibiting similar body weight compared to WT mice. Interestingly, fat-1 male mice did not exhibit a reduction in synovitis or osteophyte scores, suggesting that different mechanisms are involved in regulating degenerative changes in the cartilage and joint structure, as compared to those regulating synovitis. Our findings provide further evidence that the role of circulating FA composition and associated changes in systemic metabolic inflammation, rather than body weight, may be the major risk factor for obesity-associated OA. Furthermore, the current study also indicates the potential therapeutic benefit of decreasing the serum ω-6/ω-3 FA ratio for mitigating arthritic changes in obese individuals.
Supplementary information
Additional file 1. Supplementary methods and figures
Acknowledgements
The authors would like to thank Steve Johnson, RVT, for his technical support, and Bridgette Furman, Betty Liu, Dr. Katherine Glass, Alison Ross, and Nancy Steward for their assistance during this study. We are grateful to Dr. Karen Steger-May for the assistance with the statistical analysis.
Abbreviations
- OA
Osteoarthritis
- PTOA
Post-traumatic osteoarthritis
- DMM
Destabilization of the medial meniscus
- WT
Wild type
- HFD
High-fat diet
- FA
Fatty acid
- ω-3 FA
Omega-3 fatty acid
- ω-6 FA
Omega-6 fatty acid
- SFA
Saturated fatty acid
- PUFA
Polyunsaturated fatty acid
- MUFA
Monounsaturated fatty acid
- ETA
Eicosatetraenoic acid
- EPA
Eicosapentaenoic acid
- DPA
Docosapentaenoic acid
- DHA
Docosahexaenoic acid
- IL-1
Interleukin 1
- IL-6
Interleukin 6
- IL-10
Interleukin 10
- IL-17
Interleukin 17
- IL-12p70
Interleukin-12 heterodimer
- IFN-γ
Interferon gamma
- TNF-α
Tumor necrosis factor alpha
- MCP-1
Monocyte chemoattractant protein
- PGE2
Prostaglandin E2
- GPR120
G protein–coupled receptor 120
- DXA
-
Dual-energy
X-ray absorptiometry
- BMD
Bone mineral density
Authors’ contributions
KAK designed the research studies, conducted the experiments, acquired the data, analyzed the data, and wrote the manuscript. SJO analyzed the data and wrote the manuscript. JLH conducted the experiments, acquired and analyzed the data, and wrote the manuscript. DL conducted the experiments and wrote the manuscript. VBK designed the research studies and wrote the manuscript. JXK provided the mouse models and wrote the manuscript. CLW designed the research studies, conducted the experiments, acquired the data, analyzed the data, and wrote the manuscript. FG designed the research studies, supervised the studies, analyzed the data, and wrote the manuscript. The authors read and approved the final manuscript.
Funding
This study was supported in part by the Arthritis Foundation; the Nancy Taylor Foundation; NIH grants AR075899, AR50245, AG15768, AG46927, AR074992, and AR073752; and a Taiwan GSSA Scholarship.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to the limit of storage space but are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Chia-Lung Wu and Farshid Guilak contributed equally to this work.
Contributor Information
Chia-Lung Wu, Email: chia-lung.wu@wustl.edu.
Farshid Guilak, Email: guilak@wustl.edu.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s13075-020-02170-7.
References
- 1.Brown TD, Johnston RC, Saltzman CL, et al. Posttraumatic osteoarthritis: a first estimate of incidence, prevalence, and burden of disease. J Orthop Trauma. 2006;20(10):739–744. doi: 10.1097/01.bot.0000246468.80635.ef. [DOI] [PubMed] [Google Scholar]
- 2.Abramson SB, Yazici Y. Biologics in development for rheumatoid arthritis: relevance to osteoarthritis. Adv Drug Deliv Rev. 2006;58(2):212–225. doi: 10.1016/j.addr.2006.01.008. [DOI] [PubMed] [Google Scholar]
- 3.Dickson BM, Roelofs AJ, Rochford JJ, et al. The burden of metabolic syndrome on osteoarthritic joints. Arthritis Res Ther. 2019;21(1):289. doi: 10.1186/s13075-019-2081-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aspden RM. Obesity punches above its weight in osteoarthritis. Nat Rev Rheumatol. 2011;7(1):65–68. doi: 10.1038/nrrheum.2010.123. [DOI] [PubMed] [Google Scholar]
- 5.Daghestani HN, Kraus VB. Inflammatory biomarkers in osteoarthritis. Osteoarthr Cartil. 2015;23(11):1890–1896. doi: 10.1016/j.joca.2015.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Inadera H. The usefulness of circulating adipokine levels for the assessment of obesity-related health problems. Int J Med Sci. 2008;5(5):248–262. doi: 10.7150/ijms.5.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sward P, Frobell R, Englund M, et al. Cartilage and bone markers and inflammatory cytokines are increased in synovial fluid in the acute phase of knee injury (hemarthrosis)--a cross-sectional analysis. Osteoarthr Cartil. 2012;20(11):1302–1308. doi: 10.1016/j.joca.2012.07.021. [DOI] [PubMed] [Google Scholar]
- 8.Lewis JS, Jr, Furman BD, Zeitler E, et al. Genetic and cellular evidence of decreased inflammation associated with reduced incidence of posttraumatic arthritis in MRL/MpJ mice. Arthritis Rheum. 2013;65(3):660–670. doi: 10.1002/art.37796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Higuchi H, Shirakura K, Kimura M, et al. Changes in biochemical parameters after anterior cruciate ligament injury. Int Orthop. 2006;30(1):43–47. doi: 10.1007/s00264-005-0023-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bigoni M, Sacerdote P, Turati M, et al. Acute and late changes in intraarticular cytokine levels following anterior cruciate ligament injury. J Orthop Res. 2013;31(2):315–321. doi: 10.1002/jor.22208. [DOI] [PubMed] [Google Scholar]
- 11.Liddle DM, Hutchinson AL, Wellings HR, et al. Integrated immunomodulatory mechanisms through which long-chain n-3 polyunsaturated fatty acids attenuate obese adipose tissue dysfunction. Nutrients. 2017;9(12):1289–331. [DOI] [PMC free article] [PubMed]
- 12.Farimani AR, Hariri M, Azimi-Nezhad M, et al. The effect of n-3 PUFAs on circulating adiponectin and leptin in patients with type 2 diabetes mellitus: a systematic review and meta-analysis of randomized controlled trials. Acta Diabetol. 2018;55(7):641–652. doi: 10.1007/s00592-018-1110-6. [DOI] [PubMed] [Google Scholar]
- 13.Huang CW, Chien YS, Chen YJ, et al. Role of n-3 polyunsaturated fatty acids in ameliorating the obesity-induced metabolic syndrome in animal models and humans. Int J Mol Sci. 2016;17(10):1689–718. [DOI] [PMC free article] [PubMed]
- 14.Kang JX. Fat-1 transgenic mice: a new model for omega-3 research. Prostaglandins Leukot Essent Fatty Acids. 2007;77(5–6):263–267. doi: 10.1016/j.plefa.2007.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cai A, Hutchison E, Hudson J, et al. Metabolic enrichment of omega-3 polyunsaturated fatty acids does not reduce the onset of idiopathic knee osteoarthritis in mice. Osteoarthr Cartil. 2014;22(9):1301–1309. doi: 10.1016/j.joca.2014.06.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huang MJ, Wang L, Jin DD, Zhang ZM, et al. Enhancement of the synthesis of n-3 PUFAs in fat-1 transgenic mice inhibits mTORC1 signalling and delays surgically induced osteoarthritis in comparison with wild-type mice. Ann Rheum Dis. 2014;73:1719–27. [DOI] [PubMed]
- 17.Wu C-L, Jain D, McNeill JN, et al. Dietary fatty acid content regulates wound repair and the pathogenesis of osteoarthritis following joint injury. Ann Rheum Dis. 2015;74(11):2076–2083. doi: 10.1136/annrheumdis-2014-205601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Griffin TM, Huebner JL, Kraus VB, et al. Extreme obesity due to impaired leptin signaling in mice does not cause knee osteoarthritis. Arthritis Rheumatism. 2009;60(10):2935–2944. doi: 10.1002/art.24854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Malfait A, Ritchie J, Gil A, et al. ADAMTS-5 deficient mice do not develop mechanical allodynia associated with osteoarthritis following medial meniscal destabilization. Osteoarthr Cartil. 2010;18(4):572–580. doi: 10.1016/j.joca.2009.11.013. [DOI] [PubMed] [Google Scholar]
- 20.Griffin TM, Huebner JL, Kraus VB, et al. Induction of osteoarthritis and metabolic inflammation by a very high-fat diet in mice: effects of short-term exercise. Arthritis Rheum. 2012;64(2):443–453. doi: 10.1002/art.33332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Furman BD, Kimmerling KA, Zura RD, et al. Brief report: articular ankle fracture results in increased synovitis, synovial macrophage infiltration, and synovial fluid concentrations of inflammatory cytokines and chemokines. Arthritis Rheumatol. 2015;67(5):1234–1239. doi: 10.1002/art.39064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li J, Li FR, Wei D, et al. Endogenous omega-3 polyunsaturated fatty acid production confers resistance to obesity, dyslipidemia, and diabetes in mice. Mol Endocrinol. 2014;28(8):1316–1328. doi: 10.1210/me.2014-1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Woo SJ, Lim K, Park SY, et al. Endogenous conversion of n-6 to n-3 polyunsaturated fatty acids attenuates K/BxN serum-transfer arthritis in fat-1 mice. J Nutr Biochem. 2015;26(7):713–720. doi: 10.1016/j.jnutbio.2015.01.011. [DOI] [PubMed] [Google Scholar]
- 24.Calder PC. Marine omega-3 fatty acids and inflammatory processes: effects, mechanisms and clinical relevance. Biochim Biophys Acta Mol Cell Biol Lipids. 2015;1851(4):469–484. doi: 10.1016/j.bbalip.2014.08.010. [DOI] [PubMed] [Google Scholar]
- 25.Saini RK, Keum Y-S. Omega-3 and omega-6 polyunsaturated fatty acids: dietary sources, metabolism, and significance—a review. Life Sci. 2018;203:255–267. doi: 10.1016/j.lfs.2018.04.049. [DOI] [PubMed] [Google Scholar]
- 26.Harasymowicz NS, Dicks A, Wu CL, et al. Physiologic and pathologic effects of dietary free fatty acids on cells of the joint. Ann N Y Acad Sci. 2019;1440(1):36–53. doi: 10.1111/nyas.13999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hardy MM, Seibert K, Manning PT, et al. Cyclooxygenase 2-dependent prostaglandin E2 modulates cartilage proteoglycan degradation in human osteoarthritis explants. Arthritis Rheum. 2002;46(7):1789–1803. doi: 10.1002/art.10356. [DOI] [PubMed] [Google Scholar]
- 28.Talukdar S, Bae EJ, Imamura T, et al. GPR120 is an omega-3 fatty acid receptor mediating potent anti-inflammatory and insulin-sensitizing effects. Cell. 2010;142(5):687–698. doi: 10.1016/j.cell.2010.07.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen Y, Zhang D, Ho KW, et al. GPR120 is an important inflammatory regulator in the development of osteoarthritis. Arthritis Res Ther. 2018;20(1):163. doi: 10.1186/s13075-018-1660-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Baker KR, Matthan N, Lichtenstein A, et al. Association of plasma n-6 and n-3 polyunsaturated fatty acids with synovitis in the knee: the MOST study. Osteoarthr Cartil. 2012;20(5):382–387. doi: 10.1016/j.joca.2012.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hein S, Schönfeld P, Kahlert S, et al. Toxic effects of X-linked adrenoleukodystrophy-associated, very long chain fatty acids on glial cells and neurons from rat hippocampus in culture. Hum Mol Genet. 2008;17(12):1750–1761. doi: 10.1093/hmg/ddn066. [DOI] [PubMed] [Google Scholar]
- 32.Wu C-L, Kimmerling KA, Little D, et al. Serum and synovial fluid lipidomic profiles predict obesity-associated osteoarthritis, synovitis, and wound repair. Sci Rep. 2017;7:44315. doi: 10.1038/srep44315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ma H-L, Blanchet T, Peluso D, et al. Osteoarthritis severity is sex dependent in a surgical mouse model. Osteoarthr Cartil. 2007;15(6):695–700. doi: 10.1016/j.joca.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 34.Griffin TM, Fermor B, Huebner JL, et al. Diet-induced obesity differentially regulates behavioral, biomechanical, and molecular risk factors for osteoarthritis in mice. Arthritis Res Ther. 2010;12(4):R130. doi: 10.1186/ar3068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pettersson US, Waldén TB, Carlsson P-O, et al. Female mice are protected against high-fat diet induced metabolic syndrome and increase the regulatory T cell population in adipose tissue. PLoS One. 2012;7(9):e46057. doi: 10.1371/journal.pone.0046057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mannucci E, Ognibene A, Becorpi A, et al. Relationship between leptin and oestrogens in healthy women. Eur J Endocrinol. 1998;139(2):198–201. doi: 10.1530/eje.0.1390198. [DOI] [PubMed] [Google Scholar]
- 37.Roman-Blas JA, Castaneda S, Largo R, et al. Osteoarthritis associated with estrogen deficiency. Arthritis Res Ther. 2009;11(5):241. doi: 10.1186/ar2791. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Supplementary methods and figures
Data Availability Statement
The datasets generated and/or analyzed during the current study are not publicly available due to the limit of storage space but are available from the corresponding author on reasonable request.