Abstract
Study Objectives:
Telemedicine is a novel modality of health care delivery that can improve patients’ access to sleep medicine services, but little is known about telemedicine training during sleep medicine fellowship. We studied telemedicine training prevalence, use, and attitudes of program directors (PDs) and other faculty members, PDs’ receptiveness to a standardized telemedicine curriculum, and whether PDs have reviewed existing American Academy of Sleep Medicine (AASM) sleep telemedicine reference materials.
Methods:
This was an anonymous online survey of all 86 PDs of accredited sleep medicine fellowships in the United States.
Results:
Response rate was 45%. Thirteen (33.3%) of the PDs already offer telemedicine experience to their trainees, although none use a standard telemedicine curriculum. Among the 26 (66.7%) PDs not offering telemedicine experience, 38.5% plan to do so and 53.9% agree that it would benefit fellows. Most PDs (57.9%) report faculty using telemedicine now or within the next 3 years. Many PDs agree that telemedicine is technically feasible, but relatively few agree it is financially feasible (82.1% and 38%, respectively). Few PDs have reviewed both primary AASM telemedicine reference materials. Overall, 64.1% of PDs agree that a national sleep telemedicine curriculum could be useful.
Conclusions:
Although only a minority of current sleep medicine fellows are exposed to telemedicine, it is likely that most will get some exposure in the next 3 years. PDs’ attitudes toward telemedicine vary significantly with respect to feasibility and importance to their programs. Nevertheless, most PDs believe a standardized sleep telemedicine training curriculum could be useful.
Citation:
Fields BG, Dholakia SA, Ioachimescu OC. Sleep telemedicine training in fellowship programs: a survey of program directors. J Clin Sleep Med. 2020;16(4):575–581.
Keywords: fellowship, program director, sleep medicine, telemedicine
BRIEF SUMMARY
Current Knowledge/Study Rationale: Telemedicine is being increasingly employed to improve patient access to sleep medicine care. However, little is known about telemedicine training in sleep medicine fellowship programs, program directors’ attitudes toward telemedicine, and their receptiveness to a standard telemedicine curriculum.
Study Impact: Most responding program directors currently incorporate telemedicine into their fellowship program or anticipate doing so within the next 3 years. Although there is heterogeneity in their attitudes toward the modality, most program directors recognize a need to develop a standard telemedicine curriculum to enhance fellows’ training.
INTRODUCTION
Sleep disorders are common in the general population,1 and millions of Americans have limited access to sleep medicine care due to geography, disability, and clinician shortage.2 The American Academy of Sleep Medicine (AASM) estimates a patient-to-board-certified sleep practitioner ratio of 43,000:1, with many of these clinicians clustering in urban areas within relatively few states. Thus, large areas of the country offer few sleep medicine services. Recognizing this ongoing dilemma, the AASM advocates for telemedicine as one way to “dramatically increase sleep medicine accessibility and clinical efficacy.”3
Sleep telemedicine involves the exchange of sleep-related medical information from one site to another via electronic communications to support a patient’s health.4 The exchange can take a variety of forms, such as telephone, modem, or video. Real-time audiovisual encounters (clinical video telehealth [CVT]) emulate a more traditional, in-person visit. In a 2012 survey, 63% of patients in an academic sleep medicine clinic were willing to utilize telemedicine for their care,5 and a recent report described the Veterans Health Administration’s plans to expand its “TeleSleep” program throughout the country.6 With this growth in sleep telemedicine comes a need to ensure quality of care and the practitioner education needed to attain it. Sleep medicine fellowship training programs serve a vital role in providing that education to future sleep physicians; how (and if) they provide that telemedicine experience has significant ramifications on 21st century sleep medicine practice.
Formalized telemedicine training within sleep medicine fellowships has not been described, so we know little about trainees’ exposure to it in the United States’ 86 Accreditation Council for Graduate Medical Education (ACGME)-accredited fellowship programs. Therefore, we surveyed sleep medicine fellowship program directors (PDs) to explore the current state of telemedicine use and education in their programs. In doing so, we explored 5 overarching questions:
How common is sleep telemedicine exposure among fellowship programs?
What are sleep medicine fellowship PDs’ attitudes toward telemedicine?
How common is telemedicine use among fellowship program faculty members?
Do PDs believe a standard telemedicine curriculum could be useful?
Have PDs reviewed freely accessible, telemedicine-related resources published by the AASM?7,8
METHODS
We created a 26-item survey using the SurveyMonkey platform (https://www.surveymonkey.com) (Table 1). Using the Accreditation Council of Graduate Medical Education 2018–2019 academic year listing,9 we obtained contact information for all 86 American sleep medicine fellowship PDs (or their program coordinators). To ensure accuracy, that information was then cross-referenced with publicly available contact information on the programs’ websites. The PDs received an initial survey invitation via email on July 1, 2019. The invitation described the voluntary and anonymous nature of the data collection and analyses, offered a definition of “sleep telemedicine,” and provided a link to the survey. Any PDs who had not completed the survey were reminded approximately every 10 days until the survey closed on July 31, 2019.
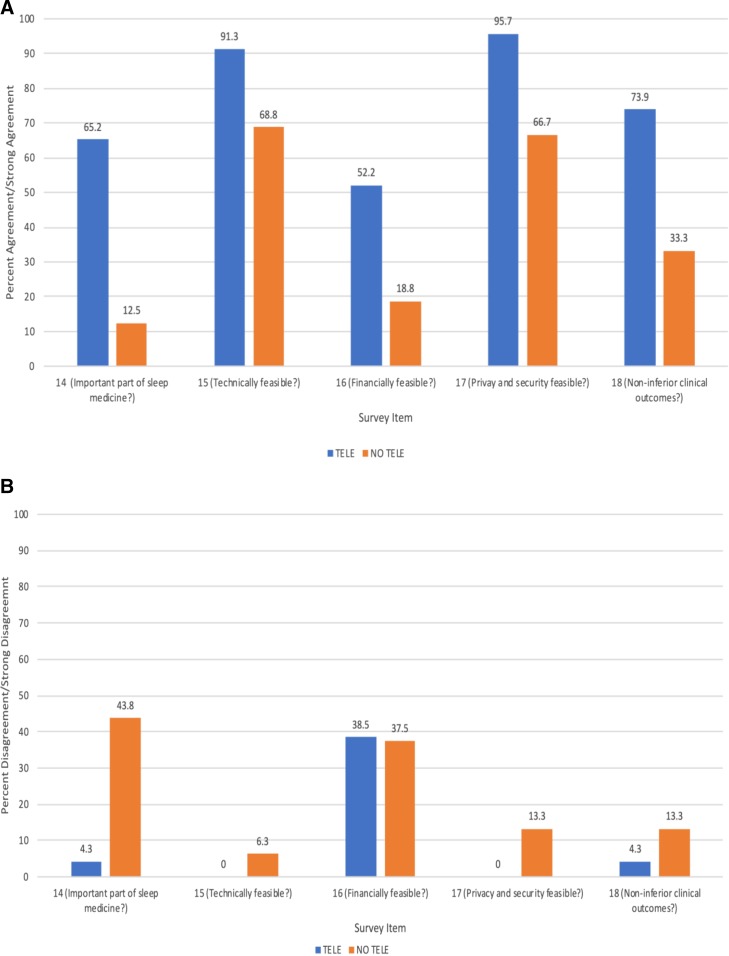
Table 1.
Online survey items.
The survey input was blinded (ie, investigators had no access to individual respondent data). It began with a “consent to participate” form approved by the Emory University Institutional Review Board. Participants completed a series of questions with branching logic; none needed to answer all 26 questions because question progression was based on previous answers. To protect participant anonymity, there was no demographic information collected. Upon completion of the last question, respondents were informed that the survey was completed and thanked for their participation. Data were collected on SurveyMonkey and made available to the investigators in de-identified, aggregate form. Duplicate survey submissions from a single participant were not possible.
The study protocol was approved by the Emory University Institutional Review Board.
RESULTS
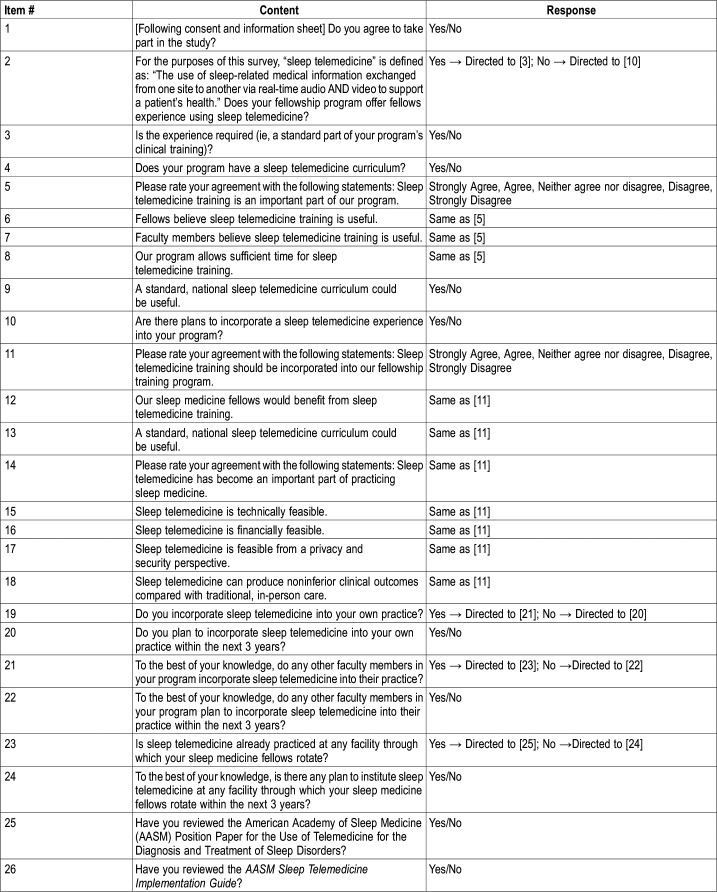
Thirty-nine (45%) PDs completed at least a part of the survey, with 38 PDs (44%) completing it fully. Thirteen (33.3%) programs offer fellows a sleep telemedicine experience (Figure 1). Of those programs, 8 (61.5%) require it as part of their training, but none offer a designated telemedicine curriculum. Nine (69.2%) of these PDs agree that telemedicine is an important part of their program, 77% agree that fellows believe telemedicine training is useful, and 61.5% agree that their faculty members believe telemedicine training is useful. Most of these PDs (69.2%) believe they allow sufficient time for sleep telemedicine training and that a standard, national sleep telemedicine curriculum could be useful.
Figure 1. Flow chart of the study.
PDs = program directors.
Of the 26 (66.7%) programs that do not offer a telemedicine experience, 10 of them report plans to do so. Therefore, 26/39 (66.7%) of all PDs who responded either currently offer or plan to offer a telemedicine experience (Figure 1). Among the 26 PDs who do not currently offer a telemedicine experience, 46.2% agree that telemedicine training should be incorporated into their program, 53.9% agree that fellows would benefit from telemedicine training, and 61.5% agree that a standard, national sleep telemedicine curriculum could be useful.
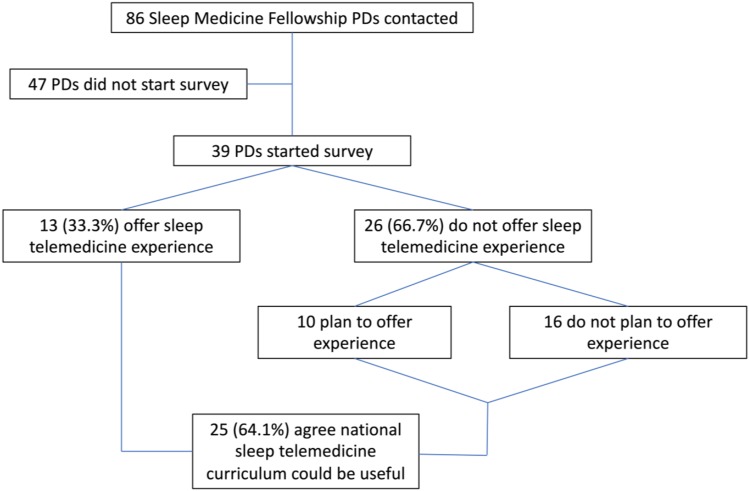
In terms of the 39 PDs’ overall attitudes toward telemedicine, 43.6% agree that it has become an important part of practicing sleep medicine, with 35.9% neither agreeing nor disagreeing (Figure 2). Additionally, 82.1% agree that telemedicine is technically feasible, 38.5% agree that telemedicine is financially feasible (with 43.6% neutral and 17.9% disagreeing), 84.2% agree that telemedicine is feasible from a privacy and security perspective, and 57.9% agree that telemedicine can produce noninferior clinical outcomes compared to in-person care (Figure S1 in the supplemental material).
Figure 2. Respondents’ degree of agreement with the statement: “Sleep Telemedicine has become an important part of practicing Sleep Medicine.”.
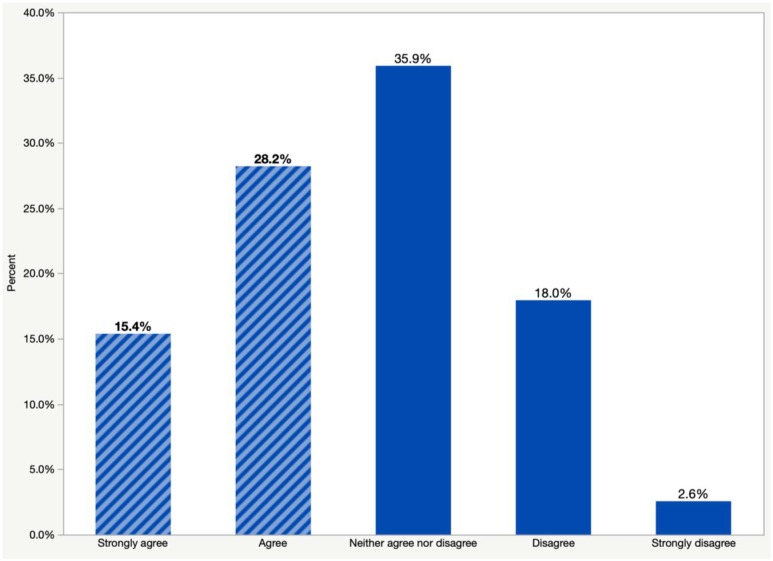
Attitudes among PDs offering telemedicine exposure now or in the near future (TELE) were compared with attitudes among PDs not offering telemedicine exposure (NO TELE). More than half (65.2%) of TELE PDs agreed that telemedicine is an important part of sleep medicine compared with 12.5% of NO TELE PDs (Figure 3A). Similarly, a higher percentage of TELE PDs agreed that telemedicine is feasible from a technical, financial, privacy and security, and clinical outcome perspective. Notably, 43.8% of NO TELE PDs disagreed that telemedicine is an important part of sleep medicine compared with 4.3% of TELE PDs who disagreed (Figure 3B). Additionally, the percentage of TELE PDs and NO TELE PDs who disagreed that telemedicine is financially feasible was nearly the same (38.5% and 37.5%, respectively).
Figure 3. Program director responses to survey items.
(A), program director agreement or strong agreement with survey items. (B), program director disagreement or strong disagreement with survey items. TELE = program directors whose fellows currently have, or will soon have, telemedicine exposure. NO TELE = program directors without plans for fellows to have telemedicine exposure.
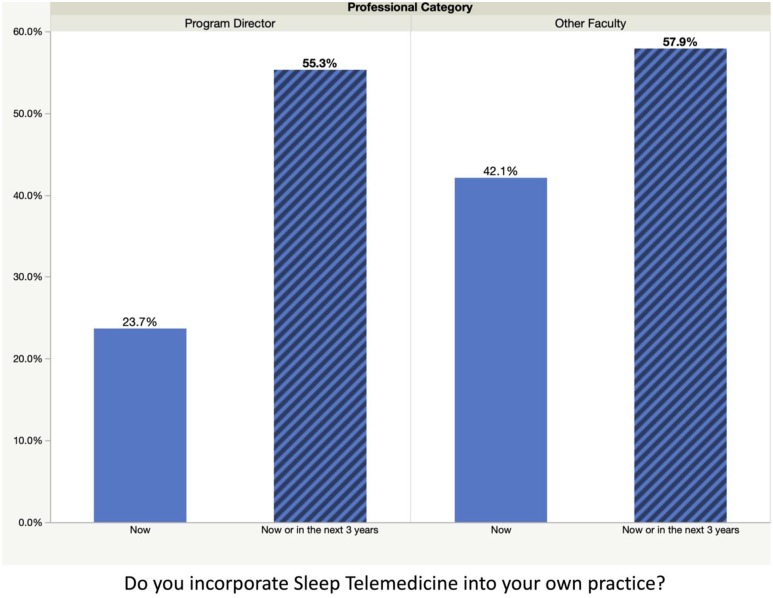
Of 38 PDs, 9 (23.7%) currently incorporate sleep telemedicine into their practice (Figure 4). However, among the PDs currently not using telemedicine, 41.4% expect to be implementing it within 3 years. Therefore, 55.3% of PDs either personally use telemedicine or plan to do so within 3 years. Sixteen PDs (42.1%) report other faculty in their program using telemedicine. Of PDs whose faculty are currently not using telemedicine, 27.3% expect them to start over the next 3 years. Therefore, 57.9% of PDs report that their faculty is either using telemedicine now or planning to use it within the next 3 years.
Figure 4. Respondents’ use of telemedicine currently or within the next 3 years and their assessment of other faculty members’ telemedicine use.
Fifteen PDs (39.5%) report fellows rotating through facilities that use telemedicine. Of the 23 respondents whose fellows do not rotate through a facility with telemedicine, 9 (39.1%) believe that they will do so within the next 3 years. Thus, 63.2% of PDs report fellows rotate through, or will soon rotate through, sites that offer telemedicine experience.
Overall, 64.1% of respondents (9 who currently use sleep telemedicine and 16 who do not) agree that a standard sleep telemedicine curriculum could be useful (Figure 1).
About half (51.4%) of PDs have reviewed the AASM sleep telemedicine position paper,7 but only 9 (24.3%) of responding PDs have reviewed the AASM Sleep Telemedicine Implementation Guide (Figure S2).8
DISCUSSION
To our knowledge, this is the first study exploring the status of telemedicine instruction in accredited sleep medicine fellowship programs. We chose to survey PDs given their influence on trainee education and future career path. Indeed, PDs’ current attitudes could have long-term societal impacts on sleep telemedicine deployment and practice through their trainees. Using this survey data, we suggest the following answers to our 5 overarching questions:
- How common is sleep telemedicine exposure among fellowship programs?One-third of responding PDs report some telemedicine exposure (Figure 1).
- What are sleep medicine fellowship PDs’ attitudes toward telemedicine?While most responding PDs agree it is feasible from technical, privacy/security, and clinical efficacy standpoints, a minority (38.5%) agree it is feasible from a financial perspective. These financial concerns are similar among both the TELE and NO TELE PD groups. Just under half (43.6%) agree that it has become an important part of practicing sleep medicine (Figure 2 and Figure 3).
- How common is telemedicine use among fellowship program faculty members?Nearly a quarter (23.7%) of PDs and 42.1% of other faculty members use telemedicine (Figure 4).
- Do PDs believe a standard telemedicine curriculum could be useful?Whether or not they offer telemedicine as part of their fellowship, most PDs (64.1%) agree that it could be useful (Figure 1).
- Have PDs reviewed freely accessible, telemedicine-related resources published by the AASM?About half of PDs have reviewed the AASM sleep telemedicine position statement, and about a quarter of them have reviewed the AASM Sleep Telemedicine Implementation Guide (Figure S2).
Considering these findings, there appears to be significant heterogeneity in both implementation of telemedicine within fellowship programs and PDs’ attitudes toward it. Figure 2 presents the near-normal distribution of responses among PDs who were asked to rate their agreement with the statement “Sleep telemedicine has become an important part of practicing sleep medicine.” Only 43.6% respondents agreed or strongly agreed with that statement. The largest group of respondents, 35.9%, felt neutral. The fact that the majority of respondents disagreed or felt neutral about the statement offers one reason as to why more programs do not offer telemedicine experiences; PDs do not all believe that it is an important part of clinical practice.
Another factor may be lack of telemedicine-focused education among PDs and their faculty. Relatively few have reviewed the 2 primary, freely accessible sleep telemedicine education resources, ie, the AASM sleep telemedicine position statement and the AASM Sleep Telemedicine Implementation Guide.7,8 Understandably, financial concerns regarding telemedicine implementation may play a role. Indeed, in our survey, most PDs expressed uncertainty or doubt regarding sleep telemedicine’s feasibility from this perspective; similar percentages of TELE PDs and NO TELE PDs disagreed with the statement of financial feasibility (Figure 3B). If fellowship programs and the health systems in which they function worry they cannot maintain telemedicine’s economic solvency, its absence should not be surprising. However, telemedicine reimbursement opportunities continue to grow in parallel with the need for these services. For instance, 36 states now require private insurers to reimburse at least as much for a CVT visit as for an in-person visit (ie, “parity laws”)10 and Medicare continues making strides to include more originating sites in their reimbursement paradigms.11 Educating potential sleep telemedicine practitioners about these financial developments is important to address some ongoing reservations.
Although our study is observational and limited by its sample size, interesting attitude trends emerged in the TELE and NO TELE groups (Figure 3). If a PD’s program did not include telemedicine (NO TELE group), that PD tended to indicate less agreement (and more disagreement) with survey items regarding telemedicine’s feasibility and importance within sleep medicine. Although these findings may appear predictable in the group studied, directionality of association is not. NO TELE PDs may exclude telemedicine from their programs due to their inherent attitudes toward it. On the other hand, a lack of telemedicine may influence their attitudes. That is, NO TELE PDs may recognize a potential deficiency in their program and adjust their attitudes to substantiate its absence. The same logic could be used for the TELE group. As such, it is difficult to ascertain if positive attitudes toward telemedicine beget its inclusion in the program or vice versa.
Also notable is that, while most programs offer or will soon offer telemedicine exposure, none report a sleep medicine curriculum. CVT has been utilized in medical training programs since the 1990s when the Medical College of Georgia used it to monitor students’ patient evaluation skills at rural clinics around the state.12 Since then, telemedicine curricula have proliferated in medical specialty training programs, such as psychiatry,13,14 dermatology,15 and neurology.16 In fact, the American Academy of Neurology convened a Telemedicine Work Group in 2017 to develop core themes for its national teleneurology curriculum.17 One pilot study has shown promise for implementing such a curriculum in terms of residents’ improved knowledge and comfort level with the technology.16 Sleep medicine’s lack of similar telemedicine curricula suggests an area for further development and study.
As with many survey-based observational studies, its results are subject to several limitations. Our response rate of 45% could have led to response bias that affects the generalizability of these findings. We relied completely on the online survey tool to collect data; eliciting responses from PDs at regional and national meetings could have been another tool to reach more participants directly (yet with potential confidentiality-related issues). Therefore, it remains unknown what percentage of nonresponders to the survey offer, or will soon offer, a telemedicine experience. Additionally, we distributed the survey at the beginning of the academic year to maximize PDs’ attention and responses. However, summer seasonality and PDs’ being away from work may have affected the survey completion rate. Another study limitation, linked to relatively small sample size, is a limited ability to perform subgroup analyses. Attitude delineation among TELE and NO TELE PDs was attempted, but our findings should be viewed with caution given the small sample size in each group. We were unable to obtain more information about how PD attitudes or telemedicine availability might influence their including telemedicine as part of their training curriculum.
In summary, we found that relatively few sleep medicine fellowship programs currently provide telemedicine exposure for their trainees. Nevertheless, most responding PDs see value in telemedicine training and in the modality itself. Although only a minority of the PDs have reviewed available AASM sleep telemedicine instruction materials, a majority of them recognize utility of a national, standardized sleep telemedicine curriculum whether or not telemedicine training is currently included in their program. Future directions for this research include a resurvey of PDs as telemedicine use proliferates and development of standardized tools to optimize telemedicine training for 21st century sleep medicine providers.
DISCLOSURE STATEMENT
All authors have seen and approved the manuscript. Work for this study was performed Atlanta VA Healthcare System. Dr. Fields served on the American Academy of Sleep Medicine’s Telemedicine Task Force 2015–2016 and reports no other conflicts of interest or financial support. No other authors report conflicts of interest.
ABBREVIATIONS
- AASM
American Academy of Sleep Medicine
- CVT
clinical video telehealth
- NO TELE
not offering telemedicine exposure
- PD
program director
- TELE
offering telemedicine exposure now or in the near future
REFERENCES
- 1.Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177(9):1006–1014. doi: 10.1093/aje/kws342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bureau of Health Workforce . Health Resources and Services Administration (HRSA), U.S. Department of Health & Human Services. Designated Health Professional Shortage Area Statistics. https://data.hrsa.gov/topics/health-workforce/shortage-areas. Accessed February 26, 2020. [Google Scholar]
- 3.Watson NF, Rosen IM, Chervin RD. Board of Directors of the American Academy of Sleep Medicine The past is prologue: the future of sleep medicine. J Clin Sleep Med. 2017;13(1):127–135. doi: 10.5664/jcsm.6406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zia S, Fields BG. Sleep telemedicine. Chest. 2016;149(6):1556–1565. doi: 10.1016/j.chest.2016.02.670. [DOI] [PubMed] [Google Scholar]
- 5.Kelly JM, Schwamm LH, Bianchi MT. Sleep telemedicine: a survey study of patient preferences. ISRN Neurol. 2012;2012:135329. doi: 10.5402/2012/135329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sarmiento KF, Folmer RL, Stepnowsky CJ, et al. National expansion of sleep telemedicine for veterans: The TeleSleep Program. J Clin Sleep Med. 2019;15(09):1355–1364. doi: 10.5664/jcsm.7934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singh J, Badr MS, Diebert W, et al. American Academy of Sleep Medicine (AASM) position paper for the use of telemedicine for the diagnosis and treatment of sleep disorders. J Clin Sleep Med. 2015;11(10):1187–1198. doi: 10.5664/jcsm.5098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.American Academy of Sleep Medicine Sleep Telemedicine Implementation Guide. https://j2vjt3dnbra3ps7ll1clb4q2-wpengine.netdna-ssl.com/wp-content/uploads/2017/12/SleepTelemedicineImplementationGuide.pdf. Published 2017. Accessed October 3, 2019.
- 9.Accreditional Council for Graduate Medical Education List of Programs by Specialty. https://apps.acgme.org/ads/public/reports/report/1. Accessed October 3, 2019.
- 10.American Telemedicine Association State Policy Resource Center. http://legacy.americantelemed.org/policy-page/state-policy-resource-center. Accessed October 3, 2019.
- 11.Centers for Medicare and Medicade Services Telehealth Services. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/TelehealthSrvcsfctsht.pdf?utm_campaign=2a178f351b-EMAIL_CAMPAIGN_2019_04_19_08_59&utm_term=0_ae00b0e89a-2a178f351b-353229765&utm_content=90024811&utm_medium=social&utm_source=linkedin&hss_channel=lcp-3619444. Published 2019. Accessed October 3, 2019.
- 12.Lentz LM, Fincher RM. Using telemedicine and standardized patients to evaluate off-campus students’ skills. Acad Med. 1999;74(5):598–599. doi: 10.1097/00001888-199905000-00072. [DOI] [PubMed] [Google Scholar]
- 13.Hoffman P, Kane JM. Telepsychiatry education and curriculum development in residency training. Acad Psychiatry. 2015;39(1):108–109. doi: 10.1007/s40596-013-0006-6. [DOI] [PubMed] [Google Scholar]
- 14.Crawford A, Sunderji N, Lopez J, Soklaridis S. Defining competencies for the practice of telepsychiatry through an assessment of resident learning needs. BMC Med Educ. 2016;16(1):28. doi: 10.1186/s12909-016-0529-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wanat KA, Newman S, Finney KM, Kovarik CL, Lee I. Teledermatology education: current use of teledermatology in US residency programs. J Grad Med Educ. 2016;8(2):286–287. doi: 10.4300/JGME-D-16-00041.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Afshari M, Witek NP, Galifianakis NB. Education research: an experiential outpatient teleneurology curriculum for residents. Neurology. 2019;93(4):170–175. doi: 10.1212/WNL.0000000000007848. [DOI] [PubMed] [Google Scholar]
- 17.Govindarajan R, Anderson ER, Hesselbrock RR, et al. Developing an outline for teleneurology curriculum. Neurology. 2017;89(9):951–959. doi: 10.1212/WNL.0000000000004285. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.