Abstract
Study Objectives:
This systematic review aimed to examine the: (1) strength of associations between prenatal sleep (ie, duration, quality, and insomnia) and psychological health (ie, depression, anxiety, and stress); and (2) moderating influence of sociodemographic characteristics (ie, maternal age, gestational age/trimester, parity, marital and socioeconomic status [SES]), body mass index (BMI), and meeting sleep recommendations.
Methods:
A systematic search was conducted using PubMed, PsycINFO, Web of Science, and CINHAL to identify studies with at least one sleep measure and a psychological health outcome. Effect sizes (ES) were calculated by associations between individual components of sleep and psychological health (eg, sleep quality-depression).
Results:
Reviewed studies (n = 32) included 14,648 participants and yielded 219 ES. ES for anxiety/stress were combined due to insufficient data to analyze individually. Average strengths of associations for sleep duration-depression (ES = .52) and sleep duration-anxiety/stress (ES = .48), sleep quality-depression (ES = .55) and sleep quality-anxiety/stress (ES = .58), and insomnia-depression (ES = .67) ranged from medium to large. Marital status, parity, BMI, and meeting sleep recommendations moderated sleep duration-depression and sleep duration-anxiety/stress. SES, gestational age/trimester, parity, and BMI moderated sleep quality-depression and sleep quality-anxiety/stress associations.
Conclusions:
Poor sleep quality and depression are prevalent during pregnancy and may negatively impact maternal and fetal outcomes. Moderating effects suggest that pregnant women of different BMI status and gestational age differ in their sleep habits and depression and anxiety/stress levels. Findings highlight the need to better understand the impact of these associations on maternal-fetal outcomes to inform interventions to improve sleep and psychological health.
Citation:
Pauley AM, Moore GA, Mama SK, Molenaar P, Symons Downs D. Associations between prenatal sleep and psychological health: a systematic review. J Clin Sleep Med. 2020;16(4):619–630.
Keywords: sleep, depression, anxiety, stress, pregnancy
INTRODUCTION
Sleep duration plays an important role in an individual’s overall health. The National Sleep Foundation guidelines suggest that adults get seven to nine hours of sleep per night.1 These recommendations also suggest that adults should not go below 6 hours or above 10 hours per night due to the increased risk of morbidity and mortality.2,3 Although sleep duration recommendations have been set for the general population, there are no pregnancy-specific recommendations for sleep duration, quality, and insomnia. This is problematic as pregnant women are at greater risk for sleep disturbances.4 Prevalence data suggest that poor sleep quality ranges from 29% to 76% among pregnant women.5,6 Poor sleep during pregnancy is associated with increased risks of negative pregnancy outcomes, such as gestational diabetes, preeclampsia, hypertension, excessive gestational weight gain, and cesarean delivery,7–12 the development of negative psychological outcomes, such as depression, anxiety, and stress,13–15 and negative health outcomes for the baby, including, but not limited to, preterm birth and fetal growth restriction.16,17
There are several proposed theoretical models to explain the relationships between sleep and health outcomes.18–22 For example, Grandner and colleagues proposed a socioeconomic framework describing the relationship between short and long sleep with mortality in the general population.20 According to this model, societal (eg, public policy, technology), social (eg, family, socioeconomic), and individual (eg, behavior, psychology) factors directly influence the bidirectional relationship between sleep duration and adverse health outcomes. Further, people from racial minority groups who reside in urban areas, have low education levels, are older, and practice poor health habits (ie, sedentary behaviors) are at a greater risk for short sleep duration and poor sleep and vice versa.23,24 Although this model includes multiple factors proposed to influence sleep, it is limited by primarily focusing on sleep duration, not specifically including psychological health factors related to sleep, and not being specific to pregnant women.
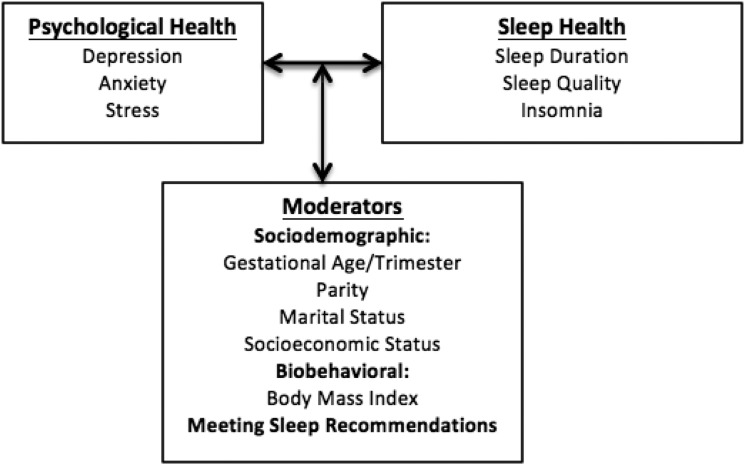
One pregnancy-specific model developed by Okun and colleagues illustrates the relationship between increased sleep disturbances, inflammation, poor health behaviors (eg, obesity), and adverse pregnancy outcomes.21 Poor health behaviors are depicted as having a bidirectional relationship with increased sleep disturbances such that poor health behaviors influence sleep disturbances and vice versa. Despite this model being multifaceted and pregnancy-specific, it does not focus on the association between sleep and psychological health. Thus, we proposed a pregnancy-specific model to address these limitations and explain the bidirectional relationships between sleep and psychological health and the potential moderating influences on these associations (Figure 1). The available evidence in support of this conceptual framework is discussed below.
Figure 1. Proposed conceptual model explaining the interrelationships between sleep and psychological health during pregnancy.
Interrelationships between psychological health sleep outcomes.
Approximately 16% of women experience minor or major depression in pregnancy, and another 5% meet the clinical criteria for major depressive disorder.25 Growing evidence shows a link between depression, poor sleep quality, and insomnia.5,6,26,27 Mellor, Chua, and Boyce examined the association between sleep-disordered breathing and depression in pregnant women and found that those who had poor sleep quality were more depressed.28 Similarly, Paavonen and colleagues reported that 28% of pregnant women with significant symptoms of insomnia had depressive symptoms, and Ko, Chang, and Chen examined sleep quality and depression during the second and third trimesters and found that those who reported depressive symptoms in both trimesters also had worse sleep quality compared to women without symptoms.29,30
There is also evidence that body mass index (BMI) has a moderating influence on the sleep quality-depression association such that pregnant women with overweight and obesity are at higher risk for poor sleep quality and depression compared to normal weight women.8,31 Furthermore, Verbeek and colleagues examined the associations between socioeconomic status (ie, the social class of an individual based on education, income, and occupation) and anxiety, and depression in first trimester pregnant women.32,33 Low socioeconomic status was associated with anxiety and depression and had adverse effects on both psychological health outcomes during pregnancy. Okun and colleagues examined associations between socioeconomic status and sleep among 170 pregnant women between 10–20 weeks gestation and found those with low socioeconomic status had poorer sleep quality.34 Conversely, Salacz and colleagues examined psychological health outcomes in pregnant women with middle to high socioeconomic status and found anxiety levels around the average prevalence but a high level of perceived stress.35
Insomnia is highly prevalent over the course of pregnancy, with symptom rates ranging from 44% to 73%.36,37 Okun and colleagues examined the relationship between sleep deficiency and stress and observed that those who had persistent sleep deficiency throughout the first and second trimesters reported greater levels of stress compared to women without persistent sleep deficiency.14 During pregnancy, stress is also highly prevalent, with 78% women experiencing low-to-moderate stress and 6% experiencing high stress.38 Sleep efficiency (ie, time spend in bed actually asleep) has been shown to be influenced by parity, such that sleep efficiency was lower in multiparous women (ie, women who experienced more than one previous childbirth) compared to nulliparous women (ie, women who have never given birth).39 However, Signal and colleagues reported that nulliparous women had less efficient sleep, more time spent awake after sleep onset, and more time spent in bed compared to multiparous women.40
There is also a small body of evidence suggesting that the prevalence of anxiety during pregnancy ranges from 7% to 60% in pregnant women, which may also be associated with sleep disturbances.41–42 A recent study examined the association between anxiety and insomnia in 1,646 women in the third trimester and found that symptoms of insomnia were influenced by anxiety.29 Shariat and colleagues examined the impact of gestational age on the relationship between sleep quality and anxiety in a sample of 283 women.43 They found that state and trait anxiety were both significantly associated with sleep quality in each trimester, such that sleep quality decreased further along in pregnancy, and the severity of anxiety symptoms increased.43 Further, marital status (eg, single or married) has been linked to anxiety and sleep quality, such that single pregnant women have high anxiety symptoms and poor sleep quality compared to their married counterparts.44,45 This is suggested, in part, due to the lack of social support from a partner.45,46 However, pregnancy impacts both the sleep and psychological health of the non-pregnant spouse, which may negatively impact the sleep and psychological health of the pregnant woman.29 Since the spouse is having sleep and psychological health issues, this may put added stress on the pregnant woman which may influence their sleep and psychological health negatively.29
Moreover, there are few systematic reviews of the literature that summarize potential moderators of the sleep-psychological health associations. Existing reviews have focused on the effect of sleep on pregnancy outcomes (eg, gestational diabetes, preeclampsia) or targeted the postpartum rather than the prenatal period.47–50 Few, if any, reviews have examined associations between prenatal sleep and psychological health and the influence of the possible sociodemographic (ie, maternal age, gestational age/trimester, parity, marital and socioeconomic status [SES]) and biobehavioral (ie, BMI and meeting sleep recommendations) moderators as intervention targets. In addition, guidelines and recommendations for sleep among pregnant women are limited. Due to the physiological and psychological changes that women experience during pregnancy, their sleep needs may change compared to non-pregnant women. For example, pregnant women experience more fragmented sleep due to increased awakenings to urinate or to get comfortable, which may decrease their sleep duration and quality, and negatively impact both mother and infant health.6
Therefore, the purpose of this systematic review was to address the limitations in the literature by examining the: (1) strength of associations between prenatal sleep duration, quality, and insomnia and psychological outcomes (ie, depression, anxiety, and stress), and (2) influence of potential sociodemographic moderators (ie, gestational age/trimester, parity, marital status, socioeconomic status), BMI, and meeting the sleep recommendations on the sleep-psychological health associations. It is hypothesized that: (1) a medium association will be observed between sleep and psychological outcomes, and (2) sociodemographic characteristics (gestational age/trimester, parity, marital status, socioeconomic status), BMI, and meeting sleep recommendations will moderate the strength of association between sleep and psychological outcomes.14,43,51–55
METHODS
A systematic review and meta-analysis of articles was conducted to examine associations between prenatal sleep and psychological health determinants. The review was prepared according to PRISMA statement guidelines.56,57 Methods for data analyses and assessing risk of bias were also identified, and results were reported systematically.
Search strategy
Electronic searches of Medline/PubMed, PsychINFO, CINAHL Complete, ProQuest Dissertations & Thesis A&I, and Web of Science from July 1, 1968 (ie, date of first study conducted examining sleep in pregnancy58 to January 15, 2018 were conducted to identify relevant peer-reviewed articles and primary studies. Search strategies were based on the terms “sleep,” “pregnancy,” and “mental and psychological health” and were limited to human participants (full list available from first author upon request). Search strategies for each database were reviewed and approved by a health science research librarian to ensure proper search terms and procedures were used.59 Reference lists of included articles were hand searched to identify additional articles and primary studies that were missed during electronic database searches.
Data extraction: study selection
Article titles and abstracts were reviewed by the first and last authors. Articles were excluded based on title/abstract review if they did not include: (1) expectant mothers (ie, women who are currently pregnant), (2) at least one measure of sleep (ie, the Pittsburgh Sleep Quality Index; PSQI), or (3) at least one psychosocial measure (ie, measured depression [Edinburgh Postnatal Depression Scale]).The full text of remaining articles were further reviewed to determine if they met additional inclusion criteria. Studies were eligible for inclusion in this review if they: (1) were written in English, (2) conducted with expectant mothers (ie, women who are currently pregnant), (3) contained at least one measure of sleep (ie, the Pittsburgh Sleep Quality Index; PSQI), (4) contained at least one psychological measure (ie, measured depression [Edinburgh Postnatal Depression Scale], anxiety [State-Trait Anxiety Inventory], and/or stress [Perceived Stress Scale]), (5) included participants with or without a confirmed clinical psychological disorder diagnosis, and (6) were cross-sectional, longitudinal, or intervention studies. Studies were excluded if they: (1) had a sample of nonexpectant mothers (mixed samples were used as long as results were reported separately for expectant and nonexpectant mothers), (2) included participants with a sleep disorder diagnosis (eg, obstructive sleep apnea, restless leg syndrome, narcolepsy), (3) review articles, (4) duplicate samples, (5) articles that did not include measures of sleep, depression, anxiety, and/or stress, and (6) did not include statistical data to compute effect sizes. The Joanna Briggs Institute Critical Appraisal tool for Cross Sectional Studies was used for critical appraisal of bias for each individual study.60
Coding procedures
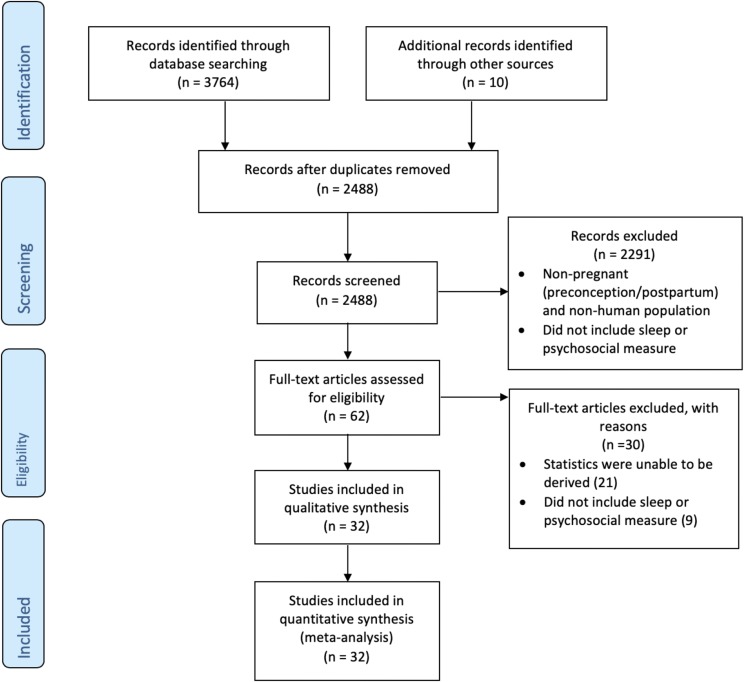
Specific participant characteristics coded were: number of participants, maternal age (in years), socioeconomic status (ie, the social class of an individual based on education, income, and occupation and calculated based on Kuppuswamy’s socioeconomic scale),33,61 marital status, height, weight, BMI category, gestational age at measurement timepoint (in weeks), trimester at measurement timepoint, and parity. Specific study characteristics coded were: author, year, publication format, journal, study type (ie, correlational, experimental, longitudinal, intervention), mode of data collection (ie, in-person, by mail, online), sample size, relevant data (ie, means and standard deviations, ranges, P values), measures of sleep and psychological outcomes, response rate, and the interrelationships of sleep and psychological outcomes (ie, Pearson correlations, odds ratios). As a result of the search strategy and study selection, 32 studies based on 14,648 participants yielded 219 number of effect sizes were retained. The PRISMA flow chart summarizing study selection is shown in Figure 2.
Figure 2. PRISMA search flow diagram.
Flow diagram of study selection.
Statistical analyses
Effect sizes (ES) were calculated to examine the strength of associations between prenatal sleep (duration, quality, and insomnia) and psychological health outcomes, including depression, anxiety, and stress (Purpose 1). To obtain an unbiased estimate of the ES, ES were corrected using the following equation: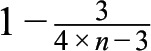 .62
.62
Weighted mean ES were then calculated using the equation:
 |
where:
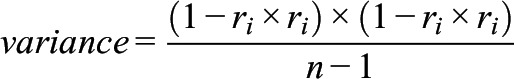 |
and ri is the ith correlation.63
Weighting ES allows for those ES with smaller variances to receive a larger weight then those with larger variances. Cohen’s d ES were then calculated with values of 0.20, 0.50, and 0.80 representing small, medium, and large effects, respectively.64 Average ES were calculated for each association between specific sleep variables (duration, quality, and insomnia) and depression, anxiety/stress.
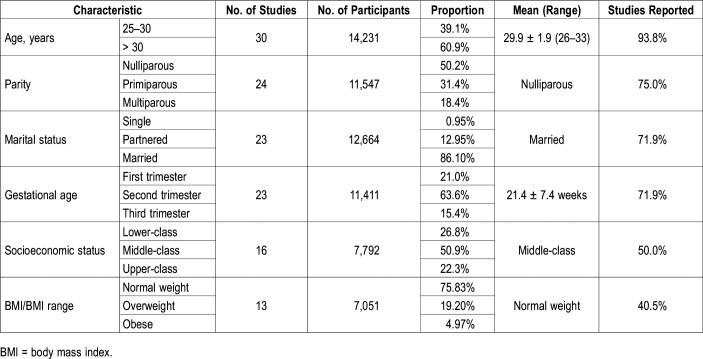
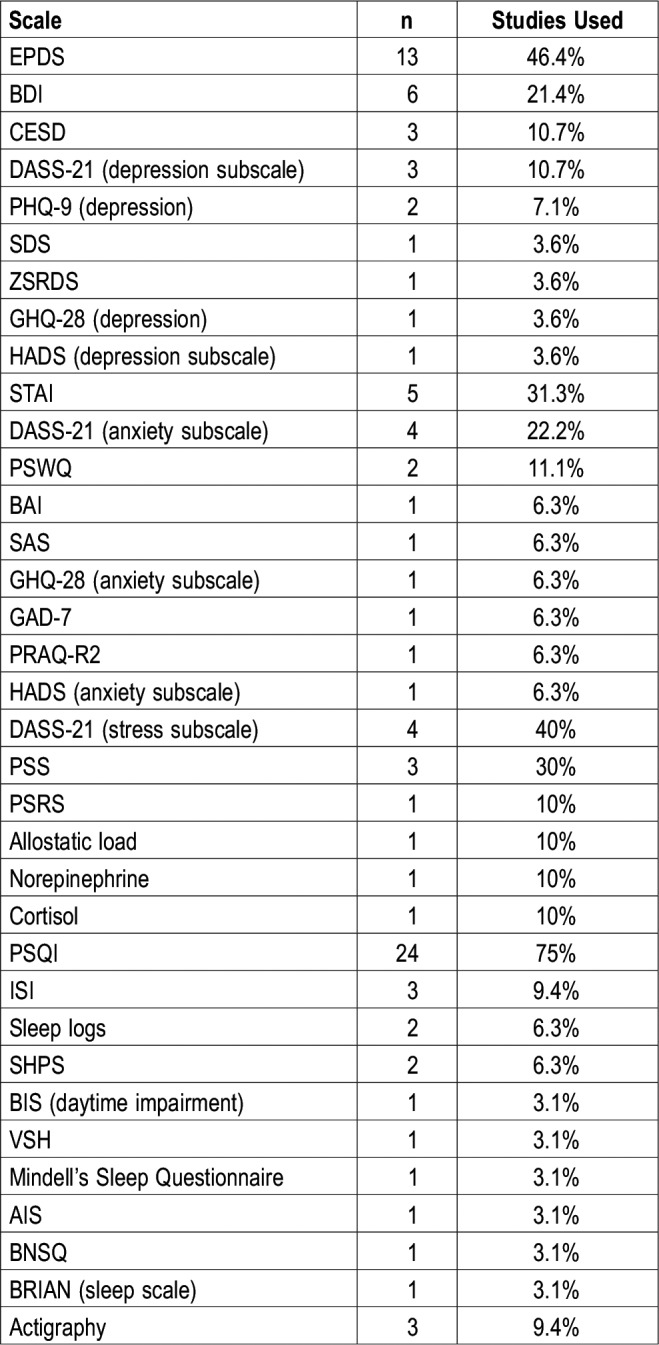
A variety of scales were used to measure the sleep and psychological health outcomes (Table 2). To examine the moderating influences on the ES (Purpose 2), one-way analyses of variance were conducted with Benjamimi-Hochberg false discovery rate procedures to adjust for multiple comparisons for the following moderators: sociodemographic characteristics (gestational age/trimester, parity, marital status, socioeconomic status), BMI, and meeting sleep recommendations.65 Gestational age/trimester was based on typical gestational weeks associated with each trimester: (1) first trimester (gestational age range 1–13 weeks), (2) second trimester (gestational age range 14–27 weeks), and (3) third trimester (gestational age range 28–40 weeks).66 Parity was divided into: (1) nulliparous (never carried a pregnancy beyond 20 weeks gestation), (2) primiparous (1 previous birth), and (3) multiparous (> 1 previous birth).38 Marital status was categorized based on the United States Census Bureau marital status classifications as: (1) single, (2) partnered, and (3) currently married.67 Socioeconomic status was based on calculations from the Kuppuswamy socioeconomic scale categorized as: (1) lower-class, (2) middle-class, and (3) upper-class.61 BMI was divided into three groups: (1) normal weight (BMI 18.9–24.9 kg/m2), (2) overweight (BMI 25–29.9 kg/m2), and (3) obese (BMI ≥ 30.0 kg/m2).68 Meeting sleep recommendations was divided into three groups: (1) < 7 hours, (2) 7–9 hours, and > 9 hours.1 Data was analyzed using SPSS 25 (IBM Corp., Armonk, New York).
Table 2.
Study characteristics.
Assessment of heterogeneity and bias
To examine the homogeneity of ES, the I2 index was calculated on a scale from 0 to 100, representing the ratio of variance among point estimates that can be attributed to heterogeneity.69 Heterogeneity thresholds are 25% for low, 50% for medium, and 75% for high.69 Funnel plots and Egger regression analysis were completed using workbooks from Suurmond and colleagues70 to determine if any publication bias was present.71 To account for studies that were unpublished, not located, or studies with null effects, a fail-safe n, using Hedges and Olkin formula with a trivial criterion value of 0.15, was calculated for each ES sleep-depression, sleep-anxiety, and sleep-stress association.63
RESULTS
Participant and study characteristics
A list of all selected studies is provided in the supplemental material. Table S1 in the supplemental material includes descriptions of selected studies. All studies included pregnant women (n = 32, 100%) with n = 14,648 participants across studies, were conducted between 2016–2017 (n = 16, 50%), 2011–2015 (n = 9, 28.2%), and 2006–2010 (n = 7, 21.8%) and were published (n = 31, 96.9%). Only 34.4% of studies reported a response rate; the average response rate across studies was 85.3%. A total of 3,774 articles were collected, 2,488 (65.9%) remained after removing duplicates; 62 (2.5%) full-text articles were assessed and 32 (51.6%) reviewed. Table S2 in the supplemental material summarizes study measures and ES. The majority of articles were removed due to insufficient data for target variables (70.0%) and due to not including a sleep or psychological measure (30.0%). Not all studies assessed all three of the specific psychological measures; studies measured depression symptoms alone (n = 12, 37.5%), depression and anxiety symptoms, and depression, anxiety and stress (n’s = 7, %’s = 21.9%), and depression and stress, anxiety alone and stress alone (n’s = 2, %’s = 6.3%). Due to insufficient data for anxiety and stress, we averaged these ES together (eg, ES reported as “sleep duration-anxiety/stress”). The majority of the studies reported sleep quality using the Pittsburgh Sleep Quality Index Global score (n = 18, 56.3%) but also reported self-report sleep duration (n = 16, 47.5%), sleep quality (n = 11, 34.4%), and insomnia (n = 5, 15.6%). Additional participant and study details can be found in Table 1 and Table 2.
Table 1.
Participant characteristics.
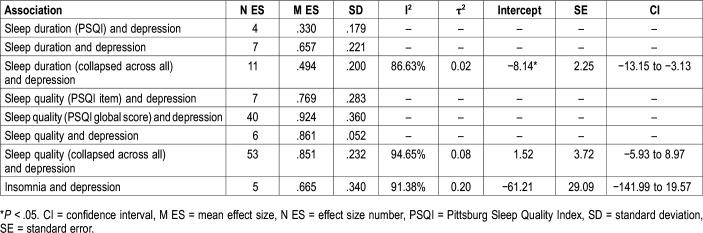
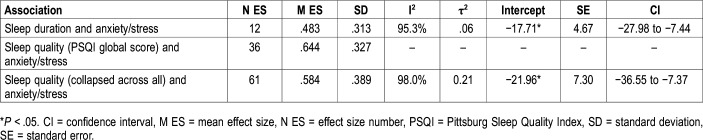
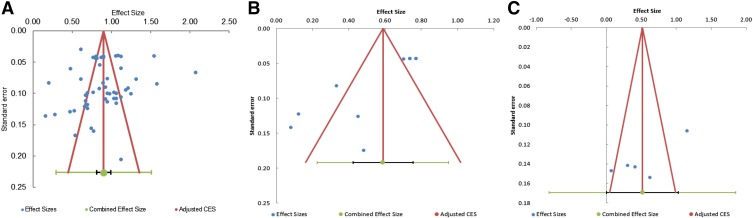
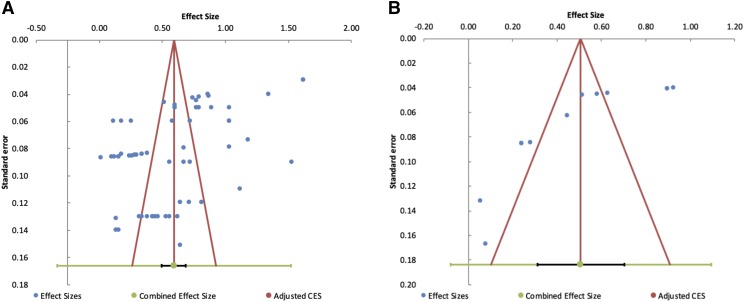
Average ES and heterogeneity scores for associations between sleep duration, sleep quality, and insomnia and depression, anxiety, and stress can be found in Table 3 and Table 4. Random effect models were used to determine overall effects of the various associations and was selected due to the difference of sample sizes among studies and the usage of different measures for sleep and psychological health.72 Average ES for all individual associations ranged from small (ES = .33) to large (ES = .92). I2 test for heterogeneity indicated high amounts of heterogeneity for all associations. Funnel plots illustrated no asymmetry (or no publication bias) except for sleep duration-depression and sleep duration-anxiety/stress, and sleep quality-anxiety/stress (Figure 3 and Figure 4). Average ES for the Pittsburgh Sleep Quality Index sleep quality item score-anxiety/stress and insomnia-anxiety/stress associations were unable to be computed due to insufficient data (ie, less than 2 studies with data to compute ES). Higher scores for sleep (duration, quality, insomnia) and depression/anxiety/stress indicated poorer sleep and greater symptomatology. Thus, shorter sleep duration, poorer sleep quality, and the presence of insomnia, were positively associated with higher depression/anxiety/stress suggesting with worse psychological health symptomatology, there may be decreases in sleep duration and quality, and insomnia may be present.
Table 3.
Effect size and statistics for the associations among self-reported sleep components and self-reported depression.
Table 4.
Effect size and statistics for the associations among sleep quality, sleep duration, and insomnia and self-reported anxiety/stress.
Figure 3. Funnel plots of effect sizes.
(A) sleep quality-depression, (B) sleep duration-depression, and (C) insomnia-depression associations. CES = Combined Effect Size.
Figure 4. Funnel plots of effect sizes.
(A) sleep quality-anxiety/stress and (B) sleep duration-anxiety/stress associations. CES = Combined Effect Size.
Moderation analyses
Table S3, Table S4, Table S5, Table S6, and Table S7 in the supplemental material display the ES means and standard deviations, and the moderating effects of gestational age/trimester, parity, marital status, socioeconomic status, BMI, and meeting the sleep duration guidelines on the strength of the sleep-depression/anxiety/stress associations. Specifically, the strength of sleep duration-depression and sleep duration-anxiety/stress associations were significantly stronger in married women compared to single and/or partnered women and stronger in normal weight women compared to overweight and/or obese women. The strength of the PSQI sleep duration-depression association was examined and was stronger in multiparous women compared to nulliparous women, and the sleep log reported duration-depression association was stronger in women meeting the sleep duration guidelines compared to women who slept > 9 h/night. The sleep quality collapsed across all sleep quality measures-anxiety/stress association was stronger in women in the first trimester compared to women in the second and third trimesters. The PSQI Global quality score-anxiety/stress association was stronger in multiparous women compared to primiparous women and women in upper-class status compared to women in middle-class status.
DISCUSSION
The goals of this review were to examine the: (1) strength of associations between sleep (ie, quality, duration, and insomnia) and psychological outcomes (ie, depression, anxiety/stress) during pregnancy; and (2) influence of potential moderators (sociodemographic: gestational age/trimester, parity, marital status, socioeconomic status; biobehavioral: BMI; meeting sleep recommendations) on these associations. Overall, strengths of all the individual sleep-psychological health associations ranged from small to large such that shorter sleep duration, poor sleep quality, and insomnia were associated with greater depression, anxiety/stress. Specifically, the strength of the sleep quality-depression association was the strongest, illustrating that poor sleep quality and depression are prevalent during pregnancy and could negatively impact maternal and fetal outcomes (eg, gestational diabetes, preterm birth). In addition, BMI had the strongest moderating influence on the sleep duration-depression association, and gestational age/trimester had the strongest moderating influence on the sleep quality-anxiety/stress association. These findings suggest that pregnant women of different BMI status and gestational age differ in their sleep habits and depression/anxiety/stress levels which can potentially influence the sleep-psychological health and in turn, maternal-fetal outcomes. These study findings suggest BMI and gestational age/trimester, as well as parity, marital status and SES, may play a crucial role in the sleep-psychological health associations and maternal-fetal outcomes and should be targeted in future research. More details on these findings are described below.
As hypothesized, the average strengths of the sleep-psychological health associations were medium to large, indicating that sleep was associated with depression/anxiety/stress with variation in the strengths of associations. Specifically, the sleep quality-depression association was the strongest followed by insomnia-depression, sleep quality-anxiety/stress, and sleep duration-depression, and -anxiety/stress suggesting that the sleep quality-depression association may be stronger and more stable compared to the other associations. The strength of the sleep quality-depression association indicates that poor sleep quality was associated with greater depression and vice versa. These findings are consistent with previous literature suggesting that with poorer sleep, shorter sleep duration, and insomnia, depression and anxiety increased and vice versa.29,73 Since the sleep quality-depression association was the strongest, by targeting this relationship, there may be improvements in the other components of sleep and psychological health during pregnancy.
However, these findings may be a result of the varying number of ES sizes between the three psychological health variables (n for depression = 116, n for anxiety/stress = 103). Despite the variation of strengths and limited number of ES, these findings ultimately suggest that the relationships between sleep and depression and anxiety/stress are prevalent during pregnancy. Due to the risk of negative health outcomes associated with poor psychological health symptoms, there is an important need for more research to better understand these interrelationships.
Secondly as hypothesized, the strength of the various sleep-psychological health associations were moderated by various participant characteristics. Specifically, the PSQI global quality score-depression association was stronger in women of upper-class status compared to those of lower-class status suggesting women of upper-class status experience poorer sleep quality and increased depression. There were no significant differences between lower-class and middle/upper-class status. Similarly, the strength of the PSQI global quality score-anxiety/stress association was stronger in women of upper-class status compared to women of middle-class status. These findings are interesting since the majority of existing evidence suggests that issues pertaining to sleep and psychological health individually are more prevalent in women of lower-class status.34,74 However, higher levels of anxiety/stress during pregnancy have been found in pregnant women.35 Since the findings regarding the influence of socioeconomic status level within this review are conflicting with the existing evidence and since research in this area is in its infancy, more research is needed to understand the specific needs and issues of pregnant women in each socioeconomic status level. Researchers may be able to provide tailored education and strategies to help pregnant women cope and deal with any pressures they feel from providing for their families, multiple work responsibilities, and their pending labor, delivery, and adjusting to life with a newborn.
The strength of the PSQI global quality score-anxiety/stress association was also stronger in multiparous women compared to primiparous women, suggesting that poor sleep and increases in anxiety/stress are prevalent in women with children compared to those who have given birth once previously. Polo-Kantola and colleagues examined sleep quality in 78 pregnant women and found that multiparous women had difficulty falling asleep and poorer sleep quality and anxiety.75,76 These current findings may be attributed to the added responsibilities and stressors associated with having multiple children at home, and any lingering anxiety due to previously difficult labor and birth experiences.76 Existing evidence examining the influence of parity is limited, which suggests a need for future research in this area.
The sleep quality-anxiety/stress association was stronger in women in their first trimester compared to women in their second and third trimesters, suggesting that at the beginning of pregnancy, sleep quality is poor and there is an increase in anxiety/stress compared to the second and third trimesters. These findings are similar to those of Lee et al who found anxiety was more prevalent in the first trimester compared to the second and third trimesters.55 These findings suggest that the first trimester may be the best time to target improving sleep and psychological health for a lasting effect throughout pregnancy since women are more amenable to receiving intervention content on these topics during this time. For example, by intervening early on negative sleep practices, improving coping techniques, and providing the education and skills needed to prepare for the later stages of pregnancy, increases in anxiety, stress, and sleep issues may be reduced throughout later pregnancy and potentially into postpartum.
The strengths of the sleep duration-depression and sleep duration-anxiety/stress associations were stronger in women who were married compared to those who were partnered and/or single. These findings are in contrast to those of Naud and colleagues who found that single motherhood was significantly associated with poor sleep quality and could be due to lack of social support.45 However, despite having spousal support, issues within the marriage and spousal sleep habits may negatively influence the sleep and psychological health of pregnant women. Spousal sleep habits were not reported in the reviewed studies and should be examined in future research. This will allow for a better understanding of what spousal sleep behaviors can be modified to improve the sleep of the expectant mothers and, in turn, the spouse. Also, since there was a limited number of studies that examined the sleep-psychological health associations in single pregnant women, studies should target single pregnant women in order to understand how single motherhood impacts sleep and psychological health.
In contrast to the hypothesis and past researchers’ conclusions,53,77 the sleep duration-depression and sleep duration-anxiety/stress associations were stronger in normal weight women compared to women with overweight/obesity. Although it is well-known that pregnant women with overweight/obesity have poorer sleep quality, shorter sleep duration, and higher risk for negative psychological health than normal weight women, these findings suggest that when normal weight women had poorer sleep quality and shorter sleep duration, there was also an increase in depression and anxiety/stress. These findings also suggest that normal weight pregnant women may need as much assistance with improving their sleep and psychological health as those with overweight/obesity. For example, all pregnant women are at risk for pregnancy-related sleep apnea which may increase the chances of snoring, disturbed sleep, and negative pregnancy outcomes.78 Thus, it is important to identify strategies to reduce sleep apnea and related sleep disturbances in all pregnant women regardless of their prepregnancy weight status to promote healthy pregnancies.
Lastly, it was hypothesized that meeting sleep recommendations (7–9 h/night) would be associated with lower levels of depression. However, the sleep duration-depression association was stronger in women who slept 7–9 h/night compared to women who slept > 9 h/night, which did not agree with the hypothesis. However, these findings are limited in that it cannot be inferred that sleeping 7–9 h/night is the same as having good quality sleep such that women may be meeting the duration recommendations but as pregnancy progresses their quality of sleep may be worsening. For example, a woman could sleep 8 hours but may not feel fully rested regardless of sleeping the recommended duration. This suggests sleep duration and quality should be considered together when developing sleep recommendations during pregnancy.
Limitations
This study included strengths such as producing a thorough synthesis and review of the evidence, providing important insight into the relationships and potential moderating effects between sleep and psychological health, and suggesting recommendations for researchers and clinicians. Despite these strengths, this study is not without its limitations. First, many of the studies reviewed used measures of depression and anxiety but did not include measures of stress, resulting in a limited number of ES. In addition, most sleep studies relied on the PSQI to assess sleep, which is limited by its self-reported nature, and lacked objective measures of sleep. Due to inconsistencies across actigraphy variables and insufficient ES, these studies (n = 2) were excluded and important sleep variables (ie, number of daytime naps and nap duration) could not be examined. More research using objective measures, in combination with consistent self-reported measures of sleep, is needed to obtain more accurate values of sleep outcomes by reducing the variability and error when self-reporting variables such as duration. Additionally, the number of ES for various sleep variable and psychological health outcome (ie, sleep-anxiety and sleep-stress, individually) associations were limited so conclusions were unable to be drawn and moderation analyses were unable to be performed. More research is needed to understand these relationships and what factors may impact these associations. Some findings of this review were in conflict with existing evidence (ie, socioeconomic status) in regard to moderation analyses, which need to be examined further in order to obtain a comprehensive understanding of the needs of pregnant women when it comes to sleep and psychological health. Also, pregnancy spacing was one factor that may explain the conflicting findings and influence these associations was not coded due to insufficient data (ie, studies did not report on pregnancy spacing). This area needs further research in order to understand how multiple pregnancies and the time in-between may impact sleep and psychological health. Lastly, additional biobehavioral factors (ie, gestational weight gain, physical activity) were to be examined but due to insufficient data, they were excluded. These variables are important during pregnancy and need to be examined and included in future research studies.
Also, the majority of the studies reviewed were observational/cross-sectional and were only conducted between 2016–2017. This research area is in its infancy and there is a need to conduct longitudinal and intervention studies. This will allow for the better understanding of the changes that occur throughout pregnancy in relation to sleep and psychological health, the potential moderating effects of other participant characteristics, and the impact of behavior modification on sleep and/or psychological health during pregnancy. Lastly, there was some evidence of publication bias found for the sleep duration-depression and sleep duration-anxiety/stress and sleep quality-anxiety/stress associations. The potential reasons for this publication bias may be due to the use of various measures to examine depression/anxiety/stress and sleep as well as the majority of the studies only reporting significant findings.
CONCLUSIONS
To our knowledge, this is one of the first systematic reviews to examine associations between sleep and psychological health, and the influence of potential moderators on those relationships. In summary, we found that poor sleep quality and depression are prevalent during pregnancy and moderating effects suggest that pregnant women of different BMI status and gestational age differ in their sleep habits and levels of depression, anxiety, and stress. These findings are significant because they can provide the evidence-base for future studies focusing on prenatal sleep and psychological health. To improve upon the gaps in the current literature, researchers aiming to study prenatal sleep and psychological health may want to consider including measures of multiple components of sleep (eg, sleep quality, total sleep time, naptime duration, etc.) and moderator variables such as gestational age/trimester, parity, BMI, marital status, and socioeconomic status.
DISCLOSURE STATEMENT
All authors have seen and approved this manuscript. Work for this study was performed at The Pennsylvania State University. The authors report no conflicts of interest.
ABBREVIATIONS
- BMI
body mass index
- ES
effect sizes
- PSQI
Pittsburg Sleep Quality Index
- SES
socioeconomic status
REFERENCES
- 1.National Sleep Foundation Sleep Hygiene. https://www.sleepfoundation.org/sleep-topics/sleep-hygiene. Accessed September 3, 2018.
- 2.Cappuccio F, D’Elia L, Strazzullo P, Miller M. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 2010;33(5):585–592. doi: 10.1093/sleep/33.5.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hirshkowitz M, Whiton K, Albert S, et al. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health J Natl. Sleep Found. 2015;1(1):40–43. doi: 10.1016/j.sleh.2014.12.010. [DOI] [PubMed] [Google Scholar]
- 4.Hashmi A, Bhatia S, Bhatia S, Khawaja I. Insomnia during pregnancy: diagnosis and rational interventions. Pak J Med Sci. 2016;32(4):1030–1037. doi: 10.12669/pjms.324.10421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gelaye B, Barrios Y, Zhong Q, et al. Association of poor subjective sleep quality with suicidal ideation among pregnant Peruvian women. Gen Hosp Psychiatry. 2015;37(5):441–447. doi: 10.1016/j.genhosppsych.2015.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mindell J, Cook R, Nikolovski J. Sleep patterns and sleep disturbances across pregnancy. Sleep Med. 2015;16(4):483–488. doi: 10.1016/j.sleep.2014.12.006. [DOI] [PubMed] [Google Scholar]
- 7.Facco F, Grobman W, Kramer J, Ho K, Zee P. Self-reported short sleep duration and frequent snoring in pregnancy: impact on glucose metabolism. Am J Obstet Gynecol. 2010;203(2):142–145. doi: 10.1016/j.ajog.2010.03.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gay C, Richoux S, Beebe K, Lee K. Sleep disruption and duration in late pregnancy is associated with excess gestational weight gain among overweight and obese women. Birth. 2017;44(2):173–180. doi: 10.1111/birt.12277. [DOI] [PubMed] [Google Scholar]
- 9.O’Brien L, Bullough A, Owusu J, et al. Pregnancy-onset habitual snoring, gestational hypertension, and preeclampsia: prospective cohort study. Am. J. Obstet. Gynecol. 2012;207(6):487–489. doi: 10.1016/j.ajog.2012.08.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Qiu C, Enquobahrie D, Frederick I, Abetwe D, Williams M. Glucose intolerance and gestational diabetes risk in relation to sleep duration and snoring during pregnancy: a pilot study. BMC Womens Health. 2010;10(1):17. doi: 10.1186/1472-6874-10-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sharma S, Nehra A, Sinha S, et al. Sleep disorders in pregnancy and their association with pregnancy outcomes: A prospective observational study. Sleep Breath. 2016;20(1):87–93. doi: 10.1007/s11325-015-1188-9. [DOI] [PubMed] [Google Scholar]
- 12.Williams M, Miller R, Qiu C, Cripe S, Gelaye B, Enquobahrie D. Associations of early pregnancy sleep duration with trimester-specific blood pressures and hypertensive disorders in pregnancy. Sleep. 2010;33(10):1363–1371. doi: 10.1093/sleep/33.10.1363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Okun M, Kiewra K, Luther J, Wisniekwski S, Wisner K. Sleep disturbances in depressed and nondepressed pregnant women. Depress Anxiety. 2011;28(8):676–685. doi: 10.1002/da.20828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Okun M, Kline C, Roberts J, Wettlaufer B, Glover K, Hall M. Prevalence of sleep deficiency in early gestation and its associations with stress and depressive symptoms. J Womens Health (Larchmt) 2013;22(12):1028–1037. doi: 10.1089/jwh.2013.4331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wolfson A, Crowley S, Anwer U, Bassett J. Changes in sleep patterns and depressive symptoms in first-time mothers: last trimester to 1-year postpartum. Behav Sleep Med. 2003;1(1):54–67. doi: 10.1207/S15402010BSM0101_6. [DOI] [PubMed] [Google Scholar]
- 16.Micheli K, Komninos I, Bagkeris E, Roumeliotaki T, Koutis A, Kogevinas M, Chatzi L. Sleep patterns in late pregnancy and risk of preterm birth and fetal growth restriction. Epidemiol. 2011;22(5):738–744. doi: 10.1097/EDE.0b013e31822546fd. [DOI] [PubMed] [Google Scholar]
- 17.Okun M, Luther J, Wisniewski S, Sit D, Prairie B, Wisner K. Disturbed sleep, a novel risk factor for preterm birth? J Womens Health (Larchmt) 2012;21(1):54–60. doi: 10.1089/jwh.2010.2670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Berger A. Update on the state of the science: sleep-wake disturbances in adult patients with cancer. Oncol Nurs Forum. 2009;36(4):E165–E177. doi: 10.1188/09.ONF.E165-E177. [DOI] [PubMed] [Google Scholar]
- 19.Germain A, McKeon A, Campbell R. Sleep in PTSD: conceptual model and novel directions in brain-based research and intervention. Curr Opin Psychol. 2017;14:84–89. doi: 10.1016/j.copsyc.2016.12.004. [DOI] [PubMed] [Google Scholar]
- 20.Grandner M, Hale L, Moore M, Patel NP. Mortality associated with short sleep duration: the evidence, the possible mechanisms, and the future. Sleep Med Rev. 2009;14(3):191–203. doi: 10.1016/j.smrv.2009.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Okun M, Roberts J, Marsland A, Hall M. How disturbed sleep may be a risk factor for adverse pregnancy outcomes. Obstet Gynecol Surv. 2009;64(4):273–280. doi: 10.1097/OGX.0b013e318195160e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Smith M, Quartana P, Okonkwo R, Nasir A. Mechanisms by which sleep disturbance contributes to osteoarthritis pain: a conceptual model. Curr Pain Headache Rep. 2009;13(6):447–454. doi: 10.1007/s11916-009-0073-2. [DOI] [PubMed] [Google Scholar]
- 23.Hale L. Who has time to sleep? J Public Health (Oxf) 2005;27(2):205–211. doi: 10.1093/pubmed/fdi004. [DOI] [PubMed] [Google Scholar]
- 24.Hale L, Peppard P, Young T. Does the demography of sleep contribute to health disparities? In: Sleep Disorders: Their Impact on Public Health. Leger D, Prandi-Perumal SR, eds. New York, NY: Informa Healthcare; 2007. [Google Scholar]
- 25.Gavin N, Gaynes B, Lohr K, Meltzer-Brody S, Gartlehner G, Swinson T. Perinatal depression: a systematic review of prevalence and incidence. Obstet Gynecol. 2005;106(5 Pt 1):1071–1083. doi: 10.1097/01.AOG.0000183597.31630.db. [DOI] [PubMed] [Google Scholar]
- 26.Leight K, Fitelson E, Weston C, Wisner K. Childbirth and mental disorders. Int Rev Psychiatry. 2010;22(5):435–471. doi: 10.3109/09540261.2010.514600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Okun M, Schetter C, Glynn L. Poor sleep quality is associated with preterm birth. Sleep. 2011;34(11):1493–1498. doi: 10.5665/sleep.1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mellor R, Chua SC, Boyce P. Antenatal depression: an artefact of sleep disturbance? Arch Womens Ment Health. 2014;17(4):291–302. doi: 10.1007/s00737-014-0427-6. [DOI] [PubMed] [Google Scholar]
- 29.Paavonen E, Saarenpää-Heikkilä O, Pölkki P, Kylliäinen A, Porkka-Heiskanen T, Paunio T. Maternal and paternal sleep during pregnancy in the child-sleep birth cohort. Sleep Med. 2017;29:47–56. doi: 10.1016/j.sleep.2016.09.011. [DOI] [PubMed] [Google Scholar]
- 30.Ko S, Chang S, Chen C. A comparative study of sleep quality between pregnant and nonpregnant Taiwanese women. J Nurs Scholarsh. 2010;42(1):23–30. doi: 10.1111/j.1547-5069.2009.01326.x. [DOI] [PubMed] [Google Scholar]
- 31.Molyneaux E, Poston L, Williams S, Howard L. Obesity and mental disorders during pregnancy and postpartum: A systematic review and meta-analysis. Obstet Gynecol. 2014;123(4):857–867. doi: 10.1097/AOG.0000000000000170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Verbeek T, Bockting C, Beijers C, Meijer J, van Pampus M, Burger H. Low socioeconomic status increases effects of negative life events and antenatal anxiety and depression. Women Birth. 2019;32(1):e138–e143. doi: 10.1016/j.wombi.2018.05.005. [DOI] [PubMed] [Google Scholar]
- 33.American Psychological Association Socioeconomic status. https://www.apa.org/topics/socioeconomic-status. Accessed January 25, 2019.
- 34.Okun M, Tolge M, Hall M. Low socioeconomic status negatively affects sleep in pregnant women. J Obstet Gynecol Neonatal Nurs. 2014;43(2):160–167. doi: 10.1111/1552-6909.12295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Salacz P, Csukly G, Haller J, Valen S. Association between subjective feelings of distress, plasma cortisol, anxiety, and depression in pregnant women. Eur J Obstet Gynecol Reprod Biol. 2012;165(2):225–230. doi: 10.1016/j.ejogrb.2012.08.017. [DOI] [PubMed] [Google Scholar]
- 36.Fernández-Alonso A, Trabalón-Pastor M, Chedraui P, Perez-Lopez F. Factors related to insomnia and sleepiness in the late third trimester of pregnancy. Arch Gynecol Obstet. 2012;286(1):55–61. doi: 10.1007/s00404-012-2248-z. [DOI] [PubMed] [Google Scholar]
- 37.Román-Gálvez R, Amezcua-Prieto C, Salcedo-Bellino I, Martinez-Galiano J, Kahn K, Bueno-Cavanillas A. Factors associated with insomnia in pregnancy: a prospective Cohort Study. Eur J Obstet Gynecol Reprod Biol. 2018;221:70–75. doi: 10.1016/j.ejogrb.2017.12.007. [DOI] [PubMed] [Google Scholar]
- 38.Dunkel Schetter C, Tanner L. Anxiety, depression and stress in pregnancy: implications for mothers, children, research, and practice. Curr Opin Psychiatry. 2012;25(2):141–148. doi: 10.1097/YCO.0b013e3283503680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lee K, Zaffke M, Mcenany G. Parity and sleep patterns during and after pregnancy. Obstet Gynecol. 2000;95:14–18. doi: 10.1016/s0029-7844(99)00486-x. [DOI] [PubMed] [Google Scholar]
- 40.Signal T, Gander P, Sandalli M, Travier N, Firestone R, Tuohy J. Sleep duration and quality in healthy nulliparous and multiparous women across pregnancy and post‐partum. Aust N Z J Obstet Gynaecol. 2007;47(1):16–22. doi: 10.1111/j.1479-828X.2006.00672.x. [DOI] [PubMed] [Google Scholar]
- 41.Andersson L, Sundstrom-Poromaa I, Bixo M, Wulff M, Bondestam K, Astrom M. Point prevalence of psychiatric disorders during the second trimester of pregnancy: a population-based study. Am J Obstet Gynecol. 2003;189(1):148–154. doi: 10.1067/mob.2003.336. [DOI] [PubMed] [Google Scholar]
- 42.Faisal-Cury A, Rossi Menezes P. Prevalence of anxiety and depression during pregnancy in a private setting sample. Arch Women Ment Health. 2007;10(1):25–32. doi: 10.1007/s00737-006-0164-6. [DOI] [PubMed] [Google Scholar]
- 43.Shariat M, Abedinia N, Noorbala A, Raznahan M. The relationship between sleep quality, depression, and anxiety in pregnant women: a cohort study. JSS. 2018;2(1-2):20–27. [Google Scholar]
- 44.Fadzil A, Balakrishnan K, Razali R, et al. Risk factors for depression and anxiety among pregnant women in Hospital Tuanku Bainun, Ipoh, Malaysia. Asia-Pac Psychiatry. 2013;5:7–13. doi: 10.1111/appy.12036. [DOI] [PubMed] [Google Scholar]
- 45.Naud K, Ouellet A, Brown C, Pasquier J, Moutquin J. Is sleep disturbed in pregnancy? J Obstet Gynaecol Can. 2010;32(1):28–34. doi: 10.1016/S1701-2163(16)34400-0. [DOI] [PubMed] [Google Scholar]
- 46.Rini C, Dunkel Schetter C, Hobel C, Glynn L, Sandman C. Effective social support: antecedents and consequences of partner support during pregnancy. Pers Relatsh. 2006;13(2):207–229. [Google Scholar]
- 47.Chang J, Pien G, Duntley S, Macones G. Sleep deprivation during pregnancy and maternal and fetal outcomes: is there a relationship? Sleep Med Rev. 2010;14(2):107–114. doi: 10.1016/j.smrv.2009.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pamidi S, Pinto LM, Marc I, Benedetti A, Schwartzman K, Kimoff RJ. Maternal sleep-disordered breathing and adverse pregnancy outcomes: a systematic review and metaanalysis. Am J Obstet Gynecol. 2014;210(1):52.e1–52.e14. doi: 10.1016/j.ajog.2013.07.033. [DOI] [PubMed] [Google Scholar]
- 49.Bhati S, Richards K. A systematic review of the relationship between postpartum sleep disturbance and postpartum depression. J Obstet Gynecol Neonatal Nurs. 2015;44(3):350–357. doi: 10.1111/1552-6909.12562. [DOI] [PubMed] [Google Scholar]
- 50.Lawson A, Murphy K, Sloan E, Uleryk E, Dalfen A. The relationship between sleep and postpartum mental disorders: a systematic review. J Affect Disord. 2015;176:65–77. doi: 10.1016/j.jad.2015.01.017. [DOI] [PubMed] [Google Scholar]
- 51.Ruiz-Robledillo N, Canário C, Dias C, Moya-Albiol L, Figueiredo B. Sleep during the third trimester of pregnancy: the role of depression and anxiety. Psychol Health Med. 2015;20(8):927–932. doi: 10.1080/13548506.2015.1017508. [DOI] [PubMed] [Google Scholar]
- 52.Facco F, Kramer J, Ho K, Zee P, Grobman W. Sleep disturbances in pregnancy. Obstet Gynecol. 2010;115(1):77–83. doi: 10.1097/AOG.0b013e3181c4f8ec. [DOI] [PubMed] [Google Scholar]
- 53.Guinhouya BC, Bisson M, Dubois L, et al. Body weight status and sleep disturbances during pregnancy: does adherence to gestational weight gain guidelines matter? J Womens Health (Larchmt) 2019;28(4):535–543. doi: 10.1089/jwh.2017.6892. [DOI] [PubMed] [Google Scholar]
- 54.Hutchinson B, Stone PR, McCowan L, Stewart A, Thompson J, Mitchell E. A postal survey of maternal sleep in late pregnancy. BMC Pregnancy Childbirth. 2010;12:144. doi: 10.1186/1471-2393-12-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lee A, Lam S, Sze Mun Lau S, Chong C, Chui H, Fong D. Prevalence, course, and risk factors for antenatal anxiety and depression. Obstet Gynecol. 2007;110(5):1102–1112. doi: 10.1097/01.AOG.0000287065.59491.70. [DOI] [PubMed] [Google Scholar]
- 56.Liberati A, Altman D, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1–e34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 57.Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Branchey M, Petre-Quadens O. A comparative study of sleep parameters during pregnancy. Acta Neurol Belg. 1968;68(7):453–459. [PubMed] [Google Scholar]
- 59.Institute of Medicine (IOM) Standards for systematic reviews. https://iom.nationalacademies.org/Reports/2011/Finding-What-Works-in-Health-Care-Standards-for-Systematic-Reviews/Standards.aspx. Updated January 16, 2018. Accessed November 11, 2018.
- 60.Moola S, Munn Z, Tufanaru C, et al. Chapter 7: Systematic reviews of etiology and risk. In: Joanna Briggs Institute Reviewer’s Manual. Adelaide, Australia: The Joanna Briggs Institute; 2007. [Google Scholar]
- 61.Saleem S. Modified Kuppuswamy Scale updated for year 2018. Paripex – Indian Journal of Research. 2018;7(3):435–436. [Google Scholar]
- 62.Hedges LV. Distribution theory for Glass’s estimates of effect size and related estimates. J Educ Stat. 1981;6(2):107–128. [Google Scholar]
- 63.Hedges L, Olkin I. Statistical Methods for Meta-Analysis. New York, NY: Academic Press; 1985. [Google Scholar]
- 64.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Mahwah, NJ: Lawrence Erlbaum Associates, Inc; 1988. [Google Scholar]
- 65.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc B Stat Methodol. 1995;B57:289–300. [Google Scholar]
- 66.American Congress of Obstetrician Gynecologists How Your Fetus Grows During Pregnancy. https://www.acog.org/Patients/FAQs/How-Your-Fetus-Grows-During-Pregnancy?IsMobileSet=false. Accessed November 29, 2018.
- 67.Kreider RM, Simmons T. Marital Status: 2000. Washington, DC: U.S. Census Bureau; 2003. [Google Scholar]
- 68.Centers for Disease Control and Prevention (CDC) About Adult BMI. https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html. Updated August 29, 2017. Accessed November 29, 2018.
- 69.Higgins J, Thompson S, Deeks J, Altman D. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Suurmond R, van Rhee H, Hak T. Introduction, comparison and validation of meta-essentials: a free and simple tool for meta-analysis. Res Synth Methods. 2017;8(4):537–553. doi: 10.1002/jrsm.1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hedges L, Vevea J. Fixed- and random-effects models in meta-analysis. Psychol Methods. 1998;3(4):486–504. [Google Scholar]
- 73.Reichner C. Insomnia and sleep deficiency in pregnancy. Obstet Med. 2015;8(4):168–171. doi: 10.1177/1753495X15600572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Nagandla K, Nalliah S, Yin L, et al. Prevalence and associated risk factors of depression, anxiety and stress in pregnancy. Int J Reprod Contracept Obstet Gynecol. 2017;5(7):2380–2388. [Google Scholar]
- 75.Polo-Kantola P, Aukia L, Karlsson H, Karlsson L, Paavonen EJ. Sleep quality during pregnancy: associations with depressive and anxiety symptoms. Acta Obstet Gynecol Scand. 2017;96(2):198–206. doi: 10.1111/aogs.13056. [DOI] [PubMed] [Google Scholar]
- 76.Hall W, Stoll K, Hutton E, Brown H. A prospective study of effects of psychological factors and sleep on obstetric interventions, mode of birth, and neonatal outcomes among low-risk British Columbian women. BMC Pregnancy Childbirth. 2012;12(1):78. doi: 10.1186/1471-2393-12-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kumpulainen S, Girchenko P, Lahti-Pulkkinen M, et al. Maternal early pregnancy obesity and depressive symptoms during and after pregnancy. Psychol Med. 2018;48(14):2353–2363. doi: 10.1017/S0033291717003889. [DOI] [PubMed] [Google Scholar]
- 78.Lockhart E, Abdallah A, Tuuli M, Leighton B. Obstructive sleep apnea in pregnancy. Obstet Gynecol. 2015;126(1):93–102. doi: 10.1097/AOG.0000000000000848. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.