Abstract
The coronavirus disease (covid19) pandemic (caused by the SARS-CoV-2 virus) is the greatest healthcare challenge in a generation. Clinicians are modifying the way they approach day-to-day procedures. Safety and reduction of transmission risk is paramount. Surgical tracheostomies in covid19 patients are aerosol generating procedures linked with a significant risk of viral contamination. Here, we describe our local approach for these procedures, introducing the “5Ts” of safe tracheostomy practice: Theatre set-up, Team Briefing, Transfer of patient, Tracheostomy Procedure, Team Doffing and De-brief. We identify the critical steps of the procedure and explain how we overcome the risks associated with breaking the transfer circuit to attach the patient to the theatre ventilator. We explain our technique to reduce secretion spillage when opening the trachea. We emphasise the importance of closed tracheal suctioning and mouth suctioning prior to patient transfer. We highlight the importance of maintaining a closed circuit throughout the procedure and describe tips on how to achieve this. We summarise the steps of our protocol in an “easy to reproduce” way. Finally, we emphasise the importance of communication in a constantly changing environment and challenging circumstances.
Keywords: covid19, tracheostomy, ARDS, airway, coronavirus, SARS
Introduction
The coronavirus disease (covid19) pandemic (caused by the SARS-CoV-2 virus) is changing the way health care professionals approach common procedures. Some of these need critical modifications to facilitate safety and minimise the risk of viral spread. There is great controversy around the role of surgical tracheostomy as part of the weaning process during the recovery from covid19.1 The advantages and disadvantages surrounding which patients will benefit from tracheostomies have been described elsewhere.1 Our decision-making on our patients’ cohort is facilitated with detailed discussions with the Critical Care team.
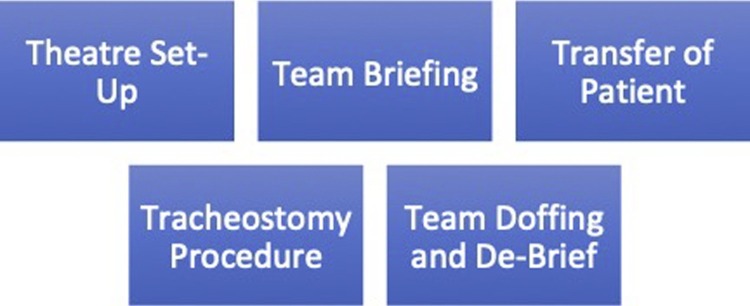
Surgical (open) tracheostomy is an aerosol generating procedure (AGP) and carries a very high risk of contamination by exposing the airway secretions to the clinical staff involved.1 The overall procedure needs to be thoroughly and appropriately planned and carefully executed in order to ensure staff and patient safety. For this reason we have framed the procedure into 5 main domains. We have coined them the ‘5Ts’ (Fig. 1 ), introducing nomenclature that can be universally applied:
-
1
Theatre Set-up
-
2
Team Briefing
-
3
Transfer of Patient
-
4
Tracheostomy Procedure
-
5
Team Doffing and De-Brief
Fig. 1.
The “5Ts” for a safe covid19 tracheostomy.
The literature around tracheostomies in covid19 patients is minimal.1, 2 We feel there are important modifications in the tracheostomy procedure that can (and should) be applied to minimise the risk of viral transmission.2 We term these ‘critical steps’. In this essay, we share our experience from our regional infectious diseases (and now covid19) centre.
Theatre set-up
All covid19 patients are operated on in a dedicated “Covid Theatre”. This theatre operates under negative pressure. Reverse laminar flow in the perimeter around the operating table is estimated to exchange 90% of air (removing the generated aerosol) in 6 minutes. The anaesthetic room allows for a circulating nurse (“runner”) to remain for the attainment of any essentials throughout the procedure. This team member holds a two-way radio and remains in communication with the theatre personnel throughout the procedure. However, if the procedure has been planned appropriately, there should not be any need for any further equipment to be handed in to the theatre during the procedure.
The surgical team’s protective equipment (PPE) is displayed in the photograph (Fig. 2 ) and is essential. The minimum PPE for an open tracheostomy should comprise a FFP3 face mask with confirmed seal, surgical hood, goggles or visor and double gloves. This is in accordance with WHO and PHE guidance.
Fig. 2.
PPE for a covid19 surgical tracheostomy.
We have found that the PPE can often make it difficult to identify members of the various teams. We have therefore colour-coded the anaesthetist’s visor (black) to allow easy identification. The team members write their names on the coronal end of the visor; allowing for safe and easy intraoperative communication.
Given the challenges and the complexity of surgical tracheostomies on covid19 patients, we aim to have weekly dedicated days and slots for these patients.
Team Briefing
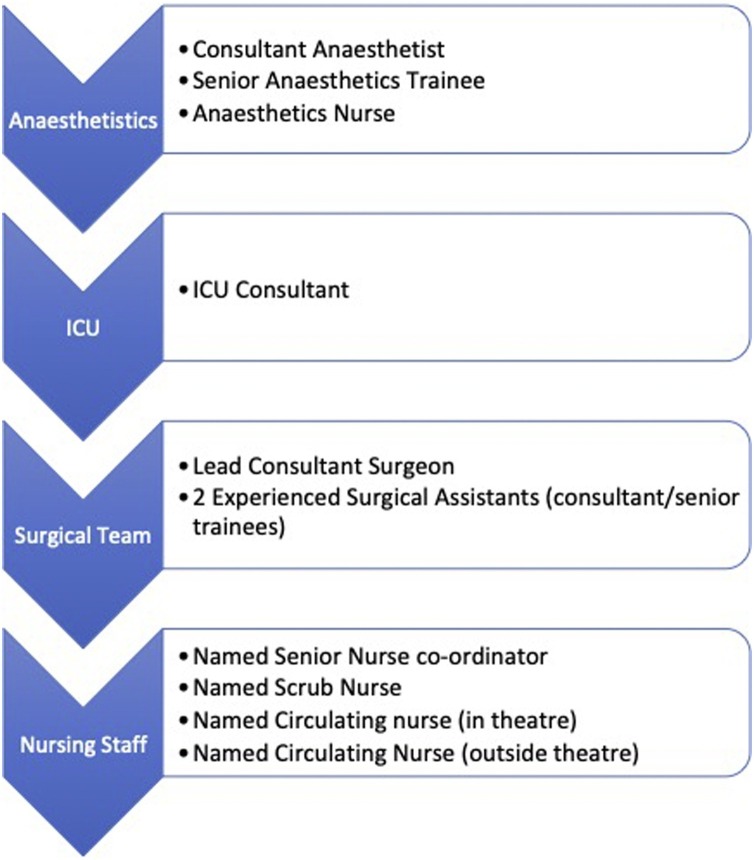
The team briefing occurs outside the “Covid Theatre”. The key personnel that needs to be present is shown in Fig. 3 , and includes critical care, anaesthetics, surgeons, and nursing teams.
Fig. 3.
The team members for a surgical tracheostomy.
We utilise a specific checklist that applies to all covid19 positive patients. Following introductions a check is undertaken to confirm that all staff are appropriately mask-fit tested and trained in “Donning and Doffing”. These elements are vital; if the appropriate training has not occurred then these members of the team are excluded and replaced for this procedure.
The team members specify what their role will be during the procedure (such as scrub nurse, lead anaesthetist). Communication is maintained with personnel outside theatre by a two-way radio. This device needs to be checked prior to the patient being sent for, and covered in a single-use membrane that will keep the equipment clean.
The anaesthetic machine, operating table and operating lights are all checked in advance to establish that they are functioning correctly. The location of emergency equipment is also identified.
At this point, similar to the pre-covid19 era, we discuss the patient's case in detail focusing on the anaesthetics/ICU and surgical aspects. The surgical aspects are described in detail below. Here, we highlight some important points:
-
•
Pre-transfer requests (such as endotracheal suctioning)
-
•
Patient positioning
-
•
Critical exposure points of the transfer and procedure
-
•
Equipment required
-
•
Type and size of the required tracheostomy tube. We aim for the largest size possible. A second tube should be available in case of malfunction, as well as one size larger and one size smaller, should they be required.
At the end of the briefing everyone’s role should be clear; this is confirmed and documented.
Transfer of the patient
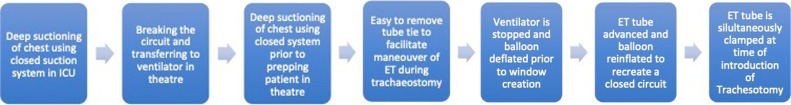
The patient’s transfer is co-ordinated by the ICU and anaesthetic team. We consider deep suctioning of the chest using the closed suctioning circuit prior to transfer to be a critical procedural step. We also request the oral cavity to be suctioned prior to transfer. This minimises the amount of secretions at the time of opening the trachea. These are the first of the series of critical procedural steps that we utilise to minimise the risk of viral transmission.
The anaesthetic team then transfers the patient using appropriate PPE (Fig. 2). The transfer time is between 20-30 minutes, mainly due to the fact that our theatres are connected to ICU via a public corridor. Security staff has to close the corridor temporarily during transfers, and the anaesthetic team needs to put on PPE prior to entering ICU.
During the transfer downtime, the surgical and nursing staff begin to ‘donn’ the PPE and enter the theatre to prepare the surgical trays and check the tracheostomy tube (Figs, 4 and 5).
The patient is transferred along the back corridor of the theatres and not through the main theatre entrance. We appreciate that not all theatres have a back corridor; but should it be present it is important to utilise it to minimise exposure.
On arrival to theatre the patient is transferred to the operating table by the anaesthetic staff and the circulating nurse. The surgeon is able to oversee the positioning of the patient at this stage. Once the anaesthetic staff are satisfied with the transfer and the positioning, the standard WHO time-out takes place.
The next critical procedural step occurs when the patient is disconnected from the transferring ventilator and connected to the anaesthetic machine. The anaesthetist announces this loudly when it is about to happen. This is crucial as it is a point of increased viral exposure. The anaesthetic viral filter should remain on the endotracheal tube; if one is not present we recommend transient clamping. For the reasons above, we advocate that all the team members who are in theatre should be in full PPE when the patient arrives in theatre. This is different to covid19 patients requiring intubation in theatre for other types of procedures; in those instances it is common practice for surgical staff not to enter theatre for 20 minutes after intubation to allow recirculation of air.
Following the procedure the patient is transferred back to ICU by the ICU team (Consultant Intensivist, Senior Trainee, ICU Nurse) using PPE and the same route and as described above.
Tracheostomy procedure
Our tracheostomy team has a lead consultant surgeon and two experienced assistants (another consultant or senior trainees). We feel it is inappropriate to have junior trainees (Foundation doctors, Dental Core Trainees) without previous tracheostomy exposure to assist in these cases.
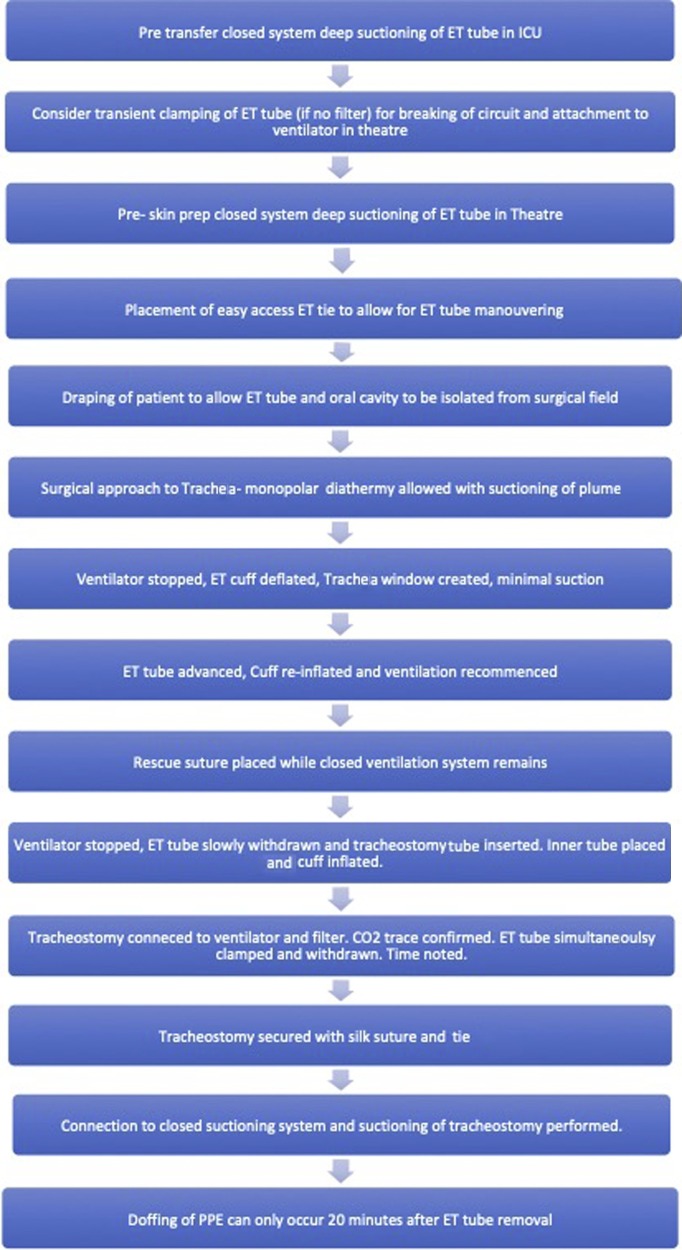
The patient should be fully paralysed for the duration of the procedure and the closed suctioning system is still attached to the endotracheal tube prior to the start of the procedure. Prior to prepping the patient, we ask the anaesthetist to suction the ET tube again, including suction of the subglottic port, and to confirm adequate muscle relaxation. We consider this a critical step. ICU patients have padded ET tube ties to secure the tube for long periods whilst preventing pressure sores. These can be cumbersome, therefore the anaesthetist removes them prior to the procedure and places an easy to release ET tube tie. Prep and drape is standard; however we ensure that the ET tube and oral cavity is draped over and is only accessible to the anaesthetist to allow for manoeuvring during the tracheostomy. We consider this another critical step (Fig. 4).
Fig. 4.
Critical steps for a covid19 surgical tracheostomy.
We have no objection to using monopolar and bipolar diathermy through the procedure. It has been suggested that they are considered AGP; however the evidence is rather weak and can be prevented with appropriate vacuum extractor suction that removes all the generated plume.1, 2 Appropriate haemostasis is crucial, as coagulation anomalies are not uncommon in covid19 patients.
Dissection down to the second tracheal cartilage ring is standard and as previously described.3 When the trachea is reached, we request the anaesthetic team to position themselves at the head end.
We feel that a crucial step is to keep a closed circuit until the tracheostomy tube is inserted in the trachea. For this reason the balloon/cuff needs to be kept intact. Prior to making the tracheal window, we request the anaesthetist to stop the ventilator and deflate the balloon/cuff. Afterwards, the surgeon makes the window in the trachea. Minimal suctioning is used. Once the window is achieved the ET tube is advanced further (past the window) and the balloon/cuff is re-inflated (over-inflated), 3 thus establishing a closed circuit. This is a critical step. It is important to recognise that the patient is at significant risk of alveolar derecruitment and may require aggressive recruitment after re-inflation of the cuff. We found that this was best achieved with two anaesthetists; one to manipulate the ET tube and one to manage the ventilator.
At this stage the patient is ventilated and the tracheal window lies above the level of the ET cuff allowing ample time for the surgeon to check haemostasis and insert a rescue-suture. We place a round-bodied 0 Prolene on the inferior aspect of the window which is brought through the skin. This allows the trachea to be brought close to the skin if the tracheostomy tube becomes dislodged.3
The ventilator is then stopped again, the cuff is deflated and the ET tube is withdrawn slowly to allow the insertion of the tracheostomy and inner tube. The tracheostomy cuff is inflated and the circuit is connected. The capnography CO2 trace is confirmed. We do not scope the tracheostomy, unless there is an absolute need. The ET tube is simultaneously clamped while the tracheostomy is being placed. This is a critical step. It is important to remember that the patient has technically been extubated and for this reason 20 minutes needs to pass to allow re-circulation before doffing. The anaesthetic nurse documents this time. The tracheostomy tube is secured with sutures. A closed suctioning is attached to the tracheostomy tube and suctioning can then be performed.
Team “doffing” and de-brief
The appropriate time to doff our PPE is a minimum of 20 minutes after removal of the ET tube. This is done in the theatre's designated area and following the current standard practice guidlines. After this 20 minute hiatus the patient can be transferred back to ICU. The ICU team transfers the patient back to ICU using the same route and procedures described above.
De-brief on these cases is crucial in order to pollinate any future practice. As a surgical team we are liaising very closely with our anaesthetic/ICU and nursing colleagues to make sure we approach these cases as safely as possible.
Conclusion
As health care professionals and indeed as human beings, we have all been challenged by the recent covid19 pandemic. This has reinforced the need for us to be adaptable and reflective practitioners. The need for surgical tracheostomies will increase over the next weeks and months; for this reason we have to approach them in a robust, repeatable and safe manner. Our experience has allowed us to identify some critical steps that we have introduced to make this procedure safer for all involved (Fig. 5 ). We have also framed the process in 5 distinct domains. It has to be recognised that these procedures are time consuming given all the steps involved and good communication can minimise unnecessary time stoppages and improve human factors. We have also recognised that due to staff self-isolating, regular head and neck scrub staff may not be available. This can also add challenges and reinforces the need for good communication and reproducible steps. We believe that our approach is safe and easily reproducible and we welcome comments towards improvement.
Fig. 5.
The North Manchester General Hospital covid19 surgical tracheostomy algorithm.
Ethics statement/confirmation of patients' permission
Not applicable.
Conflict of interest
We have no conflicts of interest.
References
- 1.Zhejiang University School of Medicine: Handbook of COVID-19 Prevention and Treatment, 18/03/2020.
- 2.Tay J.K., Chung Khoo M.L., Loh, W.S. Surgical Considerations for tracheostomy during the COVID-19 Pandemic. Lessons learned from the severe acute respiratory syndrome outbreak. JAMA Otolaryngol Head Neck Surg. Published online 31/03/2020. 10.1001/jamaoto.2020.0764. [DOI] [PubMed]
- 3.Ormandy D., Kapoor V., Kyzas P.A., Vassiliou L.V. Tracheostomy suspension: a modified approach for securing the airway. BJOMS. 2020 doi: 10.1016/j.bjoms.2020.04.013. In press. [DOI] [PubMed] [Google Scholar]