Highlights
-
•
Paper explores barriers to a universal DNP requirement for advanced practice nurses
-
•
Includes cost analysis and perceptions of the DNP in today's professional environment
-
•
Offers insight to help facilitate the implementation of a universal DNP standard
Keywords: Doctor of nursing practice; Universal DNP; Nursing doctorate; Nursing education; Nursing doctoral education,; Advanced practice nursing; Advanced practice nursing preparation
Abstract
Background
In 2004, the American Association of Colleges of Nursing (AACN) called for all nursing schools to phase out master's-level preparation for advanced practice registered nurses (APRNs) and transition to doctor of nursing practice (DNP) preparation only by 2015. Today, five years after the AACN's deadline, nursing has not yet adopted a universal DNP standard for APRN practice entry.
Purpose
The purpose of this paper is to examine the factors influencing the ability of nursing schools to implement a universal DNP standard for APRNs.
Methods
Deans from top-ranked nursing schools explore the current state of the DNP degree in the US. The authors draw upon their collective experience as national leaders in academic nursing, long-time influencers on this debate, and heads of DNP programs themselves. This insight is combined with a synthesis of the literature and analysis of previously unpublished data from the AACN on trends in nursing doctoral education.
Findings
This paper highlights issues such as the long history of inconsistency (in messaging, curricula, etc.) surrounding the DNP, certification and accreditation challenges, cost barriers, and more. The authors apply COVID-19 as a case study to help place DNP graduates within a real-world context for health system stakeholders whose buy-in is essential for the success of this professional transition.
Discussion
This paper describes the DNP's standing in today's professional environment and advances the conversation on key barriers to its adoption. Insights are shared regarding critical next steps to ensure national acceptance of the DNP as nursing's terminal practice degree.
In 2004, the American Association of Colleges of Nursing (AACN) endorsed a position statement on the doctor of nursing practice (DNP) degree. This statement named the DNP as the most appropriate entry-to-practice degree for advanced-practice registered nurses (APRNs) in the United States (US) (AACN, 2004). The AACN also set an ambitious goal for all programs preparing APRNs at the master's level to migrate to DNP preparation by 2015. Almost two decades later, and despite the AACN's vision statement, the Master of Science in Nursing (MSN) remains the predominant exit degree for APRNs. While DNP program growth has been dramatic in the last decade, with the number of US DNP programs increasing nearly fourfold, there has been only a modest reduction in MSN programs. Many schools continue to offer the MSN exclusively, and those that have developed a BSN–DNP typically retain the MSN option (Auerbach et al., 2015; Mundinger & Carter, 2019).
In a 2011 publication, several prominent academic nursing leaders predicted that the transition to a DNP standard would not occur by 2015 (Cronenwett et al., 2011). Written in the context of the Great Recession, during which severe economic challenges impacted all sectors, including higher education, Cronenwett et al., (2011) highlighted the simultaneous spike in APRN staffing needs due to rising chronic disease rates and the decline in resources, faculty, and clinical partnerships necessary for DNP preparation. The authors also discussed the potential impacts of increasing the length and costs of APRN preparation at a time when the national need for advanced practice providers was rapidly increasing. Did the factors described by Cronenwett et al., (2011) remain in play during times of more robust economic growth; and will they continue in the face of severe economic strains? Or have other factors delayed the transition from MSN to DNP education in recent years? The purpose of this paper is to describe the forces influencing nursing graduate education and to identify factors that have interfered with implementation of a universal practice doctorate.
After describing nursing's history of inconsistency surrounding the DNP, we delve into an often-overlooked barrier to DNP adoption: the fact that nursing has delayed differentiating MSN- vs. DNP-prepared APRNs, in part, due to the large number of nurses who have built off of their master's degree with an online, nonclinical DNP. Next, we address the fact that credentialing and accreditation groups have not expressly endorsed a universal practice doctorate. We describe the extent to which health care industry stakeholders, such as practice partners and employers, remain key influencers on schools’ implementation of the DNP and the importance of gaining buy-in from these constituents. Last, the ongoing debate over the need for DNP residency programs is reviewed, and financial challenges—arguably the greatest barrier to DNP acceptance—are discussed. Written in cooperation by nursing deans across the United States, this paper represents the type of open dialogue that we believe is essential for nationwide change in nursing doctoral education.
A History of Inconsistency
The DNP degree was created to prepare APRNs (i.e., clinical nurse specialists, nurse practitioners [NPs], nurse midwives, and nurse anesthetists) for leadership in clinical practice. The creation of the DNP coincided with the Institute of Medicine's (IOM's)1 reports on medical errors (1999) and quality and safety (Institute of Medicine, 2001). Based on these landmark reports, in 2003, the IOM called for health system transformation through interprofessional, evidence-based care, including expert clinical leadership by nurses. Given the growing complexity of care, and strong recommendations by the IOM, it was held that health care would benefit from doctorate-educated practitioners. Around this same time, other disciplines, such as pharmacy and physical therapy, echoed this belief and moved their disciplines to a practice doctorate exit.
In 2004, members of the AACN endorsed its Position Statement on the Practice Doctorate, which called for nursing schools to transition from a master's to a DNP standard for APRN preparation by 2015 (AACN, 2004). To promote this initiative, in 2006, the AACN published their recommendations in both The Essentials of Doctoral Education for Advanced Nursing Practice and the DNP Roadmap Task Force Report (AACN, 2006). Yet, when the IOM released itsFuture of Nursing Report in 2010, it did not explicitly address the need for a practice doctorate as a universal requirement for advanced practice nursing entry. This omission was an early indication of the challenges the profession would face surrounding adoption of the DNP (IOM, 2011).
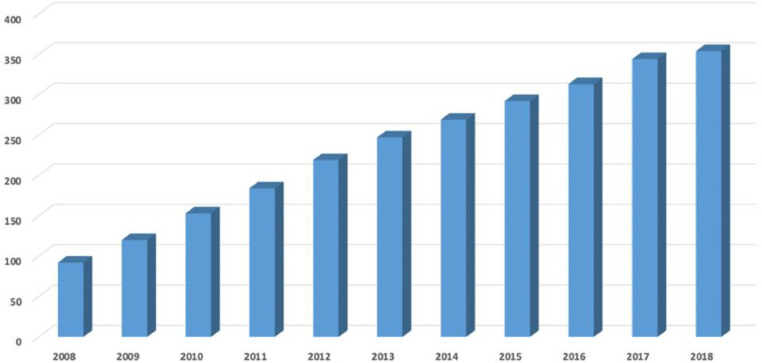
Despite inconsistent messaging among health care leadership, the number of DNP programs and graduates grew steadily over the next decade (AACN, 2019b). Specifically, the national DNP program count rose from 92 in 2008 to 354 in 2018 (AACN, 2019)—but what was happening within schools of nursing tells a different story.
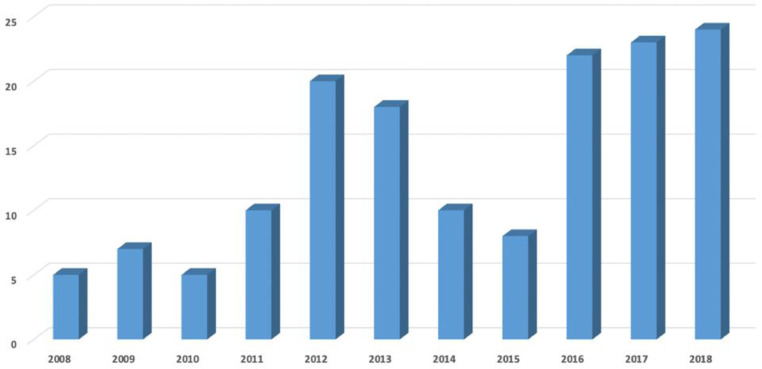
What one cannot discern from graphs depicting DNP program growth, such as Figure 1 , was that a large number of schools retained their MSN option while instituting a nonclinical version of the DNP. Many nursing schools kept up robust MSN enrollment and only added the post-MSN-DNP, which did not require extensive investment in clinical sites and could be delivered to large numbers of students online. This “add-on” approach neglected the practice component of the DNP, sidestepping one of its central purposes as a practice doctorate. Many of the post-master's DNP programs were designed for working nurse executives and practicing APRNs; these programs often did not include clinical hours at all, but rather allocated hours to the capstone or final project. The 500 additional project hours were often used to develop leadership initiatives and were not primarily designed to increase APRN clinical proficiency. In fact, some post-master's DNP programs admitted students holding MSN degrees outside of advanced practice nursing altogether. Meanwhile, the number of APRN students opting for master's-level practice entry continued to rise from 10,737 in 2004 to 46,622 in 2018 (AACN, 2019d). Figure 2 shows that only 152 master's programs closed between 2008 and 2018 (AACN, 2019).
Figure 1.
DNP programs established from 2008 to 2018.2
Figure 2.
Nursing master's program closures, 2008 to 2018.2
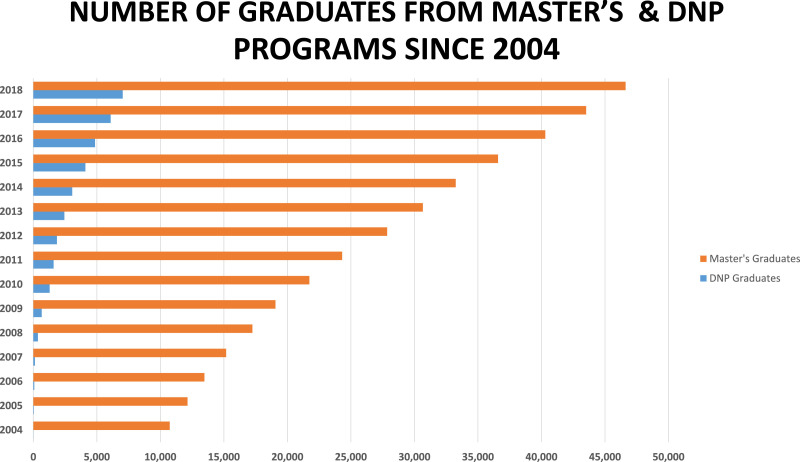
That brings us to the present day—15 years after the AACN Position Statement on the Practice Doctorate—when the American Association of Nurse Practitioners reports 79.8% of APRNs hold a master's as their highest degree and just 14% hold a DNP (AANP, 2019). Figure 3 shows a stark picture of the current state of APRN education in the United States, and how nursing has failed to move toward the vision of all APRNs holding doctorates. It is imperative that we examine the root causes of why major change has not occurred, remove roadblocks, and propose new approaches that will make this professional need a reality.
Figure 3.
DNP vs. master's graduates, 2004 to 2018.3
The Evolution of DNP Graduates
So, why did the growth of DNP programs across the United States fail to significantly impact the educational level of clinical APRNs? The original intent for DNP curricula was to prepare a workforce of leaders in advanced clinical practice; however, the decade of fast growth in post-master's DNP programs produced a majority of first-wave graduates opting for positions in administrative and educational settings instead (AACN, 2004; AACN, 2012; Grey, 2013). Out of the 7,039 DNP graduates in 2018, 4,232 (60%) entered full-time positions in schools of nursing, rather than bedside or clinical positions (AACN, 2019c). With almost five DNP graduates per year for every nursing PhD graduate, the DNP offered a quick way for schools to increase their proportion of doctorate-prepared faculty. While this wave of DNP graduates has helped to ease the perennial shortage of nursing faculty, to an extent, it has not counted toward the number of doctorate-prepared APRNs needed to address the national primary care shortage.
Yet, as a profession, it appears we have entered a transition period. In recent years, the proportion of DNP students enrolling in post-master's DNP programs seems to be declining. In 2015, enrollments in post-BSN programs exceeded post-MSN enrollments for the first time, and post-BSN DNP program enrollment increased nearly 18-fold from 1,060 students in 2009 to 18,240 in 2018 (AACN, 2019). If enrollment trends correspond to graduation trends, we can predict that the largest number of DNP graduates soon will come from post-BSN cohorts. This progress contrasts starkly with where we were a decade ago, when there were 30 post-MSN-DNP graduates for every post-BSN DNP graduate. This trend suggests that the profession might finally be gaining the buy-in it needs—at least from students—to implement the DNP standard as it was intended. Nursing leaders should apply this momentum toward enacting long-awaited professional changes, such as updated accreditation and certification standards, while also accounting for the real-world challenges that accompany DNP implementation.
One such challenge is the fact that faculty in DNP programs are grappling with how to concurrently educate experienced nurses holding master's degrees and post-baccalaureate students who may have little-to-no clinical background. The largest concentration of post-BSN-DNP students is found in nurse practitioner tracks (AACN, 2019a). However, the number of online post-baccalaureate DNP programs that focus on health system leadership and offer no advanced practice skills has risen, and post-MSN students are still opting for leadership tracks primarily. If one scans the types of nurses enrolling in DNP programs today, they represent a wide range of academic backgrounds and experience levels, including:
-
•
Nurses with years of experience as master's-prepared clinicians and/or administrators enrolling primarily in online post-MSN-DNP programs to focus on executive leadership and/or education;
-
•
Nurses holding BSNs who have health care experience and are enrolling in DNP programs to become system leaders, many of which are online;
-
•
BSNs who have health care experience and are enrolling in DNP programs to become APRNs;
-
•
Second-degree entry-to-practice graduates (BSN or MN) enrolling in DNP programs immediately after graduation in order to become APRNs, having never practiced as a generalist nurse.
This hodgepodge of DNP students presents distinct challenges for faculty trying to implement consistent DNP curricula while meeting the needs of a student body with vast differences in clinical proficiency. Upon graduation, these DNP-prepared individuals enter the workforce alongside large, clinically focused, and “consistently packaged” cohorts of MSN graduates. If we continue to prepare APRNs at the master's level, and remain inconsistent about the types of students admitted into DNP programs, how will we ever fulfill the intent of the AACN's 2004 position statement? How will health systems and the public gain a common understanding of the competencies of a DNP-prepared nurse?
Certification and Accreditation
Over the past 15 years, individual nursing schools have developed the educational approach that best fits their respective institutional strategies and capacities with little external forces influencing program design or characteristics. Neither of the two largest accreditation organizations for nursing education has weighed in on this issue. As long as certification boards continue to allow graduates with either an MSN or a DNP to sit for the same certification exam, schools will not rush to end their MSN programs. This situation is similar to the decades-old challenge of stating that the BSN should be the practice-entry degree for nursing, while retaining one licensing exam for both associate- and BSN-prepared graduates. If our licensing and credentialing bodies continue to treat the two degrees as comparable, MSN programs will remain in place, just as associate programs have persisted.
Accreditation bodies are well positioned to influence educational requirements for APRNs. This is evidenced by the fact that the Council on Accreditation of Nurse Anesthesia Education Programs (COA) moved forward with a requirement for all schools preparing CRNAs to award doctoral degrees for practice entry by 2025. This has resulted in rapid change among CRNA programs and has positioned nurse anesthesia program leaders as subject matter experts on the needs of BSN–DNP students. Although, there is little evidence yet available from the COA about how implementing the DNP requirement has impacted processes and outcomes among CRNAs.
Other accreditation/certification bodies could develop similar policy statements to move this workforce change forward; but there does not appear to be momentum in that direction. In fact, the American Council of Nurse Midwives (ACNM) has advocated against a required practice doctorate for CNMs (ACNM, 2012). Some leaders in midwifery have argued that a universal DNP requirement would make midwifery education less accessible, more cost prohibitive, and less diverse. This stance has been taken without substantive evidence that the MSN prepared workforce is more diverse than the DNP workforce. Thus far, no other APRN specialty accreditation body has advanced a position statement to transition MSN preparation to the DNP level. Without a uniform accreditation standard, nursing schools will have little incentive to phase out MSN education for advanced practice roles.
The Case for Practice Differentiation
Are there data that certification and accreditation bodies could use to guide these decisions? Do data exist to suggest DNP graduates are more clinically proficient than master's-prepared APRNs? Unfortunately, to date, the data are sparse. Many studies that do exist on the subject are descriptive, based on self-report, utilize small convenience samples, and/or do not address patient outcomes. Importantly, many studies do not differentiate outcomes between MSN- and DNP-prepared APRNs; they also tend not to distinguish between graduates of BSN–DNP programs and those who have received a post-master's DNP.
Several studies do indicate that DNP graduates are practicing in an array of settings and serving complex patients (Carter & Jones, 2017). Yet, in one 2019 study, 59% of DNP-prepared survey respondents from key professional nursing organizations (e.g., the American Academy of Nurse Practitioners, the American Organization of Nurse Executives, and the American Association of Nurse Anesthetist) reported that the DNP was neither required, nor preferred by their current employers. There was some agreement on the question of whether every APRN should hold a DNP: When asked to rate the need for a universal requirement on a scale of 1 to 10, 48% of respondents ranked necessity at an 8 or higher, with a mean rating of 6.7 (Minnick, Kleinpell, & Allison, 2019).
However, in a qualitative study of DNP employers (n = 23), respondents reportedly perceived similar functions between DNP- and master's-prepared APRNs (Beeber, Palmer, Waldrop, Lynn, & Jones, 2019). Employers were unable to differentiate between preparations due to several factors: a lack of DNP-specific positions in their organizations, limited employment of DNP-prepared nurses, and/or the fact that DNPs were too new to organizations to be accurately evaluated. Employers did, however, report that DNPs exhibited a better understanding of evidence-based clinical guidelines, a greater focus on translation of evidence into practice, and stronger knowledge of health policy, compared to master's-level APRNs (Beeber et al., 2019). This underscores the need for nursing leaders to gain consensus on what makes the DNP different, to methodically disseminate that information to health system stakeholders, and to adjust their evaluation criteria accordingly.
Gaining Health System Buy-In: Placing DNPs in Context
With care continuously increasing in complexity, and demands on nursing leaders growing exponentially, DNP-educated APRNs are demonstrating in real-time that their program of study provides the ideal breadth and depth of preparation for today's workplace realities. Their unique combination of clinical expertise and change management skills makes DNPs invaluable to employers facing a constant onslaught of industry disrupting factors (e.g., the Data Revolution, ‘omics, precision health, etc.) (Shelby & Wermers, 2020; Sherrod & Goda, 2016). But it is not enough for individual DNPs to prove their value, time and again, through singular acts of leadership and clinical aptitude. Nursing deans and nurse health care executives must call for data to tangibly demonstrate distinguishing features of DNP-educated APRNs, compared to other provider preparations, and then highlight those metrics for health system stakeholders.
Stakeholders, such as clinical partners and prospective employers, must believe that DNPs are invaluable resources in addressing the health system's most pressing issues. This list of issues is growing because systems are quickly evolving along multiple axes—from the reconceptualization of practice scope due to advancements in telehealth and data analytics, to sweeping population changes from climate change, mass migration, and novel pathogens (such as SARS-CoV-2), which are testing systems like never before. As this paper nears publication, COVID-19 is ravaging populations and threatening health systems globally, with repercussions that are not yet fully understood. In these unprecedented times, health systems need nurse problem solvers—especially those who are clinically expert and ready to lead from the frontlines.
Applying the COVID-19 crisis as a case study, it becomes clear how DNP-educated nurses are poised to interface with and direct the efforts of multiple constituents, all within the scope of one dynamic role. This ability to simultaneously lead within multiple professional spheres, and across macro/micro levels, is one of the key features of DNP–APRNs. For instance:
-
•
Their health policy and leadership foundation means DNPs may counsel metro, state, and national leaders in strategic mechanisms for virus containment.
-
•
DNP graduates have completed coursework involving assessments of the most up-to-date technologies available to providers. That means they will be ready to apply emerging technologies, in clever ways, to solve new problems. For instance, DNP-educated APRNs, with their focus on population health, would be well suited to coordinate central response command centers for mass telehealth screenings.
-
•
This population health perspective also lends itself to the collection, analysis, and reporting of epidemiological data using novel methods. For example, the self-screening app TechTank COVID-19 PRO was recently co-created by a DNP-prepared nurse. This smartphone app allows patients to self-screen for COVID-19 and enables providers to view real-time positive screening counts by zip code. Providers may then utilize in-app resources to develop locally tailored containment and mitigation strategies (Bussenius et al., 2020).
-
•
Specialized DNPs, such as gerontological APRNs, can help systems tailor protocols to triage and treat patients across the lifespan; they may also evaluate system migrations to telehealth while considering specialized population needs. This is especially important given that people over 65 are at higher risk for complications and morbidity related to COVID-19, compared to certain other demographics.
During the COVID-19 health care response, MSN- and DNP-prepared advanced practice nurses are both demonstrating their incredible value in shoring up our health care response and meeting the needs of individual patients and care teams. As this national emergency progresses, it will be important to document and differentiate the roles of DNP-prepared nurses who are health system leaders or innovators in technology and population health strategies. Data and documentation from the response may be applied to better understand the differences in roles and responsibilities of MSN- vs. DNP-prepared APRNs.
Ensuring Readiness for Practice
Challenges surrounding transition-to-practice for BSN–DNP graduates have interfered with a universal DNP requirement (Cappiello, Simmonds, & Bmrick, 2010). Program leaders have proposed implementing DNP residencies and/or fellowships as one solution; but this is not currently the standard, and programs vary widely in terms of offering residencies vs. intense specialized practice experiences (Mundinger, Starck, Hathaway, Shaver, & Fugate-Woods, 2009). Furthermore, debate exists as to whether residencies and/or fellowships should occur before or after degree conferral (Harper, McGuinnes, & Johnson, 2017). The timing of a residency is critical because if it precedes degree conferral, the cost is typically borne by students, but if it follows graduation, the employer usually assumes financial responsibility.
The argument of whether a residency or fellowship is needed is firmly entrenched in the need to document readiness to practice. While the debate surrounding APRN residencies applies to both master's- and doctoral-prepared APRNs, it is noteworthy that this was not a widespread conversation when the majority of DNP graduates were from post-MSN programs (Sciacca & Neville, 2016). If BSN–DNP clinical hours were increased to exceed those required of MSN-prepared APRNs,4 it would likely boost readiness for practice among these cohorts and further differentiate MSN- and DNP-prepared graduates. Schools could meet an increased clinical hours requirement for DNP students by allowing up to half of the hours to be inclusive of simulation experiences, thereby eliminating the burden on preceptors in the community.
Mundinger and Carter (2019) call attention to the issue of practice readiness, citing many schools’ lack of advanced practice content and inadequate clinical resources as reasons for nursing's slow transition to the DNP. One descriptive study addressing transition-to-practice indicated that, despite their rigorous education, APRNs felt unprepared for certain challenges of primary care. Respondents highlighted knowledge gaps such as difficulties managing complex patients, confusion over billing, and role uncertainty surrounding some procedures (MacKay, Glynn, McVey, & Rissmiller, 2018). However, the authors made no distinction between MSN and DNP graduates, suggesting these challenges may affect those with both types of preparation. Studies are needed to compare competencies of MSN- and DNP-prepared APRNs at graduation and 1 year later; researchers must not combine these groups in any competency assessment.
Cost Implications of Transitioning to Doctoral Preparation
Unless concerted action is taken to address current financial realities, it is unlikely that the profession will be successful in transitioning to doctoral practice entry. The financial implication of requiring the DNP degree is arguably the largest barrier to adoption, both for students and organizations. A universal DNP requirement would have financial ramifications on three levels: (1) cost to individual students, (2) cost to institutions that financially support advanced nursing practice education, and (3) cost to schools. Surmounting these challenges is not impossible, but they must be fully acknowledged and understood if change is to occur.
Cost to Students
Program costs vary considerably among schools based on a variety of factors: institution type (public vs. private), the school's research intensiveness, its enrollment statistics, and geographical location (Broome, Bowersox, & Relf, 2018). Additionally, NP programs at both the master's and DNP levels vary in the number of credit hours they require (Table 1 ). Many students contemplating graduate study already have taken on significant loan debt for their undergraduate degree, with the average undergraduate debt load totaling more than $30,000 (The Institute for College Access & Success, 2016). Seventy-one percent of master's students and 74% of DNP students then take out additional loans to support graduate school costs (AACN, 2017). If students work in health care for 2 to 3 years, they may be able to offset some of that debt, especially if their employer provides loan repayment. However, many health systems have phased out support programs like loan repayment and graduate tuition remission as profit margins have shrunk (AACN, 2017). The financial burden on hospitals caused by the COVID-19 crisis could impact tuition assistance programs even further.
Table 1.
MSN vs. BSN-DNP Nurse Practitioner Preparation
| Program | Full-Time Commitment in Years | Credit Hour Requirements | Clinical Hour Requirements | Approximate Total Program Costs |
| MSN | 2–3 | 40–56 | 500–750 | Range: $35,000–65,000+* |
| BSN-DNP | 4–5 | 65–95 | 1,000 | Range: $52,000–110,000+† |
Source: Graduatenursingedu.org, 2019.
Source: Broome, M.
Source: www.graduatenursingedu.org.(Graduatenursingedu.org 2019)Source: Broome, M.
In many cases, tuition is assumed fully by students, making debt load a crucial factor when they consider where and when to return to graduate school. Unless the DNP becomes associated with increased salary/reimbursement upon graduation, degree cost is likely to remain prohibitive for many nurses. For example, one 2019 study revealed the average 2014 salary for DNP-educated certified nurse midwives (CNMs) to be $105,968; the average salary for master's-prepared CNMs was $102,576 in 2014. (Data were sourced from active ACNM members via email survey.) This annual differential of $3,392 in mean salary dollars pales in comparison to the differences in time, effort, and tuition dollars required of DNP students, compared to MSN students (Fullerton, Schuiling, & Sipe, 2019).
Cost to the Health System
Historically, employer tuition reimbursement has been a major incentive for practicing RNs to return to school. But as health system profit margins shrink, “ancillary programs,” such as tuition support programs, are likely to undergo scrutiny. Even if not eliminated completely, employers may begin to only financially support nurses who opt for certain schools or specialties. If DNP-prepared nurses become especially costly to sponsor, or if data are not available to demonstrate return on investment, employers may simply choose to back other preparations (Morton, 2019).
At the same time, demand for providers is increasing, making time-to-practice and program length important considerations for human resources personnel. These factors help to determine the availability of providers in each professional category over time. If a full-time physician's assistant (PA) program lasts 24 months, for example, and a full-time DNP program lasts 36 months, in 12 years, six PA graduates will enter the job market for every four DNP graduates. Additionally, if PA and NP competencies are similar for a specific job category, this will impact hiring decisions and policies: When both professions are considered equal, but PAs are seen as less expensive to hire and support, the calculus for managers will be simple. If the clinical hours were increased in DNP programs and graduates could demonstrate they were practice ready with no need for a health system residency or fellowship, the value proposition of the DNP–APRN could rise dramatically.
Cost to Schools
One of the major cost barriers to DNP acceptance is the traditional capstone or final project component of DNP curricula. All schools—but particularly smaller schools—may have difficulty supporting the increased number of DNP students and their projects. Many programs lack the faculty necessary to mentor students through this process altogether, which is a serious concern (Auerbach et al., 2015; Chipps et al., 2018). Furthermore, health policy and data analytics projects often require specific faculty competencies, which many schools would have to focus time and resources on developing. Is the final project the defining assignment for the practice doctorate? If so, why do doctorates in medicine, physical therapy, and pharmacy not include projects? If the capstone is hindering DNP adoption, why not change expectations for degree completion? Methods to decrease faculty workload associated with capstone projects should at least be considered as well.
Conclusion and Recommendations
Transitioning APRN education to a universal DNP standard remains a lofty goal and heavy lift for the nursing profession. In 2014, the AACN/Rand offered strategies for implementing the BSN–DNP track, naming three conditions that need to be addressed for the pathway to succeed: accreditation and certification, student demand, and market demand (Auerbach et al., 2015). Five years later, these three conditions remain largely unaddressed. Nursing professional organizations have yet to even agree upon whether APRNs should hold doctoral degrees, let alone enact national standards.
Student demand heavily influences the speed with which schools convert their MSN programs to DNP programs. While student decisions are multifaceted, financial status is a significant driver of degree choice. Instituting DNP-specific scholarships may be one approach to easing debt load; offering flexible curricula (in which students may work, gain clinical practicum experience, and learn systems leadership content) may be another solution. If the clinical hours of a DNP program were increased, prospective students might opt for the longer, clinical-focused program even if it is more expensive. As more students pursue BSN-to-DNP programs, schools need to collect data on program outcomes and graduate career trajectories, especially as they compare to MSN outcomes (e.g., certification pass rates, volume of scholarship, and costs/ROI).
Faculty should partner with health care systems to implement programmatic change based on these evaluative data. The first decade of DNP education was focused primarily on post-MSN-DNP students who often had years of clinical experience and, in many cases, moved seamlessly into clinical leadership positions. That will not be the case for the next decade of DNP graduates, many of whom may have had limited employment as a nurse prior to obtaining their doctorate. While the same can be said of persons graduating with doctoral degrees in other fields, such as pharmacy and physical therapy, the clinical hours required in those programs exceed those of DNP programs. Academic institutions should track the progress of these new hires, optimizing education through continuous data collection, feedback, and program refinement.
Last, after our profession conducts a rigorous evaluation of DNP competencies, we need to clarify messaging surrounding those competencies, and widely publicize the information. Recent media efforts, such as the acclaimed Johnson and Johnson Campaign for Nursing, have highlighted the ability of APRNs to improve access to care for vulnerable populations, but there has not been media focus on the value of DNP-prepared APRNs specifically. To fully convey the DNP/APRN value proposition, dialogue must take place between nursing educators, the public, and health systems. When the difference between MSN and DNP outcomes is made clear, change is bound to occur—ultimately, institutions are likely to favor highly qualified APRNs who may both treat patients at the bedside or clinic, and lead organizational change.
Footnotes
Editorial bias disclaimer: The editor-in-chief (Broome) is second author on this paper. Therefore, this paper was managed from submission and assignment of reviewers, through initial disposition decision (revision) and final decision by Barbara Smith, PhD, RN, FAAN, Associate Editor.
Now the National Academy of Medicine
Unpublished AACN Data, 2019.
For example, by increasing the required BSN-DNP clinical hours from 1,000 to 1,800 hours, or by dedicating the full 1,000 hours to direct-care, rather than allocating 50% to project-based learning.
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.outlook.2020.03.008.
Appendix A. Challenges and Opportunities for DNP Education
-
•
Nursing leaders need to reach a clear consensus regarding the intent of DNP education and the roles that DNP graduates should be prepared to assume in academic and practice settings.
-
•
There is a compelling need to collect employment data on the graduates of post-master's and post-BSN–DNP programs and to determine the extent to which their roles align with the intent of DNP education.
-
•
Credentialing and certification bodies need to develop methods to differentiate MSN- vs. DNP-prepared APRNS including essential components of certification exams.
-
•
Ongoing studies are needed to document both the impacts of DNP graduates on clinical practice and their contributions to scholarly output.
-
•
Leaders exploring DNP education reform should evaluate current and future health system issues that might impact APRN practice.
-
•
Salary differences between MSN- and DNP-prepared APRNs require consistent evaluation.
-
•
Outreach is needed to increase awareness among employers about DNP role preparation.
-
•
The impact of longer education programs and increased clinical hour requirements on clinical placement sites needs evaluation.
-
•
Methods to decrease the faculty workload associated with capstone projects, or a change in the capstone requirement itself, should be considered.
-
•
The clinical proficiencies of master's and DNP graduates need careful differentiation and the feasibility of increasing the number of clinical hours of a DNP education be seriously considered.
-
•
Academic–practice partnerships are needed to successfully transition BSN–DNP graduates to advanced practice.
-
•
The financial implications of requiring a lengthier preparation for advanced practice entry should be examined in terms of effects on students, schools of nursing, clinical partners, and funding sources.
-
•
Nursing needs to identify, document, and clearly communicate the unique competencies of DNP-educated APRNs, particularly graduates from BSN–DNP programs.
Appendix B. Supplementary materials
References
- AACN . American Association of Colleges of Nursing; Washington, DC: 2004. AACN position statement on the practice doctorate in nursing.https://www.aacnnursing.org/DNP/Position-Statement Retrieved from: [Google Scholar]
- AACN . American Association of Colleges of Nursing; Washington, DC: 2006. The essentials: A doctoral education for advanced nursing practice.https://www.aacnnursing.org/Portals/42/Publications/DNPEssentials.pdf Retrieved from: [Google Scholar]
- AACN. (2012). Fact sheet: The doctor of nursing practice. Retrieved from: http://www.aacn.nche.edu/media-relations/factsheets/dnp.
- AACN (2017). The numbers behind the degree: Financing graduate nursing education. Retrieved from: https://www.aacnnursing.org.
- AACN . American Association of Colleges of Nursing; Washington, DC: 2019. 2004-2018 Enrollment and graduations in baccalaureate and graduate programs in nursing. [Google Scholar]
- AACN . American Association of Colleges of Nursing; Washington, DC: 2019. 2018-2019 Enrollment and graduations in baccalaureate and graduate programs.https://www.aacnnursing.org/News-Information/Research-Data-Center/Standard-Data-Reports Retrieved from: [Google Scholar]
- AACN. (2019b). Fact sheet: The doctor of nursing practice. Retrieved from: https://www.aacnnursing.org/Portals/42/News/Factsheets/DNP-Factsheet.pdf.
- AACN . American Association of Colleges of Nursing; Washington, DC: 2019. Salaries of instructional and administrative nursing faculty in baccaluareate and graduate programs in nursing.https://www.aacnnursing.org/Store/product-info/productcd/IDSR_19SALSINST Retrieved from: [Google Scholar]
- AACN . American Association of Colleges of Nursing; Washington, DC: 2019. 2004-2018 Enrollment and Graduations in Baccalaureate and Graduate Programs in Nursing. [Google Scholar]
- American Association of Nurse Practitioners (AANP). (2019). The state of the nurse practitioner profession: 2018. Retrieved from: https://bit.ly/2PmHIdt.
- American College of Nurse Midwives (ACNM). (2012). Position statement: Midwifery education and the doctor of nursing practice (DNP). Silver Spring, MD. Retrieved from: https://bit.ly/2Zf6lf2 [Reaffirmed in May, 2017]
- Auerbach D.I., Martsolf G.R., Pearson M.L., Taylor E.A., Zaydman M., Muchow A.N., …, Lee Y. The DNP by 2015: A study of the institutional, political, and professional issues that facilitate or impede establishing a post-baccalaureate doctor of nursing practice program. Rand Health Quarterly. 2015;15(1):3. PMID: 28083356. [PMC free article] [PubMed] [Google Scholar]
- Beeber A.S., Palmer C., Waldrop J., Lynn M.R., Jones C.B. The role of doctor of nursing practice-prepared nurses in practice settings. Nursing Outlook. 2019;67:354–364. doi: 10.1016/j.outlook.2019.02.006. [DOI] [PubMed] [Google Scholar]
- Broome M., Bowersox D., Relf M. A new funding model for nursing education through business development initiatives. Journal of Professional Nursing. 2018;34(2):97–102. doi: 10.1016/j.profnurs.2017.10.003. [DOI] [PubMed] [Google Scholar]
- Bussenius H, Moore C, Green C, Pope J, Waller B, Bussenius P, Bussenius A. (2020). TechTank Mobile App Project COVID-19 (Version #1). [Mobile Application].
- Cappiello J., Simmonds K., Bmrick K. A survey of characteristics of transition-to-practice nurse practitioner programs. The Journal for Nurse Practitioners. 2010;15(3):241–244. doi: 10.1016/j.nurpra.2018.10.006. [DOI] [Google Scholar]
- Carter M.A., Jones M.J. Nationwide doctor of nursing practice/advanced practice registered nurse survey on roles, functions, and competencies. Journal of Doctoral Nursing Practice. 2017;10(2):108–112. doi: 10.1891/2380-9418.10.2.108. [DOI] [PubMed] [Google Scholar]
- Chipps E., Tussing T., Labardee R., Nash M., Brown K. Examining the roles and competencies of nurse leaders, educators, and clinicians with a doctor of nursing practice at an academic medical center. Journal of Doctoral Nursing Practice. 2018;11(2):119–124. doi: 10.1891/2380-9418.11.2.119. [DOI] [PubMed] [Google Scholar]
- Cronenwett L., Dracup K., Grey M., McCauley L., Meleis A., Salmon M. The doctor of nursing practice: A national workforce perspective. Nursing Outlook. 2011;59(1):9–17. doi: 10.1016/j.outlook.2010.11.003. [DOI] [PubMed] [Google Scholar]
- Fullerton J.T., Schuiling K.D., Sipe T.A. The doctorate of nursing practice and entry into midwifery practice: Issues for consideration and debate. Nurse Education in Practice. 2019;36:97–100. doi: 10.1016/j.nepr.2019.02.001. [DOI] [PubMed] [Google Scholar]
- Graduatenursingedu.org. (2019). Best value MSN-family nurse practitioner programs by state for 2019-20. Retrieved from: https://bit.ly/2PSzHx4
- Grey M. The doctor of nursing practice: Defining the next steps. Journal of Nursing Education. 2013;52(8):462–465. doi: 10.3928/01484834-20130719-02. [DOI] [PubMed] [Google Scholar]
- Harper D.C., McGuinnes T.M., Johnson J. Clinical residency training: Is it essential to the doctor of nursing practice for nurse practitioner preparation? Nursing Outlook. 2017;65(1):50–57. doi: 10.1016/j.outlook.2016.08.004. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine . National Academy of Sciences; Washington DC: 2001. Crossing the quality chasm: A new health system for the 21st century.https://bit.ly/36E02VZ Retrieved from: [Google Scholar]
- Institute of Medicine (IOM) The National Academies Press; Washington DC: 2011. The future of nursing: Leading change, advancing health. [DOI] [PubMed] [Google Scholar]
- MacKay M., Glynn D., McVey C., Rissmiller P. Nurse practitioner residency programs and transition to practice. Nursing Forum. 2018;53:156–160. doi: 10.1111/nuf.12237. [DOI] [PubMed] [Google Scholar]
- Minnick A.F., Kleinpell R., Allison T.L. DNPs’ labor participation, activities, and reports of degree contributions. Nursing Outlook. 2019;67(1):89–100. doi: 10.1016/j.outlook.2018.10.008. [DOI] [PubMed] [Google Scholar]
- Morton P. Economic trends in higher education. Journal of Professional Nursing. 2019;35(5):341–343. doi: 10.1016/j.profnurs.2019.08.011. [DOI] [PubMed] [Google Scholar]
- Mundinger M.O., Carter M.A. Potential crisis in nurse practitioner preparation in the United States. Policy, Politics, & Nursing Practice. 2019;20(2):57–63. doi: 10.1177/1527154419838630. [DOI] [PubMed] [Google Scholar]
- Mundinger M.O., Starck P., Hathaway D., Shaver J., Fugate Woods N. The ABCs of the doctor of nursing practice: Assessing resources, building a culture of clinical scholarship, curricular models. Journal of Professional Nursing. 2009;25(2):69–74. doi: 10.1016/j.profnurs.2008.01.009. [DOI] [PubMed] [Google Scholar]
- Sciacca K., Reville B. Evaluation of nurse practitioners enrolled in fellowship and residency programs: Methods and trends. The Journal for Nurse Practitioners. 2016;12(6):e275–e280. doi: 10.1016/j.nurpra.2016.02.011. [DOI] [Google Scholar]
- Shelby M., Wermers R. Complexity science fosters professional advanced nurse practitioner role emergence. Nursing Administration Quarterly. 2020;44(2):149–158. doi: 10.1097/NAQ.0000000000000413. [DOI] [PubMed] [Google Scholar]
- Sherrod B., Goda T. DNP-prepared leaders guide healthcare system change. Higher Learning. 2016;47(9):13–16. doi: 10.1097/01.NUMA.0000491133.06473.92. [DOI] [PubMed] [Google Scholar]
- The Institute for College Access & Success (2016). Student debt and the class of 2015. Retrieved from: https://bit.ly/33r52Mb
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.