Abstract
Teleproctoring can be used successfully in performing challenging and innovative structural heart interventions using sophisticated technology that allows real-time bidirectional audiovisual communication with digital transmission of live videos and direct observation of the operative field by a remote proctor. The authors share an illustrative case that was performed amid the coronavirus disease-2019 global pandemic that led to travel restrictions to limit spread of the virus. Teleproctoring has future implications beyond the current global health crisis to facilitate rapid dissemination and exchange of knowledge for ultimately helping patients around the globe.
Key Words: LAMPOON, structural heart interventions, teleproctoring, transcatheter mitral valve replacement (TMVR)
Abbreviations and Acronyms: COVID-19, coronavirus disease-2019; LAMPOON, intentional laceration of the anterior mitral valve leaflet to prevent left ventricular outflow obstruction; OR, operating room
Graphical abstract
A novel coronavirus, severe acute respiratory syndrome coronavirus-2, first reported in Wuhan, China, in December 2019, has caused a worldwide outbreak of a respiratory illness named coronavirus disease-2019 (COVID-19) (1). The World Health Organization declared COVID-19 a pandemic on March 11, 2020, because of the accelerating spread of the virus across international borders with significant morbidity and mortality (2). Given the rapid spread of infection related to travel, most institutions, including health care organizations, have instituted strict business-related travel restrictions that include meetings, conferences, and professional development and training. This prohibition also includes travel to proctor invasive procedures.
Most institutions have curtailed or stopped elective procedures, including many structural heart interventions, because of growing strain on health care resources. Weighing the risks and benefits of proceeding with a planned structural heart intervention or delaying it is crucial, as some of these interventional procedures are not truly elective in nature. Although delaying a procedure is helpful in reducing the risk for the patient of novel coronavirus exposure outside the home and preserving limited hospital resources, it can have unintended consequences, such as clinical deterioration, worsening heart failure, and death in some high-risk patients. A consensus document from the American College of Cardiology and Society for Cardiovascular Angiography and Interventions suggests guidelines for structural heart interventions during the current COVID-19 pandemic (3). In accordance with this consensus document, we scheduled a valve-in-valve transcatheter mitral valve replacement for an 82-year-old woman with progressive severe symptoms of exertional dyspnea secondary to a degenerated bioprosthetic mitral valve and recent hospitalization for congestive heart failure. On the basis of neo–left ventricular outflow tract measurement by computed cardiac tomography, we chose a reverse LAMPOON (intentional laceration of the anterior mitral valve leaflet to prevent left ventricular outflow obstruction)–assisted transcatheter mitral valve replacement to reduce the risk for left ventricular outflow tract obstruction, which is associated with high risk for mortality (4). The LAMPOON procedure has been performed at only a few centers under on-site proctorship.
Accordingly, we invited a nationally renowned pioneer in this technique (A.B.G.) to join us as a proctor for the case. Unfortunately, travel to our institution became impossible because of the travel restrictions discussed previously. During a conference call the night prior to the procedure, we discussed the implications and options for our patient, including cancelation of the case and postponement until travel restrictions could be lifted versus proceeding with remote teleproctoring. Given the patient’s progressive symptoms, recent hospitalization for congestive heart failure, and uncertainty regarding the duration of the travel restrictions, the heart team decided to proceed with the case using remote teleproctoring.
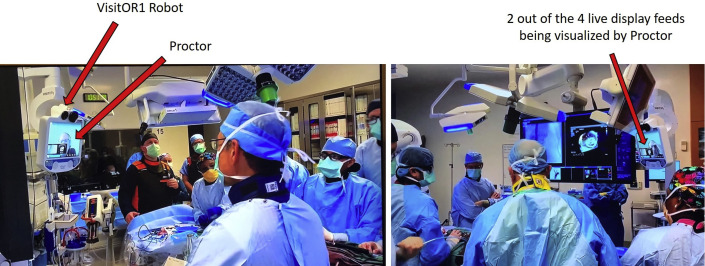
The proctor had prior experience in teleproctoring, and our institution had extensive experience in transcatheter valve replacement as well as the requisite equipment and information technology support personnel. The proctor and our team carried out two 60-min “drills” reviewing the procedural steps as well as review of a similar case their team had performed recently, using WebEx video conferencing, that night and the following morning. Within a few hours’ notice, the team was able to coordinate with and send instructions to the proctor to download and install the InTouch Provider software (InTouch Health, Santa Barbara, California), while the on-site team set up the VisitOR1 robot (Karl Storz, Tuttlingen, Germany) in the hybrid operating room (OR) (Figure 1A ). The on-site team connected digital visual interface and power cables between the robot and the OR’s integrated video feeds (live fluoroscopy and echocardiography) to allow live data transmission (Figure 1B). The proctor was then conferenced into the OR with real-time bidirectional audio and video communication from his office in Atlanta, Georgia. The proctor was able to use his Windows-based personal computer to visualize live fluoroscopy and live echocardiography (using digital rather than analog links), as well as the operating field (using a remotely controlled camera on the head of the robot) while being able to communicate with our team and operators (Figure 2 ) and to perform telestration as needed. In addition, he was able to view 2 of the 4 available video feeds at a time and to toggle between each live feed as needed (Figure 2). While viewing the main camera view of the robot, he was able to select different areas of the image for closer examination. He was also able to direct the head of the robotic camera to the areas of the OR where he believed his attention was needed, for example, the operative field or the device setup. Thus, he was able to have direct high-quality visualization of the catheter tip manipulation and of the operators’ hands during periods that required complex manual manipulations. Two novel steps that are specific to the procedure are the mating of 2 guiding catheters over a wire that is introduced transseptally and exteriorized and the creation of a specific bend in this wire known as a “flying V.” The former step requires specific catheter manipulations and was proctored using the live fluoroscopy feed, while the latter step, which involves selective denudation of wire coating along 4 to 5 mm length in the midshaft of a 300-cm, 0.014-inch steel guidewire followed by manual introduction of a specific series of bends in the wire, was proctored using the direct video feed (4). With this guidance, the proctor was able to watch the team create the flying V on the operative field before inserting it into the patient. Reverse LAMPOON was successfully performed with the proctor’s guidance, followed by valve-in-valve transcatheter mitral valve replacement in the usual fashion with a 1 mm Hg residual gradient and no left ventricular outflow tract obstruction. There were no immediate complications, and the patient was discharged home on post-operative day 1.
Figure 1.
Equipment Used for Teleproctoring and Live Information Being Transmitted to Teleproctor
(A) VisitOR1 robot. (B) Live dynamic display in the hybrid operating room with live fluoroscopy, live echocardiography, operative field, and hemodynamic status.
Figure 2.
Images From the Hybrid Operating Room Demonstrating the Proctor Live on the VisitOR1 Robot Screen With Bidirectional Visual (and Audio) Communication
This case demonstrates the utility of teleproctoring to allow successful performance of a new structural heart interventional procedure. Teleproctoring can consist of simple verbal communication by telephone or rudimentary video communication by smart phone. By reducing the need for travel, teleproctoring offers several advantages over in-person proctoring with regard to savings in cost, time, number of individuals trained, and, as in the current global COVID-19 crisis, to help reduce the risk for virus spread. In contrast to the methods that have been used traditionally, we chose a considerably more sophisticated system that allows the digital transmission of several live videos accompanied by direct observation of the operative field and the ability of a remote proctor to telestrate (add free-hand markings on the live images using the mouse cursor) important points instantly.
The VisitOR1 robot is a U.S. Food and Drug Administration–approved, Class II, Health Insurance Portability and Accountability Act–compliant telepresence device manufactured by InTouch Health and supported on-site by Karl Storz. The InTouch Provider software used to access these robots is available on Windows PC, iPhone, and iPad devices. As opposed to most commercially available video-calling applications, the InTouch network is encrypted for security and gives the remote user (in this case the proctor) the abilities to view multiple images simultaneously, to zoom, pan, tilt the robot’s camera, and to telestrate. Typically, when the robot is connected to a network that meets specific network requirements provided by InTouch Health, the robot has little to no latency during the session. As the robot was already on the secure network with the hospital information technology department’s assistance, there was no diminution of audio or video transmission during the case. The user-friendly features and reliability of the robot not only enhanced the method of video conferencing but also provided critical information to the proctor in real time, with no lag, and thus led to a favorable teleproctoring experience with a successful clinical outcome.
Although teleproctoring has been developed in other procedure-oriented medical fields (5), data on its use in structural heart interventions are nonexistent to our knowledge. Several complex techniques, including LAMPOON, BASILICA (transcatheter laceration of aortic leaflets to prevent coronary obstruction during transcatheter aortic valve replacement), and transcaval transcatheter aortic valve replacement, have been developed over the past few years to minimize complications during otherwise unfeasible transcatheter valve procedures but are still performed at a limited number of centers (6). For example, LAMPOON procedure outcomes were recently reported in 30 patients at 5 centers; all cases were proctored given the technically challenging aspect of the procedures (4). Teleproctoring has the potential to address some of the issues pertinent to this field, particularly disproportion between the number of trained experts and the number of interventionalists and surgeons who require training.
It is important to recognize several caveats. First, the operating team was extremely experienced, having performed approximately 2,000 transcatheter valve replacements over the prior 9 years, and had an established harmonious working relationship. Second, the procedure was performed with the participation of an individual who was experienced at proctoring. Most critical, perhaps, the real-time nature of the transmission and its high video quality allowed the proctor to be comfortable that his recommendations were translated immediately into appropriate actions. Finally, extensive review of the case and procedure were performed on 2 occasions prior to the procedure.
Teleproctoring has significant implications that extend well into the future, including facilitation of rapid dissemination and exchange of knowledge for innovative technical procedures helping patients across the globe.
Footnotes
Dr. Goel is a member of the Speakers Bureau of Abbott Structural Heart. Dr. Reardon is a consultant to Medtronic. Dr. Little is a consultant to Medtronic and Abbott. Dr. Greenbaum has received proctor honoraria from Edwards Lifesciences and Medtronic; and holds equity in Transmural Systems. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the JACC: Cardiovascular Interventionsauthor instructions page.
References
- 1.Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of Coronavirus disease 2019 in China. N Engl J Med 2020;382:1708–20. [DOI] [PMC free article] [PubMed]
- 2.World Health Organization WHO director-general’s opening remarks at the media briefing on COVID-19—11 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 Available at:
- 3.Shah P.B., Welt F.G., Mahmud E. Triage considerations for patients referred for structural heart disease intervention during the coronavirus disease 2019 (COVID-19) pandemic: an ACC /SCAI consensus statement. J Am Coll Cardiol. 2020;13:1484–1488. doi: 10.1016/j.jcin.2020.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Khan J.M., Babaliaros V.C., Greenbaum A.B. Anterior leaflet laceration to prevent ventricular outflow tract obstruction during transcatheter mitral valve replacement. J Am Coll Cardiol. 2019;73:2521–2534. doi: 10.1016/j.jacc.2019.02.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang E.Y., Knight S., Guetter C.R. Telemedicine and telementoring in the surgical specialties: a narrative review. Am J Surg. 2019;218:760–766. doi: 10.1016/j.amjsurg.2019.07.018. [DOI] [PubMed] [Google Scholar]
- 6.Khan J.M., Rogers T., Greenbaum A.B. Transcatheter electrosurgery: JACC state-of-the-art review. J Am Coll Cardiol. 2020;75:1455–1470. doi: 10.1016/j.jacc.2020.01.035. [DOI] [PMC free article] [PubMed] [Google Scholar]