As the COVID-19 global pandemic rapidly expands, the potential of digital health for mental health has become urgently apparent. The surge in interest and use of digital health to meet the demands of patients in quarantine, with social and physical distancing restrictions, and a lack of in-person care has centered on anxiety and depression – and largely ignored those with serious mental illnesses (SMI) such as psychotic disorders. Adapting digital health to the needs of SMI patients is an emergent need.
Initial reports suggest the mental health of patients with COVID-19 are being poorly handled (Duan and Zhu, 2020); few implementation efforts around psychological interventions had been completed in China and strict infection measures limited access to mental health providers. In place of traditional care, online mental health resources were utilized in China (Liu et al., 2020) although none appear specifically designed or tested for use in clinic care. Already in the United States there have been changes around telehealth with federal regulations temporarily permitting unprecedented access through non-secure platforms and across state lines.
This willingness to embrace digital health, especially telehealth, is common in disasters. Patients with schizophrenia may have higher levels of avoidance coping and report overall reduced coping ability, self-esteem, and social support than the general population in disaster settings (Horan et al., 2007). This higher avoidance may lead to more stress later. Patients with schizophrenia under- report their physical health symptoms (Sonoda et al., 2019). Patients with SMI may react to disaster and uncertainties with heightened anxiety, and social distancing could contribute to isolation and worsening depression. SMI Patients also may have cognitive limitations posing challenges to appropriately handle the informational overload in times of crises; tele/digital health can address cognitive deficits (Guimond et al., 2019). Telehealth can meet these mental health needs of patients with SMI (Krzystanek et al., 2017) though issues of access present new opportunities and challenges for the field.
Smartphones may be an effective way to implement telepsychiatry services in people with SMI. Telepsychiatry requires camera, internet connection, and computer all integrated into a single device – such integration is feasible via smartphones for most patients. Patients with schizophrenia are more likely to have a phone than computer (Aschbrenner et al., 2018) with nearly 50% of people with schizophrenia owning a smartphone in 2015 (Young et al., 2019) and 66% in 2018 (Torous et al., 2018). Considering that even in the general population 37% of adults access the internet primarily via smartphones and 58% for those ages 18 to 29 according to Pew data from 2019 – it is clear that telehealth cannot be separated from mobile health and smartphones.
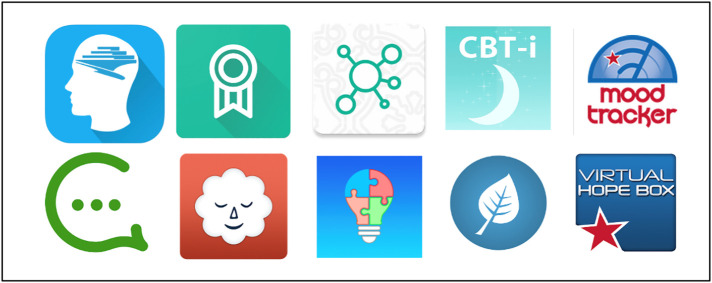
Several opportunities are emerging for improving care via smartphones. This selected brief list (see Fig. 1 ) does not do justice to the many excellent apps not mentioned and the teams behind each one mentioned. FOCUS (Ben-Zeev et al., 2019) from Dr. Dror Ben-Zeev, and PRIME (Schlosser et al., 2018) from Dr. Danielle Schlosser, Intellicare from Dr. David Mohr (Mohr et al., 2017), and CBT2Go (Depp et al., 2019) from Dr. Colin Depp as just some examples of mobile health tools for SMI. Using digital phenotyping and smartphone surveys/sensors to better monitor patients' real time, longitudinal, and dynamic experience of mental health is feasible with apps like mindLAMP from our group (Torous et al., 2019), Cross Check from Dr. John Kane (Ben-Zeev et al., 2017) and many others like the MONARCHA by Dr. Jakob Bardram plus many more (Bardram and Mati, 2020) These smartphone digital data streams can be used predict relapse (Barnett et al., 2018), and create personalized care plans responsive to the psychological and social environments of patients. Many commercial apps like Stop Breath and Think (Athanas et al., 2019) offer provide real-time interventions for anxiety that can be of help in addressing the widespread anxiety reactions generated by Covid-19 like crises. The United States Department of Veterans' Affairs offers a library of free mental health apps for anyone to use and benefit from. Finally, the ability to connect and access peer support via apps like PeerTech from Dr. Karen Fortuna (Fortuna et al., 2019) highlights yet another area of rapid expansion potentially addressing the negative consequences of social distancing (Fortuna et al., 2019). This select list covers only a fraction of the many impressive app efforts in SMI.
Fig. 1.
Many apps applicable for SMI exist. These selected examples from those mentioned in the text and found on the Android app store on March 24th, 2020: (from top left to bottom right): CBT2GO, PRIME, Intellicare, CBT-I Coach (VA), T2 Mood Tracker (VA), PeerTech, Stop Breath and Think, mindLAMP, Mindfulness Coach (VA), and Virtual Hopebox (VA).
Harnessing these exciting mobile health developments in schizophrenia to help patients today is both an issue of access as well as of awareness and implementation. There is an urgent need to train clinicians about mobile health and reduce workflow barriers to digital health. Our group has piloted a new team member, the digital navigator (Wisniewski et al., 2019), to help bridge the clinical and digital worlds and serve as the ‘glue’ to help complete the link. Some patients will also need help with digital literacy skills and competencies in order to optimally access telehealth and apps. Specifically designed for patients with serious mental illness, our group has piloted a 6 to 8-week group training to equip patients with the ability to confidently navigate the digital world (Hoffman et al., 2020). These two efforts are not headline grabbing artificial intelligence or machine learning projects but the practical foundation the field must invest in today to ensure access and equity.
Digital health also brings novel risks that the field must now consider and work to minimize. Today too often patients using mobile health tools are asked to forsake their privacy to open an app and must first agree to a privacy policy written at a college reading level. The problem is worse for mental health apps which have one of the highest rates of failing to offer even the presence of a privacy policy compared to other medical conditions (Wisniewski et al., 2019)
Many commercial apps for SMI, the ones patients access today, lack evidence or even adherence to agreed upon standards. At the time of this writing the third search result in the iTunes app store for schizophrenia is an action “game that will make you lose your mind” – a stigmatizing and unhelpful app for anyone.
The idea of using mobile technology like apps for global mental health is not new but today that idea is becoming reality for SMI. The early experiences with COVID-19 have forged that reality and now demand healthcare systems seek to rapidly keep up with the technology needs of patients. Schizophrenia already has a legacy of leadership and innovation in mobile mental health and in the near future the transformation, spurred by the COVID-19 crisis will accelerate until mobile and tele- digital health compliment if not challenge the standard of care.
Disclosure
Drs. Torous and Keshavan received grant support from the Natalia Foundation to develop the mindLAMP platform.
References
- Aschbrenner K.A., Naslund J.A., Grinley T., Bienvenida J.C., Bartels S.J., Brunette M. A survey of online and mobile technology use at peer support agencies. Psychiatry Q. 2018;4 doi: 10.1007/s11126-017-9561-4. (1–0) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Athanas A.J., McCorrison J.M., Smalley S., Price J., Grady J., Campistron J., Schork N.J. Association between improvement in baseline mood and long-term use of a mindfulness and meditation app: observational study. JMIR Ment. Health. 2019;6(5) doi: 10.2196/12617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bardram J., Mati A. A decade of ubiquitous computing research in mental health. IEEE Pervasive Comput. 2020;19(1):62–72. [Google Scholar]
- Barnett I., Torous J., Staples P., Sandoval L., Keshavan M., Onnela J.P. Relapse prediction in schizophrenia through digital phenotyping: a pilot study. Neuropsychopharmacology. 2018;43(8):1660–1666. doi: 10.1038/s41386-018-0030-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Zeev D., Brian R., Wang R., Wang W., Campbell A.T., Aung M.S.H., Merrill M., Tseng V.W.S., Choudhury T., Hauser M., Kane J.M., Scherer E.A. CrossCheck: integrating self-report, behavioral sensing, and smartphone use to identify digital indicators of psychotic relapse. Psychiatr. Rehabil. J. 2017;40(3):266–275. doi: 10.1037/prj0000243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Zeev D., Buck B., Kopelovich S., Meller S. A technology-assisted life of recovery from psychosis. NPJ Schizophr. 2019;5(1):1–4. doi: 10.1038/s41537-019-0083-y. 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Depp C.A., Perivoliotis D., Holden J., Dorr J., Granholm E.L. Single-session mobile-augmented intervention in serious mental illness: a three-arm randomized controlled trial. Schizophr. Bull. 2019;45(4):752–762. doi: 10.1093/schbul/sby135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan L., Zhu G. Psychological interventions for people affected by the COVID-19 epidemic. The Lancet Psychiatry. Epub. 2020;7(4):300–302. doi: 10.1016/S2215-0366(20)30073-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortuna K., Barr P., Goldstein C., Walker R., Brewer L., Zagaria A., Bartels S. Application of community-engaged research to inform the development and implementation of a peer-delivered mobile health intervention for adults with serious mental illness. Journal of Participatory Medicine. 2019;11(1) doi: 10.2196/12380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guimond S., Keshavan M.S., Torous J.B. Towards remote digital phenotyping of cognition in schizophrenia. Schizophr. Res. 2019;208:36–38. doi: 10.1016/j.schres.2019.04.016. [DOI] [PubMed] [Google Scholar]
- Hoffman L.I., Wisniewski H.A., Hays R.Y., Henson P.H., Vaidyam A.D., Hendel V.I., Keshavan M.A., Torous J. Digital Opportunities for Outcomes in Recovery Services (DOORS): a pragmatic hands-on group approach toward increasing digital health and smartphone competencies, autonomy, relatedness, and alliance for those with serious mental illness. J. Psychiatr. Pract. 2020;26(2):80. doi: 10.1097/PRA.0000000000000450. 2020 Mar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horan W.P., Ventura J., Mintz J., Kopelowicz A., Wirshing D., Christian-Herman J., Foy D., Liberman R.P. Stress and coping responses to a natural disaster in people with schizophrenia. Psychiatry Res. 2007;151(1–2):77–86. doi: 10.1016/j.psychres.2006.10.009. [DOI] [PubMed] [Google Scholar]
- Krzystanek M., Krysta K., Skałacka K. Treatment compliance in the long-term paranoid schizophrenia telemedicine study. J. Technol. Behav. Sci. 2017;2(2):84–87. doi: 10.1007/s41347-017-0016-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S., Yang L., Zhang C., Xiang Y.T., Liu Z., Hu S., Zhang B. Online mental health services in China during the COVID-19 outbreak. The Lancet Psychiatry. Epub. 2020;7(4):e17–e18. doi: 10.1016/S2215-0366(20)30077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr D.C., Tomasino K.N., Lattie E.G., Palac H.L., Kwasny M.J., Weingardt K., Karr C.J., Kaiser S.M., Rossom R.C., Bardsley L.R., Caccamo L., Stiles-Shields C., Schueller S.M. IntelliCare: an eclectic, skills-based app suite for the treatment of depression and anxiety. J. Med. Internet Res. 2017;19(1) doi: 10.2196/jmir.6645. 2017 Jan 5. e10. (PMID: 28057609; PMCID: PMC524 7623) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlosser D.A., Campellone T.R., Truong B., Etter K., Vergani S., Komaiko K., Vinogradov S. Efficacy of PRIME, a mobile app intervention designed to improve motivation in young people with schizophrenia. Schizophr. Bull. 2018;44(5):1010–1020. doi: 10.1093/schbul/sby078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonoda Y., Ozaki A., Hori A., Higuchi A., Shimada Y., Yamamoto K., Morita T., Sawano T., Leppold C., Tsubokura M. Premature death of a schizophrenic patient due to evacuation after a nuclear disaster in Fukushima. Case Rep. Psychiatry. 2019;3284153 doi: 10.1155/2019/3284153. (eCollection 2019) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torous J., Wisniewski H., Liu G., Keshavan M. Mental health mobile phone app usage, concerns, and benefits among psychiatric outpatients: comparative survey study. JMIR Ment. Health. 2018;5(4) doi: 10.2196/11715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torous J., Wisniewski H., Bird B., Carpenter E., David G., Elejalde E., Fulford D., Guimond S., Hays R., Henson P., Hoffman L. Creating a digital health smartphone app and digital phenotyping platform for mental health and diverse healthcare needs: an interdisciplinary and collaborative approach. J. Technol. Behav. Sci. 2019;4(2):73–85. 2019 Jun 15. [Google Scholar]
- Wisniewski H., Liu G., Henson P., Vaidyam A., Hajratalli N.K., Onnela J.P., Torous J. Understanding the quality, effectiveness and attributes of top-rated smartphone health apps. Evid. Based Ment. Health. 2019;22(1):4–9. doi: 10.1136/ebmental-2018-300069. 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young A.S., Cohen A.N., Niv N., Nowlin-Finch N., Oberman R.S., Olmos-Ochoa T.T., Goldberg R.W., Whelan F. Mobile phone and smartphone use by people with serious mental illness. Psychiatr. Serv. 2019 Nov 20;71(3):280–283. doi: 10.1176/appi.ps.201900203. (appi-ps) [DOI] [PMC free article] [PubMed] [Google Scholar]