To the Editor
Since December, 2019, corona virus disease 2019 (COVID-19) caused by SARS-CoV-2, has spread to the majority of countries worldwide [1,2]. Here, we reported the clinical characteristics of a severe case with co-infection of SARS-CoV-2 and common respiratory pathogens. The patient was a 65-year-old woman, who had severe clinical manifestations of COVID-19, including symptoms, decreased lymphocyte counts, abnormal chest CT images. Next-generations sequencing (NGS) was used to test whether she was co-infected with other pathogens besides SARS-CoV-2. The sputum samples were collected and found the presence of Haemophilus parainfluenzae and Moraxella catarrhalis by NGS.
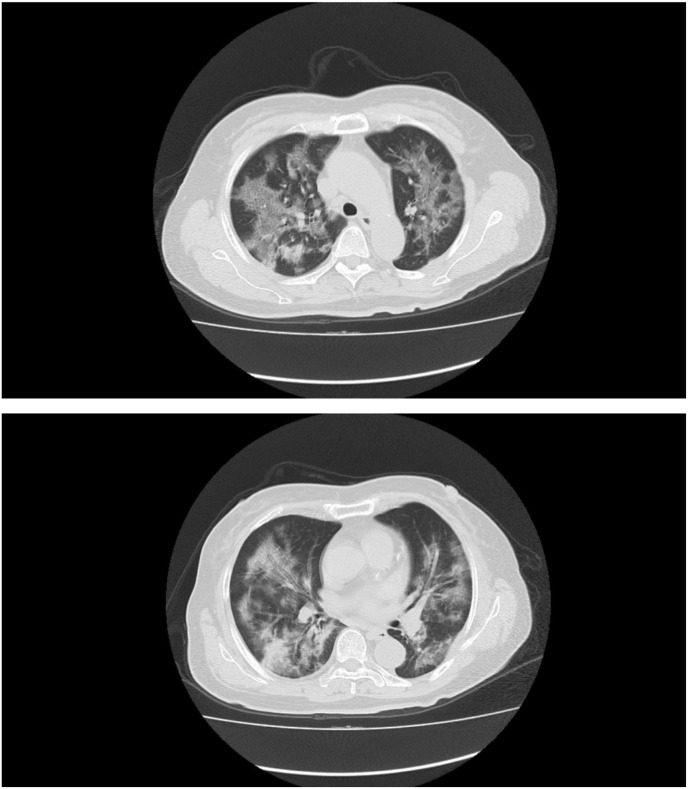
On Jan 22, 2020, she travelled from Wuhan to Guangzhou, China by high speed rail. From Feb 11, she developed fever lasted for 9 days, and developed cough as well as sore throat, without chills, headache, arthralgia, myalgia. On Feb 20, she was transferred to the Third Affiliated Hospital of Guangzhou Medical University with a body temperature of 38 °C. The next day, she developed a bit shortness of breath, with a body temperature of 37.5 °C. On Feb 21, blood routine tests showed normal white blood cell counts, but decreased lymphocyte counts. The blood glucose was increased. Chest CT scans showed bilateral diffuse ground-glass opacities and consolidation (Fig. 1 ). Nasopharyngeal swab samples were collected twice and both were negative for SARS-CoV-2 tested by qRT-PCR. However, sputum samples collected on the same day were positive for SARS-CoV-2 by NGS. Furthermore, Haemophilus parainfluenzae and Moraxella catarrhalis were also found in the sputum samples by NGS. In the afternoon of the same day, the oxygen saturation values of the patient decreased to 91.2%, and the partial pressure of oxygen in arterial blood decreased to 61.2 mmHg. Therefore, she received high-flow nasal cannula oxygen therapy (40% concentration, flow rate 60 L/min). The patient was diagnosed as severe COVID-19, and was transferred to the First Affiliated Hospital of Guangzhou Medical University for isolation and treatment where are designed to treat severe COVID-19 cases by local health authorities.
Fig. 1.
Chest CT images of the Patient. CT scans showed bilateral multiple lobular and subsegmental areas of ground-glass opacity and consolidation 9 days after symptoms onset.
More and more COVID-19 cases have been reported by the majority of countries worldwide [2]. Health-care professionals do their best to treat patients with COVID-19. Unfortunately, 85,522 cases died of COVID-19 globally by April 9, 2020 [2]. This implies that we need further to improve how to treat COVID-19, especially for severe cases. In the present study, the cause that resulted in severe condition of the patient could be the co-infection of SARS-CoV-2, Haemophilus parainfluenzae and Moraxella catarrhalis.
Nowadays, more attentions are paid to SARS-CoV-2, so it is easy to neglect patients infected with other pathogens besides SARS-CoV-2 during the outbreak of COVID-19. When we face severe COVID-19 cases, we need to think about more, especially co-infection. Older patients, having diabetes, hypertension are causes of severe COVID-19 cases [3,4]. Furthermore, patients with diabetes are also easily infected with pathogens [5].
Anyway, we should be aware of the co-infection of other respiratory pathogens in patients with SARS-CoV-2 infection. Different kinds of detection methods should be used to find out pathogens in the pandemic of SARS-CoV-2.
Declaration of competing interest
All authors declare no financial, potential personal or commercial conflict of interest.
Acknowledgments
The present study was funded by National Natural Science Foundation of China (81401306), Clinical Research Project of Guangzhou Medical University (No. 2017[160]) and Guangdong Province Science and Technology Program (No. 2016ZC0143).
Contributor Information
Xingfei Pan, Email: panxf0125@163.com.
Dexiong Chen, Email: 13926000778@163.com.
References
- 1.Munster V.J., Koopmans M., van Doremalen N., van Riel D., de Wit E. A novel coronavirus emerging in China - key questions for impact assessment. N Engl J Med. 2020;382:692–694. doi: 10.1056/NEJMp2000929. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization Coronavirus disease 2019 (COVID-19) situation report-80. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200409-sitrep-80-covid-19.pdf?sfvrsn=1b685d64_4 report.
- 3.Yang X., Yu Y., Xu J. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020 doi: 10.1016/S2213-2600(20)30079-5. pii: S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wu C., Chen X., Cai Y. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in wuhan, China. JAMA Intern Med. 2020 doi: 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shah B.R., Hux J.E. Quantifying the risk of infectious diseases for people with diabetes. Diabetes Care. 2003;26:510–513. doi: 10.2337/diacare.26.2.510. [DOI] [PubMed] [Google Scholar]