Dear Editor,
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection mostly presents with mild respiratory symptoms, although more severely affected patients may die of refractory acute respiratory distress syndrome (ARDS).1 The pulmonary function of surviving patients may decrease significantly in the early stages post-weaning due to the massive alveolar damage. Therefore, early pulmonary rehabilitation is important in these patients. We would like to share our experience of early pulmonary rehabilitation program in severe SARS-CoV-2 pneumonia.
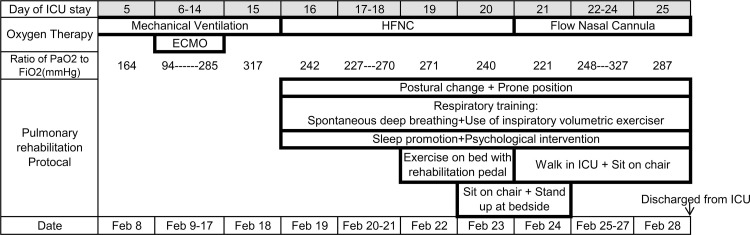
We received and successfully treated a 41-year-old man with severe SARS-CoV-2 pneumonia in the Intensive care unit (ICU) of the SARS-CoV-2 treatment center in Shenyang, China. This patient was supported with 11 days of mechanical ventilation and 9 days of extracorporeal membrane oxygenation as well as conventional supportive care. After weaning, a meticulous and individualized ICU rehabilitation program(see Fig. 1 ) was created, with four components:
-
1.
Postural change and prone position. Postural change and prone position probably improves gas exchange and reduces the incidence of secondary bacterial pneumonia by enhancing drainage of secretions. With good cooperation and assistance from medical staff, the patient underwent prone-position ventilation when conscious.
-
2.
Respiratory training to restore respiratory muscle strength and lung volume. Acute-phase ARDS-associated alveolar collapse and inflammation leads to pulmonary volume reduction.2 The chronic phase of ARDS may be characterized by pulmonary fibroproliferation, which also leads to diminished lung compliance.3 The patient was trained to undertake spontaneous deep breathing to maintain lung recruitment. An inspiratory volumetric exerciser was used to train the respiratory muscle strength.
-
3.
Early mobilization and physical exercises. Early mobilization helped avoid ICU-acquired weakness, and was aimed at improving respiratory and diaphragmatic muscle strength and promoting recovery of respiratory function.4 The patient started exercising from exercise on the bed, to sit on a chair, to assisted walking, and eventually to self-walking.
-
4.
Psychological intervention and sleep promotion. The medical staffs continued to communicate with the patient, and psychological counselling was telephonically conducted, which helped alleviate the patient's anxiety and depression. Sleep-promoting measures, including earplugs, eyeshades, relaxing music, and some sleeping medication were used to improve night sleep.
Fig. 1.
Timeline of disease and pulmonary rehabilitation. HFNC=high-flow nasal cannula; ECMO=extracorporeal membrane oxygenation.
At present, there has been no report about respiratory function injury in survivors of severe SARS-CoV-2 pneumonia. However, One third of the patients who recovered from SARS-CoV in 2003 complained of dyspnea, and approximately two thirds manifested pulmonary fibrosis in the early rehabilitation phase.5 In consideration of that, we provided special attention to the implementation of early pulmonary rehabilitation in ICU for severe SARS-CoV-2 pneumonia. We hope that our experience can remind ICUs of pulmonary rehabilitation in severe SARS-CoV-2 pneumonia other than routine respiratory support.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Competing Interest
The authors declare that they have no competing interests.
References
- 1.Yang X., Yu Y., Xu J. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020 doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Force A.D.T., Ranieri V.M., Rubenfeld G.D. Acute respiratory distress syndrome: the Berlin definition. JAMA. 2012;307:2526–2533. doi: 10.1001/jama.2012.5669. [DOI] [PubMed] [Google Scholar]
- 3.Papiris S.A., Manali E.D., Kolilekas L. Clinical review: idiopathic pulmonary fibrosis acute exacerbations–unravelling Ariadne's thread. Crit Care. 2010;14:246. doi: 10.1186/cc9241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patel B.K., Pohlman A.S., Hall J.B., Kress J.P. Impact of early mobilization on glycemic control and ICU-acquired weakness in critically ill patients who are mechanically ventilated. Chest. 2014;146:583–589. doi: 10.1378/chest.13-2046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chan K.S., Zheng J.P., Mok Y.W. SARS: prognosis, outcome and sequelae. Respirology. 2003;8(Suppl):S36–S40. doi: 10.1046/j.1440-1843.2003.00522.x. [DOI] [PMC free article] [PubMed] [Google Scholar]