Abstract
INTRODUCTION:
An oral health program for mothers starting from pregnancy in a disadvantaged district of İzmir was performed in 2013–2016. Dental behaviors and their determinants among intervention and control groups were compared in the third phase of the program.
METHODS:
This nonrandomized-controlled study was conducted in Phase 3. The intervention group began with 248 pregnant women; 69.4% (n = 172) of mothers with 6–9-month-old babies participated in Phase 2, 2014. At Phase 3 (18–24 months), 68.6% (n = 118) of mothers in the intervention group and 113 mothers living in another district as controls were included. Sociodemographic characteristics, determinants of behaviors, and outcomes defined as dental behaviors in the last week were assessed using a questionnaire.
RESULTS:
Regarding knowledge, perceived severity, and fatalistic beliefs, the intervention group had higher correct answer percentages. The percentage of mothers who could clean their children's teeth before sleep was higher in the intervention group (76.3%; P < 0.05), but the difference was lost by a child's resistance. The significant difference on avoiding bedtime nursing (65.3%) and sugary snacks (74.4%) in the intervention group disappeared with the obstacle of a child's protests or interference from relatives. In the intervention group, 32.2% of the mothers reported that they did not give any sugary snacks, 43.2% had never fed during sleep, and 26.3% cleaned their children's teeth during the last week. The results in the control group were 24.8%, 18.6%, and 8.8%, respectively (P < 0.05).
CONCLUSIONS:
The program improved the mothers' views regarding the determinants of dental behaviors, but greater support against obstacles was needed. Social environmental support is planned for the following stages of the program.
Keywords: Children, community based, intervention, oral health
Introduction
Early childhood caries (ECC) is a term that defines dental caries affecting children younger than 71 months old.[1] The situation is accepted as a public health concern due to its early onset and effect on the quality of life of young children. Studies report that ECC not only affects primary dentition but also these children frequently suffer from malnutrition, infections, growth disorders, and dental problems throughout their life.[2,3]
The studies showed that mothers play an important role in preventing the disease, not only by applying the necessary hygiene practices for their babies but also by providing a behavioral habit for further years.[4,5,6] Health-related concerns and awareness arise in expectant mothers, and pregnancy provides an appropriate time for health education both for themselves and their babies.[7] Therefore, educating expectant mothers during their pregnancy and education on the responsibility for their child's dental health is beneficial.[8]
There is no systematic oral health promotion program for pregnant women or early childhood in Turkey and no information on the oral health status or knowledge of socioeconomically disadvantaged families. Two studies conducted during pregnancy and postpartum reported lack of knowledge and negative behavior regarding oral health concerns.[9,10] Studies report that poor, less educated, and immigrant mothers and their children are at a higher need for oral health education and behavioral change support throughout the world.[2,4,11,12] Therefore, the aim of this article is to present the comparative results on oral health behaviors and their determinants in mothers from low socioeconomic status attending a promotion program and the control.
Methods
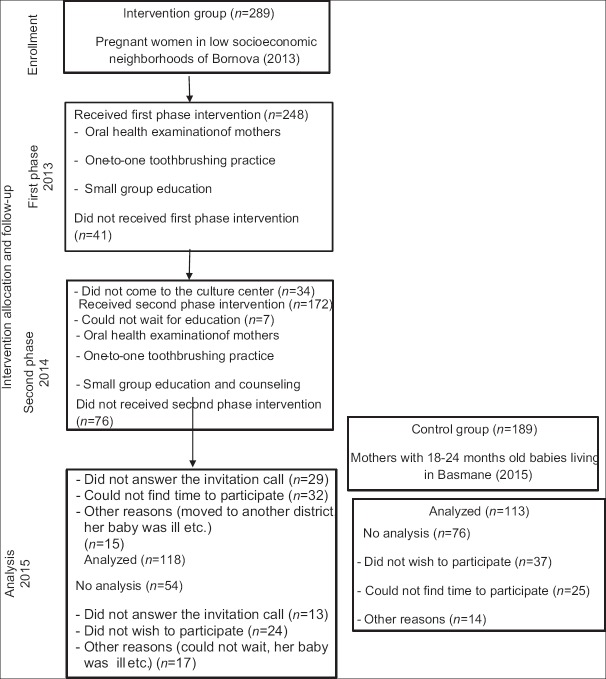
The intervention and the evaluation process of this nonrandomized-controlled study are summarized in Figure 1.
Figure 1.
The flowchart of the study population and the intervention progress
Intervention and control groups
The intervention group consisted of pregnant women living in three low socioeconomic neighborhoods in Bornova between April and June 2013 (n = 289) who were invited to take part in an educational activity by the municipality midwives. The participation rate was 85.8% (n = 248).
The second phase was performed in 2014 when the babies were 6–9 months old. The participation rate was 69.4% (n = 172); 68.6% (n = 118) of the mothers who attended the first two phases came to the third phase when the babies were 18–24 months old in 2015. In the third phase of the study, a control group was selected with consultation from Konak. A neighborhood was chosen in the Konak region with similar socioeconomic characteristics and no oral health program, including 189 mothers living in this neighborhood with 18–24-month-old babies were invited and 59.8% of the invited mothers (n = 113) participated in the study.
Our post hoc power analysis determined a statistical power of 0.99 for the analysis of our primary endpoint (brushes at least once) with a sample size of 231 patients.
Intervention
The program was performed in culture centers located in the neighborhoods where mothers lived. The primary aim of the first phase was educating mothers on oral health risks during pregnancy and to teach proper behavioral oral health habits including oral hygiene and diet. The second phase had learning objectives related to the importance of ECC, proper oral hygiene practices for their babies, and healthy eating practices.
The interventions in the first two phases were similar, with small group education and intraoral examination of mothers. Volunteer dentists who were trained as educators carried out the intraoral examinations and gave one-to-one toothbrushing education. Mothers were informed about their oral health status and were invited to be treated in the municipality's dental clinic. Mothers with periodontal problems were treated at Ege University.
In the first two phases, small groups (10–12 women in the first phase and 5–7 women in the second phase) were given 30 min of education either by a pediatric dentist (EE) or a public health (ZÖ) academician, respectively. The group education started with a 5-min video of a 4-year-old boy being treated for caries and included slides and interactive questions. Furthermore, a simple card game about proper diet was used. The authors (ZÖ and EE) had previously developed the video and the card game for this purpose. In each phase, the mothers, who attended all parts of the education and the intraoral examination, received donated packages containing baby care items such as shampoo, baby oil, and nappies. While the first phase was more informative, problem-based counseling in the second phase was performed in smaller groups. The mothers in the group were asked to report barriers they may have faced in implementing appropriate oral health behaviors. This small group discussed proposed solutions to support mothers in terms of self-efficacy. In addition to this, awareness in the social environment was provided both by an announcement of the education program in each neighborhood throughout districts by municipalities, as well as the participation of the mothers through social interaction with other participants. Siblings or mothers-in-law who accompanied most of the attending mothers were included in the education in order to provide their support about oral health. The third phase of the intervention, which is not assessed in this study, was performed when their babies were 18–24 months old.
Evaluation and statistical analysis
The variables of this study are divided into three groups: sociodemographic characteristics, dental behaviors, and determinants of the behaviors.
Sociodemographic characteristics include mothers' age, marital status, number of children, education level, time spend in Izmir, mother tongue, working status, health insurance as well as fathers' level of education and income. The determinants of dental behaviors were defined according to the frameworks of the health improvement model and social cognitive theory,[13] knowledge on bottle use, children's hygiene and treatment of caries, perceived severity, fatalistic beliefs, and social support. In addition to these, the Oral Health Self-Efficacy Scale developed by Finlayson et al. on toothbrushing[14] was modified to include giving sweet snacks and feeding during sleep. A three-point Likert scale (disagree, neutral, and agree) was used since the mothers did not effectively understand a 5-point scale in the other phases of the study.
The outcome variables were dental behaviors of the mothers in the previous week on giving sugary snacks, allowing the child to sleep with a bottle, or giving bottle during the night and tooth cleaning. The frequency was recorded as everyday, several days, or never.
Sociodemographic findings of both groups on nominal variables were evaluated by the Chi-square and the Fisher exact test, and ordinal variables were evaluated by the Mann–Whitney U-test due to nonhomogeneity of variances. Chi-square analysis was done with percentages of mothers saying “I agree” for behavior determinants and for behavior by percentages of mothers according to the frequency (never, sometimes, and everyday).
Ethics approval and consent to participate
The study received ethical approval from the Ege University Ethics Committee (13-2.1/18). Written informed consent was obtained from all mothers. The consent form was read to illiterate mothers, and their consent was obtained verbally in addition to their fingerprints.
Results
As shown in Table 1, mothers in the control group were slightly more disadvantaged on parameters such as education level, mother tongue, income, and health insurance. However, the difference was significant only in relation to mother tongue. The percentage of mothers with a mother tongue other than Turkish was 34.7 in the intervention group and 47.8 in the control group. All participants who reported that their mother tongue was not Turkish could speak and understand Turkish fluently. Two mothers in the intervention group and eight mothers in the control group reported that they do not have civil marriages. In both the groups, approximately three out of ten mothers reported that they had not completed their primary school education and two out of ten mothers had been living in Izmir shorter than 5 years. Mothers without health insurance constituted 16.1% of the intervention group and 11.5% of the control group. Almost half of the fathers were primary school graduated in both the groups. Only one out of four fathers had a salary higher than minimum wage. There was no significant difference (P = 0.275) between the groups in terms of the age of the babies calculated in months (intervention group = 18.66 ± 1.65; control group = 18.30 ± 2.60). The two groups were also not significantly different regarding the ages (intervention group = 29.44 ± 4.93; control group = 30.94 ± 6.93; P = 0.115) and number of the children (intervention group = 2.48 ± 1.36; control group = 2.86 ± 1.70; P = 0.065) of the mothers.
Table 1.
Comparison of mothers in intervention and control groups regarding sociodemographic variables
| Variables | Intervention group (n=118), n (%) | Control group (n=113), n (%) | Statistical analyses (P) |
|---|---|---|---|
| Marital status | |||
| Married | 98.3 (116) | 92.9 (105) | 0.055 |
| Other (religious marriage, not married) | 1.7 (2) | 7.1 (8) | |
| Education level | |||
| Illiterate | 11.9 (14) | 19.5 (22) | 0.094 |
| Literate | 18.5 (10) | 15.0 (17) | |
| Primary school graduate | 44.1 (52) | 42.5 (48) | |
| Middle school graduate | 20.3 (24) | 15.0 (17) | |
| High school graduate and higher | 15.3 (18) | 8.0 (9) | |
| Education level of the spouse | |||
| Illiterate | 1.7 (2) | 6.2 (7) | 0.097 |
| Literate | 5.9 (7) | 7.1 (15) | |
| Primary school graduate | 50.8 (67) | 59.3 (127) | |
| Middle school graduate | 22.0 (19) | 16.8 (45) | |
| High school graduate and higher | 19.5 (23) | 10.6 (12) | |
| Literate | 19.5 (23) | 10.6 (12) | |
| Duration of time spend in Izmir (years) | |||
| <3 | 10.2 (12) | 7.1 (8) | 0.506 |
| 3-5 | 11.0 (13) | 15.0 (17) | |
| >5 | 78.8 (93) | 77.9 (88) | |
| Mother tongue | |||
| Turkish | 65.3 (77) | 52.2 (59) | 0.007 |
| Other (Kurdish, and Arabic, etc.) | 34.7 (41) | 47.8 (54) | |
| Occupation | |||
| Homemaker | 94.1 (111) | 94.7 (107) | 0.837 |
| Other | 5.9 (7) | 5.3 (6) | |
| Mean income of the partner | |||
| Minimum wage or lower | 74.6 (88) | 78.8 (89) | 0.453 |
| Higher than minimum wage | 25.4 (30) | 21.2 (24) | |
| Health insurance of mother | |||
| None | 16.1 (19) | 11.5 (13) | 0.312 |
| Present | 83.9 (99) | 88.5 (100) |
In Table 2, mothers in the intervention and control groups were compared regarding the determinants of dental behaviors. The first determinant was knowledge of bottle use, children's oral hygiene, and treatment of caries. In both items related to bottle use, the percentages of mothers with correct answers were statistically higher in the intervention group than in the control group. While 87.3% of the mothers in the intervention group did not think that bottle feeding would help babies gain weight and grow, only 61.1% of the mothers in the control group had the same opinion. A more pronounced difference was observed between the two groups on the statement of sleeping with a bottle being harmful for oral health. The percentage of mothers who agreed on the statement “Keeping baby teeth clean is important” was 86.3% in the intervention group and 58.4% in the control group, and the difference was statistically significant. However, although being significantly higher than the control group (49.6%), the percentage of mothers who had correct information on the treatment of cavities in baby teeth was only 69.5 in the intervention group. Although not very profound, there was a statistically significant difference among groups on perceived severity. Regarding fatalism, 70.3% of the mothers in the intervention group believed that it was possible to have caries-free children, whereas only 32.7% of the mothers in the control group agreed this.
Table 2.
Comparison of mothers in intervention and control groups regarding the determinants of dental behaviors
| Determinants of dental behaviors | Intervention group (n=118), n (%) | Control group (n=113), n (%) | Statistical analyses (P) |
|---|---|---|---|
| Knowledge of bottle use, children’s hygiene, and treatment of caries | |||
| Putting a baby to bed with a bottle doesn’t help the child to gain weight and grow | 87.3 (103) | 61.1 (69) | <0.001 |
| It is wrong for oral health to let baby sleep with a bottle | 91.5 (108) | 57.5 (65) | <0.001 |
| Keeping baby teeth clean is important | 86.3 (101) | 58.4 (66) | 0.000 |
| Cavities in baby teeth should be treated | 69.5 (82) | 49.6 (59) | 0.002 |
| Perceived severity | |||
| My child’s dental caries may threaten his/her health and development | 84.7 (100) | 71.7 (81) | 0.016 |
| Oral health-related fatalism | |||
| I believe that parents can stop their child from developing dental cavities | 70.3 (83) | 32.7 (37) | 0.000 |
| Self-efficacy; oral hygiene | |||
| I can clean my child’s teeth every night | 76.3 (90) | 54.9 (62) | 0.001 |
| I can clean my child’s teeth every night even if I am very busy or tired | 58.5 (69) | 43.4 (49) | 0.022 |
| I can clean my child’s teeth every night even if he/she cries or runs away | 45.8 (54) | 43.4 (49) | 0.714 |
| I can clean my child’s teeth every night even if my spouse or mother-in-law interferes | 70.3 (83) | 50.4 (57) | 0.002 |
| Self-efficacy; not feeding during sleep | |||
| I can make sure that my child does not consume anything rather than water during sleep | 65.3 (77) | 48.7 (55) | 0.011 |
| I can make sure that my child does not consume anything rather than water during sleep even if I am very tired, sleepy, or tense | 45.8 (54) | 45.1 (51) | 0.923 |
| I can make sure that my child does not consume anything rather than water during sleep even if he/she cries | 42.4 (50) | 38.9 (44) | 0.595 |
| I can make sure that my child does not consume anything rather than water during sleep even if my spouse or mother-in-law interferes | 54.3 (63) | 42.5 (48) | 0.073 |
| Self-efficacy; avoid sweet snacks | |||
| I may avoid consumption of sweet snacks for my child | 74.4 (87) | 60.2 (68) | 0.022 |
| I may avoid consumption of sweet snacks for my child even if he/she insists and cries | 52.5 (62) | 48.7 (55) | 0.556 |
| I may avoid consumption of sweet snacks for my child even if my spouse or mother-in-law interferes or gives sweet snacks | 56.8 (67) | 46.7 (53) | 0.133 |
| Social support | |||
| My family supports me while cleaning my child’s teeth | 70.3 (83) | 69.9 (79) | 0.943 |
| My family supports me on not giving sweet snacks to my child | 58.5 (69) | 69.0 (78) | 0.209 |
| My family supports me when I am not feeding my child during sleep | 61.0 (72) | 60.2 (68) | 0.896 |
There was a significant difference in oral hygiene-related self-efficacy; while 76.3% of the mothers in the intervention group reported that she could clean her child's teeth every night, the same percentage was 54.9 in the control group. However, the difference was lowered by mother's tiredness and disappeared when the child actively refused cleaning. The teeth cleaning action was not affected because of interference of the husband or the mother-in-law. Regarding self-efficacy on bedtime nursing, although being statistically higher than the control group (48.7%), only 65.3% of the mothers in the intervention group reported that she could make sure that her child does not consume anything other than water during sleep. The percentage of mothers with self-efficacy lowered in the presence of barriers and the statistical significance was lost. Similarly, the percentage of mothers who believed that they could prevent children consuming sweet snacks was statistically higher in the intervention group (74.4%) than the control group (60.2%), whereas with the presence or interference of the husband or mother-in-law, and/or rejection of the child, the significance of the difference disappeared. Regarding the three items on social support, there were no statistically significant differences between the groups [Table 2].
According to the outputs of the program, significant differences were observed between the groups [Graph 1]. However, only 32.2% of the mothers in the intervention group stated that they did not give any sweet snacks, whereas a similar percentage was detected in the control group (24.8%). Mothers who reported that they never gave bottles at bedtime were 43.2% in the intervention group and 18.9% in the control group. Only 26.3% of the intervention group reported that they were brushing their children's teeth, whereas the same percentage was 8.8 in the control group. Although there was a statistically significant difference, the mothers who reported that they were brushing their children's teeth every night were very low in both the groups.
Graph 1.
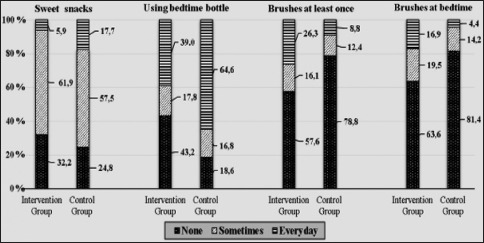
Comparison of mothers in intervention (n = 118) and control (n = 113) groups regarding dental behaviors in the previous week (%)
Discussion
This quasi-experimental study that was carried on a disadvantaged mother group revealed that all social determinants of health should be considered to change oral health behavior. The findings of the study showed that intervention was able to provide a difference regarding the knowledge-related determinants of behavior, whereas there were still obstacles on self-efficacy, the other important component of behavior change. In terms of behavior, which is the basic output of the work, the results were not at the desired level. On the other hand, this study, which was carried out in real-life situations, provided important clues as to which points should be noted in interventions for the mother, from which respects the mother should be supported for the obstacles that prohibit self-efficacy and hence dental behavior.
Success regarding knowledge and perceptions on bottle use, oral hygiene, and severity of dental caries in the intervention group in comparison with the control group was obtained. Although Finlayson et al. reported mother's knowledge about children's oral hygiene as a significant predictor of children's brushing frequency, they also indicated that improved oral health knowledge does not lead to long-lasting changes in behaviors.[14] A number of studies supported that teaching on preventing tooth decay in children has a limited effect on behaviors of parents and on children's oral health, and having knowledge about healthy behaviors is often insufficient for changing unhealthy behaviors.[15,16,17,18] This study also reflects the importance of other components of behavior other than the information obtained on behavior change.
Self-efficacy, mother's focus of control, and fatalistic beliefs are the important determinants of children's oral health and should be taken into account in interventions.[14] Naidu et al.[5] who compared the effect of motivational interview techniques in contrast to traditional health education found a reduction in oral health fatalism. In our study, where more traditional techniques were used, most mothers reported that dental caries were inevitable. On the other hand, education was effective regarding the percentage of mothers who believed that they could prevent their children from dental caries, which was higher than the control group. Reported self-efficacy in the intervention group was higher on oral hygiene, bedtime feeding, and allowing sweet snacks than the control, but the difference was lost by obstacles such as unwillingness of the child and tiredness of the mother. Interference of others such as spouses or mothers-in-law did not affect oral hygiene but was effective on bedtime feeding and sweet snacks. These findings showed that since the whole responsibility in childcare belongs to mothers, other family members do not interfere with hygiene but affect feeding habits. Findings on social support and interpersonal relationships also reflect that mothers are not supported. As a conclusion, it is expected that the results of the intervention group will not be at the desired level in terms of behaviors that had occurred in the last week. Similarly, Naidu et al.[5] identified the involvement of other family members, in particular grandparents, an important barrier to change.
The intervention in this study was mainly focused on providing information and was supported by skill development. Most of the interventions focused on knowledge have been reported not to be very successful.[15,16,17] However, techniques that aim to achieve behavioral change by not only providing knowledge but also taking advantage of psychological approaches do not always produce striking results. For example, Ismail et al.[11] found that families who participated in a randomized study that included mothers watching a DVD with the motivational interview session and a telephone call 7 months after this session did not make a significant difference in behavior in relation to the other group of mothers watching a DVD only. The common point of our study with Ismail et al.'s work is that both are made in real-life conditions and involve extremely poor and high-risk urban mothers. As researchers have pointed out, it is quite difficult to get successful results from interventions conducted on poor individuals. It is quite understandable that oral health is not a top priority for families suffering from multiple stressors.[11] For this reason, the inability to obtain the desired outcome in terms of behaviors in our study depends not only on the technique of intervention but also on the characteristics of the research group. On the other hand, the inadequacy of the “inverse care law,” as described by Hart,[19] is an appropriate approach to prioritizing disadvantaged women so that oral health promotion programs do not have an effect that further enhances inequalities. Also in Macintyre's report on inequalities in Scotland, positively discriminating in favor of both deprived places and deprived people has been nored as an important principle for effective policies to reduce inequalities in health.[20]
The intervention used in this study can be assessed in terms of compliance with other principles for effective policies to reduce inequalities in health. In accordance with the principle “prioritize early years interventions, and families with children,” the program was started when mothers were pregnant. It is also seen that a significant part of the studies that can affect the knowledge, attitudes, and behaviors of the mothers begin in pregnancy.[21,22,23] On the other hand, a large majority of the mothers who participated in the training intervention initiated during pregnancy by Clifford et al.[24] suggested that education should be given at a time when the teeth were a priority agenda, for example, during eruption. For this reason, programs should start early and should be repeated at regular intervals that are in accordance with the child's developmental stage.[25] When another principal to combat inequalities as “recognize need for more intensive support among more socially disadvantaged groups” is taken into consideration, it is seen that the yearly repetition of the program was insufficient. For example, the intervention of Weinstein et al.[6] who studied parents of infants aged 6–18 months from immigrant families in Canada included six follow-up calls and two postcards over a year in addition to an interview session reported a better outcome then less intensive traditional education.
Although integrating oral health education into home visits within the scope of primary health care may provide an important opportunity for more intensive support,[26,27] this could not be achieved due to administrative barriers faced in the program. On the other hand, the concurrence with the social work of municipality midwives, the invitation of mothers by the municipalities, the consultation with the municipal physicians and dentists, and the re-examination according to observations made at each stage was in accordance with the principle of “ensure programs are suitable for the local context.” Finally, as stated in Macintyre's principles, combating inequalities in health necessitates reducing inequalities in life circumstances and prioritizing structural and regulatory barriers.[20] Unfortunately, this study has a limited scope since it does not make any changes to the social determinants of health and the structural causes of inequalities.
In this study, only half of the mothers who participated in the first phase of the intervention attended the third phase and were evaluated for behaviors and their determinants. Mothers with a higher awareness of the importance of oral health may have been more likely to have continued the program, leading to a bias that is more effective than the program in reality. However, when compared with the participants of the first phase,[28] the percentage of having a non-Turkish mother tongue, a husband with education and income level was higher among the participants of the third phase. This difference can be explained by the fact that the motivational effect of gift packages in participating in the program is stronger on the more disadvantaged mothers. In addition, the fact that the control group was slightly more disadvantageous than the intervention group may have led to a higher measurement of the effect of the intervention as another bias source.
Conclusions
An intervention aimed at providing healthy behaviors in mothers was evaluated in this study. We targeted mothers and their children living in deprived places and started during the early years and later developed suitably to the local context. This resulted in the intervention group being at a better level than the control group in terms of behavioral determinants, especially with regard to knowledge. On the other hand, the intervention did not provide more intensive support in this group, which was extremely socially disadvantaged. The absence of an effect on the life circumstances led to a decrease in self-efficacy in the presence of obstacles and ended with a lack of positive attitudes. In the following stages of the program, it was decided to support the mothers in their social environment and to follow strategies that will strengthen their ability to overcome obstacles. However, it should not be forgotten that structural and regulatory policies, which are essential to combat inequalities, should include integrated strategies with primary care and interfere with social determinants of health.
Financial support and sponsorship
The municipalities of Bornova and Konak supported this study.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We would like to thank the municipalities of Bornova and Konak for their organizational and financial support as well as volunteering dentists of the Izmir Dentistry Chamber Community Oral Health Committee for their contributions.
References
- 1.American Academy of Pediatric Dentistry. Policy on Early Childhood Caries (ECC): Classifications, Consequences and Preventve Strategies. American Academy of Pediatric Dentistry. 2014. [Accessed June 1, 2017]. Available from: http://www.aapd.org .
- 2.Peltzer K, Mongkolchati A. Severe early childhood caries and social determinants in three-year-old children from Northern Thailand: A birth cohort study. BMC Oral Health. 2015;15:108. doi: 10.1186/s12903-015-0093-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Finlayson TL, Siefert K, Ismail AI, Sohn W. Psychosocial factors and early childhood caries among low-income African-American children in Detroit. Community Dent Oral Epidemiol. 2007;35:439–48. doi: 10.1111/j.1600-0528.2006.00352.x. [DOI] [PubMed] [Google Scholar]
- 4.Hoeft KS, Barker JC, Shiboski S, Pantoja-Guzman E, Hiatt RA. Effectiveness evaluation of contra caries oral health education program for improving Spanish-speaking parents' preventive oral health knowledge and behaviors for their young children. Community Dent Oral Epidemiol. 2016;44:564–76. doi: 10.1111/cdoe.12250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Naidu R, Nunn J, Irwin JD. The effect of motivational interviewing on oral healthcare knowledge, attitudes and behaviour of parents and caregivers of preschool children: An exploratory cluster randomised controlled study. BMC Oral Health. 2015;15:101. doi: 10.1186/s12903-015-0068-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weinstein P, Harrison R, Benton T. Motivating mothers to prevent caries: Confirming the beneficial effect of counseling. J Am Dent Assoc. 2006;137:789–93. doi: 10.14219/jada.archive.2006.0291. [DOI] [PubMed] [Google Scholar]
- 7.Singhal A, Chattopadhyay A, Garcia AI, Adams AB, Cheng D. Disparities in unmet dental need and dental care received by pregnant women in Maryland. Matern Child Health J. 2014;18:1658–66. doi: 10.1007/s10995-013-1406-7. [DOI] [PubMed] [Google Scholar]
- 8.Vamos CA, Thompson EL, Avendano M, Daley EM, Quinonez RB, Boggess K. Oral health promotion interventions during pregnancy: A systematic review. Community Dent Oral Epidemiol. 2015;43:385–96. doi: 10.1111/cdoe.12167. [DOI] [PubMed] [Google Scholar]
- 9.Ozen B, Ozer L, Başak F, Altun C, Açıkel C. Turkish women's self-reported knowledge and behavior towards oral health during pregnancy. Med Princ Pract. 2012;21:318–22. doi: 10.1159/000334635. [DOI] [PubMed] [Google Scholar]
- 10.Kısa S, Zeyneloǧlu S. Inpatient postpartum women's status of oral hygiene habits and visit to the dentist during their most recent pregnancy. TAF Prev Med Bull. 2013;12:65–74. [Google Scholar]
- 11.Ismail AI, Sohn W, Lim S, Willem JM. Predictors of dental caries progression in primary teeth. J Dent Res. 2009;88:270–5. doi: 10.1177/0022034508331011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Merrick J, Chong A, Parker E, Roberts-Thomson K, Misan G, Spencer J, et al. Reducing disease burden and health inequalities arising from chronic disease among indigenous children: An early childhood caries intervention. BMC Public Health. 2012;12:323. doi: 10.1186/1471-2458-12-323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Raingruber B. Health Promotion Theories. 2nd ed. California: Jones and Barlett Learning; 2017. Contemporary health promotion in nursing practice. [Google Scholar]
- 14.Finlayson TL, Siefert K, Ismail AI, Sohn W. Maternal self-efficacy and 1-5-year-old children's brushing habits. Community Dent Oral Epidemiol. 2007;35:272–81. doi: 10.1111/j.1600-0528.2007.00313.x. [DOI] [PubMed] [Google Scholar]
- 15.Kay E, Locker D. A systematic review of the effectiveness of health promotion aimed at improving oral health. Community Dent Health. 1998;15:132–44. [PubMed] [Google Scholar]
- 16.Ismail AI, Ondersma S, Jedele JM, Little RJ, Lepkowski JM. Evaluation of a brief tailored motivational intervention to prevent early childhood caries. Community Dent Oral Epidemiol. 2011;39:433–48. doi: 10.1111/j.1600-0528.2011.00613.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Watt RG. Strategies and approaches in oral disease prevention and health promotion. Bull World Health Organ. 2005;83:711–8. [PMC free article] [PubMed] [Google Scholar]
- 18.Freudenthal JJ, Bowen DM. Motivational interviewing to decrease parental risk-related behaviors for early childhood caries. J Dent Hyg. 2010;84:29–34. [PubMed] [Google Scholar]
- 19.Hart JT. The inverse care law. Lancet. 1971;1:405–12. doi: 10.1016/s0140-6736(71)92410-x. [DOI] [PubMed] [Google Scholar]
- 20.Macintyre S. Inequalities in Health in Scotland: What Are They and What Can We Do About Them? Medical Research Council; 2007. [Accessed November 10, 2018]. Available from: http://www.sphsu.mrc.ac.uk/reports/OP017.pdf . [Google Scholar]
- 21.Boggess KA, Urlaub DM, Moos MK, Polinkovsky M, El-Khorazaty J, Lorenz C. Knowledge and beliefs regarding oral health among pregnant women. J Am Dent Assoc. 2011;142:1275–82. doi: 10.14219/jada.archive.2011.0113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Medeiros PB, Otero SA, Frencken JE, Bronkhorst EM, Leal SC. Effectiveness of an oral health program for mothers and their infants. Int J Paediatr Dent. 2015;25:29–34. doi: 10.1111/ipd.12094. [DOI] [PubMed] [Google Scholar]
- 23.Schroth RJ, Edwards JM, Brothwell DJ, Yakiwchuk CA, Bertone MF, Mellon B, et al. Evaluating the impact of a community developed collaborative project for the prevention of early childhood caries: The healthy smile happy child project. Rural Remote Health. 2015;15:3566. [PubMed] [Google Scholar]
- 24.Clifford H, Johnson NW, Brown C, Battistutta D. When can oral health education begin? Relative effectiveness of three oral health education strategies starting pre-partum. Community Dent Health. 2012;29:162–7. [PubMed] [Google Scholar]
- 25.Plutzer K, Spencer AJ. Efficacy of an oral health promotion intervention in the prevention of early childhood caries. Community Dent Oral Epidemiol. 2008;36:335–46. doi: 10.1111/j.1600-0528.2007.00414.x. [DOI] [PubMed] [Google Scholar]
- 26.Hamilton FA, Davis KE, Blinkhorn AS. An oral health promotion programme for nursing caries. Int J Paediatr Dent. 1999;9:195–200. doi: 10.1046/j.1365-263x.1999.00132.x. [DOI] [PubMed] [Google Scholar]
- 27.Chung LH, Gregorich SE, Armitage GC, Gonzalez-Vargas J, Adams SH. Sociodemographic disparities and behavioral factors in clinical oral health status during pregnancy. Community Dent Oral Epidemiol. 2014;42:151–9. doi: 10.1111/cdoe.12075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Usturalı Mut AN, Öcek ZA, Yücel U, Çiçeklioǧlu M, Eden E. The Dental Service Needs of Pregnant Women Living in Izmir-Bornova and Socioeconomic Variables Related to The Utilization of These Services. Dokuz Eylül Tıp Fak Derg. 2014;23:93–103. [Google Scholar]