Background:
Insertional Achilles tendinopathy causes posterior heel pain at the insertion of the Achilles tendon, often in combination with a calcaneal exostosis, or Haglund deformity. Insertional Achilles tendinopathy often presents with a posterior osseous prominence and leads to calcification of the Achilles tendon1. Nonoperative treatment of these conditions includes activity modification, nonsteroidal anti-inflammatory agents, heel lifts, shoe modification, physical therapy focused on eccentric strengthening exercises, iontophoresis, and shock wave therapy. Nonoperative treatment will fail in approximately 50% of these cases, and such patients become candidates for surgical intervention2,3. Multiple surgical approaches have been described, including the medial J-shaped, lateral, Cincinnati transverse, double incision, and central-splitting approaches4. Currently, there is no consensus regarding the ideal approach. Recent literature has suggested that the central-splitting approach allows for adequate exposure of both the most commonly diseased area of the tendon and the calcaneal exostosis, with excellent postoperative pain and functional results5-13.
Description:
Place the patient in the prone position with the feet at the edge of the operating table. Make a full-thickness, 5 to 7-cm longitudinal incision centered over the Achilles tendon and the posterior aspect of the calcaneus. Make a central incision through the Achilles tendon. Sharply mobilize the medial and lateral slips and excise the diseased portion of the Achilles tendon. Expose the calcaneal exostosis and perform the calcaneal exostectomy with a microsagittal saw. Repair the remaining healthy-appearing Achilles tendon to the calcaneus with 2 suture anchors. An additional suture anchor or, alternatively, the double-row technique for the Achilles tendon repair may be used. Repair the central split in the Achilles tendon with absorbable suture. Close the soft tissue and skin in layers.
Alternatives:
Alternative approaches include the medial, lateral, or Cincinnati transverse incisions. The central-splitting approach is favored because of the excellent exposure of both the diseased tendon and the calcaneal exostosis. Additional augmentations to this procedure include a flexor hallucis longus transfer and a gastrocnemius recession.
Rationale:
This technique provides adequate exposure to the diseased Achilles tendon, calcific deposits, and calcaneal exostosis. Recent studies have demonstrated it to be a safe and effective technique with high patient-satisfaction scores5-13.
Introductory Statement
The central-splitting approach for surgical treatment of insertional Achilles tendinopathy and Haglund deformity provides adequate exposure to the most commonly diseased area of the tendon and to the calcaneal exostosis, with excellent postoperative pain and functional results.
Indications & Contraindications
Indications
Chronic calcific insertional Achilles tendinopathy refractory to conservative treatment over a course of 3 to 6 months (Figs. 1 and 2).
Fig. 1.

Preoperative lateral radiograph of the right foot showing calcific Achilles tendinopathy and Haglund deformity.
Fig. 2.

Photograph of the foot with the patient in the prone position, the knee slightly flexed, and a tourniquet applied.
Contraindications
Insertional Achilles tendinopathy without failed nonoperative treatment.
Peripheral vascular disease with substantial lower extremity ischemia.
Uncontrolled diabetes.
Patient medically unfit for a surgical procedure.
Step-by-Step Description of Procedure (Video 1)
Step 1: Positioning
Position the patient in the prone position with the feet at the edge of the operating table.
Place the patient prone with the feet at the edge of the operating table.
Place a thigh tourniquet on the operative extremity.
Pad the chest, pelvis, and upper extremities and protect the genitalia.
Place a pad under the knees and a pillow under the legs, stopping at the ankle to allow for dorsiflexion and plantar flexion (Figs. 3 and 4).
Fig. 3.

Posteroanterior photograph of the foot showing the Haglund deformity.
Fig. 4.

Lateral photograph of the foot showing the Haglund deformity.
Video 1.
Video showing the complete surgical procedure utilizing the central-splitting approach and the double-row technique for Achilles repair.
Step 2: Incision and Exposure
Make a central incision approximately 5 to 7 cm in length over the Achilles tendon and the posterior aspect of the calcaneus.
Identify the medial and lateral borders of the Achilles tendon and calcaneus. Plan a longitudinal incision centrally over the Achilles tendon and approximately 5 to 7 cm in length (Fig. 5).
Using a scalpel, make a full-thickness longitudinal incision centered over the Achilles tendon and posterior aspect of the calcaneus (Fig. 6).
Identify the paratenon and the Achilles tendon and sharply develop a longitudinal central split through the diseased tendon. Carry the split down to bone (Fig. 7).
Elevate the medial and lateral slips of the tendon at the calcaneal insertion, starting centrally and moving peripherally. Elevate enough to adequately expose the entire diseased tendon. Although some authors suggest that 50% to 70% of the Achilles tendon can be released without the need for reattachment, we prefer to repair the Achilles tendon to the calcaneal insertion (Fig. 8).
Fig. 5.

Photograph showing the incision marked centrally over the Achilles tendon.
Fig. 6.

Photograph showing the central full-thickness incision being made.
Fig. 7.
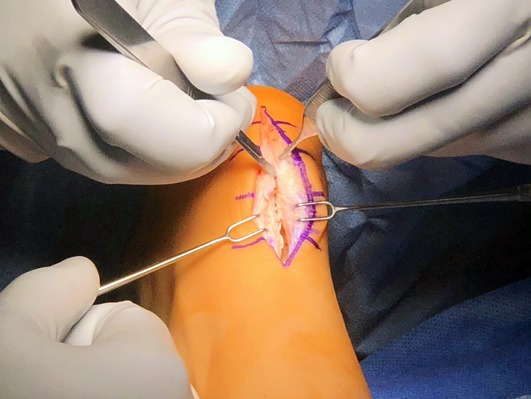
Photograph showing the central split being made through the Achilles tendon.
Fig. 8.
Photograph showing the elevated medial and lateral slips.
Step 3: Debridement of the Diseased Tendon and Exposure of the Calcaneal Exostosis
Debride the diseased tendon and remove the calcific portions.
Debride the diseased portion of the Achilles tendon. If >50% of the tendon is debrided, a flexor hallucis longus transfer may be used to augment the repair.
Remove the calcific portions of the diseased tendon.
Place a retractor on each side of the calcaneus to protect the remaining Achilles tendon.
Debride the remaining posterior fat pad overlying the calcaneus to allow adequate exposure of the Haglund deformity (Fig. 9).
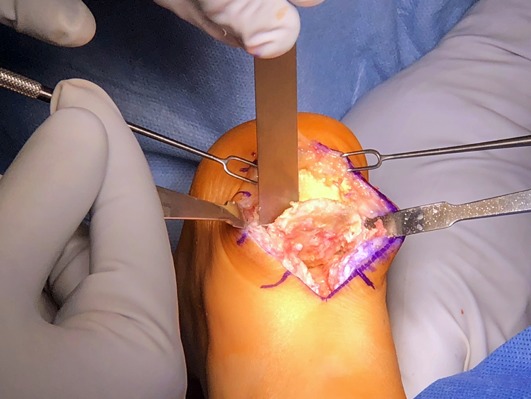
Fig. 9.
Photograph showing the debridement of the diseased tendon and any calcific deposits.
Step 4: The Calcaneal Exostectomy
Perform the calcaneal exostectomy using a microsagittal saw.
Place retractors on the medial and lateral borders of the calcaneus to protect the overlying skin and Achilles tendon.
Perform the calcaneal exostectomy obliquely from distal to proximal with a microsagittal saw (Figs. 10 and 11). Fluoroscopy can be used to help perform the osteotomy.
An osteotome may be used to elevate the osseous fragment, which should be roughly the size of a quarter (25 mm in diameter, 2-mm thickness) (Fig. 12).
Remove the bone fragment with a rongeur.
Using a high-speed rasp or the microsagittal saw, smooth out the osseous prominences (Fig. 13).
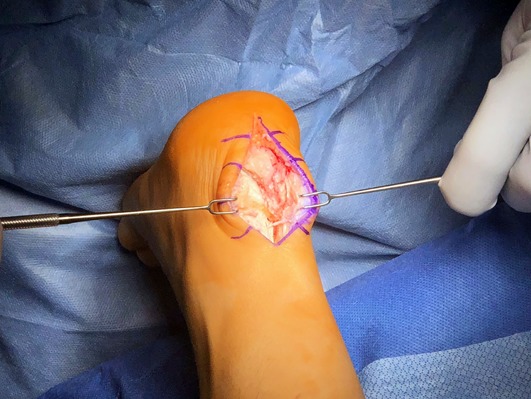
Fig. 10.
Photograph showing the calcaneal exostectomy being performed.
Fig. 11.

Photograph showing the oblique angle of the calcaneal exostectomy.
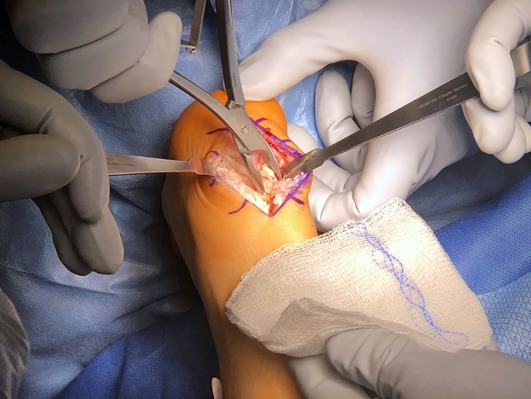
Fig. 12.
Photograph showing the elevation of the bone fragment with an osteotome. The bone fragment is roughly the size of a quarter.
Fig. 13.

Photograph showing the calcaneal insertion site of the Achilles tendon after all osseous prominences have been removed.
Step 5: Repair the Achilles Tendon (Single-Row Technique)
We prefer to repair the remaining Achilles tendon with suture anchors placed into the calcaneus.
Place two 4.5-mm Corkscrew suture anchors (Arthrex) medially and laterally in the calcaneus and test the stability of the anchors by pulling up on the sutures (Fig. 14).
Using a free needle, pass each suture through the tendon in a horizontal mattress fashion.
Balance the tension of the suture anchors and reposition the sutures if necessary (Fig. 15).
Tie each suture and repair the remaining Achilles tendon to the calcaneus.
We recommend an additional suture anchor be placed centrally and distal to the first 2 suture anchors in order to strengthen the repair.
After testing the stability, pass each suture through the distal portion of the tendon in a horizontal mattress fashion. Tie the remaining sutures to reapproximate the distal portion of the tendon to the calcaneus (Fig. 16).
Repair the central split in the tendon with number-0 Vicryl suture (Ethicon) in a simple interrupted fashion with buried knots (Fig. 17).
Radiographs may be made to evaluate anchor placement and boney resection (Fig. 18).
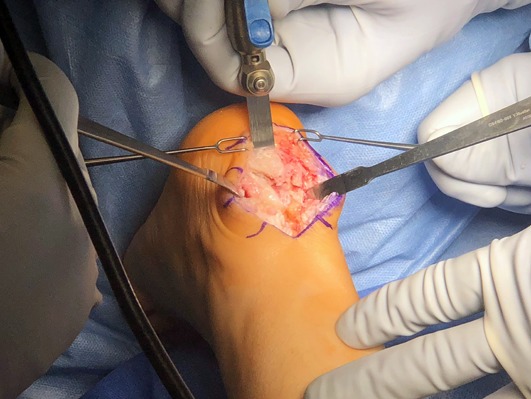
Fig. 14.
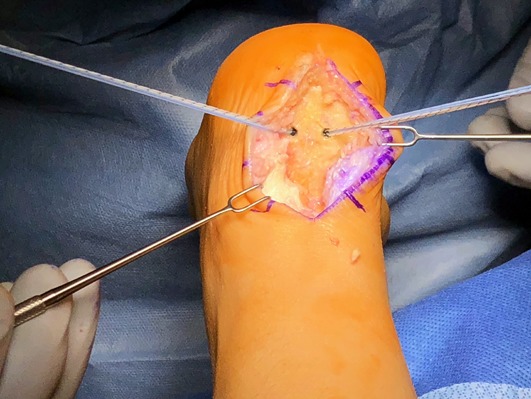
Photograph showing the placement of the two 4.5-mm Corkscrew anchors symmetrically into the calcaneus.
Fig. 15.
Photograph showing the tension of the suture anchors being balanced.
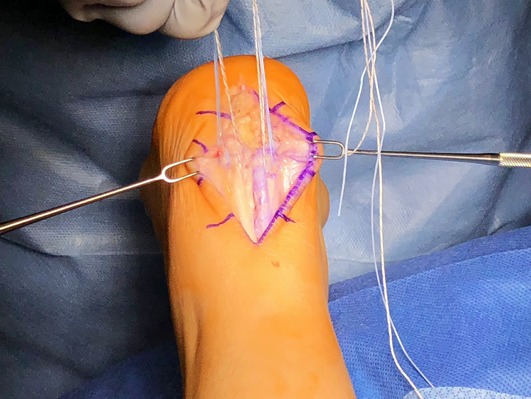
Fig. 16.

Photograph showing an additional suture anchor being placed centrally, which may be done to augment the reattachment of the 2 tendon slips.
Fig. 17.

Photograph showing the completely repaired Achilles tendon.
Fig. 18.

Postoperative lateral radiograph of the foot showing the calcaneal exostectomy with 3 suture anchors placed in the posterior aspect of the calcaneus.
Step 5: Repair the Achilles Tendon (Optional Double-Row Technique)
Repair the remaining Achilles tendon with suture anchors placed into the calcaneus.
Place 2 FiberTak suture anchors (Arthrex) medially and laterally in the calcaneus and test the stability of the anchors by pulling up on the sutures.
Using a free needle, pass each suture symmetrically into the tendon in a horizontal mattress fashion.
Tie each suture to secure the medial and lateral portions of the Achilles tendon to the calcaneus.
Repair the central tendon split with number-0 Vicryl suture in a simple interrupted fashion with buried knots.
Perform the double-row technique by taking 1 suture limb from the medial anchor and pairing it with a suture limb from the lateral anchor. Pair the 2 remaining suture limbs, with 1 from the medial suture anchor crossing 1 from the lateral suture anchor to create an X.
Pull the paired suture limbs distally to determine the amount of tension on the Achilles tendon. This is typically 1.5 to 2 cm distal to the FiberTak anchor location.
Repair the distal row to the calcaneus using two 4.5-mm PushLock anchors (Arthrex).
Cut the sutures flush to the tendon.
Step 6: Closure
Close the remaining soft tissues.
Close the paratenon with 2-0 absorbable suture.
Close the subcutaneous layer with 3-0 absorbable suture.
Close the skin with 3-0 nylon sutures.
Step 7: Postoperative Protocol
The patient should be non-weightbearing for 4 weeks.
Weeks 0 to 2: the patient should be non-weight-bearing with the ankle in a posterior splint in the resting positioning (25° of ankle plantar flexion). Sutures are removed at 2 weeks.
Weeks 2 to 4: non-weight-bearing in a controlled ankle-motion boot with a heel lift. Start gentle active ankle range-of-motion exercises.
Weeks 4 to 6: advance to weight-bearing as tolerated in a controlled ankle-motion boot with a heel lift.
Weeks 6 to 8: remove the heel lift and continue weight-bearing as tolerated in a controlled ankle-motion boot. Begin formal physical therapy.
Week 8: transition to regular walking shoes.
Results
Several approaches for the operative treatment of insertional Achilles tendinopathy and Haglund deformity have been described in the literature, including a vertical J-shaped medial or lateral, the Cincinnati transverse, a double incision, or a central-splitting approach, as described in the present article4-13. Although no consensus has been reached regarding the best approach, recent literature has suggested that the central-splitting approach is safe and effective5-15.
McGarvey et al. originally described the central-splitting technique in a series of 22 cases and reported comparable results to other approaches with regard to return to work/activity (91%) and patient satisfaction rate (82%)7. Nunley et al. reported a satisfaction rate of 96% at 7 years after operative treatment with a central-splitting approach. In the same study, isokinetic testing was performed to compare the operative and nonoperative limbs, and no significant differences were found10. In a recent study, Ahn et al. reported that the use of a central-splitting approach led to improved American Orthopaedic Foot & Ankle Society hindfoot scores (from 62.1 ± 7.5 to 92.5 ± 3.5) and Victorian Institute of Sport Assessment-Achilles scores (from 53.2 ± 7.4 to 89.6 ± 3.4) at a mean follow-up of 3.5 years. Although the study was limited to only 15 patients, all patients were satisfied and stated they would undergo the procedure again. The authors reported no substantial complications, such as wound breakdown, Achilles tendon rupture, infection, or spur recurrence9. These results are in slight contrast to those in the study by McGarvey et al., in which there were 6 scar-related issues, 2 involving hypersensitivity and 4 involving numbness, as well as 1 superficial infection that resolved with oral antibiotics7. Although no surgical procedure is without risks, the central-splitting approach appears to be safe and yields satisfactory results in the operative treatment of insertional Achilles tendinopathy and Haglund deformity.
Pitfalls & Challenges
Soft-tissue handling is very important during this procedure. Small 2-prong retractors are used to gently retract the superficial soft tissues. A full-thickness incision through the skin and subcutaneous tissue is recommended.
When sharply elevating the Achilles tendon at the calcaneal insertion, be sure to elevate every fiber off the original insertion on the calcaneus. Elevating the tendon off only the posterior enthesophyte can lead to shortening of the tendon. Use a skin rake to evert the tendon to help with excision of the deeper fibers directly off the insertion.
Diseased tendon and healthy tendon may be difficult to distinguish intraoperatively. Tactile and visual sensations can be used to help differentiate diseased tendon from normal tendon. Diseased tendon is yellowish in appearance, is friable, and feels rubbery to touch; in addition, it often houses calcific deposits. Healthy tendon is characterized by organized, longitudinally oriented fibers with a shiny white appearance and a firm feel to the touch6.
If >50% of the Achilles tendon is debrided, a flexor hallucis longus transfer may be used to augment the repair.
When performing the calcaneal exostectomy, ensure that an oblique saw cut is made. There is a tendency to make the bone cut too parallel to the plantar aspect of the foot, which risks cutting into the posterior facet of the calcaneus. Intraoperative fluoroscopy may be used to achieve proper orientation.
A high-speed rasp can be used to smooth down the osteophytes around the medial, lateral, and distal edges of the calcaneus.
If the patient has an equinus contracture, it is our preference to perform a gastrocnemius recession to relieve stress on the Achilles repair.
Published outcomes of this procedure can be found at: J Foot Ankle Surg. 2015 Nov-Dec;54(6):1053-6.
Investigation performed at The Hughston Clinic, Columbus, Georgia; and the Jack Hughston Memorial Hospital, Phenix City, Alabama
Disclosure: The authors indicated that no external funding was received for any aspect of this work. The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJSEST/A288).
References
- 1.Den Hartog BD. Insertional Achilles tendinosis: pathogenesis and treatment. Foot Ankle Clin. 2009. December;14(4):639-50. [DOI] [PubMed] [Google Scholar]
- 2.Roche AJ, Calder JDF. Achilles tendinopathy: a review of the current concepts of treatment. Bone Joint J. 2013. October;95-B(10):1299-307. [DOI] [PubMed] [Google Scholar]
- 3.Kang S, Thordarson DB, Charlton TP. Insertional Achilles tendinitis and Haglund’s deformity. Foot Ankle Int. 2012. June;33(6):487-91. [DOI] [PubMed] [Google Scholar]
- 4.Carmont MR, Maffulli N. Management of insertional Achilles tendinopathy through a Cincinnati incision. BMC Musculoskelet Disord. 2007. August 15;8:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schepsis AA, Wagner C, Leach RE. Surgical management of Achilles tendon overuse injuries. A long-term follow-up study. Am J Sports Med. 1994. Sep-Oct;22(5):611-9. [DOI] [PubMed] [Google Scholar]
- 6.Easley MM, DeOrio MJ. Insertional Achilles tendinopathy. In: Operative techniques in orthopaedic surgery. Wiesel SW. 2nd ed. Philadelphia: Wolters Kluwer; 2016. p 5007-16. [Google Scholar]
- 7.McGarvey WC, Palumbo RC, Baxter DE, Leibman BD. Insertional Achilles tendinosis: surgical treatment through a central tendon splitting approach. Foot Ankle Int. 2002. January;23(1):19-25. [DOI] [PubMed] [Google Scholar]
- 8.Leduc S, Walling AK. Posterior midline approach for treatment of Achilles calcific insertional tendonopathy. Tech Foot Ankle Surg. 2010;9(4):217-20. [Google Scholar]
- 9.Ahn JH, Ahn CY, Byun CH, Kim YC. Operative treatment of Haglund syndrome with central Achilles tendon-splitting approach. J Foot Ankle Surg. 2015. Nov-Dec;54(6):1053-6. Epub 2015 Jul 29. [DOI] [PubMed] [Google Scholar]
- 10.Nunley JA, Ruskin G, Horst F. Long-term clinical outcomes following the central incision technique for insertional Achilles tendinopathy. Foot Ankle Int. 2011. September;32(9):850-5. [DOI] [PubMed] [Google Scholar]
- 11.Johnson KW, Zalavras C, Thordarson DB. Surgical management of insertional calcific Achilles tendinosis with a central tendon splitting approach. Foot Ankle Int. 2006. April;27(4):245-50. [DOI] [PubMed] [Google Scholar]
- 12.Paavola M, Kannus P, Orava S, Pasanen M, Järvinen M. Surgical treatment for chronic Achilles tendinopathy: a prospective seven month follow up study. Br J Sports Med. 2002. June;36(3):178-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Calder JD, Saxby TS. Surgical Treatment of Insertional Achilles Tendinosis. Foot Ankle Int. 2003. February;24(2):119-121. [DOI] [PubMed] [Google Scholar]
- 14.Wagner E, Gould J, Bilen E, Fleisig GS, Wilk K, Fowler R. Change in plantarflexion strength after complete detachment and reconstruction of the Achilles tendon. Foot Ankle Int. 2004. November;25(11):800-4. [DOI] [PubMed] [Google Scholar]
- 15.Holmes GB, Lin J. Etiologic factors associated with symptomatic Achilles tendinopathy. Foot Ankle Int. 2006. November;27(11):952-9. [DOI] [PubMed] [Google Scholar]


