Abstract
Patient: Female, 51-years-old
Final Diagnosis: Choanal polyp with osseous metaplasia
Symptoms: Nasal obstruction
Medication:—
Clinical Procedure: Combined surgical approach, endoscopic and trans-oral
Specialty: Otolaryngology
Objective:
Rare co-existance of disease or pathology
Background:
Osseous metaplasia is a heterotopic normal bone in soft tissues. It is occasionally found in mucosal polyps of the external auditory canal, tongue, gut, stomach, nasal cavity, and uterus. Choanal polyp with osseous metaplasia originating from the lateral wall of the nasopharynx has not been previously reported. In fact, osseous metaplasia in nasal polyps represents a very uncommon histological finding with only 12 cases described in the literature.
Case Report:
We reported here, the clinical, radiological, and therapeutic management of a nasopharynx choanal polyp in a patient with severe nasal obstruction and rhinolalia history. Endoscopic examination of nasal cavities revealed a polypoid-like mass in the left nasal fossa, extending to the choanal area and nasopharynx. Computed tomography scan and contrast-enhanced magnetic resonance imaging confirmed the presence of a solitary and lobulated mass in the choanal area and nasopharynx. We performed the removal of the mass through careful hemostasis of left sphenopalatine artery using both transnasal and transoral paths, with no complications for the patient. Histopathological examination of the biopsy revealed a benign inflammatory polyp with osseous metaplasia. No recurrence was noted 24 months after surgery.
Conclusions:
The incidence of ossifying areas in nasal polyps is very low, with only 12 cases reported in the literature. Ossifying polyps originating from the lateral wall of nasopharynx has never been reported before. The use of a combined endoscopic and transoral surgical approach was shown to be reliable in terms of adequate exposure and visualization of the lesion, control of bleeding, and complete removal of the mass.
MeSH Keywords: Bone Neoplasms, Metaplasia, Nasal Polyps, Nasopharyngeal Neoplasms
Background
Osseous metaplasia (OM) is a rare condition that has been reported to be present in only a few cases of mucosal polyps located in the external auditory canal, tongue, gut, stomach, nasal cavity and uterine cervix [1]. Moreover, this alteration has not only been observed in patients with osteoma and ossifying fibroma, but, also in patients with inverted papilloma and esthesioneuroblastoma [2–6]. Furthermore, rare cases with osseous metaplasia in the sinonasal tract have been described [2–6]. In particular, only 12 patients have been found with osseous metaplasia in nasal polyps originating from the ethmoid sinus, middle turbinate, inferior turbinate, nasal septum, or middle meatus [7].
To the best of our knowledge, choanal polyp with osseous metaplasia has never been previously reported in the lateral wall of the nasopharynx. Here, we describe, for the very first time, a clinical case of a choanal polyp with osseous metaplasia arising from lateral wall of rhinopharynx that was successfully managed with no recurrence of the disease after 2 years from the surgical procedure.
Case Report
A 51-years-old female with a history of severe nasal obstruction associated to rhinolalia, was observed in May of 2016. Rhinofiberoptic endoscopy using a flexible instrument showed a mass resembling a polypoid formation in the left nasal cavity, which was also extended to the entire choanal area and nasopharynx. No abnormalities of the mass surface were noted. Interestingly, even though the nasal sinuses seemed normal, computed tomography (CT) scans showed the presence of a solitary and lobulated mass with clustered radio-dense material, suggesting a possible ossification in the area. In particular, from the CT images the mass seemed to be originating from the left inferior turbinate, reaching the posterior part of the left nasal cavity and extending to both the nasopharynx and the right posterior choana (Figure 1). Contrast-enhanced magnetic resonance imaging (MRI) confirmed the presence of the mass in both the nasopharynx and choanal area suggesting that the possible origin of the lesion was the nasopharynx. Moreover, the imaging showed a calcific aspect within the mass and low contrast enhancement (Figure 2). Due to the size of the mass, only during the surgical procedure was it possible to identify the exact site of origin of the lesion within the nasopharynx.
Figure 1.
Computed tomography scan, sagittal plane: solitary, lobulated mass with clustered radio dense material, suggesting ossification. The mass filled the posterior part of left nasal fossa and extended to the nasopharynx.
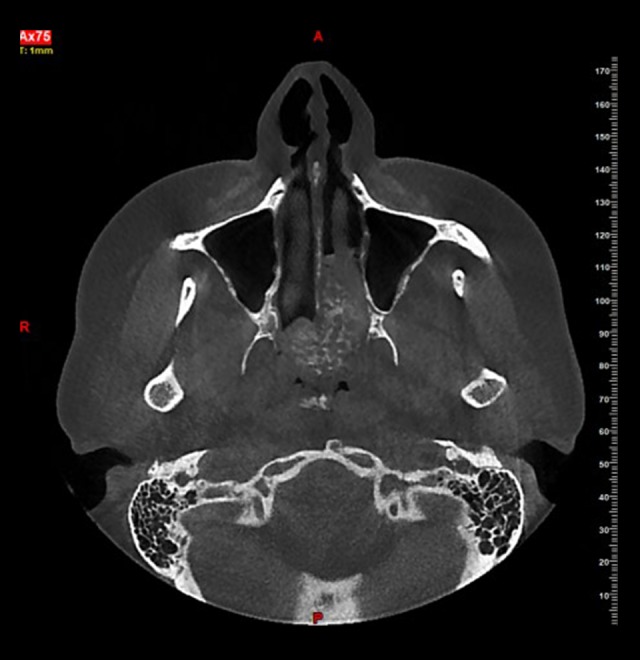
Figure 2.

Magnetic resonance imaging with contrast, axial plane: presence of the mass in left choana, that appears to be originated from rhinopharynx with calcific aspect. Low enhancement after contrast medium injection.
Surgical approach
Surgery for the patient was performed under general anesthesia. A medicated tampon with xylocaine 1% and epinephrine 1/100 000 was kept in place for 10 minutes. Then, in order to expose the mass, we performed an endoscopic resection of the left inferior turbinate. The left sphenopalatine foramen was visualized with cauterization of sphenopalatine artery. Subsequently, a transoral T-incision of the soft palate made access possible to the left lateral wall of the nasopharynx revealing the base of the lesion. Thereafter, the mass was completely and successfully removed. The surgical incision was sutured with Vicryl 4.0, and a nasal pack was positioned in both nasal cavities. Macroscopically, the mass was a hard polypoid specimen, 5×3×2 cm in size and white-grey in color and firm in consistence (Figure 3). The tissue section revealed it was diffusely calcific. Microscopically, the histological analysis revealed that the specimen was covered by respiratory epithelium, constituted by loose connective tissue with trabeculae of mature bone in the subepithelial chorion, and diffuse calcifications were located in the loose stroma together with chronic inflammatory infiltrates and some plasma cells; eosinophils were absent. Immunohistochemical investigation (S100, p63, SOX10) were not positive. Moreover, respiratory glandular elements with some cystic dilatations were found (Figure 4).
Figure 3.

Surgical specimen, 5×3×2 cm.
Figure 4.

Histological findings, the arrows show mature bone areas in the subepithelial chorion, organized in trabeculae. Within the trabeculae is interposed some stroma.
There were no postoperative complications and no recurrence of the disease at 24 months after surgery.
Discussion
Nasal polyps with osseous metaplasia are extremely rare [3]. Two possible theories have been proposed to explain the mechanism involved in the ossification of polyps: bone morphogenetic proteins (BMPs), and post-traumatic or post-surgery [4–8]. In particular, a potential role of BMP-4 in polyp ossification has been reported, even though it has been shown that TGFβ-1 and BMP-7 synergic action induces bone formation [4–8]. The osteoblasts differentiation is divided into 2 stages. In the first stage, some undifferentiated mesenchymal cells may differentiate into osteogenic progenitors when stimulated by appropriate growth factors within sinonasal polyps [4–8]. During the second stage, osteoblast progenitors become osteoblast cells ready to produce bone tissue [4–8]. The second theory suggests that ossification within polyps could originate from bones left behind during prior surgery or trauma [4,9]. The incidence of ossifying areas in nasal polyps is very low, with only 12 case have been reported (Table 1). Ossifying polyps have been described to arise from the middle turbinate, inferior turbinate, maxillary sinus, ethmoid and superior turbinate, with the most common origin in the posterior portion of the nasal septum [1–18]. Interestingly, ossifying polyps originating from the lateral wall of nasopharynx have not previously been reported. The accurate radiological examination of metaplastic ossifying polyps is useful and essential to identify not only calcifications, but also surrounding tissues patterns and erosions [9]. While polyps generally present with iso-density and a lobulated shape on CT imaging, osseous metaplasia appears to have multiple clustered densities with bony cortical and medullary cavities in the center of the polyp [15]. Usually, a diffuse process of ossification with defined margins is a benign fibroosseous type of lesions [15,16]. On the other side, poorly defined margins have been reported to be present in sarcomas or metastatic undifferentiated carcinomas [5,16]. On MRI images, normal polyps show hypo-intensity on T1WI and hyper-intensity on T2WI with marginal and septal enhancement on T1WI [4,5]. The ossification process generally shows a moderate enhancement after administrating gadolinium [4]. In opposite to normal polyps, the ones in which the ossification process has already started show thin hypo-intensity on both T1WI and T2WI in the peripheral zone of ossification, corresponding to the bony cortices [4]. Instead, ossifying polyps in the central zone exhibit mostly hyper-intensity on both T1WI and T2WI images, as an adipose component of the medullary cavities [3,4,12]. The bone tissue within a mass of nasal polyps needs a careful clinical diagnosis, since it can be associated with pathologies like rhinolith, mycetoma, inverted papilloma with calcifications, chondrosarcoma, osteosarcoma, and fibro-osseous lesions, which can mimic nasal polyps with osseous metaplasia on CT scans [3–12]. Particularly, rhinolith and sinolith are calcareous concretion derived from a deposition of salts in the nose and paranasal sinuses, a condition that may be associated to nasal polyps [17]. On the other hand, sinonasal mycetoma typically appears on CT scans as a hyper-attenuating lesion in most cases containing centrally located punctate, linear, or nodular calcifications [17]. Mycetoma usually shows marked diffuse hypo-intensity on T2-weighted images that do not enhance after injection of gadolinium; this condition is helpful in the diagnostic process in case of doubtful CT scans images [15]. Furthermore, fungal rhino sinusitis might show areas of ossification with an unclear and undefined trabecular pattern [15]. Inverted papilloma, which generally originates from the lateral nasal wall, may have calcifications as well as a bone destruction pattern which could be associated to polypoid changes [15]. Differential diagnosis between chondrosarcoma and nasal polyps with metaplastic ossification may be difficult because of the presence of multiple calcifications in the soft tissue mass on CT scans [15]. Chondrosarcoma located in the nasal cavity is found in the cartilaginous nasal septum presenting a marginal bone erosion [15]. CT scans of osteosarcoma present radiodensities diffusely distributed within the mass with focal bone destruction and a periosteal reaction such a “sunburst” aspect [15]. Fibro-osseous lesions are located at the center of the mass [15]. On CT scans, radiodensities associated with fibro-osseous lesions are well defined and distributed diffusely within the mass [15]. In most cases, 2 main surgical approaches are advised: endoscopic and transoral [15]. In particular, for larger and harder masses the transoral approach is preferred, with a low recurrence rate after years from surgery [15]. Chondroosseous respiratory epithelial adenomatoid hamartoma (COREAH) is an epithelial hamartoma with proliferation of glandular tissue, rare benign entity of sinonasal tract with 12 cases reported in literature. On CT scans, it appears as a polypoid mass with a central core of high-density not enhancing with contrast. On MRI images it has a heterogenous T2 hyperintensity and T1 hypo-intensity with cerebriform appearance after gadolinium contrast [19].
Table 1.
Ossifying polyps of the nasal cavity and paranasal sinuses reported in literature.
| Authors | Site of involvement | Treatment |
|---|---|---|
| De Vries N, 1988 [11] | Anterior-posterior ethmoid | Endonasal |
| Jacono AA et al., 2001 [8] | Nasal septum | Endonasal+transoral |
| Ramachandran K et al., 2005 [1] | Middle turbinate | Endonasal+transoral |
| Moyano JAM et al., 2007 [7] | Maxillary sinus | Endonasal |
| Kim YK et al., 2010 [15] | Nasal septum | Endonasal+transoral |
| Ylmaz M et al., 2012 [2] | Maxillary sinus | Endonasal |
| Mercan H et al., 2012 [18] | Posterior part of nasal cavity | Endonasal |
| Shafii M et al., 2013 [6] | Inferior turbinate | Endonasal |
| Lee DH et al., 2013 [9] | Nasal cavity | Endonasal |
| Lam JWK et al., 2016 [12] | Superior turbinate | Endonasal+transoral |
| Cho IY et al., 2016 [14] | Nasal septum | Endonasal+transoral |
| Promsopa C, 2016 [3] | Nasal septum | Endonasal+transoral |
| Testa D et al., 2019 | Lateral wall of rhinopharynx | Endonasal+transoral |
Interestingly, in the described case, the mass seemed to be linked to the left inferior turbinate and therefore, we decided to perform the endoscopic left inferior turbinate resection. Since the mass was large in size, we choose also transoral approach and we found that the lesion was linked to the left lateral wall of nasopharynx. The histological analysis revealed the unexpected presence of mature bone trabeculae in the sub-epithelial chorion and diffuse calcifications in the stroma.
Conclusions
Osseous metaplasia is an extremely rare finding in nasal polyposis. Radiological examination represents the only tool to individuate an ossification within polyps in a preoperative staging. Different metaplastic lesions with osseous metaplasia are well known in the sinonasal tract. CT scans and MRIs are essential for a preoperative differential diagnosis in order to discriminate any characteristics of lesion malignancy. The use of a combined surgical approach, endoscopic and transoral, allow adequate exposure and visualization of the lesion, control of bleeding, and thus, a complete removal of the mass [1,3,8,12–15]. After surgery, a histologic assessment performed on all surgical specimens helps give a definitive diagnosis.
Footnotes
Conflict of interest
None.
References:
- 1.Ramachandran K, Thomas MA, Denholm RB. Osseous metaplasia of a nasal polyp. J Otolaryngol. 2005;34(1):72–73. doi: 10.2310/7070.2005.04007. [DOI] [PubMed] [Google Scholar]
- 2.Yilmaz M, Ibrahimov M, Kilic E, Ozturk O. Heterotopic bone formation (osseous metaplasia) in nasal polyps. J Craniofac Surg. 2012;23(2):620. doi: 10.1097/SCS.0b013e3182420592. [DOI] [PubMed] [Google Scholar]
- 3.Promsopa C. Septochoanal polyp with osseous metaplasia: A case report. J Med Case Rep. 2016;10(1):149. doi: 10.1186/s13256-016-0952-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yang BT, Wang YZ, Sun FR, Dong JY. Ossifying inverted papilloma and ossifying polyp of the sinonasal tract: Comparison of CT and MRI features. Clin Radiol. 2017;72(1):84–90. doi: 10.1016/j.crad.2016.09.018. [DOI] [PubMed] [Google Scholar]
- 5.Som PM, Lidov M. The significance of sinonasal radiodensities: Ossification, calcification, or residual bone? Am J Neuroradiol. 1994;15(5):917–22. [PMC free article] [PubMed] [Google Scholar]
- 6.Shafii M, Saatian M, Aliehyai F, et al. Nasal polyp with heterotopic bone formation (osseous metaplasia): A case report. Galem Medical Journal. 2013;2(2):80–82. [Google Scholar]
- 7.Moyano JAM, Cantero AN, Iniesta FJG, et al. Metaplastic ossification in nasal polyp. Acta Otorrinolaringol (English Edition) 2007;58(6):276–77. [PubMed] [Google Scholar]
- 8.Jacono AA, Sclafani AP, Van De Water T, et al. Metaplastic bone formation in nasal polyps with histologic presence of transforming growth factor beta-1 (TGFbeta-1) and bone morphogenetic proteins (BMPs) Otolaryngol Head and Neck Surg. 2001;125(1):96–97. doi: 10.1067/mhn.2001.115857. [DOI] [PubMed] [Google Scholar]
- 9.Lee DH, Choi HS, Lee JJW, Lim SC. Nasopharynx obstruction by huge nasal polyp with metaplastic ossification. J Rhinol. 2013;20(2):136–38. [Google Scholar]
- 10.Mesolella M, Galli V, Testa D. Inferior turbinate osteoma: A rare cause of nasal obstruction. Otolaryngol Head and Neck Surg. 2005;133(6):989–91. doi: 10.1016/j.otohns.2005.03.045. [DOI] [PubMed] [Google Scholar]
- 11.De Vries N. New bone formation in nasal polyps. Rhinology. 1998;26(3):217–19. [PubMed] [Google Scholar]
- 12.Lam JWK, Lau LL. Nasal polyp with osseous metaplasia. Ear Nose Throat J. 2016;95(4/5):144. [PubMed] [Google Scholar]
- 13.Kim WS, Kim ST, Lee HH, Kim JY. A case of large septochoanal polyp with calcification. Korean J Otorhinolaryngol-Head Neck Surg. 2010;53(4):228–31. [Google Scholar]
- 14.Cho IY, Kim JW, Kim HJ, Cho KS. Septochoanal polyp with metaplastic ossification mimicking sinonasal tumor: A case report. Iran J Radiol. 2016;13(3):e35299. doi: 10.5812/iranjradiol.35299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim YK, Kim HJ, Kim J, et al. Nasal polyps with metaplastic ossification: CT and MR imaging findings. Neurorad. 2010;52(12):1179–84. doi: 10.1007/s00234-010-0758-6. [DOI] [PubMed] [Google Scholar]
- 16.Testa D, Motta S, Marcuccio G, et al. Our experience in the treatment of malignant fibrous histiocytoma of the larynx: Clinical diagnosis, therapeutic approach and review of literature. Open Med (Wars) 2016;23(1):208–14. doi: 10.1515/med-2016-0040. 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ozcan I, Ozcan KM, Ensari S, Dere H. Rhinolithiasis with a nasal polyp: A case report. Ear Nose Throat J. 2008;87(3):150–51. [PubMed] [Google Scholar]
- 18.Mercan H, Edzer DT, Kilic E, et al. Osseous metaplasia in a nasal polyp: Report of a rare case and review of the literature. Ear Nose Throat J. 2012;91(9):E4–6. [PubMed] [Google Scholar]
- 19.Daniel A, Wong E, Ho J, Singh N. Chondro-osseous respiratory epithelial adenomatoid hamartoma (COREAH): Case report and literature review. Case Rep Otolaryngol. 2019;2019:5247091. doi: 10.1155/2019/5247091. [DOI] [PMC free article] [PubMed] [Google Scholar]


