Abstract
Patient: Male, 88-year-old
Final Diagnosis: Interstitial lung disease
Symptoms: Chronic dyspnea
Medication: Nitrofurantoin
Clinical Procedure: None
Specialty: Pulmonology
Objective:
Adverse events of drug therapy
Background:
Interstitial lung disease, also known as diffuse parenchymal lung disease, is a group of diseases that affects the interstitium of the lungs and can lead to progressive fibrosis of the lungs. The potential causes of inter-stitial lung disease are broad and includes infection, malignancy, autoimmune/connective tissues diseases, inhaled substances, and certain medications. One of the medications that can cause interstitial lung disease is nitrofurantoin.
Case Report:
A 88-year-old man with recurrent urinary tract infections was treated with long-term nitrofurantoin prophylactic therapy. He took 100 mg of nitrofurantoin on a daily basis for over 10 years as prophylactic therapy for recurrent urinary tract infections, and subsequently developed chronic respiratory failure requiring supplemental oxygen. Chest radiography and high-resolution computed tomography imaging were performed and revealed pulmonary fibrosis consistent with interstitial lung disease.
Conclusions:
Although nitrofurantoin is one of the most commonly used antibiotics in the treatment of urinary tract infections and is often considered a relatively safe medication, long-term use can lead to the development of inter-stitial lung disease.
MeSH Keywords: Lung Diseases, Interstitial; Nitrofurantoin; Pulmonary Fibrosis; Urinary Tract Infections
Background
Interstitial lung disease (ILD), also known as diffuse parenchymal lung disease (DPLD), is a group of diseases that affects the interstitium of the lungs and can lead to progressive fibrosis of the lungs. The potential causes of ILD are broad and include infection, malignancy, autoimmune/connective tissues diseases, inhaled substances, and certain medications. One of the medications that can cause ILD is nitrofurantoin.
Case Report
A 88-year-old man was hospitalized following a fall at home. Radiography was positive for intertrochanteric fracture of the proximal left femur, which required surgical repair by orthopedic surgery. During pre-operative risk assessment, a chest radiograph (Figure 1) revealed diffuse reticular and interstitial opacities prominent in the lung bases, consistent with a diagnosis of ILD. A physical exam was unremarkable, except for coarse breath sounds bilaterally, along with decreased range of motion in the left hip. The patient’s medical history included hypertension, diabetes mellitus, benign prostatic hyperplasia, and recurrent urinary tract infections (UTIs) for which he had been on long-term nitrofurantoin prophylactic therapy. In addition, he was a former tobacco smoker with a 40-pack-year smoking history. He stated that he worked at an office job and denied any significant workplace exposures, including exposures potentially leading to asbestosis, silicosis, or berylliosis. He denied any prior radiation therapy and stated that he had never been exposed to amiodarone, methotrexate, or any chemotherapeutic agents.
Figure 1.
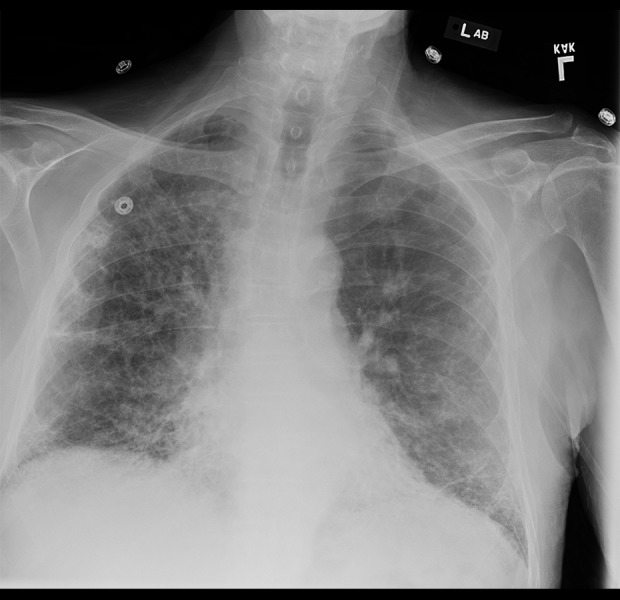
Radiograph of chest showing diffuse reticular and interstitial opacities, most prominent in the lung bases.
After further questioning, the patient stated that he had undergone an extensive urological evaluation for his recurrent UTIs and was prescribed long-term nitrofurantoin prophylactic therapy. He stated that he took 100 mg of nitrofurantoin on a daily basis as prophylactic therapy for recurrent UTIs for over 10 years. He stopped taking the nitrofurantoin in 2008 due to concern about development of pulmonary fibrosis and chronic respiratory failure requiring supplemental oxygen. Pulmonary function testing at that time did not reveal any obstructive or restrictive lung disease. He stated that he was on supplemental oxygen for several years but was eventually able to be weaned off of the supplemental oxygen. A laboratory work-up was negative for ANA, SSA/SSB antibody, Jo-1 antibody, Scl-70 antibody, c-ANCA, and p-ANCA. High-resolution computed tomography (HRCT) (Figure 2) was performed and revealed diffuse bilateral reticular septal thickening with honeycombing of subpleural and bilateral lower lobe predominance, consistent with a diagnosis of ILD. While a biopsy would have been helpful in confirming the diagnosis, it was not performed, because the benefits of the procedure did not exceed the risks. Thankfully, the patient remained stable throughout his hospitalization and successfully underwent surgical repair of the intertrochanteric facture of the proximal left femur without any complications.
Figure 2.
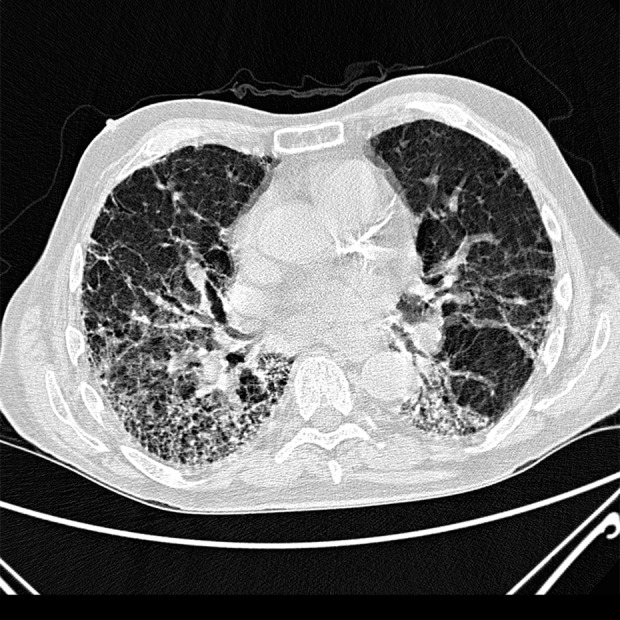
High-resolution computed tomography (HRCT) image of chest showing diffuse bilateral reticular septal thickening with honeycombing of sub-pleural and bilateral lower lobe predominance.
Discussion
Nitrofurantoin is an antibiotic commonly used in the management of UTIs. It can be used for treatment of acute UTIs as well as for prophylaxis in patients with recurrent UTIs.
It is especially commonly used during pregnancy due to its low teratogenic risk for the developing fetus. While nitrofurantoin is a relatively safe antibiotic, it can result in pulmonary injury [1]. Although the incidence of pulmonary injury from nitrofurantoin is estimated to be anywhere between 1 in 550 to 1 in 5400, it is probably underdiagnosed and underre-ported [2]. Both acute and chronic pulmonary injury can occur from nitrofurantoin use, and these occur by different mechanisms of action. The acute form of pulmonary injury is thought to be mediated by a hypersensitivity reaction to nitrofurantoin, while the chronic form of pulmonary injury is thought to occur due to a cell-mediated or toxic response to nitrofurantoin and can result in ILD.
Acute pulmonary injury has been to observed even at small doses and there does not appear to be a relationship between the dose and the development of acute pulmonary injury [3]. The chronic form of pulmonary injury is much less common than the acute form of pulmonary injury and is usually found in patients who had been taking nitrofurantoin on a long-term basis. The exact dose of nitrofurantoin required to result in chronic pulmonary injury is unclear, although the amount of injury is suspected to be dose-related [4]. HRCT, which is the criterion standard imaging test for the diagnosis of ILD, can demonstrate honeycombing, ground-glass attenuation, inter-and intra-lobular septal thickening, and traction bronchiectasis [5]. The treatment for both acute and chronic forms of pulmonary injury is the immediate discontinuation of nitrofurantoin therapy. Due to the possible irreversibility of pulmonary fibrosis, it is important for providers to be aware of the risk of developing of ILD from long-term nitrofurantoin use.
Conclusions
Although nitrofurantoin is one of the most commonly used antibiotics in the treatment of UTIs and is often considered a relatively safe medication, its long-term use can lead to development of ILD.
Footnotes
Conflicts of interest
None.
References:
- 1.Sovijärvi AR, Lemola M, Stenius B, Idänpään-Heikkilä J. Nitrofurantoin-induced acute, subacute and chronic pulmonary reactions. Scand J Respir Dis. 1977;58:41. [PubMed] [Google Scholar]
- 2.Prakash UB. Pulmonary reaction to nitrofurantoin. Semin Respir Dis. 1980;2:71–75. [Google Scholar]
- 3.D’Arcy PF. Nitrofurantoin. Drug Intell Clin Pharm. 1985;19:540–47. doi: 10.1177/106002808501900706. [DOI] [PubMed] [Google Scholar]
- 4.Mendez JL, Nadrous HF, Hartman TE, Ryu JH. Chronic nitrofurantoin-induced lung disease. Mayo Clin Proc. 2005;80:1298–302. doi: 10.4065/80.10.1298. [DOI] [PubMed] [Google Scholar]
- 5.Martins RR, Marchiori E, Viana SL, et al. Chronic eosinophilic pneumonia secondary to long-term use of nitrofurantoin: High-resolution computed tomography findings. J Bras Pneumol. 2008;34:181–84. doi: 10.1590/s1806-37132008000300009. [DOI] [PubMed] [Google Scholar]


