Abstract
Introduction
Previous qualitative reviews have summarized evidence of an association between menthol cigarette use and likelihood of smoking cessation. The objective of this meta-analysis was to provide a quantitative summary of effect sizes, their variability, and factors related to the variability in effect size for the association between menthol use and likelihood of smoking cessation.
Methods
We systematically searched Medline, PsycINFO, and Embase for prospective and cross-sectional studies of the association between menthol use and smoking cessation. We analyzed data with random effects meta-analyses and meta-regression.
Results
Our review identified 22 reports from 19 studies of the association between menthol use and cessation. All identified study samples included only US smokers, with one exception that included both Canadian and US smokers. Our overall model did not demonstrate a significant association between menthol use and cessation; however, menthol users were significantly less likely to quit among blacks/African American smokers (odds ratio = 0.88).
Conclusions
Among blacks/African Americans predominantly in the US menthol users have approximately 12% lower odds of smoking cessation compared to non-menthol users. This difference is likely the result of the tobacco industry’s ongoing marketing influence on the black/African American Community, suggesting that a menthol ban may have a unique public health benefit for black/African American smokers by encouraging quitting behavior.
Implications
This study adds a quantitative summary of the association between menthol cigarette use and smoking cessation in the United States. Findings of an association with lower likelihood of cessation among black/African American smokers, likely resulting from the tobacco industry’s marketing influence, support the ban of menthol flavoring as part of a comprehensive tobacco control effort to increase cessation among black/African American smokers.
Introduction
Tobacco is the leading cause of preventable disease in the United States and accounts for more than 480 000 premature deaths and $289 billion in health care expenditures.1 Cigarette smoking is the most common form of tobacco use, and there have been major gains in decreasing the prevalence of smoking in the past 30 years. The proportion of US adults who smoke has decreased from 20.9% in 2005 to 14% in 2017.2–5 Smoking rates are higher among men (15.8%) compared to women (12.2%) and among those identifying as non-Hispanic white (15.2%) and non-Hispanic black/African American (14.9%), compared to Hispanic/Latinx (9.9%), and non-Hispanic Asian (7.1%).5
Among all current US adult cigarette smokers, nearly 7 of every 10, or 68.8%, reported in 2010 that they wanted to quit and 52.4% had made a failed quit attempt in the previous year.3 In 2015, 68% of smokers were interested in quitting and 55.4% had made a quit attempt, whereas only 7.4% of past 2-year smokers had quit during the past year.6 There was little difference between women and men in these statistics. By race/ethnicity, interest in quitting in 2015 was comparable between non-Hispanic white smokers (67.5%), non-Hispanic black/African American smokers (72.8%), Hispanic/Latinx smokers (67.4%), and non-Hispanic Asian smokers (69.6%). Differences in past-year quit attempts were more marked; for example, 69.4% of non-Hispanic Asian smokers and 63.4% of black/African American smokers reported a past-year quit attempt, compared to 56.2% of Hispanic/Latinx smokers and 53.3% of non-Hispanic white smokers. Despite being the most likely to make a quit attempt, black/African American smokers were the least likely to have recently quit smoking (4.9%) compared to non-Hispanic white (7.l%), Hispanic/Latinx (8.2%), and non-Hispanic Asian (17.3%) smokers.
Menthol cigarette smoking is highly prevalent in the United States, with approximately 39% of all smokers using mentholated cigarettes in 2012–2014, an increase from 35% in 2008–2010.7 More women smoke menthol than men, and youth (12–17 years old) and younger adults (18–25 years old) are more likely than older populations to smoke menthol.8 Considering race/ethnicity, among past 30-day smokers, 84.6% of non-Hispanic black/African Americans, 46.9% of Hispanic/Latinx, and 28.9% of non-Hispanic whites smoked menthol cigarettes most often during the past 30 days in 2012–2014.9
In recent years, scientists and policy makers have considered the potential role of mentholated cigarettes in smoking cessation. There are various potential explanations for why menthol might be related to smoking cessation. One hypothesis is that the cooling sensation of the menthol might decrease or mask the harshness of the smoke on the tongue and throat thus allowing for a greater inhalation of nicotine, leading to greater levels of nicotine dependence.10 In mice, nicotine plus menthol relative to nicotine alone results in a greater number of nicotinic acetylcholine receptors and greater dopaminergic activation in the ventral tegmental area, both potentially leading to greater reinforcement from nicotine and greater reward-related behavior (eg, Henderson et al.11; see Wickham12 for a review). In humans, greater upregulation of nicotinic acetylcholine receptors occurs in smokers relative to nonsmokers, and this effect is enhanced by menthol, possibly contributing to greater reward from nicotine.13 This finding extends previous work demonstrating greater nicotine exposure in menthol compared to non-menthol smokers,14 providing a plausible mechanism for greater dependence and difficulty quitting smoking.
A number of studies have examined the association between menthol cigarettes and smoking cessation in the United States, but results have been inconsistent. Some studies show that menthol smokers are less likely to quit smoking,15–17 whereas others find no difference.18–21 Variability in study samples and methods may account for this heterogeneity. Studies have captured samples varying in sociodemographic characteristics, including racial/ethnic and gender identity.22–24 Samples were recruited from a variety of settings including the general population8,25 specific regions,18,26 prisons,24 and clinical samples.23,24 Study designs have been both cross-sectional8 and prospective,27 have used varying assessments of smoking cessation,28,29 and have accounted for a varying range of control variables.20,30
Four recent reviews have summarized findings across the heterogeneous literature on menthol and smoking cessation in the United States.31–34 All four reviews concluded that despite mixed evidence, it is likely that menthol cigarette use is associated with lower likelihood of smoking cessation, particularly among racial/ethnic minority smokers. These recent reviews were qualitative and consequently did not provide evidence of whether associations between menthol smoking and cessation were statistically significant when summed across the literature. Furthermore, the reviews lacked information on the strength of such an association, quantification of variability in study findings, and study-level factors that may contribute to this variability. Food and Drug Administration policy considerations are ongoing; therefore, information provided by a quantitative review may be valuable in both informing policy discussion and highlighting avenues for clarifying menthol’s contribution to the public health issue of cigarette smoking.
This review aimed to summarize the various findings from the literature on the potential effect of menthol cigarettes on smoking cessation using meta-analysis. The analysis focuses on the United States because samples from published studies on the topic are predominantly located in the United States. Considering the higher prevalence of menthol cigarettes in minority populations and females,10 this project will also investigate differences in the association between menthol use and cessation by race/ethnicity and gender. The findings of this review will allow for the design of more informed public health campaigns and treatments regarding smoking cessation.
Methods
Search Procedures, Inclusion Criteria, and Data Extraction
We searched Medline, Embase, and PsycINFO most recently in February 2019. Our search terms were: Menthol AND (smok* OR cigarette*) AND (quit* OR cessation OR abstinen*). Our inclusion criteria were as follows: (1) cross-sectional or prospective study design; (2) reported an odds ratio (OR) for the association between menthol use and smoking cessation, or provided enough information to calculate an odds ratio; and (3) measured smoking cessation with either self-report or biochemical verification. We extracted data for the following variables: study authors and year, sample location, analytic sample size, recruitment methods, intervention details, measurement of menthol use and smoking cessation, adjustment variables, and results.
Quality Review
We conducted a quality review of included studies using the previously validated Newcastle–Ottawa scale for cohort studies, as well as an adapted Newcastle–Ottawa scale for cross-sectional studies.35 The Newcastle–Ottawa scale assesses risk of bias from selection, information, and confounding, with points given for low risk. Points for cohort studies can range from 1 to 9, with 1–3 representing low quality, 4–6 representing moderate quality, and 7–9 representing high quality. Scores on the version adapted for cross-sectional studies ranged from 1 to 6 based on the applicable cohort categories. This schema accounts for the generally lower quality of evidence from cross-sectional studies compared to cohort studies, with the maximum score being of moderate quality. It is noteworthy that our assessment in quality is with specific regard to the association between menthol use and cessation. For example, a clinical trial may be high quality, but as a prospective study of the association between menthol use and cessation may be moderate or low quality, depending on biases specific to the secondary use of the data.
Meta-Analyses
We conducted meta-analyses using the Metafor package in R statistical software.36 We used random-effects models, weighting by inverse variance. When applicable, analyses accounted for clustering within study. Our effect size estimate was the natural log of the odds ratio for the association between menthol use and smoking cessation. When prospective outcomes were reported from multiple timepoints for a given study, we included the longest time of abstinence available. When multiple definitions of cessation were available from cross-sectional studies, we chose the outcome that limited recall bias to the greatest extent.
When conducting our main meta-analytic model across all included studies, we entered study-level estimates for racial/ethnic subgroups when available, rather than results combined across racial/ethnic subgroups. We analyzed the data in this way to maximize the information and variability of data in our model.
Sensitivity Analyses and Meta-Regression
We conducted sensitivity analyses, limiting studies based on the following additional inclusion criteria: (1) moderate or high quality, (2) prospective studies only, (3) published between 2008 and 2018, and (4) studies of those making a quit attempt (eliminating one prospective study that did not select for those making a quit attempt).18 We also conducted an additional analysis with imputed values for three investigations. Blot et al.,18 D’Silva et al.,26 and Fu et al.19 each tested for racial/ethnic differences in the association between menthol smoking and cessation, and as a result of finding nonsignificant differences excluded racial/ethnic-specific estimates. Consequently, we were not able to include these investigations in subgroup analyses. In the combined sample, all three found nonsignificant associations between menthol smoking and cessation. Therefore, to reduce the potential influence of this observable publication bias on the subgroup analysis estimates, we imputed racial/ethnic-specific estimates by using the combined estimate and adjusting variance estimates by the proportion of sample accounted for by each subgroup.
We conducted meta-regression to examine factors that might relate to variability in effect size for the association between menthol smoking and cessation. When conducting meta-regression, we included imputed estimates for racial/ethnic subgroups to limit the influence of reporting bias. We examined the following five variables individually, and then collectively: race/ethnicity (combined only vs. black/African American vs. white vs. Hispanic/Latinx), quality, length of follow-up (cross-sectional vs. < 6 months vs. 6–12 months vs. >12 months), statistical adjustment for cigarettes per day, and statistical adjustment for time to first cigarette. Studies controlling for composite indicators that include both cigarettes per day and time to first cigarette (Fagerstrom Test for Nicotine Dependence37 and Heaviness of Smoking Index38) were coded as not controlling for the individual variables, because of evidence that menthol smokers typically smoke fewer cigarettes per day, but may have an earlier time to first cigarette.33
Results
Search Results
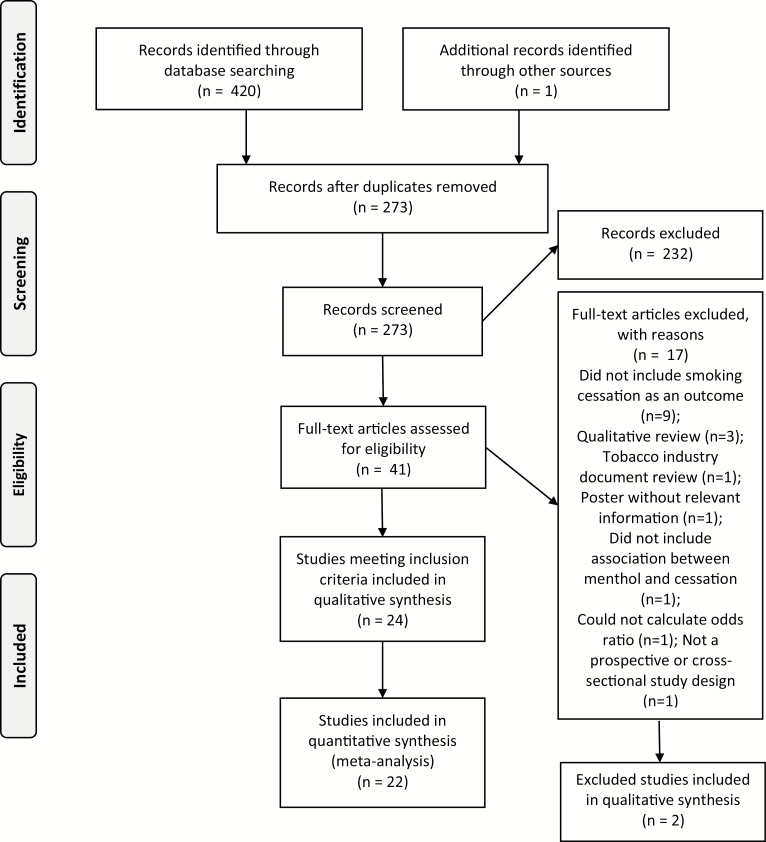
Search results presented here are based on our updated search conducted in February 2019. See Figure 1 for a PRISMA flow chart of search results.39 In summary, our database search identified 420 abstracts, and we identified one additional study through a previous qualitative review. After removing 219 duplicates, we reviewed 273 abstracts for inclusion. We identified 41 abstracts for additional full-manuscript review. Of these, 22 met all study inclusion criteria.8,15–30,40–44 In three instances, two published articles analyzed data from the same underlying study; therefore, our meta-analysis included information from 19 data sources representing 147 584 cigarette smokers. Although we did not intentionally exclude non-US studies, all identified studies except for one were conducted exclusively in the United States, and the one exception included smokers from both the United States and Canada.20
Figure 1.
Flow chart of study inclusion.
Excluded Studies
Here, we qualitatively summarize four relevant studies that were not included in our quantitative synthesis. Levy et al.,45 Keeler et al.,46 and Delnevo et al.8 used the same or overlapping sources of data: the US 2003, 2006–2007, and 2010–2011 Tobacco Use Supplement to the Current Population Survey (TUS-CPS). We included results from Delnevo et al.8 because their sample restriction of recent quit attempters was more consistent with other included studies and our research question, whereas Levy et al.45 and Keeler et al.46 did not restrict their sample to attempters.
Levy et al. concluded that in their overall sample, those smoking menthol cigarettes were slightly less likely to quit smoking (OR = 0.97), consistent with Delnevo et al.. Keeler et al. found that menthol use was not significantly associated with smoking cessation among any of the racial/ethnic groups examined: non-Hispanic white, non-Hispanic black/African American, non-Hispanic Asian, and Hispanic. This finding is in contrast to Delnevo et al.8 who also analyzed the 2006/2007 TUS-CPS data, but found that among black/African American smokers menthol smokers were less likely to quit than non-menthol. One possible explanation for this difference in conclusion is the difference in sample selection—Delnevo et al. only included those who made a quit attempt in their sample, whereas Keeler et al. did not restrict their sample to those having made a quit attempt. Both Keeler and Levy found black/African American menthol smokers were more likely to attempt quitting compared to non-menthol smokers, suggesting lower likelihood of successful cessation among black/African Americans who smoke menthol and who are trying to quit.
We excluded an investigation reported by Lewis et al.47 The study reported hazard ratios for time to quitting rather than odds ratios and therefore did not meet our inclusion criterion. The authors reported that the hazard ratio association with quitting smoking among menthol smokers versus non-menthol smokers was 0.79 (95% confidence interval [CI] = 0.64 to 0.99), suggesting that menthol smokers had a lower rate of smoking cessation; that is, menthol smokers were less likely to quit.
Muench et al.48 examined predictors of relapse using a 48-hour smoking cessation laboratory paradigm and therefore did not meet study inclusion criterion. Their investigation found menthol preference was associated with greater lapse during the 48-hour study period.
Study Characteristics
A summary of data extracted from the selected 22 articles representing 19 studies, as well as our quality review, is provided in Supplementary Table 1. Of the nineteen studies included in the review, four used cross-sectional study designs and fifteen used prospective study designs. Of the fifteen prospective study designs, two were epidemiological cohorts, five were cohorts recruited through cessation clinics or quitlines and followed from the time of a quit attempt, and eight were secondary analyses of randomized trial data. Measurement of menthol use varied; however, studies generally relied on a binary (yes vs. no) self-report of whether menthol cigarettes were preferred by the cigarette smokers. Measurement of smoking cessation varied extensively as well. Cross-sectional and prospective epidemiological studies relied on self-report, whereas clinical trials typically used biochemical verification. All studies except for one18 examined smoking cessation among those making or having recently made quit attempts. Among prospective studies, length of follow-up varied extensively both within and between studies. Clinical trials included follow-up times as little as 1 month, whereas epidemiological studies included follow-up times up to 15 years. Statistical control variables also varied widely, ranging from no controls to sociodemographic variables, to sociodemographic variables and extensive inclusion of tobacco use-related variables.
Study Quality
We provide detailed quality review results, including justification for scores, in Supplementary Table 1. Original data collection results using the Newcastle–Ottawa35 scale are available from the corresponding author on request. Our quality review identified ten studies of high-quality, six studies of moderate-quality, and three studies of low-quality evidence. The most commonly identified sources of bias were nonrepresentative samples and self-report of the exposure. Self-reported smoking cessation and lack of detail related to attrition were also common sources of bias.
Meta-Analyses
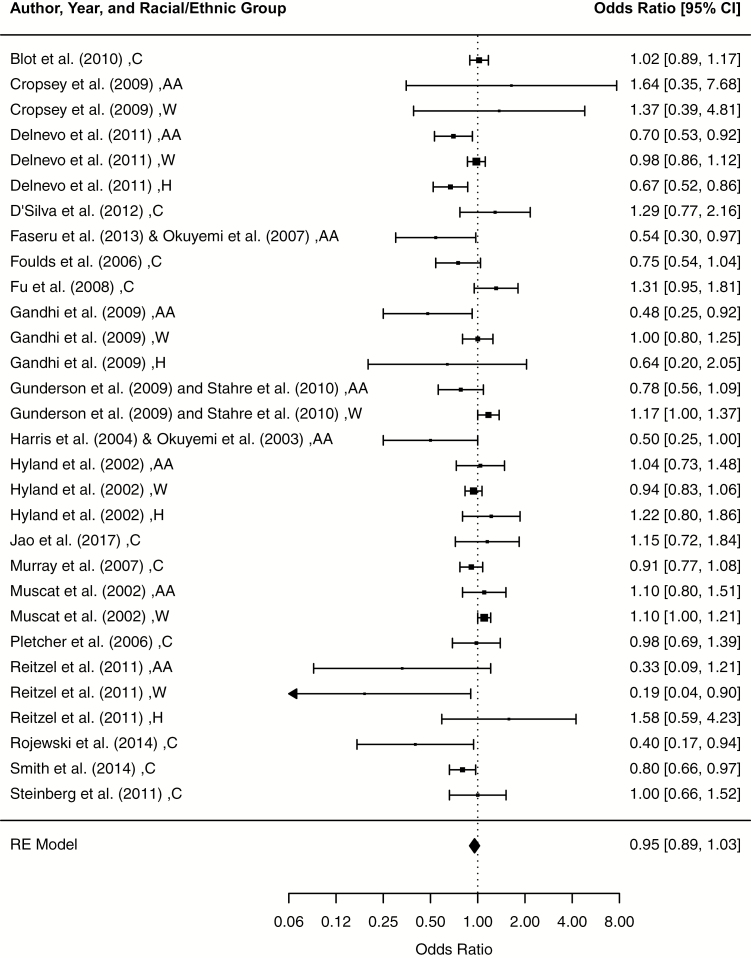
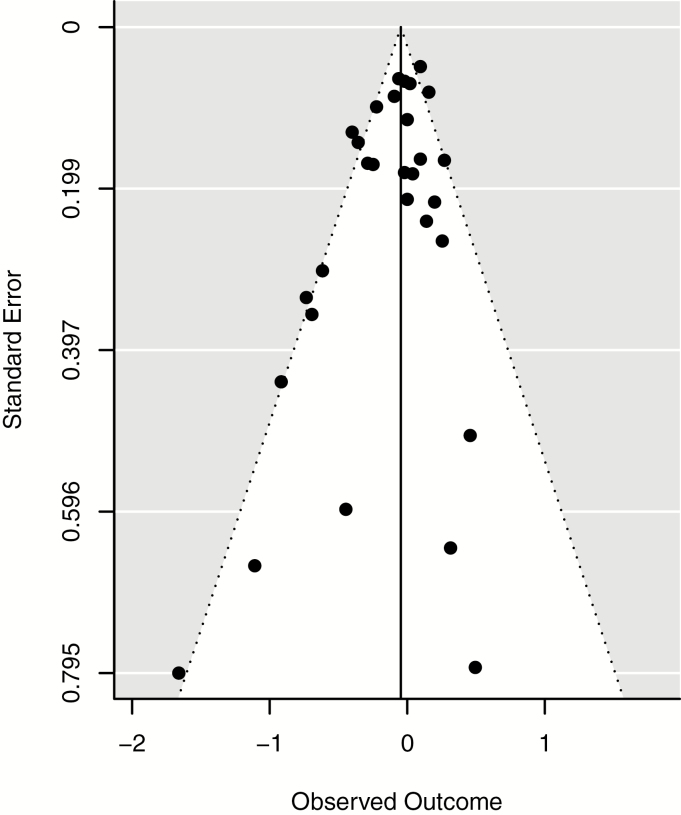
Results from the model combining all study results are depicted in a forest plot in Figure 2. The meta-analytic combined effect size was OR = 0.95 (95% CI = 0.89 to 1.03; p = .21). Heterogeneity analyses with 29 degrees of freedom estimated a Q-statistic of 66.74 (p < .001) and an I2 of 56.55, indicating that 56.55% of variability in effect sizes was because of explainable heterogeneity, rather than random variation. A funnel plot of standard errors by log odds ratios is depicted in Figure 3. The funnel plot suggests minimal publication bias.
Figure 2.
Forest plot for the association between menthol cigarette use and smoking cessation. AA = black/African American, W = white, H = Hispanic/Latinx, C = combined.
Figure 3.
Funnel plot for included effect sizes.
Sensitivity Analyses
We first limited the sample to studies with a quality rating of moderate to high, with minimal change in estimates: OR = 0.95 (95% CI = 0.87 to 1.04; p = .26); Q23 = 45.46 (p < .001), I2 = 49.41%. We then limited the sample to prospective studies only, and the odds ratio for the combined sample became statistically significant: OR = 0.92 (95% CI = 0.86 to 0.99; p = .02); Q21 = 33.65 (p < .001), I2 = 37.59%. Limiting the sample to studies published within 10 years of 2018 had little effect on the results: OR = 0.97 (95% CI = 0.88 to 1.07; p = .53); Q19 = 47.49 (p < .001), I2 = 60%. Removing one prospective study that did not select for quit attempters also had little effect on the results: OR = 0.95 (95% CI = 0.87 to 1.02); Q28 = 66.29 (p < .001), I2 = 57.8%. Finally, we added imputed values for racial/ethnic subgroups for studies that reported a nonsignificant interaction between menthol use and race/ethnicity. Results were highly similar to the original model: OR = 0.95 (95% CI = 0.89 to 1.03); Q32 = 66.43 (p < .001), I2 = 51.83%.
Meta-Regression
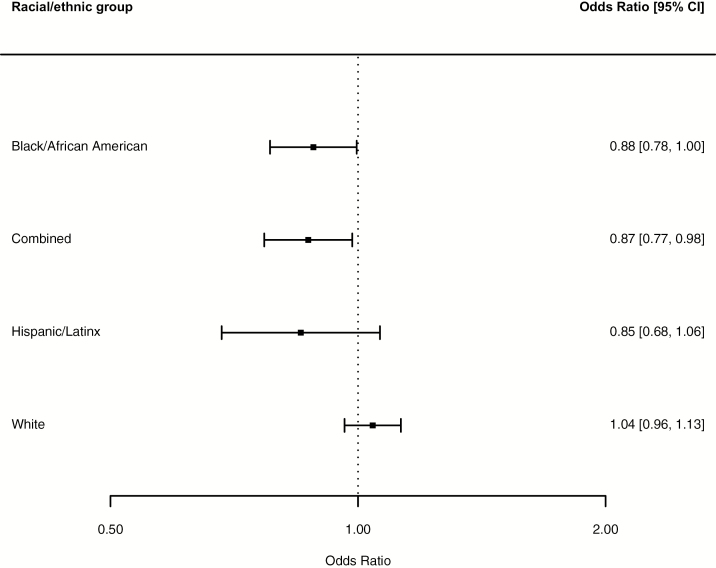
Race/Ethnicity
There was evidence of significant heterogeneity between racial/ethnic groups (Q4 = 13.66; p < .01). Figure 4 presents this heterogeneity. The association between menthol use and smoking cessation was statistically significant among black/African American smokers, and among studies that did not provide estimates for racial/ethnic subgroups. Among black/African American smokers, menthol smokers had 12% lower odds of successfully quitting smoking compared to non-menthol smokers (p = .04). Among studies that did not report results for racial/ethnic subgroups, menthol smokers had 14% lower odds of successfully quitting smoking compared to non-menthol smokers (p = .03). There was a similar effect size for Hispanic/Latinx smokers (OR = 0.85); however, the difference was not statistically significant. The odds ratio for white smokers (OR = 1.04) was not significant. Racial/ethnic differences had an adjusted R2 of 0.47, indicating that racial/ethnic category accounted for approximately 47% of explainable effect size heterogeneity.
Figure 4.
Racial/ethnic-specific associations between menthol cigarette use and smoking cessation. The overall difference among groups was statistically significant (p < .01).
Study Quality, Follow-up Length, Control Variables
The omnibus tests for group differences were nonsignificant for study quality (Q3 = 4.75; p = .19), follow-up length (Q4 = 6.36; p = .17), statistical control for cigarettes per day (Q2 = 4.05, p = .13), and statistical control for time to first cigarette (Q2 = 1.68, p = .43).
Gender Differences
Given the greater prevalence of menthol use among women compared to men, we intended to conduct analyses separately by gender. Our data extraction revealed insufficient numbers of studies with gender-specific results to conduct the analyses. Here, we report a qualitative review of these few studies. In a clinical trial for female prisoners, Cropsey et al.24 found that the association between menthol smoking and cessation at 12 months was nonsignificant among both black/African American and white women. Murray et al.27 studied smoking cessation among those with early evidence of obstructive lung impairment and found the association between menthol use and cessation was nonsignificant for both women and men. In an investigation of continued cessation following pregnancy, Reitzel et al.29 found that among white women menthol use was associated with lower odds of quitting, while among black/African American women and Hispanic/Latinx women the associations were nonsignificant. However, the large effect size for black/African American women (OR = 0.33) suggests the study was underpowered for racial/ethnic subgroup analyses.
Discussion
This meta-analytic review examined quantitative evidence for the association between menthol smoking and smoking cessation in the United States across published studies. When we combined all evidence, the association between menthol smoking and smoking cessation in the United States was nonsignificant. Despite a considerable number of differences between studies in both sample and methodological characteristics, as well as a relatively small number of total studies (k = 19), the confidence interval around the overall odds ratio of 0.95 was relatively narrow (0.89 to 1.03), suggesting the effect size estimate is an accurate representation of the underlying population of studies from which these results were drawn. The large number of cigarette smokers included across studies, approaching 150 000 likely contributed to relatively narrow confidence intervals.
Across studies, approximately half of the variance in the association between smoking menthol cigarettes and smoking cessation was found to be non-random (ie, explainable) heterogeneity. Race/ethnicity accounted for approximately 47% of this explainable heterogeneity. Among black/African American smokers menthol cigarette use was associated with 12% lower odds of smoking cessation, whereas among white smokers there was no association. Among Hispanic/Latinx smokers the effect size was similar to black/African American smokers but was nonsignificant, suggesting there may not have been enough studies to detect a meaningful association. These findings support conclusions from prior qualitative reviews. For example, the Food and Drug Administration’s 2013 report on menthol cigarettes concluded there is likely an association whereby menthol smokers are less likely to quit, and that this is particularly true for black/African American smokers.33 A recent review and original analysis by Kulak et al.49 provided evidence that black/African American smokers are less likely to successfully quit smoking than white smokers. Menthol use may play an important role in this difference, given that approximately 74%–88% of black/African American adult smokers in the United States smoke menthol cigarettes.9,50
Understanding and Addressing Menthol Use and Smoking Cessation Among Black/African American Smokers
The oppressive forces that have created the social construct of race51 manifest in a number of biological and behavioral factors that affect disease processes and that create health-related disparities between individuals grouped into racial/ethnic categories.52 Those self-categorizing as white, black/African American, or Hispanic/Latinx in the studies incorporated in this meta-analysis represent an incredibly diverse group of individuals that cannot be validly grouped with a single label; nonetheless, “white,” “Black/African American,” and “Hispanic/Latinx” are constructs that operate collectively through historical and current cultural, societal, and systemic forces; therefore, they may produce collective associations and differences such as those found in our meta-analysis.
From this perspective, understanding racial/ethnic differences in the association between menthol use and smoking cessation requires an understanding of how social forces influence menthol use among black/African American and Hispanic/Latinx individuals. As described by Dr. Phillip Gardiner,53 the “African Americanization of menthol cigarette use” is a product of tobacco industry practices and the oppressive context of a racialized United States. Dr. Gardiner writes that the tobacco industry’s use of “targeted marketing, use of segregated markets, capitalization on the growing “Black ethos” of the Civil Rights movement, and the promotion of the “healthful” qualities of menthol” created the social phenomena of menthol smoking among black/African Americans. Gardiner also writes that “The bottom line is that African Americans prefer menthol cigarettes because the tobacco industry pushed these products on and created the demand among this population. Did the industry do this on purpose? The answer to this question is an unequivocal yes.”
Evidence of how marketing and misinformation have affected knowledge and beliefs among black/African American smokers is emerging. For example, in a study of menthol use and smoking cessation among black/African American light smokers participating in a clinical trial for bupropion, Okuyemi et al.41 observed that menthol smokers had less confidence quitting smoking than non-menthol smokers, whereas confidence is a potent predictor of quit success.54. This low confidence may be reflected in qualitative research findings, which suggest black/African American menthol smokers commonly switch to non-menthol cigarettes as a cessation aid, despite considering non-menthol cigarettes to be harsher and associating non-menthol cigarettes with greater health problems.55
Addressing the use of menthol and its association with lower likelihood of smoking cessation among racial/ethnic minorities in the United States will require a multifaceted approach that is not ignorant of but rather is informed by historical and current social context.56 From a policy perspective, banning menthol flavoring will likely have a favorable effect on smoking rates among black/African Americans in the United States. There remains a large disparity in the level of point-of-sale menthol marketing towards black/African American communities.57 From a clinical perspective, there is a growing body of research supporting the efficacy of culturally specific smoking cessation interventions for black/African American cigarette smokers.58–61 Webb Hooper et al.59 designed culturally specific group-based cognitive behavioral therapy sessions for smoking cessation, and in comparison to standard cognitive behavioral therapy those in the culturally specific groups were more successful, especially for short-term outcomes. These culturally specific sessions included topics of “…medical mistrust, the history of race and smoking, race-based statistics, targeted tobacco marketing, pharmacotherapy concerns, cultural values, (eg, religion/spirituality, family/collectivism), unique stressors (eg, racial discrimination, race-related stress, financial strain), depression among African Americans, comorbid drug addiction, environmental influences (eg, neighborhood characteristics), menthol cigarettes, race-specific weight issues and concerns, and community mobilization against the tobacco industry” (p. 336).
Implications
There is a clear need for more research on menthol use among Hispanic/Latinx smokers, as well as research that examines menthol use, barriers to cessation, and tailored interventions among black/African American smokers, based in theoretical and critical perspectives. This meta-analysis provides additional evidence that a menthol ban will have a favorable impact on smoking cessation rates among blacks/African Americans, and possibly Hispanic/Latinx communities as well. The focus on menthol use in black/African American and Hispanic/Latinx smokers in this meta-analysis rises from historical context, the relatively high prevalence of use in these racial/ethnic groups, and the number of studies on this topic; however, there is evidence of increasing menthol use prevalence among other racial/ethnic categories. For example, Villanti et al. found increased prevalence of menthol use in the United States between 2008–2010 and 2012–2014 among white and Asian smokers, in addition to Hispanic/Latinx smokers.7 Hispanic/Latinx smokers increased prevalence by 9.8 percentage points, compared to 7.7 percentage points among Asian smokers, and 3.4 percentage points among white smokers. Among young adult white smokers, the increase was 9.8 percentage points. The consideration of menthol use and the need for culturally-specific public health and cessation applies to individuals identifying across the spectrum of racial/ethnic categories.
Somewhat surprisingly, very few studies examined differential associations by gender categories.62 Women are more likely to smoke menthol cigarettes than men,10 and some reports have found women are less likely to successfully quit smoking than men when making a quit attempt.63,64 However, whether menthol cigarette use is an important variable related to smoking cessation among women remains unclear. Future research examining such differences will allow for an assessment of the influence of menthol-related tobacco control efforts on gender differences in smoking and smoking cessation. Future research using qualitative methods and intersectional approaches to studying the interplay between gender, race/ethnicity, and other social categories also holds promise for illuminating knowledge on this topic.
Methodologically, in the Food and Drug Administration’s 2013 report on menthol use, the authors suggested some studies of menthol use and cessation may overcontrol by adjusting for time to first cigarette, a variable that is potentially in the causal pathway between menthol use and lower likelihood of smoking cessation.33 The report specifically highlights the analysis of Hyland et al.20 of the COMMIT study, which found the association between menthol use and smoking cessation to be nonsignificant. It is important to point out that time-to-first cigarette was actually later among menthol smokers than non-menthol smokers in this particular study; therefore, controlling for time-to-first cigarette is unlikely to have masked a significant association. Our quantitative analyses suggest that controlling for dependence-related variables such as time-to-first cigarette and cigarettes per day has had minimal influence across studies of menthol cigarette use and smoking cessation, further supporting a sociocultural interpretation of our findings. Follow-up length and study quality were also not significantly related to variability in this association, suggesting findings are robust across these examined methodological characteristics.
Limitations
This is a meta-analysis of observational studies; caution should be taken when inferring causation. Randomization to menthol versus non-menthol smoking is unfeasible because of strong cigarette brand preference, and therefore observational evidence is likely the best quality evidence to be obtained. We did not include dissertations or conference abstracts, although we did not find evidence of publication bias. We did not include meta-regression examining whether measurement of menthol use was related to variability in study findings, although this topic is clearly relevant. We found the extent of variation in wording of menthol questions, despite overlap in conceptual basis, to be prohibitive for creating a categorical independent variable in meta-regression analyses. Therefore, it remains a question whether the wording of survey items eliciting self-report menthol use is impactful on study results.
Conclusions
The main conclusion that can be drawn from this meta-analysis is that menthol smoking may be an important factor driving racial/ethnic tobacco disparities in the United States. A 12% lower odds of smoking cessation associated with menthol use among black/African American smokers when applied across all smokers, if causal, would result in many fewer smokers quitting in any given time period. A menthol ban will likely have a favorable impact on smoking rates among black/African American, and possibly Hispanic/Latinx, communities.
Funding
Funding was provided by the Grace J. Fippinger Foundation (PIs: Mazure and Smith), grant umber P50 DA033945 from National Institute on Drug Abuse (NIDA), and the Office of Research on Women’s Health (ORWH), Office of the Director, National Institutes of Health (PI: McKee), by the Yale BIRCWH Scholar Program on Women’s Health and Addictive Behaviors (ORWH, NIDA, National Institute on Alcohol Abuse and Alcoholism; K12 DA031050; PI: Mazure), and by grant number P20 CA192993 from National Cancer Institute (PIs: Ostroff, Sheffer, and Smith).
Declaration of Interests
All authors have no conflicts to disclose.
Supplementary Material
References
- 1. U.S. Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General 2014. https://www.surgeongeneral.gov/library/reports/50-years-of-progress/index.html. Accessed December 7, 2018.
- 2. Jamal A, Agaku IT, O’Connor E, King BA, Kenemer JB, Neff L. Current cigarette smoking among adults—United States, 2005–2013. MMWR Morb Mortal Wkly Rep. 2014;63(47):1108–1112. http://www.ncbi.nlm.nih.gov/pubmed/25426653. Accessed December 7, 2018. [PMC free article] [PubMed] [Google Scholar]
- 3. Centers for Disease Control and Prevention (CDC). Quitting smoking among adults--United States, 2001–2010. MMWR Morb Mortal Wkly Rep. 2011;60(44):1513–1519. http://www.ncbi.nlm.nih.gov/pubmed/22071589. Accessed December 7, 2018. [PubMed] [Google Scholar]
- 4. Ward BW, Clarke TC, Freeman G, Schiller JS. Early Release of Selected Estimates Based on Data from the January–September 2014 National Health Interview Survey https://stacks.cdc.gov/view/cdc/28996. Accessed December 7, 2018.
- 5. Wang TW, Asman K, Gentzke AS, et al. Tobacco product use among adults—United States, 2017. MMWR Morb Mortal Wkly Rep. 2018;67(44):1225–1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Babb S, Malarcher A, Schauer G, Asman K, Jamal A. Quitting smoking among adults—United States, 2000-2015. MMWR Morb Mortal Wkly Rep. 2017;65(52):1457–1464. [DOI] [PubMed] [Google Scholar]
- 7. Villanti AC, Mowery PD, Delnevo CD, Niaura RS, Abrams DB, Giovino GA. Changes in the prevalence and correlates of menthol cigarette use in the USA, 2004–2014. Tob Control. 2016;25 (suppl 2):ii14–ii20. [DOI] [PubMed] [Google Scholar]
- 8. Delnevo CD, Gundersen DA, Hrywna M, Echeverria SE, Steinberg MB. Smoking-cessation prevalence among U.S. smokers of menthol versus non-menthol cigarettes. Am J Prev Med. 2011;41(4):357–365. [DOI] [PubMed] [Google Scholar]
- 9. Giovino GA, Villanti AC, Mowery PD, et al. Differential trends in cigarette smoking in the USA: is menthol slowing progress? Tob Control. 2015;24(1):28–37. [DOI] [PubMed] [Google Scholar]
- 10. Giovino GA, Sidney S, Gfroerer JC, et al. Epidemiology of menthol cigarette use. Nicotine Tob Res. 2004;6 (suppl 1):S67–S81. [DOI] [PubMed] [Google Scholar]
- 11. Henderson BJ, Wall TR, Henley BM, Kim CH, McKinney S, Lester HA. Menthol Enhances nicotine reward-related behavior by potentiating nicotine-induced changes in nAChR function, nAChR upregulation, and DA neuron excitability. Neuropsychopharmacology. 2017;42(12):2285–2291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wickham RJ. How menthol alters tobacco-smoking behavior: a biological perspective. Yale J Biol Med. 2015;88(3):279–287. http://www.ncbi.nlm.nih.gov/pubmed/26339211. Accessed April 11, 2019. [PMC free article] [PubMed] [Google Scholar]
- 13. Brody AL, Mukhin AG, La Charite J, et al. Up-regulation of nicotinic acetylcholine receptors in menthol cigarette smokers. Int J Neuropsychopharmacol. 2013;16(5):957–966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Benowitz NL, Herrera B, Jacob P III. Mentholated cigarette smoking inhibits nicotine metabolism. J Pharmacol Exp Ther. 2004;310(3):1208–1215. [DOI] [PubMed] [Google Scholar]
- 15. Faseru B, Nollen NL, Mayo MS, et al. Predictors of cessation in African American light smokers enrolled in a bupropion clinical trial. Addict Behav. 2013;38(3):1796–1803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gandhi KK, Foulds J, Steinberg MB, Lu SE, Williams JM. Lower quit rates among African American and Latino menthol cigarette smokers at a tobacco treatment clinic. Int J Clin Pract. 2009;63(3):360–367. [DOI] [PubMed] [Google Scholar]
- 17. Smith SS, Fiore MC, Baker TB. Smoking cessation in smokers who smoke menthol and non-menthol cigarettes. Addiction. 2014;109(12):2107–2117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Blot WJ, Cohen SS, Aldrich M, McLaughlin JK, Hargreaves MK, Signorello LB. Lung cancer risk among smokers of menthol cigarettes. J Natl Cancer Inst. 2011;103(10):810–816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Fu SS, Okuyemi KS, Partin MR, et al. Menthol cigarettes and smoking cessation during an aided quit attempt. Nicotine Tob Res. 2008;10(3):457–462. [DOI] [PubMed] [Google Scholar]
- 20. Hyland A, Garten S, Giovino GA, Cummings KM. Mentholated cigarettes and smoking cessation: findings from COMMIT. Community Intervention Trial for Smoking Cessation. Tob Control. 2002;11(2):135–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Steinberg MB, Bover MT, Richardson DL, Schmelzer AC, Williams JM, Foulds J. Abstinence and psychological distress in co-morbid smokers using various pharmacotherapies. Drug Alcohol Depend. 2011;114(1):77–81. [DOI] [PubMed] [Google Scholar]
- 22. Foulds J, Gandhi KK, Steinberg MB, et al. Factors associated with quitting smoking at a tobacco dependence treatment clinic. Am J Health Behav. 2006;30(4):400–412. [DOI] [PubMed] [Google Scholar]
- 23. Okuyemi KS, Ahluwalia JS, Ebersole-Robinson M, Catley D, Mayo MS, Resnicow K. Does menthol attenuate the effect of bupropion among African American smokers? Addiction. 2003;98(10):1387–1393. [DOI] [PubMed] [Google Scholar]
- 24. Cropsey KL, Weaver MF, Eldridge GD, Villalobos GC, Best AM, Stitzer ML. Differential success rates in racial groups: results of a clinical trial of smoking cessation among female prisoners. Nicotine Tob Res. 2009;11(6):690–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Gundersen DA, Delnevo CD, Wackowski O. Exploring the relationship between race/ethnicity, menthol smoking, and cessation, in a nationally representative sample of adults. Prev Med. 2009;49(6):553–557. [DOI] [PubMed] [Google Scholar]
- 26. D’Silva J, Boyle RG, Lien R, Rode P, Okuyemi KS. Cessation outcomes among treatment-seeking menthol and nonmenthol smokers. Am J Prev Med. 2012;43 (5 suppl 3):S242–S248. [DOI] [PubMed] [Google Scholar]
- 27. Murray RP, Connett JE, Skeans MA, Tashkin DP. Menthol cigarettes and health risks in Lung Health Study data. Nicotine Tob Res. 2007;9(1):101–107. [DOI] [PubMed] [Google Scholar]
- 28. Muscat JE, Richie JP Jr, Stellman SD. Mentholated cigarettes and smoking habits in whites and blacks. Tob Control. 2002;11(4):368–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Reitzel LR, Etzel CJ, Cao Y, Okuyemi KS, Ahluwalia JS. Associations of menthol use with motivation and confidence to quit smoking. Am J Health Behav. 2013;37(5):629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Harris KJ, Okuyemi KS, Catley D, Mayo MS, Ge B, Ahluwalia JS. Predictors of smoking cessation among African-Americans enrolled in a randomized controlled trial of bupropion. Prev Med. 2004;38(4):498–502. [DOI] [PubMed] [Google Scholar]
- 31. Foulds J, Hooper MW, Pletcher MJ, Okuyemi KS. Do smokers of menthol cigarettes find it harder to quit smoking? Nicotine Tob Res. 2010;12 (suppl 2):S102–S109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hoffman AC, Miceli D. Menthol cigarettes and smoking cessation behavior. Tob Induc Dis. 2011;9 (suppl 1):S6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. U.S. Food and Drug Administration. Preliminary Scientific Evaluation of the Possible Public Health Effects of Menthol Versus Nonmenthol Cigarettes | Search Results 2013. https://wayback.archive-it.org/7993/20170404193211/https://www.fda.gov/downloads/ScienceResearch/SpecialTopics/PeerReviewofScientificInformationandAssessments/UCM361598.pdf. Accessed December 7, 2018.
- 34. Villanti AC, Collins LK, Niaura RS, Gagosian SY, Abrams DB. Menthol cigarettes and the public health standard: a systematic review. BMC Public Health. 2017;17(1):983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Well G, Shea B, O’Connell J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-analyses Ottawa Hospital Research Institute; 2012. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed December 7, 2018. [Google Scholar]
- 36. Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010;36(3):1–48. [Google Scholar]
- 37. Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström Test for nicotine dependence: a revision of the Fagerström Tolerance Questionnaire. Br J Addict. 1991;86(9):1119–1127. https://web.b.ebscohost.com/ehost/detail/detail?vid=0&sid=6f5e6411-462c-4d70-9da8-a26b2421d812%40sessionmgr103&bdata=JnNpdGU9ZWhvc3QtbGl2ZSZzY29wZT1zaXRl#AN=6623842&db=aph. Accessed December 7, 2018. [DOI] [PubMed] [Google Scholar]
- 38. Heatherton TF, Kozlowski LT, Frecker RC, Rickert W, Robinson J. Measuring the heaviness of smoking: using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. Br J Addict. 1989;84(7):791–799. [DOI] [PubMed] [Google Scholar]
- 39. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–9, W64. [DOI] [PubMed] [Google Scholar]
- 40. Jao NC, Veluz-Wilkins AK, Smith MJ, et al. Does menthol cigarette use moderate the effect of nicotine metabolism on short-term smoking cessation? Exp Clin Psychopharmacol. 2017;25(3):216–222. https://web.a.ebscohost.com/ehost/detail/detail?vid=0&sid=c8049737-5a81-47ff-aa00-85ce9d8fe6ef%40sessionmgr4009&bdata=JnNpdGU9ZWhvc3QtbGl2ZSZzY29wZT1zaXRl#AN=6609959&db=aph. Accessed December 7, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Okuyemi KS, Faseru B, Sanderson Cox L, Bronars CA, Ahluwalia JS. Relationship between menthol cigarettes and smoking cessation among African American light smokers. Addiction. 2007;102(12):1979–1986. [DOI] [PubMed] [Google Scholar]
- 42. Pletcher MJ, Hulley BJ, Houston T, Kiefe CI, Benowitz N, Sidney S. Menthol cigarettes, smoking cessation, atherosclerosis, and pulmonary function: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Arch Intern Med. 2006;166(17):1915–1922. [DOI] [PubMed] [Google Scholar]
- 43. Rojewski AM, Toll BA, O’Malley SS. Menthol cigarette use predicts treatment outcomes of weight-concerned smokers. Nicotine Tob Res. 2014;16(1):115–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Stahre M, Okuyemi KS, Joseph AM, Fu SS. Racial/ethnic differences in menthol cigarette smoking, population quit ratios and utilization of evidence-based tobacco cessation treatments. Addiction. 2010;105 (suppl 1):75–83. [DOI] [PubMed] [Google Scholar]
- 45. Levy DT, Blackman K, Tauras J, et al. Quit attempts and quit rates among menthol and nonmenthol smokers in the United States. Am J Public Health. 2011;101(7):1241–1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Keeler C, Max W, Yerger V, Yao T, Ong MK, Sung HY. The association of menthol cigarette use with quit attempts, successful cessation, and intention to quit across racial/ethnic groups in the United States. Nicotine Tob Res. 2017;19(12):1450–1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Lewis M, Wang Y, Berg CJ. Tobacco control environment in the United States and individual consumer characteristics in relation to continued smoking: differential responses among menthol smokers? Prev Med. 2014;65:47–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Muench C, Juliano LM. Predictors of smoking lapse during a 48-hour laboratory analogue smoking cessation attempt. Psychol Addict Behav. 2017;31(4):415–422. [DOI] [PubMed] [Google Scholar]
- 49. Kulak JA, Cornelius ME, Fong GT, Giovino GA. Differences in quit attempts and cigarette smoking abstinence between whites and African Americans in the United States: literature review and results from the international tobacco control US survey. Nicotine Tob Res. 2016;18 (suppl 1):S79–S87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Lawrence D, Rose A, Fagan P, Moolchan ET, Gibson JT, Backinger CL. National patterns and correlates of mentholated cigarette use in the United States. Addiction. 2010;105 (suppl 1):13–31. [DOI] [PubMed] [Google Scholar]
- 51. Smedley A, Smedley BD. Race as biology is fiction, racism as a social problem is real: anthropological and historical perspectives on the social construction of race. Am Psychol. 2005;60(1):16–26. [DOI] [PubMed] [Google Scholar]
- 52. Kuzawa CW, Sweet E. Epigenetics and the embodiment of race: developmental origins of US racial disparities in cardiovascular health. Am J Hum Biol. 2009;21(1):2–15. [DOI] [PubMed] [Google Scholar]
- 53. Gardiner PS. The African Americanization of menthol cigarette use in the United States. Nicotine Tob Res. 2004;6 (suppl 1):S55–S65. [DOI] [PubMed] [Google Scholar]
- 54. Garvey AJ, Bliss RE, Hitchcock JL, Heinold JW, Rosner B. Predictors of smoking relapse among self-quitters: a report from the Normative Aging Study. Addict Behav. 1992;17(4):367–377. [DOI] [PubMed] [Google Scholar]
- 55. Richter P, Beistle D, Pederson L, O’Hegarty M. Small-group discussions on menthol cigarettes: listening to adult African American smokers in Atlanta, Georgia. Ethn Health. 2008;13(2):171–182. [DOI] [PubMed] [Google Scholar]
- 56. Kong AY, Golden SD, Berger MT. An intersectional approach to the menthol cigarette problem: what’s race(ism) got to do with it? Crit Public Health. 2018;1–8. doi:10.1080/09581596.2018.1478066 [Google Scholar]
- 57. Lee JG, Henriksen L, Rose SW, Moreland-Russell S, Ribisl KM. A systematic review of neighborhood disparities in point-of-sale tobacco marketing. Am J Public Health. 2015;105(9):e8–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Webb MS. Does one size fit all African American smokers? The moderating role of acculturation in culturally specific interventions. Psychol Addict Behav. 2008;22(4):592–596. [DOI] [PubMed] [Google Scholar]
- 59. Webb Hooper M, Antoni MH, Okuyemi K, Dietz NA, Resnicow K. Randomized controlled trial of group-based culturally specific cognitive behavioral therapy among African American Smokers. Nicotine Tob Res. 2017;19(3):333–341. [DOI] [PubMed] [Google Scholar]
- 60. Orleans CT, Boyd NR, Bingler R, et al. A self-help intervention for African American smokers: tailoring cancer information service counseling for a special population. Prev Med. 1998;27(5 Pt 2):S61–S70. [DOI] [PubMed] [Google Scholar]
- 61. Nollen N, Ahluwalia JS, Mayo MS, et al. A randomized trial of targeted educational materials for smoking cessation in African Americans using transdermal nicotine. Health Educ Behav. 2007;34(6):911–927. [DOI] [PubMed] [Google Scholar]
- 62. Smith PH, Akpara E, Haq R, El-Miniawi M, Thompson AB. Gender and menthol cigarette use in the United States: a systematic review of the recent literature (2011–May 2017). Curr Addict Rep. 2017;4(4):431–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Smith PH, Bessette AJ, Weinberger AH, Sheffer CE, McKee SA. Sex/gender differences in smoking cessation: a review. Prev Med. 2016;92:135–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Smith PH, Kasza KA, Hyland A, et al. Gender differences in medication use and cigarette smoking cessation: results from the International Tobacco Control Four Country Survey. Nicotine Tob Res. 2015;17(4):463–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.