Abstract
Case series
Patients: Female, 29-year-old • Female, 25-year-old • Male, 24-year-old
Final Diagnosis: Xeroderma pigmentosum
Symptoms: Decreased visual acuity • red eye
Medication: —
Clinical Procedure: —
Specialty: Ophthalmology
Objective:
Rare disease
Background:
Xeroderma pigmentosum (XP) is an autosomal recessive disease caused by mutations in DNA repair genes. Clinical manifestations include extreme sensitivity to ultraviolet (UV) rays, freckle-like pigmentation, ocular abnormalities, and an increased risk of developing neoplasms in sun-exposed areas of the skin, mucous membranes, and eyes. This paper describes the clinical outcome of pegylated interferon alpha 2b (PEG-IFN-α-2b) subconjunctival injections and topical mitomycin C (MMC) in the treatment of ocular surface squamous neoplasia (OSSN) in patients with XP.
Case Reports:
A series of 3 patients with histopathologically-proven biopsy specimens of XP-associated neoplasia of the eyelids and ocular surface underwent subconjunctival injections of PEG-IFN-α-2 band topical cycles of MMC. There was a noticeable decrease in the size and severity of ocular surface squamous neoplasia, with minimal adverse effects of flu-like symptoms with mild fever and generalized malaise. Transient mental depression was reported in 2 of our patients, and only 1 patient developed autoimmune diabetes mellitus, which required insulin therapy after the discontinuation of the PEG-IFN-α-2b.
Conclusions:
The literature on the specifics of ocular care using PEG-IFN-α-2b for XP-associated OSSN is sparse. However, according to our clinical experience, the combination of PEG-IFN-α-2b subconjunctival injection and the topical cycles of MMC is a promising long-term medical therapy to minimize the development and recurrence of OSSN in XP patients.
MeSH Keywords: DNA, Neoplasm; Interferon-alpha; Mitomycin; Xeroderma Pigmentosum
Background
Xeroderma pigmentosum (XP) is an autosomal recessive disease caused by mutations in DNA repair genes [1]. It has an estimated prevalence of 1 per million in the United States and Europe [2], 15–20 per million in Saudi Arabia [3], and 1: 20 000 in Japan [4].
XP can be classified into 7 complementation groups (XP-A to XP-G plus a variant group called XPV) and the clinical manifestations can be quite variable, not only between groups, but also within a group or even within an individual family [5,6]. These clinical manifestations include extreme sensitivity to ultraviolet (UV) rays, freckle-like pigmentation, ocular abnormalities, and a greater than 10 000-fold increased risk of developing neoplasms in sun-exposed areas of the skin, mucous membranes, and eyes [1,5]. According to previous reports in the literature, XP-C is the most common form of XP reported in the Arabian gulf region [3].
There is a growing body of evidence on the effectiveness of using interferon alpha 2b (IFN-α-2b) and mitomycin C (MMC) as primary or adjuvant medical treatment of ocular surface squamous neoplasia (OSSN) [7,8]. The combination of topical MMC and IFN-α-2b is currently considered an effective treatment approach for OSSN in XP patients and avoids the need for surgical intervention [9–11]. The effectiveness of pegylated interferon alpha 2b (PEG-IFN-α-2b) has previously been reported in a pilot study, concluding that it is a viable medical alternative for the treatment of OSSN [12]. Nonetheless, we were unable to find any randomized control trials comparing the clinical outcome of pegylated and non-pegylated IFN-α-2b. In this paper, we report a series of 3 patients with XP and histopathologically-proven biopsy specimens of OSSN that were seen at the Ophthalmology Department in King Faisal Specialist Hospital & Research Center (KFSH&RC) and treated with subconjunctival injections of PEG-IFN-α-2b (1 million IU/mL) at the site of the lesion with topical cycles of MMC 0.02% eye drops. All patients were monitored every 2 weeks with external eyelids, regular slit lamp, and dilated fundus examinations. To the best of our knowledge, this is the first report in the English literature to present the clinical outcome of peg-IFN a2b and MMC for the treatment of OSSN in patients with XP.
Case Reports
Case 1
A 29-year-old Saudi woman with XP-C presented with an ocular lesion on the left eye. Her past medical history was significant for nodular goiter and diabetes mellitus. On ocular examination, the left eye had a vascularized lesion on the corneal surface with pink irregular masses extending to the surrounding conjunctiva close to (but not reaching) the superior-medial conjunctival fornix with a 360-degree limbal tumor growth (Figure 1B). Her visual acuity was 20/70 in the right eye and only light perception in the left eye.
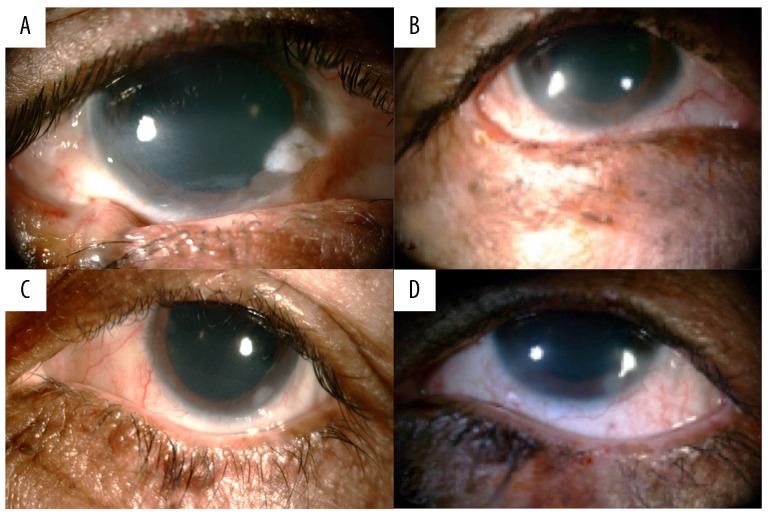
Figure 1.
Three images of the left eye from Case 1, taken 3 years apart. (A) Baseline before current presentation. (B) Left eye at time of presentation, showing vascularized lesion on the corneal surface with pink irregular masses extending to the surrounding conjunctiva. (C) Taken at 18 months of treatment, showing opaque cornea with severe fibrosis and no active lesions.
The histopathology results showed squamous cell carcinoma (SCC) and she was started on subconjunctival PEG-IFN-α-2b injections (3 million IU/0.5 mL) alone every 2 weeks for 2 months. At 8-week follow-up, the tumor was found to be smaller in size but did not resolve completely, as she tended to miss her follow-up appointments.
Then, she was lost to follow-up for 4 months while recovering from a uterine surgery, and presented with a 3-mm recurrent corneal tumor in the left eye, with a high-grade squamous cell dysplasia. She was started on a combination of subconjunctival PEG-IFN-α-2b injections (3 million IU/0.5 mL) every 4 weeks with intervening topical chemotherapy MMC 0.02% formulated eye drops cycles.
She received a total of 11 subconjunctival PEG-IFN-α-2b injections and 19 cycles of topical chemotherapy with MMC 0.02% formulated eye drops for 2 years. The only adverse effect reported by this patient was flu-like symptom with mild fever and generalized malaise, which resolved after a single dose of acetaminophen 650 mg. This patient did not develop transient mental depression as an adverse effect.
On follow-up, her tumors gradually reduced in size and became undetectable (Figure 1C). At 18 months of treatment, the patient was clinically free of tumors. Biopsies taken at month 18 and month 23 of treatment were also negative for any malignancy. However, her cornea remains opaque from the severe fibrosis (Figure 1C compared to the baseline in Figure 1A) and the visual acuity mildly improved: 20/50 in the right eye (OD) and brisk hand motion at half a meter in the left eye (OS). Moreover, the patient was following up with the Dermatology clinic for skin surface tumors, which were treated as recurrent basal cell carcinoma (BCC) on the face and hands. The patient was informed about the proper use of sun blockers and the importance of covering sun-exposed areas. She was also covering her arms and face (including the eyes) using the Saudi traditional dress for women as a UV-protective measure.
Case 2
A 25-year-old Saudi woman with XP-C presented with multiple OSSN in both eyes. On ocular examination, her visual acuity was 20/30 OD and 20/30 OS. The IOP was 21 mmHg in both eyes (OU). In the right eye, the lateral third of the lower eyelid had a full-thickness BCC extending to the right lateral canthus, and the ocular surface had a lateral palpebral conjunctival lesion. Also, in the right eye, the corneal limbus was involved at 360 degrees by an irregular hazy strip of abnormal growth. The strip thickens at 05: 00 position into a tumor mass with whitish color (Figure 2A). In the left eye, the cornea had limbal 360-degree involvement with an irregular hazy white limbal growth, which was identified as fibrosis, with no malignant cells on biopsy (Figure 2C). Both eyes had melanocytic conjunctival areas with atypia. Irises of both eyes had dark-colored nevi. The fundus exam showed pigmentary retinal degeneration in the right eye only.
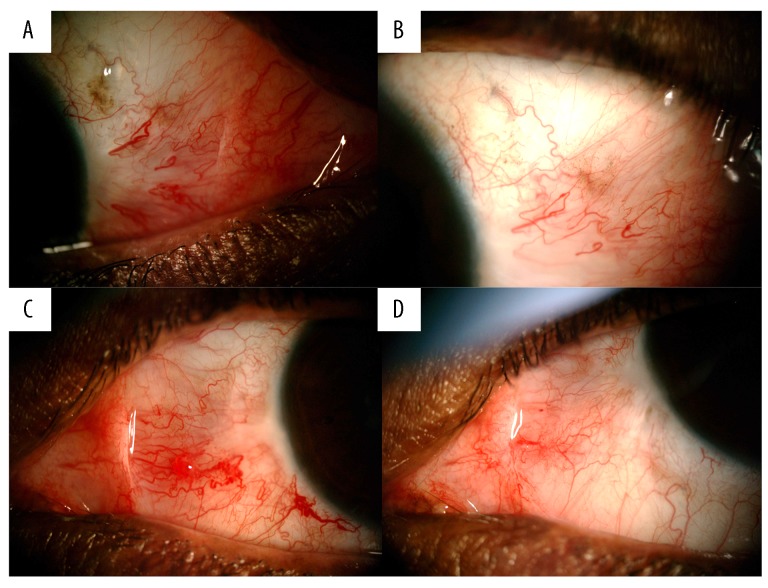
Figure 2.
Four images from Case 2 taken 2 years apart. (A) Right eye before treatment with basal cell carcinoma involving the lateral third of the lower eyelid and extending to the right lateral canthus. (B) Right eye after surgical excision and 21 months of therapy. (C) Left eye before treatment, showing the cornea with the limbal 360-degree involvement by an irregular hazy white growth which was identified as fibrosis with no malignant cells on biopsy. (D) Left eye after surgical excision and 21 months of therapy.
As the histopathology showed BCC, this patient underwent surgical excision and removal of the lesion followed by adjuvant bilateral subconjunctival PEG-IFN-α-2b injection (3 million IU/0.5 mL) in each eye. Injections were given 9 times, 2 weeks apart over 14 months, with an intervening 15 cycles of MMC 0.02% (0.2 mg/ml) formulated eye drops, for the squamous dysplasia and the ocular melanosis with atypia.
Bilateral subconjunctival PEG-IFN-α-2b injection (3 million IU/0.5 mL) in each eye was given for a total of 21 months from June 2015 until March 2017. At her last visit, the patient continued to show significant improvement and remained free from any recurring OSSN (Figure 2B, 2D).
Adverse effects encountered during treatment included transient mental depression and flu-like symptoms with mild fever and generalized malaise that resolved after a single dose of acetaminophen 650 mg. No intervention was needed for the transient mental depression. Also, this patient developed leukopenia soon after the second injection and autoimmune diabetes mellitus at around the 10th injection. She was started on intensive insulin therapy with close monitoring of her blood glucose levels, and needed insulin therapy after the discontinuation of subconjunctival PEG-IFN-α-2b injection. Moreover, the patient was following up with the Dermatology Department for resection of nodular melanoma tumors on the scalp. The patient was informed about the proper use of sun blockers and the importance of covering sun-exposed areas. She was also covering her arms and face (including the eyes) using the Saudi traditional dress for women as a UV-protective measure.
Case 3
A 24-year-old Saudi man with XP-C (and a positive family history of XP) presented with ocular surface melanosis, congested conjunctival areas, and irregular vascularization.
On examination, the right lateral canthus had scars from a previous surgical excision of a tumor. Conjunctival map biopsies showed residual right eye focal squamous cell carcinoma in situ (SCC in situ) at 03: 00 limbal and a focal epithelial dysplasia at the 07: 00 limbal area (Figure 3A). The left eye showed a focal epithelial dysplasia at 04: 00 limbal conjunctiva (Figure 3C). The patient was prescribed 2 cycles of MMC 0.02% formulated eye drops.
Figure 3.
Four images of Case 3 taken 2 years apart. (A) Post-surgical excision on the right eye, showing focal squamous cell carcinomas in situ at 03: 00 limbal area. (B) Right eye after 18 months of therapy. (C) Post-surgical excision on left eye showing focal epithelial dysplasia at limbal conjunctiva with irregular vascularization. (D) Left eye after 18 months of therapy.
Four years later, he presented to the clinic with a conjunctival mass on the left eye. An excisional biopsy was sent to Pathology and showed high-grade squamous dysplastic changes of 0.5×0.5×0.3 cm. His visual acuity was 20/40 in the right eye and 20/30 in the left eye. Both eyes had an IOP of 21 mmHg.
He was started on subconjunctival PEG-IFN-α-2b injection of (3 million IU/0.5 mL) and received a total of 4 injections given 2–4 weeks apart. He remained stable, with no new lesions at 18 months of treatment (Figure 3B, 3D). The only adverse effect reported by the patient was transient mental depression, which did not require any intervention, and flu-like symptoms with mild fever and generalized malaise, which resolved after a single dose of acetaminophen 650 mg. The patient was following up with the Dermatology clinic and underwent chemical peeling and surgical excision of multiple facial basal cell carcinomas. He was informed about the proper use of sun blockers and the importance of covering sun-exposed areas. He was using sunglasses to protect his eyes from UV exposure while outdoors, and his arms and scalp were covered with the traditional dress of Saudi Arabia.
Discussion
All patients presented with XP – group C, which is the most common group of XP in the Arabian Gulf region [3]. About 40% of patients with XP develop ocular abnormalities caused by UV-induced DNA alteration to epithelial cells of the conjunctiva, the cornea, and the eyelid [3]. Continuous sunlight exposure can result in photophobia associated with prominent conjunctival injection, and severe keratitis, leading to vascularization and corneal opacification, hyperpigmentation of the eyelids, and loss of lashes [13].
Complete surgical excision with visible clear margins and intra-operative cryotherapy is considered the traditional treatment of OSSN [11]. Nonetheless, extensive surgical excision is associated with stem cell deficiency, which can be prevented by the use of medical therapy, as it also has the theoretical advantage of treating the entire ocular surface [12].
Complete control in 95% of cases can be achieved using interferon alpha 2b (IFN-α-2b) drops, alone or with intralesional injections, when given as a standalone treatment or appropriately combined with surgical excision [14]. The drops are reserved for cases that only involve the cornea, while intralesional injections are used for cases that involve both the cornea and conjunctiva. The exact mechanism of IFN-α-2b in the treatment of OSSN remains unclear, but it was proven to be an efficient and cost-effective treatment modality among Asian Indian patients [15]. Also, IFN-α-2b and topical MMC were found to be effective in the management of OSSN and ocular melanosis with atypia [16].
Since the development of new treatments for hepatitis C, the use and importation of IFN-α-2b injections and eye drops have progressively declined in our hospital. Thus, we had to rely on the use of PEG-IFN-α-2b injections instead, and it became a viable alternative to IFN-α-2b due to its longer half-life, which provided a longer interval between injections, and improved compliance [17].
We found that the combination of PEG-IFN-α-2b subconjunctival injection every 4 weeks with intervening topical cycles of MMC formulated eye drops is a practical approach to treating OSSN, especially for patients who do not keep follow-up appointments or are unwilling to undergo biweekly injections. The use of MMC 0.02% formulated eye drops was tolerated for prolonged cycles of treatment up to 10 weeks along with lubricant drops.
The main adverse effect observed with subconjunctival injections of PEG-IFN-α-2b in all 3 patients was flu-like symptoms with mild fever and generalized malaise, which resolved within 1 day of treatment with acetaminophen 650 mg, q6 hours. Only 1 of the patients (Case 2) developed leukopenia and auto-immune diabetes mellitus, which required insulin therapy after discontinuation of the PEG-IFN-α-2b. These complications may have developed due to the long-term use of PEG-IFN-α-2b, but we do not have sufficient data to support causation in this patient. Nonetheless, previous studies have shown an association between type-1 diabetes mellitus and PEG-IFN-α-2b in the treatment of hepatitis C, so it would be advisable to consider the possibility of onset of type 1 diabetes mellitus in patients receiving PEG-IFN-α-2b therapy [18].
These 3 cases were referred from the Dermatology Department for ocular evaluation, and they were concurrently evaluated by the Dermatology and Ophthalmology Departments. XP can be associated with multiple neurologic findings such as reduced cognition and hearing defects. However, as our patients did not present with a history of neurological involvement, the Neurology Department was not involved in the care of these patients. Moreover, we also found that PEG-IFN-α-2b treatment was associated with transient mental depression, and multiple studies in the literature have reported that pegylated IFN-α used in the treatment of hepatitis C can induce major depression, and it can do so even in patients without a history of major depression disorders. Moreover, prophylactic therapy can be considered for euthymic patients, as it can trigger a distinct condition of worsening hostility [19]. All 3 cases underwent psychiatric evaluation before administering the treatment, and they were cleared for therapy. Further psychiatric evaluation was provided to the 2 patients who reported transient mental depression after onset of therapy. This highlights the need for developing an integrated and holistic approach to patient care in the Ophthalmology clinic to provide these patients with education, social support, and psychological evaluation before and after therapy.
Finally, XP is more common in populations with a high prevalence of consanguineous marriages [13]. Thus, genetic counseling may be indicated in the management of our patients, as all 3 cases had a strong family history of XP and consanguineous marriages. Early diagnosis and intervention are vital to keep the development of cutaneous cancers to a minimum, as the rapid progression of these tumors, particularly in the cornea and limbus, can cause blindness. The use of subconjunctival injections of PEG-IFN-α-2b and the topical cycles of MMC showed positive outcomes in our patients. However, MMC produces a variety of adducts with DNA, including inter-strand cross-links (ICLs) and xeroderma pigmentosum (XP) proteins, including XPG, XPE, and XPF. Moreover, there are multiple studies in the literature linking MMC with various types of DNA damage that cause significant cytotoxicity to cells. Therefore, as XP patients already have defective DNA repair, the long-term use of MMC may not be feasible, and follow-up of the patients may be warranted for a few years after therapy to monitor for recurrences [20,21]. Thus, there is a need for the development of PEG-IFN-α-2b eye drops, as XP patients can require lifelong monitoring and treatment to prevent recurrences or formation of new OSSN [11].
Conclusions
The literature on the specifics of ocular care using PEG-IFN-α-2b for XP-associated OSSN is sparse. However, according to our patient experience, the combination of PEG-IFN-α-2b subconjunctival injection and the topical cycles of MMC is a promising long-term medical therapy to prevent development and recurrence of OSSN in XP patients.
Acknowledgments
Dr. Doaa Alshammari, Ophthalmic Photographer, Ophthalmology Department, King Faisal Specialist Hospital and Research Center.
Footnotes
Department and Institution where work was done
Department of Ophthalmology, King Faisal Specialist Hospital and Research Center, Riyadh, Saudi Arabia
Conflicts of interest
None.
References:
- 1.Brooks BP, Thompson AH, Bishop RJ, et al. Ocular manifestations of xeroderma pigmentosum: Long-term follow-up highlights the role of DNA repair in protection from sun damage. Ophthalmology. 2013;120(7):1324–36. doi: 10.1016/j.ophtha.2012.12.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kleijer WJ, Laugel V, Berneburg M, et al. Incidence of DNA repair deficiency disorders in western Europe: Xeroderma pigmentosum, Cockayne syndrome and trichothiodystrophy. DNA Repair (Amst) 2008;7(5):744–50. doi: 10.1016/j.dnarep.2008.01.014. [DOI] [PubMed] [Google Scholar]
- 3.Alwatban L, Binamer Y. Xeroderma pigmentosum at a tertiary care center in Saudi Arabia. Ann Saudi Med. 2017;7(3):240–44. doi: 10.5144/0256-4947.2017.240. 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hirai Y, Kodama Y, Moriwaki SI, et al. Heterozygous individuals bearing a founder mutation in the XPA DNA repair gene comprise nearly 1% of the Japanese population. Mutat Res. 2006;601(1–2):171–78. doi: 10.1016/j.mrfmmm.2006.06.010. [DOI] [PubMed] [Google Scholar]
- 5.Lehmann AR, McGibbon, Stefanini M. Xeroderma pigmentosum. Orphanet J Rare Dis. 2011;6:70. doi: 10.1186/1750-1172-6-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kraemer KH, DiGiovanna JJ. Xeroderma pigmentosum. Seattle: University of Washington; Seattlee: 2003. [PubMed] [Google Scholar]
- 7.Al Bayyat G, Arreaza-Kaufman D, Venkateswaran N, et al. Update on pharmacotherapy for ocular surface squamous neoplasia. Eye Vis (Lond) 2019;6:24. doi: 10.1186/s40662-019-0150-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Basti S, Macsai MS. Ocular surface squamous neoplasia: A review. Cornea. 2003;22(7):687–704. doi: 10.1097/00003226-200310000-00015. [DOI] [PubMed] [Google Scholar]
- 9.Shah SU, Kaliki S, Kim HJ, et al. Topical interferon alfa-2b for management of ocular surface squamous neoplasia in 23 cases: Outcomes based on american joint committee on cancer classification. Arch Ophthalmol. 2012;130(2):159–64. doi: 10.1001/archophthalmol.2011.385. [DOI] [PubMed] [Google Scholar]
- 10.Cradoso Pinto NQ, de Paula Araujo Ferreira J, Mendes Carneiro GJA, et al. Topical Interferon alfa-2b for ocular surface squamous neoplasia in one case of patient with xeroderma pigmentosum. Rev Bras Oftalmolmol. 2017;76(4):202–6. [Google Scholar]
- 11.Kalamkar C, Radke N, Mukherjee A, Radke S. Xeroderma pigmentosum with bilateral ocular surface squamous neoplasia and review of the literature. BMJ Case Rep. 2016;2016:bcr2016215364. doi: 10.1136/bcr-2016-215364. : pii: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Karp CL, Galor A, Lee Y, Yoo SH. Pegylated interferon alpha 2b for treatment of ocular surface squamous neoplasia: A pilot study. Ocul Immunol Inflamm. 2010;18(4):254–60. doi: 10.3109/09273948.2010.486687. [DOI] [PubMed] [Google Scholar]
- 13.Mareddy S, Reddy J, Babu S, Balan P. Xeroderma pigmentosum: Man deprived of his right to light. ScientificWorldJournal. 2013:534752. doi: 10.1155/2013/534752. 2 013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shields CL, Kaliki S, Kim HJ, et al. Interferon for ocular surface squamous neoplasia in 81 cases: Outcomes based on the American Joint Committee on Cancer classification. Cornea. 2013;32(3):248–56. doi: 10.1097/ICO.0b013e3182523f61. [DOI] [PubMed] [Google Scholar]
- 15.Kaliki S, Singh S, Iram S, Tripuraneni D. Recombinant interferon alpha 2b for ocular surface squamous neoplasia: An efficient and cost-effective treatment modality in Asian Indian patients. Indian J Ophthalmol. 2016;64(10):702–9. doi: 10.4103/0301-4738.195010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Besley J, Pappalardo J, Lee GA, et al. Risk factors for ocular surface squamous neoplasia recurrence after treatment with topical mitomycin c and interferon alpha-2b. Am J Ophthalmol. 2014;157(2):287–93.e2. doi: 10.1016/j.ajo.2013.10.012. [DOI] [PubMed] [Google Scholar]
- 17.Karp CL, Galor A, Chhabra S, et al. Subconjunctival/perilesional recombinant interferon α2b for ocular surface squamous neoplasia: A 10-year review. Ophthalmology. 2010;117(12):2241–46. doi: 10.1016/j.ophtha.2010.03.052. [DOI] [PubMed] [Google Scholar]
- 18.Nakamura K, Kawasaki E, Imagawa A, et al. Type 1 diabetes and interferon therapy: A nationwide survey in Japan. Diabetes Care. 2011;34(9):2084–89. doi: 10.2337/dc10-2274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lotrich FE, Rabinovitz M, Gironda P, Pollock BG. Depression following pegylated interferon-alpha: Characteristics and vulnerability. J Psychosom Res. 2007;63(2):131–35. doi: 10.1016/j.jpsychores.2007.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ahn B, Kang D, Kim H, Wei Q. Repair of mitomycin C cross-linked DNA in mammalian cells measured by a host cell reactivation assay. Mol Cells. 2004;18(2):249–55. [PubMed] [Google Scholar]
- 21.Blasiak J. DNA-damaging anticancer drugs – a perspective for DNA repair – oriented therapy. Curr Med Chem. 2017;24(15):1488–503. doi: 10.2174/0929867324666170124145557. [DOI] [PubMed] [Google Scholar]