In a previous issue of Clinical Endocrinology, Leow et al. 1 describe a post‐SARS (severe acute respiratory syndrome) condition characterized by mild sickness syndrome manifestations (malaise, anorexia, fatigue, myalgia) and transient, mild hypoactivation of the hypothalamic–pituitary–adrenal (HPA) axis. The authors have provided well‐collected and analysed data obtained in difficult clinical circumstances on an infectious condition that is potentially lethal. The phenomenon described is robust and reminiscent of other postviral infection syndromes. However, some of the endocrine findings in this study are of uncertain value and some of the secondary conclusions conjectural. In this brief editorial, we will try to put the phenomenon described in this remarkable study into a more general perspective.
The symptomatology of the post‐SARS sickness syndrome manifestations can hardly be contested, given that they were of sufficient severity to warrant presentation to the caring physicians. In addition, one can hardly contest the concurrent mild hypocortisolism examined by the well‐accepted time‐integrated measure of 24‐h urinary free cortisol excretion. 2 Caution should, however, be exercised on conclusions based on HPA axis evaluation during the morbid state of SARS, and the validity of single, low‐dose ACTH stimulation tests is dubious as an unquestionable index of low or high HPA axis activity. 2 This is because the initial test was performed during a time of major physical and emotional stress, while subsequent short synacthen tests used a single submaximal dose of the peptide. The short, low‐dose synacthen test has considerable intraindividual variability, even when a stress‐producing condition is stable. 3 , 4 This assessment would have been more valid if a number of doses of synacthen were used to span the dose–response curve.
The findings of Leow et al. 1 have added the post‐SARS sickness syndrome and hypocortisolism to a long list of mostly transient conditions that are characterized by sudden reversal of a state of chronic cortisol hypersecretion (Table 1). These include prolonged regular exercise, states of chronic stress, treatment of Cushing's syndrome and cessation of exogenous glucocorticoids. 5 , 6 , 7 In the same list one could include the premenstrual, postpartum and perimenopausal periods, the post‐traumatic stress disorder in adults, the abrupt cessation of chronic smoking, the chronic fatigue syndrome (CFS) and fibromyalgia (FM) and other chronic pain and fatigue syndromes. 5 , 6 , 7
Table 1.
States associated with decreased hypothalamic–pituitary–adrenal (HPA) axis activity (Modified with permission from Journal of the American Medical Association 5 )
| Adrenal insufficiency (Addison's disease) |
| Glucocorticoid withdrawal states |
| Post stress period |
| Post abrupt cessation of regular chronic exercise |
| After Cushing syndrome cure |
| Post discontinuation of glucocorticoid therapy |
| Oestrogen and CRH withdrawal syndromes |
| Premenstrual tension syndrome |
| Postpartum period |
| Perimenopausal period |
| Atypical/seasonal depression |
| Chronic fatigue syndrome |
| Fibromyalgia |
| Other chronic pain and fatigue states |
| Hypothyroidism |
| Nicotine withdrawal |
CRH, corticotropin‐releasing hormone.
Sickness syndrome is generated primarily by activated immune and immune‐related cells via proinflammatory cytokines, such as tumour necrosis factor‐alpha (TNF‐α), the interleukins (IL)‐1, IL‐6 and IL‐8, and other nonpeptide mediators of inflammation. 8 It includes symptoms such as malaise, somnolence, fatigue, anorexia with or without nausea, and hyperalgesia with or without headache (Table 2). As a product of active systemic inflammation, sickness syndrome is accompanied by activation of the acute‐phase reaction and the pain and fatigue system, with which it represents an extremely important composite biological programme responsible for generating behaviours and somatic responses that protect us from tissue damage and allow time and energy for a speedy and efficient tissue repair. 8 An immune and inflammatory reaction of sufficient magnitude, however, through the proinflammatory cytokines, also activates the HPA axis, which to some extent serves as a valuable negative feedback system that prevents this reaction from overshooting. 8
Table 2.
The immune and inflammatory response generates the sickness syndrome, i.e., the sickness behaviour, the pain and fatigue response and the acute‐phase reaction. The classic stress syndrome is mostly antagonistic to the sickness syndrome (Modified with permission from Annals of the New York Academy of Sciences 8 )
| Sickness syndrome | Classic stress syndrome | |
|---|---|---|
| Sickness behaviourPain and fatigue response Acute‐phase reaction | Anorexia/nausea | Anorexia/stimulation of appetite* |
| Fatigue and/or depressed affect | Motivation/stimulated affect | |
| Somnolence | Arousal | |
| Hyperalgesia ± headache | Analgesia | |
| Elevated temperature/fever | Pyretic/antipyretic* | |
| Increased metabolic rate | Increased metabolic rate/return to normal* | |
| Acute‐phase reaction +++++ | Acute‐phase reaction + | |
| Cellular effectors | Immune and immune‐related cells, Neurones, endocrine cells | Immune and immune‐related cells |
| Neurones, endocrine cells | ||
| Molecular effectors | Inflammatory cytokines/mediators, immune CRH | CRH, AVP, glucocorticoids, catecholamines, immune |
| CRH, acetylcholine | ||
| Transcription factors: GR, NF‐κB, CREB, AP1, STATs | Transcription factors: GR, NF‐κB, CREB, AP1, STATs |
Initial stimulation via CRH and catecholamines, then inhibition by glucocorticoids.
AP1, activating protein 1; AVP, arginine‐vasopressin; CREB, cAMP response element‐binding protein; CRH, corticotropin‐releasing hormone; GR, glucocorticoid receptor; NF‐κB, nuclear factor kappa B; STAT, signal transducer and activator of transcription.
One to 5 +, degree of activation.
Indeed, the HPA axis, a major component of the stress system of the organism, suppresses the secretion of the proinflammatory cytokines and other mediators of inflammation and renders their target tissues resistant to these proinflammatory molecules 8 , 9 (Fig. 1). Hence, when properly activated, this axis diminishes the manifestations of sickness syndrome and the activity of the pain and fatigue response. 8 Acute Addison's disease is associated with varying degrees of sickness syndrome manifestations because the intrinsic levels of cortisol are insufficient to counteract the proinflammatory molecules that generate the syndrome. 8 , 10 , 11 , 12 These manifestations may vary from a very mild sickness syndrome all the way to circulatory collapse and death, when an immune and inflammatory reaction has become unconstrained and uncompensated. Even slight hypocortisolism of the degree detected in the post‐SARS period could explain the presence of the mild sickness syndrome manifestations in these patients.
Figure 1.
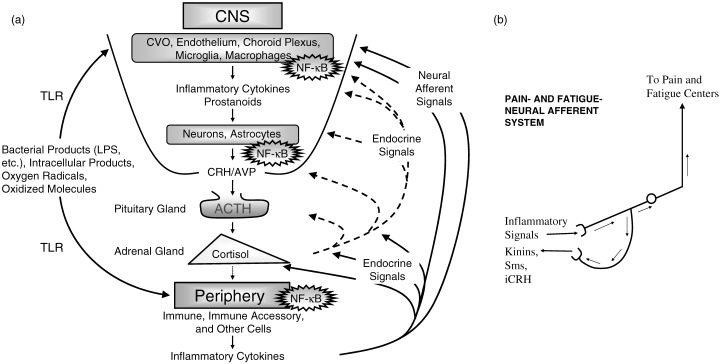
(a) Activation of the immune and inflammatory response of any aetiology leads to peripheral production and/or circulation of proinflammatory agents, which, through endocrine or neural afferent signals, stimulate a central nervous system (CNS) inflammatory cascade, cause manifestations of the sickness syndrome and spur the hypothalamic–pituitary–adrenal (HPA) axis at all levels. Note the involvement of NF‐κB, a major proinflammatory transcription factor in both CNS and peripheral inflammation. On the other hand, the activated HPA axis, through its end‐hormone, cortisol, and its receptor (GR), inhibits CNS and peripheral inflammation, as well as its own activity. (b) The presence of increased proinflammatory cytokines and other agents in the vicinity of peripheral somatic and autonomic afferent nerves decreases the pain and fatigue threshold of an individual and hence produces hyperalgesia and fatigue. This is further accentuated by post‐stress hypocortisolism and diminished by cortisol elevations or administration. iCRH, immune corticotropin‐releasing hormone; Sms, somatostatin; TLR, Toll‐like receptor.
If we rule out persistent infection by the SARS virus or residual post‐SARS myopathy as two nonmutually exclusive explanations for the post‐SARS syndrome described in this study, the sickness syndrome manifestations and the hypocortisolism demonstrated may represent a generic, transient adaptive response following a major stressful event, which improves the speed and quality of recovery of the organism after major stress. What are the mechanisms that generate this post‐stress syndrome, and is it possible that some patients are more prone to develop it than others? In our opinion, this syndrome is produced by a period of prolonged central nervous system suppression of the HPA axis that results when a major stressor, in this case the virus, is of sufficient magnitude and duration that it causes sustained hypercortisolism. The degree and duration of this post‐stress neuroendocrine HPA axis alteration, the activity of the immune system that generates the sickness syndrome and the sensitivity of the pertinent target tissues to glucocorticoids and cytokines are defined by genetic and developmental/constitutional factors, which determine whether an individual is more prone or more resistant to developing the syndrome. It is quite likely that syndromes such as CFS, FM, and other chronic pain and fatigue states represent pathological conditions in which such an important adaptive biological programme has gone awry, has lost its adaptive value, and in fact prevents healthy functioning of the suffering individual. 6
The real practical question is on what should be done with patients with post‐SARS sickness syndrome manifestations and hypocortisolism. It is obvious that patients with a truly subnormal standard, high‐dose ACTH test should be treated for adrenal insufficiency with glucocorticoids, as the current standards of care dictate. 2 However, in all others, who appear to be the majority of those with the syndrome, in the absence of data, a conservative approach should be taken. We do not treat patients with the euthyroid sick syndrome, which is an adaptive state that conserves energy in an individual that is under stress. On the same logical basis, we should probably not administer exogenous glucocorticoids for what is essentially an adaptive response of the HPA axis after major or prolonged stress. We recognize that there are no data to support this opinion at the present time and that properly designed, double‐masked and placebo‐controlled studies should be undertaken to test this hypothesis.
See Clinical Endocrinology, 63, 197–202.
References
- 1. Leow, M.K.‐S. , Kwek, D.S.‐K. , Ng, A.W.‐K. , Ong, K.‐C. , Kaw, G.J.‐L. & Lee, L.S.‐U. (2005) Hypocortisolism in survivors of severe acute respiratory syndrome (SARS). Clinical Endocrinology, 63, 197–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chrousos, G.P. & Harris, A.G. (1998) Hypothalamic–pituitary–adrenal axis suppression and inhaled corticosteroid therapy. Part I. General principles. Neuroimmunodulation, 5, 277–287. [DOI] [PubMed] [Google Scholar]
- 3. Demitrack, M. , Dale, J. , Straus, S. , Laue, L. , Listwak, S. , Kruesi, M. , Chrousos, G.P. & Gold, P.W. (1991) Evidence of impaired activation of the hypothalamic–pituitary–adrenal axis in patients with chronic fatigue syndrome. Journal of Clinical Endocrinology and Metabolism, 73, 1224–1234. [DOI] [PubMed] [Google Scholar]
- 4. Laue, L. , Peck, G. , Gallucci, W.T. , Loriaux, D.L. & Chrousos, G.P. (1991) Adrenal androgen secretion in postadolescent cystic acne: increased adrenocortical function without hypersensitivity to ACTH. Journal of Clinical Endocrinology and Metabolism, 73, 380–384. [DOI] [PubMed] [Google Scholar]
- 5. Chrousos, G.P. & Gold, P.W. (1992) The concepts of stress and stress system disorders: overview of physical and behavioral homeostasis. Journal of the American Medical Association, 267, 1244–1252. [PubMed] [Google Scholar]
- 6. Clauw, D.J. & Chrousos, G.P. (1997) Chronic pain and fatigue syndromes: overlapping clinical and neuroendocrine features and potential pathogenic mechanisms. Neuroimmunomodulation, 4, 134–153. [DOI] [PubMed] [Google Scholar]
- 7. Glass, J.M. , Lyden, A.K. , Petzke, F. , Stein, P. , Whalen, G. , Ambrose, K. , Chrousos, G. & Clauw, D.J. (2004) The effect of brief exercise cessation on pain, fatigue, and mood symptom development in healthy, fit individuals. Journal of Psychosomatic Research, 57, 391–398. [DOI] [PubMed] [Google Scholar]
- 8. Chrousos, G.P. (2000) The stress response and immune function: clinical implications, the 1999 Novera H. Spector lecture. Annals of the New York Academy of Sciences, 917, 38–67. [DOI] [PubMed] [Google Scholar]
- 9. Meduri, G.U. , Tolley, E.A. , Chrousos, G.P. & Stentz, F. (2002) Prolonged methylprednisolone treatment suppresses systemic inflammation in patients with unresolving ARDS: evidence for inadequate endogenous glucocorticoid secretion and inflammation‐induced immune cell resistance to glucocorticoids. American Journal of Respiratory and Critical Care Medicine, 165, 983–991. [DOI] [PubMed] [Google Scholar]
- 10. Papanicolaou, D.A. , Tsigos, C. , Oldfield, E.H. & Chrousos, G.P. (1996) Acute glucocorticoid deficiency is associated with plasma elevation of interleukin‐6: does the latter participate in the symptomatology of the steroid withdrawal syndrome and adrenal insufficiency? Journal of Clinical Endocrinology and Metabolism, 81, 2303–2306. [DOI] [PubMed] [Google Scholar]
- 11. Papanicolaou, D.A. , Petrides, J.S. , Tsigos, C. , Bina, S. , Kalogeras, K.T. , Wilder, R. , Gold, P.W. , Deuster, P.A. & Chrousos, G.P. (1996) Exercise stimulates interleukin‐6 secretion: inhibition by glucocorticoids and correlation with catecholamines. American Journal of Physiology, E601–E605. [DOI] [PubMed] [Google Scholar]
- 12. Hochberg, Z. , Pacak, K. & Chrousos, G.P. (2003) Endocrine withdrawal syndromes. Endocrine Reviews, 24, 523–548. [DOI] [PubMed] [Google Scholar]


