Approach to primary immunodeficiency in children and adults
S1 Classification of primary immunodeficiencies
C. Picard* (Paris, FR)
Human primary immunodeficiencies (PIDs) comprise a broad group of inherited disorders characterised by developmental or functional defects of myeloid or lymphoid haemapoietic-derived cells, as well as non-haemapoietic cells involved in protective immunity. More than 150 different forms of PIDs affecting distinct components of the innate and adaptive immune system, such as neutrophils, macrophages, dendritic cells, complement proteins, natural killer cells, and T and B lymphocytes have been described [1]. Clinically, PIDs can be associated with any combination of infectious disease, autoimmunity, auto-inflammatory, allergy and malignancy. The best known PIDs show Mendelian inheritance and first become symptomatic during childhood. However, the field of PIDs is rapidly expanding and PIDs showing non-Mendelian inheritance and/or affecting primarily adult patients is being increasingly recognized. Conventional PIDs are typically seen as rare monogenic conditions associated with detectable immunologic abnormalities, resulting in a broad susceptibility to multiple and recurrent infections caused by weakly pathogenic and more virulent microorganisms. By opposition to these conventional PIDs, nonconventional primary immunodeficiencies as Mendelian conditions manifesting in otherwise healthy patients as a narrow susceptibility to infections, recurrent or otherwise, caused by weakly pathogenic or more virulent microbes are now reported [2]. By now, up to 120 disease-causing genes have been identified. This molecular characterisation of PIDs has helped to increase our understanding of their physiopathology. The study of these diseases has provided essential insights into the functioning of the immune system with the ultimate goal of facilitating diagnosis and treatment.
S2 Clinical manifestations
N. Rezaei* (Tehran, IR)
Primary immunodeficiency diseases are a heterogeneous group of disorders, caused by inherited defects in the immune system, and characterised by wide spectrum of clinical manifestations, particularly an increased susceptibility to infections and a predisposition to autoimmune diseases and malignancies.
Recurrent infections or infection with unusual organisms are the most commonly presentation of primary immunodeficiency diseases. Although recurrent respiratory tract infections and gastrointestinal manifestations are the most common features of these diseases, especially in predominantly antibody deficiencies and combined immunodeficiencies, other organs can be involved as well. Recurrent cutaneous abscesses with unusual organisms or deep abscesses may represent infections with an association with immunodeficiencies, particularly in phagocytes defects. Meningococcal infections could have an association with complement deficiencies. Meanwhile other bacterial infections, mainly Streptococcus pneumoniae and Staphylococcus aureus, as well as infections with viruses, fungi and parasites are also common in several primary immunodeficiency diseases.
Autoimmune diseases such as idiopathic thrombocytopenic purpura, autoimmune haemolytic anaemia, systemic lupus erythematosus, juvenile arthritis, sclerosing cholangitis, and vasculitis are common in primary immunodeficiency diseases. Whilst some syndromic immunodeficiencies (e.g., Wiskott Aldrich syndrome, Di George syndrome) have a strong association with autoimmunity, there are a group of disorders (e.g., ALPS, APECED, IPEX) that the autoimmune manifestations are typically the first and most significant findings.
Malignancies are also common in some primary immunodeficiency diseases (e.g., CVID, ALPS, XLP, and DNA repair defects). Other manifestations such as dysmorphic features, associated anomalies, skeletal dysplasia, and oculocutaneous hypopigmentation can be unique characteristics of some cases with primary immunodeficiency diseases. The clinical manifestations of these diseases are often helpful in guiding the appropriate evaluation of the patients. Prompt and precise diagnostic laboratory evaluation should be performed in the patients with such features, whereas early diagnosis and successful management of these patients prevent irreparable organ system damage and improve the prognosis.
S3 Diagnosis
E. de Vries* ('s-Hertogenbosch, NL)
Immunodeficiency specialists from all over Europe have composed a multistage diagnostic protocol that is based on their expert opinion, in order to increase the awareness of PID among doctors working in different fields. The protocol starts from the clinical presentation of the patient; immunological skills are not needed for its use. A list of relevant symptoms and signs from the history and physical examination that should alert any physician to potential PID is given. These are grouped together to form eight typical clinical presentations of PID: recurrent ENT and airway infections; failure to thrive from early infancy; recurrent pyogenic infections; unusual infections or unusually severe course of infections; recurrent infections with the same type of pathogen; autoimmune or chronic inflammatory disease, or lymphoproliferation; characteristic combinations of clinical features in eponymous syndromes; and angioneurotic edema. These presentations lead the user towards different algorithms, which in fact represent the traditional division into antibody, complement, lymphocyte, and phagocyte deficiencies, respectively. The algorithms each are comprised of several steps. This multistage design allows cost-effective screening for PID within the large pool of potential cases in all hospitals in the early phases, while more expensive tests are reserved for definitive classification in collaboration with an immunologist at a later stage.
Update on HIV for the non-HIV expert
S5 Male circumcision – only for Sub-Saharan Africa?
G. Schmid* (Geneva, CH)
In 1986, articles suggesting that male circumcision (MC) decreased the risk of HIV infection appeared. Over the next 15 years, studies of two epidemiologic types – ecologic and observational – increasingly supported this contention. Ecologic studies showed strong correlations between prevalences of MC and HIV, e.g., tribes with low prevalences of MC had high prevalences of HIV infection. Observational cross-sectional studies showed that uncircumcised men had higher rates of HIV than circumcised men. Observational cohort studies confirmed these weaker study design findings. A systematic review of observational studies in 2000 found a relative risk (RR) of 0.42 (95% CI, 0.34–0.54), a 58% protective effect.
In 2005 and 2007, results from three randomised controlled trials, all from sub-Saharan Africa, were reported. Results were consistent, and the pooled RR of 0.42 (95% CI, 0.31–0.57) was identical to that of the observational studies. The protective effect in the three trials, found at about 21–24 months' follow-up, has been extended in one trial to a protective effect of 64% at 42 months of follow-up. WHO and UNAIDS have strongly endorsed MC as an effective HIV prevention strategy in generalised HIV epidemics where MC is uncommon.
What about Europe? MC is uncommon with an adult male prevalence of <20%. HIV incidence is low enough that MC for HIV prevention purposes is unlikely to have much impact. No public health authority recommends routine neonatal circumcision.
Increasingly, however, data are showing benefits of MC in addition to HIV prevention. Lessened risk of urinary tract infection in infants (RR 0.13, 95% CI 0.08–0.20) and lifetime avoidance of phimosis and associated conditions occur when MC is performed neonatally.
Other benefits occur in males circumcised at any age. MC protects against acquiring sexually transmitted infections characterised by genital ulcers–syphilis, chancroid and herpes–and possibly trichomoniasis. Circumcised men may be less likely to acquire HPV and are more likely to clear the infection. Through the protective effect against HPV, MC halves risk of penile cancer (RR 0.52, 95% CI 0.33–0.82) and partners of circumcised men are at lessened risk of cervical cancer.
Other issues must be considered in making public health decisions about MC. Cultural objections may occur, but MC in the developing world is readily accepted in non-circumcising societies. Studies of sexual pleasure and function have found no relationship to circumcision status. MC may be advised for subgroups, even if not for the entire population. And, surgical risk and cost must be considered.
While many sub-Saharan African countries are scaling up MC services to prevent HIV infection, public health agencies in many industrialised countries are reconsidering MC policies–the outcomes of both efforts are being followed with interest.
Prevention and management of acute otitis media: a case for the prudent use of antibiotics
S9 Bacteria and viruses in acute otitis media
T. Heikkinen* (Turku, FI)
Acute otitis media (AOM) is generally considered a bacterial infection that is treated with antibiotics. However, despite extensive use of broad-spectrum antibiotics for this condition, the clinical response to the treatment is often poor. This fact, together with vast clinical experience connecting AOM with viral respiratory infections, has prompted research into the role of viruses in AOM. To date, ample evidence from studies ranging from animal experiments to large clinical trials supports a crucial role for respiratory viruses in the aetiology and pathogenesis of AOM. In most cases, viral infection of the upper respiratory mucosa initiates the whole cascade of events that finally leads to the development of AOM as a complication. The pathogenesis of AOM involves a complex interplay between viruses, bacteria, and the host's inflammatory response. Recent studies indicate that with sensitive techniques viruses can be found in the middle-ear fluid in most children with AOM, either alone or together with bacteria. Viruses appear to enhance the inflammatory process in the middle ear, and they may profoundly impair the resolution of otitis media. It is important to understand, however, that our increasing knowledge of the importance of viruses in the etiopathogenesis of AOM does not diminish the central role of bacteria in AOM. Therefore, while viruses may explain many of the problems encountered in treating AOM, the ultimate decision on whether or not to treat AOM with antibiotics cannot be based solely on the degree of viral involvement in AOM.
S11 The role of guidelines
D. Spiro* (Portland, US)
The non-judicious use of antibiotics has lead to an epidemic in antimicrobial resistance. Acute otitis media (AOM) is the most common indication for use of antibiotics in children in the United States (US). Despite available evidence that supports a wait and see approach, most US physicians immediately prescribe antibiotics for the treatment of AOM.
The American Academy of Pediatrics published a guideline in 2004 that addressed the diagnosis and treatment of AOM. This guideline recommends the use of observation as a potential strategy for the treatment of AOM. The key components of this published guideline will be discussed, as well as the evidence and rationale that supports the use of observation as an initial strategy to treat AOM.
S12 The role of vaccination in the prevention of otitis media
R. Dagan* (Beer-Sheva, IL)
Otitis media (OM) is the most common bacterial infection in children aged <5 years for which antibiotic treatment is prescribed worldwide. Although most of the time this entity resolves spontaneously it is associated with morbidity, family dysfunction, antibiotic use and burden on the medical system. Efforts to reduce the burden of OM by vaccination have not been extremely rewarding, but some progress has been made. The first obvious step would be to reduce viral infections leading secondarily to OM. In the modern era, the only viral vaccine with proven effect on AOM is the influenza virus vaccine. Both the inactivated and the live virus showed some effect, but since influenza virus has only a limited season yearly the effect on the overall OM rate is far from being remarkable.
Haemophilus influenzae (Hi) b vaccine did not reduce OM since most Hi causing OM are nontypable (NTHi) and not Hib. The newly developed pneumococcal conjugate vaccines (PCVs) have all been shown to reduce >50% of the OM caused by the serotypes included in the vaccines, but some replacement with serotypes not included in the vaccines and non pneumococcal organisms was demonstrated to reduce the overall effect of pneumococcal vaccines. The effect of PCV on the reduction of recurrent OM, OM with effusion, the need for ventilation tubes and frequent visits for AOM has been suggested, and the real impact is still being studied. Aiming with PCV at those with established recurrent OM has proved disappointing. PCVs can reduce OM caused by antibiotic-resistant S. pneumoniae but the continued overuse of antibiotics is responsible for the increase in antibiotic resistance in non-vaccine serotypes. A newly developed PCV with an outer membrane protein for Hi (PnPD) is suggested to reduce also OM caused by Hi, but confirmation studies are needed. The expansion of the 7 serotypes included in the current licensed PCV to 10 or more serotypes may add to the prevention of OM in the near future.
In the next decade, OM will continue to be an important disease in children. However, we can expect it to be modified in terms of bacteriologic aetiologies, antibiotic resistance and hopefully short and long term consequences.
War, famine and beyond … infections in disaster settings
S14 Earthquakes
V. Korten* (Istanbul, TR)
Infectious consequences of an earthquake mainly involve several types of communicable diseases and crush related infections. Water-borne and food-borne illnesses often result from the disruption of the public water and sewage systems and contamination of water supply. Overcrowding, poor hygiene and sanitation in temporary shelters also may be factors. The type of infectious diseases are associated with the epidemiology of communicable diseases in the area where the earthquake occurred. The most common outbreaks associated with earthquakes are gastroenteritis, infectious hepatitis and pulmonary infections. In unvaccinated populations, there are reports of increased measles. Tetanus can be seen in populations where vaccination coverage levels are low. The risk for diarrhoeal disease outbreaks following earthquakes is higher in developing countries than in industrialised countries. An outbreak of acute watery diarrhoea involved >750 cases occurred in a camp after the 2005 earthquake in Pakistan. Acute respiratory infections, hepatitis E clusters and measles (>400 clinical cases in the 6 months) also occurred among the displaced victims after the same earthquake. Contamination of drinking water led to an outbreak of rotavirus after the 2005 earthquake in Kashmir, India. An unusual outbreak of coccidiomycosis associated with exposure to increased levels of airborne dust occurred after the 1994 Southern California earthquake.
Persons who have been trapped by rubble for several hours or days may develop compartment syndromes requiring fasciotomy or amputation. Infectious complications were common in renal victims of the 1999 Marmara Earthquake in Turkey and were associated with increased mortality when complicated by sepsis. Of 639 renal victims, 223 (34.9%) had infectious complications, mainly sepsis and wound infections. Most of the infections were nosocomial in origin and caused by Gram-negative aerobic bacteria and Staphylococcus spp. Multivariate analysis of the risk-factors for nosocomial infections revealed a significant association with fasciotomy and length of hospital stay in a back up university hospital. The most frequent pathogens isolated from pus and/or wounds culture in 2008 Wenchuan earthquake survivors were S. aureus, E. coli, A. baumannii, E. cloacae, and P. aeruginosa.
Disaster-preparedness plans, focused on trauma and mass casualty management and also on health needs of the surviving affected populations may decrease the health impact of earthquakes.
S16 Infections in the disaster setting: famine. Experience from Darfour, Sudan
V. Krcmery* (Bratislava, SK)
Clinic malnutrition is a known risk factor for ID worldwide. Subsaharan Africa and India is at higher risk due to vegetarian habits on absolute absence of animal meat proteins, resulting to depletion of micronutritients (Zinc, Iron, Selenium), responsible for recovery of postmalarial anaemia. In addition, depletion of proteins results to immunoglobulinaemia and to delayed response to many bacterial pathogens causing ID in topics (pneumococci, Salmonella, etc.). Third problem is absence of vitamins dissolved in oil and fat, resulting to delayed phagocytic activity. Therefore proteinocaloric malnutrition results to significant adverse outcome in HIV, TB (diarrhoea, pneumonia), the major killers of children under five. St. Elizabeth University Tropical programme runs 4 antimalnutrition centres: 1 in Sudan, Darfour and 2 in Kenya Amaong upcountry refugees from major conflict areas (Sudan – Turrana Border) and 1 in Uganda trying to rehabilitate malnourished children under 5 and helping them to combat disease, responsible for 12.5 million deaths in children mean 5 a year – malaria (1.2 mil), TB (1.1 mil), HIV (2.0 mil), pneumonia (7.5 mil) and diarrhoea (0.5 mil. children deaths approximately a year).
Use and abuse of antimicrobials: are we getting what we deserve?
S17 The Greek experience with carbapenem resistance in Enterobacteriaceae
H. Giamarellou* (Athens, GR)
For the last six years Greece has faced a large number of infections, mainly in the intensive care units (ICU), due to carbapenems-resistant Klebsiella pneumoniae. The proportion of imipenem-resistant K. pneumoniae has increased from less than 1% in 2001, to 23% in isolates from hospital wards and to 53% in isolates from ICUs in 2008. Likewise, in 2002, these strains were identified in only three hospitals, whereas now they are isolated in at least 32 of the 40 hospitals participating in the Greek Surveillance System. Until 2007 this situation was due to the spread of the blaVIM-1 cassette among the rapidly evolving multiresistant plasmids and multiresistant or even panresistant strains of mainly K. pneumoniae and also other enterobacterial species. However, the fact that most strains display MIC values below or near the CLSI resistance breakpoint create diagnostic and therapeutic problems, and possibly obstruct the assessment of the real incidence of these strains. As of 2007, the emergence of KPC-producing K. pneumoniae has been noted in ICUs of some Greek hospitals and has now spread to most hospitals throughout the country creating a countywide outbreak in 2008. In Attikon University Hospital we recently described the ICU outbreak of KPC-producing K. pneumoniae. Twenty-nine patients (admitted from February to December 2008) were colonised mainly in GI tract. Fifteen patients were male (52%) and the median APACHE II was 19. Patients had already long hospital stays preceding ICU admission with a median of 25 (17–40) days. In twenty-two of these patients (76%) KPC-producing K. pneumoniae colonisation was definitely ICU-acquired while in 7 (24%) acquisition in other wards or other hospitals was hypothesized. Five of these patients are still hospitalised in the ICU and, of the remaining 24, 11 died (ICU mortality 46%). Ten of the 29 colonised patients were clinically infected. Fifteen infections were documented, mostly BSI (11/15), followed by VAP (2/15) and SSI (2/15). Only 1 patient died from this infection (1/15, 6.7%).
An evidence-based consensus on the therapeutic strategy for these infections has been reached by KEELPNO and the Greek Ministry of Health which proposed the use of high dose meropenem (6–8 g/day) combined with an active aminoglycoside or colistin for strains with an MIC ≤ 4 mg/ml whereas for strains with a higher MIC the use of carbapenems is contraindicated and active alternatives (monotherapy with tigecycline, colistin, or an aminoglycoside or aztreonam-based combinations) could be used.
Antibiotic stewardship is of great importance in such a dismal situation but stringent adherence to infection control measures is probably of even greater importance for the effective containment of these pandrug-resistant strains.
S18 ESBL-producing Escherichia coli in the UK
N. Woodford* (London, UK)
The first E. coli with CTX-M-type ESBLs to cause infections in the UK were detected in 2001, and CTX-Ms were the dominant ESBLs by 2004. Currently >12% of E. coli from bacteraemias are resistant to third-generation cephalosporins. Most (>90%) ESBL-producing E. coli produce CTX-M group 1 enzymes (CTX-M-15 or -3); less common are group 9, 9%, and other groups, 1%. Producers have diverse PFGE patterns, but 5 major strains (A-E), and those clustering with them at >65% similarity, belong to the international O25:H4-ST131 clone. This belongs to phylogroup B2 and is uropathogenic, although the complement of virulence genes varies. Strain A is the most widespread UK ST131 variant (isolates referred from >50 laboratories); D is local to one centre; B, C and E are nationally scattered. Strain A produces CTX-M-15 ESBL encoded on a 118-kb IncFII-FIA plasmid, which encodes resistance to 8 antibacterial classes and is related to internationally-disseminated blaCTX-M plasmids. ST131 E. coli producing CTX-M ESBLs also occur outside the hospital. In a Belfast study, 74/135 nursing home residents carried strain A (CTX-M-15) in their gut flora; 60 others had ST131 variants with IncI1 plasmids encoding CTX-M-3 enzyme. The means of spread in Belfast and nationally is not clear. CTX-M ESBL-producing E. coli are isolated from raw meat, but most produce group 2 or 8 enzymes, which account for <1% of ESBLs from E. coli causing infections. Associations with foreign travel have not yet been fully explored. Are we getting what we deserve? Cephalosporin use drives accumulation of resistance mechanisms, but the rise of CTX-M ESBLs in E. coli could not have be predicted. Their dominance reflects expansion of uropathogenic clones and spread of plasmids. The success of these clone/plasmid combinations implies intrinsic/acquired advantages compared with diverse E. coli strains with CTX-M enzymes. However, not all ST131 E. coli are equal, as illustrated by the national vs. local distribution of UK strains A and D, respectively. As prevalence increases, therapeutic options for ESBL producers are increasingly pushed towards carbapenems. On rare occasions, E. coli strain A has developed carbapenem resistance through OmpC loss combined with non-carbapenemase β-lactamases. The UK sees a few Enterobacteriaceae with carbapenemases (KPC, OXA-48, VIM or IMP enzymes), though rarely in E. coli. Acquisition of a carbapenemase by a pandemic E. coli clone would have immense public health implications.
S19 Antimicrobials and Clostridium difficile infection in the Netherlands and Europe
E. Kuijper*, B. Goorhuis, T. van der Kooi, P. Filius (Leiden, Bilthoven, Rotterdam, NL)
The presentation of Clostridium difficile infection (CDI) varies from mild diarrhoea to a potentially fatal pseudomembranous colitis. The recent emergence of types 027 and 078 of C. difficile has been associated with increased virulence. C. difficile takes advantage of disruption of the normal intestinal flora as caused by antibiotic therapy. The antibiotical class and the antimicrobial resistance pattern of C. difficile influence the development of disease. In The Netherlands, significantly more patients with CDI due to Type 027 used fluoroquinolones (OR, 2.88; 95% CI, 1.01–8.20) compared with those who were infected with other PCR ribotypes. Similar as Type 027 CDI, patients infected with Type 078 also more frequently received fluoroquinolones therapy (OR, 2.17; 95% CI 1.06–4.44). The risk to develop CDI due to Type 027 was particularly high in persons receiving a combination of cephalosporin and fluoroquinolone (OR 57.5, 95% CI 6.8–483.6). This association was also strongly dependent on the duration of therapy. The use of clindamycin was found as a protective factor. However, the recent detection of clindamycin-resistant C. difficile Type 027 strains in other European countries is an important and worrying development. Since the association of CDI with fluoroquinolones has only been investigated at patient level, a study was performed to investigate the relationship between CDI incidence and the preceding use of different antibiotic classes at hospital level in The Netherlands. Comparisons were made between hospitals where type 027 caused an epidemic, hospitals where only isolated cases of type 027 were observed and hospitals where no outbreak of CDI or type 027 were encountered. In the pre-epidemic period, the total use antibiotics was comparable between affected and unaffected hospitals. Higher use of second-generation cephalosporins, macrolides and all other studied antibiotics were independently associated with a small increase in CDI incidence, but the effect was too small to predict which hospitals might be more prone to 027-associated outbreaks.
Despite the fact that The Netherlands is known by its restrictive and conservative use of antibiotics, outbreaks of CDI due to new emerging types have been recognized. This is probably associated with the use of antibiotics at patient level and hospital department level rather than the use of antibiotics at the level of the healthcare institute.
Pharmacokinetics/pharmacodynamics: clinical relevance
O21 PK-PD of posaconazole in a murine model of disseminated aspergillosis
R.J.M. Brüggemann*, E. Mavridou, D.M. Burger, W.J.G. Melchers, P.E. Verweij, J.W. Mouton (Nijmegen, NL)
Objectives: Recently, Aspergillus fumigatus (Af) strains with reduced azole susceptibility have been discovered. A non-neutropenic murine model of invasive aspergillosis was used to determine the pharmacokinetics and pharmacodynamics (PK-PD) of posaconazole (POS) against various Af strains.
Methods: Groups of 11 female CD1 mice were inoculated in the tail vein with Af strains having MICs of 0.031, 0.5, 0.5 and 16 mg/l, reflecting 1 wildtype and 3 mutations in CYP51a, respectively. Antifungal therapy with POS was administered through oral gavages for 14 days as once-daily dosages of 1, 4, 16 and 64 mg/kg or placebo starting 24 hours after inoculation. PK were determined in infected animals by collecting plasma at day 2 of POS treatment through the orbital vein at: 0, 0.5, 1, 2, 4, 8, 12 and 24 h after POS administration, n = 3 per time point. The arithmetic mean plasma concentrations were calculated per time point. A non-compartmental analysis (WinNonLin 5.2) was then used to determine PK parameters of POS. Survival (previously determined) was determined daily until day 14. Results were analyzed by survival curve analysis and plotting PD indices against survival and fitting the Hill equation with variable slope (HEVS) using Prism 5.0.
Results: PK: 96 mice were assessable. The AUC normalised to a dose of 1 mg/kg was 10.19, 11.27, 9.96 and 4.64 mg/L·h for dosages of 1, 4, 16 and 64 mg/kg, respectively. The AUC was strongly correlated with dose in a linear fashion from 1 to 16 mg/kg (r2 = 0.99). Higher dosages of 64 mg/kg however resulted in a slightly less linear relation (r2 = 0.92). The apparent oral clearance (CL/F) was 0.10, 0.09, 0.10 and 0.22 L/h/kg for dosages of 1, 4, 16 and 64 mg/kg respectively. PD: 176 mice were available for PD assessment. Survival curves indicated that exposure responses were obtained for all 4 strains, with increasing exposure needed to obtain the same result if the MIC was higher. Survival best correlated with AUC/MIC ratio; an AUC/MIC – survival plot of all four strains indicated a clear sigmoid exposure-response. The HEVS fitted the data well with a R2 of 0.93. The EI50 was 357 (95% CI 222.1–573.8).
Conclusion: The AUC–dose correlation of POS is linear for dosages up to 16 mg/kg. The higher apparent oral clearance in the 64 mg/kg group is most probably caused by a lower bioavailability possibly related to saturation of uptake. The concentration effect relationships indicate that AUC/MIC of POS best correlates with outcome.
O22 Pharmacological interaction between benzodiazepines and voriconazole in patients with haematological malignancies
W.J. Heinz*, C. Kloeser, A. Kuhn, K. Kahle, D. Keller, H. Einsele, H. Klinker (Wurzburg, DE)
Objective: Voriconazole is recommended as first line antifungal therapy for invasive aspergillosis and is often used in patients suffering from haematological malignancies. Metabolised by cytochrome P450 (mainly isoenzymes 2C9, 2C19 and 3A4), voriconazole is also a potent inducer and inhibitor of this important enzyme system. Otherwise, voriconazole metabolism may be influenced by different comedication. Thus, drug-drug interactions are frequent in patients on voriconazole and may lead to treatment failure in case of enzyme induction or increased side effects in case of enzyme inhibition.
Especially, patients of older age and/or those undergoing chemotherapy receive sedatives also interacting with cytochrome P450. In the present study we investigated the impact of this often unintended combination on voriconazole pharmacokinetic.
Methods: Serum samples from hospitalised patients receiving voriconazole have been collected routinely since 2005. Comedication and patient characteristics were recorded. Trough levels of serum concentrations were determined by a high performance liquid chromatographic method (HPLC). Statistic analyses were performed by t-test.
Results: 259 voriconazole concentrations from 91 patients were determined including 17 samples from 14 patients receiving temazepam (group I), 20 samples from 9 patients with lorazepam (group II) and 222 samples from 68 patients without benzodiazepines (group III). Mean voriconazole concentration was 726 ng/ml in group I (p for I versus III: 0.0167), 1153 ng/ml in group II (p for II versus III: 0.17), and 1701 ng/ml in group III, the median levels were 302 ng/ml, 764 ng/ml and 1159 ng/ml, respectively. Comparing all samples with (n = 35) and without comedication of benzodiazepines, mean voriconazole levels were 1007 ng/ml and 1579 ng/ml with a statistical power of p = 0.0123.
Conclusion: Benzodiazepines have a significant influence on the serum concentration of voriconazole. This pharmacological interaction should be taken into account during antifungal therapy. Therapeutic drug monitoring of voriconazole is helpful to identify patients who are at risk for treatment failure or increased side effects.
O23 Competition between ciprofloxacin and antiviral agents (adefovir, saquinavir, ritonavir) for efflux transporters in J774 macrophages
L. Garcia*, B. Marquez, S. Carryn, M.P. Mingeot-Leclercq, P.M. Tulkens, F. Van Bambeke (Brussels, BE)
Background: Ciprofloxacin (CIP) is substrate for a multidrug efflux transporter that reduces its accumulation and intracellular activity in J774 macrophages (AAC 2004, 48:2673) and was recently identified as MRP4 (ICAAC 2008, A-045). Adefovir (PMEA) is described as a substrate for MRP4 and MRP5 (Mol Pharmacol. 2003, 63:1094), and saquinavir (SQV) and ritonavir (RTV) for MRP1 and MRP2 (JAC, 2002, 50:583; AIDS 2002, 16:2295). This study examines the possibility of cross-competition between CIP and antiviral agents for efflux.
Methods: We used wild-type (WT) and CIP-resistant (overexpressing the CIP transporter [AAC 2006, 50:1689]) macrophages. PMEA was used as its prodrug Bis(POM)PMEA. Cells were incubated for 2 h with CIP, the antiviral agent alone, or together (competition). Cellular concentration was measured by fluorimetry for CIP and HPLC for antiviral agents.
Results: As shown in the Table, CIP and PMEA accumulations were markedly reduced in CIP-resistant cells. High concentrations of BIS(POM)PMEA and SQV increased CIP accumulation in both cell types, while RTV was ineffective. High concentrations of CIP increased PMEA accumulation in both cell types.
Conclusions: CIP and PMEA are both substrates and inhibitors, and SQV inhibitor of the CIP transporter (MRP4 overexpressed in CIP-resistant cells). These data (a) illustrate that MRP4 is truly a multidrug transporter and (b) call for caution about potential drug interactions between CIP and some of the antiviral agents studied due to competition for transport.
| Condition | Cellular accumulation (% drug alone in WT cells) |
|||
|---|---|---|---|---|
| WT cells |
CIP-resistant cells |
|||
| CIP | PMEA | CIP | PMEA | |
| Drug alone (50 μM) | 100±9 | 100±7 | 15±10 | 37±3 |
| + CIP 540 μM | − | 146±4 | − | 187±34 |
| + Bis(POM)PMEA 1000 μM | 170±21 | − | 141±28 | − |
| + SQV 300 μM | 414±32 | ND | 278±13 | ND |
| + RTV 300 μM | 112±13 | ND | 25±9 | ND |
Values in bold characters highlight values that are significantly different from those measured for the drug alone
O24 Pharmacokinetics/-dynamics of piperacillin-tazobactam in plasma and alveolar epithelial lining fluid when administered as continuous infusion in severely ill patients
M. Peiffer, J. Bulitta, H.A. Haeberle, M. Kinzig-Schippers, M. Rodamer, V. Jakob, B. Nohé, F. Sörgel, W.A. Krueger* (Trier, DE; Albany, US; Tubingen, Nuremberg, Constance, DE)
Piperacillin-tazobactam (pip-tazo) is a broad spectrum antibiotic, used for treatment of severe infections such as ventilator-associated pneumonia (VAP). The effectiveness of betalactams is best predicted by the duration of free drug concentrations above the minimal inhibitory concentration (t > MIC) of infecting pathogens [1]. Animal experiments suggest that more than 50% of t > MIC should be reached. Continuous infusion (CI) of pip-tazo may enhance the therapeutic performance, but there is little data on pharmacokinetic/-dynamic (PK/PD) parameters, when CI is used in critically ill patients.
Objectives: The aim of our study was to determine concentrations of pip-tazo in plasma and broncho-alveolar epithelial lining fluid (ELF) at steady state during CI. Based on these results, the penetration ratio (plasma/ELF) and PK/PD parameters for pip-tazo are derived.
Methods: After approval by the Ethics Committee, 16 mechanically ventilated critically ill patients were enrolled during treatment in 3 intensive care units. Each patient received a loading dose of 4 g/0.5 g of pip-tazo, followed by CI of 12 g/1.5 g over 24 h. At steady state (67.8 + 39.5 h after loading dose), a total of 30 blood samples were drawn and bronchoalveolar lavage (BAL) was simultaneously performed in 8 cases (1 sample discarded for technical reasons). Samples were stored at −80°C until analysis by liquid chromatography coupled with mass-spectrometry (LC-MS). ELF-concentrations were calculated from BAL-samples using the relation of ureaplasma:ureaBAL as dilution factor.
Results: Plasma concentrations of pip and tazo (n = 30 in 16 pts.) amounted to 15.38+8.89 mg/ml, and 1.31+0.95 mg/ml, respectively. ELF-levels (n = 7) were 56.63+27.24 µg/ml, and 5.95+3.74 µg/ml. ELF-levels were 368+236%, and 587+584% of corresponding plasma levels (n = 7) for pip and tazo, respectively. The ratio pip:tazo was 11.74:1 in plasma, and 9.52:1 in ELF.
Conclusions: Using advanced analytical techniques, ELF concentrations were higher compared to traditional bolus administration [2]. CI yielded steady state plasma concentrations in excess of MICs of susceptible bacteria (<8 mg/ml, according to EUCAST) in 76.6% of measurements, respectively, but ELF levels exceeded 8 mg/ml in all cases. Taken together, our data provide further arguments for CI being the preferred mode of administration for pip-tazo in critically ill patients with suspected VAP.
O25 Serum bactericidal activity of three different dosing regimens of colistin against Pseudomonas aeruginosa
A. Skiada*, J. Pavleas, C. Vafiadi, K. Salatas, A. Markoyannakis, P. Tofas, K. Tzanetou, G. Thomopoulos, A. Rigas, E. Vafiadi, K. Rigas, G. Petrikkos, G.L. Daikos (Athens, GR)
Objectives: Although colistin has been used extensively in critically ill patients, the optimum dosing regimen has not been defined. The aim of this study was to evaluate the serum bactericidal activity of three different dosing regimens of colistin methanesulphonate (CMS) against P. aeruginosa.
Methods: Adult patients with purulent bronchitis who had not received any antibiotic over the last 72 hours and had normal renal function were administered CMS in three different dosing regimens; 3 million units (MU) q8 h (regimen A), 4.5 MU q12 h (regimen B), and 9 MU q 24 h (regimen C) intravenously. Blood samples were collected on the third day of treatment at 0, 1, 2, 4, 8, 12 and 24 h following drug infusion. CMS and colistin (CS) levels were determined by HPLC. The serum bactericidal activity containing various concentrations of colistin against P. aeruginosa ATCC 27853 (MIC 2 mg/L) was measured at 0, 1, 3, 5 and 24 hours.
Results: Thirteen patients were included in the study, 7 males and 6 females, their mean age was 63.4 years. Four received regimen A, 4 regimen B, and 5 regimen C. Mean serum concentrations of CMS+CS/CS were ranging from 4.65/2.00, 5.05/1.63, 5.28/2.60 to 7.71/3.33, 7.72/2.97, 13.86/5.62 µg/ml for regimens A, B and C respectively. The mean serum concentrations of CS in the samples which achieved killing at 24 hours were 4.12± 1.80 mg/L and for the samples with no killing 2.55±0.76 µg/L (P = 0.001). Serum concentrations of CS >3 mg/L achieved killing in 70.8% (17/24) of the samples whereas concentrations ≥ 3 mg/L achieved killing in 36.8% (7/19) of the samples tested and serum concentrations of CS >4 mg/L were always bactericidal. The MIC90 of CS for 55 blood isolates of P. aeruginosa was 2.0 mg/L.
Conclusions: Serum concentrations of CS >2 × MIC is most of the time bactericidal against P. aeruginosa. Regimen A and regimen B yielded Cmax of CS marginally above the MIC90 for P. aeruginosa whereas regimen C resulted in Cmax of CS >2 × MIC. These findings together with the concentration-dependent activity of CS give a rationale for administering the total dose of the drug once daily.
O26 Determination of pharmacokinetic/pharmacodynamic index for patients treated with high-dose vancomycin by continuous infusion
E. Ampe*, P. Tulkens, B. Delaere, J.D. Hecq, Y. Glupczynski (Brussels, BE)
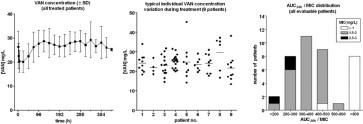
Background and Aims: Over the past 10 years, the susceptibility of Staphylococci to vancomycin (VAN) has decreased. In parallel, it has been suggested that an AUC24 h/MIC ratio of at least 400 h-1 is necessary for optimal therapy (Moise-Broder et al. Clin Pharmacokinet. 2004;43:925–42). Since continuous infusion (CI) is easier both for nursing and for monitoring than conventional Q12 h dosing, we have examined whether it can be applied to patients with infections caused by organisms with increased MICs.
Methods: 54 patients (40 documented infections) were enrolled to receive VAN by CI with a target concentration of 25–30 mg/L, a value above which significant increase in the risk of nephrotoxicity has been reported (Ingram et al., J Antimicrob Chemother. 2008;62:168–71). We used a loading dose of 20 mg/kg and an infusion rate of 2.5 g/day (adapted to renal function and corrected by therapeutic drug monitoring of actual serum levels [immuno-assay Architect, Abbot Diagnostics, Solna, Sweden]). MICs were measured by E-test (AB BIODISK, Solna, Sweden)
Results: Treatment duration ranged from 1 to 37 days (mean: 12±10). The left figure shows that the target concentration range was reached and remained constant as an average after the first 48 h (with correction of the infusion rate). However, intra-individual variability was quite important between successive determinations in individual patients (middle). MIC's of isolates (MRSA, 14; MSSA, 6; coagulase negative Staphylococci, 16; others, 4) ranged between 0.25 and 3 mg/L. A mean AUC24 h/MIC of 400 h-1 (calculated over the whole duration of treatment) was reached in about half of the cases, with lower values seen mainly for patients infected by organisms with an MIC of 1.5 mg/L of greater (right).
Conclusion: High dose vancomycin by CI with adjustment based on therapeutic drug monitoring does not allow reaching a pharmacodynamic/pharmacokinetic index sufficient for optimal therapy in all patients. Patients infected with organisms having MIC's >1.5 mg/L should be considered at risk for treatment failure. The PK/PD data observed in this study further suggest that lowering the current EUCAST susceptibility breakpoint of VAN (S ≤ 4/R > 8 mg/L) is warranted.
O27 Anti-mutant antibiotic concentrations predicted using in vitro dynamic models: the impact of duration of simulated treatment
A. Firsov*, M. Smirnova, S. Zinner, Y. Portnoy (Moscow, RU; Cambridge, US)
Objective: Time-dependent enrichment of resistant sub-populations and/or concomitant loss in susceptibility of antibiotic-exposed bacteria have been reported in studies with fluoroquinolones and lipo- and glycopeptides using in vitro dynamic models. Typically, at a given ratio of the 24-hour area under the concentration-time curve (AUC) to the MIC, greater maximal numbers of resistant mutants are seen with longer treatments. To explore whether the duration of simulated treatment also influences the anti-mutant AUC/MIC ratio, AUC/MIC relationships with resistance were reconstructed from reported data.
Methods: Time courses of resistant mutants reported from studies that expose Staphylococcus aureus to 5-day treatments with daptomycin (Firsov, JAC 2006) and 10-day treatments with garenoxacin (Tam, JID 2007) at sub-optimal AUC/MICs were quantified using a recently introduced integral parameter (area under the bacterial mutant kinetic curve – AUBCM). The AUBCMs determined within 3, 4 and 5 days (daptomycin) and within 4, 6, 8 and 10 days (garenoxacin) were related to simulated AUC/MIC ratios using a Gaussian-type function.
Results: Regardless of the duration of the simulated treatment, the general pattern of AUC/MIC relationships with AUBCM was similar. The Gaussian-type function fits the AUBCM versus AUC/MIC data well (r2 0.64–0.92 for the 3–5-day treatments with daptomycin and 0.97–0.99 for the 4–10-day treatments with garenoxacin). With an increase in the treatment/observation period, the maximal AUBCM increased systematically. For example, the maximal AUBCM derived from the 5-day daptomycin treatment was 2.3 times greater than the AUBCM based on truncated 3-day observations (Figure ). However, despite these differences, the anti-mutant AUC/MIC ratio was practically independent of the duration of treatment (around 200 h with daptomycin and 100–200 h with garenoxacin – both are lower than the clinically attainable AUC/MIC ratios for S. aureus).
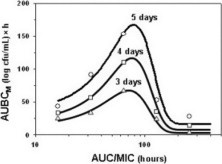
Conclusions: This analysis suggests that the duration of treatment might be critical for in vitro estimates of the maximal enrichment of resistant mutants but not the anti-mutant AUC/MIC ratio, i.e., the ratio that prevents such enrichment and/or suppresses amplification of resistant mutants.
O28 In vivo pharmacodynamics of TR-701, a new oxazolidinone antibiotic, against methicillin-susceptible and methicillin-resistant Staphylococcus aureus strains
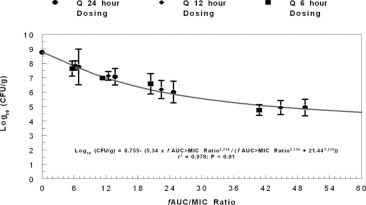
A. Louie, C. Fregeau, W. Liu, H. Conde, R. Kulawy, G. Drusano* (Albany, US)
Objectives: TR-701, the phosphate monoester prodrug of the oxazolidinone TR-700, demonstrates potent in vitro activity against Gram-positive bacteria, including methicillin-susceptible Staphylococcus aureus (MSSA) and methicillin-resistant S. aureus (MRSA). The pharmacodynamics index linked to bacterial cell kill of TR-701 against Staphylococcus aureus is incompletely defined. It was our objective to define this index.
Methods: Single-dose pharmacokinetic studies were conducted in mice for TR-701 and linezolid. Forty-eight hour dose-range and 24-hour dose-fractionation studies were conducted in a neutropenic mouse thigh model of S. aureus infection to identify the dose and schedule of administration of TR-701 that is linked with optimised antimicrobial effect. The dose-range studies also compared the efficacies of TR-701 and linezolid for one MSSA and one MRSA strain. MIC values were determined by CLSI methodology. TR701, TR700 and linezolid concentrations in mouse serum were determined by LC/MS/MS. PK analysis was by BigNPAG. For the Trius compound, the model included both TR701 and TR700.
Results: Population pharmacokinetic analysis showed that terminal half-lives of TR-700 and linezolid were 5.7 and 3.4 hours, respectively. The TR-700 observed–predicted plot was: observed = 1.076·predicted–0.0884; r2 = 0.969. In dose-range studies, TR-701 was bactericidal against both MSSA and MRSA, with 37.3 and 59 mg/kg/day of TR-701 resulting in stasis and 1 log (CFU/g) decreases in bacterial densities at 24 hours and 36.2, 47.8 and 71.1 mg/kg/day of TR-701 resulting in stasis, 1 and 2 log (CFU/g) reductions at 48 hours. Linezolid doses as high as 150 mg/kg/day did not achieve stasis at either time point. Dose-fractionation studies demonstrated that AUC/MIC was the pharmacodynamic index that was linked with efficacy for both TR-701/700 and linezolid. The dose fractionation experiment for TR701/700 is shown in the Figure.
Conclusion: TR-701 was highly active against both MSSA and MRSA in vivo, and was substantially more efficacious than linezolid. Dose-fractionation studies showed that AUC/MIC was the pharmacodynamic index linked with efficacy, suggesting that once-daily dosing in man is feasible.
O29 The novel oxazolidinone radezolid (RX-1741) accumulates in THP-1 macrophages: comparative studies with linezolid and azithromycin
S. Lemaire, P.M. Tulkens, F. Van Bambeke* (Brussels, BE)
Background: Radezolid is a new oxazolidinone, which shows a similar lipophilicity as linezolid (logP: 0.73 vs. 0.47) but bears a protonable aminogroup. Using human THP-1 macrophages, we have compared the pharmacokinetic profile of radezolid with that of linezolid (LNZ) and of azithromycin (AZM), a more lipophilic [logP 2.98], di-protonable macrolide known to accumulate to high levels in the acidic compartments of eucaryotic cells and to be a substrate for P-glycoprotein [Int J Tissue React. 1994, 16:211–20; AAC 2003, 47:1047–51].
Methods: Cellular concentration was determined using 14C RX-1741 or microbiological assay (LZD, AZM), in the following conditions: control; + 100 µM verapamil or 250 µM gemfibrozil (as inhibitors of P-glycoprotein and MRP, respectively [AAC, 2007; 51:2748–57]); + 60 mM deoxyglucose and 5 mM sodium azide (ATP-depletion [AAC 2004, 48:2673–82]), + 50 µM monensin (to collapse pH gradient between extracell. medium and intracell. compartments [AAC 2004, 48:2673–82]), or in media at different pH. Results were expressed as cellular to extracell. concentration ratio (Cc/Ce).
Results: In contrast with LZD (Cc/Ce ≈ 1–2), radezolid was quickly, highly, and reversibly accumulated in THP-1 macrophages (apparent plateau of 8–10-fold; t1/2 for uptake ˜7 min; t1/2 for release ˜20 min), with no sign of saturation over a wide range of extracell. conc. (2 to 50 mg/L), and no influence of ATP-depletion. Accumulation levels of LZD and radezolid were not affected by addition of efflux pump inhibitors (2-fold increase for AZM with verapamil). Radezolid accumulation was reduced (3-fold) at pH 5.5 (10-fold for AZM) or 5-fold with 50 µM monensin (10-fold for AZM).
Conclusions: Radezolid shows a larger cellular accumulation than LZD in THP-1 macrophages, and is not substrate for efflux pumps. The lack of saturation upon concentration increase, of ATP-dependence, and the defeating effect of monensin strongly suggest that radezolid enters the cells by diffusion and accumulates by proton trapping in cell acidic compartments. Radezolid's higher cellular accumulation rationalises its improved potency against intracellular bacteria (see companion abstract: O30) and may help the drug to concentrate in infected tissues, as suggested for macrolides (Int. J. Antimicrob. Agents. 2001, 18 Suppl 1:S11–5).
O30 Radezolid (RX-1741), a novel oxazolidinone, is active against intracellular S. aureus, L. monocytogenes and L. pneumophila phagocytosed by human THP-1 macrophages
S. Lemaire*, P.M. Tulkens, F. Van Bambeke (Brussels, BE)
Background: Intracellular bacteria cause chronic, difficult to treat, and relapsing infections that require antibiotics capable of accumulating and expressing activity in the infected compartment. Using 3 bacteria sojourning in different subcellular compartments (S. aureus (S.a.)., phagolysosomes [pH 5.4]; L. pneumophila (L.p.), acidic vacuoles [pH 5.6]; L. monocytogenes (L.m.)., cytosol [pH 7]) and a model of human THP-1 macrophages, we have examined the intracellular activity of radezolid, a new oxazolidinone for which we have demonstrated a high and acid-pH driven cellular accumulation (see companion abstract: O29) in comparison with linezolid.
Methods: MICs were determined in MHB (S.a. ATCC 25923) or TSB (L.m. EGD) after 24 h, or in BYEa (L.p. ATCC 33153) after 48 h. Intracellular activity against bacteria phagocytosed by human THP-1 macrophages was assessed as previously described (AAC 2002;46:2095–2103; AAC 2006;50:841–851) or with minor adaptations for L.p. Results were expressed as the change from initial inoculum after 24 h (48 h for L.p.) of exposure to the antibiotic.
Results: The Table shows the MICs and the concentration of each drug causing intracellular static effects. Maximal efficacy (Emax) for both radezolid and linezolid were similar for all organisms tested (−0.3 to −0.6 log CFU for S.a. and L.m. −1.2 log CFU for L.p.)
| Organisms | Linezolid |
Radezolid |
||||
|---|---|---|---|---|---|---|
| MIC (mg/L) |
Static conca | MIC (mg/L) |
Static conca | |||
| pH 7.4 | pH infected comp. | pH 7.4 | pH infected comp. | |||
| S. aureus ATCC 25923 | 2 | 2 | 4.3 (2.1) | 0.25 | 4 | 0.9 (0.23) |
| L. pneumophila ATCC 33153 | 4–8 | N.V.b | 5.1 | 0.5–1 | N.V.b | 0.4 |
| L. monocytogenes EGD | 1–2 | 1–2 | 5.5 (5.5) | 0.03–0.06 | 0.03–0.06 | 0.4 (6.9) |
Extracellular concentration (mg/L) yielding a static effect, calculated from non-linear regression [sigmoidal] of dose-effect response studies (values in parentheses = multiples of MIC at the pH of the infected compartment).
No Value (because of insufficient growth of L.p. in broth at pH < 6.9).
Conclusions: Radezolid is significantly more potent than linezolid against pathogenic bacteria that survive inside eukaryotic cells. Overall, the activity of radezolid is consistent with its ability to accumulate within cells and halt the proliferation of bacteria that reside in poorly accessible cellular compartments.
Surveillance of antimicrobial resistance
Gram negatives
O31 The majority of European invasive E. coli isolates is resistant to one or more antibiotics commonly used for treatment
B. Roede*, J. Monen, N. van de Sande-Bruinsma, M. de Kraker, H. Grundmann on behalf of EARSS
Objectives: In Europe, until 2006, the majority of invasive E. coli isolates was still susceptible to fluoroquinolones (FQ), aminoglycosides (AMINO) or third generation cephalosporins (G3CEP). Unfortunately, the EARSS results from 2007, described here, show a different picture.
Methods: Since 2001, EARSS (European Antimicrobial Resistance Surveillance System) has been collecting routine antimicrobial susceptibility testing (AST) data from invasive E. coli isolates. In 2007, over 900 laboratories in 31 European countries contributed data from aminopenicillins (AMIPN), FQ, AMINO, and G3CEP susceptibility of at least 43,072 isolates. Resistance proportions were calculated for each participating country and trends in resistance were calculated using the Cochran Armitage test (two-sided p-value <0.05).
Results: FQ resistance has increased over the past seven years all over Europe. In 2007, all countries reported resistance proportions over 5%. Nine countries reported FQ resistant E. coli in excess of 30%, with three countries reporting resistance proportions above 35%: Malta (35%, n = 117), Cyprus (40%, n = 108) and Turkey (53%, n = 1,062). From 2001 to 2007, FQ resistance increased significantly in all countries except Estonia.
For G3CEP most countries reported more than 5% resistance (18 of 31). From 2001 to 2007, G3CEP resistance increased significantly in most countries (23 of 29). Three countries already reported levels above 20%, Bulgaria (23%, n = 127), Romania (28%, n = 57) and Turkey (40%, n = 1,068).
More than half of all E. coli isolates was resistant to one or more of the four classes tested (53%). Single AMIPN resistance was most common (31%), followed by AMIPN+FQ resistance (9%), AMIPN+FQ+AMINO resistance (3%) and AMIPN+FQ+AMINO+G3CEP resistance (3%). In about half of the countries FQ+AMINO+G3CEP resistance was still below 3% (17 of 31), but in Romania and Turkey combined resistance was already above 20%. Again, the majority of countries (24 out of 29) showed a significant increase from 2001 to 2007.
Conclusion: EARSS recorded an Europe-wide increase of resistance of E. coli to all of the antimicrobial classes under surveillance. For the first time, most of the European E. coli isolates showed resistance to one or more of the antibiotics commonly used for treatment. As a result, the choice of empirical treatment for invasive E. coli infections becomes more and more difficult. Measures to reduce the increasing resistance amongst E. coli bacteria are most urgently needed.
O32 The use of EUCAST wild-type distributions for calibration and a quality control parameter for multi-centre surveillance data
B. Grabein, M. Hoeck, H.M. Just, I. Schwede, B. Wiedemann* (Munich, Berlin, Nuremberg, Frankfurt-Oder, Schaalby, DE)
Objectives: Throughout the world clinical microbiology laboratories test bacteria for their susceptibility to antimicrobial agents. As methods and interpretation criteria can differ markedly these data cannot be used for surveillance purposes. [Kahlmeter and Bruinsma]. We started the EPICENTER network, in which we want to use routine data in order to obtain high numbers of isolates for reliable epidemiological data and to overcome the problems of inadequate methodology and use of different breakpoints. We used EUCAST wild type distributions to validate their usefulness for calibration of methods for susceptibility testing, and to verify the quality of our routine data.
Methods: At this time 4 Laboratories participate in the network using the automated BD PHOENIX-systems measuring MICs. The BD EPICENTER Data-Management-System is used for the evaluation of the data in the laboratory and for the transfer of the data to the concentrator. Here the data are interpreted using, appropriate breakpoints. Copy strains are excluded. Quality control is mandatory.
Results: To date about 100 thousand isolates in the sample period from July 2005 until January 2009 are availlable. Most common species are E. coli, S. aureus, P. aeruginosa S. epidermidis, E. faecalis, K. pneumoniae, Enterobacter cloacae, P. mirabilis, and E. faecium. We analysed the MIC distributions of these species comprising a total of 62,103 strains and compared them with the EUCAST wild type populations. Not for all antibiotic-species combination the range of concentrations was broad enough for a comparison as many strains cumulated at an MIC category ≤, away from the wild type population. As an example we demonstrate here a comparison of the MIC distributions for the above mentioned species with gentamicin (table ). These, like 37 other antibiotic-species combinations, revealed good matching of the data, demonstrating the quality of the data from routine bacteriology.
MIC distributions with gentamicin
| 0.016 | 0.032 | 0.064 | 0.125 | 0.25 | 0.5 | 1 | 2 | 4 | 8 | 16 | 32 | n | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Enterobacter cloacae | |||||||||||||
| EUCASTZ | 15.6 | 57.7 | 23.4 | 2.4 | |||||||||
| EPICENTER | 77.5 | 19.6 | 0.6 | 0.7 | 1.6 | 2918 | |||||||
| Enterococcus faecalis | |||||||||||||
| EUCAST | 1.1 | 2.2 | 5 | 21.1 | 49 | 20.8 | |||||||
| EPICENTER | 0.03 | 0.3 | 3 | 17.4 | 45.8 | 33.4 | 6171 | ||||||
| Enterococcus faecium | |||||||||||||
| EUCAST | 3 | 21.3 | 47.4 | 23.3 | 3.6 | ||||||||
| EPICENTER | 0.4 | 3.7 | 30 | 18.9 | 47.1 | 1679 | |||||||
| Escherichia coli | |||||||||||||
| EUCAST | 1.3 | 18.2 | 48.4 | 26.8 | 5.2 | ||||||||
| EPICENTER | 63 | 29 | 0.8 | 3.1 | 4.1 | 18733 | |||||||
| Klebsiella pneumoniae | |||||||||||||
| EUCAST | 1.4 | 18 | 57.4 | 20.3 | 2.7 | ||||||||
| EPICENTER | 76.7 | 17.5 | 0.5 | 2.5 | 2.9 | 4625 | |||||||
| Proteus mirabilis | |||||||||||||
| EUCAST | 10.7 | 34.3 | 37.9 | 16.7 | |||||||||
| EPICENTER | 12.9 | 68.6 | 12.3 | 3.2 | 3.1 | 3451 | |||||||
| Pseudomonas aeruginosa | |||||||||||||
| EUCAST | 2.23 | 6.4 | 20.3 | 41.8 | 21.6 | 7.4 | |||||||
| EPICENTER | 39.8 | 35.8 | 12.5 | 7.4 | 4.6 | 5752 | |||||||
| Staphylococcus aureus | |||||||||||||
| EUCAST | 5 | 27.6 | 43 | 21.1 | 3.9 | ||||||||
| EPICENTER | 23.7 | 51.6 | 18.8 | 0.7 | 2.1 | 3.1 | 12535 | ||||||
| Staphylococcus epidermidis | |||||||||||||
| EUCAST | 3.3 | 8.5 | 64.5 | 13.3 | 3.8 | 6.6 | |||||||
| EPICENTER | 24.1 | 24.2 | 9.9 | 1.1 | 15.2 | 25.5 | 6239 |
Conclusion: We demonstrated the serviceability of the EUCAST wild type distributions for the calibration of sensitivity test methods. This tool provides security for the routine data entering the EPICENTER Network which will provide reliable epidemiological data for the resistance of pathogens in the clinical laboratory without additional workload.
O33 Resistant Escherichia coli on the rise? Data from the project Surveillance of Antimicrobial Use and Antimicrobial Resistance in Intensive Care Units (SARI); 2001–2007
E. Meyer*, P. Gastmeier, B. Schroeren-Boersch, F. Schwab (Berlin, DE)
Objectives: To analyse E. coli resistance in intensive care units (ICUs) participating in the project Surveillance of Antimicrobial Use and Antimicrobial Resistance in Intensive Care Units (SARI) from 2001–2007 and to look for temporal changes.
Methods: Prospective unit and laboratory based surveillance in 49 German ICUs from 2001–2007. The data were specified as resistant by the clinical laboratory using interpretive criteria recommended by CLSI or DIN. The proportion of non-duplicate resistant isolates (RP) and resistance densities (RD; i.e. the number of resistant isolates of a species per 1000 patient days) were calculated. Linear regression analysis was performed for monthly resistance data.
Results: From 1/2001–12/2007, 49 ICUs reported data on 16,576 E. coli isolates. The median percentage of ampicillin/sulbactam resistant E. coli was 32% (interquartile range (IQR) 20–48), of ciprofloxacin resistant 15% (IQR 11–21), of piperacillin/tazobactam 7% (IQR 4–11) and of 3rd generation cephalosporin resistant (3GC) E. coli 4% (IQR 2–6). RP and RD of the above-named resistant E. coli continuously increased over the last seven years (linear regression coefficients p < 0.001). From 2001 to 2007, in the SARI-ICUs E. coli resistance to 3GC increased from 1 to 11%, to piperacillin/tazobactam from 6 to 15%, to ciprofloxacin from 8 to 21% and to ampicillin/sulbactam from 22 to 40%. E. coli strains remained susceptible for imipenem and amicacin.
Conclusion: The resistance situation of E. coli in individual German ICUs is extremely heterogeneous; however, there was a significant and continuous increase in E. coli resistant to ampicillin/sulbactam, piperacillin/tazobactam, ciprofloxacin and 3GC from 2001–2007. The increase was most dramatic for resistance to 3GC by 950%. Calculated antibiotic therapy has to consider this changed resistance situation and might reconsider aminoglycosides for combination therapy.
O34 Increase of antimicrobial resistance among major Enterobacteriaceae species in Germany
M. Kresken*, H. Seifert, E. Leitner, B. Körber-Irrgang, F.-J. Schmitz (Rheinbach, Cologne, Munster, Minden, DE)
Objectives: Tigecycline encompassing a broad spectrum of bacterial pathogens has been introduced in Germany in May 2006. The German Tigecycline Evaluation Surveillance Trial (G-TEST) is an ongoing surveillance programme comprising 15 laboratories monitoring the susceptibility of bacterial pathogens to tigecycline. The objective of this study was to compare the in vitro activities of tigecycline and comparators against clinical isolates of E. coli and four other major Enterobacteriaceae species obtained in 2005 with those recovered in 2007.
Methods: A total of 1,869 strains (592 E. coli, 455 E. cloacae, 371 K. pneumoniae, 209 K. oxytoca, 242 S. marcescens) collected in 2005 (n = 936) and 2007 (n = 933) was included. Agents tested were tigecycline, doxycycline, ciprofloxacin, cefotaxime, imipenem, piperacillin-tazobactam and other drugs. MICs were determined by the broth microdilution according to the standard of the guideline EN ISO 20776–1 in a central laboratory and interpreted by EUCAST criteria, if available. Changes in resistance over time were assessed.
Results: Comparing data of 2005 and 2007, rates of resistance (%) were as follows: E. coli – tigecycline 0/0, doxycycline 44/40, ciprofloxacin 22/28, cefotaxime 5/12, imipenem 0/0, piperacillin-tazobactam 4/6; E. cloacae – tigecycline 7/6, doxycycline 11/11, ciprofloxacin 6/7, cefotaxime 41/42, imipenem 0/0, piperacillin-tazobactam 19/22; K. pneumoniae – tigecycline 12/7, doxycycline 27/26, ciprofloxacin 8/17, cefotaxime 5/14, imipenem 0/0, piperacillin-tazobactam 8/10; K. oxytoca – tigecycline 2/2, doxycycline 4/17, ciprofloxacin 6/14, cefotaxime 3/16, imipenem 0/0, piperacillin-tazobactam 14/24; S. marcescens – tigecycline 3/2, doxycycline 42/43, ciprofloxacin 6/13, cefotaxime 7/18, imipenem 0/0, piperacillin-tazobactam 3/10. The rate of strains with an ESBL phenotype among E. coli, K. pneumoniae and K. oxytoca isolates rose from 5%, 4%, and 9% in 2005 to 12%, 15% and 17% in 2007, respectively. In contrast, MIC90 values (mg/l) of tigecycline in 2005/2007 remained almost unchanged with 0.25/0.25, 2/1, 4/2, 0.5/1, and 2/2 for E. coli, E. cloacae, K. pneumoniae, K. oxytoca, and S. marcescens, respectively.
Conclusion: The in vitro activity of tigecycline and imipenem against the Enterobacteriaceae species tested did not change compared to pre-marketing baseline values. In contrast, susceptibility to ciprofloxacin, cefotaxime and piperacillin-tazobactam decreased considerably in nearly all species tested.
O35 Escherichia coli resistance to fluoroquinolones at a comprehensive cancer centre
C. Mihu*, P.R. Rhomberg, R.N. Jones, E. Coyle, R.A. Prince, K. Rolston (Houston, North Liberty, US)
Objective: To determine the impact of quinolones as infection prophylaxis for high risk patients with haematological malignancies undergoing intensive chemotherapy to minimise episodes of neutropenic fever and significantly reduced all cause mortality. Routine use of quinolones for infection prophylaxis started in our institution in early 1990's. Because increased use of antibiotics leads to emergence and spread of resistance in Enterobacteriaceae we monitored quinolone resistance in Enterobacteriaceae that generally occurs as a result of chromosomal mutations leading to modification of target, but the qnr gene via plasmids has been recently described.
Methods: Our institution has participated in the MYSTIC/USA Surveillance Programme, along with 14 other institutions. A central, reference laboratory (JMI Laboratories, Iowa, USA) processed all the isolates. The broth microdilution methods and breakpoints were used according to CLSI standards. All the isolates were tested for susceptibility to 10 antimicrobials, including carbapenems, cephalosporins, anti-pseudomonal penicillins, aminoglicosides and fluoroquinolones (screening for qnr).
Results: A total of 271 E. coli isolates from our institution were tested over a 10 year period. Figure 1 illustrates the annual percentage of isolates susceptible to the most commonly prescribed antimicrobials. A decline in susceptibility of E. coli isolates to fluoroquinolones and aminoglycosides was noted over the 10-year span (p < 0.0001). When compared to the average susceptibility of all sites, the isolates from our institution showed significantly reduced susceptibility to these 2 antimicrobial agents.
Figure.
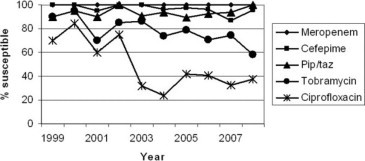
Annual percentage of E. coli isolates susceptible to meropenem, cefepime, piperacillin/tazobactam, tobramycin and ciprofloxacin.
Two of 17 strains investigated were positive for qnr enzymes (qnrA and qnrB2). Four clones encompassing 27 strains were identified among the E. coli isolates submitted.
Conclusions: The introduction of quinolones prophylaxis has led to significant decline in susceptibility of E. coli to all quinolones. Similarly, use of aminoglycosides as part of antimicrobial combination regimens resulted in increasing resistance. Carbapenems, cefepime and piperacillin/tazobactam remain most useful for severe E. coli infections. Structured surveillance allows for detection of resistance patterns (and mechanisms) and adjustment of empiric antibiotic choice in patients at high risk for infection.
Gram positives
O36 Decreasing trends in MRSA in Europe
B.M. Roede*, J. Monen, N. van de Sande-Bruinsma, M. de Kraker, H. Grundmann on behalf of EARSS
Objectives: MRSA is currently the most commonly identified antibiotic-resistant pathogen in hospitals. Resistance proportions have risen to alarming rates; about half of the European countries have MRSA proportions of 25% or higher. Therefore, all available means should be applied to turn the tide and maintain the effectiveness of antimicrobials. We investigated differences in MRSA proportions over time across Europe.
Methods: Since 1999, EARSS (European Antimicrobial Resistance Surveillance System) has been collecting routine antimicrobial susceptibility testing (AST) data from invasive S. aureus isolates. In 2007, over 900 laboratories in 31 countries in the European region collected data from 31,591 isolates. Here, we report trends in resistance from 1999 to 2007, using the Cochran Armitage test (two-sided p-value <0.05) to identify significant changes.
Results: MRSA proportions vary from 0% in the north to over 50% in southern European countries. Thirteen countries reported MRSA proportions equal or higher than 25%; in which all Mediterranean countries, Romania, the United Kingdom and Ireland were included. Four countries had MRSA proportions over 40%. In the northern part of Europe, MRSA rates are below 3%, except for the Baltic States (8–9%). From countries reporting MRSA proportions equal or higher than 25%, France, Turkey, Italy, and the UK showed a significant decrease; whereas Portugal and Malta still show a continuing increase.
In Latvia (25% in 2004) and Slovenia (21% in 2000) MRSA rates continue to decrease strongly to 8% in 2007. For the first time in 2007, proportions in Austria (9%) and Bulgaria (13%) also showed a significant decrease. In Belgium, the decrease of 2006 was maintained, although not (yet) reflected as a statistically significant trend. However, in the Netherlands, Finland, Denmark, Czech Republic, Hungary and Germany a significant increase was reported.
Conclusion: The EARSS data for 2007 show that in Europe, resistance rates of S. aureus reach levels of alarming rates of up to 50% in southern European countries. On the other hand, more and more countries show decreasing MRSA proportions. Therefore, it can be concluded that antimicrobial resistance proportions can decrease, thus giving hope for future containment of antimicrobial resistance.
O37 Antibiotic resistance of Staphylococcus aureus isolates from intensive care units in the Netherlands over a ten-year period
M. Rijnders*, R. Deurenberg, M.L. Boumans, M. Hoogkamp-Korstanje, P. Beisser, E. Stobberingh on behalf of the Dutch Antibiotic Resistance Surveillance group (SWAB)
Objectives: Staphylococcus aureus is a potential pathogenic microorganism and a causative agent of ˜25% of infections in intensive care patients. An optimal empiric choice for the treatment of these infections will result in a reduction in morbidity and mortality. Therefore, it is essential to provide the clinician with resistance data of the bacterial population to be treated. To optimise the empiric choice and to monitor the emergence of microbial resistance, a national surveillance program of the SWAB was started in the Netherlands in 1996. This study describes the results of the resistance development of S. aureus from ICU's of 14 hospitals all over the Netherlands over a ten year period.
Methods: In the first 6 months of each year, the participating hospitals collected clinical isolates from among others blood and respiratory samples. In total 943 isolates were collected: 250 from 3 hospitals in the north, 187 from 2 in the east, 229 from five in the west and 280 from four in the south. The antimicrobial susceptibility was determined as a micro broth dilution method according to the CLSI guidelines.
Results: An increase in resistance to ciprofloxacin was observed from 4% until 2002 to 14% from in 2005, which dropped again to 7% in 2006. The resistance to moxifloxacin was rather constant over time, i.e. ˜2%, only in 2003 8% resistance was found. Resistance to clarithromycin increased to 10% in 2003, but decreased in 2006 to 6% the level before 2003. Resistance to penicillin, clindamycin and tetracycline fluctuated over time at ˜75%, 4–8% and 2–10% respectively. During the study period seven methicillin resistant S. aureus were isolated, no resistance to vancomycin, teicoplanin and linezolid was observed. Resistance to gentamicin and rifampicin was sporadicly found.
Regional differences were observed for ciprofloxacin, being the highest in the western and southern part and tetracycline being the lowest in the northern part.
Conclusion: During the 10 year study period only an increase in resistance to ciprofloxacin was observed. The data presented justify the empiric choice of flucloxacillin, (with rifampicin or gentamicin depending on the indication) in case of an infection in ICU patients probably caused by S. aureus.
O38 Clonal dissemination of vancomycin-intermediate and methicillin-resistant Staphylococcus aureus in Taiwan
J.J. Lu*, P.R. Hsueh, S.Y. Lee (Taichung, Taipei, TW)
Objectives: To investigate the prevalence of VISA in hospitalised patients with MRSA infections or colonisations at a teaching hospital in Taiwan and to evaluate the possible clonal spread of VISA in the hospital.
Methods: From September 2001 to August 2002, 1500 consecutive MRSA isolates were collected from various clinical specimens of 637 patients hospitalised at a teaching hospital in Taiwan. Minimum inhibitory concentrations (MICs) of vancomycin for all MRSA isolates were determined by the broth microdilution method in accordance with CLSI guidelines. Molecular characteristics and antimicrobial susceptibilities of VISA isolates were investigated and Pulsed-field gel electrophoresis was used to evaluate the clonality of the isolates.
Results: Among the 1500 MRSA isolates, 43 (2.9%) were VISA. Of the 43 VISA isolates, 35 had vancomycin MICs of 4 microgram/mL and 8 had vancomycin MICs of 8 microgram/mL. All isolates were inhibited by tigecycline at 0.5 microgram/mL, linezolid at 1 microgram/mL, and ceftobiprole at 2 microgram/mL. Five (11.6%) isolates had reduced susceptibility to daptomycin (MICs of 1–2 microgram/mL). Six of the 43 VISA isolates had decreased susceptibility to autolysis in 0.05% Triton X-100. The 43 VISA isolates were recovered from 21 patients; 13 of these patients had received glycopeptide treatment prior to the isolation of VISA. Five (23.8%) patients died despite vancomycin therapy. All 43 VISA isolates carried SCCmec type III and agr group I but were negative for PVL gene (lukS–lukF). None of the enterococcal van genes were detected in the 43 VISA isolates. Results of PFGE analysis revealed that one major clone of VISA isolates (90.5%, clone A exhibiting SCCmec type III, agr group I, and absence of PVL gene) had disseminated in the hospital.
Conclusion: This retrospective study demonstrated that clonal dissemination of VISA had occurred in the hospital. Rapid and correct detection of VISA and proper use of antibiotics are the most effective approaches for preventing its emergence and spread.
O39 No change in MRSA vancomycin MICs among isolates from paediatric infections (2000–2007)
X. Zheng*, C. Qi, A. O'Leary, M. Arrieta, S. Shulman (Chicago, US)
Objectives: Vancomycin remains one of the major options for treating methicillin-resistant S. aureus (MRSA) related infections. Some but not all studies have shown an increase in prevalence of MRSA isolates with elevated vancomycin MIC values among recent clinical isolates, so called “MIC creep”. Although still within the susceptible range, higher MICs may be associated with increased chance of treatment failure. Because of the conflicting reports and lack of published data from paediatric patients, we sought to assess possible MIC change over time and to compare results generated by using different methodologies including Etest, agar dilution, and broth microdilution (MicroScan) methods.
Methods: We studied 318 MRSA isolates predominantly community acquired including all blood and normally sterile site isolates collected in our large Children's hospital in 2000/2001, 2003, 2005, and 2007/2008. In addition, MRSA from non-sterile sites included all collected in 2000/2001, and the first 70 from each of 2003, 2005, and 2007. Antimicrobial susceptibility testing was conducted with MicroScan Positive Combo Panel 29 plates. Vancomycin MIC was also measured by both Etest and standard agar dilution methods. Inducible clindamycin resistance was assessed by D-test. MRSA typing was performed by pulse field gel electrophoresis (PFGE).
Results: We found no vancomycin MIC increase among paediatric MRSA isolates collected from 2000 to 2007. The highest vancomycin MIC value observed was 2 ug/ml. We found significant inter-assay variations, with proportions of isolates with vancomycin MIC = 2 ug/ml from 85–92% for Etest 43–48% for MicroScan and 2–4% for agar dilution. We found a progressive decrease in prevalence of inducible clindamycin resistance by D-test, from 65% in 2000 to only 5% in 2007. PFGE analysis showed that US300 accounted for 26% isolates in 2000/2001, and increased to 95% in 2007.
Conclusions: MRSA vancomycin MICs did not increase in our paediatric isolates from 2000 to 2007 despite the fact that US300 strains increased dramatically. In addition, inducible clindamycin resistance declined markedly from 2000 to 2007. Considerably different proportions of isolates with vancomycin MIC = 2 ug/ml are found when different laboratory methodologies used, suggesting caution in their interpretation.
O40 Mupirocin resistance in staphylococci from blood in the UK and Ireland, 2006–2007
R. Reynolds*, R. Hope on behalf of the BSAC Working Party on Resistance Surveillance
Objective: The English Department of Health has mandated MRSA screening for all elective hospital admissions, with few exceptions, by March 2009, and for all emergency admissions as soon as practicable within the next three years. The expected resulting increase in use of mupirocin for decolonisation will increase selective pressure for mupirocin resistance. The BSAC Bacteraemia Resistance Surveillance Programme therefore began testing for mupA genes (encoding high-level mupirocin resistance) in staphylococci from blood in 2006, and measuring mupirocin MICs in 2007.
Methods: Each year, 25 laboratories in the UK and Ireland sent up to 10 isolates each of S. aureus and coagulase-negative staphylococci (CoNS) for central MIC testing by BSAC methods. mupA and mecA genes were sought by multiplex PCR in 2006 and 2007. (mecA encodes penicillin binding protein 2a, conferring methicillin resistance.) Mupirocin MICs were measured in 2007 only.
Results: In 2006–2007, mupA was found in 10/487 S. aureus (2%) and 74/384 CoNS (19%). mupA was found much more commonly in mecA-positive than in mecA-negative isolates (5% vs. 0.3% for S. aureus, and 23 vs. 6% for CoNS). Based on 2007 data only, mupA was associated with high-level mupirocin resistance (MIC > 256 mg/L), as expected. Modal mupirocin MICs were 0.25 mg/L for mupA-negative and >1024 mg/L for mupA-positive isolates of both S. aureus and CoNS. Curiously, 5 of 181 CoNS collected in 2007 lacked mupA, as tested with standard primers, but still had high-level mupirocin resistance, all with MICs ≤1024 mg/L.
Conclusion: mupA was more widespread in CoNS (19%) than in S. aureus (2%), and was strongly associated with mecA. Most high-level mupirocin resistance was associated with mupA, but 5 isolates of highly mupirocin-resistant CoNS appeared mupA-negative by standard PCR and will be investigated further. Since mupA is often coded by transferable plasmids, there is a risk of its spreading from CoNS to S. aureus, and of accumulation in the latter species if selection pressure is increased.
| Mupirocin susceptibility (2007 isolates only) |
S. aureus |
CoNS |
||
|---|---|---|---|---|
| mupA-negative | mupA-positive | mupA-negative | mupA-positive | |
| Susceptible (MIC ≤ 4 mg/L) | 241 | 127 | 1 | |
| Low-level resistant (4 < MIC ≤ 256 mg/L) | 1 | 9 | 4 | |
| High-level resistant (MIC >256 mg/L) | 35 | 35 | ||
| Total | 242 | 3 141 | 40 | |
Molecular bacteriology and biology including diagnostics
Molecular bacteriology
O41 Genome sequence of a virulent, methicillin-sensitive Staphylococcus aureus clinical isolate that encodes the Panton-Valentine leukocidin toxin
L. Faraj, L.A.S. Snyder, N.J. Loman, D.P. Turner, M.J. Pallen, D. Ala'Aldeen, R. James* (Nottingham, Birmingham, UK)
Objective: To determine the genome sequence of a virulent meticillin-sensitive Staphylococcus aureus (MSSA) clinical isolate SANOT01.
Methods: Roche 454 sequencing determined the genome sequence of the clinical isolate at 12 times coverage. Newbler sequence assembly (Roche) generated 10 scaffolds that were annotated using GenDB and compared with other S. aureus genome sequences.
Results: An 11-year-old Asian girl presented with fever and a 1-week history of knee pain following a trivial fall. An MR scan revealed a large subperiosteal abscess around the upper tibia secondary to metaphyseal osteomyelitis. A PVL-positive, MSSA was isolated from blood cultures and pus. The child deteriorated, required repeated debridement and developed septic shock. Further investigation revealed aortic valve endocarditis with an aortic root abscess.
Whole genome sequencing revealed that SANOT01 is the first sequence of an ST30 S. aureus isolate to be determined. SANOT01 is agr type III and carries three coding regions that are not found in any other S. aureus genome sequences. Amongst the unique genes present in these regions is a dihydrofolate reductase gene (dfrG) which is present in addition to the usual dfrB gene. Downstream of the orfX gene, a 6.5 kb remnant of SCCmec type IVc was found. This sequence has only previously been found in the MRSA252 genome sequence where it is located between the orfX and SCCmec type II sequences. MRSA252 is unique in sharing 14 genome regions with S. aureus strain RF122, a causative agent of contagious bovine mastitis. All but one of these 14 genome regions are also present in SANOT01.
Conclusions: Comparison of the genome sequence of SANOT01 and the closely related MRSA252 HA-MRSA (EMRSA-16) isolate reveals new insights in the evolution of both CA-MRSA and HA-MRSA isolates and the link to S. aureus RF122. PVL-encoding MSSA strains can be significant pathogens but are not currently under mandatory surveillance in UK. As the cost of whole genome sequencing falls further it will become feasible to use this technology to monitor the evolution of both MSSA and MRSA in healthcare settings and reveal clinically relevant information that will help to improve patient outcomes.
O42 Panton-Valentine leukocidin gene sequence and the PVL-encoding bacteriophage vary with lineage in community-associated methicillin-resistant Staphylococcus aureus
J.A. Otter*, M.J. Ellington, A.M. Kearns, G.L. French (London, UK)
Objectives: CA-MRSA often produce Panton-Valentine leukocidin (PVL), a leukocidin encoded by two co-transcribed genes located on lysogenised phages. Five PVL-encoding phages have been described in S. aureus: phiPVL, phi108PVL, phiSLT, phiSa2mw and phiSa2958. Single nucleotide polymorphisms (SNPs) in the PVL genes tend to vary with lineage and may have structural and functional implications. We examined a selection of PVL-positive CA-MRSA reported in our hospital to determine whether sequence variation and the PVL-encoding phage vary with lineage.
Methods: Twenty-two PVL-positive isolates were chosen to reflect MLST clonal complexes identified in our hospital: CC1, 5, 8, 59, 80, 88 and 154. Isolates were characterised by antimicrobial resistance profile, SCCmec and spa type, pulsed-field gel electrophoresis (PFGE) profile and multilocus sequence typing (MLST); an oligonuleotide array (Clondiag ArrayTube) was used to detect a range of toxin and antimicrobial resistance genes. Primers were designed to amplify and sequence the lukSF-PV genes. The PVL-encoding phage was characterised using a recently described PCR-based assay (Ma et al. J Clin Microbiol 2008;40:3246–58).
Results: SNPs were identified at seven positions in the lukSF-PV genes and the SNP profile varied with lineage. Three of the SNPs were coding mutations, which may have structural and functional implications. CC1 and CC80 isolates were both found to carry phiSa2mw. The PVL-encoding phage was not definitively identified in the other lineages, although the CC59 isolates carried a phiSa2958-like phage and the CC8, CC80 and CC154 isolates carried elongated head-type phages. One of the CC1 isolates had an unexpected SNP pattern compared with other CC1 isolates; this isolate also carried a novel or variant phage.
Conclusion: PVL gene sequence and the PVL-encoding phage vary with lineage in PVL-positive CA-MRSA isolates. This suggests that certain lineages are susceptible to infection or lysogeny with certain phage types. Although CA-MRSA commonly carry PVL genes, some strains do not; it is possible that some PVL-negative types are resistant to infection with PVL-encoding phage, perhaps via restriction modification systems. Crucially, our findings suggest the PVL genes have co-evolved with their phage and are not freely transmitted between different phages. Further work is required to characterise the PVL-encoding phage in other isolates and to investigate whether the PVL sequence variants result in biological differences.
O43 Characterisation of PVL phages carried by MRSA in England and Wales
E. Boakes*, A.M. Kearns, M.J. Ellington (London, UK)
Objectives: Community-associated MRSA (CA-MRSA) of many different MLST clonal complexes (CCs) can harbour lysogenised bacteriophage DNA (prophage) encoding Panton-Valentine Leukocidin (PVL). Five PVL phages (phiPVL, phiSLT, phiSa2mw, phi108PVL, and phiSa2958) have been reported to date. We sought to determine the distribution of chromosomally integrated copies of these lysogenised PVL-phages amongst dominant clones of PVL MRSA in England and Wales.
Methods: Seventy isolates of previously characterised PVL-MRSA were analysed by PCRs developed by Ma et. al, (JCM, 2008), to identify and discriminate between the five known PVL phages. To maximise any underlying diversity, representatives of each CC were selected based upon their spa, staphylococcal cassette chromosome mec (SCCmec), toxin gene and Pulsed-field Gel Electrophoresis (PFGE) profiles. These included isolates of internationally disseminated PVL-MRSA lineages CCs 8, 30 and 80 which resemble the USA300, South West Pacific (SWP) and European clones, respectively. In addition we analysed PVL-MRSA from CCs 1, 5, 22, 59, 88 and ST93.
Results: All seven CC80 isolates, which included representatives of the European clone, possessed an elongated-head-type phage and were positive by the PCR specific for the phiSa2MW phage. One of the CC30 isolates possessed a phi108PVL phage, four SWP representatives had elongated head type phages, whilst the remaining four CC30 isolates harboured an icosahedral-head-type phage. One CC30 was positive for both head shapes. The 12 CC8 (including representatives of USA300), eight CC1, six CC88 isolates and the ST93 isolate were all positive for elongated-head-type phage. Nine CC5 isolates were non-typeable for phage head shape and specific phage PCRs. Three of four CC59 isolates, harboured a phiSa2958-like phage of an unknown head type and the other CC59 isolate was non-typeable. All 14 CC22 isolates possessed an icosahedral-head-type phage, 13 were positive for the phiPVL phage type and one possessed phi108PVL type.
Conclusion: We have determined the PVL phages present in a diverse panel of distinct PVL-MRSA clones and found considerable inter-lineage variation in the PVL prophage present. There was also evidence of intra lineage variation in some major CCs such as CCs 22, 30 and 59. Together with variation in MLST CC and SCCmec, these data suggest PVL-MRSA have evolved on multiple occasions, sometimes within the same lineage.
O44 Transcriptional profiling of Klebsiella pneumoniae genes controlled by the transcription factor, ramA
T. Schneiders*, A. Ivens (Edinburgh, UK)
Objectives: RamA is an AraC/XylS family transcriptional activator where over expression is associated with a multidrug resistance phenotype. In both multidrug resistant Klebsiella and Salmonella isolates, the ramA gene has been associated with increase in expression of the acrAB efflux pump. In Salmonella it has been shown that a deletion of the ramA locus prevents the emergence of multidrug resistant mutants. Therefore in order to understand the role of this key regulator in the emergence and development of antibiotic resistance, transcriptomic analyses of its regulon were undertaken in K. pneumoniae.
Methods: RNA was extracted from a combination of isogenic mutants and clinical isolates using the Qiagen or RiboPure Kits. RNA integrity was assessed using nanodrop and Agilent Nanochip systems. The RNA was transcribed into double stranded cDNA prior to labelling with Cy3. The cDNA was hybridised to the Nimblegen expression array platform designed from the K. pneumoniae MGH 78578 genome.
Results: Approximately 50 genes were found to be affected by ramA expression, of which twenty (involved in metabolism, physiology, transcription, drug efflux, protection responses and the cell envelope) were confirmed by RT-PCR. The RamA protein appears to affect drug efflux operons not previously shown to be associated with multidrug resistance and or affected by similar proteins such as MarA. Comparative transcriptome analyses of different K. pneumoniae clinical isolates overexpressing ramA showed that variations exist in the levels of expression of the drug efflux genes. Of note genes shown to be directly regulated by RamA have a marbox-like sequence within the promoter sequences.
Conclusion: In this study, the transcriptome of the regulatory protein, RamA, was determined in the pathogen K. pneumoniae. Drug efflux proteins not previously associated with ramA overexpression were found to be directly affected. The RamA regulon overlaps with the MarA and SoxS regulons in E. coli and Salmonella but is directly associated with regulating the expression of a subset of genes via a marbox sequence. Interestingly, variations in the levels of the expression of the regulon genes were found in the different ramA overexpressing strains.
O45 Rapid detection and identification of tick-borne pathogens directly from clinical samples using PCR and electrospray ionisation mass spectrometry
M. Eshoo*, C. Crowder, H. Li, H. Matthews, S. Meng, S. Sefers, R. Sampath, C. Stratton, D. Ecker, Y.W. Tang (Carlsbad, Nashville, US)
Objectives: The potential for fatal outcome from tick-borne human infections such as ehrlichiosis emphasizes the need for rapid diagnosis. We developed and validated an Ibis T5000 assay (Ibis Biosciences, Inc., Carlsbad, CA) that can detect and identify a wide range of tick-borne pathogens from clinical samples.
Methods: A multi-locus assay was used that employs 16 broad-range PCR primer pairs targeting all known bacterial tick-borne pathogen families. Electrospray ionisation mass spectrometry of the PCR amplicons was used to determine their base composition. These base composition signatures were subsequently used to identify the organisms found in the samples. The assay was developed using field collected ticks and a wide range of clinical sample types and has been shown to be sensitive to the stochastic limits of PCR.
Results: Whole blood (198), cerebrospinal fluid (20) and plasma (1) samples, which were originally submitted for Ehrlichia species detection by a colorimetric microtiter plate PCR (PCR-EIA), were collected consecutively from January 5 to August 1, 2008 at Vanderbilt University Hospital. Among the total 219 specimens, PCR-EIA detected 40 Ehrlichia species with a positive rate of 18.3%. The Ibis system detected Ehrlichia in 38 of the 40 PCR-EIA-positive samples and 1 in 179 of the PCR-EIA-negative specimens, giving sensitivity and specificity of 95.0% and 99.4%, respectively. The Ibis system further characterised the 38 Ehrlichia-dual positive specimens to the species level (E. cheffeensis, 35; E. ewingii, 3) with a 100% agreement to that identified by PCR-EIA using additional species-specific probes. In addition we demonstrated the detection of Borrelia burgdorferi from the blood and skin of a patient with Lyme disease.
Conclusions: We demonstrate broad-range detection of tick-borne pathogens in a single assay using skin, whole blood, plasma, skin and CSF. In addition to Ehrlichia, the Ibis system detected 4 Rickettsia rickettsii positive specimens, which were confirmed by serology and clinical findings. The Ibis T5000 system, which can be completed within five hours from specimen processing to result reporting, provides rapid and accurate detection and identification of a broad range of pathogens causing tick-borne human infections.
Molecular biology
O46 Rapid detection and characterisation of pathogens causing healthcare-associated infections using PCR/ESI-MS
R. Sampath*, L. Blyn, R. Ranken, C. Massire, T. Hall, M. Eshoo, R. Lovari, H. Matthews, D. Toleno, R. Housley, S. Hofstadler, D. Ecker (Carlsbad, US)
Objective: To investigate the use of a novel platform-based approach for rapid characterisation of HAI organisms. Pathogens that cause healthcare-associated infections (HAIs) pose an ongoing and increasing challenge to hospitals, both in the clinical treatment and in the prevention of the cross-transmission of these problematic pathogens. Here we describe the utility of a PCR Electrospray Ionization Mass Spectrometry (PCR/ESI-MS) detection platform as an innovative, rapid approach for detection and complete characterisation of important HAI pathogens.
Methods: We have developed PCR/ESI-MS based methods to rapidly identify and characterise MRSA, VRE, C. difficile (NAP-1 strain), P. aeruginosa and A. baumannii. Each target organism can be analyzed using an independent 8-well assay that can be run on the same platform and can provide species and strain ID, virulence factors, antibiotic resistance and genotyping as appropriate. Validation studies were performed using 100–300 retrospective, well-characterised clinical isolates for each organism. This was followed by a prospective study for one of the 5 organisms, MRSA, that included screening of 557 clinical specimens (nares swab) from patients who were admitted to a medical unit with a high prevalence of MRSA clinical infections.
Results: For each of the five HAI organisms, PCR/ESI-MS species identifications were compared to Gold Standard testing results from the clinical microbiology laboratory and showed 100% concordance. For S. aureus, P. aeruginosa and A. baumannii, molecular genotyping by PCR/ESI-MS was compared to pulse field gel electrophoresis (PFGE) clusters and showed >95% concordance. Characterisation of virulence and/or drug resistance was performed for MRSA, VRE and C. difficile and showed 90–95% correct detection compared to existing testing methods. Analysis of clinical specimens for MRSA showed that of the 557 swabs, 95 (15%) contained MRSA, either singly or as a dual infection with CoNS, 33 (5%) were MSSA and 358 (58%) contained mecA+ coagulase negative Staphylococcus (MR-CoNS). Comparison to gold standard analysis showed 100% sensitivity for MRSA detection with 96.8% specificity, 84% PPV and 100%NPV.
Conclusion: The PCR/ESI-MS technology is a high throughput assay system useful for infection control and for epidemiological studies. It is capable of simultaneous identification of HAI organisms while detecting presence of key phenotypic markers and genotypic strain characterisation.
O48 Multiplex real-time assay for the detection of 7 viruses causing infections of the central nervous system
M. Reijans*, J. Ossel, J. Keijdener, G. Simons (Maastricht, NL)
Objective: Molecular diagnostics play an increasingly important role in the detection of infectious agents in cerebrospinal fluids. However, the growing list of targets and the relatively small sample volumes are challenges that demand an improved molecular diagnostic approach. The MeningoFinder is a MultiFinder assay allowing the simultaneous detection of 7 viruses and 1 internal control in 1 reaction. Until now, the analysis of MultiFinder assays was based on size-fractionation, identifying each MultiFinder probe due to its specific length. Here we present an alternative approach allowing realtime detection of eight MeningoFinder probes in a single tube. The realtime detection enables a faster analysis, less handling and lowers the risk of contamination.
Method: The MeningoFinder assay is a MultiFinder assay which detects herpes simplex virus 1 and 2 (HSV1–2), human parechovirus (HPeV), cytomegalovirus (CMV), Epstein–Barr Virus (EBV), enterovirus (EV) and varicella-zoster Virus (VZV) plus an internal control in a single reaction. Each MeningoFinder probe can be distinguished based upon the specific length of each probe by size-fractionation using gel or capillary electrophoresis. We developed an alternative detection method using fluorescently labelled probes which allow specific identification of 8 MultiFinder probes in a realtime PCR machine.
Results: A large number of QCMD samples (N = 44), several enterovirus types (N = 27) and characterised clinical samples (N = 66) were analyzed using the MeningoFinder. All MeningoFinder reactions were analyzed by capillary electrophoresis and by fluorescently labelled probes in a realtime PCR machine. The results of the MeningoFinder showed a very good correlation with the expected results (>95%). Furthermore, the results of both MeningoFinder analyses showed a high degree of correlation. The realtime detection of the MeningoFinder probes decreases the analysis time and post PCR handling dramatically.
Conclusions: We developed a new assay for the realtime detection of 8 MeningoFinder probes. The realtime analysis showed a very good correlation with the conventional capillary electrophoresis analysis. In addition, the realtime detection reduced contamination risk and patient results became available more quickly. The combination of MultiFinder technology combined with realtime detection shows great potential in fast and easy multiparameter screening of clinical samples for infectious pathogens.
O49 Performance of monoplex and multiplex nucleic acid amplification tests for the detection of a range of respiratory pathogens
K. Loens*, E.C.J. Claas, F. Coenjaerts, H. Goossens, W.G. MacKay, P. Wallace, C. Scott, A.M. Van Loon, M. Ieven on behalf of the GRACE Study Team
Objectives: In the framework of the GRACE NoE, a panel containing most of the respiratory viruses and atypical bacteria was developed to evaluate the performance of different mono- and multiplex (MX) realtime nucleic acid amplification tests (NAATs).
Methods: The EQA panel consisted of 42 samples spiked with various concentrations of reference strains of M. pneumoniae, C. pneumoniae, L. pneumophila, adenovirus (ADV), influenza A and B (InfA/B), hCoV, parainfluenzavirus types 1 and 3 (PIV1/3), respiratory syncytial virus A and B (RSV A/B), human metapneumovirus (hMPV), and rhinovirus (hRV) as the sole agent. Furthermore, a total of 6 negative samples were also included. The panel was analyzed in 3 different centres for the presence of M. pneumoniae, C. pneumoniae, L. pneumophila and ADV DNA and InfA/B, CoV, PIV1/3, RSV A/B, hMPV, and hRV RNA by inhouse mono and MX NAATs. In-house NAATs were applied to nucleic acid extracts obtained by own in-house methodology in each centre.
Results: Sensitivities for the detection of the respiratory viruses were 40% for commercial MX NAAT, 86% for in-house MW NAAT, and 90% for mono in-house NAAT. The viral load was low each time false-negative results were obtained. False positive results were obtained by all methods used, resulting in specificities ranging from 88%-97%. For the atypical bacteria, the 2 multiplex NAATs failed to detect low L. pneumophila positive samples and low M. pneumoniae positive sample resulting in sensitivities of 25% and 75% compared to 100% in the inhouse mono NAATs. The commercial MX NAAT also failed to detect strong positive samples. No false positive results were obtained for the atypical bacteria.
Conclusion: Substantial differences between the performances of the assays were found. The two in-house viral NAAT methods evaluated showed no significant differences in sensitivity and specificity. None of the viral NAATs used were free of false positive and false negative results. The commercial assay evaluated was significantly less sensitive; based on the results on this panel the assay is being adapted. Both mono NAATs evaluated for the detection of atypical bacteria were equally sensitive, the multiplex NAATs failed to detect the low positive samples.
O50 A novel DNA micro-array system for rapid detection of TEM, SHV and CTX-M extended-spectrum β-lactamases in Enterobacteriaceae
J. Cohen Stuart, D. Mevius, N. Al Naiemi, A. Karczmarek, A. van Hoek, P. Vos, A. Fluit, C. Dierikx, J. Scharringa, B. Duim, M.A. Leverstein-van Hall* (Utrecht, Lelystad, Amsterdam, Wageningen, NL)
Objective: The phenotypic detection of ESBLs is time consuming, laborious, and frequently inconclusive. Since rapid and adequate ESBL detection is crucial for infection control measures and the outcome of antimicrobial therapy, a faster and more accurate detection method is desirable.
The aim of this study was to develop and evaluate a novel ESBL assay based on the ArrayTube system of Clondiag Chip Technologies using ligation-mediated amplification combined with microarray analysis to detect the most prevalent ESBLs in Enterobacteriaceae: TEM, SHV and CTX-M.
Methods: The mutations conferring an ESBL phenotype were identified from the Lahey database for the TEM and SHV genes. A selection of mutations was made covering >95% of the ESBLs described in the Western World. Oligonucleotide probes were designed to detect amino acid changes conferring TEM and SHV ESBL phenotypes, and sequences to distinguish CTX-M families 1, 2, 9 and 8/25. Each microarray contained 90 DNA tags allowing parallel analysis of 3 isolates. The reaction products were detected by hybridisation to generic DNA tags. Software was developed to interpret the array data. For evaluation 218 phenotypically and genotypically characterised Enterobacteriaceae isolates were selected, covering all mutations tested in the array except one. Initial evaluation was performed with 82 isolates (43 ESBL positive). After this evaluation the PCR amplification step was modified by introduction of dUTP and incubation of the PCR reaction with uracil-DNA-glycosylase prior to thermal cycling to prevent cross-contamination from previous amplifications. Currently the final evaluation with 218 isolates takes place using this modified protocol.
Results: In the initial evaluation performance time was 8 h per 36 isolates (3 h DNA isolation; 5 h ligation, amplification and detection). For 42 of 43 ESBL positive isolates (13/14 TEM, all 8 SHV and 21CTX-M) the test results were correct (sensitivity 98%; 95% confidence interval (CI) 87–100%). For 3 of 39 ESBL-negative isolates the result were false positive (specificity 92%; 95%CI 90–97%) and for 2 of these 39 inconclusive.
Conclusion: This proof-of-principle study shows that this DNA microarray system may offer an attractive option for rapid and accurate detection of CTX-M, TEM and SHV ESBL genes in Enterobacteriaceae in the clinical laboratory. The results of the final evaluation will be presented.
Revisiting phage therapy against problematic pathogens
S61 How the past feeds the future: from d'Herelle to modern phagotherapy
T. Häusler* (Basel, CH)
The increasing antibiotic resistance problem boosts the interest in alternative treatments for infections. A prominent example for this is the so-called phagotherapy. It makes use of bacterial viruses – bacteriophages – as drugs against bacterial agents.
These bacteriophages are isolated from nature, characterised and then tested against the bacterial strains that are targeted. In theory, this approach has several advantages. For instance, bacteriophages infect, as a rule, their bacterial prey very specifically. Therefore, they do not harm the commensal bacteria of the patient. Additionally, if a bacterial strain becomes resistant against a certain bacteriophage strain, evolution will provide for new and active bacteriophage strains.
In practice, phagotherapy has been used for a long time. Already one of the two discoverers of bacteriophages, Félix d'Herelle, was an ardent advocate of this method. In fact, he was the first to use bacteriophages against infections – 1919 against bacterial diarrhoea (Shigella spp.). After that, phagotherapy has been used to quite some extent in Europe, the US and other parts of the world until penicillin entered the market in the 1940 s. In some parts of the former Soviet Union and the Eastern Bloc, the method has been utilised until today. Now, several companies and university researchers are developing bacteriophages for therapeutical purposes again.
Historical documents related to phagotherapy and oral history reveal a fascinating past. Bacteriophages have been employed against a wide variety of bacterial diseases in a time in which there were virtually no other anti-infectives. For example, in India, millions of cholera patients were treated with bacteriophages in the 1930 s. Anti-cholera phages were also poured into drinking wells as prophylactics. Bacterial viruses have also been utilised by the German and Soviet armies in the Second World War.
The history of phagotherapy makes for more than an exciting story, however. Analysis of the old literature helps identify important factors for success and failure. This is especially relevant for a field which holds promise but which has had limited funds at its disposal in the past few years – and which, therefore, has been making rather slow progress. Additionally, examination of the strategy used for phagotherapy in the Soviet Union and Poland also contributes to a better application of this method today.
S64 Experience and perspectives of phage therapy in Eastern Europe
M. Kutateladze* (Tbilisi, GE)
The discovery of bacteriophages, particularly their ability to replicate and lyse pathogenic bacteria may have been among the most important milestones in the history of biomedical sciences. In the pre-antibiotic era of the early 20th century, phage therapy was becoming a powerful weapon against infectious diseases of bacterial aetiology. Unfortunately, phage treatment and research was largely forgotten in the Western world as antibiotics became widely available. Nowadays, the rapid propagation of multi-drug resistant bacterial strains is leading to renewed interest in phage therapy.
In contrast to its decline in the West, phage therapy remained a standard part of the healthcare systems in Eastern Europe and the USSR during the second half of the 20th century. Phage preparations were used for diagnostic, therapeutic and prophylactic purposes to combat various bacterial infections.
The Eliava Institute of Bacteriophages, Microbiology and Virology (Tbilisi, Georgia) is perhaps the most famous institution in the world focused on the study of bacteriophages, particularly the isolation and selection of phages active against various bacterial pathogens. Phages have been isolated against bacterial strains received from all over the former USSR and socialist East European countries; consequently, a huge collection of phages and pathogenic bacterial strains has been constructed at the Institute. Thousands of people were treated with individual phages and phage mixtures during the Soviet era. The preparations developed in Tbilisi have been studied through extensive preclinical and clinical trials. However, little of this information has ever been published and even when details are available, the trial reports do not meet internationally approved regulations and standards.
Bacteriophages have a number of advantages in comparison to antibiotics. Phage therapy as an alternative approach for treatment of infections has become an evident and promising remedy. Today, many people from various parts of the world express their willingness to take phage treatment against different infections, including those that are caused by antibiotic-resistant bacterial pathogens. The Eliava Institute has elaborated new, phage-based products and technological schemes for their production. Strong collaboration with the medical community in the design of clinical trials according to international standards is absolutely critical to supporting the broader implementation of phage therapy.
New aspects of viral disease and transplantation
S65 The new LCM-like arenavirus and transplantation
P. Charles* (Melbourne, AU)
An Australian male aged 57 years died from an intracerebral haemorrhage ten days after he returned from a trip to rural Yugoslavia. His kidneys and liver were donated to three female recipients aged 44 years (kidney), 63 years (kidney), and 64 years (liver). Four to five weeks after the organ donation, all three recipients died. All had febrile illnesses with altered mental status. Subsequent testing of post-mortem tissues from the recipients identified a novel arenavirus, which was related to lymphocyctic choriomeningitis virus (LCMV). This viral detection process involved the use of high-throughput sequencing techniques to identify novel microbial RNA sequences. Confirmatory testing was performed using the techniques of reverse transcriptase-polymerase chain reaction, immunohistochemical analysis for arenavirus antigens, and immunofluorescent testing for IgG and IgM antibodies. The clinical features in these four patients as well as other similar problems with transplant-related illness from classic LCMV will be discussed, as well as details of the laboratory identification of this new virus, and implications for organ transplantation protocols in future.
News from the clinical mycology laboratory
S69 Yeast susceptibility testing: CLSI and EUCAST
J.L. Rodriguez-Tudela* (Madrid, ES)
Yeast antifungal susceptibility testing has become a routine diagnostic test in many laboratories. EUCAST and CLSI have published the reference standards for Europe and USA respectively. Once this task has been achieved, the main commitment is the development of breakpoints. CLSI has published breakpoints (BPs) for fluconazole, itraconazole, voriconazole and the candins and EUCAST for fluconazole and voriconazole. Posaconazole is in the agenda of EUCAST for 2009 whereas the breakpoints for candins will have to wait until the development of a new standard that identifies properly the resistant strains. Recent studies have proved that resistant strains to candins are not properly detected by EUCAST or CLSI standards. BPs are crucial to advice on therapy in the patient as well as for measuring resistance development in hospitals and the community and for measuring the effect of interventions and for developing strategies to counteract further resistance development. Unfortunately, EUCAST and CLSI BPs are different as it can be seen in the table.
The reasons for these discrepancies are not straightforward. The process for establishing BPs designed by EUCAST takes into account pharmacokinetic (PK)-pharmacodynamic (PD) data and other factors, such as dosing regimens, toxicology, resistance mechanisms, wild type MIC distributions, and clinical outcome data. EUCAST develops species specific breakpoints with the basic principle that they cannot divide wild type MIC distributions for target species. This ensures that all microorganisms lacking of resistance mechanisms are uniformly categorised as susceptible, intermediate or resistant. This also warrants a good reproducibility of MIC results. CLSI follows a similar process but they do not produce species specific BPs. Clinical outcome data has been always analyzed following the 90–60 rule. This rule states that infections due to susceptible isolates respond to therapy approximately 90% of the time, whereas infections due to resistant isolates respond approximately 60% of the time. Recently, EUCAST has used data mining tools to analyze and interpret clinical outcome data. Data mining models develops a complex statistical analysis including performance measures like sensitivity, specificity, false positive rate and area under the ROC curve which enable to assess whether the results have statistical relevance or they are chosen at random. This presentation will deal with data mining analysis of clinical outcome data produced by EUCAST and CLSI in order to ascertain the statistical support of the data as well as whether this kind of analysis explain or not the differences in the BPs developed by both organisations.
| EUCAST BPs (mg/L) |
CLSI BPs (mg/L) |
|||||
|---|---|---|---|---|---|---|
| Susceptible | Intermediate | Resistant | Susceptible | S-DDa | Resistant | |
| Fluconazole | ≤2 | 4 | >4 | ≤8 | 16–32 | ≥64 |
| Itraconazole | NA | NA | NA | ≤0.125 | 0.25–0.5 | ≥1 |
| Voriconazole | ≤0.12 | − | ≥0.12 | ≤1 | 2 | ≥4 |
| Caspofungin | NA | NA | NA | ≤2 | − | >2 |
| Micafungin | NA | NA | NA | ≤2 | − | >2 |
| Anidulafungin | NA | NA | NA | ≤2 | − | >2 |
S-DD: susceptible dependent upon dose.
S70 Recent advances for the routine mycology laboratory
M. Arendrup* (Copenhagen, DK)
Successful management of invasive fungal infections depends on timely and correct treatment. Over the last decades a number of new tests have become available which have improved the diagnostic options.
In contrast to the scenario for bacterial infections, acquired resistance in fungi is rare and thus species identification is a valuable tool guiding choice of treatment. Therefore, microscopy & culture is still a corner stone in diagnosis, but culture and identification are time consuming (app. 1–5 and 1–3 days, respectively).
The sensitivity and speed of microscopy have been improved by the use of fluorescent brighteners such as calcofluor white or blankophor. But only with the recent development of PNA probes specific for a number of the Candida spp. has species identification become possible directly from a positive blood culture before subculture on agar media.
Chromogenic agars allow a presumptive identification of several Candida spp. and facilitate the recognition of yeast isolates in samples containing several yeasts or yeast and bacteria in combination. The use of such plates has been shown to lead to a better identification of mixed cultures in a recent Nordic EQA scheme including more than 50 laboratories. Rapid species identification of the most important Candida spp. is possible in the routine laboratory using easy commercially available kits. Thus, a species identification of C. albicans, C. dubliniensis and C. krusei can be obtained within minutes using latex agglutination kits (BICHRO-DUBLI, KRUSEI-COLOR; Fumouze Diagnostics) and C. glabrata can be rapidly identified due to its high amounts of preformed intracellular trehalase enzyme (Glabrata RTT; Fumouze Diagnostics). Finally, PNA probes and fluorescence microscopy can also be used for a same day identification of a range of the clinically relevant Candida spp. (AdvanDx).
Susceptibility testing is possible using Etest and the results are comparable with those obtained by reference methodologies in head to head comparisons. However, recent data from EQA distributions suggest that detection of isolates with acquired resistance causes many laboratories difficulties. This illustrates that a critical number of isolates should be tested per technician per week and quality control strains should be included on a regular basis.
In conclusion, a number of new diagnostic tests have become available over the last decade and the diagnostic laboratories are encouraged to take advantage of these new options.
S72 Molecular mycology tissue diagnosis
V. Rickerts* (Seattle, US)
Since the introduction of newer antifungals with different in vitro spectra, the aetiology of invasive fungal infections (IFI) has become a major diagnostic issue as a prerequisite for a guided antifungal therapy.
While molecular methods, such as PCR and Sequencing for the diagnosis of IFI have been evaluated from specimens such as blood and bronchoalveolar lavage fluid for some years, they have been less studied for biopsies. Characteristics inherent to these molecular methods, e.g. sensitivity, specificity and short turnaround time makes them promising as adjuncts to conventional diagnostic tests, e.g. culture and histopathology from organ biopsies.
Studies using tissue from animal models of mould infections suggest that PCR might be more sensitive than culture and allows for a better species identification than histopathology. However, most of these studies used assays detecting only a small range of agents or even single organisms. While this may increase the sensitivity of the assays and reduces the likelihood of contaminations it limits the usefulness in the clinical setting, given the broad range of potential fungal pathogens.
Studies using fresh clinical samples suggest that the detection and identification of a wide range of fungi is possible using broad range assays in combination with sequencing or by combining more specific PCR assays. Further studies are needed to optimise DNA extraction, define the best molecular targets and the best method for amplicon detection. The prevention of contaminations due to ubiquitous fungi and unspecific amplifications are a major problem, especially when using broad range assays. In contrast, FISH probes may potentially be more specific than PCR due to the visualisation of fungal elements in tissue. In contrast to PCR, they appear to work well with formalin fixed specimens. Species identification might be more challenging than by PCR and sequencing. Direct comparisons between FISH and PCR are needed to characterise the pros and cons of each method in determining the aetiology of IFI.
Molecular tissue diagnosis has the potential to evolve into a useful method to describe the aetiology of IFI even in culture negative samples. Results might be obtained fast enough to guide the antifungal therapy in patients with IFI progressive to empiric antifungal therapy. In these patients, the risk associated with invasive tissue sampling might be outweighed by potential benefits of a guided antifungal therapy.
Plasmid-mediated emerging resistance to antibiotics
S73 Carbapenem resistance
T. Walsh* (Cardiff, UK)
The two groups of carbapenemases (serine carbapenemases and metallo-beta-lactamases (MBLs)) can be encoded by genes that can be carried on plasmids. The serine carbapenemases are distinctly either class A or OXA (class D); the latter being mainly associated with Acinetobacter spp.
The dominant MBL subgroups, VIM and IMP have genes that are reportedly carried on plasmids and chromosomes. Recent evidence has shown that the majority of blaVIM-2, even those initially reported, are indeed plasmid mediated and probably accounts for their rapid dissemination. blaVIM-1 genes have been recently shown to be carried on IncN and IncW plasmids. The “Brazilian” MBL gene, blaSPM-1, is exclusively chromosomally encoded. The MBLs SIM-1 and AIM-1 are both chromosomally encoded whereas GIM-1 is encoded from a plasmid of approx. 48 kb. The recently described blaKMH-1 gene is also carried on a plasmid (200 kb). Hitherto, only two MBL-positive plasmid sequences are available thus far – those carrying blaIMP-8 and blaVIM-7. The former carries other resistance genes and are approx. 302 kb (IncHI2), whereas the latter is a small plasmid (24 kb) and shows similarities with IncP plasmids.
OXA carbapenemase genes have been shown to be both plasmid and chromosomally mediated. Thus far, the blaOXA-23 and blaOXA-24/40 clusters can be both plasmid and chromosomal and have mainly been found in Acinetobacter spp. The blaOXA-48 and blaOXA-58 clusters have been found in K. pneumoniae and Acinetobacter spp., respectively, and both are plasmid mediated. blaOXA-48 and blaOXA-58 have been shown to be carried on 70 kb and 28–100 kb plasmids, respectively. A blaOXA-58 plasmid has been recently sequenced and shown to carry two different replicases.
The class A carbapenemase genes, blaKPC, blaIMI-2 and blaGES are all carried on plasmids. blaKPC is found mainly in K. pneumoniae and carried on plasmids that vary in size 12–95 kb and mostly possessing the origin of replication IncN. However, KPC-2 has recently described in a Pseudomonas as being chromosomally mediated. blaIMI-2 is exclusive to the USA and carried on a 66 kb plasmid although blaIMI-1 is chromosomal. The blaGES genes have been found in P. aeruginosa and Enterobacteriaceae of which GES-2, 4, 5 and 6 have been shown to be plasmid mediated although little else in known.
This lecture will provide a synopsis, discuss the evolution of resistance due to plasmids and briefly predict what we may face in the 21C with respect to carbapenemase resistance.
S74 Aminoglycoside resistance and plasmid-mediated 16S rRNA methylases
Y. Arakawa* (Tokyo, JP)
Nosocomial infections caused by multidrug-resistant pathogens, especially Gram-negative bacilli, have become a serious clinical concern in every healthcare setting worldwide. As well as carpapenem-hydrolysing metallo-β-lactamases, CTX-M-type β-lactamases, and qunolone-resistance genetic determinants such as qnr, aac(6”)-Ib-cr, and qepA, plasmid-mediated novel molecular mechanisms such as RmtA, RmtB, RmtC, RmtD, ArmA, and NpmA responsible for pan-resistance to aminoglycosides have recently been identified in Pseudomonas aeruginosa, Acinetobacter spp., Serratia marcescens, Esherichia coli, Klebsiella pneumoniae, Proteus mirabilis etc. since 2003, and these enzymes have indeed methylation activity of 1405G or 1408A at the A-site of the bacterial 16S rRNA as found in aminoglycoside-producing actinomycetes.
These plasmid-mediated 16S rRNA methylases are speculated to be originated from some nonpathogenic environmental microbes that produce aminoglycosides or some similar compounds, so it is quite natural that several new enzymes would be further identified hereafter in both clinical and livestock farming environments. RmtB and ArmA have widely spread in Asia, Europe, America and Australia via various pathogenic Gram-negative bacilli, we should pay special attention to the further spread of such hazardous microbes.
In my talk, I would like to give an outline of newly identified molecular mechanisms that confer pan-resistance to aminoglycosides in pathogenic microbes isolated from both human and veterinary environments.
S75 Quinolone resistance
V. Cattoir* (Caen, FR)
Acquired resistance to quinolones mainly results from chromosomal mutations responsible for modification(s) of DNA gyrase and topoisomerase IV, and for a decrease of drug accumulation into bacteria due to decreased permeability and/or overexpression of efflux systems. Plasmid-mediated quinolone resistance (PMQR) was first reported in 1998 from the USA, and two other mechanisms have been identified to date.
The first PMQR determinants, Qnr proteins, belong to the family of pentapeptide repeat proteins. Five determinants have been identified: QnrA, QnrB, QnrC, QnrD, and QnrS with 6, 20, 1, 1, and 3 different variants, respectively. They may act by binding directly to both DNA gyrase and topoisomerase IV leading to protect them from quinolone inhibition. They confer resistance to nalidixic acid and reduced susceptibility to fluoroquinolones (FQs), but may facilitate recovery of mutants with higher level of resistance. The overall prevalence of QnrA, QnrB, and QnrS determinants generally ranges from 1 to 5%, and they have been identified worldwide mostly in ESBL-producing enterobacterial isolates. The origin of the qnrA and qnrS genes were identified as Shewanella algae and Vibrio splendidus, respectively.
The second type of PMQR determinant, AAC(6')-Ib-cr, is a variant of the aminoglycoside acetyltransferase AAC(6')-Ib which confers resistance to kanamycin, tobramycin and amikacin. This variant possesses two substitutions (Trp102Arg and Asp179Tyr) that are sufficient to acetylation of ciprofloxacin and norfloxacin with a 2-to-4-fold MIC increase. The overall prevalence of aac(6')-Ib-cr may range from 0.4 to up to 34%, and it has been reported mainly in Escherichia coli and Klebsiella pneumoniae.
The third type of PMQR determinant, QepA, has been identified in two E. coli clinical isolates from Japan and Belgium. The qepA gene encodes a 14-transmembrane-segment putative efflux pump belonging to the major facilitator superfamily. This protein confers decreased susceptibility to hydrophilic FQs (e.g. norfloxacin, ciprofloxacin and enrofloxacin) with an 8-to-32-fold MIC increase. The two epidemiological surveys for QepA may indicate its low prevalence (<1%). The natural reservoir of qepA remains unknown but might be an actinomycetal species.
Discovering of three main mechanisms of PMQR within the last ten years is peculiar. It may reflect the emergence of novel mechanisms of resistance but also a deeper investigation of resistance mechanisms in clinical isolates.
Emerging infections: can we cope with them?
O77 Seroprevalence of tularaemia under foxes and raccoon dogs in Germany
A. Kühn*, C. Schulze, H. Ranisch, P. Kutzer, H. Nattermann, R. Grunow (Berlin, Frankfurt-Oder, DE)
Objective: Little is known about the prevalence of Francisella tularensis in humans and animals in Germany. Interestingly, the pathogen emerged recently when several marmosets (Callithrix jacchus) died from tularaemia and a group of hunters became infected in the areas of western Germany. To find out more about the distribution of the pathogen also in eastern Germany we investigated the seroprevalence of tularaemia under foxes (Vulpes vulpes) and raccoon dogs (Nyctereutes procyonoides) in the area of Brandenburg (around Berlin).
Methods: Sera of animals (n = 351 and n = 32, respectively) from the years 2007 and 2008 were tested for F. tularensis – LPS antibodies in an indirect ELISA and suspicious samples were confirmed by Western blot for LPS ladder recognition using Protein G – POD conjugate. Furthermore we investigated the serum samples by a competitive ELISA using a peroxidase-conjugated anti – LPS monoclonal antibody.
Results: From the serum collection, we tested 31 (8.8%) foxes and 3 raccoon dogs (9.4%) positive for specific F. tularensis antibodies. The geographical distribution showed hot spots in the area of the investigated region.
Conclusions: Our results indicate for a higher seroprevalence in wildlife for tularaemia in eastern regions of Germany than assumed. Since the reported human cases for the last decade seem to be underestimated, the real prevalence of the pathogen is unknown. The high number of tularaemia antibody positive foxes and raccoon dogs indicates that this zoonose is present in wildlife in eastern Germany. However, the impact of transmission of zoonotic pathogens from wildlife to domestic animals and humans is not yet well studied.
O78 Aetiological and epidemiological studies on Q fever and Mediterranean spotted fever in animals
S. Martinov* (Sofia, BG)
Q fever and Mediterranean spotted fever (MSF) are leading in presence and importance rickettsial diseases in Bulgaria. The aim of the work is to present the contemporary state of these diseases on the basias of vast aetiological, clinical and eppidemiological investigations. Employed were complement fixation test, microimmunofluorescent test, isolation of the agent, immunofluorescent haemocytic test (IFHT). A retrospective analysis of the state of the agricultural foci of Q fever was carried out by examination of more than 320 000 blood sera. During 2003–2008 the mean seropositivity for C. burnettii in domestic ruminants was 10, 11%. Seropositive swine, geese, ducks, cats and dogs were also established. In general 88 Coxiella burnettii isolates from animal clinical and pathological materials were obtained. By means of IFHT was found that 16.8% ixodic ticks out of 1769 examined were infected with C. burnettii. Eleven Coxiella strains were isolated from ticks. Significant seropositive rate (20, 42%) for Rickettsia conorii was established in 2473 sheep, goats and cattle from MSF endemic and non-endemic regions. The IFHT examination of 865 ticks revealed 19.76% R. conorii positive. From ticks were isolated three strains of R. conorii and two of R. sibirica. In conclusion, the obtained data will contribute for creating of up-to-date strategy for more efficient control of the two rickettsial zoonoses.
O79 High rate of Pneumocystis jirovecii colonisation among inpatients and hospital healthcare workers
F. Medrano, V. Friaza*, R. Morilla, C. de la Horra, I. Martín-Garrido, A. Gasch, R. Valencia, M. Montes-Cano, J. Varela, E. Calderón (Seville, ES)
Objectives: In two recent pilot studies Pneumocystis has been detected in immunocompetent health care workers (HCW) suggesting the possibility of nosocomial transmission of the infection. The aim of this study was to evaluate the prevalence of P. jirovecii carriage among hospitalised patients (HP) and staff members in a general hospital.
Methods: Cross-sectional study carried out from 2004 to 2006 including 130 HP hospitalised at the Virgen del Rocio University Hospital in different areas at risk for Pneumocystis: (i) High risk units (Paediatric Onco-haematology, Paediatric HIV, Adults HIV and Neumology, n = 57); (ii) Indeterminate risk units (Internal Medicine and Gynaecology, n = 73). At the same time in each unit were evaluated a total of 145 HCW. Each participant underwent a clinical-epidemiologic examination, and oropharyngeal wash (OW) samples were collected for analysis. P. jirovecii colonisation was identified by nested PCR at mtLSUrRNA gene using the external primers pAZ102-E/-H and the internal primers pAZ102-X/-Y in OW samples. The genotyping was based in analysis of two independent genetic loci of P. jirovecii: mtLSUrRNA fragment by direct sequencing, and dihydropteroate synthase (DHPS) locus by a restriction fragment length polymorphism assay.
Results: P. jirovecii DNA was identified in 39/130 (30%) of HP and in 40/145 (27.6%) of HCW. None of colonised patients had PcP. Among HP the prevalence rates of colonisation ranged from 27.2% to 40% in high risk units and from 17.6% to 33.3% in indeterminate risk units. Among HCW the prevalence rates ranged from 18.2% to 53.8%. All colonised HCW were asymptomatic at the time of their enrolment in the study and none have any evident cause of immunosuppression or risk factors for HIV infection. The distribution of genotypes among HP and HCW were similar: (i) mtLSUrRNA type 1 in 11/30 of HP and in 15/31 of HCW; (ii) Mutant DHPS genotypes associated with sulfa-resistence in 3/30 of HP and in 2/30 of HCW. DNA was amplified by PCR in 2/8 air samples from the rooms of hospitalised patients.
Conclusion: The study shows for the first time a high rate of P. jirovecii colonisation among hospitalised patients and staff members in all the evaluated areas of a general hospital. This finding, besides the concordance of genotypes in both groups and the detection of DNA of the pathogen in the hospital environment air support the role of potential nosocomial transmission of Pneumocystis infection.
Supported by CIBERESP
O80 Isolation of Helicobacter bizzozeronii from a Finnish patient with severe dyspeptic symptoms and chronic active gastritis
R. Kivistö*, J. Linros, M. Rossi, H. Rautelin, M.L. Hänninen (Helsinki, Kerava, FI)
Objective: Helicobacter pylori is established as the primary cause of gastritis and peptic ulceration in humans. In a minority of patients with upper gastrointestinal symptoms long tightly coiled spiral bacteria, clearly distinct from H. pylori, and provisionally named as “H. heilmannii”, can be observed in gastric biopsies. Our objective was to isolate and identify the spiral organism, resembling “H. heilmannii” from the gastric mucosa of a Finnish patient presenting with severe dyspeptic symptoms.
Methods: We used two different selective media for the isolation of the bacteria from gastric biopsy samples before and after treatment of the patient with a 7-day course with lansoprazole, tetracycline and metronidazole. The isolates were characterised by testing for urease and catalase activity, light and electron microscopy, and sequencing the partial 16S rRNA and ureAB genes. Single enzyme AFLP was used to analyse the genetic diversity among the isolates.
Results: Growth of long spiral organisms was obtained from 7 out of 8 antrum and all 8 corpus biopsies before and all three antrum biopsies after treatment of the patient. The partial 16S rRNA gene sequence showed high sequence similarities with other gastric Helicobacter species. The partial ureAB gene showed high sequence similarity with H. bizzozeronii and was clearly distinct from other gastric Helicobacter species. AFLP indicated that the isolates belonged to the same clone however some minor genetic diversity was observed among the isolates. Conclusions: H. bizzozeronii remains as the only “H. heilmannii” species isolated from the human gastric mucosa. The treatment with lansoprazole, tetracycline and metronidazole did not clear the H. bizzozeronii infection neither were the symptoms totally resolved. AFLP analysis suggested that all the isolates belong to the same clone with some evidence of genetic diversity among the H. bizzozeronii isolates in the human gastric mucosa. Further studies are needed to clarify this in more detail.
O81 The habitat of the melioidosis bacterium Burkholderia pseudomallei in endemic tropical Australia
M. Kaestli*, G. Yang, G. Williamson, M. Mayo, L. Ward, G. Harrington, F. Watt, A.C. Cheng, B.J. Currie (Darwin, AU)
Objectives: The soil bacterium Burkholderia pseudomallei causes the severe disease melioidosis in humans and animals and is endemic in tropical Australia and Southeast Asia. Despite the recognition that melioidosis is an emerging infectious disease, its natural habitat and distribution are unknown in tropical northern Australia, as well as worldwide, which is a major limitation for public health education programs. We aim to characterise the habitat of B. pseudomallei and based on our findings, generate prediction maps for endemic northern Australia to reveal areas with increased risk for exposure to these potentially deadly bacteria.
Methods: 809 soil samples from rural Darwin in northern Australia collected in the dry and wet season 2006/2007 were screened for B. pseudomallei using a previously validated real-time PCR-based direct soil B. pseudomallei detection method. Multivariate cluster logistic regression analysis was performed to assess the association of B. pseudomallei with environmental factors. These factors were incorporated into a Bayesian model which was used to generate maps predicting the presence of B. pseudomallei in endemic northern Australia.
Results: B. pseudomallei was primarily found in close proximity to streams and in grass-rich areas but was also correlated with environmentally disturbed soil such as caused by the presence of animals, farming or irrigation. Prediction maps are currently being verified by sampling predicted B. pseudomallei “hot-” and “cold-spots”. See in figure a prediction map for rural Darwin with red areas indicating high probability for presence of B. pseudomallei.

Conclusions: This study contributes to the elucidation of the environmental distribution of B. pseudomallei in endemic tropical Australia and to the clarification of environmental factors influencing its occurrence. It also raises concerns that B. pseudomallei are spreading due to changes in land management.
O82 Concurrent multi-serotypic dengue infections in various body fluids
W. Kulwichit*, S. Krajiw, D. Chansinghakul, G. Suwanpimolkul, O. Prommalikit, P. Suandork, J. Pupaibool, K. Arunyingmongkol, C. Pancharoen, U. Thisyakorn (Bangkok, TH)
Objectives: Dengue virus infection is one of the rapidly-spreading emerging diseases worldwide. The virus is divided into 4 distinct serotypes with limited cross-protective immunity; therefore, one can be reinfected with different serotypes. While each episode is usually caused by a single serotype, an individual can occasionally be infected by concurrent multiple ones. Our group has previously detected dengue virus from urine and oral specimens of some patients. In this study, we sought to determine the characteristics of multi-serotype infections when analysing beyond the patients' blood compartments.
Methods: During 2003–2007, paediatric and adult patients suspected of dengue infections were enrolled. Plasma, peripheral blood mononuclear cells (PBMC), urine pellets, buccal brushes, and saliva were collected during and after the febrile episode. Only specimens from patients with both positive dengue serology and pan-dengue-specific RT-PCR were included. Serotype-specific RT-PCR was then performed on the aforementioned various specimens of each patient.
Results: 95 patients met the above criteria. Serotyping was successful in 85 patients. DEN-4 was the most common serotype, accounting for half of the cases. 20 of these 85 (23.5%) demonstrated multi-serotypic infections when combining data from all specimen types in each individual. Serotyping using single, conventional serum/plasma specimens, however, would detect only half of the cases. The phenomenon of concurrent multi-serotypic infections was present in all examined specimen types, including urine pellets, buccal brushes, and saliva. The most frequent combinations were DEN-1 + DEN-4 and DEN-2 + DEN-4 (5 cases each). Two patients were simultaneously infected by serotypes 1, 2, and 4 and one by serotypes 1, 3, and 4. There was no demonstrable significant difference in clinical severity between single- and multi-serotypic infections.
Conclusion: In a dengue-hyperendemic country with simultaneous circulation of all four serotypes, the phenomenon of concurrent multi-serotypic infections are more common than previously demonstrated by traditional serotyping on single serum/plasma specimens. This may be explained by the sensitivity limitation of the detection method or by biological behaviour of the virus. Our findings have an implication for potentially more accurate epidemiologic studies in the future, and for further exploratory investigations regarding dengue virus in various secretions and excretions.
O83 Emerging concepts about the evolutionary history of hantaviruses
H.J. Kang, S.N. Bennett, L. Sumibcay, S. Arai, A.G. Hope, J.A. Cook, J.W. Song, R. Yanagihara* (Honolulu, Albuquerque, US; Tokyo, JP; Seoul, KR)
Objective: Recent discovery of genetically distinct hantaviruses in shrews (family Soricidae), captured in widely separated geographic regions, challenges the conventional view that rodents are the principal and progenitor reservoir hosts of hantaviruses, and raises the possibility that other soricomorphs, notably moles (family Talpidae), harbour hantaviruses.
Methods: Using oligonucleotide primers based on conserved genomic regions of rodent- and soricid-borne hantaviruses, RNA extracts from tissues of the Japanese shrew mole (Urotrichus talpoides), American shrew mole (Neurotrichus gibbsii) and European common mole (Talpa europaea) were analyzed for hantavirus sequences by RT-PCR. Newfound S-, M- and L-segment sequences were aligned using Clustal W and were analyzed phylogenetically by the maximum-likelihood and Markov Chain Monte Carlo tree-sampling methods, with the GTR+I+G model of evolution.
Results: Novel hantavirus genomes, designated Asama virus (ASAV), Oxbow virus (OXBV) and Nova virus (NVAV), were detected in tissues of Urotrichus talpoides, Neurotrichus gibbsii and Talpa europaea, respectively. Sequence and phylogenetic analyses indicated that ASAV and OXBV were related to hantaviruses harboured by soricine shrews in Eurasia and North America, respectively. By contrast, phylogenetic analyses of full-length S- and L-segment sequences showed that NVAV formed a unique clade, clearly distinct and evolutionarily distant from all other hantaviruses. Despite the high degree of sequence divergence at the nucleotide and amino acid levels, the secondary structures of the nucleocapsid proteins, as well as the L-segment motifs, of the mole-associated hantaviruses were well conserved.
Conclusions: While cross-species transmission has influenced the course of hantavirus evolution, such host-switching events alone do not satisfactorily explain the co-existence and distribution of genetically distinct hantaviruses among species in two taxonomic orders of small mammals spanning four continents. When viewed within the context of molecular phylogeny and zoogeography, the close association between distinct hantavirus clades and specific subfamilies of rodents, shrews and moles is likely the result of alternating and variable periodic co-divergence at certain taxonomic levels through evolutionary time. Thus, the primeval hantavirus might have arisen from an insect-borne virus, with ancestral soricomorphs, rather than rodents, serving as the original mammalian hosts.
O84 High transmission of hepatitis E virus among piglets in farms from south-eastern France
M. Kaba, B. Davoust, J.L. Marié, M. Barthet, M. Henry, C. Tamalet, J.M. Rolain, D. Raoult, P. Colson* (Marseille, Toulon, FR)
Objectives: Autochthonous hepatitis E is currently considered as an emerging disease in industrialised countries and several studies suggest that hepatitis E is a zoonosis, especially in pigs, boars and deer. We aimed to study whether hepatitis E virus (HEV) is commonly present in domestic pigs in southern France, and to determine the relationship between HEV sequences detected from pigs and those described in human hepatitis E cases.
Methods: Serum and stools samples were collected from 207 three or six-month-old pigs from different regions of southern France. 107 six-month-old pigs were from a slaughterhouse, and 100 three-month-old pigs were from a pig farm. Swine IgG anti-HEV antibodies testing was performed using a commercial ELISA kit for clinical diagnosis with minor modifications. Swine HEV RNA detection was conducted by realtime PCR and amplification/sequencing assays using in house protocols targeting the 5'ORF2 region of the HEV genome.
Results: 40% of pigs were seropositive, and 65% of three-month-old pigs were HEV RNA-positive, whereas none of the six-month-old pigs were HEV RNA-positive. HEV RNA was significantly more frequently detected from stools than from serum (65% versus 22%; p < 0.001). Phylogenetic analysis showed that swine HEV sequences belong to genotype 3f or 3e and formed two clusters within which sequences showed high nucleotide homology (>97%). These clusters were correlated with the geographical origin of pigs as well as with their repartition into pens and buildings in the pig farm where samples were collected. Swine HEV sequences from the present study were genetically close to HEV sequences found from humans or swine in Europe, although no strong phylogenetic link could be observed neither with these latter sequences nor with those from human hepatitis E cases diagnosed in the laboratory.
Conclusion: Our data indicate that three-month-old farm pigs from southern France might represent a potential source of contamination to humans, and they underscore the great potential of HEV to cause epizootic infections in populations of farm pigs.
O85 Clostridium difficile: changing epidemiology trends, 2000–2007
S.N. Reddy*, S. Taori, P. Kalima, I.R. Poxton (Edinburgh, UK)
Objectives: Clostridium difficile Infection (CDI) has become a growing concern world-wide with an increased reported incidence and an increase in the associated financial burden. Our aim therefore was to review trends in CDI occurring from 2000–2007 inclusive.
Methods: All patients admitted to Lothian University Hospitals Division (LUHD) tested for C. difficile toxins A+B by EIA were included. Retrospective analysis of prospectively collected data was performed. The number of occupied bed days was provided by NHS-Lothian Statistics Department. The most recent published costs associated with CDI were used to estimate potential costs to Lothian NHS Trust.
Results: 50,590 faecal samples were tested for C. difficile toxins from 2000–2007 inclusive; of these 7301 samples were positive. Overall CDI was identified in 15.2 cases/10000 patient days and 5.8 cases/1000 inpatient hospital admissions.
The incidence of identified CDI rose from 3.6cases/10000 patient days in 2000 to 14.8cases/10000 patient days in 2007. Incidence also increased with age from 3.3cases/10000 patient days in the 0–20 years age group to 18.1cases/10000 patient days in the 61–80 years age group.
Renal Medicine and Intensive Care had the highest incidences of identified CDI with greater than 57cases/10000 patient days each followed by Infectious Diseases and Gastrointestinal Medicine whose rates were 47.5 and 42.6 cases/10000 patient days respectively. Medicine of the Elderly in comparison had an incidence of 19.5cases/10000 patient days.
Of note 10% of all patients were transferred through a minimum of two specialties during the period in which they remained positive for C. difficile toxins.
Estimated costs over the study period for toxin testing alone were in the region of £126,500 and the minimal potential hospitalisation costs of patients with CDI was in the region of £20,000,000.
Conclusion: The incidence of patients identified with CDI has risen markedly and not surprisingly the incidence has also been noted to increase with age. Medicine of the Elderly however had a much lower incidence than several other specialties and therefore risk assessment of CDI development and containment should now also be targeted within other specialties.
With 10% of identified CDI patients transferred through different specialties and the significant financial burden CDI imposes on healthcare institutions judicious application of infection control measures remains an important factor to prevent CDI spread.
O86 First results of the European Clostridium difficile infection survey (ECDIS)
M.P. Bauer*, D.W. Notermans, B.H.B. van Benthem, M.H. Wilcox, D. L. Monnet, J.T. van Dissel, E.J. Kuijper on behalf of the ECDIS Study Group and local coordinators
Objectives: To perform a survey on the incidence and the demographic, clinical and microbiological characteristics of Clostridium difficile infection (CDI) in hospitals in Europe.
Methods: We organised a network of 106 laboratories capable of isolating C. difficile strains in 34 European countries. In November 2008, 1–7 hospitals per country, depending on population size, tested all stool samples of patients >2 years of age who developed diarrhoea after ≥3 days of admission or were suspected of CDI. CDI was defined as having a positive enzyme immunoassay for C. difficile toxin A and/or B, a positive cytotoxicity test or a positive toxinogenic culture. Hospitals collected clinical data of the first 10 CDI patients and cultured their stools for C. difficile. Isolates were characterised by PCR-ribotyping and toxin A, toxin B and binary toxin genes.
Results: Detailed information was obtained for 506 patients in 69 hospitals in 28 countries. Eighty percent of cases were healthcare-associated (HA), 15% community-associated (CA) and 6% of indeterminate association (i.e., 4 to 12 weeks after discharge from a healthcare facility) (ECDC definitions; data available for 480 cases). Median age was 71 (IQR 56–81) yrs. Fever, ileus, leukocyte count ≥15 10E9/l and creatinin increase >50%, used as markers of severe CDI, were present in 37%, 4%, 29% and 8%, respectively. Colonoscopy was performed in 28 cases, revealing ulceration in 46% and pseudomembranes in 21% of cases. Bowel distension was observed in 26 (23%) of 115 imaging studies and colonic wall thickening in 26 (42%) of 62 CT scans. Serious comorbidity, as defined by an APACHE II chronic health score >0 was present in 42%. Of 460 patients, 79% had used antibiotics in the month and 92% in the 3 months preceding CDI. The most frequently used antibiotics were fluoroquinolones, cephalosporins and aminopenicillins with beta-lactamase inhibitors. The extrapolated median incidence of HA CDI was 3.8 cases per 10,000 patient-days (IQR: 0.8 to 8.1), based on 48 hospitals that had submitted data on all CDI cases by February 23rd, 2009. Results of the typing studies and follow-up of CDI patients 3 months after the inclusion will be available in May 2009.
Conclusion: In this pan-European hospital-based study, the median incidence of HA CDI was 3.8 per 10,000 patient-days. Most patients fulfilled the classical risk profile of the elderly patient with significant co-morbidities and recent antibiotic use.
Staphylococci: epidemiology and resistance
O87 Clinical and bacteriologic characteristics of a 5-year cohort of MRSA patients at a large U.S. metropolitan hospital
M. Pastagia*, L. Kleinman, S. Huprikar, S. Jenkins (New York, US)
Objective: Vancomycin therapy for methicillin resistant Staphylococcus aureus (MRSA) may fail even when minimum inhibitory concentrations (MIC) indicate susceptibility. Patients also fail therapy when heteroresistant vancomycin intermediate Staphylococcus aureus (hVISA) develops. This study integrates laboratory and clinical data to identify factors correlated with mortality in patients with MRSA sepsis.
Methods: In a large urban hospital, 699 blood culture isolates of MRSA from 2002–2007 with vancomycin MIC initially reported as <2 µg/mL using an automated system were retrieved from a −70°C freezer and subcultured. Etest (AB Biodisk) MIC determinations for vancomycin, daptomycin, and linezolid were performed on the isolates. Strains for which the MIC exceeded 1 µg/mL were tested with teicoplanin by Etest to detect possible hVISA. VISA was defined using Clinical and Laboratory Standards Institute criteria of 4–8 mg/mL, and hVISA using published criteria. We abstracted clinical and demographic data from all 699 medical charts. Outcomes data included in-hospital mortality and facility of discharge. We performed univariate and bivariate analyses, and multiple logistic regression.
Results: Mortality was 28.3%; 16.9% of isolates were VISA and 6.4%, hVISA. Bivariate analysis revealed higher mortality associated with several clinical factors: admission from a long term facility, hospitalisation in the past month, surgery in the past 90 days, endocarditis, soft tissue infections, infections of nonvascular prosthetics or the presence of cirrhosis, diabetes mellitus, or renal failure (all p < 0.05). Infectious diseases (ID) consult was protective (p < 0.001). Although VISA and hVISA did not predict MRSA-attributed mortality (p = .43), having either increased the odds of all cause mortality even after controlling for age, race, and ID consult, with an adjusted odds ratio (AOR) = 1.6 (p = 0.03) in multivariable models. Asian race had AOR = 1.8 (p = 0.02). The AOR for ID consult was 0.8, but not significant (p = 0.29). Table 1 shows: many patients deteriorate from their pre-morbid health status (p = 0.06)
| Strain | N | Admitted from |
Discharged |
Dead | |||||
|---|---|---|---|---|---|---|---|---|---|
| Home | Outside hospital | Nursing home | Home | to Rehab | to Nursing home | to Hospice | |||
| hVISA | 45 | 60% | 22% | 18% | 27% | 18% | 13% | 2% | 40% |
| VISA | 118 | 59% | 15% | 26% | 32% | 14% | 16% | 4% | 34% |
| Neither hVISA nor VISA | 536 | 61% | 21% | 18% | 35% | 17% | 19% | 3% | 26% |
| “Healthy” admission | “Sick or Frail” admission | “Good or Healthy” discharge | “Frail or Bad” discharge | ||||||
| hVISA | 45 | 60% | 40% | 45% | 55% | ||||
| VISA | 118 | 59% | 41% | 46% | 54% | ||||
| Neither hVISA nor VISA | 536 | 61% | 39% | 52% | 48% | ||||
Conclusions: Many patients with MRSA sepsis will die; others leave the hospital needing more care than when admitted. Integrating clinical and laboratory data may permit risk stratification, identify patients most likely to benefit from an ID consult, and provide prognostic information. Comorbidities and recent medical history should be included in future studies of MRSA care and outcomes.
O88 Modelling the effect of time-dependent exposure on hospital mortality using data from the BURDEN study group
M. Wolkewitz*, M. Schumacher, P. Davey for the BURDEN Study Group
Objectives: To explore the time dynamics of exposure to hospital acquired Staph aureus bacteraemia (SAB) and its impact on hospital mortality by using modern survival models.
Methods: The study population was adults resident in Tayside, Scotland, who had a new admission to Ninewells Hospital between 1st July 2005 and 30th June 2006. The cohort enrolled patients from this population who stayed in hospital for at least two days and were admitted to wards with at least one case of SAB in the study period. Our primary analysis used a survival model, which has two key differences compared to a logistic regression model. First the exposure to SAB is regarded as a time-dependent variable. Second the primary outcome (hospital mortality) is recognised as a competing event for the secondary outcome of being discharged alive from hospital. This is furthermore important because increased length of stay is likely to be associated with increased risk of death in hospital.
Results: The cohort enrolled 3132 patients of whom 203 died in hospital. There were 58 cases of SAB, 31 patients had MRSAB (SAB with meticillin resistant Staph aureus) of whom 12 died and 27 had MSSAB (SAB with meticillin sensitive Staph aureus) of whom 5 died. MRSAB occurred later than MSSAB (median 14.5 days after admission, inter quartile range 9 to 34 days versus 8 days, inter quartile range 5 to 12 days for MSSAB). After adjusting for age, sex, comorbidity and previous hospitalisation the hazard ratio for hospital mortality from the subdistribution hazard model was 15.1 (95%-CI: 8.3 to 27.4) for MRSAB and 5.9 (95%-CI: 2.4 to 14.7) for MSSAB. Cause-specific hazard analysis showed that both MRSAB and MSSAB significantly reduced the hazard of being discharged alive and suggested that increased length of stay contributed to the increased hazard of death in hospital.
Conclusion: The timing of events is crucial in hospital epidemiology when time-dependent exposures and competing events are present. Standard logistic regression ignores the time-dependent nature of the data and is only a crude approach. Cumulative hazards and probability plots provided additional insights into the mechanism, suggesting SAB has both a direct impact on hospital mortality and an indirect effect through increased length of stay.
O89 Update on mandatory bacteraemia surveillance in English national health service acute trusts: trends and sources of methicillin-resistant Staphylococcus aureus
A. Pearson*, R. Guy, R. Blackburn, R. Mandalia, J. Davies, M. Murray, M. Painter, S. Batley, B. Duerden, J. Giltrow, M. Fleming (London, UK)
Objectives: This paper describes the trends in mandatory reporting of Meticillin-resistant Staphylococcus aureus (MRSA) bacteraemia identified in community and hospital healthcare facilities and reviews the available information on the presumed source of these infections.
Methods: Data were collected via a web-enabled data capture system. All National Health Service (NHS) Trusts (hospital groups) are required to report all MRSA bacteraemia cases, with the exception of those reoccurring within 14 days of the first report. Cases of MRSA bacteraemia diagnosed on presentation or within 2 days following admission to an acute NHS hospital are defined as “community associated” whilst cases diagnosed 2 or more days after admission are defined as “healthcare acquired” as the bacteraemia is believed to be acquired during the current hospital stay. Cases were excluded from analysis if either there was missing data or the blood culture was taken outside of an acute Trust setting.
Enhanced data has been collected since May 2006, since then Trusts provided data on more than 12,400 MRSA bacteraemia cases. 45% of cases (64% of which were reported with an acceptable degree of certainty) had data on source of bacteraemia.
Results: More than 16,500 reports of MRSA bacteraemia were received from 170 English NHS acute Trusts between October 2005 and December 2008.
Two thirds of MRSA bacteraemia cases were diagnosed two or more days after admission indicating hospital acquisition during the current stay. The remaining third of cases either acquired their MRSA bacteraemia in the community, or from nursing care homes (18%) or from the healthcare facility from which they were admitted (6%).
The suspected source of bacteraemia varied according to timing of detection. In community associated cases the most frequently identified source was skin or soft tissue infection (26%) while in healthcare acquired cases intravenous catheters were the most frequently identified source of bacteraemia (37%).
Conclusion: Reports of healthcare associated MRSA bacteraemia cases between Quarter 4 in 2005 and Quarter 4 in 2008 have reduced by more than 70% as compared to a 51% decrease in community associated cases. These data also provide an important means of identifying sources of bacteraemia, enabling target of infection control measures (care bundles) to specific routes of transmission and source. Mandatory enhanced surveillance has provided an evidence base on which to target interventions.
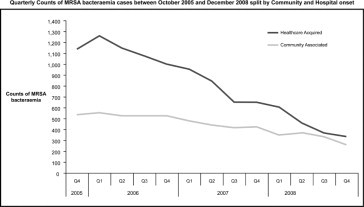
O90 Molecular characterisation of S. aureus involved in varicella superinfections in France
O. Raulin, G. Durand, M. Croze, M. Bes, H. Meugnier, F. Vandenesch, Y. Gillet, G. Lina, F. Laurent*, J. Etienne (Lyon, FR)
Varicella has traditionally been regarded as a benign disease that most commonly occurs in childhood, but serious complications are reported. One can estimate that patients with complications represent 4 to 9% of all varicella cases. The most common complications are bacterial superinfections (31 to 70%) and particularly superficial skin infections (20 to 50% of all complications). Streptococcus pyogenes and Staphylococcus aureus are the bacteria more frequently related to these superinfections.
Method: Between 2002 and 2007 the French Reference Center for Staphylococci received 58 S. aureus isolates involved in varicella superinfections. The aim of this study was to characterise their toxin profiles and to seek correlation between toxin expression and clinical manifestations. The toxinic profile (eta, etb, tst, pvl, sea-c, seh, sek-m, seo, hlb, lukM) and the presence of gene mecA were determined by PCR completed by the determination of the agr group; spa typing was used to complete characterisation of some strains.
Results: Results show a high incidence of MRSA (n = 19, 32%) among which a majority (n = 12, 63%) belonged to the emergent Geraldine clone (agr2, ST5, tst+); the PVL positive MRSA ST80 clone was detected for 2 isolates and the exfoliatin positive MRSA ST88 was detected for one. Overall, the presence of a major toxin such as TSST-1, ETA and/or ETB, and PVL was detected for 54% (35/58) of the isolates (TSST-1 28%, ETA/ETB 17%, PVL 9%). Clinical manifestations were correlated with manifestations usually described for these toxins: exfoliatins were associated with bullous impetigo or staphylococcal scalded-skin syndrome whereas PVL was associated with abscesses. Nevertheless, for TSST-1, clinical manifestations were more heterogeneous, including staphylococcal scarlet fever, toxic shock, septic shock, and suppurative diseases. When TSST-1, ETA/ETB and PVL were absent, clinical manifestations were polymorphous.
Conclusion: These data lead i) to discuss the empiric antibiotherapy of these community-acquired superinfections, and ii) to highlight the severity of staphylococcal varicella complications.
O91 Differentiation of CC59 community-acquired MRSA strains
S. Monecke*, F. O'Brien, G. Coombs, H.L. Tan, J. Pearson, R. Ehricht (Dresden, Jena, DE; Perth, AU)
Objectives: A collection of clonal complex 59 community acquired MRSA strains collected in Western Australia (WA) from 2003 to 2008 was to be characterised with special emphasis on PVL and SCCmec elements.
Methods: Previously described (Monecke & Ehricht 2006–2008) diagnostic microarrays as well as PFGE, MLST and several PCRs for characterisation of SCCmec elements were used.
Results: Carriage of toxin genes and SCCmec elements allowed to distinguish six strains. One strain, ST87-MRSA-IV (WA MRSA-24) carried a SCCmec IV element, enterotoxins seb, sek and seq, but no PVL. There was one deviant isolate related to that strain which warrants further characterisation, especially with regard to its SCCmec element. A second strain included ST59-MRSA-IV and ST922-MRSA-IV (WA MRSA-49 and -55), which differed in pta and yqil alleles. It carried a SCCmec IV element, seb, sek and seq, and it was PVL-positive. A third strain, ST59-MRSA-IV (WA MRSA-56) carried a SCCmec IV. It was positive for PVL and enterotoxin genes sea, seb, sek and seq. A fourth strain was ST59-MRSA-IV+V (WA MRSA-15) carrying SCCmec elements of type IV and V, or a composite element combining features of both. Isolates of this strain were PVL negative, but positive for enterotoxin A (sea) and, in most cases, also for seb, sek and seq. A fifth strain was the “Taiwan Clone”, ST59/952-MRSA-V (WA MRSA-9 and -52) which also comprised two closely related sequence types. This strain carried a SCCmec element of type V(T) or VII as well as PVL and, usually, seb, sek and seq. It was the most common CC59 strain in WA. The sixth strain differed from the “Taiwan Clone” in the presence of a SCCmec type V element and in the absence of PVL.
Conclusion: The differentiation of this clonal complex into various different strains indicates a rapid evolution and spread of SCCmec elements, and the diagnostic microarray technology allows one to distinguish beyond MLST level and hence to accurately trace outbreaks and spread of these strains.
O92 Identification of a clinical methicillin-resistant Staphylococcus aureus strain containing both SCCmec type IV and SCC476-like sequences
P. Beisser*, C. von Wintersdorff, M.L. Boumans, H. de Neeling, E. Stobberingh (Maastricht, Bilthoven, NL)
Objectives: SCCmec typing has become a valuable tool for the molecular epidemiology of methicillin-resistant Staphylococcus aureus (MRSA) infections. To date, 8 SCCmec types have been described worldwide. The aim of the study was to characterise a new, yet untypable SCCmec from a clinical MRSA isolate.
Methods: Samples from an outbreak in a paediatric ward in a Dutch university hospital were subjected to both previously described PCR-based SCCmec typing assays, and a novel typing assay involving multiplex realtime-PCR. From one isolate, SCCmec DNA was obtained using long-range PCR. The DNA sequence was subsequently obtained by shotgun-sequencing.
Results: Two isolates (Spa type 447, PFGE cluster 55) from a hospital outbreak were investigated and identified as type II SCCmec MRSA by conventional SCCmec typing. Interestingly, by using a novel typing assay (see Abtract 1354) both ccr1- and ccr2-like sequences were detected in each of these samples–a combination that has not been reported before. Preliminary sequence data reveal that the untypable SCCmec (approximately 50 kb) contains both SCC476-like and SCCmec type IV-like sequences in tandem.
Conclusions: The previously published SCC467 sequence was identified in an MLST ST1 strain, whereas the strain containing the untypable SCC467/SCCmec type IV-like cassette has MLST CC5-like traits. It is likely that this new SCCmec variant is prevalent MRSA outbreaks in several Dutch hospitals. To investgate this further, a larger collection of PFGE cluster 55 isolates is currently being screened.
O93 Acquisition and persistence of methicillin-resistant Staphylococcus aureus Clonal Complex 398 during occupational exposure
B. van Cleef*, A. Haenen, M. van den Broek, X.W. Huijsdens, M. Mulders, J. Kluytmans (Bilthoven, Zutphen, Amsterdam, NL)
Objective: To determine the risk of acquiring Methicillin-resistant Staphylococcus aureus Clonal Complex 398 (MRSA-CC398) after short-duration occupational exposure to pigs, and to determine the persistence of MRSA-CC398 colonisation after acquisition.
Methods: In a pilot study on the prevalence of MRSA-CC398 in pig farms [1] veterinary sample takers were tested before, directly after and 24 hours after visiting the farm. These sample takers all had short contact with pigs and dust on the farms, and were therefore at risk of acquiring MRSA if it was present on the particular farm. Data on farm characteristics (i.e. kind of farm, number of pigs, other animals present, and hygiene measures), veterinary samples and nasal samples of sample takers were collected. MRSA isolates were typed by staphylococcal protein A (spa) typing.
Results: Complete data sets (samples taken before, directly after and 24 hours after a visit) were collected on 141 visits by 29 sample takers visiting 50 farms. On 28 farms MRSA was collected from pigs or stable-dust (56%). These farms were visited 78 times by 23 different sample takers. One sample taker (#12) was positive for MRSA before visiting a farm, he was removed from the following analysis.
Fifteen of the 78 (19%) visits to MRSA-positive farms resulted in acquisition of MRSA and 11/23 (48%) sample takers acquired MRSA at least once after visiting a positive farm. Of these 11 positive sample takers 2 acquired MRSA twice and 1 sample taker acquired MRSA three times after separate visits. Of the 15 acquisitions of MRSA, 13 were negative after 24 hours. The spa-types of MRSA isolates found on the farms and sample takers were grossly comparable. On the 32 negative farms, none of the 60 visits resulted in MRSA acquisition. For further information see the table .
Table.
Positive MRSA-tests of sample takers. Tests were taken before, directly after and 24 hours after visiting a farm. MRSA-status is indicated as + (positive) and – (negative), spa-types are shown between brackets.
| Sample taker | farm MRSA-status (spa-type) | MRSA-test (spa-type) |
||
|---|---|---|---|---|
| before visit | directly after visit | 24 hours after visit | ||
| 1 | + (t011) | − | + (t011) | − |
| 2 | + (t011) | − | + (t011) | − |
| 3 | + (t011) | − | + (t011) | − |
| + (t108) | − | + (t108) | − | |
| 4 | + (t108) | − | + (t108) | − |
| + (t011) | − | + (t011) | − | |
| + (t108) | − | + (t108) | − | |
| 5 | + (t011) | − | + (t108)b | − |
| 6 | + (t011, t108, t1456) | − | − | + (t108)c |
| 7 | + (t011, t108, t2330) | − | + (t108) | − |
| + (t567) | − | + (t567) | − | |
| 8 | + (t108) | − | + (t108) | − |
| 9 | + (t011) | − | + (t011) | + (t011)d |
| 10 | + (t011) | − | + (t011) | − |
| 11 | + (t108) | − | + (t108) | − |
| 12a | + (t899) | + (t011) | + (t011) | + (t011) |
| + (t011) | + (t011) | + (t011) | + (t011) | |
| − | + (t108) | + (t108) | + (t108) | |
Sample taker 12 has daily contact with poultry and is excluded from analysis.
Sample taker 5 reported no contact with livestock elsewhere than in this study at that moment (spa-types of sample taker 5 and farm are not corresponding).
Sample taker 6 tested MRSA-negative in following tests.
Sample taker 9 was not tested again.
Discussion: MRSA-CC398 was acquired by 48% of the sample takers after occupational exposure in this study. However, in 11 of the 13 cases the strain was not recovered the next day, therefore acquisition was of short duration, posing a limited treat to human health. Some persons seemed to be more vulnerable to acquire MRSA during their work. The sample size of this study was too small to draw final conclusions concerning this inter-personal variation. This requires a more extensive study.
O94 Methicillin-resistant Staphylococcus aureus in retail pork
J.S. Weese, R. Reid-Smith*, J. Rousseau, B. Avery (Guelph, CA)
Objectives: Community-associated MRSA is an increasing problem and an association with food animal contact has been made in some regions. This has led to concerns about the potential role of food in MRSA transmission. The objective of this study was to evaluate the prevalence of MRSA colonisation of retail pork in Canada.
Methods: Pork chops, ground pork and pork shoulders were purchased at retail outlets in four Canadian provinces in conjunction with the Canadian Integrated Program for Antimicrobial Resistance Surveillance. Both direct inoculation of meat into enrichment broth and rinsing of meat in broth were performed for pork chops and shoulders, followed by inoculation onto Chromogenic agar. Ground pork was tested only using the direct method. MRSA isolates were typed by PFGE and spa typing. Real time PCR was used to detect Panton-Valentine leukocidin genes.
Results: MRSA was isolated from 31/402 (7.7%, 95% CI 5.5–10.7%) of samples. There was a significant difference between provinces (P < 0.001) but no difference between different products, with MRSA isolated from 23/296 (7.7%) pork chops, 7/94 (7.4%) ground pork and 1/12 (8.3%) pork shoulders (P = 0.99). 21/403 (5.2%) samples were positive using direct culture while MRSA was isolated from 15/355 (4.2%) of samples testing using the rinse method. Nine samples were positive on direct culture but negative using the rinse method, while 10 others were positive only with the rinse method and only 5 were positive with both methods. Seven samples (ground pork) that were positive on direct culture were not tested using the rinse method. 3 main clones were present. The most common (40% of isolates) was a group of 3 related spa types (t064, t008 and new related type) were classified as Canadian epidemic MRSA-5 by PFGE, an ST8 human epidemic clone that has been associated with horses. PFGE-non-typable spa t034 were not surprisingly common, accounting for 30% of isolates. The 3rd main group was 3 related spa types (t002, t045 and new type) that were CMRSA-2 (USA100), an ST5 clone that is common in humans in Canada, that also accounted for 30% of isolates.
Discussion: The clinical relevance of MRSA contamination of pork is currently unclear. It is possible that contact with contaminated food could be a mode of MRSA transmission in the community, although further study of the prevalence of contamination, amount of MRSA in contaminated samples, sources of contamination and implications on human health are required.
O95 Prevalence of the novel trimethoprim resistance gene dfrK among German staphylococcal isolates of the Bft-GermVet monitoring study
K. Kadlec*, S. Schwarz (Neustadt-Mariensee, DE)
Objectives: Very recently a novel trimethoprim resistance gene, dfrK, was identified on a tet(L)-harbouring plasmid in a porcine MRSA isolate from the BfT-GermVet monitoring study. This study included in total 248 independent coagulase-positive and coagulase-variable staphylococci collected between 2004 and 2006 all over Germany: 46 isolates from infections of the urinary-genital tract of pigs, 44 isolates from skin infections of pigs, 57 isolates from respiratory tract infections of dogs/cats, and 101 isolates from infections of skin/ear/mouth of dogs/cats. In this study, we investigated the prevalence and the plasmid location of the dfrK gene among these isolates.
Methods: PCR primers were designed and a PCR with subsequent restriction analysis of the PCR product was established to detect dfrK. Isolates with positive results were tested for a plasmid location of dfrK by transfer experiments and dfrK-carrying plasmids were further analysed.
Results: The trimethoprim resistance gene dfrK was detected in another 10 isolates. All isolates were from pigs: 9 from skin infections and the remaining 1 from a urinary-genital tract infection. Six Staphylococcus hyicus subsp. hyicus isolates, 3 S. aureus isolates (2 MRSA and 1 MSSA) and 1 S. pseudintermedius. All these isolates harboured plasmids. In 7 isolates (4 S. hyicus, 2 MRSA and the single S. pseudintermedius), the plasmid location of dfrK was confirmed by protoplast transformation with subsequent susceptibility testing and PCR analysis of the transformants. In all 7 cases, the plasmids harbouring dfrK also carried a tet(L) tetracycline resistance gene. The results of a combined PCR assay with primers from tet(L) and dfrK confirmed that the dfrK gene was always located immediately downstream of the tet(L) gene. Further analysis of these dfrK- and tet(L)-harbouring plasmids showed that they varied in size between 6 and 40 kb and that similar sized plasmids differed in their EcoRV and HindIII restriction patterns.
Conclusion: The novel trimethoprim resistance gene dfrK occurred in 11 (12.2%) of the 90 porcine staphylococcal isolates from the BfT-GermVet study. In 8 (72.7%) of the 11 isolates, it was located on structurally diverse plasmids, however, always in close proximity to a tet(L) gene. The linkage of the dfrK and tet(L) genes allows the maintenance and co-selection of such plasmids under selective pressure by either tetracyclines or trimethoprim, both of which are widely used in veterinary medicine.
O96 Acquisition of cfr gene by an epidemic cluster of S. epidermidis causing bloodstream infections in hospitalised patients from Rome, Italy
R. Mendes*, L. Deshpande, T. Spanu, R. Jones, G. Fadda (North Liberty, US; Rome, IT)
Objectives: S. aureus and S. epidermidis (SE) are the most frequent species recovered from nosocomial bloodstream infections. Increasing prevalence of methicillin-resistant staphylococci has been reported. Vancomycin and linezolid are the antimicrobial options for treating infections caused by these organisms. Linezolid resistance remains rare in staphylococci; however, sporadic occurrence has been documented. Here we report the acquisition of the cfr gene by an epidemic cluster of SE in Rome, Italy.
Methods: Strains recovered as part of the SENTRY Antimicrobial Surveillance Program were tested for susceptibility by the CLSI broth microdilution method. Identification was performed by Vitek 2. Isolates displaying linezolid MIC values at ≥4 mg/L were further screened for mutations at the central loop of domain V of 23S rRNA, L4 and L22 genes followed by sequencing. The isolates were also screened for cfr gene and clonality assessed by PFGE. Gene location was performed by Southern blot and hybridisation.
Results: Ten SE recovered from blood cultures during February 06 through May 2008 met the screening criteria. Strains displayed linezolid MIC values of 4 or 8 mg/L, except for one isolate showing an MIC value of 64 mg/L (Table ). The isolates were resistant to ciprofloxacin, clindamycin, erythromycin, gentamicin but susceptible to vancomycin. Only one SE was methicillin-susceptible and two isolates were quinupristin/dalfopristin non-susceptible. All strains were clonally related and clustered into three subtypes (A, A1 and A2). cfr gene was detected in a linezolid non-susceptible strain (MIC, 64 mg/L), which was recovered from a 57 y/o male who underwent liver transplantation. Plasmid analysis identified six plasmid bands ranging from c.a. 1.5- to 154-kb in the cfr-carrying strain. Hybridisation signals were observed from the 154-kb plasmid band as well as from a chromosomal band after I-CeuI digestion. Mutations at the 23S rRNA, L4 or L22 were not detected.
| Isolate no. | PFGE | cfr | LZ | CP | CM | EM | GM | Q/D | Age | Sex | Year | ICU |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 5174 | A | Neg | 8 | >4 | >2 | >2 | >8 | 2 | 46 | F | 2006 | Y |
| 15443 | A | Neg | 8 | >4 | >2 | >2 | >8 | 1 | 60 | M | 2006 | Y |
| 12327 | A1 | Neg | 4 | >4 | >2 | >2 | >8 | 1 | 60 | F | 2007 | N |
| 12332 | A1 | Neg | 4 | >4 | >2 | >2 | >8 | 1 | 37 | F | 2007 | N |
| 12337 | A1 | Neg | 4 | >4 | >2 | >2 | >8 | 1 | 29 | M | 2007 | Y |
| 12375 | A2 | Neg | 8 | >4 | >2 | >2 | >8 | ≤0.25 | 78 | M | 2007 | Y |
| 12382 | A | Neg | 8 | >4 | >2 | >2 | >8 | 1 | 78 | F | 2007 | N |
| 12417 | A | Neg | 8 | >4 | >2 | >2 | >8 | ≤0.25 | 58 | M | 2007 | Y |
| 12421 | A1 | Neg | 4 | >4 | >2 | >2 | >8 | 0.5 | 45 | M | 2007 | Y |
| 4303 | A | Pos | 64 | >4 | >2 | >2 | >8 | >2 | 57 | M | 2008 | Y |
LZ, linezolid; CP, ciprofloxacin; CM, clindamycin; EM, erythromycin; GM, gentamicin; Q/D, quinupristin/dalfopristin; ICU, intensive care unit.
Conclusion: The cfr increased the linezolid MIC value between 8- and 16-fold. This report highlights the ability of SE to acquire linezolid resistances. The potential mobility of cfr combined with the clonal tendency for dissemination among Staphylococcus spp., represent a serious threat to several potent Gram-positive-active agents, including oxazolidinones. Active surveillance combined with effective infection control and molecular studies seem prudent to minimise the spread of these resistance mechanisms.
Reflections of infectious diseases in music
K105 Reflections of infectious diseases in music
H. Peltola* (Helsinki, FI)
The objective is to get a glimpse of the potential impact of infectious diseases on music, as regards to the composer's or performing musician's own disease, living conditions or other relevant elements which might have affected the end result, the music we enjoy today.
As music is an art of senses, full of drama, despair, realities of life – or just the opposite, blissful ignorance of those realities, full of romance, beauty, and delicacy – various forms of music was researched paying special attention to infections which potentially have played a significant role in the birth of that particular piece or performance. The entire research process was subjective, biased, and emotional, but done wholeheartedly. It aimed at to taking into account, not only the personal life of a composer or performing musician, but also the historical context in which the music was born.
Musical examples, served to the audience along with the essential background data, will show the extent to which infections have impacted music. Regarding the aetiology of those infections, bacterial, viral and parasitic agents are well represented. In addition, many epochs in history have played their role. Sometimes, the connections are surprising, even dramatic.
If listened to with a tender ear, music quite often turns out to be affected also by infectious diseases. As physicians we should realise the strength with which some people are driven by this demonic, divine – but altogether beautiful force: music.
Common problems in antibiotic abuse and solutions from around the globe
S114 Asia
A. Kamarulzaman* (Kuala Lumpur, MY)
The prevalence of antibiotic resistance has been increasing in Asian countries in recent years. This problem has most likely arisen due to a combination of inadequate infection control practices particularly in hospital settings and the widespread misuse of antibiotics in hospital and community settings.
Factors that lead to antibiotic misuse include inappropriate antibiotic prescription due to a lack of clinical, microbiological and/or imaging data in many clinical settings in the Asian region. A lack of separation of prescribing and dispensing by medical practitioners as practised in many countries in Asia as well as the easy availability of over the counter medications also contribute to antibiotic misuse.
Optimal control of antibiotic use can only be achieved through a multipronged approach that includes better education of the public and medical practitioners on rational use of antibiotic, a review of the health system structure, as well as better control of over the counter sales of antibiotics. Upgrading of microbiology and other laboratories and radiological facilities that will enhance the accuracy of clinical diagnosis is also urgently needed in most developing countries to keep pace with the complexities of managing patients in this new era to minimise the widespread practise of inappropriate antibiotic use.
Bacterial meningitis (Symposium arranged with EMESG)
S117 Old and new diagnostic tests
C. Østergaard* (Herlev, DK)
Examination of the CSF for microorganisms, WBC and differential counts, and concentrations of glucose and protein is the primary investigation to diagnose meningitis. However, this CSF examination may not always be conclusive, and it can be difficult to distinguish bacterial from viral meningitis. Therefore, improvement in diagnostic sensitivity and specificity of bacterial meningitis and development of rapid test for a bacterial aetiology are still needed. This presentation gives a review of the strength and weakness of several analyses and methods to reveal the microbiological agent (i.e. CSF microscopy and culture, antigen or antibody detection, molecular methods to detect DNA or RNA) and the use of several mediators of the host immune response for diagnostic and prognostic purposes.
S118 Management of acute bacterial meningitis
D. van de Beek* (Amsterdam, NL)
Bacterial meningitis is a medical emergency that requires a multidisciplinary approach. A diagnosis of bacterial meningitis is often considered, but the disease can be difficult to recognize. Recommendations for antimicrobial therapy are changing as a result of the emergence of antimicrobial resistance. In this lecture, current concepts of the initial approach to the treatment of adults with bacterial meningitis will be summarised. The management of the critically ill patient with bacterial meningitis poses important dilemmas. Controversial areas (i.e., prehospital admission antibiotics) will be reviewed and relevant literature will be discussed in the framework of current treatment guidelines, highlighting new developments in adjunctive dexamethasone therapy.
S119 Pathogenesis and pathophysiology: potential adjunctive therapies
U. Koedel* (Munich, DE)
Acute bacterial meningitis (ABM), especifically when caused by infection with Streptococcus pneumoniae, still has an unacceptably poor prognosis with a mortality of 10–30%.
Bacterial infection of the meninges causes one of the most powerful inflammatory reactions known in medicine. Yet 50 years ago, this inflammatory reaction was suggested to contribute substantially to brain damage. This concept underlies the use of anti-inflammatory agents as adjunctive therapy in ABM. Of all adjunctive treatments in ABM, only corticosteroids have been properly evaluated in clinical trials. These trials recommend corticosteroids in patients with Haemophilus influenzae type B and pneumococcal meningitis (PM). However, adjunctive corticosteroid therapy has several weaknesses such as a narrow treatment window and borderline effects on neurologic sequelae. Thus, there is still the need for additional or alternate adjuvants in the therapy of ABM. Experimental studies using animal models (predominantly of PM) have provided insight into the pathogenic mechanisms underlying brain injury in ABM. It is now clear that the autodestructive inflammatory reaction is initiated by the interaction of bacterial components with host pattern recognition receptors (PRR) like Toll-like receptors (TLR). PRR signaling results in the activation of transcription factors like NF-kB which up-regulate the production of proinflammatory cytokines. Cytokines like IL-1β are also potent triggers of NF-kB activation and therefore can exaggerate the inflammatory reaction (via positive feedback loops). As a consequence, great numbers of neutrophils are recruited to the meninges. Activated neutrophils release many potentially cytotoxic agents including oxidants and matrix metalloproteinases that can cause collateral damage to brain tissue. Additionally to the inflammatory response, direct bacterial cytotoxicty has been identified as a contributor to tissue damage in ABM.
Thus, experimental studies point at four different targets of adjunctive therapy, namely interference with (I) the induction of inflammation (e.g., TLR blockade), (II) the exaggeration of inflammation (e.g., IL-1 antagonism), and (III+IV) the generation of cytotoxic factors (either of host or bacterial origin, e.g., scavenging of oxidants). This presentation will give an overview of the pathophysiology of ABM (with special emphasis on PM) and highlight promising targets for adjunctive therapy in ABM, as deduced from experimental studies.
A clinician's approach to managing difficult infections
S120 Acute post-surgical prosthetic joint infection
J. Cobo* (Madrid, ES)
Optimal management of prosthetic joint infections (PJI) remains undefined. Important issues such us when the implant can be retained (conservative strategy), optimal duration of antimicrobial therapy (AT) or the role of rifampin are yet matter of controversy. In spite of a number of reports, literature appears confusing. Among the limitations of the literature we must emphasize: 1) Different criteria to classify PJI; 2) Different criteria to select for conservative strategy (CS); 3) No description of the initial population from which patients were selected for CS; 4) Very different AT (from 4 weeks to chronic suppressive therapy); 5) Low numbers of patients or short follow-up; 6) Absence of clinical trials. It is not so surprising that the rates of CS success have varied from 0 to almost 100%. The most useful classification to approach PJI was proposed by Tsukayama (1996). In his series 25 out of 35 patients with early PJI managed by a CS (debridement, exchange of polyethylen and implant retention) were cured after 4 weeks of AT. The Spanish group for the study of PJI was constituted in 2003 within the Spanish network for the study of infectious pathology (REIPI), a public funded initiative. Data from 139 consecutive cases of early PJI attended in 10 hospitals were recorded in an online database. 117 cases managed with CS could be analysed (mean follow-up of 2 years). Sixty-seven patients (57.3%) were cured after a mean of 81 days of AT. In 35 (29.9%) the infection was not controlled (or relapsed) after a mean of 84 days of AT, and the implant had to be removed. In other 15 patients (12.8%) the implant was not removed, but suppressive AT was given because of suspected ongoing infection. Results were significantly worse in one hospital. No other factors resulted statistically significant, but there was a trend of worse results for MRSA produced infections (p = 0.06). Time from the symptoms appearance to debridement was shorter in successfully treated cases (median, 7 days) than in failures (median, 10 days); p = 0.08. Good functional results were obtained in patients with successfully CS. In summary, a substantial proportion of early PJI can be managed with CS strategy and a definite (non suppressive) AT. It is difficult to identify patients at higher risk for failure, although MRSA aetiology and longer time until debridement seem to predict failures. Different outcomes in some centres suggest that surgical technique could be an important factor for failure.
S121 Pacemaker infections with multiresistant pathogens
J.L. Mainardi* (Paris, FR)
More than 3 million cardiac pacing systems are implanted worldwide and the estimated rate of infections after implantation of permanent endocardial leads is 1% to 2%, but varies between 0.1 to 20%. Pacemaker infections correspond to different clinical situations including localised infection in the device pocket, pacemaker leads to systemic infection associated with bacteraemia and lead-associated endocarditis. This latter represents 10 to 25% of all cases of pacemaker infections. The severity of pacemaker related infective endocarditis is sustained by a mortality range between 10 to 20%. Risk factors related to infections of implanted pacemakers are correlated with fever before 24 h before implantation, temporary pacing before implantation and early re-interventions (haematoma, lead dislodgment). In contrast, an inverse correlation is observed between development of infection and antibiotic prophylaxis and implantation of a new system. Data to guide therapy in patients with pacemaker infection are limited and the most appropriate management remains to be determined. According to different series, staphylococci accounted for 60 to >90% of the responsible organisms. Coagulase-negative staphylococci (CNS) are reported as predominant pathogens following by Staphylocococcus aureus. The biofilm production, responsible for bacterial survival, and the emergence of methicillin-resistant in S. aureus and CNS have complicated the management of pacemaker infections. This implies that empiric treatment of suspected pacemaker infection should coverage for staphylococci including methicillin-resistant strains. Streptococci, Corynebacterium spp, Propionibacterium acnes, Gram-negative bacilli and Candida spp can cause occasional infections. The optimal therapy combines complete device extraction (percutaneous ablation or surgical removal during extracorporeal circulation) and prolonged course of antibiotics, in particular in case of multiresistant bacteria. Leaving the device intact is associated with increased mortality and risk of relapsing or persistent infections. In absence of prospective studies, the duration of antibiotic treatment remains to be determined but 1 month has been shown not to be associated with an increased incidence of relapse. Shortest course of treatment (2 weeks) has been proposed in case of vegetations strictly localised to leads without affecting cardiac valves. Antibiotic therapy working alone should be reserved for highly selected patients.
S122 Difficult ventricular shunt infections
S. Sacar* (Denizli, TR)
Infection remains the most critical complication of ventriculoperitoneal shunt placement with an incidence of 2.2–39%. Factors as the age of patient, aetiology of hydrocephalus, the type of shunt implanted, and the surgeon's experience are determined to be associated with increased risk of infection. Children are more likely than adults to acquire shunt infection. The possible reasons are longer hospital stay, higher skin bacterial concentrations, immature immune systems, or more adherent strains of bacteria. Staphylococci, as skin commensals, are the main causative organisms. Nevertheless, in recent years a change in the epidemiology of microorganisms was observed with an increase of Gram-negative bacteria. Appropriate systemic antibiotics according to the antimicrobial susceptibility testing and surgical removal of the shunt with temporary external cerebrospinal fluid drainage and shunt replacement following the eradication of the infection are the cornerstone of the treatment of cerebrospinal fluid shunt infections. Good compliance with infection control practices, inserion of the catheter under aseptic techniques and short-term perioperative antimicrobial prophylaxis in order to prevent the emergence of drug-resistant subpopulations are important steps in the prevention of shunt infections.
Respiratory tract infection in the community
O124 Epidemiology of influenza illness requiring intensive care unit admission in Toronto, Canada
A. McGeer*, K. Green, S. Drews, I. Davis, J. Downey, K. Katz, D. Rose, A. Sarabia, A. Simor, J. Pataki, R. Fowler, S. Lapinsky, D. McRitchie, C. Simone for the ICU Influenza Working Group, Toronto Invasive Bacterial Diseases Network
Background: The epidemiology of illness requiring ICU admission in association with influenza infection in adults has not been well studied.
Methods: Population-based surveillance for laboratory confirmed influenza in adults (>15yrs) requiring ICU admission in Toronto/Peel (pop 4M) was performed from 12/04 to 5/08. Consenting patients with a positive direct test (antigen or PCR) or culture for influenza were enrolled. During the 2006/7 and 2007/8 seasons, active surveillance for influenza was conducted in 6 of 19 ICUs in the surveillance area.
Results: From 1/12/04 to 31/5/08, 161 adults with LCI requiring ICU admission were identified (1.3/100000/yr). The median age was 73 years (range 17–97 years); 85 (50%) were male. 156 (92%) had at least one chronic underlying condition qualifying them for influenza vaccine, but only 61% had been vaccinated; the median Charlson score was 1 (range 0–8); 28 (17%) were residents of long term care facilities. 123 (73%) of infections were due to influenza A, and 46 (27%) due to influenza B. Most (103 61%) had an admitting diagnosis of pneumonia; 33 (20%) had another cardio-respiratory diagnosis. Fifteen (9%) had a concomitant bacteraemia (8 S. aureus, 4 S. pneumoniae, 2 E. coli, 1 GAS). 151 (90%) of patients received antibacterials at admission; 68 (40%) were treated with antivirals (all with oseltamivir). Forty-two patients (25%) died within 15 days of the onset of symptoms; these included 8/68 (12%) patients treated with oseltamivir and 34/100 (34%) other patients (P = 0.002). In multivariable analysis, only APACHEII score and failure to treat with oseltamivir therapy predicted mortality (odds ratio for death with oseltamivir treatment = 0.27, 95%CL 0.12–0.64, P = 0.001).
Conclusions: Influenza is an important cause of respiratory illness requiring ICU admission during the winter season, particularly in unvaccinated, at-risk adults. S. aureus is the most common complicating bacterial infection. Treatment with oseltamivir was associated with a significant reduction in mortality.
O125 Influenza in adults admitted to Canadian hospitals: data from two seasons
A. McGeer, D. Gravel, G. Taylor*, C. Weir, C. Frenette, J. Vayalumkal, A. Wong, D. Moore, S. Michaud, B. Amihod (Toronto, Ottawa, Edmonton, Montreal, Saskatoon, Sherbrooke, CA)
Objective: Seasonal influenza (flu) remains a cause of substantial morbidity and mortality. Antiviral treatment should be considered for all hospitalised patients with influenza. To better understand the epidemiology and burden of illness within the hospital sector in Canada and the current use of antiviral therapy, we carried out a multihospital survey of virologically confirmed flu in hospitalised adults.
Methods: CNISP is a network of largely teaching hospitals across Canada that collaborates to collect data on infections in hospitalised patients. During two consecutive years (2006/2007 and 2007/2008) hospitals within CNISP identified inpatients >16 years who had virologically confirmed flu. Case patient charts were reviewed to capture demographic and clinical data and to determine whether flu was community (CA) or hospital acquired (HA). Cases were reviewed at 30 days to determine outcomes. Deaths at 30 days were reviewed to determine whether flu was a main or contributing cause.
Results: Fifteen (06/07) and 11 (07/08) hospitals were recruited from the CNISP network. 532 virologically confirmed cases of flu were found, 182 in 06/07 (95% flu A) and 358 in 07/08 (56% flu A). Mean patient age was 67 years, 52% were male. There was documentation of patient vaccination that season in 29%. Incidence of CA flu was 11/10,000 admissions in 06/07 (range by hospital 2 – 23) and 27 in 07/08 (1 – 47). Admitting diagnoses in CA cases were: pneumonia or influenza 48%, exacerbation of COPD 20%, sepsis or fever not otherwise specified 9%, cardiac diagnoses 7%, other diagnoses 16%. 24% of cases were HA, range by hospital 3.9 – 5.4/100,000 patient days. 68% of patients were managed with droplet and contact isolation practices, an N-95 mask was used in 19%. 29% of CA cases but 75% of HA cases received antiviral therapy p < 0.01, almost entirely oseltamivir. 9% of cases were admitted to an ICU; 30-day mortality was 8% with 2.6% attributed to influenza.
Conclusion: There is considerable season-season and hospital-hospital variation in flu in patients in Canadian hospitals. Hospitalised patients CA flu present with a wide spectrum of clinical diagnoses; nearly a quarter of all cases were HA. Few CA cases but most HA cases were treated with antiviral drugs. Attributable 30 day mortality was 2.6%.
O126 Influenza vaccination coverage among Greek adults
V. Papastamopoulos, E. Kakalou*, T. Panagiotopoulos, J. Baraboutis, M. Samarkos, A. Skoutelis (Athens, GR)
Objectives: Our study sought to describe influenza vaccination coverage among adults in Greece for the season 2007/08.
Methods: We conducted a random-sampling, telephone based household survey among adult individuals in Greece. For this purpose a sample of 1104 adults representative of the basic demographic, social and geographical characteristics of the overall Greek population according to the latest national survey, was used. Two target groups were determined for analysis: persons >65 years of age and persons with chronic conditions such as respiratory and heart conditions (other than hypertension), diabetes mellitus and other conditions.
Results: The influenza vaccination rate for the season 2007/08 among the adult population in Greece was: 16% for the overall adult population (19.5% for men, 12.7% for women), 48.1% for people >65 years of age, 31% for persons with chronic illness (32.5% for persons with respiratory illness, 50.2 for persons with heart conditions, 35% for persons with diabetes mellitus). A high rate of 81% of the overall population reaching 88% among persons with chronic conditions report having had any type of contact with the National Health System or a private physician within the last three years. Among them only 20.1% had been recommended to get vaccinated. Among the ones recommended any vaccination, 80.5% of persons with respiratory illness, 100% of persons with diabetes mellitus and 89.1% of persons with heart conditions had been recommended to get the influenza vaccine.
Conclusions: Available data show unacceptably low levels of influenza vaccination coverage among vulnerable groups such as the population over 65 years of age and people living with chronic illness. Influenza vaccination is the only preventive measure reducing influenza morbidity and mortality and its use has proven cost-effective among high risk groups. It is also the main vaccine recommended by physicians. However the overall rate of physicians recommendation of vaccination is very low. Dynamic efforts are thus needed to design and implement strategies and policies that have demonstrated their rigorous effectiveness in enhancing influenza vaccination coverage rates.
O127 The role of respiratory viruses and M. pneumoniae in lower respiratory tract infections in primary care
M. Ieven*, K. Loens, F. Coenjaerts, C. Lammens, A. Vanderstraeten, T. Verheij, P. Little, H. Goossens, E.C.J. Claas, A.M. Van Loon on behalf of the GRACE Study Team
Objectives: The role of viruses and especially of the newly recognised viruses is not well known in adult respiratory infections in the community. We therefore investigated the viral aetiology and the role of M. pneumoniae in lower respiratory tract infections (LRTI) at the GPs office in the European GRACE primary care network (PCN) using sensitive real-time nucleic acid amplification tests (NAATs).
Materials and Methods: From October 2007 through May 2008, a total of 711 adult patients with LRTI in the community were enrolled during the first winter period in a prospective study in 11 PCNs in 8 European countries. Among other samples, nasopharyngeal flocked swabs (COPAN) were collected and sent to the local laboratory to be frozen. Specimens were transported regularly to the central lab in Antwerp for subsequent nucleic acid extraction by the NucliSens EasyMAG (bioMérieux) and in-house real-time PCR for M. pneumoniae detection. Aliquots of nucleic acid extracts were sent to the collaborating LUMC and UMC-UTRECHT for detection of influenzavirus (INF) A/B, parainfluenzavirus (PIV)1–4, human rhinoviruses (HRV), human metapneumovirus (hMPV), respiratory syncytial virus (RSV), adenovirus (ADE), Bocavirus (BOCA), coronaviruses (COR) OC43, NL-63, 229E, polyomaviruses KI and WU by in-house mono and multiplex real-time PCR.
Results: In 618/711 (86.9%) of the patients, a nasopharyngeal specimen could be collected. In 302 (48.9%) patients a respiratory virus was detected. A total of 322 respiratory viruses were detected in 618 specimens: 114 HRV (18.5%), 78 INF (12.6%), 41 CoV (6.6%), 28 hMPV (4.5%), 23 RSV (3.7%), 19 polyomaviruses (3.1%), 12 PIV (1.9%), 4 ADE (0.7), 3 BOCA (0.5%). The new polyomaviruses WU and KI were detected in 13 and 6 specimens, respectively. M. pneumoniae was not detected. 19 viral double infections (3.1%) were detected: in 10/19 double infections a human polyomavirus was involved, and in 8/19 cases a co-infection of HRV with another virus was found.
Conclusions: Nasopharyngeal sampling with flocked swabs is well tolerated and suitable to be used in an outpatient setting. Implementation of real-time mono and multiplex NAATs results in a significant improvement of the rate in diagnosing LRTI. HRV account for the majority of viral LRTI in primary care followed by influenza and coronaviruses but also RSV and hMPV are prevalent in an adult population. In this study, 19 polyomaviruses were detected of which 10 were involved in a double infection.
O128 PVL-SA as a cause of CAP in England: A review of cases during 2008
A.M. Kearns*, M. Ganner, C. Perry, B.D. Cookson, M.J. Ellington (London, UK)
Objectives: The association of Panton-Valentine Leukocidin-positive Staphylococcus aureus (PVL-SA) with severe necrotising Community-Acquired Pneumonia (CAP) is well recognised, with mortality rates of up to 75% reported. Through the implementation of an initiative to enhance the ascertainment for disease associated with PVL-SA nationally, we sought to identify and characterise cases of CAP occurring in England during 2008.
Methods: Isolates of S. aureus referred to the National Staphylococcus Reference Unit from patients with suspected CAP were tested for the PVL genes by PCR. All PVL-positive isolates were characterised genotypically, including screening for additional toxin genes and mecA. All MRSAs were also subjected to Pulsed-Field Gel Electrophoresis to assist with assigning lineage. Patient demographic and clinical data were sought in all microbiologically confirmed cases.
Results: During 2008, 33 cases of CAP due to PVL-SA were identified in England. Cases were sporadic in occurrence, and were geographically and temporally dispersed. Patients were previously healthy; ages ranged from 0 to 82 years (median 24 y); 17 (51.5%) were female. All infections were community-acquired and most patients (24; 72.7%) required admission to ICU. Twelve (36.4%) cases were fatal, half of these died within 48 hours of admission to hospital. Airway bleeding and raised CRP levels were common features; WCCs were variable (range 0.5 to 28); Influenza A or B was confirmed in 7 individuals. The majority of PVL-SA (27; 81.8%) were susceptible to oxacillin, and multiple lineages were identified (including clonal complexes 1, 8, 22, 25, 30, 80 and 121).
Conclusion: The propensity of PVL-SA to cause life-threatening disease in young, previously healthy individuals is a public health concern. Based on our experience, the mortality rate of PVL-related CAP (36.4%) was lower than previously published data. The majority of infections were caused by PVL-MSSA, no single lineage of S. aureus predominated. To inform algorithms for prompt recognition and diagnosis of suspected cases, and therapeutic strategies to improve patient outcomes, continued vigilance is required at an international level.
O129 Biomarkers improve the ability of clinical scores to predict intensive care unit admission in patients with community-acquired pneumonia
W.C. Albrich*, P. Schuetz, M. Batschwaroff, M. Christ-Crain, W. Zimmerli, H.C. Bucher, B. Müller (Aarau, Basel, Liestal, CH)
Objectives: A clinical prediction tool (SMART-COP), based on eight clinical, laboratory and radiologic parameters, compared favourably with the PSI and CURB65 scores to predict intensive respiratory and vasopressor support in patients with community-acquired pneumonia (CAP) (Charles et al. Clin Inf Dis 2008;47:375–84). We compared the diagnostic accuracy to predict Intensive Care Unit (ICU) requirements in CAP between clinical scores and biomarkers.
Methods: In patients with CAP enrolled in the Swiss multicentre Pro-HOSP study, receiver operating characteristic curves (ROC) to predict ICU admission were compared between the clinical scores SMART-COP, PSI and CURB65 and the biomarkers Pro-Adrenomedullin (Pro-ADM) and Endothelin-1 precursor peptides (Pro-ET1).
Results: In preliminary analysis, a SMART-COP score of ≥3 was present in 30 of 83 (36.2%) patients requiring ICU admission compared with only 64 of 842 (7.6%) without ICU admission (p ≤ 0.0001). The ROC values of ICU admission were highest for SMART-COP score (0.75, 95% CI: 0.69–0.81), Pro-ET1 (0.73, 95% CI: 0.68–0.79) and Pro-ADM (0.72, 95% CI: 0.66–0.77), and lower for PSI score (0.68, 95% CI: 0.63–0.73) and CURB65 score (0.64, 95% CI: 0.58–0.70). Combining Pro-ET1 and the SMART-COP score (AUC = 0.80, 95% CI: 0.75–0.85) in a combined logistic model significantly improved the diagnostic accuracy for ICU admission over each individual predictor (p < 0.01, for each comparison). To predict the outcome of death (n T50) and ICU admission or both (n T118), the combination of Pro-ADM and the SMART-COP score was significantly better (AUC = 0.80; p < 0.05 for each comparison) than any predictor individually (AUC: Pro-ADM 0.72, SMART-COP 0.73, PSI 0.73, CURB65 0.68, Pro-ET1 0.73).
Conclusion: As biomarkers Pro-ADM and Pro-ET1 are prognostic markers for a severe course of CAP, combining biomarkers and clinical severity assessment tools might become useful measures for more appropriately triaging CAP patients in an era of limited healthcare resources. This hypothesis has to be tested in intervention studies.
O130 Pneumococcal pneumonia presenting with septic shock: characteristics, outcomes, serotypes and genotypes
C. Garcia-Vidal*, C. Ardanuy, F. Tubau, D. Viasus, J. Liñares, F. Gudiol, J. Carratalà and CIBER de Enfermedades Infecciosas
Objectives: We aimed to ascertain the characteristics, outcomes, serotypes and genotypes of pneumococcal pneumonia (PP) presenting with septic shock.
Methods: Observational analysis of a prospective cohort of 1041 nonseverely immunosuppressed adults with PP requiring hospitalisation (1995–2008). Of them, 556 were diagnosed by urinary antigen and/or 650 were diagnosed by culture. Overall, 86% of pneumococcal strains were available for serotyping (Quellung) and 58% for PFGE (Smal) and or MLST. The diagnosis of septic shock was based on a systolic blood pressure <90 mmHg and peripheral hypoperfusion with clinical or bacteriologic evidence of uncontrolled infection.
Results: A total of 114 (11%) patients with PP had septic shock at presentation. Patients with shock were younger (61 vs 66 yrs; p = 0.003), were more frequently current smokers (45% vs 28%; p = 0.002), had received more commonly corticosteroid therapy (13% vs 6%; p = 0.015), and were more frequently classified into high-risk PSI classes (81% vs 60%; p < 0.001) than those who did not have this complication. They were also less likely to have received prior influenza vaccine (31% vs 48%; p = 0.007) and had more frequently bacteraemia (41% vs 30%; p = 0.014). No significant differences were found in rates of penicillin-(2% vs 2%) and erythromycin-resistance (16% vs 12%). Serotype 3 was more commonly associated with shock (40% vs 24%; p = 0.007), whereas serotype 1 was rarely associated with this complication (2% vs 9%; p = 0.041). No significant differences were found regarding genotypes: ST2603 (26% vs 16%), Netherlands-ser8-ST53 (10% vs 3%), Netherlands-ser3-ST180 (10% vs 8%), Spain-ser9V-ST156 (10% vs 12%). Patients with shock required more frequently mechanical ventilation (38% vs 4%; p < 0.001), and had longer LOS (19 vs 10 days; p < 0.001). Early (10% vs 1%; p < 0.001) and overall case-fatality rates (25% vs 5%; p < 0.001) were higher in patients with shock.
Conclusions: PP presenting with septic shock is still associated with a poor outcome. It occurs mainly in current smokers, patients receiving corticosteroids, and in those infections caused by serotype 3. Prior influenza vaccination and PP caused by serotype 1 are associated with a lower risk of shock.
O131 High long-term mortality rate after initial recovery from severe community-acquired pneumonia
A. Bruns, J.J. Oosterheert*, M. Cucciolillo, A. Hoepelman on behalf of the SAT-P Study Group
Background: Despite the presence of antibiotics and vaccination strategies against pneumocci, community-acquired pneumonia (CAP) is still a major cause for mortality in developed countries. However, it is unclear how an episode of CAP influences long-term survival after initial recovery. Therefore, we determined mortality up to 5 years after discharge in patients hospitalised because of an episode of severe CAP in a non-intensive care setting.
Methods: In 5 hospitals in the Netherlands, patients (pts) with severe CAP (PSI class IV and V without need for treatment in ICU) were prospectively followed for 28 days and mortality up to 5 years after discharge was determined using the Dutch Municipal Public Records Database. We used Cox regression analysis to examine predictors for mortality.
Results: 276 patients were included. 246/276 (89%) pts survived to hospital discharge. Of those, 7 (3%) pts died in the first month after hospitalisation. Cumulative 1, 2, 3, 4 and 5-year mortality rates were (n = 56) 23%, (n = 83) 34%, (n = 104) 43%, (n = 117) 48% and (n = 138) 56% respectively.
In a Cox model, pleural fluid on chest X-ray on admission was a strong predictor for mortality in the first month after discharge (Hazard ratio (HR) 12.6, 95%CI 2.45–65.00). Increasing age, (HR 1.04, 95%CI 1.02–1.05), arterial pH <7.35 on admission (HR 1.64, 95%CI 1.02–2.64), co-morbid malignancy (HR 1.78, 95%CI 1.24–2.56) and liver disease (HR 4.46, 95%CI 1.38–14.40) were associated with increased 5-year mortality.
Conclusions: After initial recovery from an episode of severe CAP, 5-year mortality rate is almost 60%. Factors associated with 5 year mortality are mostly co-morbidity related and not pneumonia related. Therefore, vaccination strategies are unlikely to increase long-time survival in patients after an episode of severe CAP.
O132 Direct costs in adults with community-acquired pneumonia in emergency clinical hospital
S. Ratchina*, E. Shal, I. Ustuzhanin, O. Asafjeva, Y. Vandenzhan (Smolensk, RU)
Objectives: Community-acquired pneumonia (CAP) is a widespread disease associated with a large economic burden, mostly due to inpatient treatment. Identification of determinants of health care costs could help define strategies for efficient use of existing resources. This study was conducted to identify the direct hospitalisation costs of treating adult patients with CAP in an emergency clinical hospital of RF.
Methods: A prospective observational study was performed in patients admitted to a hospital ward between July 2006 and December 2007 with confirmed diagnosis of CAP. Direct medical costs (year 2007 values, calculated in Russian rubles and converted to Euros) of infection-related hospital resources, including hotel cost, laboratory tests, diagnostic procedures, treatment (antibacterial therapy, adjunctive medical treatment and nondrug therapy) were analyzed.
Results: A total of 127 patients aged from 16 to 87 years (mean age 51.3±17.7 years), 91/127 (71.7%) males, were enrolled. Complications were diagnosed in 88/127 (69%) and concomitant diseases in 105/127 (83%) of patients; 46/127 (36.2%) received antibacterial treatment before admission. Severe CAP was diagnosed in 26/127 (20.5%) of cases; in total 3/127 patients died. Mean ±SD length of hospital stay was 13.4 ± 4.1 days. The median (interquartile range) total hospital cost was €273 (€224–317); the distribution of each component was as follows: hotel cost €107 (€92–122); laboratory tests €40 (€34–52), diagnostic procedures €36 (€23–50), antibacterial therapy €56 (€32–90), non-antibacterial medical treatment €11 (€6–20), non-drug therapy €2 (€0–6).
Conclusion: Major determinants of direct costs in hospitalised adults with CAP were hotel cost due to prolonged hospital stay and antibacterial therapy. They should be considered as key components for further analysis and intervention programs.
O133 Anti-pneumococcal polysaccharide antibody profiles during community-acquired pneumonia
G. T. Rijkers*, E. van Hannen, S. Meijvis, D. van Kessel, H. Endeman, D.H. Biesma, J.C. Grutters, B.J. Vlaminckx, H. van Velzen-Blad (Nieuwegein, Utrecht, NL)
Objectives: Streptococcus pneumoniae and Haemophilus influenzae are the main causative micro-organisms of community acquired pneumonia (CAP). We were interested to find out whether natural exposure to S. pneumoniae would lead to a systemic, serotype-specific antibody response. As a secondary aim we studied whether changes in pneumococcal antibody levels could be used as an additional diagnostic tool for CAP patients in which the causative micro-organism could not be identified.
Methods: In the St. Antonius Hospital, Nieuwegein, the Netherlands, we have conducted a prospective study in which 200 consecutive patients above 18 years of age with CAP hospitalised in the period October 2004–August 2006 were included. Plasma samples were obtained at day 1 (= day of admission), day 2, 3, 5, 10 and 30 and stored at −80°C. In 60 patients, S. pneumoniae was identified as causative micro-organism, H. influenzae in 7%. In 28% of patients other micro-organisms were identified and in 36% the cause of CAP remained unknown. As control populations for the S. pneumoniae CAP patients, age and Fine-score matched patients with CAP from the same cohort but with another micro-organism as causative agent or with an unknown cause were used. A number of patients with an S. pneumoniae CAP was, after recovering from the disease, vaccinated with the 23-valent pneumococcal polysaccharide vaccine. Antibodies were also be determined in the post-vaccination samples. Pneumococcal antibodies against serotypes 1, 3, 4, 6B, 7F, 8, 9N, 9V, 12F, 14, 18C, 19A, 19F, and 23F were determined with the XMAP Pneumococcal Immunity Panel (Luminex Inc. Austin TX USA).
Results: Preliminary data indicate that in most but not all patients with pneumococcal CAP, serum IgG antibodies to the causative pneumococcal serotype increase between 10 to 30 days after onset of disease. Antibody levels to other serotypes do not change during the course of CAP. Conclusions: Multiplex serotype-specific antibody determination can monitor (the kinetics of) the antibody response to causative pneumococci in CAP.
Infection control: burden and interventions
O134 Cost-effectiveness analysis of universal rapid screening for methicillin-resistant Staphylococcus aureus at hospital admission
A. Murthy*, G. De Angelis, D. Pittet, J. Schrenzel, S. Harbarth (Geneva, CH)
Objective: Policy-makers have called for universal screening on admission to reduce nosocomial MRSA infection. Risk-profiling tools and rapid PCR tests are now available and have been evaluated in controlled trials. However, data on the cost-effectiveness of rapid MRSA screening is limited. This study aimed to assess the cost-effectiveness of such screening.
Methods: A decision analytic Markov model from the hospital perspective compared costs and effects of 3 control strategies: (1) rapid PCR screening; (2) screening for risk-factors (hospitalisation or antibiotics within past year) plus pre-emptive isolation & contact precautions pending chromogenic agar screening results; (3) no screening. Data, taken from clinical trials at a Swiss teaching hospital and published literature, included test turn-around-time & performance, MRSA cross-transmission, isolation & contact precaution efficacy, and prevalence of colonisation on admission. Costs, derived from hospital accounting systems, included tests, laboratory & staff time, surgical bed-days, contact precautions, decolonisation and MRSA infection.
Results: Compared to strategy 2, strategy 1 resulted in slightly higher costs (CHF 8,748 vs. 8,981) but fewer infections (.008 vs. 0.006) during patients' mean length-of-stay, producing an incremental cost-effectiveness ratio (ICER) of CHF 83,303 per MRSA infection avoided. Strategy 3 was dominated by strategies 1 and 2 (both more costly and less effective). Sensitivity analyses suggest that prevalence of colonisation on admission is a stronger predictor of cost-effectiveness than the costs of infection or rapid screening, the probability of cross-transmission, or the incremental costs of isolation and contact precautions. Increasing the relatively low on-admission prevalence at our centre by 20% lowers the ICER to CHF 60,973 per infection avoided. In contrast, increasing the cost of each infection, the cost of rapid screening, or the risk of cross-transmission by 20% only marginally affects the ICER.
Conclusion: This analysis suggests that compared to risk factor identification and pre-emptive isolation, universal rapid screening upon surgical admission is not strongly cost-effective at our centre. However, local epidemiology plays an important role. In particular, settings with higher prevalence of colonisation on admission may find universal rapid screening more cost-effective. Of note, no screening is undesirable, as costs and infections would be higher.
O135 Model-based assessment of the effectiveness and cost-effectiveness of methicillin-resistant Staphylococcus aureus infection control programmes in the intensive care unit
J. Robotham*, A. Barnett, N. Graves, B. Cookson, J. Wilson, B. Cooper (London, UK; Brisbane, AU)
Objectives: To provide model-based assessments of the effectiveness and cost-effectiveness of methicillin-resistant Staphylococcus aureus (MRSA) infection control programmes in intensive care units (ICUs), with a particular emphasis on comparing currently available screening technologies.
Methods: Screening technologies evaluated included conventional culture, chromogenic agar and polymerase chain reaction (PCR) based systems. Estimates of sensitivity, specificity and turnaround time were obtained from the literature. A dynamic stochastic individual-based model of MRSA transmission in the ICU was developed to enable the comparison of different policies. Model calibration was performed by synthesizing evidence from multiple sources including longitudinal MRSA surveillance data, published literature and formally elicited expert opinion. The model was then used to assess changes in health benefits and resource use associated with different policies.
Results: Admission and weekly screening coupled with patient isolation was found to dramatically reduce the number of MRSA acquisitions. The largest reductions were obtained with PCR technology, followed by chromogenic agar. The differences, however, were surprisingly small, and all screening technologies achieved reductions in MRSA acquisition of close to 80% compared with the no-intervention scenario. Nonetheless, chromogenic and PCR-based systems were able to decrease the number of unisolated MRSA-bed-days by approximately 15 and 35% respectively.
Conclusions: The small differences in the ability of the screening technologies to reduce MRSA acquisition reflect both a relatively low estimated isolation efficacy and the observed highly skewed distribution of ICU-stays, and may provide some important insights into the reasons for recent disappointing trial results. In particular, the skewed length of stay distribution means that most MRSA-bed days are accounted for by relatively long-stay patients for whom rapid detection will make the least difference. Key sources of uncertainty were found to be isolation effectiveness and attributable mortality due to MRSA infections, both of which are difficult to accurately estimate with currently available data. The model results allow us to quantify the expected value of reducing these key uncertainties, and help to provide a rational basis for setting future research priorities.
O136 Infection control practices associated with methicillin-resistant Staphylococcus aureus rates of 116 German hospitals
I.F. Chaberny*, F. Schwab, A. Cohrs, M. Behnke, P. Gastmeier (Hanover, Berlin, DE)
Background: The German guideline for MRSA infection control was published in 1999. Despite these recommendations a continuous increase of MRSA could be observed in hospitals.
Objectives: To test the hypothesis whether the recommendations were not adequately implemented or whether they were insufficient to prevent MRSA spread.
Methods: This study analyzed MRSA prevention measures in MRSA KISS hospitals by the use of a questionnaire. Then, a validation study was performed by local side visits. The prevention measures and structure parameters were associated with the MRSA incidence densities in a multiple logistic regression analysis.
Results: In 2007, a questionnaire was sent via internet to 145 MRSA KISS hospitals. 134 completed forms were retrieved and analyzed. A random sample of 35 hospitals was created for validation. After visiting and validating these hospitals, the data of 116 hospitals were used for further analysis. Hospitals with the main focus on transplant medicine (OR 8.1; CI95 1.8–36.1; p = 0.006) and hospitals, which have implemented an admission MRSA screening in at least one ICU in addition to standard screening (known MRSA patients and roommates), (OR 2.9; CI95 1.17–7.4; p = 0.031) were associated with the highest incidence of MRSA case-patients per 1,000 patient days. The hospitals with transplant medicine (OR 8.0; CI95 1.7–38.4; p = 0.01) and the hospitals with an admission screening on at least one ICU (OR 4.8; CI95 1.7–12.9; p = 0.002) showed a high incidence of nosocomial MRSA case-patients per 1,000 patient days (>75th percentile); a decolonisation procedure with mupirocin nasal ointment and antiseptic body wash was protective (OR 0.3; CI95 0.1–0.9; p = 0.023).
Conclusion: This study highlighted significant associations between MRSA incidence densities and various prevention measures. However, due to the uncertain cause-effect relation between screening frequencies and infection rates it remains difficult to evaluate the real influence of intensified screening activities. The results of this study confirm decolonisation procedures as a protective factor.
O137 Methicillin-resistant Staphylococcus aureus in nursing homes: can an improvement in infection control practices decrease MRSA prevalence?
N. Baldwin, D. Gilpin*, C. Hughes, P. Kearney, C. Cardwell, M. Tunney (Belfast, Antrim, UK)
Objectives: We have shown that there is substantial colonisation of MRSA among nursing home residents and staff with our recently conducted point prevalence study in 45 nursing homes which revealed an overall prevalence rate of 24% in residents and 7.6% in staff.1 The aim of this study was, therefore, to test the effectiveness of an intervention in nursing homes which sought to improve standards of infection control as a means of reducing MRSA prevalence.
Methods: A cluster randomised controlled trial (cRCT) involving 32 nursing homes, with each home representing the unit of analysis, was performed. The study ran for 12 months with data collected at baseline, 3, 6 and 12 months. Nasal swabs were taken at baseline from consenting residents and staff in all homes prior to randomisation with an audit of infection control procedures also undertaken. Following collection of these baseline data, nursing homes were allocated to the intervention or control arm (1:1). Intervention home staff were trained in infection control, specifically hand hygiene, catheter care, barrier approaches such as use of gloves, aprons and masks, and decontamination of equipment and the environment with usual practice continuing in control homes. After each data collection timepoint, feedback was given to the intervention homes in terms of their performance and further education and training provided as required. The primary outcome was the prevalence of MRSA in intervention homes compared to control sites.
Results: Preliminary analysis of the data has revealed no significant change in the prevalence of MRSA in the intervention and control homes, taking account of the clustering, over the one-year intervention period [risk ratio 0.83; 95% confidence intervals (CI) 0.53–1.29]. However, there was an improvement in infection control audit scores in the intervention homes, with a mean score in control homes at 12 months of 64.4% compared with 81.7% in the intervention sites; these scores were significantly different (paired t-test, p < 0.0001).
Conclusions: The results suggest that infection control education and training as implemented in this study was not sufficient to affect MRSA prevalence. Therefore, a more detailed education and training package either alone or in combination with MRSA decolonisation of staff and residents, may be required to reduce MRSA prevalence within this unique environment.
O138 Psychological impact of short-term isolation for infection control
M. Wassenberg*, D. Severs, M. Bonten (Utrecht, NL)
Objectives: In a response to the rapid global increase in the nosocomial prevalence of multi-resistant micro-organisms, infection control measures, such as patient isolation, are increasingly used. It is unknown how these measures influence the quality of life (QOL) of patients during short-term isolation, and this was determined in a prospective matched cohort study.
Methods: All adult patients needing isolation in a single-patient room between 11/06 and 03/07 in the UMC Utrecht were eligible and included 24–48 hours after start of isolation (after giving informed consent and being able to fulfil study requirements). For each index patient we identified two control patients, admitted to the same wards at the same time, yet not subjected to any isolation measure. Anxiety and depression and QOL were assessed using the Hospital Anxiety and Depression Scale (HADS) and Visual Analogue Scale (EQ-5D-VAS) in all patients. Opinions on and experiences with isolation were measured in isolated patients by means of a self-developed ‘isolation evaluation questionnaire’.
Results: 42 isolated patients and 84 controls were included, with comparable baseline characteristics (age, sex, nationality, level of education, length of hospital stay and severity of underlying disease and co-morbidity (using the Cumulative Illness Rating Scale)). Reasons for isolation were clostridium difficile-associated disease (n = 17, 40%), high risk for MRSA carriage (n = 12, 29%), or resistant Gram-negative bacteria (n = 7, 17%). Mean scores of questionnaires are presented in table 1 . isIn univariate analysis only duration of isolation of 48 hours (compared to 24 hours) was associated with a reduced quality of life (VAS 57.7 compared to 68.7, p 0.02). On a visual analogue score of opposite terms isolation measures were rated with means of 87.5, 83.3 and 70.8 for safety, usefulness and quietness, respectively.
| HADS-A | HADS-D | HADS-total | VAS | |
|---|---|---|---|---|
| Index patients (n = 42), mean (SD) | 4.7 (3.5) | 5.3 (3.5) | 9.9 (6.0) | 62.3 (15.5) |
| Control patients (n = 84), mean (SD) | 5.4 (3.7) | 5.2 (3.6) | 10.6 (6.5) | 63.0 (15.3) |
| p-value | 0.61 | 0 90 | 0.31 | 0.64 |
Conclusion: Short-term isolation (up to 48 hours) is not associated with anxiousness or depression, but with positive feelings about safety, usefulness and quietness.
O139 The burden of healthcare-associated infection: the patient experience
E. Burnett*, K. Lee, R. Rushmer, M. Ellis, M. Noble, P. Davey (Dundee, UK)
Objectives: There is a lack of data about the impact of Healthcare Associated Infection (HAI) on the experience of individual patients. This information is essential to empower health organisations to understand, prioritise, develop and implement solutions that will minimise risks to patients. This study explored comparable narratives from patients who had experienced a Staphylococcus aureus blood stream infection with patients who had not.
Methods: We conducted qualitative semi-structured interviews with eighteen adults who had previously been an in-patient in an acute teaching hospital in Scotland. Nine patients had had a laboratory diagnosed Staphylococcus aureus blood stream infection and nine had no blood stream infection. All patients were interviewed for 20–40 minutes. The interviewer asked patients about their thoughts around HAI, what concerns they had or still do, what measures they took to safeguard themselves from HAI and how their experience impacted on their confidence of the NHS. Probing questions were then asked depending on the responses given to the initial questions. All interviews were recorded, transcribed and analysed thematically.
Results: Analysis of transcribed interviews is ongoing. Preliminary analysis showed that all patients had positive and negative comments about infection prevention and control practice in the hospital. Specific concerns included poor communication, poor cleanliness, awareness of patient boarding, lack of facilities, staff shortages and multi-tasking. Some patients who had experienced bacteraemia said they had not been informed about the infection. Those who had been informed were not given clear information about treatment or subsequent results. Most patients were not specifically told what they or their family should do to safeguard them from infection and little or no written information about HAI was provided. Most patients are worried about HAI on future admissions.
Conclusions: The concerns of patients were not fundamentally different if they did or did not experience blood stream infection. The patient's reported experiences show that they have a broad awareness of systems issues that may increase risk of infection. Consequently we need to involve patients in the design and evaluation of systems change and information that will improve patient experience. Improving the safety and reliability of the system will have direct benefits for all patients in the hospital, not just the ones at risk of HAI.
O140 The success and effectiveness of the world's first national cleanyourhands campaign in England and Wales 2004–2008: a prospective observational interrupted time-series
S. Stone*, C. Fuller, R. Slade, J. Savage, A. Charlett, B. Cookson, B. Cooper, G. Duckworth, M. Murray, A. Hayward, A. Jeanes, J. Roberts, L. Teare, J. McAteer, S. Michie (London, UK)
Objectives: The world's first national hand hygiene (HH) campaign (cleanyourhands CYHC) targeting healthcare workers (HCW) was rolled out in Jan-Jun 2005 to all acute hospitals in England & Wales. It comprised: bedside availability of alcohol handrub (AHR); ward posters endorsing HH; materials helping patients to ask HCWs to perform HH; audit & feedback of HH compliance. An independent 4 year study assessed its implementation, sustainability, & effects on HH and Healthcare associated infection (HCAI).
Methods: CYHC implementation was assessed by 6-monthly questionnaires to 187 acute hospitals. Monthly procurement data for soap and AHR acted as a proxy for HH compliance. National mandatory quarterly HCAI data [meticillin resistant & sensitive S. aureus bacteraemia (MRSAB & MSSAB) & C. difficile infection] & bed occupancy were collected for each hospital & data on potentially confounding national interventions (Saving Lives, Department of Health Improvement Team Visits & MRSA screening). Analyses: Generalised estimating equation (population-averaged) models with an exchangeable within-group correlation structure.
Results: 82% of all hospitals responded to the last questionnaire (June 2008). Even after 3 years, CYHC was still a top priority in 92% of hospitals, with bedside AHR in most wards in 94%. Posters were displayed in most wards by 96% of hospitals, with Audit & Feedback in most wards in 86%. Patient Empowerment materials were less successful. Procurement of AHR, but not soap, rose significantly during CYHC roll out, plateaued for a year, before rising continuously & significantly, as did soap, from mid 2006 (Figure ). Combined soap & AHR procurement tripled over the study period.
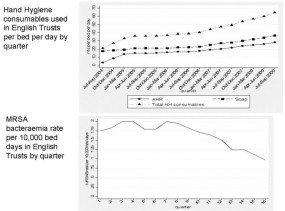
MRSAB rates halved (Figure) but no other HCAI fell. From July 2006-Dec 2007, each extra ml of AHR per patient-bed-day was significantly associated (p < 0.0001) with a 1% fall in MRSAB but this association did not continue in Jan-Jun 2008. Specialist & Teaching Hospitals (p < 0.001) & Improvement team visits (p = 0.004) were strongly associated with MRSAB rates.
Conclusions: The CYHC is associated with a sustained change in HH behaviour in acute hospitals nationally, with a three-fold rise in procurement/use of AHR & soap. There appears to be a strong association between reduction in MRSAB & use of AHR. This may reflect interactions between improvement team visits or other confounders & CYHC. The campaign should be continued & is a model that other countries could adopt/adapt.
O141 Effect of peri-operative mupirocin and chlorhexidine on mortality in nasal carriers of Staphylococcus aureus
M.M.L. van Rijen*, L.G.M. Bode, M.C. Vos, J.A.J.W. Kluytmans for the STEP Study Group
Objectives: A multicentre double-blind randomised-controlled trial (M-RCT), carried out in the Netherlands between October 2005 and June 2007, showed that hospitalised patients with S. aureus nasal carriage who were treated with mupirocin nasal ointment and chlorhexidine gluconate medicated soap (MUP-CHX), had a significantly lower risk of nosocomial S. aureus infections than patients receiving placebo (3.4% vs. 7.7%, 95% CI 0.23–0.75). In this study the effect of MUP-CHX on mortality in surgical patients with S. aureus nasal carriage was determined.
Methods: Patients were followed for survival up to one year after inclusion in the M-RCT. Mortality within one week after surgery was excluded from the analysis, based on the assumption that nosocomial S. aureus infection is unlikely to be the cause of death in these cases. Sub-group analysis was performed for cardiothoracic surgery, orthopaedic surgery, and for all other surgical specialties.
Results: In total, 799 surgical patients were included in the M-RCT. Two patients were lost to follow up and five patients died within one week after surgery. So, for mortality analysis 792 patients were included, i.e. 431 in the MUP-CHX group and 361 in the placebo group. Mortality after one year in all surgical specialties combined was 4.6% (20/431) in the MUP-CHX group vs. 7.5% (27/361) in the placebo group (p = 0.092). Analysis of surgical specialties separately revealed a significant reduction of mortality in cardiothoracic surgery who had been treated with MUP-CHX (2.3% (5/218) vs. 6.5% (11/170), p = 0.040, figure). In other surgical specialties no significant difference was found.
Conclusion: Peri-operative application of MUP-CHX in nasal carriers of S. aureus undergoing cardiothoracic surgery results in a threefold reduction of mortality after one year.
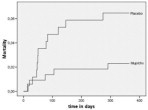
O142 A lot done, more to do – a survey of teaching about healthcare-associated infections in UK and Irish medical schools
H. Humphreys*, D. O'Brien, J. Richards, K. Walton, G. Phillips (Dublin, IE; Norwich, Newcastle-upon-Tyne, Dundee, UK)
Objectives: Patient safety and the prevention of healthcare-associated infections (HCAI) are increasingly important health issues. Medical doctors have traditionally been poor in complying with preventative measures to minimise HCAI such as hand hygiene compliance. We surveyed medical schools in the UK and Ireland to assess what is being taught and assessed in this area.
Methods: A questionnaire was drafted, piloted and then subsequently forwarded to the heads of medical schools as well as to known contact professionals with an interest in HCAI in 38 medical schools. The questionnaire surveyed topics covered in the curricula, the modalities used to assess knowledge and practice, the usefulness of various teaching methods and materials, e.g. lectures, and what education resources were available.
Results: Replies were received from 31 (82%) medical schools; two supplied data on their undergraduate and postgraduate courses. Only 18 (60%) covered HCAI as a quality and safety issue but over 90% covered prevalence, recognised risk factors, transmission, and preventative measures. 24 (80%) medical schools assessed competence in undertaking aseptic techniques and the disposal of sharps and MCQs were the most common (87%) means of assessment. Case scenarios, resource materials and clinical skills stations were used in educating students in 26 (87%), 22 (73%) and 22 (73%) medicals schools respectively. 25 (83%) medical schools would be willing to share educational resources on HCAI with other medical schools.
Conclusions: Medical schools in the UK and Ireland include HCAI in their curricula but its importance as a safety and quality issue needs to be further emphasized. There is potential for agreeing a core curriculum on HCAI and for sharing teaching resources such as videos and e-learning material.
O143 Modelling transmission and control of norovirus in healthcare settings
Z. Sadique*, B. Cooper, J. Edmunds, B. Lopman (London, UK)
Objectives: Noroviruses are most common cause of outbreaks of gastroenteritis in UK National Health Service hospitals, leading to ward closure costing as much as£115 million per annum. Using a detailed data set on norovirus outbreaks from three hospital systems in the South West of England, we estimated (1) the relative importance of introduction of norovirus from the community and within the hospital and (2) the cost effectiveness of ward closure at different time points during an outbreak.
Methods: Using regression models we examined the association between number of new outbreaks in a hospital and community levels of activity and number of outbreaks currently occurring in other wards within the hospital. We examined the effect of different ward types (admission, general and long stay units) and whether the ward was open or closed to new admissions on a given day. We then undertook as analysis of cost (-effectiveness) of unit closure by developing a dynamic transmission model taking into account that ward closure may reduce norovirus transmission within and between wards. The stochastic simulation model was based on the actual characteristics of an acute hospital and the norovirus transmission parameters quantified in the statistical analysis. We measured the costs and benefits of closing affected wards at 1, 3 and 5 days after the onset of symptoms in the first case.
Results: Community level of norovirus infection had a significant effect on the occurrence of new outbreaks as did outbreaks in admission and general medical units. The cost of closing wards to new admissions varied between £0.5 million to £0.9 million depending on the assumed effectiveness of closure in curtailing transmission. Cost of bed day loss – compared with staff illness – accounted for around 90% of the total cost of closure. Although the total number of cases tends to fall with rapid ward closure (by around 50% compared with no closure), the actual cost of control is similar regardless of when the closure is performed.
Conclusion: We have developed a modelling framework to assess the effectiveness and cost-effectiveness of strategies to control norovirus outbreaks in hospital settings. Ward closure is effective at preventing cases but since closure itself is an expensive intervention, it may not always be cost-effective.
Clostridium difficile
O144 Clindamycin resistance among Clostridium difficile PCR ribotype 027 in Scotland
D.J. Brown, C. Wiuff*, H. Mather, J. Coia (Glasgow, UK)
Objectives: To determine the susceptibility of Clostridium difficile PCR ribotype 027 isolates towards clindamycin and 8 other antibiotics obtained from patients with CDAD in Scottish healthcare facilities, and to compare resistance patterns to those of other prevalent ribotypes.
Methods: In Scotland testing for C. difficile toxin is mandatory for all patients aged 65 and over with diarrhoea. Since November 2007 culture of C. difficile has been mandatory for all severe cases of CDAD and/or cases from outbreaks. Isolates are typed centrally by the Scottish C. difficile Reference Laboratory using PCR ribotyping according to the method of O'Neill et al. (1996). Isolates of PCR ribotype 027 were susceptibility tested against 9 antibiotics using Etest (AB Biodisk, Solna, Sweden). Breakpoints were derived from the Clinical and Laboratory Standards Institute (CLSI) criteria and aligned with those used in England and Wales.
Results: A total of 635 isolates of C. difficile were obtained from patients in healthcare facilities in Scotland in the period November 2007-October 2008. Of the 635 isolates 75 were PCR ribotype 027 (12%). Other prevalent ribotypes were 001 (25%) and 106 (36%). 76% of the 027 isolates originated from 5 hospitals located in 2 healthboard areas. The remaining 18 isolates of ribotype 027 originated from 11 hospitals across Scotland. In vitro 96% of 027 isolates were resistant to clindamycin with a MIC range of 8–24 mg/L, MIC50 of 12 mg/L and MIC90 of 16 mg/L. Furthermore 100% of the 027-isolates were highly resistant to erythromycin (MIC50 ≥256 mg/L, MIC90 ≥256 mg/L), and to levofloxacin and moxifloxacin (MIC50 ≥32 mg/L, MIC90 ≥ 32 mg/L for both), while 65% of these isolates were resistant to cefotaxime (MIC50 = 64 mg/L, MIC90 = 96 mg/L). All 027-isolates were susceptible to metronidazole, vancomycin, meropenem and piperacillin-tazobactam. High frequencies of clindamycin, erythromycin, levofloxacin, moxifloxacin and cefotaxime resistance were also found among isolates of ribotype 001 (90–99%) and 106 (94–100%).
Conclusion: Until 2008 C. difficile ribotype 027 was only reported infrequently in Scotland. In 2008, reports of ribotype 027 became more frequent and clusters were detected in 5 hospitals. The majority (96%) of ribotype 027 isolates were resistant to clindamycin. Three other European countries have previously reported clindamycin resistance in PCR ribotype 027, albeit with a higher MIC90 of >256 mg/L.
O145 Trends in mortality due to Clostridium difficile enterocolitis in Brussels and Flanders, 1998–2006
I. Gutiérrez*, M.L. Lambert, A. Kongs, D. Mazina, H. van Oyen (Brussels, BE)
Objectives: To analyze trends in mortality due to Clostridium difficile enterocolitis and to describe the most affected groups in order to better understand current Clostridium difficile changing epidemiology.
Methods: We reviewed mortality data from the Flanders and Brussels regions in Belgium (about 7 million inhabitants). We selected those records in which ICD-10 code A04.7 (enterocolitis due to Clostridium difficile) appeared as underlying cause of death within the death certificate. Age- and sex-specific mortality rates were calculated for the period 1998–2006. Direct standardisation was performed using the European standard population and 95% confidence intervals were calculated. Stata 10® and Excel® were used as statistical software.
Table 1.
Standardised and crude ratesa of enterocolitis due to Clostridium difficile as underlying cause of death in Brussels and Flanders, 1998–2006
| 1998 | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | |
|---|---|---|---|---|---|---|---|---|---|
| Crude mortality rate | 0.1 | 0.1 | 0.1 | 0.2 | 0.3 | 0.7 | 1.7 | 1.7 | 1.6 |
| Standardised mortality rate | 0.1 | 0.1 | 0.1 | 0.1 | 0.2 | 0.4 | 1.0 | 0.9 | 0.9 |
| males standardised | 0.1 | 0.1 | 0.2 | 0.1 | 0.1 | 0.4 | 0.9 | 0.9 | 0.9 |
| females standardised | 0.1 | 0.1 | 0.1 | 0.1 | 0.3 | 0.5 | 1.0 | 0.9 | 0.8 |
| Age- and sex-specific mortality | |||||||||
| Males <65 | 0.0 | 0.0 | 0.0 | 0.0 | 0.1 | 0.1 | 0.0 | 0.1 | 0.1 |
| 65–79 | 0.3 | 0.5 | 0.7 | 0.5 | 0.2 | 0.7 | 4.6 | 2.2 | 2.9 |
| ≥80 | 0.0 | 0.0 | 4.0 | 2.5 | 2.3 | 14.3 | 20.9 | 29.7 | 26.3 |
| Females <65 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.1 | 0.1 |
| 65–79 | 0.4 | 0.2 | 0.0 | 0.6 | 1.4 | 2.0 | 3.5 | 1.8 | 1.6 |
| ≥80 | 1.2 | 1.8 | 1.2 | 2.9 | 6.6 | 12.2 | 32.4 | 31.3 | 29.3 |
Rates are expressed as deaths per 100,000 population.
Results: Standardised mortality rate increased from 0.06 deaths per 100,000 persons in 1998 to 0.85 deaths per 100,000 persons in 2006. A marked increase in mortality started in year 2002 (0.21 deaths per 100,000) and continued in 2003 and 2004 (0.43 and 0.95 deaths per 100,000).
In the age group of over eighty, crude mortality rate increased from 0.00 to 26.32 deaths per 100,000 persons for males, and from 1.16 to 29.31 deaths per 100,000 persons for females for the period 1998 to 2006. Standardised mortality rates for men of 0.05 (CI 95%:0.03–0.08) to 0.90 (CI 95%:0.82–0.99) deaths per 100,000 persons, were similar to those for women, 0.06 (CI 95%:0.04–0.08) to 0.79 (CI 95%: 0.73–0.85) deaths per 100,000 persons from 1998 to 2006.
Conclusion: Mortality due to Clostridium difficile enterocolitis has dramatically increased in Brussels and Flanders, mainly in the oldest age group during the period 1998–2006. We did not find significant differences between sexes. Further studies should address the causes of the described increase in mortality by Clostridium difficile.
O146 Contamination of a public tap water distribution system and possible water-borne transmission of Clostridium difficile
S. Kotila*, T. Pitkänen, A. Virolainen, E. Könönen, M. Kuusi, I. T. Miettinen, E. Eerola, R. Vuento, J. Brazier (Helsinki, Kuopio, Turku, Tampere, FI; Cardiff, UK)
Objectives: Toxigenic Clostridium difficile is an enteric pathogen typical in the hospital environment but also community-acquired cases have been reported. However, relatively few attempts have been made to clarify the role of soil or water as a source of C. difficile infection. In November-December 2007, the drinking water distribution system in the town of Nokia, Finland was massively contaminated with treated sewage effluent resulting in a large gastroenteritis outbreak. The aim of the present study was to evaluate if contaminated water in this outbreak was also a potential source of C. difficile infection.
Methods: A sample from the contaminated tap water and a treated sewage effluent sample were collected as soon as possible after the massive faecal contamination of the drinking water distribution system had occurred. C. difficile was isolated from heat-treated water samples by filtrating of 100 ml, 10 ml and 1 ml volumes of water and placing the membranes on selective CCEY agar plates, which were anaerobically incubated for 3 d. Stool samples from the patients fallen ill during the epidemic were examined for enteric pathogens, including C. difficile. All potential C. difficile colonies were subcultured on CCFA agar plates and toxin-positive isolates were identified by PCR. PCR ribotyping was performed according to the protocol of the Anaerobe Reference Unit in Cardiff, UK, using the Cardiff-ECDC culture collection as a set of reference strains. After gel electrophoresis, the band patterns were analyzed using the BioNumerics software.
Results: Altogether 22 C. difficile isolates were found in water samples. Twelve isolates were toxin-positive; 5 isolates were from contaminated tap water and 7 isolates from treated sewage effluent, the latter being the contamination source. Among the tap water and sewage effluent isolates, 4 and 5 distinct PCR ribotype profiles were identified, respectively. The 9 human faecal C. difficile isolates detected were divided into 4 distinct PCR ribotype profiles. None of the profiles were identical with that of the hypervirulent PCR ribotype 027. Two isolates, one from tap water and another from a patient, had an indistinguishable PCR ribotype profile. Conclusion: Our observation implies that C. difficile contamination of a tap water distribution system had occurred. Waterborne transmission of toxigenic C. difficile and subsequent C. difficile infection seems possible.
O147 Typing of Clostridium difficile strains with an automated repetitive PCR system in comparison to PCR ribotyping
T. Pasanen*, S. Kotila, S. Mero, J. Antikainen, E. Tarkka, E. Eerola, J. Jalava, A. Virolainen-Julkunen, E. Könönen, M. Vaara, P. Tissari (Helsinki, Turku, FI)
Objectives: An accurate and rapid method is needed for typing of toxigenic Clostridium difficile. A commercial automated repetitive PCR system (rep-PCR; DiversiLab®, Biomérieux Inc., St Louis, USA) utilises amplification and subsequent automated electrophoretic separation of the repetitive extragenic palindromic sequences of C. difficile. Our aim was to evaluate the performance of this rep-PCR method for genotyping of C. difficile isolates and to compare it to PCR ribotyping. In addition, the correlation between the rep-PCR and the virulence gene profiles of C. difficile strains was studied.
Methods: A total of 195 toxin-positive C. difficile isolates were studied. We included consecutive isolates from two laboratories in Finland, containing also strains of the hypervirulent C. difficile ribotype 027. In addition, selected C. difficile strains with >18bp deletions in their tcdC genes were analyzed.
The DNA was extracted and the rep-PCR performed according to the manufacturer's instructions. The amplification products of rep-PCR were detected and analyzed using the DiversiLab system. Further analysis was performed with the web-based software accompanying the system. The usefulness of the library construction option of the DiversLab system for isolate comparison was tested. The virulence genes (tcdA, tcdB, cdtA, cdtB and tcdC) were analyzed by conventional PCR and the whole gene sequencing of tcdC was performed from isolates with deletions >18 bp. PCR ribotyping was performed using the protocol of the Anaerobe Reference Unit in Cardiff, UK.
Results: The correlation between the rep-PCR profile and the ribotype was excellent. All major ribotype groups were clustered in their own rep-PCR groups. Interestingly, subgroups could be found with rep-PCR within two most prevalent ribotypes 001 and 027.
The automated rep-PCR proved to be reproducible; the results from separate DNA isolations and PCR-runs/microfluid electrophoresis as well as the results performed by different individuals of laboratory personnel were comparable. The rep-PCR profiles and PCR ribotypes correlated also with the virulence gene profiles.
Conclusion: This automated rep-PCR represents an effective and reproducible method for the genetic characterisation of C. difficile strains in clinical laboratories with molecular biology facilities. The constructed C. difficile library allows comparing the relatedness of C. difficile strains and their fingerprints over time.
O148 A randomised, double-blind clinical trial of OPT-80 versus vancomycin in Clostridium difficile infection
T.J. Louie*, K.M. Mullane, K. Weiss, A. Lentnek, Y. Golan, S. Gorbach, P. Sears, Y.K. Shue, M.A. Miller (Alberta, CA; Chicago, US; Montreal, CA; Marietta, Boston, San Diego, US)
Objectives: Clostridium difficile infection (CDI) is a serious diarrhoeal illness associated with high morbidity and mortality. Currently available treatments (oral vancomycin or metronidazole) usually produce good resolution of diarrhoea but are associated with a 20% to 30% incidence of recurrence. OPT-80, the first in a new class of macrocyclic antibiotics, is bactericidal via unique inhibition of RNA polymerase. This phase 3, non-inferiority clinical trial was conducted in more than 100 sites in North America and compared the efficacy and safety of OPT-80 and vancomycin in treating CDI.
Methods: Eligible patients were adults with acute CDI symptoms and a positive stool toxin test. Patients received oral OPT-80 (200 mg twice daily) or oral vancomycin (125 mg 4 times daily) for 10 days. Primary end point was clinical cure (resolution of symptoms and no further need for CDI therapy 2 days after stopping study drug). Secondary end point was CDI recurrence (diarrhoea and positive stool toxin test within 4 weeks after treatment). Global cure was defined as a clinical cure with no recurrence.
Results: 629 patients were enrolled and 87% were evaluable. In the per protocol (PP) population (n = 548), mean age was 61.3±17.1 years and 44.0% of patients were male. Equivalent rates of clinical cure were observed with OPT-80 (92%) and vancomycin (90%) in the PP analysis; similar outcomes were observed in a modified intent-to-treat (mITT) analysis. Significantly fewer patients treated with OPT-80 (13%) than vancomycin (24%) experienced recurrence in the PP analysis (P = 0.004) and in the mITT analysis (15% vs 25%; P = 0.005). Significantly more OPT-80-treated patients achieved global cure (78%) than vancomycin-treated patients in the PP analysis (67%; P = 0.006) and in the mITT analysis (75% vs 64%; P = 0.006). OPT-80 was well tolerated with an adverse event profile similar to that of vancomycin.
Conclusions: In this study – the largest comparative trial of a new antimicrobial agent versus vancomycin for the treatment of CDI – clinical cure rates after treatment with OPT-80 or vancomycin were equivalent. However, OPT-80 was associated with a significantly lower recurrence rate and a higher global cure rate than vancomycin. OPT-80 is an oral, non-absorbed agent that has a convenient (twice daily) dosing schedule and low risk of adverse events. OPT-80 represents a potential new treatment option for CDI that is associated with a lower recurrence rate than currently available treatments.
| OPT-80 (200 mg bid) | Vancomycin (125 mg qid) | P-value | 95% CI | |
|---|---|---|---|---|
| Per Protocol Analysis | ||||
| Clinical cure, % (n/N) | 92.1% (244/265) | 89.8% (254/283) | NA | −2.6,a |
| Recurrence, % (n/N) | 13.3% (28/211) | 24.0% (53/221) | 0.004 | −17.9, −3.3 |
| Global cure, % (n/N) | 77.7% (206/265) | 67.1% (190/283) | 0.006 | 3.1, 17.9 |
| Modified Intent-to-Treat (mITT) Analysis | ||||
| Clinical cure, % (n/N) | 88.2% (253/287) | 85.8% (265/309) | NA | −3.1,a |
| Recurrence, % (n/N) | 15.4% (39/253) | 25.3% (67/265) | 0.005 | −16.6, −2.9 |
| Global cure, % (n/N) | 74.6% (214/287) | 64.1% (198/309) | 0.006 | 3.1, 17.7 |
CI, confidence interval; NA, not applicable (non-inferiority end point was met).
One-sided 97.5%CI.
O149 Tackling Clostridium difficile at Kingston hospital – a case study
J. Yang*, S. Furrows, H. Lo, A. Jones, F. Brooke-Pearce, K. Lyons (London, UK)
Objectives: Kingston Hospital is a general hospital in London and, in common with acute Trusts, sees a number of cases of C. difficile toxin (CDT) associated disease.
The objective of the audits of CDT conducted in 2007 and 2008 was to develop a better understanding of CDT infections at Kingston Hospital: to investigate antibiotic prescribing, to understand the risk factors associated with CDT, to determine if CDT patients are treated in accordance with Trust guidelines and to study CDT-related mortality.
Methods: Both samples included all patients with a CDT positive stool sample in May-July 2007 and March-May 2008. Patient demographics, medical history and information on the CDT episode were collected retrospectively from medical notes, drug charts and multidisciplinary forms. Double entry ensured data quality. When relevant, consultant opinion on cause of death and information on the death certificate were compared.
Results: In 2008, 26% of CDT patients had diarrhoea on admission compared to 36% in 2007.
The mean time between diarrhoea onset and CDT diagnosis was 2.5 days. 85% diagnosed patients were seen every day or every other day by a doctor. 89% cases were discussed with Microbiology. Proton pump inhibitor prescribing decreased from 63% in 2007 to 48% in 2008.
96% patients took antibiotics during the 3-month period before developing CDT. Cephalosporins were prescribed for 19% patients, compared to 37% in 2007. Ciprofloxacin was not prescribed at all, compared to 45% patients prescribed ciprofloxacin in 2007 (p = 0.001, df = 1). All patients were treated for CDT according to Trust guidelines. In 2007, the percentage of patients with CDT who died was 40% and this dropped to 30% in 2008. However, according to Consultant opinion, CDT was only a definite/probable case of death in 3.7% patients. Consultant opinion on the death and information available on the death certificate differed in 4 out of the 8 patients who died.
Conclusion: The 2007 audit led to the implementation of an action plan and CDT rates gradually decreased in 2007–08. There was a marked improvement in antibiotic prescribing and in CDT treatment. These results are due to enhanced cleaning, a restricted antibiotic policy, a new isolation policy, an integrated care pathway for CDT, a new policy for management of CDT, new equipment, improved staff education and regular auditing.
In 2008, Kingston Hospital was one of only five Trusts out of 51 in England to be fully compliant with the Health Act.
O150 Optimisation and application of a multi-locus variable tandem repeat analysis for Clostridium difficile ribotype 078, toxinotype
D. Bakker*, J. Corver, C. Harmanus, W. Fawley, M. Wilcox, E. J. Kuijper (Leiden, NL; Leeds, UK)
Background: Recently, we reported an increase in C. difficile infection (CDI) caused by PCR-ribotype 078 (Type 078) in the Netherlands. C. difficile Type 078 is also the predominant ribotype in cattle. To investigate the relatedness between human and animal strains we optimised a Multi Locus Variable tandem repeat Analysis (MLVA) developed for Type 027, for type 078. MLVA was applied on 54 Type 078 strains of human (n = 43) and porcine (n = 11) origin, and on a further 67 human Type 078 isolates obtained in 2007–8 from England (E) and N. Ireland (NI).
Methods: Sequencing of the MLVA loci originally described for type 027 by van den Berg et al, J Clin Microbiol. 2007) was done in 15 type 078 strains, both human and porcine origin using primers in the adjacent ORFs. The Variable Number Tandem Repeats (VNTR) was determinate by manual examination of the sequence data. PCR products sizes were analyzed with ABI 3100 sequence analyzer and the VNTR were calculated from the PCR product sizes. To validate the calculated VNTR we compared it with the manual analyzed VNTR sequence data. Finally, we applied the optimised MLVA on all available type 078 strains which were previously tested with a first generation MLVA.
Results: Sequence analysis (SA) revealed that locus A is absent in Type 078 and that some mismatches are present in the primer annealing sites for loci B, C and G. Lowering the annealing temperature and increasing the magnesium chloride concentration for loci B, C and G resolved the low yield of PCR products. Applying the MLVA on 54 type 078 strains revealed that 42 (80%) strains, encompassing isolates from human (n = 42) and porcine (n = 11) origin, are genetically related with a summed tandem repeat differences (STRD) ≤10). Three clonal complexes (CC, defined by STRD ≤2) were recognized; one CC contained both human (n = 4) and porcine (n = 3) strains. The optimised MLVA identified 3 genetically related clusters and 6 CC among the 67 isolates from E and NI. CCs contain isolates from more than one hospital and indeed for several clusters isolates from both E and NI. 2 isolates obtained from NI 8 years earlier were part of one large CC.
Conclusions: The optimised MLVA can distinguish and/or group Type 078 strains from distinct settings. Type 078 strains from human and animal origin are genetically related. The clustering of some isolates from distinct settings is consistent with community sources for Type 078. The last 2 observations suggest zoonotic transmission.
O151 Community-associated Clostridium difficile infection: an analysis of cases reported to the English NHS mandatory surveillance system from April 2007 to September 2008
A. Pearson*, R. Guy, R. Blackburn, R. Mandalia, J. Davies, M. Murray, S. Batley, B. Duerden, J. Giltrow, M. Painter, M. Fleming (London, UK)
Objectives: This paper updates our assessment of the contribution that community-associated Clostridium difficile infection (CDI), as reported to the English mandatory surveillance scheme since 2007, makes to both the acute and community sectors of the National Health Service (NHS) in England.
Methods: NHS acute Trusts (hospital groups) in England are required to report all C. difficile toxin positive diarrhoeal specimens processed by their laboratories whether the patients were in hospital or the community at the time of onset of the illness or when the specimen was taken via a web enabled reporting system. Positive specimens from the same patient within 28 days are not reported. Reported cases in patients under 2 years of age were omitted from this analysis.
Enhanced surveillance data (including information on date of admission, patient location prior to testing, sex, age and patient category) on CDI have been collected through a web-enabled reporting system since April 2007. Risk factor information is completed on a voluntary basis.
Results: More than 75,000 cases of CDI in patients aged >2 years were reported, 23% of these cases were taken in non-acute settings of which 74% were taken by a General Practitioner. A further 17% of specimens were taken on presentation or <2 days of admission into an acute Trust. Approximately 32% of all cases had at least one risk factor field completed, >19,000 cases reported risk factor information on episode category; 23% of these cases were community associated and 77% were hospital acquired. The information reported suggests that only 3% of the community associated cases were from patients with continued infection or relapsed episodes of CDI, this is compared to 8% of the hospital acquired cases who had continued infection or relapsed episodes of CDI.
Conclusions: 23% of the C. difficile specimens reported by acute Trusts were diagnosed in a community setting. Published studies suggest that 12–15% of these might be expected to have been acquired during a hospital stay within the previous month (i.e. were community onset hospital acquired cases). Future work is required to investigate whether there are differences in the epidemiology, risk factors e.g. antibiotic exposure and outcome of patients with community onset disease.
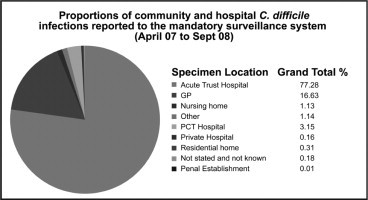
O152 Clostridium difficile-associated disease: a newly notifiable disease in Ireland
M. Skally, F. Roche, D. O'Flanagan, P. McKeown, F. Fitzpatrick* (Dublin, IE)
New cases of Clostridium difficile-associated disease (CDAD) became notifiable in Ireland on 4th May 2008. The main objective of this new notification process was to provide a national overview of the epidemiology and burden of CDAD. This paper review the first six months of preliminary data notified.
Methods: The interim case definitions for new and recurrent CDAD cases proposed by the European Society for Clinical Microbiology and Infectious Diseases (ESCMID) Study Group for C. difficile were employed. This report reviews the weekly events of CDAD extracted from the Computerised Infectious Disease Reporting (CIDR) system in January 2009. Census of Population 2006 figures were used as denominator data in the calculation of incidence rates. Results presented represent 34 weeks of data submitted.
Results: There were 1581 new CDAD cases notified on CIDR between the 4th May 2008 and 27th December 2008, representing a crude incidence rate (CIR) of 37.3 cases/100000 population (estimated annual CIR is 57.0 cases/100,000). All cases were laboratory confirmed. There was a higher occurrence of cases in females. The male:female ratio for the period was 1:1.6. In 0.4% of cases the sex was unknown. 71.4% of cases were in the greater than 65 years age category. The preliminary data submitted on CIDR indicate that 63.0% of cases were hospital inpatients and 8.9% of cases were either GP patients or outpatients. The origin of 28.1% of samples is unknown. There was large variation between the 8 public health regions (Table 1 ).
Table 1.
Number of cases and CIR of human CDAD in Ireland, May–December 2008 (CIDR)
| Region | Number of cases | CIR incl. 95% CI | Estimated annual CIR incl. 95% CI |
|---|---|---|---|
| ERHA | 747 | 49.8 [46.2–53.38] | 76.2 [71.8–80.6] |
| MHB | 37 | 14.7 [9.97–19.4] | 22.5 [16.6–28.3] |
| MWHB | 79 | 21.9 [17.1–26.7] | 33.5 [27.5–39.4] |
| NEHB | 36 | 9.1 [6.2–12.1] | 14.0 [10.3–17.7] |
| NWHB | 93 | 39.2 [31.3–47.2] | 60.0 [50.1–69.8] |
| SEHB | 118 | 25.6 [21.0–30.2] | 39.2 [33.5–44.9] |
| SHB | 254 | 40.9 [35.9–45.9] | 62.5 [56.3–68.8] |
| WHB | 217 | 52.4 [45.4–59.35] | 80.1 [71.5–88.7] |
| Ireland | 1581 | 37.3 [35.5–39.1] | 57.03 [54.8–59.3] |
Conclusions: The incidence of CDAD in Ireland is prominent in older age groups and in healthcare settings. What is more remarkable is the regional variation of cases reported. This varies from 9.1 per 100,000 in the North East to 52.4 per 100,000 in the West. The seasonal trend is indistinguishable at present due to late and batch notifications from institutions.
O153 Clostridium difficile-associated diarrhoea in immunosuppressed patients with cancer
C. Gudiol*, C. Garcia-Vidal, J. Niubó, R. Duarte, L. Jiménez, J. Carratalà (Barcelona, ES)
Objective: To assess the epidemiology, clinical features and outcome of Clostridium difficile (CD) associated diarrhoea in immunosuppressed patients with cancer.
Methods: Review of all episodes of CD associated diarrhoea documented in adults with cancer and haematopoietic stem cell recipients (2000–2008). Microbiologic diagnosis included CD isolation from stool samples, direct detection of CD toxin, and testing for cytotoxin production by the isolated strain.
Results: We documented a significant increase of CD associated diarrhoea, from 0.34/1000 admissions in 2000 to 4.05/1000 admissions in 2008 (p < 0.01). There were 56 episodes in 54 patients. Thirty-one patients were male (55%) with a mean age of 52 years (± 16). Forty three (77%) patients had an haematological underlying disease and 13 had solid tumour; 41 (73%) had received previous chemotherapy, 14 (25%) were stem cell transplant recipients (3 presenting with GVHD) and 17 (30%) were neutropenic (<500). In the previous month 52 patients (93%) had received one or more antibiotics (cephalosporins 63.5%, glycopeptides 40%, carbapenems 38.5%, betalactam + betalactam inhibitors 29%, quinolones 19%). Fever >38°C (71%) and abdominal pain (44%) were the most frequent manifestations, and the diarrhoea was hemorrhagic in 8% of the cases. Most patients (77%) were treated with metronidazole (median 11 days), and the antibiotic therapy was discontinued in 56%. In 5 patients who had recovered from neutropenia, the diarrhoea resolved just by discontinuing the antibiotic therapy. No patient developed toxic megacolon or needed surgery. Three patients (5.5%) had relapses. Overall mortality (<30 days) was 22% (12 patients). Conclusion: The incidence of CD associated diarrhoea in cancer patients has increased significantly in recent years. It is related with important morbidity and mortality. Better strategies to improve its prevention and treatment are needed.
From lab to ward: optimising treatment strategies for invasive Candida infections (Symposium organised by Astellas)
S154 Linking research to the clinic: how laboratory findings relate to management of invasive Candida infections
F. Odds* (Aberdeen, UK)
The role of the research laboratory in the management of invasive Candida infections goes beyond routinely available tests for identification of Candida species and susceptibility testing of antifungal agents. Cutting-edge molecular epidemiology technologies have been used to type isolates of Candida species based on their DNA sequences. Multilocus sequence typing schemes have been designed for C. albicans, C. dubliniensis, C. glabrata, C. krusei and C. tropicalis.
Multi-locus sequence typing can be used to investigate possible hospital outbreaks of infection (finding widely different strain types within a unit indicates no outbreak, although the converse is not true). For C. albicans, typing multiple isolates from the same patient has shown that people tend to harbour as commensals a mixture of closely related but different strain types, which may provide for selection of the most appropriate type for invasion of a particular tissue or in response to antifungal treatment. Strains in C. albicans clade 1, the largest group of related strain types, have a higher proportion of isolates resistant to flucytosine than other clades, and they all share a common resistance mechanism. Research on mechanisms of resistance of Candida species to many types of antifungal has progressed to the point that some investigators are looking to design DNA chips that could be used both for identification and for susceptibility testing of a Candida isolate.
Much research effort goes into detailed study of host–fungus crosstalk in experimental Candida infections. Animal models of infection have been greatly refined and the latest research shows how early release of chemokines that attract neutrophils into infected tissues contributes to the immunopathology of Candida infection. This rapid, innate immune response also emphasizes the need for antifungal intervention at the earliest possible stage to provide the best chance for successful treatment of a disseminated Candida infection – a finding now supported by clinical data as well as experimental models.
Translation of the latest research advances into practical diagnostic tests and new therapeutic approaches for Candida infections always takes a long time – typically years – and not all research results find clinical applications. However, the level of effort invested in basic Candida research ensures support for steady progress in diagnosis and management.
S155 Pharmacokinetics and pharmacodynamics of the echinocandins: from models to medicine
W. Hope* (Manchester, UK)
The echinocandins are semi-synthetic lipopeptides that are increasingly used for the prevention and treatment of invasive fungal infections. Understanding the pharmacokinetic and pharmacodynamic (PK/PD) characteristics of these compounds is critical for their optimal clinical use.
The echinocandins have potent in vitro activity against Candida spp., although C. parapsilosis is less susceptible than other Candida species. The molecular mechanisms of resistance in Candida species, which relate to amino acid substitutions in ‘hot spots’ within the FKS1 gene, are becoming well characterised. Susceptibility breakpoints for all three clinically available compounds have been determined recently by the Clinical Laboratory Standards Institute, with a ‘susceptible-only’ breakpoint of >2 mg/l suggested.
The PK/PD of the echinocandins have been determined in experimental models of disseminated candidiasis, and of both disseminated and pulmonary invasive aspergillosis. These studies suggest that the echinocandins: (1) display concentration-dependent antifungal killing (or effect); (2) are extensively distributed into peripheral tissues, where they exhibit prolonged mean residence times at the site of infection; (3) are fungicidal against Candida spp. and induce dose-dependent morphological changes in Aspergillus spp.; and (4) result in a diminished propensity for angioinvasion by Aspergillus spp. Recent evidence also suggests that the echinocandins have important immunomodulatory properties, which may contribute significantly to their observed antifungal effect. PK/PD modelling and laboratory animal-to-human bridging techniques have been used to identify safe and effective dosages for the echinocandins for relatively uncommon clinical syndromes such as neonatal haematogenous Candida meningoencephalitis. These techniques are an efficient method of identifying effective regimens for humans that can be expedited for study in clinical trials.
PK/PD modelling techniques can and should be used to address outstanding clinical queries in relation to these compounds, including optimal dosages, decision-support analysis for the setting of in vitro antifungal susceptibility breakpoints and the clinical relevance of inherent or acquired reduced antifungal susceptibility.
S156 Invasive candidiasis: which antifungal treatment for which patient?
B. Dupont* (Paris, FR)
Management of patients with invasive candidiasis represents a complex issue owing to the heterogeneity of patients in whom these infections occur. Established risk factors for invasive candidiasis, which include total parenteral nutrition, multiple organ failure and Candida colonisation, are common to many types of patients that are treated within the critical care setting. Furthermore, the severity of the underlying condition in these patients necessitates swift antifungal treatment to ensure optimal outcomes. An additional factor for consideration when treating Candida infections is the changing epidemiology of Candida species; potentially fluconazole-resistant species such as C. glabrata and C. krusei are becoming more common, particularly in patients with prior fluconazole exposure.
A range of antifungal agents is available with in vitro activity against Candida species. However, not all of these agents are suitable options for the clinical management of invasive candidiasis because of the overall complexity of both infection and underlying condition. For example, the position of the polyenes, particularly amphotericin B deoxycholate, is becoming less tenable as the risk of renal complications is increasingly regarded as unacceptable in patients that are likely to have or be at risk of multiple organ failure. Furthermore, because of the increasing prevalence of fluconazole-resistant species, recent guidelines no longer recommend the use of azoles as first-line treatment for invasive candidiasis except in special cases, focusing instead on the echinocandin agents.
There is now a wealth of clinical data available for the echinocandins. Micafungin, for example, has been assessed in invasive candidiasis in clinical trials that included a wide variety of underlying conditions and patterns of infection, including neutropenic patients and those with deep infections such as peritonitis. Furthermore, micafungin is the most extensively evaluated of the echinocandins in paediatric patients, having been tested both in children up to the age of 16 years and in premature infants and neonates.
Optimal management of patients with invasive candidiasis depends on a strategy that takes into account the complex nature of the disease. Judicious selection of antifungal treatment should be accompanied by consideration of non-drug-related factors that improve survival, such as careful assessment of intravenous catheters and their potential involvement in Candida infections.
S157 Effective treatment of invasive candidiasis: case studies
J. Perfect* (Durham, US)
Patients with invasive candidiasis often have underlying conditions that are severe illnesses in themselves. These range from neutropenia during cancer chemotherapy to the multi-organ failure of intensive care unit patients. Against this background of severe underlying illness, it can be difficult to appreciate the success or otherwise of treatment strategies for Candida infections.
In the last decade, major advances have been made in antifungal therapy with the introduction of
-
1.
echinocandins;
-
2.
extended-spectrum azoles; and
-
3.
lipid formulations of amphotericin B.
Robust clinical studies for their successful use in candidaemia have been published. However, it is important to translate these studies into practical strategies for the care of individual patients.
In this presentation, individual cases will be used to provide insights into the successes and failures of these antifungal classes for the management of invasive candidiasis. Specific interest will be focused on the use of fluconazole versus the echinocandins. These micafungin-based cases will be supported by insights from the evidence-based literature combined with practical experiences at the bedside. The factors to be considered are:
-
1.
spectrum of activity;
-
2.
drug toxicity;
-
3.
drug interactions;
-
4.
drug resistance;
-
5.
pharmacology;
-
6.
diagnosis;
-
7.
site of infection;
-
8.
use of biomarkers/cultures in treatment strategies; and
-
9.
costs.
It is important to realise that large clinical trials exclude many patients with invasive candidiasis. Therefore, with the use of individual cases, it is possible to provide further insights into the clinical use of these outstanding antifungal agents.
Patient management: the era of rapid diagnostic results (Symposium organised by Cepheid)
S161 Will community MRSA and Clostridium difficile change infection control in hospitals?
F.C. Turnover* (Sunnyvale, US)
Infections caused by methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant enterococci, and Clostridium difficile are inter-related in healthcare institutions. The emergence of epidemic MRSA and C. difficile strains has placed a greater burden on infection control systems in healthcare facilities, which often must increase surveillance and change disinfection strategies to halt the transmission of these pathogens in hospitals. Ironically, the USA300 MRSA strain arose in the community but now is being transmitted frequently in healthcare settings, while the epidemic NAP1/BI/027 C. difficile strain was originally a healthcare-associated pathogen, which now is causing considerable morbidity in community settings. To successfully slow the spread of these pathogens, infection control must work closely with both the laboratory and pharmacy services to ensure that these organisms are detected rapidly and that the selective pressure to maintain the organisms in the institution are reduced. Clearly, bundles of interventions, rather than single approaches, are necessary to contain the spread of these organisms in hospitals. The continued influx of patients with community-acquired MRSA and C. difficile infections into healthcare institutions is a challenge for infection control practitioners that will clearly increase in the future.
The bacterial pathogen Listeria monocytogenes: a multi-faceted model
K170 Listeria monocytogenes: a bacterial pathogen responsible for severe infections and a multi-faceted model in biology
P. Cossart* (Paris, FR)
The food borne pathogen L. monocytogenes discovered by Murray in 1926 is responsible for a severe infection with various clinical features (gastroenteritis, meningitis, meningoencephalitis and materno foetal infections) and a high mortality rate (30%). The disease is due to the ability of Listeria to cross three host barriers during infection: the intestinal barrier, the placental barrier and the blood brain barrier. It is also due to Listeria capacity to survive in macrophages and to enter into non phagocytic cells, such epithelial cells. Recovery from infection and protection against reinfection are due to a T-cell response, explaining why Listeria has since many years has become a model in immunology. Nearly three decades of molecular biology and cell biology approaches coupled to genetic and post-genomic studies have promoted Listeria among the best models in infection biology. In depth studies of the mechanism of entry into cells has help unraveling how Listeria crosses the intestinal and placental barrier. Unsuspected concepts in cell biology were discovered. Post-genomic studies have recently allowed to unveil the Listeria transcriptional landscape during switch from saprophytism to virulence.
The talk will give an overview highlighting recent results in the frame work of well established data.
FUN-gi: thoughts on yeasts, moulds and medicine
K172 FUN-gi: thoughts on yeasts, moulds and medicine
F. Odds* (Aberdeen, UK)
The last several decades of research in medical mycology have offered great insights into fungal cell biology, epidemiology, phylogenetics and the cells and molecules involved in the pathogenesis of fungal disease. A legitimate question is to ask to what extent our extensive advances in comprehension of the biology of fungal pathogens have contributed to improvements in diagnosis and treatment. To what extent do patients benefit from translation of basic research into tools for clinical management? And the equally valid question: to what extent does biological science benefit from study of fungi that are opportunistic pathogens?
The speaker will examine some of these questions from the perspective of long experience in the field and the curmudgeonly attitude that develops with age.
News from the world of vaccines in a nutshell
O173 Meningococcal vaccines and vaccination strategy in the Czech Republic
J. Kalmusova, M. Musilek, P. Kriz* (Prague, CZ)
Objectives: The incidence of invasive meningococcal disease (IMD) has been reported in the Czech Republic since 1943. In response to the emergence of a new hypervirulent clonal complex, cc11, nationwide enhanced surveillance of invasive meningococcal disease was implemented by the National Reference Laboratory for Meningococcal Infections (NRL) in 1993.
Methods: The case definition is consistent with the ECDC guidelines. Culture and PCR are used for confirmation of cases. Notification is compulsory and is performed by local epidemiologists. Strains of Neisseria meningitidis isolated from IMD cases are referred by the field laboratories to the NRL to be characterised by serogrouping, PorA and FetA sequencing (http://neisseria.org/nm/typing/) and multilocus sequence typing (MLST) (http://pubmlst.org/neisseria/). In the NRL, the epidemiological database is matched against that of strains to avoid duplicate reporting in the final enhanced surveillance database.
Results: Despite the stable trend in IMD incidence (0.8/100 000) since 2005, the case fatality rate was high (11.8%) in 2007. The disease was caused mainly by serogroup B meningococci (67.4%) in 2007, followed by serogroups C (20.9%) and Y (9.3%). The most frequent clonal complexes were cc18, cc41/44 and cc32 (typical for serogroup B) and cc11 (typical for serogroup C). The highest age-specific morbidity rates were observed in the lowest age groups, i.e. 0–11 months and 1–4 years (11.4/100 000 and 4.5/100 000, respectively), and were associated with high prevalence of serogroup B. The case fatality rate was the highest in infants under 1 year of age (38.5%). The incidence of IMD caused by serogroup C is currently low and there is no indication for mass vaccination with MenC conjugate vaccine. MenB vaccine is needed for infants, but the sero/subtype coverage by the currently developed porin-based vaccines is low for Czech meningococcal isolates (maximum 56.8% for nine-valent meningococcal PorA vaccine).
Conclusion: There is no indication for mass vaccination with MenC conjugate vaccine in the Czech Republic, but MenB vaccine and conjugated tetravalent ACYW135 vaccines are required. Other than porin-based vaccine effective against N. meningitidis B needs to be developed.
O174 The impact of structured vaccine programme of care on vaccine uptake in the HIV population attending an urban clinic – a 5-year review
C. Rock*, A. Dillon, E. de Barra, C. Dowling, S. Kelly, C. McNally, C. Bergin (Dublin, IE)
Objectives: HIV infected persons may experience considerable morbidity and mortality due to vaccine preventable diseases. Vaccination guidelines for HIV patients are constantly under review. Current British HIV Association Guidelines recommend regardless of CD 4 count that all should get annual influenza, 1–2 doses pneumococcal and if not immune hepatitis vaccination. MMR and varicella vaccination are considered for those non-immune with CD4 > 200. This is particularly significant for HIV positive patients migrating from COHP.
In 2002 a structured multi-disciplinary vaccination programme was established. In our clinic we routinely offer annual influenza vaccination, pneumococcal vaccination, hepatitis B, A and varicella vaccinations to all non immune and travel vaccinations as appropriate.
Methods: The vaccination programme incorporates dedicated vaccine clinic with a multi-disciplinary team including a nurse, data manager, a pharmacist specifically appointed to the unit. Additional interventions to improve vaccine uptake and outcome have included use of SMS texting to announce availability of influenza annually and improve adherence to completion of hepatitis B vaccination, educational programmes changes in guidelines e.g. varicella vaccination and creation of a vaccine passport. We reviewed vaccination clinic activity in the cohort of 1,700 HIV positive patients since introduction of a dedicated vaccine service.
Results: There has been a large increase in the uptake of vaccinations since introduction of this service. The varicella vaccination uptake increased from 8 (2007) to 43 (2008) due to targeted vaccine programme. (see graphic , legend reads left to right)
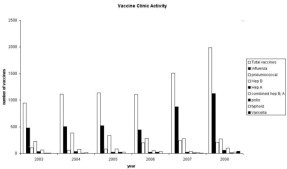
Conclusion: Strategies implemented increased the uptake of recommended vaccinations in our HIV population. These included appointment of a dedicated health professional team, use of IT supports, education of staff and patients and development of a vaccine passport. We developed the vaccine passport to help with patient education and awareness and it will serve as a record of vaccine administration for physicians off site. In the latter year, post guideline change, we have targeted our varicella non immune population. The next intervention planned is to assess all late entrants to our healthcare system to determine need for catch up vaccines, including MMR.
O175 An umbilical cord blood model of dendritic cell vaccination demonstrates the ex vivo generation of de novo strain-specific T-lymphocyte responses
W. Decker, E. Shpall, A. Safdar* (Houston, US)
Background: In patients with haematologic malignancy response to standard influenza vaccine is not encouraging (Safdar et al. JID 2006). Toward the goal of addressing this issue, we have developed an in vitro model of dendritic cell (DC) immunotherapy utilising DCs generated from umbilical cord blood (UCB). Here we demonstrate that this model can truly generate immune responses de novo, excluding the possibility that in utero priming contributes to observed antigen-specific responses.
Methods: UCB units were obtained from the MD Anderson Cord Blood Bank under research protocol Lab03–0796 with IRB approval. UCB monocytes were harvested by adherence, and UCB DCs were generated by incubation in GM-CSF and IL-4. Immature DCs were loaded with purified rHA protein [A/New Caledonia/20/99 (H1N1), A/Vietnam/1203/2004 (H5/N1), and A/Netherlands/219/03 (H7/N7)] (Protein Sciences, Meridian, CT) or with purified rLuciferase (Promega, Madison, WI). DC were loaded both individually and with a mix of all three rHA isoforms. Subsequently, loaded DC were matured and used to stimulate autologous non-adherent lymphocytes. T-lymphocyte priming and development were supported by supplementation with IL-12, IL-2, IL-7, and IL-15 (R&D Systems, Mineapolis, MN). Following two restimulations and expansion, antigen specific responses were verified by IFN-gamma ELISpot. Following priming and restimulation with New Caledonia-loaded, Vietnam-loaded, Netherlands-loaded, mixture-loaded, luciferase-loaded, or unloaded DC, T-lymphocytes were stimulated a third time, and IFN-gamma secretion was quantitated by ELISpot analysis.
Results: T-cells primed by New Caledonia-loaded DC responded only to restimulation with New Caledonia-loaded DC (p < 0.004). T-cells primed by Vietnam-loaded DC responded only to restimulation with Vietnam-loaded DC (p < 0.02) with only slight cross-reactivity to New Caledonia-loaded DC. T-cells primed by Netherlands-loaded DC responded only to restimulation with Netherlands-loaded DC (p < 0.005). T-cells primed by luciferase-loaded DC responded only to restimulation with luciferase-loaded DC (p < 0.006). T-cells primed by DC loaded with all a mix of all three HA isoforms were also able to respond to restimulation by singly-loaded DC.
Conclusions: The model demonstrates that de novo HA-specific immune responses may be generated from UCB lymphocytes, excluding the possibility that observed responses were generated by in utero priming.
O176 SspB1 – streptococcal surface protein as possible component of recombinant streptococcal vaccine
K. Grabovskaya, T. Gupalova, G. Leontieva, A. Korjueva, L. Meringova, E. Kuleshevitch, A. Totolian, A. Suvorov* (St. Petersburg, RU)
Objectives: Group A (GAS) and group B (GBS) streptococci are the most common human pathogens of bacterial origin causing various diseases including severe invasive cases. Recently several laboratories of the world attempted to generate a vaccine but there is none on the market so far. Previously we demonstrated that effective protection against streptococci can be achieved by the immunisation with complex of recombinant surface expressed proteins where different proteins provide different degree of protection against different individual strains belonging to various serotypes. Here we describe the features of the novel vaccine candidate – surface protein SspB1 encoded by the gene localised on the pathogenicity island.
Methods: Recombinant protein SspB1 was obtained after cloning of 3000 bp fragment of the sspB1 gene in the expression vector pQE30 and purification of the protein on His-tag columns. Protein was used for immunisation of mice and rabbits. Raised antibodies were tested for in vitro protection against GBS serotypes I, II and III and GAS (M type 49) in opsonophagocytosis and in the experiments in vivo employing passive and active protection on mice model. Adherence of GBS expressing SspB1 was tested on tissue cultures Hep-2 and A-431.
Results: Column purified recombinant protein SspB1 was found to be a good antigen for both groups of animals used for immunisation. Antibodies against the recombinant SspB1 tested by opsonophagocytosis were found to enhance phagocytosis of 4 GBS strains belonging to different serotypes at the average 5.5 times relatively to control. Affect against GAS strains was less pronounced (2.5 times) but still statistically significant. Antibodies were also capable to interfere with adherence of GBS strains carrying SspB1 relatively to the strain without the protein. Adherence of the strain with SspB1 towards different cell lines was dramatically higher which proves the function of the protein as adhesin. In passive protection test carried out with mice challenged with virulent GBS or GAS strains introduced intranasaly were eliminated from the lungs of the animals 20 times faster in case of the usage of anti SspB1 serum relatively the control. In the experiments with active protection SspB1 immunised animals were found be significantly better protected against GBS and GAS infection.
Conclusion: SspB1 – novel GBS adhesion might be considered as candidate for generation of recombinant streptococcal vaccine.
O177 Effect of vaccines made in developing countries on measles mortality: a case study
H. Peltola*, S.V. Kapre, S.S. Jadhav, P.S. Kulkarni (Helsinki, FI; Pune, IN)
Objectives: UNICEF started procuring vaccines for low- and middle-income countries in 1978. In 1993, for the first time, a measles vaccine from a developing country, India, was prequalified by WHO. Since then it has been the most commonly used vaccine across the developing world. Here we correlate its use to the reduction of measles mortality worldwide.
Methods: Measles data were collected from literature and the WHO press releases for 1990 and 2007. Since we have an access to the database of the largest Indian company, we calculated the number of vaccine doses it supplied to UNICEF and PAHO from 1996 till 2008. We also found out the price UNICEF paid for the measles, measles-rubella, and measles-mumps-rubella vaccines.
Results: In 1990, there were 872,000 measles deaths worldwide of which no less than 869,000 (>99%) occurred in the less privileged countries. The vaccine prices were not attractive enough to the manufacturers in industrialised countries to prequalify and supply UNICEF and PAHO. Since only 1993 large enough quantities of measles vaccine have been available from a developing country company, which in the 12-year period (1996–2008), supplied these agents with >1.6 billion doses of the measles component containing vaccines. Now, the largest supplier to UNICEF and PAHO is India, not an industrialised country. Since these agents purchase low-price vaccines, the costs almost certainly have been much less than for the Big Pharma vaccines. In 2007, UNICEF paid just USD0.222, 0.525, and 0.860 per dose of the measles, measles-rubella, and measles-mumps-rubella vaccine, respectively. Global measles deaths in 2000–2007 declined by 74%, from estimated 750,000 to 197,000, respectively (BMJ 2008;337:a2949).
Conclusions: While costly new vaccines are pushed forwards with lavish campaigns, “old”, and often considerably more relevant vaccines are left behind. Measles is a good example of severe disease, still rampant in the non-industrialised world, to which little attention is paid by Big Pharma. Some less privileged countries such as India have taken the initiative in their own hands and started own vaccine manufacturing. Availability of good-quality vaccines at affordable price in huge quantities is the main reason of the spectacular reduction of the measles mortality; now also countries with the highest burden can afford this pivotal vaccination. Contribution of the high-standard developing country manufacturers credits recognition.
Bacteraemia
O178 Mortality impact of positive blood cultures in patients with suspected community-acquired bacteraemia. A Danish population-based cohort study
M. Søgaard*, M. Nørgaard, H.T. Sørensen, H.C. Schønheyder (Aalborg, Aarhus, DK)
Objective: We examined the prognostic impact of positive blood cultures compared to negative cultures on mortality in patients, who had blood cultures obtained during the first 72 hours of admission to a medical ward.
Methods: We conducted this population-based cohort study of adults (n = 20,210) with a first-time registered blood culture during 1995 through 2006 in Northern Denmark. We obtained information on blood cultures, coexisting chronic diseases (for this study identified as the 19 chronic diseases included in the Charlson Comorbidity Index), laboratory findings, and immunosuppressive therapy from medical databases. Positive cultures were defined as those with growth of one or more pathogen given an aetiological role based on joint clinical and microbiological assessment.
Mortality within 180 days following the date of first blood culture was determined through the Danish Civil Registration System. We computed Kaplan-Meier curves and product limit estimates for the main study variables. Next, time-dependent Cox regression analyses was used to compare the risk of death in patients with positive blood cultures and patients with negative cultures at days 0–7, 8–30, and 31–180, controlling for age, gender, coexisting chronic diseases, marital status, use of immunosuppressives, and calendar period. Further, we conducted analyses restricted to patients a discharge diagnose of infectious diseases (ICD-10 codes A00-B99).
Results: In total, 1,665 (8.2%) patients had positive blood culture. Mortality among patients with positive cultures was higher than among patients with negative during the first 30 days of follow-up: 8.4% vs. 4.6% after 7 days, and 5.5% vs. 4.9% during days 8–30, corresponding to adjusted mortality rate ratios (MRRs) of 1.5 (95% CI: 1.2–1.8) and 0.9 (95% CI: 0.7–1.2), respectively. Beyond day 30, mortality was 8.2% among patients with negative culture and 10.4% among patients with positive culture (adjusted MRR 1.0, 95% CI: 0.9–1.2). 2,934 patients had a discharge diagnosis of infectious disease, of which the blood culture was positive in 646 (22.0%). Among these patients the prognostic impact of bacteraemia persisted throughout the follow-up period (0–7 days: MRR = 1.7 (95% CI 1.2–2.6); 8–30 days: MRR = 1.2 (95% CI 0.7–1.9); 31–180 days: MRR = 1.6 (95% CI 1.0–2.1)).
Conclusion: Positive blood culture is a predictor of mortality in patients with suspected bacteraemia.
O179 Mortality of Staphylococcus aureus bacteraemia and infectious diseases specialist consultation – a study of 521 patients at a tertiary care centre in Germany
S. Rieg*, G. Peyerl-Hoffmann, K. de With, C. Theilacker, D. Wagner, J. Hübner, M. Dettenkofer, A. Kaasch, H. Seifert, C. Schneider, W. Kern (Freiburg, Cologne, DE)
Objectives: To evaluate the relationship between mortality of S. aureus bacteraemia (SAB) and infectious diseases (ID) specialist consultation and other factors potentially associated with outcomes.
Methods: A new ID service was established in 2002 at a 1,600-bed university hospital in southwestern Germany. Consecutive adult patients with SAB admitted between January 1, 2002 and December 31, 2007, were assessed using a standardised data collection and review form. Patients admitted during the first three years of the study were evaluated retrospectively, patients of the second three years were evaluated prospectively. ID consultation included physical examination, chart and laboratory result review and written recommendations for therapy and follow-up examinations based on established guidelines, literature review and individual case discussions.
Results: A total of 521 patients with SAB were enrolled and evaluated for in-hospital mortality; 430 patients completed a 90-day follow-up. ID consultation rates increased from 33% cases in 2002 to >80% in 2007. Overall, ID consultation was performed in 67% of SAB cases. All-cause in-hospital mortality was 21.7%, and 90-day mortality was 32.1%. Factors significantly associated with in-hospital mortality in a multivariate logistic regression analysis were comorbidity, expressed as McCabe ultimately fatal (OR 4.0, CI 2.3–6.9) or as McCabe rapidly fatal (OR 7.9, CI 2.9–21.7), initial ICU admission (OR 5.9, CI 3.6–9.7), MRSA (OR 2.7, CI 1.4–5.0), age ≥60 years (OR 2.4, CI 1.4–4.2), a diagnosis of endocarditis (OR 2.9, CI 1.4–5.8), and ID specialist consultation (OR 0.6, CI 0.4–1.0). There was no statistically significant relationship between mortality and mode of acquisition, source of bacteraemia, or presence of metastatic disease (Table 1 ). Similar results were obtained in the analysis of factors associated with 90-day mortality.
Table 1.
Univariate end multivariate analysis of inhouse mortality of 521 SAB patients
| Parameter/Risk factor | Inhouse deaths (113 of 521 patients, 21.7%) |
|||
|---|---|---|---|---|
| Univariate analysis |
Multivariate analysis |
|||
| Number (%) | p value | OR (95% CI) | p value | |
| MSSA vs. MRSA | ||||
| MSSA | 85/454 (18.7%) | <0.01 | 2.7 (1.4–5.0) | <0.01 |
| MRSA | 28/67 (41.8%) | |||
| Mode of acquisition | ||||
| community-acquired | 25/109 (22.9%) | |||
| healthcare-associated | 31/147 (21.1%) | |||
| nosocomial | 57/265 (21.5%) | 0.93 | NI | |
| Age | ||||
| <60 years | 28/204 (13.7%) | |||
| ≥60 years | 85/317 (26.8%) | <0.01 | 2.4 (1.4–4.2) | <0.01 |
| Source | ||||
| unknown or catheter-related | 74/364 (20.3%) | |||
| others | 39/157 (24.8%) | 0.25 | NI | |
| Metastatic infection | ||||
| no | 69/332 (20.8%) | |||
| yes | 44/189 (23.3%) | 0.51 | NI | |
| ID consultation | ||||
| no | 47/171 (27.5%) | |||
| yes | 66/350 (18.9%) | 0.03 | 0.6 (0.4–1.0) | 0.05 |
| Endocarditis | ||||
| no | 91/465 (19.6%) | |||
| yes | 22/56 (39.3%) | <0.01 | 2.9 (1.4–5.8) | <0.01 |
| Comorbidity | ||||
| McCabe non-fatal | 25/239 (10.5%) | |||
| McCabe ultimately fatal | 77/258 (29.8%)a | <0.01 | 4.0 (2.3–6.9)a | |
| McCabe rapidly fatal | 11/24 (45.8%)a | 7.9 (2.9–21.7)a | <0.01 | |
| Initial ICU admission | ||||
| no | 40/335 (11.9%) | |||
| yes | 73/186 (39.2%) | <0.01 | 5.9 (3.6–9.7) | <0.01 |
OR, odds ratio; CI, confidence interval. NI, not included in final regression model.
Compared to McCabe non-fatal.
Conclusion: These data suggest that outcomes of both community-onset and nosocomial bloodstream infections due to S. aureus may be improved by an expert consultation service. The factors most critical for better outcomes and modifiable in time by ID specialist consultation remain to be determined and may be explored as process of care quality indicators.
O180 Nosocomial, community and healthcare-associated bloodstream infections in Spain
P. Retamar*, J. Rodríguez-Baño, M.D. López-Prieto, M.M. Portillo, F Rodríguez, M.V. García, M. Herrero, F. Fernández, A. Muñoz, A. Sánchez, B. Becerril, A. Martín, J.C. Alados, R. Moya, C. Florez, L. León, T. Escobar, A. Arroyo and SAEI/SAMPAC
Objectives: Health care-associated (HCA) bloodstream infections (BSI) has been proposed as a new subclass of community-acquired (CA) BSI in USA. There are scarce data from other health care systems. We analysed the epidemiology and clinical features of bacteraemia according to acquisition in Andalucía, Spain.
Methods: A prospective multicentre cohort study including of all BSI episodes in 15 public hospitals (11 tertiary, 4 community) from Andalucía, Spain, from November 2005 throughout March 2006, was performed. BSI were classified as nosocomial (NOS), HCA or CA according to Friedman's criteria (Ann Intern Med 2002). Etiology, epidemiologic and clinical data were collected.
Results: 822 episodes of BSI were included: 476 (58%) were NOS, 227 (28%) HCA, and 119 (14%) CA. Chronic renal failure and liver disease were more frequent in HCA than in NOS (23% vs 9%, p < 0.001; and 13% vs 7%, p = 0.004); renal failure, cancer, and immunodeficiency were also more frequent in HCA than in CA. Venous catheter was more frequent in NOS than in HCA (87% vs 41%, p < 0.001). Urinary catheter use was similar in HCA and in CA (13% vs 13%, p = 0.9). The most frequent sources in NOS, HCA and CA were: unknown (27%, 23%, 14%), venous catheter (25%, 2%, 0), urinary tract (15%, 21%, 31%), gastrointestinal tract (14%, 21.6%, 22.2%), and respiratory tract (12%, 11%, 19%). The most frequent organisms in NOS, HCA and CA BSI were: Escherichia coli (20%, 37%, 36%), Streptococcus pneumoniae (1%, 6%, 18%), coagulase-negative staphylococci (CNS) (14%, 10%, 5%), Staphylococcus aureus (14%, 11%, 7%), and Pseudomonas aeruginosa (6%, 7%, 1%). Methicillin-resistant S. aureus (MRSA) was found in 3%, 5% and 0% of the episodes. Empirical treatment was appropriate in 69%, 81% and 84%, and mortality at day 14 was 20%, 19% and 15%, respectively.
Conclusion: There were significant differences between HCA and COM episodes. MRSA, CNS or P. aeruginosa caused BSI with similar frequency in NOS and HCA episodes, but were rare in COM BSI. HCA BSI should be considered as a distinct class within CA also in Spain.
O181 The value of FDG-PET for detection of metastatic infectious foci complicating Gram-positive bacteraemia
F. Vos*, C. Bleeker-Rovers, P. Sturm, B.J. Kullberg, W. Oyen (Nijmegen, NL)
Objectives: Timely detection of metastatic infectious foci in Gram positive bacteraemia is crucial, because they often require prolonged antibiotic treatment or drainage. Diagnosis of complicating infectious foci is difficult, since up to 32% of these foci do not have localising symptoms and signs.
Methods: A prospective, descriptive analysis with a matched historical control group was performed. All non-neutropenic, adult patients having positive blood cultures growing S. aureus, Streptococcus species or Enterococcus species were eligible when at least one risk factor for the presence of complicating infectious foci was present. FDG-PET was performed within 2 weeks after the first positive blood culture.
Results: The results of 115 study patients and 230 control patients were analysed. Significantly more metastatic foci were found in study patients. FDG-PET was the first to delineate infectious foci in 35 patients. Sensitivity and specificity of FDG-PET were 100% and 87% respectively. The NPV was 100% with a PPV of 89%. Relapse rates decreased from 7.4%to 2.6%, p = 0.09, and from 8.9%to 1.4% in the S. aureus subgroup (P = 0.038). Infection related mortality decreased from 24% to 15% after 6 months, (p = 0.049).
Conclusion: Addition of FDG-PET to the diagnostic work-up of patients with Gram positive bacteraemia with at least one additional risk factor for developing metastatic infection results in both a decrease relapse rates, which is significant among patients with a Staphylococcus aureus bacteraemia and lower mortality rates. FDG-PET is a valuable technique in the diagnostic work-up of all high risk patients with Gram positive bacteraemia.
O182 Incidence of zoonotic Salmonella species bacteraemia: a multi-national population-based study
K. Laupland*, H. Schonheyder, O. Lyytikämen, L. Valiquette, K. Kennedy, P. Collignon on behalf of the International Bacteraemia Surveillance Collaborative
Objectives: Although zoonotic (non-typhoidal) Salmonella species are important causes of invasive infections worldwide, few studies have investigated their epidemiology at the population level. The objective of this study was to define the incidence of zoonotic Salmonella species bacteraemia in a large multi-national population and to evaluate temporal and regional differences.
Methods: Population-based laboratory surveillance for all zoonotic Salmonella species bacteraemias was conducted in five regions (Finland, Canberra, Australia, North Jutland Region, Denmark, and Calgary and Sherbrooke, Canada; combined population 7.5 million residents annually) during 2000–2007.
Results: A total of 480 zoonotic Salmonella species bacteraemias were identified for an overall annual incidence of 8.1 per million population. The incidence was lowest in the spring and highest in the summer, and progressively increased during the eight years of the study with a doubling of the rate from 6.1 per million in 2000 to 12.2 per million in 2007. Overall the acquisition risk increased with advancing age and males were at significantly higher risk as compared to females (10.2 vs. 6.2/million; relative risk 1.7; 95% confidence interval 1.4–2.0). The occurrence varied significantly among the five study regions with annual incidence rates per million population of 22.2 in Sherbrooke, 18.7 in North Jutland Region, 7.5 in Finland, 6.1 in Calgary, and 4.2 in Canberra.
Conclusions: Zoonotic Salmonella species bacteraemias are increasing. The determinants of increased risk among males, older individuals, and between regions merit further investigation.
Tuberculosis
O184 Dominance of Beijing family strains in XDR tuberculosis in Samara Oblast, Russian Federation
V. Nikolayevskyy*, Y. Balabanova, N. Malomanova, I. Fedorin, T. Simak, I. Kontsevaya, O. Ignatyeva, S. Mironova, Y. Mashkova, A. Naumov, A. Kovalev, A. Shakhmistova, F. Drobniewski (London, UK; Samara, RU)
Objectives: Russian Federation is of one of the WHO-defined high tuberculosis (TB) incidence countries with high prevalence of multidrug resistant TB (MDRTB). Significant associations between MDRTB and Beijing family strains have been reported for many regions in the Russian Federation. In Samara oblast (Central Russia) converging HIV and TB epidemics, including MDRTB and extensively drug resistant TB (XDRTB) pose a significant public health problem. The aim of the study was to characterise transmission of XDRTB in Samara oblast using molecular tools.
Methods: A total of 189 individual XDR M. tuberculosis strains isolated from patients between January-September 2008 in Samara were genotyped using spoligotyping and multilocus VNTR typing using an extended 24-loci panel (Supply et al., 2006) supplemented by an additional panel of hypervariable loci (VNTR 3232, 1982, 2163A, 3336) specifically for differentiation within highly conserved groups. First and second line drug susceptibility tests (DST) were performed using standardised protocols (Kruuner et al., 2007); mutations associated with resistance to rifampicin (RIF) and isoniazid (INH) were detected using a non-commercial reverse hybridisation assay (Brown et al., 2006).
Results: Mutations responsible for resistance to RIF and INH were detected in 187 (98.9%) and 185 (97.9%) strains demonstrating excellent agreement between phenotypical and molecular DST results. Beijing strains dominated comprising 92.6% with minority of strains (7.4%, N = 13) belonging to other modern TB lineages including LAM9, Haarlem 3, T1, T4, and Family 33. Multilocus VNTR typing allowed the differentiation of Beijing strains into 43 types although clustering rates remained substantial (82.3%) indicating high rates of active drug resistant TB transmission. Five major clusters within the Beijing family included 130 isolates (74.3% of a total; clone size varied from 4 to 78 strains) with four clusters being indistinguishable with those identified in Samara oblast in 2002–2004 suggesting that a limited number of emerging Beijing clones is responsible for an MDR and XDRTB transmission in Samara oblast.
Conclusions: VNTR genotyping using highly discriminative loci including MIRU26, VNTR3232, 1982, and 4052 allowed the differentiation of strains within the Beijing family. XDRTB in Samara is associated with a limited number of expanding Beijing family M. tuberculosis clones.
O185 Rapid detection of Mycobacterium tuberculosis and rifampin-resistance from sputum samples with an easy-to-use PCR test system with near-patient capability
M. Jones*, D. Helb, E. Story, C. Boehme, E. Wallace, K. Ho, J. Kop, M. Owens, R. Rodgers, P. Banada, H. Safi, R. Blakemore, N. Lan, E. Jones-López, M. Levi, M. Burday, I. Ayakaka, R. Mugerwa, B. McMillan, E. Winn-Deen, L. Christel, P. Dailey, M. Perkins, D. Persing, D. Alland (Sunnyvale, Newark, Bronx, US; Geneva, CH; Ho Chi Minh City, VN; Kampala, UG)
Background: Current nucleic acid amplification methods used to detect Mycobacterium tuberculosis are complex, labour-intensive and technically challenging. The Xpert™ MTB real-time PCR assay was developed to overcome these limitations and to rapidly and simultaneously detect M. tuberculosis and rifampin resistance-associated mutations in sputum samples with minimal hands-on effort. Sample processing and real-time nested PCR reactions are integrated in a single, disposable plastic cartridge which contains all of the reagents necessary for sample processing and PCR reactions so that the technician need only add the sample to the cartridge. All steps following sample addition are done automatically on the GeneXpert platform in less than 2 hours.
Objective: The objective was to evaluate the Xpert™ MTB assay sensitivity and specificity for both M. tuberculosis detection and rifampin resistance.
Methods: Analytical studies were performed using sputum spiked with known numbers of M. tuberculosis colony forming units (cfu). Clinical studies were performed with sputum samples from tuberculosis patients in Uganda and Vietnam.
Results: The limit of detection for M. tuberculosis in sputum samples was 131 cfu/mL. As few as ten cfu of M. tuberculosis could be detected in 35% of the samples. All common rifampin-resistance-associated mutations could also be detected. Analysis of samples collected from suspected tuberculosis cases in Vietnam and Uganda showed a sensitivity of 98–100% for smear-positive sputum samples. Sensitivity in smear-negative samples was 84.6% (33/39) when M. tuberculosis was identified by solid media culture, and 71.7% (38/53) when both solid and liquid media were used for identification. Specificity was 100% in all cases. Tests of 64 smear-positive samples collected from retreatment tuberculosis cases in Uganda showed a sensitivity of 100% for detecting rifampin-resistance. Specificity for rifampin-resistance was 98% (63/64), but this rose to 100% after correcting for an error in conventional susceptibility test results.
Conclusions: The Xpert™ MTB Assay is highly effective at detecting smear-positive and smear-negative tuberculosis and rifampin-resistance. This simple-to-use system can perform point-of-care detection of M. tuberculosis directly from sputum in less than two hours.
O186 Drug-resistant tuberculosis: quantitative drug susceptibility testing and correlation with genotyping
B. Springer, K. Lucke, R. Calligaris-Maibach, C. Ritter, E. Boettger* (Graz, AT; Zurich, CH)
Objective: Worldwide, the present tuberculosis epidemic is characterised by an alarming emergence in drug resistance. Given the limited therapeutic options in MDR (and especially XDR) tuberculosis, there is a need to define the resistance levels and mechanisms present in clinical isolates categorised as drug resistant on the basis of critical concentration testing, so as to facilitate rapid therapeutic decisions.
Methods: We determined quantitative resistance levels of drug resistant isolates of Mycobacterium tuberculosis sampled in Switzerland over the past 3 years. Resistance-conferring genetic alterations were identified by probe assays and PCR-mediated gene sequencing.
Results: Rifampicin resistant isolates unanimously showed a high-level resistant phenotype (>50 mg/L) associated with mutations in rpoB. In contrast, a significant fraction of clinical TB isolates categorised as isoniazid resistant on the basis of critical concentration testing showed a low-level resistant phenotype (mostly mutations in inhA); heterogeneous phenotypic resistance levels were associated with mutations in katG. One third of streptomycin resistant clinical isolates had a low-level resistance phenotype (<10 mg/L). Ethambutol resistance occurred mostly in MDR strains and was linked to alterations in embB, but resistance never exceeded 25 mg/L.
Conclusions: Our data indicate that some first line agents may be considered as therapeutic treatment option despite in vitro resistance at the critical concentration. Diagnostic mycobacteriology would benefit from standardised measures of quantitative drug susceptibility testing in particular for those drugs were significant variations in phenotypic resistance levels are found in clinical isolates, e.g. isoniazid, ethambutol and streptomycin.
O187 Impact of XDR-TB on treatment outcome of patients with MDR-TB
P. Tabarsi*, P. Baghaei, M. Marjani, M. Amiri, M. Masjedi, J. Caminero (Tehran, IR; Las Palmas, ES)
Design: The very limited experience treating patients with extensively drug-resistant tuberculosis (XDR-TB) shows a therapeutic success rate under 50 to 60% and there are not publications regarding the outcome of these patients treated with standardised regimes.
Material and Methods: All MDR-TB patients hospitalised at Masih Daneshvari Hospital in Tehran, Iran during 2004–2007. A drug susceptibility to 13 drugs (included 8 second line drugs – SLD) were performed and a standardised regimen with ofloxacin, cycloserine, prothionamide, and amikacin was administered. Outcome of the patients was studied, comparing between the MDR-TB non XDR-TB and the XDR-TB.
Results: 51 patients were included, 12 with XDR-TB criteria. XDR-TB infection was significantly only associated with age (p = 0.039). The success rate for the 51 total MDR-TB, the 39 MDR-TB non XDR-TB and the 12 XDR-TB patients was 76.5% (39 patients), 87.2% (34 patients) and 41.6% (5 patients), respectively. Resistance to Ofloxacin, Ciprofloxacin, and Amikacin, were found to have statistically significant association with unsuccessful outcome.
Conclusions: In this setting, a standardised SLD regimen produces high treatment success rates in MDR-TB patients unless XDR-TB is present.
Introduction
Contemporary issues in varicella zoster virus infections
S188 Varicella zoster virus encephalitis and cerebral vasculitis
T. Bergström* (Gothenburg, SE)
Recent advances in the diagnostics of varicella zoster virus (VZV) infections have changed the perception of this virus as a CNS pathogen. A real-time PCR method amplifying a 70 nt segment of the VZV gB region gave 0.5 log improved sensitivity over conventional PCR and was employed for routine diagnosis of VZV DNA in samples of cerebrospinal fluid (CSF). In addition, a new ELISA method for detection of antibodies in the CSF to glycoprotein E was developed, using a mammalian cell expression system for optimal glycosylation of the antigen. These methods were utilised for studies of VZV-induced CNS infections.
In a retrospective study, almost all patients had a reactivated VZV infection, but only 60% showed skin lesions. The following diagnoses were made: acute aseptic meningitis (AAM), n = 34; encephalitis, n = 22; meningoencephalitis, n = 6; cranial nerve affections, n = 20; encephalopathy, n = 5; and cerebrovascular disease, n = 6. In 66 patients in whom VZV DNA levels were determined, significantly higher viral loads were found in those with AAM and encephalitis compared to patients with cranial nerve affection (including Ramsay Hunt syndrome). Of the 50% (n = 50) who had a follow-up, 50% (n = 25) had neurological complications after 3 months. Sixty-two percent had a CT/MRI scan of the brain performed and 46% of these had pathological findings.
VZV encephalitis showed a more broad disease spectrum as compared with herpes simplex encephalitis (HSE), as will be presented. Detection of intrathecal synthesis of VZV gE antibodies was positive in the VZV encephalitis patients, as well as in some of the HSE patients, arguing for a previous suggested role for VZV as a co-pathogen at least in some cases of the latter disease.
VZV vasculitis was a more common finding (6% of all cases) than expected from the literature of case reports. MR findings showed that middle and posterior cerebral arteries were targeted. Surprisingly, despite substantial VZV DNA loads in the CSF of these patients, investigated serum samples were PCR negative. Thus, VZV might be suggested to be neuronally transported to the arterial walls rather than haematogenously spread.
Conclusions: VZV is a serious and underestimated cause of CNS infection. A substantial number of the patients presented with serious neurological symptoms and sequela, and pathological findings on CT/MRI of the brain were abundant, especially in patients with encephalitis and vasculitis.
PK/PD controversies for the clinician
S190 PK/PD and azoles
W. Hope* (Manchester, UK)
The triazoles have revolutionised the treatment of invasive and allergic fungal diseases. Fluconazole, itraconazole, voriconazole and posaconazole are available for clinical use. Isavuconazole and ravuconazole are in development. The triazoles have broad spectrum antifungal activity. The pharmacokinetics and pharmacodynamics (PK-PD) of the triazoles have been extensively investigated in murine models of disseminated candidiasis. The PD parameter that optimally links drug exposure with the observed antifungal effect is the ratio of the area under the concentration-time curve (AUC) to MIC (AUC:MIC). There is increasing information on the magnitude of the AUC:MIC that is required for optimal antifungal effect. PK-PD principles have been used to define in vitro susceptibility breakpoints. The triazoles are fungistatic against Candida spp. Their mode of action against Aspergillus spp. is less well defined, although they clearly exhibit dose-dependant decrement in fungal burden in laboratory animal models of invasive pulmonary aspergillosis. The triazoles accumulate in tissues and this is important for an understanding of their antifungal effect.
In humans, the triazoles are characterised by complicated pharmacokinetic properties. Both itraconazole and voriconazole exhibit nonlinear pharmacokinetics. The triazoles all exhibit clinically relevant exposure-response relationships. Recent work from our laboratory suggests that itraconazole exhibits clinically relevant concentration-toxicity relationships. Higher concentrations of voriconazole are associated with a progressively higher probability of hepatotoxicity, photopsia and central nervous system toxicity.
Because of the significant pharmacokinetic variability and clinically relevant drug exposure-response relationships, therapeutic drug monitoring (TDM) is frequently used. A strong argument can be made for the routine monitoring of itraconazole and voriconazole. There may also be grounds to consider monitoring posaconazole levels. TDM should be considered for all patients receiving triazoles who have refractory disease. Furthermore, TDM should be considered when compliance, drug interactions and variable pharmacokinetics result in uncertainty about resultant drug exposures.
An understanding of the PK-PD relationships of the triazoles has been instrumental in optimising their clinical efficacy.
Innate immunity
S192 The inflammasomes: danger sensing complexes triggering innate immunity
J. Tschopp* (Lausanne, CH)
The NOD-like receptors (NLR) are a family of intracellular sensors of microbial motifs and ‘danger signals’ that have emerged as being crucial components of the innate immune responses and inflammation. Several NLRs (NALPs and IPAF) form a caspase-1-activating multiprotein complex, termed inflammasome, that processes proinflammatory cytokines including IL-1beta. Amongst the various inflammasomes, the NALP3 inflammasome is particularly qualified to sense a plethora of diverse molecules, ranging from bacterial muramyldipeptide to monosodium urate crystals. The important role of the NALP3 inflammasome is emphasized by the identification of mutations in the NALP3 gene that are associated with a susceptibility to inflammatory disorders. These and other issues related to the inflammasome will be presented.
S193 Critical players in signalling control
N. Gay* (Cambridge, UK)
It is now 20 years since Charles Janeway hypothesized the existence of clonally derived pattern recognition receptors and pointed to the importance of these in initial responses to bacterial and viral infections. Janeway's hypothesis has been validated by the discovery of three groups of PRRs. First, are the Toll-like receptors which detect microbial lipids and non-self nucleic acids at the cell surface an in intracellular compartments. In addition cytoplasmic sensors of bacteria (NODs) and of viral nucleic acids (RIGs) have also been characterised. As well as being critical for responses to infections, these PRRs also underlie a large burden of autoimmune and inflammatory disease in the human population and are thus important targets for therapy.
In my talk I will describe the molecular mechanisms by which these conserved pathogen associated moecules are recognized by the TLRs with particular reference to lipo polysaccharide and single stranded viral RNAs. I will also present new results which show how receptor activation is coupled to downstream signal transduction and in particular the role played by oligomeric signaling platforms assembled form adaptors and other signaling molecules involved in the pathway. I will discuss the potential for structural analysis to be used in the rational design of new drugs.
The year in infection control
S195 The year in infection control
M. Struelens* (Brussels, BE), D. Pittet* (Geneva, CH)
This session proposes a critical review of the most salient recently published papers in the field with a special focus on control of multi drug-resistant organisms, prevention of infections in the intensive care unit, surgery etc. and highlights the need for validity/scope assessment. It emphasizes also the importance to prioritise information published in the abundant literature available so as to be able to summarise and understand the potential changes in clinical practice, and identify unresolved issues and areas of possible future clinical research.
Infectious diseases on the move
S199 Travellers and tourists from Latin America
R. Isturiz* (Caracas, VE)
Tourism is Europe's face to the world. It is also a major source of revenue, employment and productivity. Each year over 450 million arrivals are recorded into the continent, and of those, approximately 4 million are from Latin America. Returning travelers are even more numerous and more often associated with disease transmission into Europe.
Within countries of the European continent, imported cases of environmental and zoonotic illnesses such as cholera, dengue, malaria, viral haemorrhagic fevers and West Nile virus infections are a rare but established fact. Diseases imported from Latin America with the potential for autochthonous transmission (chikungunya, malaria, yellow fever) and or high infectivity (viral haemorrhagic fevers) will be described in detail and the possibility of European outbreaks from Latin American countries will be discussed. The importance of early clinical recognition of individual cases and prevention of spread to large populations make this discussion relevant in 2009.
External migration to European has been responsible for impoverished outskirt areas, where cases of tuberculosis and food and waterborne diseases have increased, but the role of immigrants from Latin America seems less that that of African countries.
The returning European traveler poses infrequent but important challenges to clinicians and epidemiologists; the risk of travelers from Europe to Latin America of acquiring, incubating, suffering and transmitting Yellow Fever, Dengue, Malaria, Leptospirosis, Chagas Disease, Meningococcal disease, TB, Measles, Varicella, Rabies, Traveler's Diarrhoea, HIV, Cysticercosis, Leishmaniasis, or a multiresistant bacteria, as well as the vaccination and behavioural strategies to prevent them will be discussed.
The overall patterns of communicable diseases in Europe have not been noticeably affected by travelers and tourists from the Latin American region, and the opposite is also probably true, but the wide range of diseases with different modes of transmission and with different relevance for European Public Health and individual practitioners would require closer monitoring of imported cases to uncover minimal trends.
News from the tropical front
O200 Clinical and epidemiological study of imported Chagas disease in Madrid, Spain
A. Pérez de Ayala, F. Norman, J.A. Pérez-Molina, J.M. Herrero, B. Monge, M. Navarro, R. López-Vélez* on behalf of RICET
Objectives: Description of epidemiological and clinical characteristics of a cohort of Latin American immigrants in Madrid diagnosed with Trypanosoma cruzi infection.
Methods: All Latin American immigrants attended at the Tropical Medicine Unit of the Ramon y Cajal Hospital between January 2003 and December 2008 were tested for T. cruzi infection. Diagnosis was considered when two different serological tests (IFAT and ELISA) were positive, PCR was also performed. A clinical/epidemiological protocol was performed for all positive patients. An ECG, echocardiogram and oesophageal manometry was performed in all asymptomatic patients and cardiac MRI, barium swallow or barium enema if specific symptoms were present. Treatment with benznidazole (5 mg/kg/d/60 days) was given to all infected patients. An estimation of the potential number of chagasic cardiomyopathies in Spain was calculated taking into account the number of Latin Americans registered and the infection prevalence rates in their countries of origin.
Results: A total of 710 patients were analyzed for T. cruzi infection: 196 (27.6%) were positive. Most of them (95.9%) were Bolivians, 69.4% women, with a mean age of 36 years. Regarding possible transmission routes, 83.7% had seen the vector in their houses, 12.2% had received a blood transfusion in their country of origin, and in 12.8% of cases vertical transmission was suspected (mother with positive test, although 42.3% maternal test results were not available). 60 patients (30.6%) were still under clinical study and 136 had a completed clinical evaluation: 93 patients (68.3%) were in the indeterminate form of the disease and 43 (31.6%) had chronic Chagas disease: 37 (27.2%) with cardiac involvement, 4 (2.9%) with digestive involvement and 2 (1.4%) with both. 90 patients had received antitrypanosomal treatment: 35 (38.8%) had adverse side effects, and 18 of them (20%) stopped treatment because of cutaneous intolerance: The main side effects were cutaneous hypersensitivity, observed in 28 patients (31.1%), gastrointestinal symptoms in 9 (10%), perifheral polyneuropathy in 2 (2.2%) and transitory leucopenia in one patient (1.1%).
An estimated 29,500 cardiomyopathies may occur in adult Latin American immigrants in Spain in the near future.
Conclusions: Chagas disease has now become a public health problem in European countries receiving a large proportion of Latin American immigrants.
O201 Double-blind, randomised controlled trial, to evaluate the effectiveness of a controlled nitric oxide releasing patch versus meglumine antimoniate in the treatment of cutaneous leishmaniasis
R.G. García*, M. Rincón Acelas, S.Y. Silva, M. Lopez, I.D. Velez, D. Smith, H. Mosquera, C. García, J.P. Lopez Jaramillo (Floridablanca, Medellín, Bucaramanga, CO; Ohio, US)
Cutaneous Leishmaniasis (CL) is a worldwide disease, endemic in 88 countries, that has shown an increasing incidence over the last two decades. So far, pentavalent antimony compounds have been considered the treatment of choice, with rates of curing close to 85%. However, the high efficacy of these drugs is counteracted by their adverse events. Recently, in vitro and in vivo studies have shown that NO plays a key role in the eradication of the leishmania parasite
Objective: To determine whether a NO donor patch (developed by electrospinning technique) is as effective as meglumine antimoniate in the treatment of CL while causing less adverse events
Methods: A double-blind, randomised, placebo-controlled clinical trial was conducted with 178 patients diagnosed with CL in Santander, Colombia, South-America. The patients were randomly assigned to two groups. During 20 days Group 1 received simultaneously meglumine antimoniate and placebo of nitric oxide patches while Group 2 received active nitric oxide patches and placebo of meglumine antimoniate. Biochemical determinations (aspartate aminotransferase, alanine aminotransferase, creatinine and pancreatic amilase) were measured at he beginning and at the end of the treatment. A follow up was realised 21, 45 and 90 days after the beginning of the treatment
Results: The study included 69 (38.77%) women and 109 (61.23%) men. The average age in group 1 was 30.80± 14.23 years; while in group 2 it was 27.88± 13.79 years. Clinical and demographic data were similar in the two groups. After the follow up period, the complete clinical healing of Group 1 was 94.81% versus 37.14% for Group 2 (p = 0.0001). Treatment with NO patches generated both, a lower frequency of non-serious adverse events (fever, anorexia, myalgia, arthralgia, headache), and a reduced variation in biochemistry determinations (ASAT 26.93±8.61 vs 41.02 ±27.87UI p = 0.99; ALAT 25.05±8.79 vs 39.06 ± 35.89UI p = 0.001 and Amylase 77.13±21.1 vs 90.87±34.62UI p = 0.0008)
Conclusions: The treatment with NO patches resulted in a lower percentage of complete clinical response compared with meglumine antimoniate. Despite its inferior effectiveness, the safety, the lower frequency of adverse events, the facility of administration (topical) and the low cost of the patches justifies its evaluation in further poblational studies, especially in populations as the Colombian ones, where the serious adverse events due to glucantime have increased dramatically.
O202 First documented outbreak of human trichinellosis in Taiwan: association with soft-shelled turtles
Y.C. Lo*, D.S. Jiang, C.H. Chiu (Taipei, TW)
Objectives: Trichinellosis is a zoonotic disease which has never been reported in Taiwan and is rarely linked to consumption of reptiles. We investigated the first documented outbreak of trichinellosis in Taiwan consisting of 8 patients who became acutely ill after eating at the same restaurant in May 2008.
Methods: We conducted a retrospective cohort study by interviewing the patients and persons who ate together with them. A case was defined as illness in an attendee who had fever (>38.0°C) or myalgia ≤4 weeks after the festivals and was seropositive to Trichinella antigen using an enzyme-linked immunoassay and immunohistochemical staining. Environmental study of the soft-shelled turtle farm was performed.
Results: Of the 23 attendees, 8 persons met the case definition (attack rate = 35%). The most common presenting symptoms were myalgia (88%), fever (88%), and periorbital swelling (38%). All 8 patients sought medical care; five were hospitalised. Of the 7 patients who underwent blood test, all had moderate eosinophilia. All 8 patients' serum samples were strongly reactive to Trichinella excretory-secretory antigen. The only food item significantly associated with illness was the raw soft-shelled turtle meat (relative risk undefined; p = 0.005). Traced back to the farm, histological examination of soft-shelled turtles was negative for Trichinella species.
Conclusion: The most likely cause of this outbreak was consumption of raw soft-shelled turtle served in the festivals. This investigation indicates Taiwan is not free of trichinellosis. Prevention and control programs of trichinellosis should be established. The public should be aware of the risk of acquiring trichinellosis from consumption of raw soft-shelled turtle.
O203 Rapid five-minute Giemsa staining for detection of malaria parasites in blood smears
M. Jager*, R. Pique, C. Vandenbroucke-Grauls, T. Hekker (Amsterdam, NL)
Objective: To develop and evaluate a modified, rapid Giemsa staining procedure for detection of malaria parasites in blood smears. Disadvantage of the rapid commercially available staining methods is that they require highly experienced technicians for interpretation of results because the interpretation can be difficult. For this reason, many laboratories use the Giemsa stain. Shorter Giemsa staining times have been reported previously, however, to our knowledge, the effect of 5 and 10 minute staining in different Giemsa dilutions have not been evaluated.
Methods: The stock solution of Giemsa stain (Merck, Darmstadt, Germany) was used in different dilutions (1:10 and 1:5) and incubated for different lengths of time (10 min and 5 min). The staining effect was compared to our standard Giemsa stain (1:40, 45 min). Sensitivity was determined by examining smears of P. falciparum from fresh and EDTA blood. The level of parasitaemia was followed in two patients admitted to our hospital with P. falciparum parasitaemia's of 21.5% and 28.8% (see table; patient A and B) by examination of blood smears taken at different time points after initiation of therapy. These samples were used to evaluate the different Giemsa dilutions and staining times. Smears were read by three independent observers (a clinical microbiologist, a laboratory technician specialised in parasitology, and a resident in clinical microbiology).
Results: In the table results of the three staining methods on blood from two patients from Ghana with high parasitaemia's on admission and during follow-up are shown. All smears were equally easy to read and yielded parasite counts within internationally accepted ranges of variation (see United Kingdom National External Quality Assessment Service).
Conclusion: Staining blood smears for detection of Plasmodium falciparum parasites with a 1:5 dilution of Giemsa stain for five minutes provides easy to read slides and results comparable to those obtained with the standard Giemsa staining. Advantage of the rapid method is the shorter turnaround time, disadvantage is the larger amount of stain used.
O204 Innovation in diagnosis of gastrointestinal protozoan parasites
S. Gross, V. Hurgin*, J. Kopelowitz, O. Babai, A. Hananel, V. Sasson, Z. Greenberg (Ashdod, IL)
Objectives: Diarrhoeal diseases are common in developed and developing countries and are major causes of morbidity and mortality worldwide. The need to differentially diagnose protozoan parasites versus other gastrointestinal (GI) aetiologies is well recognized. The most common GI protozoan parasites infecting humans worldwide are considered to be Entamoeba histolytica, Giardia lamblia, Blastocystis hominis, Dientamoeba fragilis and Cryptosporidium spp. Laboratory detection of these parasites is relying on microscopic analysis of stool samples and water concentrates, as well as enzyme immunoassay (EIA) tests. Utilising the microscopic examination usually results in underdetection of GI parasites, while usage of EIA is often not cost-effective.
Methods: Savyon Diagnostics is currently engaged with developing an approach aiming to address the unmet needs and the current limitations in this field. This approach includes 3 major aspects: (1) the ability to detect a panel of all the above 5 organisms in one test kit, (2) the possibility to perform the diagnosis in two steps – first, simultaneous detection of these organisms without distinguishing between the different species for screening of large number of specimens, and second, distinctive detection of the specific aetiology in the positively-found specimens, and (3) the ability to apply EIA diagnosis in formalin-preserved specimens for all the mentioned parasites.
Results: Polyclonal antibodies were produced in-house based on native antigen extracts, recombinant antigens and synthetic peptides. The resulted inventory of antibodies enabled finding the optimal combination that provided the desired performance parameters for separate detection of each of the parasites in fresh, frozen or formalin preserved faeces specimens. The analytical limit of detection and the performance in characterised clinical specimens were comparable to microscopy or to reference EIA, when available. The results show unique detection of E. histolytica in formalin-preserved specimens, which is comparable to detection in fresh specimens.
Furthermore, we demonstrate simultaneous detection of the parasites without compromising performance characteristics in fresh or preserved specimens.
Conclusions: The presented work is a paradigm of an innovative approach, expected to advance the diagnosis of protozoan parasites in GI patients, thus, enabling appropriate and cost-effective diagnosis and treatment.
Bacterial biofilm: from formation to treatment
O205 Biofilm formation during tumour colonisation by Salmonella typhimurium
K. Kochrübe*, K. Westphal, H. Lössner, M. Rhode, K. Wolf, S. Weiss (Braunschweig, DE)
Objectives: Systemic administration of certain facultative anaerob bacteria to mice bearing solid tumours leads to accumulation in tumours compared to normal target organs, like spleen and liver, and to retardation of tumour growth. Salmonella enterica serovar Typhimurium (S. typhimurium) as well as Escherichia coli 1917 Nissle (EcN) are such bacteria. Preliminary experiments showed that such bacteria that exhibit the ability to form biofilms in vitro might also do so in tumours. In the present study this was systematically investigated.
Methods: Biofilm formation of bacteria were detected on low-salt biofilm plates. Additionally, Salmonella- or E. coli-infected CT26-tumours of BALB/c mice that were left untreated or were treated with anti-Gr1 to deplete neutrophilic granulocytes were removed two days post infection, fixed and prepared for electron microscope analysis. The expression of different genes which are probably involved in the biofilm formation were tested via Real-time PCR.
Results: When examined after colonising tumours S. typhimurium SL7207 and SL1344 as well as EcN are almost exclusively found extracellular although they are able to invade the CT26 cells in vitro. Interestingly, like in vitro all three bacteria form biofilms to various extend when residing in the tumours. This was followed in more detail for S. typhimurium SL7207. Biofilms were not formed by SL7207 when neutrophils had been removed by antibodies. In addition, when ardA a central switch for biofilm formation in the Salmonellla had been deleted no biofilms could be found. Importantly, now bacteria could be found intracellularly most likely in neutrophilic granulocytes.
Conclusion: The formation of biofilms by facultative anaerobic bacteria when residing in solid tumours is a novel and surprising finding. When neutrophils were removed, no biofilms are formed, while uptake into neutrophils is allowed when the ability of the bacteria to form biofilms was blocked. Hence, it appears that the bacteria use biofilm formation as a defence system against the immune system of the host.
O206 RamR: a dual regulator of antibiotic susceptibility and biofilm formation in Klebsiella pneumoniae Kp342
J. Findlay, T. Schneiders* (Edinburgh, UK)
Objectives: RamA is an AraC/XylS family transcriptional activator found in Klebsiella pneumoniae, Salmonella spp. and Enterobacter spp., the overexpression of which is associated with an MDR phenotype. Recently a tetR-like gene that lies upstream of ramA, known as ramR, has been identified as a repressor of ramA. K. pneumoniae Kp342 is a diazotrophic endophyte strain which has been reported to exhibit notable resistance to antibiotics. Despite its MDR phenotype Kp342 has been shown to exhibit attenuated pathogenicity in mouse models in comparison to clinical K. pneumoniae strains. The aims of this study were to: determine the levels of ramA expression and establish its role in Kp342's MDR phenotype; determine the effect of ramR complementation on ramA expression and antibiotic susceptibility.
Methods: Genome and sequence analysis performed in K. pneumoniae strain Kp342 demonstrated a 96 bp deletion within the ramR gene. Cloning and complementation with full size wild type ramR was performed in Kp342 (hereby known as Kp342/ramR). RT-PCR was used to assess levels of gene expression which were subsequently quantified using Bio-Rad Quantity One software. MIC testing was performed against chloramphenicol (Cm), norfloxacin (Nor) and tetracycline (Tet) according to BSAC guidelines. Biofilm formation was measured using a modified protocol of O'Toole and Kolter.
Results: Kp342 containing the mutated ramR gene (96 bp deletion) was shown to overexpress ramA and the putative outer membrane protein romA. Complementation of the ramR gene resulted in the repression of both ramA and romA transcription by 3–4 fold. Interestingly, the ramR complemented strain demonstrated increased biofilm formation (up to 9-fold increase) over a 72 hour period in both LB and M9 medium after static growth at 37°C. MICs of the tested antibiotics were reduced up to 16-fold in Kp342/ramR compared to the ramR mutated Kp342.
Conclusions: This result demonstrates that ramR acts as a repressor of both ramA and putative outer membrane protein romA thereby increasing its susceptibility to antibiotics. However the restoration of a functional ramR in Kp342 also increases biofilm formation significantly, suggesting that ramR plays a role in the regulation of biofilm formation genes and possibly bacterial virulence.
O207 In vitro effect of different classes of antibiotics on viable mass and matrix of Staphylococcus aureus and Pseudomonas aeruginosa biofilms
K. Toté*, M. Deschacht, T. Horemans, D. Vanden Berghe, L. Maes, P. Cos (Antwerp, BE)
Objectives: Bacteria and matrix are essential for the development and maintenance of biofilms; hence, antibacterials should be tested against both components. The aim of this study was to determine class-specific inhibitory effects of different antibiotics against biofilm-forming Staphylococcus aureus (Sa) and Pseudomonas aeruginosa (Pa) strains, using in vitro discriminatory assays.
Methods: Twelve antibiotics were selected that represent different classes and mechanisms of action. For every antibiotic, MIC and MBC against planktonic microbes were determined. The antibiotics were evaluated on biofilms at concentrations ranging from 16× MBC to MIC/4. To determine the anti-biofilm spectrum of antibiotics in greater detail, tests were performed with one biofilm-producing Sa strain and two adherent Pa strains. Sa biofilms were quantified using the DMMB-resazurin test system.[1] The dye dimethylmethylene blue (DMMB) allows the specific colorimetric detection of the Sa biofilm matrix, while the fluorescent redox indicator resazurin detects the viable bacterial burden. Mature Pa biofilms were quantified using crystal violet and resazurin.
Results: Only four out of twelve antibiotics showed adequate efficacy against Sa biofilms. Rifampicin had 50% inhibitory activity on both matrix and bacteria at 16× MBC. Polymyxin B killed nearly all bacteria at 8×MBC, but leaving the matrix undisturbed. Both Pa biofilms responded differently on antibiotic treatment. Rifampicin showed highest activity against Pa viable mass with a minimum of 93% killing of microorganisms at MBC. Surprisingly, this was combined with a 90% matrix inhibition at 4×MBC for only one Pa strain. The results also showed a significant stimulatory effect of doxycycline and polymyxin B at sub MIC concentrations through an increase in bacterial population.
Conclusion: This study confirms the unusual high resistance of both Sa and Pa biofilms to several antibiotic classes as no complete biofilm destruction is achieved at concentrations higher than their MBC. Rifampicin showed the highest activity on biofilm matrix and bacteria in Sa and Pa biofilms. Results also indicated that biofilm viable mass was more susceptible to treatment than the biofilm matrix, which is mainly responsible for biofilm persistence. Further research should specifically focus on compounds destroying matrix and which can be used as an adjunct to antibiotic therapy.
O208 Immunisation against SesC reduces S. epidermidis biofilm formation
M. Shahrooei*, V. Hira, B. Stijlemans, S. Kucharikova, H. Heremans, R. Merckx, P. Van Dijck, P.W.M. Hermans, J. Van Eldere (Leuven, BE; Rotterdam, NL; Brussels, BE; Nijmegen, NL)
Objectives: Staphylococcus epidermidis is a common cause of foreign-body infections (FBI) because of its ability to form biofilms. Biofilms are very resistant to antibiotics. Active and passive immunisation against biofilm-associated bacterial antigens may be an alternative. We studied the effect of immunisation against the LPXTG protein SesC in S. epidermidis biofilms in vitro and in vivo. We previously reported that SesC is present in all S. epidermidis strains tested. SesC is mainly expressed during the early and late FBI and at a higher level in sessile cells than in planktonic cells.
Methods: We used rabbit polyclonal anti-SesC-IgGs (4 µg/ml) to study biofilm inhibition in vitro and in vivo in our rat model (50 µg IgG per rat) on 1-day old biofilms. We also vaccinated rats twice with SesC according to standard protocols. Serum samples taken at day 0 and 2 weeks after the 1st and 2nd immunisation were tested by ELISA and showed an increase in anti-SesC antibody levels. S. epidermidis strains 10b and 1457 are biofilm forming strains and have been described before. For in vitro experiments, S. epidermidis 10b or 1457 were mixed with anti-SesC-IgGs and incubated for 2 hours at 4°C. Subsequently 106 cells were added to each well. After 24 h at 37°C biofilms were washed and stained with crystal violet and OD595 was measured. For in vivo experiments, catheter fragments were pre-incubated with S. epidermidis 10b and implanted subcutaneously in each rat. After explantation, the average number of CFU was determined after 24 hrs.
Results: Our data show that rabbit anti-SesC-IgGs inhibit in vitro biofilm formation by S. epidermidis strains 10b and 1457 by 74% and 65%, respectively (n = 9). In the in vivo rat model, rabbit anti-SesC-IgGs reduced the bacteria in a 1-day old biofilm 60-fold (n = 18). Active immunisation with recombinant SesC led to a 10-fold reduction of CFU compared to control rats in 1 day-old biofilms (n = 10). After 3 days, the reduction in biofilm-associated bacteria in the immunised rats was 15-fold (n = 10) (Fig 1 .).
Fig 1.
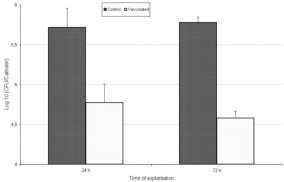
Effect of active immunisation against SesC on S. epidermidis biofilms 1 and 3 days after catheter implantation.
Conclusion: SesC represents a promising target for prevention of S. epidermidis biofilm formation. The higher effect of passive immunisation compared with active immunisation is probably due to the subcutaneous injection of anti-SesC-IgGs at the place of catheter insertion.
O209 Relative reverse-transcription real-time PCR and microscopy for studying slime production by Staphylococcus epidermidis under various physicochemical and flow conditions
A. Foka*, M. Katsikogianni, V. Chini, Y.F. Missirlis, E.D. Anastassiou, I. Spiliopoulou (Patras, GR)
Objectives: Staphylococcus epidermidis has emerged as a pathogen associated with infections of implanted medical devices impeding their long-term use. Characteristics of S. epidermidis that allow persistence of infection are the ability of bacteria to adhere to surfaces in multilayered cell clusters, followed by the production of a mucoid substance more commonly known as slime, encoded by the ica operon. The adherent bacteria and slime are collectively known as biofilm. The coupled effects of specific chemical terminal surface groups and flow conditions on slime production and biofilm formation by S. epidermidis were investigated in correlation to the expression of two genes of the ica operon.
Methods: Reference control strains (ATCC35984, slime-positive and ATCC12228, slime-negative), and two clinical strains isolated from different hospitalised patients, (one ica-positive/slime-positive and one ica-positive/slime-negative) were tested. Bacteria grown in BHI medium were suspended in physiological saline at a concentration of ˜3×109 cells/ml. Hydroxyl (OH)-terminated (hydrophilic) and methyl (CH3)-terminated (hydrophobic) glass surfaces were used as substrates in a parallel plate flow chamber. Bacterial adhesion was examined under two flow rates: 2 ml/min and 20 ml/min for two and four hours. Total RNA from both planktonic (p) and adherent (a) bacteria, after detachment with trypsin, was isolated by the Trizol method. Reverse transcription followed by relative Real-Time PCR (rRT-PCR) towards a 207 bp part of 23S rRNA gene, allowed the detection of expression levels of icaA and icaD. Adherent bacteria were investigated with Scanning Electron and Confocal Laser microscopes.
Results: Higher expression levels of both icaA and icaD genes onto glass and especially methyl-terminated glass surfaces were calculated by rRT-PCR, under higher flow rate in two hours by the reference and the clinical slime-positive strains. These results correlate well with adherent bacterial cell counts and images taken by both microscopes. The ica-positive slime-negative clinical strain showed lower expression levels of ica genes, less adherent ability and PIA production on glass surfaces, as observed by microscopes.
Conclusions: Higher flow rate enhances the expression level of both ica genes, with a peak in two hours. Hydrophobic biomaterial surfaces seem to play a crucial role to initial adherence, increasing ica gene expression and PIA synthesis.
Clinical trials of antibiotics: what can be proven?
O210 Appropriate vs. inappropriate empirical antibiotic treatment: systematic review and meta-analysis of effects and modifiers
V. Shani*, G. Kariv, E. Muchtar, L. Leibovici, M. Paul (Petach-Tikva, IL)
Objectives: To quantify the effect of appropriate empirical antibiotic treatment on mortality and to assess methodological and biological modifiers of this effect.
Methods: Systematic review of prospective studies assessing the effect of appropriate (matching in-vitro susceptibility) vs. inappropriate empirical initial antibiotic treatment (prior to availability of susceptibility results, IET) among adults with sepsis and microbiologically documented infections. Duplicate reports were excluded. Unadjusted and adjusted effect estimates were extracted and pooled using the random effects model. Modifiers were assessed through subgroup analyses and metaregression, including baseline patient characteristics, covariates used in adjusted analyses and study methods. Odds ratios (OR) with 95% confidence intervals for all-cause mortality are reported. OR = 1 was imputed when results for IET were not significant, with standard errors matched for study's weight.
Results: The pooled effect of IET was 2.19 (1.81–2.64, N = 63 studies) when unadjusted and 2.17 (1.73–2.72, N = 47) when adjusted for other risk factors for mortality. Unadjusted ORs underestimated the effect of IET by 24% in studies reporting both analyses. All analyses were significantly heterogenous. Studies varied significantly in the covariates evaluated for inclusion in adjusted analyses. Assessment of in-hospital rather then 30-day mortality (p = 0.004) and lack of adjustment for severity score (p = 0.046) and background conditions (p = 0.013) were associated with significantly lower adjusted ORs for mortality. Lack of adjustment for septic shock and neutropenia were non-significantly associated with higher ORs. Adjusted ORs increased with increasing rates of IET in the studies (p = 0.002). Age was negatively associated with ORs (p = 0.038). The effect was higher in intensive care units (OR 2.65, 1.62–4.34) than elsewhere in the hospital (OR 1.77, 1.47–2.13), but the difference was not statistically significant. Prospective planning to assess the effects of IET was associated with non-significantly higher ORs than post-hoc analyses. The types of pathogens assessed did not significantly affect the observed ORs. There was no association between study years and the effects of IET.
Conclusions: The pooled odds for mortality with IET is 2.17 with narrow confidence intervals. Methodological variables, more than biological effects, affect the ORs reported in different studies.
O211 Efficacy and safety of linezolid as treatment of proven diabetic foot infections caused by methicillin-resistant S. aureus. Preliminary report of a non-comparative Spanish trial
R. Zaragoza*, J. Blanes, J. Flores, A. Chacón, E. Escudero on behalf of the MRSA Foot Infections Spanish Group
Background: The aim of this study was to assess the clinical efficacy and safety of linezolid (L) treating documented diabetic foot infections (DFI) caused by MRSA.
Methods: This non-comparative multicentre open-label trial was conducted at 10 sites in Spain from September 2006 through Jan 2008. Consenting men and women with DFI (predefined by clinical signs and symptoms) caused by MRSA were potentially eligible including those associated with bacteraemia. Patients with initial osteomyelitis were excluded. Patients could receive L 600 mg bid either iv or po. Primary end point were cure or improvement rates (C+I) and microbiologic eradication (ME) at 60 days after the beginning of L. Secondary end points were C+I on days 5 and 30 after the beginning of treatment and hospital discharge day, need of amputation, duration of therapy and mortality rates. All the adverse events were collected.
Results: 70 patients were enrolled. Relation men:women was 2.1. The age of patients was 63.2±13 years and the average period from the diagnosis of diabetes was 16.5±9.7 years. Associated bacteraemia was present in 27.1% of patients included. Primary end points: C+I 60 days after the beginning of L was achieved in 91.4% of patients and ME was obtained in 84.3% of patients. Secondary end points: C+I on day 5, hospital discharge day and day 30 after the beginning of treatment and were; 70%; 84.3% and 88.6% respectively. Only 8 patients needed a minor amputation. The primary and secondary end points in the subgroup of bacteraemic episodes were not statistically different of those previously described. The mean duration of therapy was 29.5±18.4 days. Global mortality was 4.3%. Only one episode of polineuropathy was reported. Neither thrombocytopenia nor lactic acidosis was found.
Conclusions: L achieved excellent C+I even at first evaluation visit in documented DFI caused by MRSA. L also showed high ME rates. Although patients received prolonged periods of treatment, L was a safe drug.
O212 Single-dose azithromycin microspheres versus 5-day moxifloxacin in acute exacerbation of chronic bronchitis
Y. Zhang*, D. Zhu, T.C. Atienza, M.L. Ong on behalf of the ASSET Study Group
Objectives: Azithromycin microspheres formulation (AZM) was developed to enable a higher dosage of 2 g to be administered as a single oral dose without decreasing the safety profile. This study compared AZM with moxifloxacin (MOX) aimed at confirming the efficacy and safety of AZM in acute exacerbations of chronic bronchitis (AECB).
Methods: This prospective, multicentre, randomised, double-blind, double dummy study compared AZM 2 g single dose with MOX 400 mg once daily for 5 days, enrolled AECB patients 50 years old and above, with Anthonisen Type 1 exacerbations, and with at least 2 exacerbations of AECB in the past 12 months. Subjects were to have a history of smoking of at least 20 pack-years and documented forced expiratory volume in 1 second (FEV1) less than 80% of predicted. They were followed up for up to 9 months.
Results: A total of 396 patients were treated (198 in each of the treatment groups) The distribution of the age, and mean FEV1 were similar for the 2 treatment groups. Pathogens were isolated from 62.9% of the patients (61.1% of patients on AZM and 62.9% of patients on MOX).
The clinical success (signs and symptoms related to the acute infection had returned to the subject's normal baseline level, or clinical improvement was such that no additional antibiotics were deemed necessary) rate for the Per Protocol Population at Test of Cure (TOC) at Day 12–19 was 93.0% for AZM and 94.2% for MOX group (95% CI – 5.8, 3.9). Bacterial eradication rate (Bacteriologic Pre Protocol population) at TOC was 96.0% for AZM group and 96.7% for MOX group (95% CI – 4.5, 3.3). Although the study population had history of at least 2 exacerbation in the past 12 months, less than half of the subjects experienced a recurrence during the follow-up, and there was no statistically significant treatment difference in time taken to first occurrence of AECB.
Both treatments were well tolerated. The incidence of treatment related adverse events was low, being reported by 17% of subjects receiving AZM and 12% of subjects receiving MOX. Most AEs were mild or moderate in severity. The most common AEs were gastrointestinal disorders, being reported by 14% of subjects receiving AZM and 8% of subjects receiving MOX.
Conclusions: A single oral dose of AZM was as effective as a 5-day course of MOX in the treatment of AECB and was well tolerated.
O213 Optimal duration of gentamicin containing regimen for the treatment of uncomplicated brucellosis
M.R. Hasanjani Roushan*, M.J. Soleimani Amiri, N. Janmohammadi, M. Javanian, M. Baiani (Babol, IR)
Objectives: Optimal duration of gentamicin containing regimen for therapy of human brucellosis is not clearly determined.
Methods: This randomised clinical study was conducted to compare the efficacy of gentamicin 5 mg/day for 5 days plus doxycycline 100 mg twice daily for eight weeks (GD group) versus streptomycin 1 gr IM for 2 weeks plus the same dose of doxycycline for 45 days (SD group). All cases were followed for one year after cessation of therapy. Efficacy of both regimens (failure of therapy or relapse) were compared.
Results: Seventy-nine patients with the mean age of 35±14.5 years and 75 cases with the mean age of 36.7±13.9 years were treated with regimen of GD or SD, respectively. The clinical manifestations in these two treated groups were similar. Failure of therapy was seen in one patient in GD group and in 2 cases in SD group (95%CI, 0.042 to 5.271, OR = 0.468, p = 0.613). Relapse was seen in 2 (2.5%) cases in GD group and in 5 (6.7%) cases in SD group (95%CI, 0.067 to 1.905, OR = 0.358, p = 0.264)
Efficacy of therapy was seen in 76 (96.2%) cases treated in GD group and in 68 (90.7%) cases in SD group (95%CI, 0.095 to 1.542, OR = 0.383, p = 0.201). Risk for developing of relapse and failure of treatment in patients treated with SD group was 2.61 times higher than those treated with SD group (95% CI, 0.649–10.486, p = 0.201).
Conclusion: Efficacy of gentamicin for 5 days plus doxycycline for 8 weeks is similar with that of streptomycin for 2 weeks plus doxycycline for 45 days.
O214 Telavancin for the treatment of major skin and soft tissue abscesses: the ATLAS studies
G.R. Corey, E. Rubinstein, S.L. Barriere, A. Hopkins, M.E. Stryjewski* on behalf of the ATLAS Study Group
Objectives: To study the efficacy of telavancin (TLV), an investigational bactericidal lipoglycopeptide, for the treatment of complicated skin and soft tissue infections (cSSTI) caused by presumed or confirmed Gram-positive organisms.
Methods: ATLAS 1 and ATLAS 2 were methodologically identical, double-blind, randomised, multinational, Phase 3 studies. Adult men and women presenting with cSSTI including major abscess were randomised 1:1 to TLV 10 mg/kg intravenous (IV) q24 h or vancomycin (VAN) 1 g IV q12 h for 7 to 14 days. Test-of-cure (TOC) visit was conducted 7 to 14 days after end of study treatment. The all-treated population (AT) included patients with confirmed diagnosis of cSSTI who received ≥1 dose of study medication. This analysis examined the baseline characteristics and cure rates at TOC for patients with major abscess in the combined ATLAS AT population.
Results: In the pooled AT population of ATLAS, 772 patients presented with major abscess. More than 60% of these patients required hospitalisation. The baseline lesion surface area exceeded 5 cm2 in 98% of the cases, while 65% of the patients presented with lesions exceeding 50 cm2 (Table 1 ). Elevated white blood cell counts were found in more than 40% of the cases (Table 1). Nearly all patients required surgical drainage, with approximately 2/3 performed prior to the first dose of study medication. Very few patients required a surgical procedure more than 4 days after the start of study medication. Clinical cure rates at TOC are presented in Table 1. Overall, adverse events in the AT population were similar between the treatment groups with regard to type and severity.
Table 1.
Signs, symptoms and cure rates in patients with major abscess – combined all-treated population
| TLV (N = 375) | VAN (N = 397) | |
|---|---|---|
| Fever >38°C | 44 (12%) | 52 (13%) |
| WBC >10×109/L | 152 (41%) | 169 (43%) |
| Bacteraemia | 10 (3%) | 7 (2%) |
| Lesion size ≥5cm2 | 368 (98%) | 385 (97%) |
| Lesion size ≥50 cm2 | 248 (66%) | 252 (64%) |
| Cure rates at TOC | 289 (77%) | 296 (75%) |
Conclusion: Telavancin administered once daily was non-inferior to vancomycin for the treatment of major abscess.
Does antibiotic resistance matter when treating anaerobic infections? (Symposium arranged with the ESGARAB)
S217 Changes in the antibiotic resistance of Bacteroides fragilis group strains in Europe: 20 years of experience
E. Nagy* (Szeged, HU)
Objectives: B. fragilis and related species, members of the normal bowel flora, are the most widely isolated anaerobic bacteria from different infections. To follow the development and spread of the resistance among these strains is difficult, as antibiotic susceptibility testing of clinically relevant anaerobes in different routine laboratories in Europe is less and less frequently carried out due to the fact, that clinicians treat many presumed anaerobic infections empirically. To follow the changes in the antibiotic resistance of Bacteroides strains three Europe-wide studies were organised during the past twenty years. The evaluation of the results of these studies may show changes in the resistance to different antianaerobic drugs.
Methods: Only clinical isolates and no normal flora members of Bacteroides strains belonging to different species were collected from different countries throughout Europe during these studies. Agar dilution method was used for the antibiotic susceptibility determination. Actual breakpoints accepted by NCCLS (CLSI) and EUCAST were used. Molecular genetic investigations were carried out to detect resistance mechanisms.
Results and Conclusions: Since the first study the chromosomally mediated beta-lactamase production and tetracyclin resistance is the most prevalent among Bacteroides strains in Europe. Clindamycin resistance in Bacteroides is mediated by a macrolide-lincomycin-streptogramin (MLS) mechanism and its frequency differs in different countries in Europe. Resistance to beta-lactam-beta-lactamase inhibitor combinations was studied using amoxicillin-clavulanic acid and/or piperacillin-tazobactam. Increase in resistance was observed to both combinations throughout the years. The same is true for cefoxitine and in the third study several hetero-resistant isolates were found. The occurrence and spread of resistance to imipenem and metronidazole among Bacteroides strains merit special clinical importance. The presence of the cfiA gene is much more prevalent than the expression of the imipenem resistance; however the spread of the cfiA gene among species other than B. fragilis is still very rare. The molecular genetic methods looking for the resistance genes among strains with elevated MICs against these antibiotics prove that resistance breakpoints should be reconsidered. The resistance to moxifloxacin shows great differences in different countries. The lowest resistance rate was observed in the case of tigecyclin.
S218 The relevance of susceptibility testing in anaerobes
L. Dubreuil* (Lille, FR)
Many factors may affect the response to treatment such as site of infection, surgical procedures, severity of the illness, patient status, presence of other pathogens (mixed infection), Pk/Pd parameters of the antibacterial drugs. Thus, correlation between treatment failure and antibiotic resistance among anaerobes remains difficult to assess. The main discrepancies came from intra-abdominal infections and a worrisome disjunction between surgeon and microbiologist opinions emerged in the 1990's. But, patients in whom primary therapy failed had more resistant strains compared with patients in whom therapy succeeded. In contrast many failures may be due to the lack of isolation of anaerobes from clinical samples! During anaerobic bacteraemia, Salonen et al. demonstrated that mortality increased dramatically from 17% for initially effective treatment to 55% when an ineffective treatment was started. Facing new mechanisms of resistance and global increase resistance to many antibiotics among anaerobes may lead nowadays to a different answer. Clindamycin vs. penicillin studies for the treatment of lung infections pointed out the failure due to β-lactamase production among Gram-negative anaerobes. We found many reports of failure after clindamycin treatment in osteomyelitis, septic arthritis, brain abscess in presence of clindamycin-resistant anaerobes (Bacteroides fragilis group and Prevotella), probably because when resistance occurs, clindamycin MIC's are high. Similarly, the lack of coverage of an undetected resistant anaerobe allows the selection of an anaerobic strain resistant to the treatment chosen against the associated aerobes such as imipenem-resistant Eghertella lenta or metronidazole-resistant strains of Prevotella or Bacteroides fragilis. The later failures may give opportunity to set up a new metronidazole breakpoint for resistance (MIC > 4 mg/L). The main problem is related to the difficulty to detect some heterogeneous resistant strains, that needs prolonged incubation period on agar medium. This kind of situation is probably the most suitable to correlate the bacterial antibiotic resistance with the failure of the antibiotic treatment. The difficulty to detect heterogeneous resistant strains may explain some failures observed during metronidazole treatment of C. difficile. Clinicians should be encouraged to publish the clinical failures of their first line treatments when associated with a bacterial resistance among anaerobic bacteria.
Community-acquired MRSA (Symposium arranged with the ICAAC Program Committee)
S221 What we know about the pathogenesis of CA-MRSA infections?
J. Etienne*, G. Lina, F. Vandenesch (Lyon, FR)
The pathogenesis of CA-MRSA has to be considered according to the spectrum of human infections. The USA300 and the European ST80-IV clones which contain the Panton Valentine leukocidin (PVL) genes, are responsible for skin and soft tissue infections. PVL is expressed in skin abscesses with concentrations up to 2 mg/L and PVL-positive S. aureus strains elicit significant anti-PVL antibody production in humans. Intra-dermal injection of PVL (rLukS-PV and rLukF-PV) in rabbits caused a severe dermonecrosis. Mice infected intradermally with USA300 S. aureus or the isogenic Δ-pvl derivative did not differ in the superficial sizes of the lesions but in the depth of the infection. Active immunisation with rLukS-PV or LukF-PV protects rabbits against PVL induced dermonecrosis. Mice subcutaneously vaccinated with LukF-PV and LukS-PV are protected against an intradermal infection.
PVL-positive CA-MRSA are responsible for necrotising pneumonia. PVL is detected in broncho-alveolar lavages from patients with necrotising pneumonia with concentrations up to 20 mg/L. In a murine model of pneumonia, PVL-positive clinical strains of S. aureus, laboratory strains lysogenised with the PVL-encoding phage, and purified PVL all cause histological lung changes similar to those seen in patients with necrotising pneumonia. The LukS-PV subunit administered intranasally protects mice against USA300-induced pneumonia.
PVL-positive CA-MRSA bone and joint infections need repeated surgical drainage and require prolonged treatment. Experimental osteomyelitis with PVL positive strain in rabbits are characterised as an aggressive infection with rapid local extension, in contrast to osteomyelitis due to PVL negative strain.
Other clones of CA-MRSA contain other virulence factors such as the toxic-shock toxin (tst) gene. A tst-positive MRSA clone is associated with community infections such as cellulitis and systemic infections (scarlet fever and toxic shock syndrome). This clone has not been tested in any experimental models, but the role of superantigens such as TSST-1 in the pathogenesis of certain infections is well known.
In total, a diversity of virulence factors is associated with the diversity of CA-MRSA clones and CA-MRSA infections. Depending of the type of infections, certain virulence factors have a predominant role. For instance, PVL appears to play a crucial pathogenic role in CA-MRSA necrotising pneumonia.
S223 Paediatric approach to the management of CA-MRSA infections
S. Kaplan* (Houston, US)
Methicillin-resistant S. aureus isolates causing community-acquired infections (CA-MRSA) in children is a major problem in several areas around the world. CA-MRSA are associated with both skin and soft tissue infections and invasive infections. Recurrent soft tissue infections and infections within the family caused by CA-MRSA isolates are common. CA-MRSA S. aureus isolates containing gene coding for PVL have been associated with serious staphylococcal pneumonia as well as osteomyelitis complicated by subperiosteal abscesses or venous thromboses. In addition to vancomycin, CA-MRSA generally are susceptible to clindamycin and trimethoprim-sulfamethoxazole. Treatment of superficial skin and soft tissue infections involves surgical drainage of abscesses followed by an oral agent such as TMP-SMX or clindamycin. Minocycline or doxycycline is a consideration for children >8 years old. Empiric vancomycin is typically administered for more serious and invasive infections such as osteomyelitis, septic arthritis, serious head and neck infections or suspected Staphylococcal pneumonia. Clindamycin is efficacious in treating invasive CA-MRSA infections caused by susceptible organisms. Linezolid or daptomycin is another option in selected circumstances. MRI is the optimal imaging modality for assessing children with CA-MRSA osteomyelitis. Aggressive surgical drainage of subperiosteal abscesses or sites of pyomyositis is recommended. Venous thombosis is increasingly recognized as a complication of CA-MRSA osteomyelitis. Anti-coagulation until the thrombus has resolved is recommended. The optimal approach to prevention of recurrent CA-MRSA infections is unclear but a strategy that includes emphasizing personal hygiene, plus/minus antimicrobial soaps, mupirocin to the nose or “bleach baths” is frequently suggested.
Invasive group A streptococcal disease
S226 Understanding the pathogenesis of group A streptococcal disease: the bedside-to-bench approach
S. Sriskandan* (London, UK)
Invasive group A streptococcal (GAS) infection presents itself in a range of guises, most notoriously necrotising fasciitis and the streptococcal toxic shock syndrome. As a human pathogen, GAS pathogenesis research should ideally be shaped by clinical questions arising from either epidemiological or case-based investigation of human disease. In the mid 1990 s, large epidemiological studies pointed to a central role for specific T cell-stimulating superantigens in the aetiology of streptococcal toxic shock. This sparked a series of clinical and laboratory investigations that demonstrated production of superantigens during infection which were indeed capable of triggering massive T cell activation in patients but were unlikely, alone, to account for all the features observed in toxic shock. Genomic, clinical and laboratory-based investigations have identified novel and highly potent superantigens that appear to directly contribute to sepsis pathogenesis and, together, may constitute targets for adjunctive treatments in invasive disease.
Epidemiological, clinical, and laboratory studies have highlighted a role for blunt trauma in the aetiology of at least a quarter of cases of GAS necrotising fasciitis. One of the most striking findings on examination of tissues from patients suffering with necrotising fasciitis is the failure of neutrophils to migrate to the focus of infection. Investigation of patients with invasive GAS infection led to the discovery that GAS produces an enzyme that can cleave and inactivate human chemokines and study of patients with bacteraemia has highlighted a likely role for the causal enzyme SpyCEP in disease pathogenesis; this bacterial surface enzyme has also shown promise as a potential vaccine antigen. Notwithstanding a potential role for individual virulence factors in disease causation, clinical studies have demonstrated that GAS bacteria may persist at the site of infection despite high concentrations of bactericidal antibiotics, and this has been borne out by experimental studies; the reasons behind such persistence are unclear but may include internalisation of GAS by immune cells, formation of biofilm, and antibiotic penetration of necrotic tissues. The persistence of viable bacteria in such cases is not widely recognized and deserves focused consideration in the research laboratory.
S227 New understanding of group A Streptococcus pathogenesis provided by integrated systems biology studies
J.M. Musser* (Houston, US)
Genome-wide analysis of microbial pathogens and molecular pathogenesis processes has become an area of considerable activity in the last 10 years. These studies have been made possible by several advances, including completion of the human genome sequence, publication of genome sequences for many human pathogens, development of microarray technology and high-throughput proteomics, and maturation of bioinformatics. Despite these advances, relatively little effort has been expended in the bacterial pathogenesis arena to develop and use integrated research platforms in a systems biology approach to enhance our understanding of disease processes. We have exploited an integrated genome-wide research platform to gain new knowledge about how the human bacterial pathogen group A Streptococcus causes disease. Results of these studies have provided many new avenues for basic pathogenesis research and translational research focused on development of an efficacious human vaccine and novel therapeutics. New data stemming from use of a systems biology approach to provide new data about group A Streptococcus pathogenesis will be presented.
S228 Managing group A streptococcal infection: the role of IVIg
A. Norrby-Teglund* (Stockholm, SE)
Streptococcal toxic shock syndrome and necrotising fasciitis caused by group A streptococcus are rapidly progressive invasive diseases that are associated with significant morbidity and mortality, ranging from 30–80% despite prompt antibiotic therapy and surgical debridement. S. pyogenes is known to primarily cause disease by activating and modulating host immune responses. The exotoxins with superantigenic activities have been demonstrated to be crucial triggers of excessive inflammatory responses and consequently systemic toxicity, organ dysfunction, tissue necrosis and shock. Another important virulence determinant is the M-protein, which is classically known for its anti-phagocytic properties, and lately, was shown to trigger pro-inflammatory responses as well as induction of vascular leakage and shock. This likely represents important mechanisms contributing to the rapid development of shock and systemic toxicity in patients with severe invasive group A streptococcal infections. The understanding of these infections as hyperinflammatory diseases highlighted the potential of immunotherapy to improve outcome. One such strategy includes the administration of intravenous polyspecific immunoglobulin (IVIG) as adjunctive therapy. The mechanistic actions of IVIG in this setting are believed to include opsonisation of the bacteria, neutralisation of the superantigens and suppression of the pro-inflammatory responses. There is growing evidence to support the use of IVIG in patients with streptococcal toxic shock syndrome. These studies include one observational cohort study based on Canadian patients identified through active surveillance of invasive group A streptococcal infections, and one European multicentre placebo-controlled trial.
However, the question remains whether IVIG is efficacious also for the severe streptococcal deep tissue infections. An observational study of seven patients with severe streptococcal deep tissue infections suggested that the use of high-dose IVIG in patients with severe GAS soft tissue infections may allow an initial non-operative or minimally invasive approach, which can limit the need to perform immediate wide debridements and amputations in unstable patients. The fact that seven patients with severe group A streptococcal infections survived with this approach definitely warrants further studies to be conducted on the use of IVIG in these severe infections.
Blood-borne viral diseases
Hepatitis
O229 Prevalence and outcome of pregnancy in chronic hepatitis C virus infection
I. Julkunen*, A. Sariola, M. Sillanpää, K. Melen, P. Koskela, P. Finne, A.L. Järvenpää, S. Riikonen, H.M. Surcel (Helsinki, Oulu, FI)
Objectives: In the Western countries the incidence of hepatitis C virus (HCV) infection has steadily been increasing especially among young adults. It is thus likely that an increasing prevalence of HCV infection is also found in pregnant women.
Methods: To assess the frequency of HCV infection in the metropolitan area of Helsinki selected anti-HCV antibody testing was carried out for pregnant women during the years 1991–1999. In addition, HCV prevalence was analysed in serum specimens collected from pregnant maters during the years of 1985–2005.
Results: Altogether 145 mothers were identified among 44680 mothers. The frequency of anti-HCV positivity rose from 0.13% in 1991 to 0.43–0.53 in 1997–1999. In early 90's only 20% of mothers knew about their seropositivity, whereas by the end of the follow-up period almost 70% of mothers knew about their HCV infection already before the pregnancy. Intravenous drug abuse was the major risk factor (71% of cases) for contracting the disease. In 90% of the mothers chronic HCV infection was well under control and in this population the mean serum alanine aminotransferase (ALT) values decreased towards the end of the pregnancy. However, 10% of anti-HCV Ab positive mothers developed intrahepatic cholestasis (odds ratio 16.4) as characterised by itching and elevated serum bile acid levels. The correspondig value in the control pregnancies was only 0.7%. Anti-HCV Ab positive mothers were younger, delivered earlier and gave birth to babies with smaller birth weight as compared to control deliveries. To have a more comprehensive view of the problem of HCV infection during pregnancy randomly selected serum specimens from the Finnish maternity cohort were tested. 2000–5000 serum specimens were tested in selected cohorts (1985, 1990, 1995, 2000 and 2005). In 1985 the nationwide prevalence was 0.19% and it steadily role to 0.50% in 2005. In the metropolitan area of Helsinki the prevalence was higher being 0.68% and 0.70 in 1997 and 2002, respectively.
Conclusion: Our study indicates that there is an increasing problem of HCV infection in pregnant women in Finland. Although most women cope well with their disease during pregnancy there is a subpopulation of mothers who develop cholestasis and their liver status should thus be followed-up carefully. Testing of all mothers for serum anti-HCV antibodies is recommended.
O230 HCV core, NS3, NS4B and NS5A are the major immunogenic proteins in humoral immunity in chronic HCV infection
M. Sillanpää*, K. Melen, P. Keskinen, R. Fagerlund, K. Nevalainen, K. Lamminaho, M. Lappalainen, I. Julkunen (Helsinki, FI)
Objectives: The viral genome of hepatitis C virus constitutes a 9.6-kb single-stranded positive-sense RNA which encodes altogether 11 viral proteins. In order to study the humoral immune responses against different HCV proteins in patients suffering from chronic HCV infection, we produced three structural (C, E1 and E2) and six nonstructural proteins (NS2, NS3, NS4A, NS4B, NS5A and NS5B) in Sf9 insect cells by using the baculovirus expression system.
Methods: The recombinant HCV proteins were purified and used in Western blot analysis to determine antibody responses against individual HCV protein in 68 HCV RNA and antibody positive human sera that were obtained from patients suffering from genotype 1, 2, 3 or 4 infection.
Results: These sera were also analysed with INNO-LIA Score test for HCV antibodies against core, NS3, NS4AB and NS5A, and the results were similar to our Western blot method. Based on our Western blot analyses we found that the major viral antigens were the core, NS4B, NS3 and NS5A proteins and they were recognized in 97%, 86%, 68% and 53% of patient sera, respectively. There were no major genotype specific differences in antibody responses to individual HCV proteins. A common feature within the studied sera was that all except two sera recognized the core protein in high titers, whereas none of the sera recognized NS2 protein and only three sera (from genotype 3) recognised NS5B.
Conclusion: The data shows significant variation in the specificity in humoral immunity in chronic HCV patients. Anti-HCV antibody pattern also remains very stable within one individual.
O231 Occult hepatitis B virus infection in “anti-HBc alone” haemodialysis patients
A. Ramezani, A. Aghakhani, M. Mohraz, A. Eslamifar, A. Khadem-Sadegh, M. Banifazl*, A.A. Velayati (Tehran, IR)
Objectives: Occult hepatitis B virus (HBV) infection is characterised by presence of HBV infection with undetectable hepatitis B surface antigen (HBsAg). Occult HBV infection harbours potential risk of HBV transmission through haemodialysis (HD). The aim of this study was to assess the occult HBV infection in hepatitis B core antibody (anti-HBc) alone haemodialysis patients.
Methods: A total of 289 HD patients from five dialysis units in Tehran, Iran were included in this study. HBsAg, anti-HBs, anti-HBc, anti-HCV, ALT and AST levels were tested in all subjects. The presence of HBV-DNA was determined quantitatively in plasma samples of HD patients with anti-HBc alone (HBsAg negative, anti-HBs negative and anti-HBc positive) by real-time PCR using the artus HBV RG PCR kit on the Rotor-Gene 3000 real-time thermal cycler.
Results: Of 289 patients enrolled in this study, 18 subjects (6.2%, 95% CI, 3.5%-8.9%) had anti-HBc alone. HBV-DNA was detectable in 9 of 18 HD patients (50%, 95% CI, 27%-73%) with anti-HBc alone. Plasma HBV-DNA load was less than 50 IU/ml in all of these patients.
Conclusion: Our study showed that detection of anti-HBc alone could reflect unrecognized occult HBV infection in HD patients. The majority of these infections are associated with low viral loads.
O232 Long-term protection against carriage of hepatitis B virus after newborn vaccination
L. Roznovsky*, A. Kloudova, L. Kabieszova, L. Hozakova, I. Orsagova, I. Lochman, J. Mrazek, A. Zjevikova (Ostrava, CZ)
Objectives: Carriage of hepatitis B virus is a major risk factor for liver cirrhosis and hepatocellular carcinoma. Vaccination of newborn of hepatitis B surface antigen (HBsAg) positive mothers practically interrupted the vertical transmission of hepatitis B virus. However it is unknown whether protection is maintained into early adulthood.
Methods: Combine passive-active immunisation of newborns of HBsAg positive mothers against hepatitis B was commenced in northeastern part of the Czech Republic in 1988 year. The number of immunised children gradually increased till the January 2009. All 715 children were protected with hepatitis B immunoglobulin at birth. The children received 10 microgram doses of plasma-derived or recombinant vaccine at interval 0, 1 and 6 months, only thirty children of HBeAg positive mothers at interval of 0, 1 and 2 months. Since 2007 year, after first dose of monovalent hepatitis B vaccine at birth, next 4 doses of combine hexavalent vaccine were used. Combine vaccine contained 10 microgram of HBsAg; first dose was used at 6 weeks of age. Blood samples were obtained after immunisation, at 2 years of age, and biennially thereafter. Samples were tested by ELISA method for HBsAg, anti-HBs and anti-HBc. The immunisation schedules were completed in 674 children.
Results: Vertical transmission of hepatitis B virus with chronic HBsAg carrier status was proved in 2 children, escape mutant of HBsAg infected one of them. No other breakthrough infection was observed in toddlers or older children.
Asymptomatic infections with new appearance or long-term presence of anti-HBc antibodies were observed in 10 children. The anamnestic response with double increase of anti-HBs without revaccination was proved in 68 children. Two anamnestic responses were observed in 6 of them. Anti-HBs antibodies were tested in 657 children after immunisation; protective anti-HBs antibodies were proved in 613 of them (93%). Waning of protective anti-HBs antibodies was detected in 30%, 49% and 62% children in 5, 10 and 13 years of their life.
Conclusion: The vaccination of neonates of HBsAg positive mothers practically interrupted the vertical transmission of hepatitis B virus. The study have shown persistent protection at least for 15 years after newborn vaccination despite waning anti-HBs antibodies, suggesting there is no need for booster before adolescence.
Grant support: IGA Ministry of Health, Czech Republic, NR/9257–3/2007.
O233 Effectiveness of hepatitis B virus (HBV) vaccination among persons at high risk for HIV transmission two decades after implementation of nationwide HBV vaccination programme in Taiwan
W.C. Liu, C.H. Wu, H.Y. Sun, C.C. Hung*, S.C. Chang (Taipei, TW)
Background: Taiwan used to be hyperendemic for hepatitis B virus (HBV) infection and perinatal or childhood infection is the main route for HBV transmission. Seroprevalence of HBV surface antigen (HBsAg) was estimated 15–20% among the adults, regardless of HIV serostatus. After implementation of nationwide HBV vaccination program in Taiwan in 1 July, 1984, several epidemiological studies among children have shown that seroprevalence of HBsAg has declined significantly among the children who were born after 1984. Long-term effectiveness of this program among persons at high risk for HIV transmission, however, is unknown in Taiwan.
Methods: HBV serological markers (HBsAg, anti-HBs antibody, anti-HBc antibody) were determined among HIV-negative homosexuals or heterosexuals who presented for voluntary HIV counseling and testing (VCT group) (N = 397), HIV-positive homosexuals or heterosexuals (HIV sexually-transmitted group) (N = 69), HIV-positive and HIV-negative injecting drug users (IDU group) (N = 59), and persons undergoing health check-up for military services (healthy controls) (N = 856). All of the subjects were born after July 1, 1984. HBV serological markers were determined using a commercial kit (ANTICORASE B-96, General Biologics Corp., Hsin-Chu, Taiwan).
Results: Seroprevalence of HBsAg, anti-HBs antibody and anti-HBc antibody was 2.8%, 52.4%, and 27.7%, respectively, for VCT group (mean age, 20.7 years). The respective value of the three HBV serological markers for HIV-positive sexually-transmitted group (mean age, 22.3 years) was 1.7%, 73.1%, and 20.5%; for IDU group (mean age, 22.6 years), 3.7%, 80.9%, and 35.3%; and for healthy controls (mean age, 23.0 years), 8.5%, 66.7%, and 27.9%. The seroprevalences of HBsAg and anti-HBc antibody were not statistically significantly different when comparisons were made among the three groups of persons at risk for HIV infection, while VCT group had a lower prevalence of HBsAg compared with control group (P < 0.001). In contrast, seroprevalence of anti-HCV antibody was 5.2% for HIV-positive sexually-transmitted group and 96.2% for IDU (P < 0.0001).
Conclusions: Our findings suggest that persons born in the era of nationwide HBV vaccination that was initiated in Taiwan two decades earlier remain to have a low prevalence of HBV infection despite their risky behaviours for both HIV and HBV transmission.
AIDS and HIV
O234 Primary resistance among HIV-1 positive patients naive to antiretroviral therapy
L. Skoura*, A. Papoutsi, E. Papadimitriou, P. Kollaras, I. Ntoutsos, P. Nikolaidis, N. Malisiovas (Thessaloniki, GR)
Objective: The aim of the study was to estimate the prevalence of genotypic resistance among HIV-1 positive patients naive to antiretroviral therapy, since primary resistance has emerged as a potential barrier to the successful antiretroviral therapy and a threat for further transmission of resistant variants.
Methods: 218 newly diagnosed cases, reported to the National AIDS Reference Laboratory of Northern Greece between 2006 and 2008, were included in the study. All the subjects had never been exposed to antiretroviral therapy. Genotypic resistance testing was performed at the time of diagnosis with a sequence-based assay (TRUGENE HIV-1 genotyping test) targeted at the protease region (codons 1 to 99) and RT region (codon 40 to 247) of the HIV-l genome.
Results: 21 of 218 patients (9.63%) harboured a virus with at least one mutation associated with phenotypic resistance; 1/218 with mutations associated with resistance to nucleoside reverse-transcriptase inhibitors (NRTIs), 17/218 to non-nucleoside reverse-transcriptase inhibitors (NNRTIs) and 3/218 to protease inhibitors (PI). Resistance to NRTIs was associated with the key mutation M184V, while resistance to NNRTIs was associated with Y181C and K103N mutations. Among mutations to PI, major resistance mutations L90M and D30N were found in three patients, whereas there was a high prevalence of accessory PI resistance mutations at positions 10, 20, 36 and 63.
Conclusion: Our data estimate the prevalence of primary resistance and mutations patterns among naive HIV patients, underlining the importance of genotypic resistance testing in HIV patients before starting treatment, especially when NNRTIs would be included in the initial antiretroviral therapy.
O235 Comparison of protease inhibitor resistance-associated mutations between protease inhibitor-naive and protease inhibitor-experienced HIV-1 infected patients in Thailand where subtype A/E is predominant
S. Wiboonchutikul, S. Sungkanuparph*, C. Sukasem, W. Chantratita (Bangkok, TH)
Objectives: Few data are available on the genetic mechanisms of protease inhibitor (PI) resistance in non-B HIV-1, and PI resistance-associated mutations (RAMs) are commonly observed in PI-naive patients with subtype A/E infection. This study aimed to compare PI-RAMs between PI-naive and -experienced patients.
Methods: Genotypic resistance testing was conducted among a cohort of HIV-1 infected patients who had virologic failure. Patients were categorised into 2 groups: PI-naive and PI-experienced. We focused on PI-RAMs previously described by IAS-USA 2008.
Results: We studied 137 patients (mean age, 41.8 years; 64% male). Median CD4 cell count and HIV-1 RNA at virologic failure were 169 cells/cu.mm. and 14100 copies/mL, respectively. 85% of patients were infected with subtype A/E; the others had subtype B (12%), AB (2%), and C (1%). There were 75 patients in PI-naive group and 62 patients in PI-experienced group. The clinical characteristics between 2 groups were similar (p > 0.05) except for the duration of antiretroviral therapy which was shorter in PI-naive group (31.5 vs. 46.8 months, p = 0.028). Percentage of patients who had primary PI-RAMs was 1% in PI-naive and 19% in PI-experienced groups (p = 0.001). The most common primary PI-RAMs in the latter group were V82A (10%) and I54V (7%). Percentage of patients with secondary PI-RAMs in the corresponding groups was 99% and 98%, respectively (p = 1.000). Median number of secondary PI-RAMs was also similar between 2 groups (p = 0.244). The most common secondary PI-RAMs in both groups were M36I (91%), H69K (34%), L89M (30%), I13V (26%), L63P (25%), L10I (18%), and K20R (18%). Interpretation of genotypic test results with TRUGENE HIV-1 Software showed that resistance to atazanavir, darunavir, indinavir, lopinavir, nelfinavir, and saquinavir were observed only in PI-experienced patients and significantly higher (p < 0.05) whereas resistance to amprenavir, fosamprenavir, and tipranavir were found in both PI-naive and PI-experienced patients (p > 0.05).
Conclusion: Primary PI-RAMs are observed exclusively among PI-experienced patients whereas secondary PI-RAMs are equally found in both PI-naive and PI-experienced patients. Secondary PI-RAMs previously described by IAS-USA are common among PI-naive patients with subtype A/E infection. PI resistance (esp. amprenavir, fosamprenavir, and tipranavir) should be interpreted with caution. Further study for clinical validation of PI-RAMs in HIV-1 subtype A/E is essentially needed.
O236 HIV-1 pol evolution under lamivudine pressure
V. Micheli*, M. Zazzi, P. Meraviglia, P. Corsi, A. Gonnelli, G. Penco, A. Callegaro, F. Maggiolo, N. Gianotti, L. Calza, L. Butini, G. Casazza, M.R. Gismondo (Milan, Siena, Florence, Genoa, Bergamo, Bologna, Ancona, IT)
Background: In vitro assays on HIV-1 RT suggest that replicative fidelity is increased in enzymes with RT-M184V mutation. That could be associated with a reduced fitness shown by M184V+ strains. M184V can affect replicative capacity in vivo too.
Objective: to assess the impact of M184V on the genetic stability of HIV-1 PR and RT.
Methods: We selected 280 HIV-1 experienced patients analysed for PR and RT sequences from the Italian ARCA database (Antiretroviral Resistance Cohort Analysis): 151 M184V+ (group A) and 129 M184V–(group B) [mean (sd) VL: 4.01 Log (0.72) cps/mL]. Two consecutive HIV-1 genotypic tests were available for all patients with a median (IQR) distance of 247 (161–411) days; in all cases M184V presence/absence in the second test was confirmed. All patients were on therapy, none made STI, none changed the ARV regimen after the first test and none reached VL < 50 cps/mL in the period between the tests, in order to minimise the changes of the selection pressure exerted on the viruses.
Comparing the sequences of PR and RT, between 2 consecutive tests, we recorded: Jukes-Cantor distance (DJC), Kimura 2 parameters distance (DK2p), ds/dn (ratio between synonymous mutations per synonymous site and non synonymous mutations per non synonymous site), # synonymous mutations and # resistance mutations (IAS 2008). We also defined a “silent score” (SS) and a “resistance score” (RS) as the number of synonymous mutations and of resistance mutations (in the second sequence in comparison with the first one) divided by number of days between the two tests, respectively.
Results: We compared all above-mentioned parameters between group A and B by means of Mann Withney two-tailed test: we didn't find any statistically significant difference. The only relevant finding is a trend in a lower ds/dn in the M184V+ group [median (IQR) 4.062 (2.771–6.596) versus 4.221 (2.205–7.076; p: ns]. This could mean a wider variability of M184V+ viruses (higher dn represents more efforts to generate mutant escape viruses), consistent with the great genetic variation acrrued among patients who had slow development of disease relative to patients with a rapid progression to AIDS (published data).
Conclusion: The clinical benefit (lower VL and higher CD4+) due to the presence of M184V observed in vivo should be interpreted as the impact of the immune pressure on viral load control instead of a crude effect on the replication capacity.
O237 Drug resistance mutations and sub-type circulation in newly diagnosed HIV-infected subjects
S. Parisi*, C. Boldrin, M. Cruciani, R. Scaggiante, O. Bosco, V. Manfrin, R. Ferretto, S. Panese, M.C. Rossi, F. Dal Bello, M.G. Cecchetto, S. Andreis, G. Palù (Padua, Verona, Vicenza, Schio, Venice, Treviso, Rovigo, IT)
Objectives: to evaluate circulation trends of drug resistance mutations (DRM) and viral sub-types (ST) among subjects recently diagnosed as HIV infected (pts), over a five years period in a region with a wide availability of therapeutic options.
Methods: Plasma from 832 pts diagnosed from July 2004 to December 2008 in the Veneto region (Italy) were studied. The protease (PR) and the reverse transcriptase (RT) were sequenced and analysed for the presence of major DRMs, for drug susceptibility profile (Stanford database) and ST. Potential low level resistance were not considered. A χ-square test for linear trends was applied.
Results: The main results were as follows: in four different periods, 2004–5, 2006, 2007 and 2008, were recruited 168, 166, 244 and 254 pts respectively; mean cd4 percentage (±SD) were 20.9 (±11), 21 (±10.6), 22 (±10.5), 20.9 (±10.8); B-ST pts (% of total) were 138 (82.2), 123 (74.1), 173 (70.9) and 183 (72); pts with DRMs in B-ST (% of total B-pts) were 30 (21.7), 25 (20.3), 20 (11.6) and 22 (12); pts with DRMs in Non-B-ST (%) were 7 (23.3), 6 (14), 5 (7) and 3 (4.2). A significant increase of non-B-ST (p = 0.021) and a significant decrease in DRMs (p < 0.001) were observed. CRF02_AG was the prevalent non-B ST (44%). 35.3% of non-B ST pts were italians. Among B-ST, DRMs predicted a reduced susceptibility to one drug class in 23, 17, 15 and 14 cases in the different periods; to two drug classes in 4, 6, 5 and 8; to three classes in 3, 2, 0 and 0. In non-B-ST, a reduced susceptibility to one drug class was found in 6, 6, 4 and 0 cases; to two drug classes in 1, 0, 0 and 2; to three drug classes in 0, 0, 1 and 1, respectively. Among pts with one or two classes of resistance, a decrease of percentage of Protease Inhibitors related DRMs, and a persistence of Non Nucleoside RT Inhibitors involving DRMs, mainly 103N and 190A, were observed.
Conclusions: An increase of non-B strains was observed, only partially related to a modification of the ethnic composition of the cohort. The observed decrease of the DRMs prevalence and of the multidrug resistant strains in both B and non-B groups is probably related to the reduction of viraemic and failing pts spreading resistant viruses, and to the increase of subjects unaware of their infection and transmitting wild-type viruses. The substantial circulation of NNRTI-related DRMs has important implications on the selection of the first-line HAART.
O238 Longitudinal local immune analysis in HIV+ persons with oropharyngeal candidiasis
E. Lilly, J. Rufener, M. Zacharek, M. Barousse, K. McNulty, J. Leigh, T. Wiegand, J. Vazquez*, P. Fidel (New Orleans, Detroit, US)
Oropharyngeal candidiasis (OPC), caused by Candida albicans, is the most common infection in HIV-infected persons. An evaluation of tissue-associated T cells and adhesion molecules in OPC lesions of HIV+ persons with reduced CD4+ T cells showed an accumulation of activated memory CD8+ T cells at the epithelial-lamina propria interface together with reduced expression of E-cadherin. These results suggested a role for CD8+ T cells against OPC, but a dysfunction in the mucosal migration of the cells in those with OPC.
Objective: To evaluate changes in tissue-associated CD8+ T cells and E-cadherin expression of HIV+ persons during and after an episode of OPC.
Methods: From HIV+ persons with a history of, or an acute episode of OPC, oral fungal burden was evaluated bi-weekly and buccal mucosa tissue was collected bimonthly for a period of one year. Tissue was evaluated for the presence of CD8+ T cells and E-cadherin by immunohistochemistry or flow cytometry.
Results: Patients evaluated under OPC– conditions and low oral fungal burden revealed the presence of CD8+ T cells and E-cadherin, but expression was usually unremarkable over time. In situations where OPC– patients had increased oral Candida colonisation (indicative of a potential pre-clinical OPC condition), higher numbers of CD8+ T cells were observed throughout the tissue with normal E-cadherin expression. In patients with an acute episode of OPC where CD8+ T cells were accumulated at the epithelial-lamina propria interface together with reduced E-cadherin expression, evaluations following successful treatment revealed normal conditions. Finally, viable CD8+ T cells could be extracted from OPC+ lesions.
Conclusion: These results suggest that under reduced CD4+ T cells, CD8+ T cells typically migrate to the site of a pre-clinical infection under normal expression of E-cadherin and that reduced E-cadherin expression in those with OPC is not permanent. This work was supported by R01DE-12178 from NIDCR.
Clinical fungal infections
O239 The increasing incidence of candidaemia and the increasing importance of non-ICU/non-haematology patients: secular trends, Queensland, Australia, 1999–2008
E.G. Playford*, G.R. Nimmo, M. Tilse, T.C. Sorrell (Brisbane, Sydney, AU)
Objectives: To define the secular trends in the epidemiology of candidaemia in Queensland, Australia (population, 4.1 million) over a 10-year period.
Methods: All episodes of candidaemia within Queensland public hospitals from 1999–2008 were identified from laboratory information systems. Data on species identification, antifungal susceptibility, demographics, and hospital ward of diagnosis, and denominator data (hospital admissions, accrued patient-days (pt-days) and fluconazole usage) were collected.
Results: Over the 10-year period, 1137 unique episodes (100% case ascertainment) were identified from 42 healthcare facilities (8 tertiary, 2 paediatric, 11 secondary and 21 smaller hospitals). The median patient age was 56.4 years. The overall incidence-density was 0.45/10000 pt-days, highest in paediatric (1.28/10000 pt-days) and tertiary hospitals (0.62/10000 pt-days). Over the 10 years, the incidence-density increased 3.2-fold in tertiary hospitals and 6.6-fold in secondary hospitals (both p < 0.0001 for trend), but not in paediatric or smaller hospitals. The incidence-density in ICUs (5.2/10000 pt-days) was 10-fold higher than in non-ICU wards, but did not significantly increase over the study period. The relative proportion of episodes occurring in adult general medical/surgical (ie non-oncology/non-ICU) wards significantly increased (p < 0.001), accounting for 62% of episodes at the end of the 10-year period, whereas that occurring in paediatric and adult oncology wards decreased (p < 0.001 and p = 0.07 respectively). Overall, C. albicans accounted for 44%, C. parapsilosis 27% and C. glabrata 13%. Although the incidence-density of all species increased over the study period, the relative proportion caused by C. albicans decreased (p = 0.007) and C. parapsilosis increased (p = 0.01). Despite significantly increased fluconazole usage (from 19.7 to 30.6 DDD/1000 pt-days, p < 0.0001), the relative proportion caused by C. glabrata/C. krusei did not change (p = 0.5).
Conclusions: The overall incidence of candidaemia has increased almost 400% in Queensland public hospitals over the last 10 years. The relative proportion of episodes occurring among general medical/surgical patients and caused by C. parapsilosis has increased. Candidaemia is an increasing problem the epidemiology of which continues to evolve. It is increasingly affecting patients outside traditional risk groups.
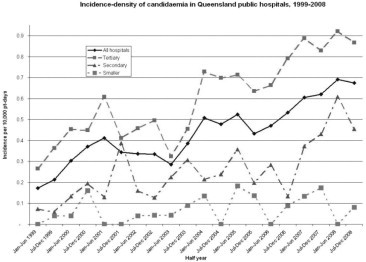
O240 Invasive candidiasis: role of pharmaco-economic modelling in improving patient care, diagnosis and guiding cost-effective therapy at a large district hospital in northern England
A. Guleri*, J. Patterson, S. Ellershaw, B. Lunt, E. Trautt, R. Palmer (Blackpool, UK)
Background: Nosocomial candidaemia is a serious life threatening infection with considerable mortality and healthcare costs. Average daily cost of treatment varies from £10.36 (fluconazole) to £568.05 (liposomal amphotericin). Overall mortality rate varies between 30 and 40% worldwide. Blackpool Victoria is a large district hospital in northwest England offering referral haematology and cardiac centres.
Objectives: Epidemiological surveillance of candidaemia over 5-years, comparing turnaround times [TAT]; choice/cost of antifungal and processing costs[outsourcing versus in-house testing]and trends in mortality over this period.
Methods: In-house identification and fluconazole susceptibility testing [FST] by E-test strip was introduced in September 2006. Surveillance of candidaemias from laboratory database between Jan 2004 to Oct 2008 included TAT, cost of in-house processing versus outsourcing to Bristol Mycology laboratory [BML], cost of antifungals and mortality.
Results: During the study period, there were 61 candidaemia episodes (non-duplicated). Rate of candidaemia rose from 15.4%[2004] to 24.62% [projected – 2008]. C albicans was the commonest cause [28.7%], followed by C glabrata[16%] and C parapsilosis[11.7%]. C albicans candidaemia varied from 16.7%[2008]to 64.3%[2006]. Resistance to fluconazole was noted in 3.3%(2 glabrata/61 isolates]. Overall associated mortality was 24.2% [30% in 2004 to 16.7% estimated for 2008]. C albicans was associated with highest associated mortality [79%]. Preceeding in-house testing and this surveillance study, all germtube negative candida species required empiric antifungal treatment with either liposomal amphotericin, caspofungin or voriconazole. The average duration of treatment as per hospital formulary is 2 weeks. Cost of a two week treatment Fluconazole [£72.52]; Caspofungin [£6268.92]; voriconazole [£6814.08]; posaconazole [£1647.38] and liposomal ampotericin [£7952.7]. TAT and cost comparison per isolate of inhouse processing [72-h and £6.04] versus outsourcing to BML [15d and £103.76).
Conclusions: This surveillance study and pharmaco-economic modelling has proved immensely beneficial in setting up inhouse processing, improved TAT, reduced costs of outsourcing and subsequent use of expensive antifungals. Reduction in mortality has been noted but is not statistically significant. C. albicans was the commonest isolate; fluconazole resistance is minimal and associated mortality is lower than reported from Europe.
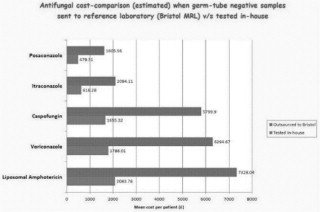
O241 Invasive aspergillosis in acute myeloid leukaemia: report of Seifem-2008 multi-centre survey
M. Caira, A. Candoni, M. Picardi, M. Offidani, G. Specchia, M. Stanzani, C. Cattaneo, R. Fanci, C. Caramatti, F. Rossini, L. Potenza, F. Ferrara, M.E. Mitra, R. Invernizzi, T. Aloisi, B. Martino, A. Bonini, G. Lanasa, A. Chierichini, L. Melillo, C. de Waure, L. Fianchi, M. Riva, F. Aversa, G. Leone, A. Nosari, L. Pagano* on behalf of SEIFEM. group (Sorveglianza Epidemiologica Infezioni Fungine Emopatie Maligne)
Objectives: To evaluate epidemiological characteristics and outcome of invasive aspergillosis (IA) in acute myeloid leukaemia patients (AMLs) and to analyse efficacy of different therapeutic approaches.
Methods: A survey was conducted over 2004–2007 in 21 Italian Haematology Divisions. All proven/probable IA were reported. AMLs submitted to transplant were excluded. The parameters we analyzed were: age, sex, AML phase, site of IA, severity, duration and recovery from neutropenia, antifungal prophylaxis, empirical/pre-emptive therapy, 1st/2nd line target therapy, aetiologic agent, G-CSF use, neutrophil transfusion, outcome. We also collected date of symptoms onset, diagnosis, antifungal therapy start and exitus. All variables were investigated as predictors of death. Follow up was assessed at 90th day from diagnosis.
Results: 140 cases were collected. Infection mostly occurs after the 1st course of chemotherapy (61%). The majority of AMLs experienced a deep neutropenia before symptoms onset (90%). Probable IA were 66%. As expected, pulmonary localisation was predominant (126/140, 90%). Infection disseminated in 5 pts. Aspergillus subtype was known in 55 pts only. Overall attributable mortality rate was 27% (38/140); it remained stable over years. Outcome was significantly influenced by AML phase (p < 0.001), duration of (p = 0.05) and recovery from neutropenia (p < 0.001). Role of neutropenia duration was confirmed at multivariate analysis (p < 0.005).
Antifungal approaches are reported in table 1 .
| AMLs | Deaths (AMR%) | p value | |
|---|---|---|---|
| Systemic prophylaxis | |||
| Not administered | 39 | 8 (20.5) | 0.27 |
| Administered | 101 | 30 (30) | |
| Empirical/pre-emptive | |||
| Caspofungin | 28 | 9 (32) | |
| L-AmB | 54 | 12 (22) | |
| Itraconazole | 5 | 2 (40) | 0.79 |
| Voriconazole | 25 | 6 (24) | |
| Other | 16 | 5 (31) | |
| Not done | 12 | 4 (33) | |
| First-line therapya | |||
| Caspofungin | 28 | 9 (32) | |
| L-AmB | 37 | 9 (24) | 0.65 |
| Voriconazole | 38 | 7 (18) | |
| Combined | 22 | 5 (23) | |
| Other | 11 | 4 (36) | |
4 early deaths
Many pts received systemic prophylaxis (72%); itraconazole and fluconazole were used in 68 and 33 pts respectively. No differences emerged between empirical vs pre-emptive therapy and none of the drugs resulted to significantly influence outcome. In 66% of pts initial empirical/pre-emptive drug remained unchanged after IA diagnosis, while in 16% clinicians shifted to a combined treatment.
Conclusion: This study allows as to analyzed multiple factors as potentially influencing outcome. We confirmed that AML phase and neutropenia influence IA outcome. Present data confirm the perception that during last years the application of a correct and timely diagnostic work-up and the availability of more efficacious and less toxic drugs (i.e. voriconazole, liposomal amphotericin B, caspofungin) have modified the course of IA. However none of the new drugs emerged as the most efficacious in our series. Even combined treatment did not confer any advantage in survival analysis.
O242 Prospective surveillance of invasive aspergillosis in 4 French regions: 2005–2007
O. Lortholary, J.P. Gangneux, K. Sitbon, B. Lebeau, F. de Maubrisson, F. Dromer, B. Coignard, S. Bretagne* (Paris, Rennes, Grenoble, Lyon, St-Maurice, Créteil, FR)
Objective: An active prospective collection of invasive aspergillosis (IA) cases was implemented in 2005 in 12 French academic hospitals from 4 geographical regions, to describe IA epidemiology, diagnostic modalities and therapeutic practices.
Methods: Each notification was reported by hospital microbiologists through a secured website and missing data were checked at the national reference centre. Only proven and probable IA according to 2002 EORTC/MSG criteria were considered. Numbers of patient admissions per hospital were obtained from national health statistics.
Results: From 2005 to 2007, 442 case-patients (male gender 62%, median age 55 yrs) were included, 71 of whom (16%) had proven IA. Overall, the median incidence of IA was 0.223 per 1000 admissions (range 0.095 to 1.078). Among the 442 case-patients, 354 (80%) had haematological malignancies, with acute leukaemia and lymphoid malignancies including myeloma representing 60% and 32% of cases, respectively. Cancer and solid organ transplantation patients represented 8 and 9%, respectively. IA involved the lungs (94%), brain (12%), sinus (10%), or was disseminated (6%). CT scan was performed for 373 (84%) patients and showed major signs in 201 (halo sign in 56; cavitation in 145). Galactomannan serum detection was performed for 433 (98%) patients, and 362 (82%) had samples processed for mycological culture, mainly through BAL. When positive (n = 268), culture yielded A. fumigatus (85%), A. flavus (4.5%), or few other spp. (<3% each). The first line therapy was monotherapy with voriconazole (49%), caspofungin (14%), lipid formulations of AMB (9%) or used antifungal drugs combination (20%). The mortality rate at day 90 was 41% when first line therapy included voriconazole compared to 60% when it did not (p < 0.001).
Conclusion: Comprehensive collections of cases based on systematic reporting and description of cases using a dedicated network of hospitals in selected regions and stringent definition criteria applied by trained clinicians and microbiologists are useful to describe IA, to assess its burden and secular trends, and to identify potential changes in diagnostic and therapeutic procedures. This network will expand to other regions in the near future, and data will help assessing the impact of new management strategies such as prophylaxis with posaconazole, the impact of modification of new diagnostic criteria as recently proposed (Clin Infect Dis, 2008), and identifying new populations at risk for IA.
O243 Airborne fungus – exposure prior hospitalisation as risk factor for mould infections in immunocompromised patients
C. Lass-Flörl*, S. Eschertzhuber, J. Auberger, C. Geltner, D. Nachbaur (Innsbruck, AT)
Nosocomial aspergillosis represents a serious threat for severely immunocompromised patients and outbreaks have been attributed to airborne sources. The role of hospital-independent fungal spread sources e.g. the private homes or business suites are not known. We investigated the relationship between fungal exposure prior hospitalisation and the ensuing onset of invasive mould infections (IMI) in patients at risk. Patients admitted to the Department of Haematology and Oncology or to the Department of Transplant Surgery of the Innsbruck Medical University received a structured questionnaire regarding their fungal exposure prior hospitalisation. Questions inquired heavy fungal exposures up to five days prior hospitalisation.
234 patients were enrolled in this study and 19% were smokers, 22% suffered from an airborne allergy, 62% lived in old buildings, 73% were ruralists, 82% and 92% were exposed to any outdoor or indoor fungus sources. Poor housing conditions and other fungus exposures were associated with the onset of community-acquired IMI only in patients with acute myelogenous leukaemia (P < 0.01). AML patients being more at risk for IMI when smoking cigarettes (P < 0.05), living on the country site (P < 0.05), having two or more fungus exposures (P < 0.05) and suffering from allergy to dust, pollen and/or moulds (P < 0.05). A similar trend was for lung transplant recipients receiving extensive immunosuppressive agents to treat allograft rejection. Overall, 88% of IMI were community-acquired cases.
Hospital-independent fungal sources highlight risk-factors for IMI in severe immunocompromised patients and the rate of community-acquired IMI does increase. An analysis of an individual patient's risk factors for fungal infection and the type of fungus to which they are most susceptible, indicates the preventative strategies that are likely to be successful.
O244 Outbreak of invasive aspergillosis in an intensive care unit for major heart surgery. The case for abnormally high levels of airborne Aspergillus conidia: presence of similar genotypes in air and clinical samples
T. Peláez*, J. Guinea, C. Klaassen, P. Muñoz, J. Meis, D. García de Viedma, R. Flores, B. Gama, S. Recio, E. Bouza (Madrid, ES; Nijmegen, NL)
Objectives: Invasive aspergillosis (IA) is presumed to be caused by airborne Aspergillus conidia. However, few studies have shown the presence of similar genotypes of Aspergillus fumigatus in the air and clinical samples of patients with IA. We aimed to evaluate the relationship between the presence of airborne Aspergillus conidia and IA in a major heart surgery intensive care unit (ICU-MHS).
Methods: From November 2006 to May 2008, 11 patients were admitted to the ICU-MHS with Aspergillus spp detected in significant amounts in clinical samples. The underlying conditions of the patients were heart transplantation (n = 5), major heart surgery (n = 4), and other (n = 2). Eight (72.7%) patients developed proven/probable IA (4 with lung infection, 2 with mediastinitis, 1 with disseminated IA, and 1 with prostate involvement). The mortality of patients with IA was 87.5%. The ICU-MHS is divided into 3 areas, one of which is equipped with HEPA filters. Only 1 case of IA occurred in the protected area. We measured the fungal conidia levels in the air of each of the 3 areas (508 samples analyzed) monthly. A total of 172 strains of A. fumigatus (110 clinical strains from 10 patients and 62 environmental strains) were genotyped using microsatellites (de Valk et al, JCM 2005).
Results: The mean airborne conidia levels (6 months) before and after the outbreak were, respectively, 5.6 (0–15) CFU/m3 and 1.8 (0–10) CFU/m3. No cases of IA occurred during these periods. However, all cases of IA were linked to 4 peaks of abnormally high airborne conidia levels (65, 70, 200 and 500 CFU/m3). A. fumigatus was involved in 7 cases of IA; 1 patient was infected by non-fumigatus Aspergillus (not further genotyped). In 4 patients (1 mediastinitis, 2 pulmonary IA and 1 colonisation), we demonstrated similar genotypes in the air and in clinical samples. Patient 1 was located in the protected area and had a unique genotype. Patient 2 had two different clusters of genotypes: one cluster was similar to that of patient 3 and the other was also found in patient 4 and in the air. The genotype present in patients 2 and 4 was also detected in the air during a 6-month period.
Conclusions: Epidemiologic and molecular typing suggests that there is a causal relationship between Aspergillus causing IA and those present in the air. Our finding also supports the need for HEPA filtration in ICU-MHS. J. Guinea is contracted by FIS (CM05/00171).
O245 Galactomannan testing in the bronchoalveolar lavage for the diagnosis of invasive aspergillosis in lung transplant recipients
M.O. Xavier, A.C. Pasqualotto*, I.C.E. Cardoso, S.M. Schio, L. Sánchez, C.O. Costa, L.C. Severo (Porto Alegre, BR)
Objectives: This prospective study was performed to evaluate the performance of galactomannan (GM) detection in the diagnosis of invasive aspergillosis (IA) in lung transplant recipients, using bronchoalveolar lavage (BAL) samples.
Methods: 117 BAL samples from 60 lung transplant recipients were studied, during Mar 2007-Nov 2008. The EORTC/MSG criteria for the diagnosis of IA were modified to allow lung transplantation as a host factor. BAL samples were processed according with manufacturer's instructions for serum samples (Platelia Aspergillus EIA, Bio-Rad). Sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) were calculated in reference to proven and probable cases of IA. Reasons for performing bronchoscopy on patients were also recorded. The protocol received approval by the local ethic committee.
Results: From the 117 samples studied, 5 (4.3%) were classified as proven, 6 (5.1%) as probable, and 35 (29.9%) as possible cases of aspergillosis. Twelve samples (10.3%) represented colonisation, and 59 BAL samples were obtained during routine surveillance. Pulmonary aspergillosis was the main clinical presentation of IA (63.6%). Using ROC analysis, the best cut-off for galactomannan testing in BAL was defined as 1.5 (sensitivity 90.9%, specificity 90.6%, PPV 48% and NPV 99.1%). Median BAL GM index for the group of patients with proven/probable aspergillosis and for ‘negative cases’ were 3.3 and 0.5, respectively (p < 0.001). Overall mortality was 20% (n = 12). The odds for death for patients diagnosed with IA were 11.8, in comparison to patients who did not have this infection (95% CI 2.9–48.4).
Conclusion: GM testing in the BAL added to the diagnosis of IA in lung transplant recipients. In order to avoid false-positive results, a higher test cut-off should be applied to BAL samples, in comparison to sera. Increasing the cut-off to 1.5 resulted in a very high NPV, with an associated sensitivity of >90%.
O246 Prospective evaluation of clinical utility and pronostic value of broncho-alveolar lavage galactomannan assay in haematology-oncology patients
M. L. Luong*, C. Filion, A.C. Labbe, J. Cardin-Tourigny, S. Carrignan, S. Belanger, J. Roy, M. Laverdiere (Montreal, CA)
Objectives: 1) Determine the performance characteristics of the Galactomannan (GM) assay in broncho-alveolar lavage (BAL) in haematology-oncology patients; 2) Evaluate the prognostic value of the GM assay in this particular population.
Methods: The Platelia GM EIA assay (Bio-Rad) was performed on all BAL specimens obtained from haematology-oncology patients at our institution between March 2005 and April 2008, in addition to routine laboratory stains and cultures. All results were reported to physicians. We conducted chart reviews to classify cases as proven, probable, possible or without invasive pulmonary aspergillosis (IPA) according to the Revised Definitions of Invasive Fungal Disease from the EORTC/MSG Consensus Group. For performance characteristics, proven and probable cases were considered as IPA; possible cases were considered as without IPA. The result of BAL GM was not considered as a criterium to classify cases in order to avoid incorporation bias. In patients with >1 positive (GM index >0.5) specimen, only the first one was considered for the analysis. Mortality was calculated at 60 days following the first BAL procurement. Data were analyzed with Stata 8.0.
Results: There were 173 BAL samples from 145 patients, including 101 haematopoietic stem cell transplant (HSCT) recipients. We found 5 proven, 7 probable and 35 possible cases of IPA (total of 12 IPA cases; 6.9%). GM on BAL was positive in 47 (27.2%) specimens. The sensitivity and specificity of the GM assay in BAL were 100% and 78.3% respectively. Positive predictive and negative predictive values were 25.5% and 100%, respectively. False-positive results were found in 21 patients without IPA and in 14 with possible IPA. An index value 0.5 was significantly associated with a 60-day mortality risk (12/39 patients with a positive GM died within 60 days after BAL compared to 13/106 with a negative GM (OR = 3.2, 95%CI 1.3–7.8; p = 0.01). This association was even stronger when restricted to HSC recipients (OR = 4.6, 95%CI 1.5–13.6; p = 0.006).
Conclusions: The clinical utility of GM assay in BAL mainly lies in its negative predictive value, identifying patients at low risk of IPA. This test also carries a prognostic value in predicting patients at higher risk of mortality.
O247 Pneumocystis jirovecii colonisation induces the systemic inflammatory response in COPD patients
R. Morilla, L. Rivero, V. Friaza, E. Campano, N. Respaldiza, S. Gutierrez-Rivero, M.A. Montes-Cano, F.J. Medrano, J.M. Varela, E. Calderón, C. de la Horra* (Seville, ES)
Background: Chronic obstructive pulmonary disease (COPD) is a slowly progressive condition characterised by air flow limitation, which is not fully reversible. The air flow limitation is associated with a chronic inflammatory response in both airways and lung parenchyma. Besides the presence of chronic local inflammation in the respiratory organ, there is increasing the evidence of the important role systemic inflammation in these patients. Thus high levels of airway and systemic inflammatory markers are associated with a faster decline in lung function. In a recent pilot study, Pneumcystis-colonisation in COPD patients has been associated with increase of systemic inflammation, suggesting a possible pathogenic link with COPD.
Aim: To confirm the ability of P. jirovecii colonisation to increase the inflammatory response in COPD
Patients and Methods: 126 COPD patients diagnosed according to GOLD classification. Identification of P. jirovecii was performed by nested PCR at mt LSU rRNA from respiratory samples. The systemic inflammatory levels were analysed in serum samples from all patients. The assay were performed using a commercial ELISA (R&D systems) for IL-6, IL-8, TNF-alpha and MCP-1.
Results: The systemic inflammatory response was evaluated in 84 COPD subjects non colonised vs 42 COPD patients colonised by P. jirovecii paired by clinical characteristics and COPD severity. The analysis shows a significant increase in the systemic proinflammatory cytokines from Pneumocystis colonised than non colonised subjects (see table below). Not significant differences have been found among Pneumocystis colonisation and COPD status evaluated by FEV-1%. As well as no significant differences respect to age, sex or lymphocytes and leucocytes blood count were found.
| Systemic cytokine levels (pg/ml) | COPD without P. jirovecii (n = 84) | COPD with P. jirovecii (n = 42) | P-value (Student-T) |
|---|---|---|---|
| IL-8 | 5.3±10 | 21.9±16.9 | 0.003 |
| TNF-alpha | 19.0±12.2 | 25.3±17.1 | 0.069 |
| IL-6 | 2.5±6.2 | 9.8±5.4 | 0.016 |
| MCP-1 | 505.1±295 | 802.5±407 | 0.000 |
Conclusion: The data suggest a relationship between P. jirovecii colonisation and high level of systemic inflammatory response in patients with COPD suggesting strongly that P. jirovecii is an infectious agent thar play a role in COPD physiopathology.
This study was supported by ERA-NET Pneumocystis-PathoGenomics and FIS CP04/217
O248 High rate of Pneumocystis jirovecii colonisation in patients treated with infliximab
C. de la Horra, G. Wissmann, N. Respaldiza, I. Martin-Garrido *, S. Gutierrez-Rivero, L. Rivero, F.J. Medrano, J.M. Varela, E. Calderon (Seville, ES)
Background: Infliximab, a monoclonal antibody targeting tumour necrosis factor alpha (TNF-a), is indicated for the treatment of rheumatoid arthritis (RA) and other autoimmune diseases. However, its use has been associated with opportunistic infections, including Pneumocystis jirovecii pneumonia (PcP). Moreover, P. jirovecii has been observed colonising to humans with several disorders.
Objectives: To obtain information about P. jirovecii colonisation among patients with rheumatologic disease treated with infliximab. This information could be useful for assessing new strategies in the prevention of PcP in patients at risk.
Methods: 62 consecutive patients treated with infliximab for rheumatic disorders were included in the study. Oropharyngeal washes (OW) samples were collected for P. jirovecii detection. Clinical and demographic data were collected (sex, age, rheumatologic diagnosis, duration of infliximab use, concomitant use of other drugs for rheumatologic treatment, use of any other anti-TNF-α agent, use of anti-Pc drugs in the last six months, smoking, and diagnosis of chronic pulmonary respiratory disease). P. jirovecii colonisation was identify in OW samples by PCR at mtLSU-rRNA gene, with primers pAZ102-X and pAZ102-Y. We adapted a method previously described to a real-time PCR setting, using a LightCycler 1.5 (Roche, Germany). Individuals in whom the presence of P. jirovecii was detected at two independent assay in the absence of respiratory symptoms or radiological findings suggestive of PcP were considered to be colonised.
Results: Clinical and demographic data for 62 patients treated with infliximab are presented in Table 1 . jirovecii was detected by real-time PCR in the OW of 18 (29.0%) out of 62 patients.
| Characteristic | Colonised patients (18) | Non-colonised patients (44) | p-value |
|---|---|---|---|
| Age, mean years ± SD (range) | 57.3±12.5 (29–73) | 45.7±11.3 (24–74) | 0.002* |
| Male gender, no. (%) | 8 (44.4) | 26 (59.1) | 0.441 |
| Diagnosis rheumatoid arthritis, no. (%) | 11 (61.1) | 19 (43.2) | 0.316 |
| Diagnosis ankylosing spondylitis, no, (%) | 5 (27.8) | 20 (45.5) | 0.316 |
| Diagnosis psoriatic arthritis, no. (%) | 2 (11.1) | 5 (11.4) | 0.999 |
| Duration of infliximab treatment, weeks, median (range) | 205 (38–283) | 95 (2–192) | <0.001* |
| Corticosteroid use, no. (%) | 8 (44.4) | 6 (12.8) | 0.007* |
| Corticosteroid dose, deflazacort mg/day, median (range) | 6.75 (6.0–45.0) | 6.0 (6.0–10.0) | 0.999 |
| Methotrexate use, no. (%) | 16 (88.9) | 26 (59.1) | 0.048* |
| Methotrexate dose, mg/week, median (range) | 8.75 (7.5–20.0) | 7.5 (5.0–20.0) | 0.270 |
p<0.05.
Conclusions: P. jirovecii colonisation is associated with infliximab use, which is mainly demonstrated by the fact that the percentage of colonised individuals increases with the length of infliximab use. The detection of P. jirovecii in specimens, such as in OW, may be important to define which patients treated with this immunosuppressive drug are at greater risk of developing PcP.
Diagnostic methods
O249 Rapid one-step antigen detection method for human bocavirus
J.O. Koskinen*, M. Söderlund-Venermo, K. Hedman, R. Osterback, T. Heikkinen, M. Waris, T. Allander, R. Vainionpää, A.E. Soini (Turku, Helsinki, FI; Stockholm, SE)
Objectives: Most research with human bocavirus, a recently found respiratory pathogen, has been done by molecular biology (polymerase chain reaction, PCR). The results have been ambiguous because the virus has often been found in co-infection with other viruses, and also in clinically healthy subjects. It has been proposed that, for bocavirus, antigen detection could better indicate the aetiology than qualitative nucleic acid detection. We have developed a rapid antigen detection test for the virus.
Methods: The one-step test for bocavirus VP2 antigen is based on a separation-free two-photon excitation fluorometry (ArcDia TPX assay technique). The assay protocol is simple; the swab sample is dissolved in sample buffer, and the solution is dispensed (20 µl) onto a 384-well microtitre plate (containing the reagents in dry form) for incubation and automated quantitative measurement. The immunoassay applies microspheres as solid-phase carriers of purified bocavirus-specific polyclonal antibodies. The virus antigens concentrate onto the solid-phase which is probed in real-time with fluorescently labelled antibody reagents. Strong positive samples are reportable in 15 minutes, while low positive and negative samples are reported in 2 hours. The performance of the method was studied with recombinant human bocavirus-like particles (VP2), and purified respiratory pathogens (Group A streptococci, Streptococcus pneumoniae, and influenza A and B, respiratory syncytial, metapneumo, adeno, and parainfluenza 1–3 viruses).
Results: Analytical detection sensitivity of the method (lowest limit of detection, 0-control + 3SDs) was 3 ng/ml, dynamic concentration range was three orders of magnitude, and intra-assay imprecision was 5–10%. Cross-reactions with the other respiratory pathogens were not found.
Conclusion: The new method enables rapid detection of bocavirus antigens. The new test is very easy to perform in comparison to standard ELISAs. The analytical sensitivity of the method is expected to allow analysis of clinical samples. The sensitivity of the antigen detection test could be significantly increased by the use of monoclonal antibodies (10–100 fold). Our future objectives include increasing the detection sensitivity, and analysis of clinical samples in order to study the correlation of antigen detection and the clinical aetiology.
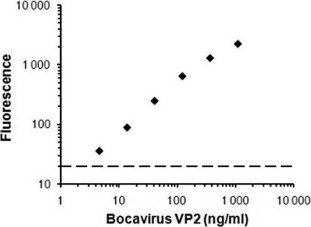
O250 Mortality and cost-effectiveness of rapid MRSA PCR testing in hospitalised patients with bacteraemia: a decision model
J. Brown*, J. Paladino (Buffalo, US)
Objective: Patients hospitalised with Staphylococcus aureus bacteraemia have an unacceptably high mortality rate. Literature available to date has shown that timely empiric selection of the most appropriate antibiotic may reduce morality. One tool that may help with this selection is the Xpert MRSA/SA Blood Culture PCR assay which determines methicillin resistant S. aureus from methicillin-susceptible S. aureus in less than 1 hour. To date no information is available evaluating the impact of this PCR technique on mortality and quality of life as compared to traditional empiric therapy.
Methods: A peer reviewed Europe (EU) and United States (US) literature search for information regarding the treatment regimens, outcomes, costs and utilities was performed. Information detailing the rate of infection, specificity and sensitivity of the PCR were also obtained from the peer reviewed literature. Hospital and testing costs were calculated using direct and indirect hospital costs discounted to 2009 costs. Adjusted life years were determined using US and WHO life tables. Cost effectiveness ratio (C/E) is defined as the costs per life-year for patients who survived. All analyses were performed using TreeAge Software (2008).
Results: The overall mortality rates for empiric vancomycin (V) and semi-synthetic-penicillin (SSP) was 30% and 35%, respectively, as apposed to 24% for those receiving the rapid MRSA PCR testing. These mortality rates were similar in both the EU and US subsets. Furthermore, the number needed to test in order to save one life was 20 and 11 for empiric V and SSP, respectively. Using sensitivity analysis the prevalence of MRSA was varied from 5% to 80% and yielded an absolute mortality difference favouring the PCR testing group of 10% and 2%, respectively as compared to empiric V and 1% and 18% compared to empiric SSP. In EU the C/E for empiric V and SSP treated patients was €873 and €949, respectively as compared to €807 for rapid PCR testing. In the US the C/E for empiric V was $1,049 as compared to $971 for rapid PCR testing. Using sensitivity analysis the prevalence of MRSA was varied from 5% to 80% and yielded favourable C/E in both the EU and US for rapid PCR testing regardless of the empiric treatment regimen.
Conclusion: Rapid MRSA PCR testing using the Xpert MRSA/SA Blood Culture PCR assay appears to improve mortality rates and is cost effective in the EU and US across a wide range of MRSA prevalence rates.
O251 Evaluation of culture-based approaches for rapid detection of glycopeptide-resistant enterococci: a randomised, investigator-blinded study
S. Malhotra-Kumar*, J. Cortiñas Abrahantes, C. Lammens, G. Molenberghs, M. Aerts, H. Goossens on behalf of the MOSAR WP2 study group
Background: Rapid detection of gastro-intestinal carriage of glycopeptide-resistant enterococci (GRE) from screening cultures is crucial for an efficient control of their spread. We assessed 4 media – 2 chromogenic, ChromID, (bioMérieux), and CHROMagar (CHROMagar Microbiology), and 2 selective, VRE Selective (Oxoid) and ECCV (BD) – for their ability to detect GRE using well-characterised isolates and stool samples from hospitalised patients at high risk of GRE colonisation.
Methods: Twenty-five isolates consisting of 13 GRE. faecalis/faecium carrying various van genes and 12 non-VRE at concentrations of 106-101 CFU/ml and 106 CFU/ml, respectively, and 37 stool samples were randomised and spiral plated on all media and scored by 5 blinded investigators for characteristic colonies after 24 hrs incubation. Standard confirmatory tests were done on 1 putative GRE colony or on 1 characteristically coloured colony each for E. faecalis/faecium from the selective and chromogenic media, respectively. Detection of van genes, and ddl or sodA based speciation was done on PCR-sequencing. Mean sensitivity (SEN) and specificity (SPEC), and confidence intervals (CIs) were estimated for each medium by a logistic regression model using a penalised likelihood approach based on the reader response for the stool samples and isolates, and additionally on confirmation test results for the stool samples, both at the aggregated (GRE detected) and penalised level (correct species–colony colour correlation).
Results: CHROMagar showed the highest SEN based on reader response at the aggregated and penalised level for both stool samples and isolates (Table ). Using confirmation test results at the aggregated level, SEN for ECCV was highest while the two chromogenic media showed a decrease in SEN by at least 11% in comparison to the values obtained based on reader response. SENs for the 2 chromogenic media were even lower (<70%) based on confirmation test results at the penalised level. ECCV and ChromID showed the highest SPECs with both reader response (stool samples) and confirmation test results at the aggregated level, and ChromID also at the penalised level, with narrow CIs indicating a high precision of this parameter estimate. For isolates, SPECs were highest for CHROMagar at both levels.
Table.
Mean sensitivities and specificities of media for detection of GRE after 24 hrs incubation
| Samples | Variable | Medium for GRE detection | Aggregated |
Penalised |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivity (%) |
Specificity (%) |
Sensitivity (%) |
Specificity (%) |
|||||||
| Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | |||
| Stools | Reader response | ECCVa | 86.1 | 77.6–92.1 | 98.8 | 96.0–99.7 | NA* | NA | NA | NA |
| VRE Selectiveb | 57.0 | 44.6–69.1 | 93.7 | 86.6–97.5 | NA | NA | NA | NA | ||
| ChromIDc | 83.3 | 73.7–90.0 | 98.9 | 96.1–99.7 | 82.9 | 73.8–89.5 | 98.6 | 95.6–99.6 | ||
| CHROMagard | 91.4 | 85.5–95.2 | 96.2 | 91.8–98.4 | 88.6 | 82.2–93.2 | 95.5 | 90.5–98.0 | ||
| Confirmation tests | ECCVa | 82.9 | 74.1–89.5 | 99.1 | 96.6–99.8 | NA | NA | NA | NA | |
| VRE Selectiveb | 33.5 | 23.6–44.6 | 98.4 | 95.5–99.5 | NA | NA | NA | NA | ||
| ChromIDc | 72.3 | 61.6–81.3 | 99.4 | 97.4–99.9 | 64.8 | 53.7–76.8 | 98.1 | 94.3–99.4 | ||
| CHROMagard | 72.0 | 61.7–80.7 | 98.5 | 96.2–99.5 | 67.9 | 57.6–76.8 | 94.4 | 89.4–97.2 | ||
| Isolates | Reader response | ECCVa | 83.4 | 77.7–87.8 | 96.3 | 91.7–98.3 | NA | NA | NA | NA |
| VRE Selectiveb | 65.9 | 58.3–72.8 | 94.2 | 87.8–97.2 | NA | NA | NA | NA | ||
| ChromIDc | 87.3 | 82.3–91.0 | 97.4 | 93.9–98.9 | 78.2 | 72.2–83.1 | 95.1 | 90.0–97.6 | ||
| CHROMagard | 91.5 | 87.4–94.2 | 99.7 | 98.3–99.9 | 86.4 | 81.4–90.1 | 99.4 | 97.0–99.9 | ||
Selective media do not differentiate between GRE. faecalis/faecium and thus, the aggregated and penalised responses are the same.
BD, BE
Oxoid, UK
BioMérieux, FR
CHROMagar Microbiology, FR.
Conclusions: CHROMagar showed the best overall performance considering both SEN and SPEC estimates. ECCV performed well as a selective medium for GRE detection from stool samples.
O252 Evaluation of a new E-test to detect metallo-beta-lactamases in Enterobacteriaceae
L. Bylund*, P. Ho, T. Walsh, G. Zambardi, A. Engelhardt (Solna, SE; Cardiff, UK; La Balme, FR)
Objectives: Metallo-beta-lactamases (MBLs) expressed from Pseudomonas are able to confer resistance to all beta-lactams with the exception of aztreonam. However, Enterobacteriaceae possessing MBLs exhibit moderate cephalosporin and low carbapenem MICs and thus are often underestimated. Herein, we describe data from new Etest prototypes specifically designed to detect this problematic resistance mechanism.
Methods: 82 MBL-positive (VIM or IMP derivatives) Enterobacteriaceae clinical isolates from 8 countries and 27 randomly selected Enterobacteriaceae negative controls (including the ATCC type strains) were tested against the 4 different Etest MBL prototypes. Beta-lactam substrates used were imipenem (IP), meropenem (MP), ceftazidime (TZ) and cefotaxime (CT) with or without the inhibitors dipicolinic acid (DPA) and EDTA. The Etest standard procedure for Gram negative aerobes was used and a reduction of beta-lactam MIC by equal to or greater than 3 dilutions by EDTA or DPA was interpreted as positive for MBL. Presence of ESBLs was tested using the Etest CT/CTL, TZ/TZL and cefepime (PM)/PML strips. AmpC production was detected using the Etest cefoxitin (FX)/FXI and cefotetan (CN)/CNI strips.
Results: The Results are summarised in the Table . The highest level of detection occurred with MP/EDTA with a sensitivity of 96.3% and a specificity of 97.2% even though most MP MICs were below 8 mg/l. ESBLs and AmpC (derepressed native or acquired) were detected in 20/82 and 18/20 strains, respectively. The presence of ESBL and AmpCs can occlude the presence of MBLs when TZ and/or CT are used as substrates. Accordingly, the sensitivity increased – 93% and 89% for TZ/EDTA and CT/EDTA, respectively – when cloxacillin (150 mg/l) and clavulanic acid (4 mg/l) was added to the medium on a subset of strains.
| N | Etest Combinations |
||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| IP/EDTA |
IP/DPA |
MP/EDTA |
MP/DPA |
TZ/EDTA |
TZ/DPA |
CT/EDTA |
CT/DPA |
||||||||||||||||||
| + | − | ND | + | − | ND | + | − | ND | + | − | ND | + | − | ND | + | − | ND | + | − | ND | + | − | ND | ||
| MBL-positive isolates | 82 | 53 | 28 | 1 | 26 | 47 | 9 | 79 | 3 | 0 | 76 | 3 | 3 | 69 | 5 | 8 | 67 | 7 | 8 | 62 | 9 | 11 | 59 | 13 | 10 |
| Negative controls | 27 | 0 | 27 | 0 | 0 | 27 | 0 | 0 | 27 | 0 | 0 | 27 | 0 | 0 | 27 | 0 | 0 | 27 | 0 | 0 | 27 | 0 | 0 | 27 | 0 |
| Total | 109 | ||||||||||||||||||||||||
| Sensitivity | 64.6 | 31.7 | 96.3 | 92.7 | 84.1 | 81.7 | 75.6 | 72.0 | |||||||||||||||||
| Specificity | 73.4 | 48.6 | 97.2 | 94.5 | 88.1 | 86.2 | 81.7 | 78.9 | |||||||||||||||||
Conclusion: Etest with EDTA performed marginally better than with DPA. Interestingly, the IP/EDTA performed poorly whereas the MP/EDTA gave the highest rates of detection. When clavulanic acid and cloxacillin was added to the TZ/EDTA combination, the detection rates were also acceptable. Such a method could prove invaluable for detecting MBLs mediating sub-breakpoint carbapenem MICs in Enterobacteriaceae.
O253 Evaluation of StrepB Select medium for the detection of group B Streptococcus
L. Louie*, L. Kotowich, H. Meaney, M. Vearncombe, A. Simor (Toronto, CA)
Objectives: As group B Streptococcus (GBS) is a significant cause of neonatal morbidity and mortality, antenatal screening for GBS is recommended. Current methods are time-consuming and labour-intensive, but newer, chromogenic based media may improve sensitivity while reducing turn-around time. We compared StrepB Select (Select; Bio-Rad Laboratories) with conventional culture including broth enrichment for the detection of GBS from genital specimens submitted for GBS screening.
Methods: A total of 1025 genital specimens were processed with direct inoculation of colistin-nalidixic agar with 5% sheep blood (CNA) and enrichment with Streptococcus Selective Broth (SSB). After overnight incubation, the CNA plate was examined for the presence of suspicious colonies. The SSB was subcultured onto CNA (if direct CNA was negative for GBS) and Select, and incubated overnight at 37°C. Suspicious colonies, turquoise-blue on Select, and grey colonies ± narrow haemolysis on CNA were worked up by separate, experienced technologists. Select cultures were incubated and read at both 24 and 48 hours. Identification of GBS was performed by conventional tests. Discrepancies between the two methods were confirmed by PCR for the cfb gene.
Results: Of the 1025 specimens tested, 243 specimens were positive (by either method) for GBS, for a positivity of 23.7%. Select detected 241/243 GBS, for a sensitivity of 99.2%, while CNA/SSB detected 224/243, for a sensitivity of 92.2% (P < 0.0001). At 24 hours, direct culture onto CNA isolated 201 GBS while SSB enrichment with CNA subculture detected another 23 isolates (224/243 isolates, 92.2%) at 48 hours. All but one GBS was recovered on Select after overnight incubation following SSB enrichment (240/241, 99.6%). One isolate required 48 hours. Of the 784 Select specimens that were negative for GBS, 345 grew turquoise-blue colonies, but the majority that required further work to rule out GBS grew after 48 hours. Two strains of GBS that were missed grew as white colonies on Select, and even at 48 h, did not exhibit the characteristic turquoise-blue colour.
Conclusion: SSB enrichment followed by Select subculture was extremely sensitive (99.2%) and superior to CNA/SSB for detection of GBS from genital specimens. However, non-GBS organisms can produce turquoise-blue colonies on Select and further work must be performed to rule out the presence of GBS.
O254 Comparison of 5 commercial serological tests for detection of anti-Chlamydia trachomatis antibodies
D. Baud, L. Regan, G. Greub* (Lausanne, CH; London, UK)
Objectives: Screening for Chlamydia trachomatis (CT) specific antibodies is valuable in investigating recurrent cause of miscarriage, pelvic inflammatory disease and tubal damage following repeated episodes of pelvic inflammatory disease. Immunofluorescence (IF) is considered the gold standard for detection of CT antibodies. The present study aims to compare the performance of 4 other commercial tests for the detection of serum IgG antibodies specific for CT: two CT IgG pELISA both using major outer membrane protein (MOMP; [“MOMP-Medac”, CT-IgG-pELISA; Medac, Wedel, Germany and “MOMP-Ruwag”, CT pELISA; Ruwag, Bettlach, Switzerland), one CT HSP-60 IgG pELISA (“HSP60-Medac”, cHSP60-IgG-pELISA; Medac, Wedel, Germany), and a new automated epifluorescence immunoassay (“Inodiag”, “MuST Chlamydiae; Inodiag, Signes, France).
Methods: A total of 405 patients with (n = 251) and without (n = 154) miscarriages were tested by all 5 serological tests described above. Sensitivity and specificity were calculated using IF as gold standard. A second standard, defining true positive or negative samples as sera respectively positive and negative in all 4 others tests, was also used (see table ).
| Standard | Sensitivity |
Specificity |
||
|---|---|---|---|---|
| IF | 4 tests | IF | 4 tests | |
| IF | − | 80 | − | 94 |
| hSP60-Medac | 55.4 | 90.9 | 80.9 | 84.6 |
| MOMP-Medac | 50 | 90.9 | 91.1 | 95.8 |
| MOMP-Ruwag | 48.1 | 95.2 | 93.1 | 99.5 |
| Inodiag | 63.8 | 100 | 80.1 | 86.8 |
Results: The prevalence of CT-specific IgG antibodies as determined by IF, HSP60-Medac, MOMP-Medac, MOMP-Ruwag and Inodiag was 14.3%, 23.2%, 14.3%, 11.9% and 26.2%, respectively. Inodiag exhibited the highest sensitivity whereas MOMP-Ruwag and MOMP-Medac showed the best specificity (see table). Serological cross-reactivity with Chlamydia psittaci was observed with all 5 tests (p < 0.001). Moreover, cross-reactivity with Chlamydia pneumoniae was also observed with IF, MOMP-Ruwag and Inodiag tests (p < 0.001). None of the tests appear to cross-react with other Chlamydiales (Parachlamydia, Neochlamydia, Waddlia), except for HSP60-Medac which cross-react with Parachlamydia.
Conclusion: Tests in the ELISA format based on peptides from the MOMP of Chlamydia trachomatis show good sensitivities and specificities. The new automated epifluorescence immunoassay from Inodiag exhibited similar performance than the ELISA tests and represent an interesting alternative especially when few numbers of samples have to be processed.
O255 Evaluation of serum Aspergillus galactomannan antigen in the diagnosis of penicilliosis
Y.T. Huang, C.H. Liao*, P.R. Hsueh, C.C. Hung (Taipei, TW)
Objective: This study aimed to examine the sensitivity, specificity, and positive and negative predictive avlue of serum Aspergillus galactomannan (GM) antigen assay in the diagnosis of penicilliosis in patients with human immunodeficiency virus (HIV).
Methods: From March 2007 to May 2008, patients with HIV infection who presented with pulmonary infection or suspicious cutaneous lesions were enrolled for a commercial Aspergillus GM antigen assay (Bio-rad, Platelia) of the serum samples. Patients receiving amoxicillin/clavulanate or piperacillin/tazobactam were excluded for analysis.
| Cut off value (O.D. index) | Serum galactomannan antigen interpretation | Culture positive (N = 21) | Culture negative (N = 111) | Sensitivity | Specificity | Positive predictive value | Negative predictive value |
|---|---|---|---|---|---|---|---|
| 0.5 | Positive (N = 43) | 17 | 26 | 80.9% | 76.6% | 39.5% | 95.5% |
| Negative (N = 89) | 4 | 85 | |||||
| 0.7 | Positive (N = 35) | 16 | 19 | 76.2% | 82.9% | 45.7% | 94.8% |
| Negative (N = 97) | 5 | 92 | |||||
| 1.0 | Positive (N = 27) | 16 | 11 | 76.2% | 90.1% | 59.3% | 95.2% |
| Negative (N = 105) | 5 | 100 | |||||
| 1.5 | Positive (N = 21) | 16 | 5 | 76.2% | 95.5% | 76.2% | 95.5% |
| Negative (N = 111) | 5 | 106 |
Results: During the study period, 132 serum samples were obtained for analysis, including 21 from patients with culture-confirmed Penicillium marneffei infection. A cut-off GM optic density index (ODI) of 0.5 yield a sensitivity (SE) of 80.9%, specificity (SP) of 76.6%, positive predictive value (PPV) of 39.5% and negative predictive value (NPV) of 95.5%. The SE, SP, PPV and NPV when different cut off ODI was used were as follows: 76.2%, 90.1%, 59.3% and 95.2% for ODI = 1.0; and 76.2%, 95.5%, 76.2% and 95.5% when ODI = 1.5. Diagnosis of penicilliosis could be made 2 days earlier by elevated GM ODI than by microbiologic cultures (range, 6 days after culture results became available to 15 days before culture results available). Of the five patients who had no penicilliosis but had GM ODI greater than 1.5, one had Paecilomyces sepsis, one had cryptococcosis and the remaining three did not have any fungal infection. One patient had follow-up GM ODI greater than 1.5 despite being asymptomatic after treatment for penicilliosis. The fitted ROC curve area was 0.903.
Conclusions: Our study indicated that serum Aspergillus GM assays may assist timely diagnosis of penicilliosis in patients with HIV infection in endemic regions.
O256 Quality control for diagnostic oral microbiology laboratories
R. Rautemaa-Richardson*, A. Smith, D. Lockhart for the COMB Network – Clinical Oral Microbiology Network
Objectives: Participation in diagnostic microbiology internal and external quality control (QC) processes is good laboratory practice, an essential component of a quality management system and compulsory in some European countries. Currently, there is no QC scheme for diagnostic oral microbiology. The aim of this study was to collate information on current QC needs, and processes undertaken in diagnostic oral microbiology laboratories.
Method: An on-line questionnaire was devised to ascertain interest in participating in an oral microbiology QC scheme and sent to oral microbiology diagnostic laboratories. The laboratories were identified from participants attending the European Oral Microbiology Workshop in Helsinki, 2008. Following this, a pilot round of QC samples was distributed to all interested laboratories.
Results: We identified 12 individuals that worked in diagnostic oral microbiology laboratories and received 7 (58%) positive responses. Of these 7 laboratories (representing 6 European countries) 71% did not participate in either internal or external QC. Each laboratory processed on average a total of 4135 samples annually. 86% of participants were in favour of a European-wide oral microbiology QC scheme. The preferred frequency for receiving external QC specimen was once in 3–4 months. The most preferred specimen types were periodontal pocket and oral pus specimens (both 29%), followed by oral mucosal swabs and caries activity tests. All participating laboratories were willing to share and harmonise their specimen processing and interpretation standard operating procedures. The pilot round specimen was a periodontal pocket sample. Six laboratories reported their findings in the specified time. The predominant pathogens (Aggregatibacter actinomycetemcomitans, Porphyromonas gingivalis) were identified by 5 of 6 laboratories. In addition to conventional culture, one laboratory used PCR. 5 laboratories performed antibacterial sensitivity testing primarily by disc diffusion.
Conclusions: This is the first attempt to a standardised European-wide approach to diagnostic oral microbiology. The findings from this feasibility study have indicated that a QC scheme for oral microbiology is of interest and have raised a number a pointers for subsequent rounds of specimens. Further work to improve the quality, to standardise the methodology and the interpretation of diagnostic oral microbiology at the European level is on-going.
O257 Evaluation of MALDI-TOF mass spectrometry for the identification of bacteria under routine conditions in a clinical laboratory
W. Moussaoui, A. Birgy, G. Prévost, Y. Piémont, J.M. Scheftel, M. Kostzrewa, P. Riegel* (Strasbourg, FR; Leipzig, DE)
Objective: Evaluation of MALDI-TOF mass spectrometry (MT-MS) for species identification of bacteria isolated in a clinical laboratory under routine conditions.
Methods: For evaluation of different culture conditions and routine identification, measurements were performed with a Microflex (Bruker Daltonik) and spectra were recorded for the mass range of 3,000 to 15,000 Da. Identification was obtained by using the BioTyper database 2. 0 (Bruker), giving a log score of similarity with spectra of reference strains included in the database.
A set of strains belonging to seven relevant species (S. aureus, E. coli, P. aeruginosa, S. pneumoniae, L. monocytogenes, H. influenzae, N. sicca) was used in order to determine the influence of different cultivation media (Mueller-Hinton, Sheep blood Columbia agar and chocolate agar) and different storage conditions (4°C, 37°C and room temperature after to 3 days storage) on the quality of the spectra. To evaluate species identification, all the relevant bacteria isolated over a six-weeks period from patients specimens were identified under routine conditions by MT-MS in parallel with conventional identification methods. A total of 531 clinically significant strains, consisting of 467 aerobic strains and 64 anaerobic strains was included in this study.
Results and Conclusions: Extraction, preparation of the ground steel plate, MT-MS of 48 samples, and a search of the database for similarity for species identification took about 2 h with the Microflex instrument. In all cases of culture or storage conditions, MT-MS resulted in usable spectra and correct identification. In total, MT-MS identified 87% of 531 strains with a concordant identification in comparison to the results of the conventional methods, leading to 93% for aerobic strains. Enterobacteria, enterococci and staphylococci exhibited more than 95% concordance whereas streptococci and strictly aerobic Gram-negative bacilli had a concordant identification for 82% and 86% of strains, respectively. Anaerobic, especially clostridia, showed a high rate of discordant results (43%). 424 of the 467 (90.1%) aerobic strains had log score values of >2.0 and were 97% concordant with the conventional identifications. Thus, MALDI-TOF provided accurate results for the identification of aerobic bacteria and is a reliable method for the identification of such clinical isolates under routine conditions.
O258 CRP/CD11b RATIO: a novel parameter for detecting Gram-positive sepsis
J. Nuutila*, P. Jalava-Karvinen, U. Hohenthal, I. Laitinen, P. Kotilainen, A. Rajamäki, J. Nikoskelainen, E.M. Lilius (Turku, FI)
Objectives: Since severe sepsis with acute organ dysfunction can be fatal within hours, it is customary to start empirical broad-spectrum antimicrobial therapy in all patients hospitalised for a suspicion of systemic inflammatory response syndrome. However, increased use of broad-spectrum antimicrobials over the years has contributed to the emergence of drug resistant strains of bacteria. Especially, drug resistance among Gram-positive bacteria, the leading cause of sepsis, is now a serious problem. The objective of this preliminary study was to develop a method for distinguishing between Gram– and Gram+ bacterial infection.
Methods: In this prospective study, leukocyte and neutrophil counts, CRP, ESR, and quantitative flow cytometric analysis of neutrophil complement receptors 1 (CR1/CD35) and 3 (CR3/CD11b), were obtained from 289 hospitalised febrile patients, of which 89 had bacterial and 38 viral infection. The patient data were compared to 60 healthy controls.
Results: It was noticed that in Gram– infection (n = 21) the average amount of CD11b on neutrophils was significantly higher than in Gram+ infection (n = 22). On the contrary, serum CRP level was significantly higher in Gram+ than in Gram– infection. Other measured parameters did not differ significantly between Gram+ and Gram– infections.
We derived a CRP/CD11b RATIO dividing the serum CRP value by amount of CD11b on neutrophils. In thirteen (76%) out of 17 patients with GRAM+ sepsis had CRP/CD11b RATIO ≥ cutoff value of 3.1 (Figure 1 ). Of these 13 patients, 9 (70%) were diagnosed with Streptococcus pneumoniae, 2 with Staphylococcus aureus, 1 with Enterococcus faecalis, and 1 with both Streptococcus intermedius and Streptococcus oralis. Corresponding percentages in patients with local Gram+ infection, Gram– infection, clinical pneumonia, other clinical infection, and viral infection were 20%, 14%, 30%, 15%, and 0%, respectively.
Figure.
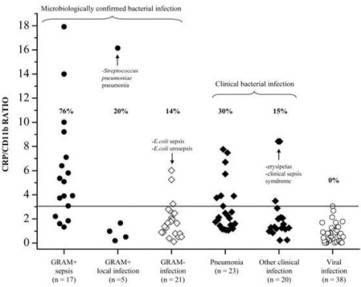
CRP/CD11b RATIO in clinical practice. The horizontal line indicates the optimal cut-off point value of 3.1 in detecting Gram-positive sepsis.
Conclusion: The detection of Gram+ sepsis is possible after combination of neutrophil CD11b data and serum CRP level. CRP/CD11b RATIO displayed 76% sensitivity and 80% specificity for detection of Gram+ sepsis. The proposed CRP/CD11b RATIO test could, for its part, assist physicians to decide appropriate antibiotic treatment in patients with severe bacterial infection.
Failure of antibiotic therapy in the absence of antibiotic resistance
S279 Biofilms
N. Høiby* (Copenhagen, DK)
A bacterial biofilm is a structured consortium of bacteria cells surrounded by a self-produced polymer matrix. Biofilms may be monospecies or polyspecies biofilms. Biofilm growing bacteria give rise to chronic infections, which persist in spite of therapy and in spite of the host's immune- and inflammatory responses. Biofilm infections are characterised by persisting pathology and immune response (in contrast to colonisation). Bacterial biofilms use both biofilm specific (B) and conventional (planktonic) resistance mechanisms (P) when they are exposed to antibiotics. The following resistance mechanisms have been described in bacterial biofilms:
-
1.
Stationary phase physiology (B), low oxygen tension (B) and slow growth (B) especially inside biofilms whereas the surface of biofilms is more similar to planktonic growth.
-
2.
Penetration barriers (B), binding to the polymer matrix (B).
-
3.
Mutations, hypermutators (B, P).
-
4.
Chromosomal betalactamase is upregulated (B, P).
-
5.
Antibiotic tolerance/adaptive resistance (B).
-
6.
Efflux pumps (B, P).
-
7.
Alginate production (B).
-
8.
High cell density and quorum sensing (B, P).
-
9.
PBP 3 – SOS response ? (B).
The knowledge of these resistance mechanisms can, however, be used to design new therapeutica approaches especially as regards quorum sensing inhibitors.
S280 Antibiotic treatment failure in the absence of resistance: the contributions of bacterial density and physiology
B. Levin*, K. Udekwu, F. Baquero (Atlanta, US; Madrid, ES)
We consider two factors that contribute to treatment failure in the absence of inherited resistance, the density of the population being treated and the physiological state of the bacteria. We also explore how these factors might contribute to the evolution of inherited resistance during the course of treatment. We conclude with a computer- and chemostat-assisted consideration of the potential clinical implication of these density and physiology effects and make suggestions for treatment protocols to deal with them.
Using in vitro cultures of Staphylococcus aureus ATCC25923 or the clinical isolate ps80 and antibiotics of six different classes we determined the functional relationship between the inoculum density and the efficacy of the antibiotics. As measured by the rates and extent of kill and/or the minimum inhibitory concentration (MIC), the efficacy of all of these antibiotics declined with increases in the density of bacteria, albeit to different extents. For daptomycin and vancomycin, much of this density effect can be attributed to bacteria-associated declines in the effective concentration of the antibiotic in the medium. For gentamicin, vancomycin, ciprofloxacin and oxacillin, our bioassays failed to reveal significant reductions in their effective concentration in the medium.
The effects of the physiological state of S. aureus on the efficacy of these antibiotics were examined for bacteria from cultures in “stationary phase” for different times and from chemostats run at different generation times. These experiments are currently under way but by the time of the symposium we will have the full (and true) story. It is, however, clear that the efficacy of all of these antibiotics declines with the time in stationary phase (its “age”). And, even slowly dividing cultures from chemostats are more susceptible to antibiotic-mediated killing that early stationary phase batch cultures. The efficacy in killing non-growing bacteria varies among the bactericidal antibiotics examined.
To ascertain the potential clinical implications of these density and physiological effects, we use both computer and in vitro simulations of antibiotic treatment. The results of these simulations provide compelling support for the proposition that antibiotic treatment regimes, including those designed to prevent the ascent of resistance, should take into account the anticipated density and physiological state of the target population of susceptible bacteria.
Viral infections of the central nervous system
S282 Modern molecular methods of diagnosis of viral encephalitis
H.G.M. Niesters* (Groningen, NL)
There have been an increasing number of neurotrophic viral infections playing an important role in the World over the last decade. The list includes West Nile Virus, Nipah and Hendra virus (both paramyxoviruses), as well as Chikungunya virus which suddenly emerged. Furthermore, the relation between JC virus in Progressive Multifocal Leukoencephalopathy (PML) in patients with multiple sclerosis treated with a new immunosuppressive drug, has triggered our attention.
The development and implementation of molecular based amplification method has assisted us to detect these viruses more efficiently. These technologies have been used now routinely in a large number of laboratories to enable the detection of more commonly known neurotrophic viruses, like HSV, VZV and the neurotrophic picornaviruses like enterovirus and parechovirus. The pitfalls of these molecular methods have been generally solved by implementing regular quality control testing schemes, like organised by QCMD (quality control of molecular diagnostics) and the introduction of internal controls during the whole diagnostic process. Finally, with the ability to quantify the amount of nucleic acid present in CSF, more information on the pathogenesis of these viral infections, as well as significant tool to monitor the antiviral effect of treatment options for these viruses, has become available.
S284 Changing epidemiology of viral encephalitis in the Old World
T. Avsic Zupanc* (Ljubljana, SI)
Encephalitis can be caused by wide variety of infectious agents, including viruses, bacteria, fungi and parasites. In addition to common viral pathogens, arthropod-borne viruses (transmitted through insect or tick-bite) can cause arboviral encephalitis. In Europe, the most important pathogens responsible for arboviral encephalitis are tick-borne encephalitis virus (TBEV), West Nile virus (WNV) and Sandfly fever virus (SFV). Tick-borne encephalitis (TBE) is the most important flavivirus infection of the central nervous system (CNS) in Europe and Russia. The epidemiology of TBE is closely related to the ecology and biology of ticks. In nature, TBE virus is propagated in a cycle involving permanently infected ticks and wild vertebrate hosts. Virus transmission occurs horizontally between tick vectors and vertebrates, with small mammals serving as virus reservoirs. TBE is distributed in an endemic pattern of natural foci over a wide geographical area focused on central Europe, the Baltic States and Russia. During the past two decades, both new endemic foci and an increase in cases have been reported in many European countries, with the major exception being Austria, which has a high vaccine coverage (>86%). The disease has also been considered outside the traditional endemic areas. Some reports of new endemic areas are attributed to a previous under diagnosis of cases. However, the true nature of this rise is supported by an increase in areas with high awareness of the disease and with well established diagnostic routines. Environmental factors important for sustaining natural foci for tick-borne encephalitis can be modeled with satellite data. These models suggest that climate change is partly responsible for increased incidence in Europe. But, existing methods for risk assessment have limitations. Thus, risk assessment should combine human habits and socioeconomic variables with functional variables in natural foci. West Nile virus (WNV) is a flavivirus that is maintained in a bird-mosquito transmission cycle. Humans and horses are usually incidental hosts. Historically, WNV has been associated with asymptomatic infections and sporadic disease outbreaks in humans and horses in Africa, Europe, and Asia. Although, WN fever was a minor arbovirosis, some cases of encephalitis associated with fatalities were reported in Israel in the 1950 s. However, after few silent decades, the virus has caused frequent outbreaks of severe neuroinvasive disease in humans and horses in Europe and the Mediterranean Basin. Even more, new modes of transmission through blood donations, organ transplants, and the intrauterine route have been reported. In Europe, an enhanced surveillance of WN infection in humans, horses, birds, and vectors may reveal the presence of the virus in different locations. Nevertheless, outbreaks of WN virus remain unpredictable. Further coordinated studies are needed for a better understanding of the ecology and the pathogenicity of the WN virus.
Autochthonous European parasites
S287 Tumours from the centre: Echinococcus multilocularis
P. Kern* (Ulm, DE)
Alveolar echinococcosis (AE) was first described by Rudolf Virchow. In his article “Die multilokuläre, ulcerirende Echinokokkengeschwulst der Leber” (1855) he clarified that the disease is caused by the larval stage of Echinococcus, and is not a form of cancer. It took another 100 years until the natural cycle involving foxes as definitive hosts and rodents as intermediate hosts was described. For many years, AE has been assigned to as a rare disease in Europe restricted to some endemic foci. However, current data suggest that the incidence of AE has significantly increased, and the disease is spreading to the North, West, and East. AE has become an emerging disease in the Baltic countries. Thus, human infections with E. multilocularis have arrived in the “centre” of Europe. AE is a life-threatening disease, and is characterised by a tumour-like lesion in the liver. The larva can infiltrate the surrounding tissues and metastasize to distant organs. In an attempt to classify the large variety of anatomical findings in AE, the PNM-classification system was developed and serves as a benchmark for standardised evaluation of diagnostic and therapeutic measures. Modern imaging techniques, such as ultrasound, CT or MRI and PET/CT contributed not only to a much better description of the lesions, but also to a judgment upon the activity of the metacestode. The differential diagnosis of AE varies from haemangioma-like lesion of the liver or cancer. The diagnostic skills are limited, and are the reason for frequent misdiagnosis in geographic areas where AE is rather unknown. Continuous treatment with benzimidazoles is the backbone of a lifelong management of AE. However, radical resection is the procedure of choice and should always be strived for. AE is still a rare disease in Europe, but where it occurs, it is often diagnosed too late. Patients are misdiagnosed for months and years, before receiving the correct treatment. At that late stage the disease has progressed, and radical cure of the liver lesion(s) is not anymore possible. Recent reports provided hints for an accelerated larval growth of Echinococcus spp. in the immunodeficient host. A careful monitoring of patients receiving immune-modifying drugs is warranted. The modern clinical management and long-term parasitostatic treatment with benzimidazoles are highly effective. Thus, a higher alertness for the “tumours from the centre” would increase the prognosis of this hepatic disease resembling liver cancer.
S288 Stage-specific approach and percutaneous treatment in the management of cystic echinococcosis
O. Akhan* (Ankara, TR)
The percutaneous treatment of liver hydatid cysts were considered to be contraindicated due to two main potential risks: anaphylactic shock and abdominal dissemination of the disease. Since the first case percutaneously treated was published, several series of successful percutaneous treatment of the liver and the other abdominal organs, peritoneum, thorax, soft tissue and orbital cavity hydatid cysts have appeared in the literature.
The main indication for percutaneous treatment of hydatid cyst includes “viable cysts”. Different types according to Gharbi or WHO classifications are treated by different percutaneous techniques. According to WHO classification, CE 1 and 3A are considered to be most appropriate for PAIR; CE 2 for Catheterisation technique or Modified catheterisation technique (MoCaT or PEVAC); CE 3B for MoCaT. No treatment is necessary in patients with CE 4 and 5 which are managed by “Wait and Watch approach”. Although surgery is a traditional method of treatment, the indication for surgery is now limited by the hydatid cysts ruptured into biliary system, pleura or peritoneum.
Three different techniques are used in percutaneous treatment of liver hydatid cysts. The first one is; the PAIR technique described by Ben-Amour et al. in 1986. PAIR is the abbreviation of Puncture, Aspiration of cyst content, Injection of hypertonic saline solution, and Reaspiration of all fluid. The second one is the Catheterisation technique with hypertonic saline and alcohol described by Akhan et al. in an experimental study in sheep in 1993. The third one is called as modified catheterisation techniques such as MoCaT or PEVAC. After standard steps of catheterisation techniques a 14F catheter is inserted into the cavity to evacuate all the content. Aggressive irrigation with isotonic NaCl is employed via the catheter to have the cavity emptied.
Considering the number of percutaneously treated patients, it is reasonable to conclude that the mortality rate is about 0.047%. Dissemination after percutaneous treatment of the liver hydatid disease was never reported in any of the published series. Other major complications need to be addressed are superinfection of the cavity, cystobiliary communication and severe anaphylactic reaction with a reported overall rate of about 10%. Minor complications such as urticaria, severe itching and hypotension can easily be treated with antihistaminic. In some patients fever, not exceeding 38.5°C, may also be observed and generally does not necessitate any medication.
Recurrence rate varies among 0–4%. Recurrent cysts are also managed by percutaneous approach. Considering the overall data in the literature regarding hospital stay is about 2.5–4.2 days.
Percutaneous treatment of hydatid liver disease is an effective and safe procedure with its unique advantages (e.g., shorter hospital stay, low complication rate). Today, the percutaneous approach has an important role in treatment of hydatid cysts not only in the liver but also in the other organs and tissue. Therefore it must be first treatment option whenever it is indicated.
S289 Frequent heart disease in dogs, emerging cutaneous disease in humans: dirofilariasis
P. Marty* (Nice, FR)
In Europe, Dirofilaria immitis and Dirofilaria repens are responsible of autochthonous filariases in dogs. Adults of D. immitis kills the dogs with an heart location and D. repens is often found in subcutaneous nodules in dogs and cats. The microfilariae are present in the blood of these animals. Dirofilariasis is due to the transmission of microfilariae by some mosquito bites (Aedes, Culex, Anopheles, Mansonia, Psorophora and Taeniorhynchus). Usually non pathogenic to humans, these parasites are particularly present around the Mediterranean basin. D. immitis is very rare in humans in Europe, sometimes found in a pulmonary nodule and the heart location is not described. D. repens is more frequent and emerging in humans. Usually, only one larva develops, producing an immature adult worm inside a subcutaneous nodule. Ultrasound examination may suggest the parasitic origin of the lesion before an extraction and a parasitological diagnosis of the worm. More often, a fortuitous diagnosis is made on histological examination. Very rarely, an adult worm may mature and produce systemic diffusion of microfilariae. Dirofilariasis due to D. repens can present problems in diagnosis and treatment. An ocular and subconjunctival location of the worm and a subcutaneous nodule enclosing an immature adult are the commonest clinical forms. Exceptional pulmonary locations are described. The subcutaneous locations described are: skull, cheek, breast, inguinal area, buttocks, arms and legs. Cases of testicular location with painful symptoms have been observed. Blood hypereosinophilia was exceptionally observed in human. It is treated surgically, by excision, without chemotherapy.
Current and future trends in rapid diagnostics for detection of nosocomial superbugs
S292 Current methods for rapid detection of ESBL
T. Naas* (Paris, FR)
While the majority of ESBLs, isolated in clinically-relevant Gram negative bacteria (GNB) (mostly Enterobacteriaceae, P. aeruginosa, A. baumannii) are TEM-, SHV- or CTX-M-types, a few others have been reported (SFO, BES, BEL, TLA, GES, BEL, PER, VEB-types, and some OXA-ESBLs). Laboratory detection of ESBL-producers is important to avoid clinical failure due to inappropriate antimicrobial therapy and to prevent nosocomial outbreaks.
Selective culture media (MacConkey and Drigalski agar supplemented with cefotaxime and/or ceftazidime) have been proposed for detection of GNB resistant to expanded-spectrum cephalosporins (ESC). Media using chromogenic based substrates and selective antibiotics have been developed recently for the detection and presumptive identification of ESBL-producing Enterobacteriaceae directly from clinical specimens. Detection of ESBLs based only on susceptibility testing is not easy due to the variety of β-lactamases and their variable expression of β-lactam resistance. Commercially available ESBL detection methods yield at most 90% accurate ESBL identification, since some ESBL-producers may appear susceptible to some ESCs. Therefore, any organism showing reduced susceptibility to ESC should be investigated using ESBL confirmatory tests. These tests should be able to discriminate between ESBL-producers and those with other mechanisms conferring ESC resistance. These phenotypic tests (double-disk synergy test, ESBL Etest, and the combination disk method) are based on clavulanate inhibition and ESC susceptibility testing. They often need slight changes by either reducing the distance between the disks of ESC and clavulanate, the use of cefepime (not hydrolysed by AmpCs), the use of cloxacillin-containing plates (that inhibits AmpC), or by double inhibition by EDTA and clavulanate (masking metallo-enzymes). Enzymatic tests have also been proposed for identification of ESBL-producers.
Several PCR-based techniques (end-point or real time) have been developed on clinical samples or on colonies. Several ESBL genes have been detected using PCR coupled to either pyrosequencing, inverse hybridisation, to dHPLC, or to fluorescent probes. These techniques even though more specific require technical knowledge, special equipment, are costly and detect only known genes, regardless of their expression. Detection of ESBL-producer remains a challenge for the microbiology laboratory and one shall be aware that ESBL screening media are now available.
S293 Future trends for rapid detection of antibiotic resistant pathogens
F. Tenover* (Sunnyvale, US)
Resistance to antimicrobial agents has become common in many bacterial species, particularly those that cause human infections. The rapid detection of resistant organisms directly in clinical samples by real-time PCR coupled with molecular beacons, or of potentially resistant bacteria and yeast in blood culture bottles by peptide nucleic acid-fluorescence in situ hybridisation (PNA-FISH) is already having a positive impact on antimicrobial therapy. The direct detection of Mycobacterium tuberculosis in sputum in approximately 2 hours with concomitant detection of mutations in rpoB indicating rifampin resistance (as a surrogate for multidrug resistance) in the near future will likely improve the outcomes for tuberculosis patients in many developing and developed countries. Several molecular technologies, including microarrays, bacterial tag encoded FLX amplicon pyrosequencing (bTEFAP), and ultra deep sequencing, have not yet transitioned to clinical laboratories but will likely provide even greater information about antimicrobial resistance not in just a single species, but in a whole community of microorganisms. Complex wounds, like diabetic foot ulcers, containing multiple resistance genotypes are amenable to analysis by bTEFAP. The implementation of these technologies in the clinical laboratory will be expensive but the potential to dramatically improve therapeutic outcomes especially for life-threatening diseases is unprecedented.
Antibiotic use in hospitals
O294 The ESAC Point Prevalence Survey of patterns of antibiotic use in 50 European hospitals in 2008
A. Muller*, B. Amadeo, E. Hendrickx, V. Vankerckhoven, P. Davey, H. Goossens on behalf of the ESAC Hospital Care Sub-project Group
Objectives: To perform a Point Prevalence Study (PPS) on antimicrobial prescription in a larger sample of European hospitals, as compared to the PPS-2006 study.
Methods: Data was collected during two subsequent calendar weeks in May-July 2008 in 50 hospitals in 26 European countries. The study protocol was a simplified version of the 2006 one. An internal web-based application was developed and PDA was used in a subset of hospitals. Antimicrobial prescriptions were recorded using the ATC classification. Demographic data on treated patients, indications, diagnoses, culture pre-therapy and reasons for treatment recorded in notes were collected.
Results: Among the 25,710 admitted patients, 8,126 (31%) received antimicrobials for a total of 11,208 therapies of which 5,601 (69%, 68% in 2006) were monotherapy. Antibiotics represented 90% of the prescriptions (range: 74–96). The most commonly prescribed antibiotics were penicillins with beta-lactamase inhibitor (22%, range: 0–55), cephalosporins (20%, range: 3–60), and fluoroquinolones (13%, range: 0–40). In intensive care wards, glycopeptides represented the third class (7%, range 0–25), followed by the fluoroquinolones. The proportions of parenteral use within the total antibiotic prescriptions, the penicillins and the fluoroquinolones were 74% (64% in 2006), 32% and 6% respectively, however wide variations occurred between hospitals. Infections represented 74% (78% in 2006) of all the indications. Among the curative treatments, 66% (62% in 2006) were for community-acquired infections. Pneumonia and skin and soft tissue infections were the predominating diagnoses representing respectively, 25% and 16%. Surgical prophylaxis represented 72% (68% in 2006) of all prophylactic treatments. The >1 day course for surgical prophylaxis that was already high in 2006 (56%) increased to 65% (range: 57–100 depending of the site) in 2008. The use of single dose pre-operative prophylaxis ranged from 0% to 91% within the hospitals.
Conclusion: The PPS 2008 results, based on a larger sample of hospitals and countries are in accordance with the 2006 PPS data. The survey confirmed the too long duration of surgical prophylaxis and the predominance of the parenteral route. ESAC successfully developed a web-based and PDA tool for surveying antibiotic use and quality assessment in European hospitals, which will be rolled out in 2009 to many European hospitals.
O295 Appropriateness of antimicrobial use in 11 Dutch hospitals
I. Willemsen*, J. Manniën, B. Benthem, J. Wille, J. Kluytmans (Breda, Bilthoven, Utrecht, Amsterdam, NL)
Objective: To determine the appropriateness of antimicrobial therapy (AMT) in 11 Dutch hospitals.
Method: Data were obtained from a prevalence survey performed within the Dutch surveillance network for nosocomial infections (PREZIES). AMT administrated on the day of the survey was registered. Antiviral and antifungal drugs, tuberculostatics, cements containing AMT and prophylaxis administrated in the operation-theatre were excluded. The appropriateness of AMT was assessed according to a standardised algorithm based on the local antimicrobial prescription guidelines. Per patient a classification in appropriate use, inappropriate use and insufficient information was made.
Results: A total of 3,546 patients were included of which 1,075 (30%, range per centre (RPC): 23–37%) received AMT. In the latter group, AMT was considered appropriate in 70% (RPC: 57–84%), inappropriate in 17% (RPC: 3–32%) and was not judged because of insufficient information in 13% (RPC: 1–30%). There was considerable variation in inappropriate use among the participating centres (figure ). In univariate analysis older age, the use of quinolones, being on the urology ward and presence of a suprapubical catheter were associated significantly with inappropriate use. Admission on the ICU and presence of an intravascular catheter were associated significantly with appropriate use. In a multivariate analyses the presence of suprapubical catheter, being on the urology ward and the use of quinolones were determinants for inappropriate use.
Figure.
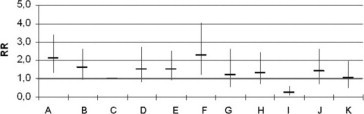
Relative risk of IA use of AMT against largest hospital (hospital C).
Conclusion: This study showed large differences in overall use and appropriateness of use of AMT between hospitals. Based on these results it is possible to define targets for intervention to improve the prudent use of AMT. The high fraction of patients with insufficient information in several centres may have influenced the analyses and should be addressed in future studies.
O296 Validation of quality indicators for hospital antibiotic use by the ABS International – Quality Indicators (QI) Project
M. Struelens*, S. Metz-Gercek, R. Mechtler, F. Buyle, A. Lechner, H. Mittermayer, F. Allerberger, W. Kern and the ABS QI Team & Feasibility Study Participants
Objectives: The EU-Project Antibiotic Strategy International (ABS) QI team developed process QIs for auditing the performance of key treatment and prophylactic practices. An international network of pilot hospitals tested these tools for feasibility, reliability and sensitivity to improvement.
Methods: QIs included:
-
1.
surgical prophylaxis (indication, drug choice, timing and duration of administration);
-
2.
management of community-acquired pneumonia (CAP) (blood culture and Legionella antigen tests and drug choice for empirical treatment);
-
3.
management of S. aureus bacteraemia (echocardiography, IV catheter removal and duration of therapy); and
-
4.
iv-po switch for bio-available antibiotics.
A minimum of 40 consecutive cases per centre and QI were retrospectively reviewed from clinical, laboratory and administrative records and assessed for data availability, inter-observer reliability, data collection workload and performance score.
Results: A total of 1240 patients were evaluated in 11 acute care hospitals from 5 countries, with a range of 80 to 500 cases and 2 to 9 centres per indicator. Seven centres had already implemented antibiotic quality improvement and audit programmes. Availability of data was >85% of cases and ranged between 87% (catheter removal in S. aureus bacteraemia) and 100% (diagnostic tests for CAP). 13/14 indicators were found to be reliable with kappa ≥ 0.60 (good to excellent agreement). The workload per case ranged from a median time of 16 (CAP) to 35 min (iv-po switch). The intention to treat QI scores showed high levels of adherence to the surgical prophylaxis QI bundle, with median values of 81 to 97% for hip prosthesis and 65 to 92% for colo-rectal surgery. For CAP management, diagnostic testing appeared sub-optimal (<56% compliance with IDSA guidelines). For S. aureus bacteraemia management, indicator results ranged from 60 to 65%. For use of bio available antibiotics, a median of 45% iv administrations were avoidable. There were marked differences of scores between centres for all QIs.
Conclusions: The ABS QIs are reliable and broadly applicable tools for auditing antibiotic treatment and prophylactic practices. Inter-hospital variation in adherence to recommended practice indicates substantial potential for improvement with different local priorities. These QIs can be recommended for assessing the effect of quality of care interventions at either local or multi-centre level.
O297 Does a laminated hand-held card describing antibiotic policy influence the junior doctor prescribing in a geriatric medicine department? A controlled interrupted time-series
D.J. Noimark*, E. Charani, S. Smith, B. Cooper, I. Balakrishnan, S.P. Stone (London, UK)
Introduction: Reduction of Clostridium difficile infection (CDI), which often follows use of third generation cephalosporins, is a national priority. Over a three year period, antibiotic policies were reviewed and changed in an elderly medicine department according to local sensitivities of common pathogens and levels of CDI. A laminated pocket-sized card describing antibiotic policies was given to all doctors in the department on induction with instructions not to depart from these without microbiologists' approval. This prospective controlled interrupted time series examines whether this intervention increased compliance with antibiotic policy and decreased CDI incidence.
Methods: The department's “narrow-spectrum, no cephalosporin” antibiotic policy was changed on 1st August 2006 to replace Trimethoprim with Cephradine (1st generation cephalopsporin) as empiric treatment for urinary tract infection, reflecting local Escheriscia Coli sensitivities. In October 2007, all cephalosporins and quinolones were removed from the policy as CDI levels had increased. Notional 7 day antibiotic usage was calculated from prospective pharmacy generated data with aspirin, calcium, bisphosphonate & laxative prescription use as a non-antibiotic control, and analysed by segmented regression with a robust variance estimator. CDI rates were prospectively collected separately & analysed by a Poisson regression model.
Results: An immediate response to change in antibiotic guidelines was observed (Figure ). From August 06-Sep 07 there was a highly significant increase in cephalosporins (85–100% of which was Cephradine alone) (p < 0.001), a significant fall in trimethoprim (p < 0.004) and a significant increasing trend in CDI (incidence rate ratio [95% CI]) for monthly increase: 1.07 [1.00, 1.14], p = 0.04). From Oct 07-Sep 08 there was a significant decrease in cephalosporins (p < 0.01), quinolones (p < 0.001) & CDI (IRR 0.78 [0.65, 0.94], p = 0.01) & a significant rise in trimethoprim (p < 0.001). There were no significant changes in other antibiotics including amino & benzyl penicillins & gentamicin. Control drug usage did not change except for laxatives.
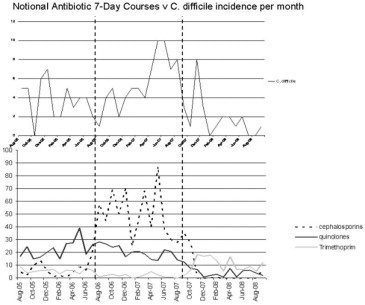
Conclusion: This study, which used a strong prospective quasiexperimental design, showed that a pocket-sized laminated card appeared to be an effective way to reinforce antibiotic policy and help control CDI. This is the first report to associate high CDI levels with 1st generation cephalosporins.
O298 When is a hospital ready to introduce electronic antimicrobial stewardship? The use of a Readiness Assessment Tool
S. Luu, K. Buising, M. Robertson, K. Thursky* (Melbourne, AU)
Background: A multidisciplinary team from The Royal Melbourne Hospital developed an electronic antimicrobial stewardship system called Guidance DS in 2005. Since then, this system has been successfully implemented at two other Melbourne hospitals. The impact of the system on antimicrobial usage and resistance has previously been reported [1]. Recently, the Victorian Government ‘Infection Control Strategy’ funded the introduction of electronic antimicrobial stewardship to all major public hospitals in the state. These hospitals had widely variable existing infectious diseases support, IT infrastructure and prescribing cultures. No tools existed to assess the readiness of public hospitals to receive this technology, and therefore guide resource allocation to facilitate implementation.
Aim: To assess the readiness of Victorian public hospitals to introduce electronic antimicrobial stewardship.
Method: Literature on readiness for change, organisational culture and information technology acceptance were reviewed. Group interviews with project teams at site initiation meetings, one on one interviews with project officers at subsequent meetings, and observation where appropriate were all used to determine potential barriers and enablers. This information was recorded using a ‘Readiness Assessment Tool’ and analysed to identify a number of key domains. To triangulate the data, questionnaires were distributed to project officers asking them to assess their sites' readiness to implement the system.
Results: A novel ‘Readiness Assessment Tool’ was developed. It covered the domains of technical readiness, skills readiness, process readiness, administrative support readiness, resource readiness and hospital organisational characteristics. Assessments at several hospitals highlighted a variety of issues at different sites and allowed early efforts to address these.
Conclusion: A formative readiness assessment can be used to identify systematic problems that might facilitate or hinder uptake of electronic antimicrobial stewardship and to inform the adopters of potential resources required.
O299 Fluoroquinolone prophylaxis in haematology-oncology patients – is it still useful?
W.V. Kern*, M. Steib-Bauert, A. Pritzkow, G. Peyerl-Hoffmann, H. von Baum, U. Frank, M. Dettenkofer, C. Schneider, K. de With, H. Bertz (Freiburg, Ulm, DE)
Objectives: Fluoroquinolone prophylaxis (FQPx) may reduce morbidity and mortality in cancer patients (pts) with neutropenia, but the development of fluoroquinolone resistance (FQR) in Escherichia coli and other target organisms limits its usefulness. We evaluated changes in the incidence density of Gram-negative bloodstream infection (GNB) and in the in vitro FQR rates after the introduction of FQPx (with levofloxacin) as a standard of care for pts with high risk neutropenia in a university hospital.
Methods: We collected individual data for 357 pts admitted during baseline and during the first months following the intervention to assess clinical outcomes. Individual pt data were compared with aggregate data (3-month periods). Aggregate data analysis (unit-wide antibiotic consumption, GNB and numbers of in vitro FQR bloodstream isolates) was continued for a total of eight 3-month periods for both the haematology-oncology service and for general internal medicine.
Results: The new policy was introduced in the second half of the year 2005 when unit-wide baseline FQR of E. coli and of coagulase-negative staphylococcal (CoNS) bloodstream isolates had been 15% and 80% in the haematology-oncology unit, and 8% and 60% in general internal medicine, respectively. The individual pt data analysis revealed that pts not given FQPx had a much higher incidence of GNB than those given FQPx (22/254 [9%] vs 2/103 [2%], p = 0.01) following the policy change, and this difference remained significant after adjustment for potentially confounding variables. Aggregate data also demonstrated this reduction in GNB incidence density, but only until the second quarter of 2007 after which the GNB incidence density rose to preintervention level. This was associated with increased FQR rates among E. coli bloodstream isolates from pts admitted to haematology-oncology (25% in 2006 vs 72% in 2007), but increased FQR rates among E. coli bloodstream isolates were also observed in general internal medicine pts (12% in 2006 vs 21% in 2007) although the FQ consumption had remained fairly stable in both services.
Conclusion: The efficacy of FQPx in cancer pts with neutropenia appears to diminish as FQR rates in E. coli isolates from pts in general internal medicine increase, possibly reflecting community trends relevant to the cancer pt setting. Based on aggregate data analysis, a resistance rate in general medicine exceeding 20% was associated with a virtually complete loss of FQPx efficacy.
O300 Improving antimicrobial use in the hospital: targeting quinolones using multiple interventions
I. Willemsen*, B. Cooper, C. Buitenen, M. Winter, J. Kluytmans (Breda, NL; London, UK; Amsterdam, NL)
Objectives: To determine the effects of interventions on the use of Quinolones (QUIN) in a hospital.
Methods: During a prospective study, from 2005 through 2007, 4 interventions to improve the use of QUIN were executed. First, promotion of a switch from IV to oral medication (01–2006); second, education programs for interns/residents and physicians and the release of a new antimicrobial formulary (06–2006); third, a restriction note was printed on all laboratory reports (10–2006); and fourth, active monitoring and feedback on prescriptions (01–2007). The monthly use of iv and oral QUIN was calculated based on data from the pharmacy department. Statistical analyses were performed using segmented linear regression analysis. Bayesian Model Averaging was used to account for model uncertainty.
Results: Before the interventions the use of QUIN (both iv and total) was stable. The best fitting models indicated that the first intervention was associated with a stepwise reduction in IV use of 71 prescribed daily doses (PDD) (95% CI: 47, 95 (p < 0.001)). There was also an indication of smaller reduction in IV use associated with intervention 4, but only the intervention 1 effect was robust to model uncertainty.
The overall use of QUIN was also significantly reduced (figure ) with a large stepwise reduction of 107 PDD (95% CI: 58, 156) associated with intervention 2.
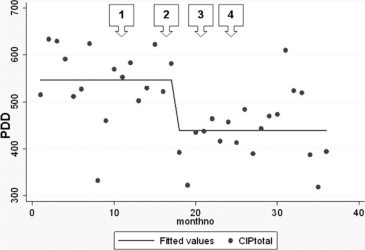
Conclusions: This study showed that the hospital-wide use of QUIN can be significantly improved (and decreased) by an active policy consisting of multiple interventions.
O301 Cohort study of adult patients with complicated skin and soft-tissue infections
C. Marwick*, J. Broomhall, C. McCowan, S. Gonzalez-McQuire, K. Akhras, S. Merchant, P. Davey (Dundee, High Wycombe, UK; Raritan, US)
Aim and Objectives: to describe the antibiotic treatment and outcomes stratified by severity in a representative sample of adult patients aged 18 or older who were treated in hospital for skin and soft tissue infections.
Background: Skin and soft tissue infection (SSTI) is one of the common indications for antimicrobial therapy in hospital. In the ESAC (European Surveillance of Antimicrobial Chemotherapy) point prevalence survey of 19 European hospitals in 2006 SSTI was the second most common infection after respiratory infection and accounted for 13% of all treatments. However, in comparison with respiratory infections there is little information about the outcomes of treatment for SSTI or about the validity of clinical severity scores.
Results: We identified 341 patients aged 18 or over in 2005 who had a new admission to Ninewells Hospital, Scotland between 1st January and 31st December 2005 and were discharged with one or more ICD10 codes for SSTI. There were 187 valid cases of SSTI. Microbiology samples (n = 480) were taken from 75% of patients. The most common isolates were Staphylococcus aureus (50% of positive cultures, of which 47% were MRSA) and Pseudomonas aeruginosa (17% of positive cultures). Death in hospital or within 30 days of treatment occurred in 19 (10%) patients. The patients received a total of 80 different empirical antimicrobial regimens. We stratified patients by Eron classification. We defined sepsis as presence of Systemic Inflammatory Response Syndrome (SIRS) and severe sepsis as a Standardised Early Warning Score >4. Two Infectious Diseases Physicians (CM and PD) independently judged empirical antimicrobial therapy as inadequate if it did not cover the most likely pathogens for any Eron Grade or if it was oral for Grades 2 to 4. Agreement between raters was 88%. Mortality and inadequate therapy both increased with Eron grade:
-
1.
No SIRS or co-morbidity: 45% patients, 4% mortality, 10% therapy inadequate.
-
2.
Significant co-morbidity but no SIRS: 33% patients, 7% mortality, 41% therapy inadequate.
-
3.
Sepsis, with SIRS: 17% of patients, 22% mortality, 40% therapy inadequate
-
4.
Severe sepsis: 5% of patients, 50% mortality, 100% therapy inadequate.
We also judged that 43% of patients received unnecessarily broad spectrum therapy.
Conclusions: SSTI is common and is associated with significant mortality. However, choice of empirical therapy is not evidence based, with significant under treatment of high risk patients.
O302 Formal infectious disease consultation is associated with decreased mortality in Staphylococcus aureus bacteraemia
J. O. Robinson*, S. Pozzi Langhi, M. Phillips, J. Pearson, K. Christiansen, G. Coombs, R. Murray (Perth, AU)
Objective: Staphylococcus aureus Bacteraemia (SAB) is associated with considerable mortality. We conducted a study to see if the direct input of an infectious disease specialist was associated with outcome.
Methods: A retrospective analysis on all methicillin resistant (MRSA) and a random subset of methicillin susceptible (MSSA) SAB over 10 years comparing those with to those without an infectious disease consultation (IDC). All blood cultures were phoned to the treating team by a microbiologist, but only formal clinical review of that patient was considered as IDC.
Results: Of 599 SAB episodes, 162 (27%) had an IDC. Patients with an IDC were younger (median 57 vs 65, p = 0.001), and more likely to be intravenous drug users (16.7% vs 4.1%, p < 0.001) but less likely to be resident in a long term care facility (6.8% vs 15.1%, p = 0.007) or indigenous (6.8% vs 12.8%, p = 0.038). Bone/joint infection and intravenous drug use were more frequently identified as the source of bacteraemia in the IDC group, whereas pneumonia or primary bacteraemia were less frequent. The proportion of SAB due to MRSA was similar between groups (33.2% vs 32.1%, p = 0.802). Length of stay was longer in the IDC group (29.5 vs 17 days, p < 0.001) and endocarditis (19.1% vs 7.3%, p < 0.001) and metastatic seeding (22.2% vs 10.1%, p < 0.001) were more frequent in the IDC group. However, SAPS scores were lower in IDC group (27 vs 37, p < 0.001), whilst ICU admission rates were similar between groups. The S. aureus isolate tested susceptible against initial therapy more frequently in the IDC group (88.9% vs 78.0%, p = 0.003). 7-day (3.1 vs 16.5%), 30-day (8.0% vs 27.0%) and 1-year mortality (22.2% vs 44.9%) were all lower in the IDC group (p < 0.001). Multivariate analysis showed that effective initial therapy was the only variable associated the protective effect of IDC.
Conclusion: All cause mortality was significantly lower in patient with SAB who had an infectious disease consult as a result of a higher proportion of effective initial antibiotic therapy.
O303 Determinants of antibiotic use in nursing homes in 18 European countries: results of the European Surveillance of Antimicrobial Consumption (ESAC) Nursing Homes subproject
B. Jans*, L. Fontaine, E. Hendrickx, A. Muller, V. Vankerckhoven, H. Goossens on behalf of the ESAC Nursing Home Subproject group
Objectives: In the framework of the nursing home (NH) subproject of the European Surveillance of Antimicrobial Consumption (ESAC) project, structural, functional and regulatory determinants of antibiotic (AB) use in NHs in Europe were explored.
Methods: A standardised questionnaire collected national data in 2008 on structural and functional features, characteristics of resident population, organisation of medical and nursing home care, and national/regional regulations on infection prevention and AB policy in NHs in 18 European countries.
Results: Eighteen countries returned the questionnaire. Important structural NH differences were observed between Member States (MS), especially regarding mean NH size, resident age and length of stay. Also, there was no unique scale/score measuring the NH case mix. Medical care, often provided by individual general practitioners (GP), was coordinated by a co-ordinating physician (CP) in 7 countries. The CPs were officially charged to develop the AB policy and to set up infection prevention in the NH in only 4 MS.
AB were mostly (16/17) prescribed by GPs and delivered by public (n = 14) or hospital pharmacies (n = 3). Surveillance of AB use in NHs was organised in only 4 MS. In 3 countries a NH specific pharmaceutical formulary was available. Prescription profiles by prescriber were available in 5 countries. Other quality improvement initiatives in NHs such as regular training of prescribers, promoting microbiological sampling, collection of antimicrobial resistance profiles or pharmacist advice on AB prescription were scarce. Guidelines for AB treatment of most frequent infections were available in many countries but were focussing on ambulatory care and did not consider the specific NH situation. Only in 1 country the presence of an infection control practitioner was compulsory and partnership with hospital infection control teams was legally imposed in 3 MS.
Conclusion: Important structural, functional and regulatory NH differences exist between EU countries. Specific tools to improve infection prevention and AB therapy in NHs should take into account these differences. A European NH network was created in the framework of the ESAC NH subproject, which will organise point prevalence surveys on AB use in 2009.
CTX-Ms for ever
O304 Emergence of CTX-M type ESBLs among urinary tract Escherichia coli in south-western Finland
J. Jalava*, O. Meurman, H. Marttila, A. Hakanen, M. Lindgren, K. Rantakokko-Jalava (Turku, FI)
Objectives: Extended-spectrum betalactamases (ESBLs), especially enzymes of the CTX-M group, are spreading rapidly in Europe. Enterobacteriaceae with reduced susceptibility to third generation cephalosporins and a positive ESBL confirmatory test are also increasing in Southwest Finland. The purpose of this work was to study the resistance genetics of these ESBL-positive Enterobacteriaceae.
Methods: The study comprises a total of 271 clinical Enterobacteriaceae strains isolated from both inpatient and outpatient specimens. All Enterobacteriaceae strains that were ESBL confirmatory test positive between January 2004 and December 2008 were included in this study (263 Escherichia coli, 8 Klebsiella pneumoniae, one isolate per patient). Of these strains, 225 (83%) were urine isolates.
Resistance determinations were done using disk diffusion method (CLSI) or Vitek 2 and ESBL confirmations by the double disk method using cefotaxime and ceftatzidime with and without clavulanate. Thus far, 219 strains (those collected by end of June 2008) have been analysed for the presence of the most important ESBL genes (TEM, SHV and CTX-M) using PCR and pyrosequencing as described before (Haanpera et al. AAC, 52:2632; 2008).
Results: In 2004 only 10 ESBL-positive strains were found. All of them harboured a CTX-M type ESBL gene. Since then, the number ESBL-producing Enterobacteriaceae strains has increased significantly being tenfold in 2008 compared to year 2004 (Figure ). A high majority, 197 (90%) of the 219 strains analysed thus far had a CTX-M-type ESBL gene. Most of those (79%) belonged to the CTX-M-1 group according to the pyrosequencing results. CTX-M-9 group was the next common, with 20% of the CTX-M genes belonging to this group. Only two strains with CTX-M group 2 enzyme were found.
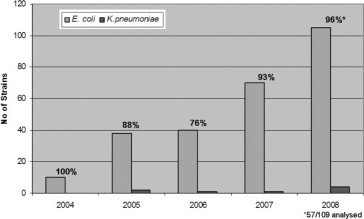
ESBL strains and the proportion of CTX-M genes in 2004–2008.
Conclusions: Enterobacteriaceae strains which produce ESBL are increasing rapidly in Southwest Finland. This is especially true with E. coli strains isolated from urine. Towards the end of the study period, the ESBL enzymes were almost exclusively CTX-M, CTX-M-1 group being the most common. Further research is needed to characterise genetic elements that carry these ESBL genes.
O305 International dissemination of extended-spectrum beta-lactamase CTX-M-14 in Enterobacteriaceae isolates is mainly associated with the spread of IncK and IncF plasmids
A. Valverde*, R. Canton, P. Hawkey, J.D. Pitout, P. Nordmann, L. Peixe, F. Baquero, T.M. Coque (Madrid, ES; Birmingham, UK; Calgary, CA; Paris, FR; Porto, PT)
Objectives: CTX-M-14 constitutes a widely spread extended-spectrum-beta-lactamase (ESBL), mainly in the community setting. Diversity of CTX-M-14-carrying plasmids of Enterobacteriaceae isolates from 8 countries is analyzed.
Methods: 52 Enterobacterial isolates [47 Escherichia coli (EC), 4 Klebsiella pneumoniae (KP) and 1 Citrobacter freundii (CF)] recovered (2000–2006) in France (n = 6), Spain (n = 4), Portugal (n = 6), UK (n = 11), Kuwait (n = 2), Canada (n = 13) and China (n = 10), including Hong Kong (n = 3) were studied. Clonality was established by PFGE and phylogenetic groups of EC and KP were determined as reported. Susceptibility testing (CLSI), blaCTX-M-14 transferability and location (I-Ceu-I/S1 nuclease) were investigated. Plasmid analysis included determination of Inc group (PCR-replicon typing, hybridisation, sequencing) and comparison of RFLP patterns. Association of blaCTX-M-14 with ISEcp1, ISEcp1-IS10 or ISCR1 was established by PCR and sequencing.
Results: We identified 42 PFGE types among 52 isolates: 38/47 EC, 3/4 KP and 1/1 CF. Distribution among phylogroups were as follows: i) EC: A (n = 7), B1 (n = 3), B2 (n = 5) and D (n = 23), and ii) KP: KpI (n = 2) and KpII (n = 1). Resistance to tetracycline (76%), nalidixic (74%), streptomycin (67%), sulfonamides (67%), ciprofloxacin (60%) and trimetroprim (43%) was common. Transfer of blaCTX-M-14 was achieved in 62% of the isolates. Analysis of plasmids showed 6 RFLP (Rx) patterns: i) types Ra, Rb, and Rc correspond to IncK plasmids (80 kb) found among different EC phylogroups, being Ra found among isolates of Spain, Portugal and Canada and Rb among those from UK and China; ii) types Rd, Re and Rf correspond to IncF plasmids (80 and 100 kb) of CF, EC-D and Kp respectively, being Re pattern identified in different clones of EC-D from Canada, and Rf from China and UK; iii) two IncHI2 plasmids of 242 kb from Spain were isolated from EC clones. blaCTX-M-14 was mainly identified downstream ISEcp1 in IncK or IncF plasmids or downstream ISEcp1 truncated by IS10 in an IncF plasmid (Re) from Canada (n = 5 isolates/2 clones). Association with ISCR1 was detected among IncHI2 plasmids.
Conclusions: International dissemination of blaCTX-M-14 is mainly associated to epidemic IncK and IncF plasmids. The association with specific EC clonal groups might have also contributed to its dissemination and maintenance.
O306 Diversity of conjugative blaCTX-M-carrying plasmids from Klebsiella pneumoniae strains in Slovenian hospitals
K. Mesko Meglic*, S. Koren, D.M. Livermore, A. Andlovic, S. Jeverica, V. Krizan-Hergouth, M. Mueller-Premru, K. Seme, N. Woodford on behalf of the Slovenian ESBL Study Group
Objectives: Diverse strains of K. pneumoniae with blaCTX-M were noted during a nationwide survey in Slovenia in 2005 and 2006. All had group 1 CTX-M genes, with blaCTX-M-15 identified by sequencing. Efficient in vitro transfer suggested that plasmids carrying blaCTX-M-15 were spreading horizontally in our hospitals and, here, we characterised the plasmids responsible in the major K. pneumoniae strains identified during the survey.
Methods: Plasmids from representative K. pneumoniae strains with CTX-M-15 enzyme were extracted by alkaline lysis and compared by ApaI, PstI and EcoRI restriction analysis. They were transferred into E. coli DH5a by electroporation. Transformants were selected on cefotaxime-containing agar and were screened by PCR for beta-lactamase genes, the aminoglycoside resistance genes aac(6')-Ib and aac3-IIb, and the plasmid-mediated quinolone resistance genes qnrA/B/S.
Results: Twelve isolates were characterised, representing 5 major strains (A-D, and F) found in the most-affected hospitals. Restriction analysis divided their plasmids into several groups. Representatives of strain A (n = 4) had essentially the same plasmid (group 1), as did the two representatives of strain D (group 2a). One strain F isolate had a plasmid (group 2b) very similar to plasmid 2a from strain D, indicating possible horizontal transfer. Plasmids of group 3 were retrieved from representatives of strains B and C, again indicating probable transfer. Plasmids from three other strains differed substantially from each other and from plasmids 1, 2a, 2b and 3. Nevertheless, on all plasmids, blaCTX-M genes were linked to an upstream ISEcp1 element, known to be involved in their mobilisation. All encoded multi-resistance: all but one group 1 and one ungrouped plasmid carried aac(6')-Ib; blaOXA-1 and aac(3)-IIa were detected on all except group 1 plasmids; blaTEM was found on group 1, 2b, one group 3 and two ungrouped plasmids. blaSHV and qnrA/B/S genes were not detected.
Conclusion: The considerable diversity of plasmids encoding CTX-M-15 enzyme in major Slovenian K. pneumoniae strains suggested only limited transfer, even when multiple strains were present in the same hospital. Evidence of plasmid transfer was between strains B and C, and possibly between strains D and F, although these plasmids were not strictly identical. Analysis of resistance genes encoded by the plasmids revealed diversity, with groupings coinciding largely with those based on restriction profiles.
O307 Regional study of the genetic context of class 1 integron harbouring blaCTX-M-2 linked to ISCR1 in nosocomial Klebsiella pneumoniae isolates from Uruguay, Argentina and Chile
A. Ingold, G. Borthagaray, A.K. Merkier, D. Centrón, H. Bello, C.M. Márquez* (Montevideo, UY; Buenos Aires, AR; Concepción, CL)
Objectives: To examine the genetic context of class 1 integron harbouring blaCTX-M-2 in fifteen nosocomial K. pneumoniae isolates from South America in order to enhance the understanding of the antibiotic resistance spread among the region.
Methods: DNA was extracted with the use of AxyPrepTM Bacterial Genomic DNA Miniprep Kit. The analysis of the cassette array was carried out with the use of primers HS458/HS459 targeting adjacent conserved regions.
The examination of the surroundings were performed using two PCR primer pairs, HS817/HS818 and HS825/HS826, to amplify the initial(IRi) and the terminal(IRt), inverted repeat boundary, respectively. The primer pair HS825/HS911 was used whenever a negative result was obtained with HS825/HS826. All PCR products were purified and sequenced and the data was analyzed with NCBI Blast Tool.
Results: The sequence obtained with primers HS817/HS818 revealed the presence of three different transposons backbones at the IRi end. The Tn5036-like module and the Tn21-like module were present in 4 isolates, the Tn1696-like module was present in 7 isolates. No amplicons were obtained with the use of primers HS825/HS826 that amplify a Tn21-like insertion. Two Uruguayan isolates with a Tn5036 boundary at the IRi end were tested with HS825/HS911 that target a Tn5036-like backbone and one generated a product consistent with a Tn5036-like mer region. Uruguayan isolates carried a single aadA1 cassette (4/5) and the other one contained a dfrA17-aadA5 array, while the four Argentinian isolates carried the combination aacA4-aadA1-orfD. Chilean isolates arrays are in process.
Conclusions: Among the extended-spectrum beta-lactamases, the cefotaximases constitute a rapidly growing cluster of enzymes that have disseminated geographically. There is a high frequency of isolation of CTX-M-2 producing K. pneumoniae associated with a class 1 integron in the region. Despite being common the presence of ISCR1 linked to blaCTX-M-2 in K. pneumoniae isolates, this study provides new and relevant information in the sequence context at the IRi. Here we report about the cassette array diversity and the diversity of elements in which the class 1 integron are embedded. Different integron/transposons carrying the blaCTX-M-2 gene seem to be circulating and different regional patterns could be emerging, this study highlights the ability of different genetic elements to act cooperatively to spread and rearrange antibiotic resistance.
O308 Escherichia coli clones and plasmid-mediated later transfer disseminate CTX-M-1 and CTX-M-32 among animals and humans
L. Vinué, A. García-Fernández, D. Fortini, P. Poeta, M.A. Moreno, C. Torres, A. Carattoli* (Logroño, ES; Rome, IT; Vila Real, PT; Madrid, ES)
Objectives: CTX-M enzymes are frequently detected in Europe. In particular, CTX-M-1 and CTX-M-32-producing strains have been recovered from both humans and farm animals in Spain, Italy, Greece, and Portugal, suggesting the existence of community reservoirs for these enzymes. The aim of this study was to compare Escherichia coli strains and plasmids harbouring blaCTX-M-1 and blaCTX-M-32 genes isolated from human and animals.
Methods: Four E. coli CTX-M-1 and eight CTX-M-32 epidemiologically unrelated producers from sick or healthy animals (pig, dog, cow and chickens) and from humans (urine, blood and faecal samples) were analysed by XbaI-PFGE, plasmid transferability, PCR-based replicon typing, plasmid restriction analysis and Southern blot hybridisation. All isolates were from Spain but the dog isolate was from Portugal. The genetic context of the blaCTX-M genes was previously investigated for all the strains.
Results: three CTX-M-32 strains (one from healthy chicken and two from hospitalised patients) showed the same PFGE pattern. A chromosomal localisation of the blaCTX-M-32 gene was suspected in these strains. The five remaining CTX-M-32 producers showed the blaCTX-M-32 gene on plasmids belonging to the IncN (4 strains) or untypable groups (1 strain). Two IncN plasmids showed identical PvuII-restriction patterns: one was identified in a strain from a healthy chicken and one was from a hospitalised human patient; these two strains were isolated in 2002 and 2004, respectively and showed different PFGE patterns.
CTX-M-1 producers (three from animal strains and one a healthy human) did not show clonality by PFGE and the blaCTX-M-1 gene was always located on plasmids, three belonging to the IncN and one to the IncI1 groups. Two of the IncN plasmids carrying the blaCTX-M-1 gene showed highly related restriction patterns: one was from a healthy dog and one from a healthy human.
Conclusion: This study demonstrated the presence of clonal E. coli CTX-M-32 producers in animal and human sources and also detected epidemic IncN plasmids disseminating among unrelated isolates from humans and animals, clearly suggesting a potential animal reservoir for the blaCTX-M-1/32 genes.
Wide spectrum beta-lactamases in Pseudomonas
O309 Characterisation of blaDIM-1, a novel integron-located metallo-beta-lactamase gene from a Pseudomonas stutzeri clinical isolate in the Netherlands
L. Poirel*, J. Rodriguez-Martinez, N. Al Naiemi, Y. Debets-Ossenkopp, P. Nordmann (K.-Bicetre, FR; Amsterdam, NL)
Objectives: Characterisation of the mechanism involved in the uncommon resistance to carbapenems observed from a Pseudomonas stutzeri isolate recovered from a patient hospitalised in the Netherlands with a chronic tibia osteomyelitis. That strain was resistant to ticarcillin, piperacillin-tazobactam, imipenem and meropenem, of intermediate susceptibility to ceftazidime and cefepime, and susceptible to aztreonam.
Methods: Screening for metallo-beta-lactamase (MBL) production was performed using the E-test method with a strip combining imipenem and EDTA. Shotgun cloning was performed with XbaI-digested DNA of P. stutzeri and pBK-CMV cloning vector. Selection was performed on amoxicillin and kanamycin-containing plates.
Results: E. coli TOP10 (pDIM-1) recombinant strains were obtained, displaying resistance to penicillins and ceftazidime, reduced susceptibility to cefepime, imipenem and meropenem, and full susceptibility to aztreonam. Sequence analysis identified a novel Ambler class B beta-lactamase DIM-1 for “Dutch IMipenemase” (pI 6.1) weakly related to all other MBLs. DIM-1 shared 52% amino acid identity with the most closely related MBL GIM-1, and 45 and 30% identity with the IMP and VIM subgroups, respectively. DIM-1 hydrolyzes very efficiently imipenem and meropenem, expanded-spectrum cephalosporins, but spares aztreonam. The blaDIM-1 gene was as a form of a gene cassette located at the first position in a class 1 integron, but the 59be of that gene cassette was truncated giving rise to a fusion with an aadB gene cassette encoding an aminoglycoside adenylyltransferase. The third and last gene cassette corresponded to the qacH cassette encoding resistance to disinfectants.
Conclusion: A novel MBL gene was identified in P. stutzeri further underlining (i) the diversity of acquired MBL genes, especially among non-fermenters, (ii) that Pseudomonas sp. may be a reservoir of these genes and (iii) the possibility of spread of important resistance determinants in Northern part of Europe.
O310 Metallo-beta-lactamases in Pseudomonas aeruginosa clinical isolates in Greece
P. Giakkoupi, O. Pappa, M. Polemis, A. Bakosi, A. Vatopoulos * (Athens, GR)
Objectives: Metallo-beta-lactamases of the VIM family are the main mechanism of carbapenem resistance in P. aeruginosa in Greece. In this preliminary report we attempted to survey the subtypes of VIM beta-lactamase currently prevailing in P. aeruginosa clinical isolates in Greek hospitals, the genetic relatedness of the respective isolates, as well as the genetic environment of the blaVIM gene.
Methods: Fifteen MBL producing and epidemiologically unrelated P. aeruginosa clinical isolates were collected in September 2006 from fifteen different hospitals around Greece. MBL production was initially identified by an EDTA synergy test. Identification of blaVIM gene, as well as mapping of the blaVIM cassette carrying integrons were performed by PCR and sequencing of the products. The O serotypes of the isolates were determined by a slide agglutination test using P. aeruginosa antisera (Biorad). Molecular typing was performed by pulse-field gel electrophoresis of SpeI-restricted genomic DNA.
Results: blaVIM-2 gene was detected in nine isolates, blaVIM-4 in five and blaVIM-1 in only one isolate. The blaVIM-2 cassette of all nine isolates was located on the 1600 bp variable region of a class I integron, preceded by aacA29 gene cassette. blaVIM-4 cassette of all five isolates was the first cassette of the 3200 bp variable region of a class I integron, followed by the aacA4 and blaPSE-1 gene cassettes. blaVIM-1 was the unique cassette of a class I integron. VIM-2 producers belonged to O8, O11 and O12 serotypes, whereas four isolates were non-typeable. VIM-4 producers belonged to the same three serotypes, whereas only one was non-typeable. The VIM-1 producer belonged to O12 serotype. The nine VIM-2 producing P. aeruginosa isolates revealed a great degree of variability in PFGE molecular typing, belonging to seven types. Contrary, the five VIM-4 producing P. aeruginosa isolates displayed higher genetic similarity and fell into one major type with 85% homology, which also included the VIM-1 producing isolate. There was no correlation between the results of serotyping and molecular typing.
Conclusions: MBL production in P. aeruginosa in Greece seems to be mainly due to specific class I integrons harbouring either blaVIM-2 or blaVIM-4 genes. Genetic variability was higher among bacteria carrying VIM-2 beta-lactamase, a fact indicating wider intraclonar spread of the respective integron.
O311 Extended-spectrum cephalosporinases hydrolysing carbapenems in Pseudomonas aeruginosa
J.M. Rodriguez-Martinez, L. Poirel*, P. Nordmann (K.-Bicetre, FR)
Objectives: Extended-spectrum beta-lactamases of AmpC-type (ESACs) contributing to reduced susceptibility to imipenem have been recently reported from Enterobacteriaceae. The aim of the study was to evaluate the putative role of natural AmpC-type beta-lactamases of P. aeruginosa in a similar resistance profile.
Methods: Thirty-two non-repetitive P. aeruginosa clinical isolates recovered in our hospital in 2007 were included. They were selected on the basis of criteria of intermediate susceptibility or resistance to ceftazidime and intermediate susceptibility or resistance to imipenem. MICs were determined by agar dilution and E-test techniques. The level of expression of the AmpC beta-lactamases was evaluated by measuring specific activities. PCR, sequencing, and cloning allowed to characterise the different bla(ampC) genes. Identified ESACs were purified and their Km and kcat values for beta-lactams determined by spectrophotometry.
Results: Using cloxacillin-containing (an AmpC beta-lactamase inhibitor) plates, the susceptibility to ceftazidime was restored for 25 out of 32 isolates, suggesting overproduction of the AmpC. In addition, in presence of cloxacillin, reduced MIC values were also observed with ceftazidime, cefepime and imipenem for 21 out of those 25 isolates. Cloning and sequencing identified 10 distinct AmpC β-lactamase variants among the 32 isolates. Recombinant plasmids expressing the AmpCs were transformed into reference P. aeruginosa strain and reduced susceptibility to cefepime and imipenem was observed only with recombinant P. aeruginosa strains expressing AmpC beta-lactamases that had an arginine residue at position 105. The catalytic efficiencies (kcat/Km) of the AmpC variants possessing this arginine residue were increased against oxyiminocephalosporins and imipenem. In addition, in-vitro assays demonstrated that those AmpC variants constituted a favourable background for selection of additional degree of carbapenem resistance.
Conclusions: Some AmpCs of P. aeruginosa possessing extended activity torward carbapenems may contribute to carbapenem resistance.
O312 Two novel OXA-type extended-spectrum b-lactamase in Pseudomonas aeruginosa in Hunan province, China: blaOXA-128 and blaOXA-129
W.E. Liu*, X.Y. Liu, Y.L. Zhang, X.H. Liang, H.L. Li, J.Z. Liao, Z.J. Jian (Changsha, CN)
Background: Most OXA-type ESBLs are OXA-10, OXA-2 or OXA-1 derivatives. They display a very low homology, the percentage of which is between 20% and 30%. OXA-type ESBLs are divided into five groups according to the different homology by Frederic Bert, etc. Group 1 includes OXA-5, OXA-7, OXA-10 and its derivants; Group 2 includes OXA-2, OXA-3, OXA-15 and OXA-20; Group 3 includes OXA-1, OXA-4, OXA-30 and OXA-31; Group 4 is named after OXA-9; Group 5 only includes a single enzyme called LCR-1. OXA-type ESBLs has been reported widespread in the world since the first report in 1987, such as Turkey, France, England and so on. But there is few report about it in China.
Objective: To investigate the prevalence and genotype distribution of OXA-type extended-spectrum beta-lactamases (ESBLs) in clinical Pseudomonas aeruginosa strains isolated from Xiangya Hospital of Central South University in Changsha city, Hunan Province, China.
Methods: Ninety-seven non-repetitive clinical isolates of P. aeruginosa were collected between October 2006 and January 2007 from the hospital. They were screened for OXA-type ESBLS production by polymerase chain reaction PCR with five pairs of primes specific for blaOXA genes, respectively. Then amplification of OXA-type ESBLS production was performed by PCR with specific primers. The purified and amplified products were sequenced to confirm the genotype of the OXA-type ESBLS.
Results: The sequences of the three OXA-type ESBLS PCR products were then compared in GenBank database and there were no the completely same ribonucleotide and amino acid sequence with them. They were two novel OXA-type ESBLS, named as blaOXA-128 and blaOXA-129, which have been registered in GenBank database under accession numbers EU573214 and EU573215, respectively.
Conclusions: There have occurred infections caused by P. aeruginosa producing OXA-type ESBLs in Xiangya Hospital of Central South University. Two novel OXA-type ESBLS in P. aeruginosa strains have been discovered in our study, which are named blaOXA-128 and blaOXA-129, respectively.
Nosocomial pneumonia: the role of multidrug-resistant Gram-positive infections (Symposium organised by Astellas)
S314 Nosocomial pneumonia: the role of multidrug-resistant Gram-positive infections
E. Bouza (Madrid, ES) A.P. MacGowan (Bristol, UK); R. Read (Sheffield, UK)
Pneumonia is one of the most common nosocomial infections and is associated with high mortality. In the last 15 years, Gram-positive bacterial pathogens have risen in prevalence as a cause of hospital-acquired pneumonia (HAP), including that occurring during mechanical ventilation (ventilator-associated pneumonia; VAP). In particular, Staphylococcus aureus is a major cause of HAP, including VAP. The rise of multidrug-resistant infections is a source of concern, with methicillin-resistant S. aureus (MRSA) accounting for >40% of S. aureus isolates in some European hospitals. This symposium will take the format of a question-and-answer roundtable session in which experts will answer questions and initiate discussion surrounding emerging concerns and appropriate therapeutic strategies in nosocomial pneumonia, including that caused by multidrug-resistant Gram-positive pathogens.
Recently, shifts in the susceptibility of S. aureus to established therapeutic agents for nosocomial pneumonia have added to the challenge of selecting appropriate empiric therapy. In patients with suspected multidrug-resistant infections or those who are mechanically ventilated, prompt initiation of therapy, often before the pathogen has been confirmed, is critical. Vancomycin is the gold-standard treatment for multidrug-resistant infections and resistance has been remarkably slow to emerge. However, clinical reports in Europe of ‘MIC creep’ and the emergence of vancomycin-intermediate S. aureus (VISA), hVISA and linezolid-resistant MRSA have presented new clinical dilemmas. Elevated vancomycin MICs are linked to treatment failure and increased mortality. Hence, while vancomycin remains a useful therapeutic tool, treatment decisions present an increasing challenge, especially in groups of patients in whom rapid eradication of infection with appropriate agents is critical.
Telavancin is a novel lipoglycopeptide under investigation for treatment of nosocomial pneumonia. A number of key features suggest telavancin as a potentially attractive option for nosocomial pneumonia. Telavancin has a unique dual mechanism of action that disrupts both bacterial cell wall biosynthesis and cell membrane integrity. The agent is rapidly bactericidal against a broad range of clinically relevant Gram-positive bacteria, including MRSA. Two pivotal Phase III studies have demonstrated telavancin efficacy equivalent to vancomycin in HAP, including VAP, including in seriously ill patient subgroups and in that caused by MRSA.
Hantavirus infections in Europe
K328 Hantavirus infections in Europe
A. Vaheri* (Helsinki, FI)
Hantaviruses are enveloped RNA viruses, each carried primarily by rodents or insectivores of specific host species. They have coevolved with the hosts in which they cause almost asymptomatic and persistent infections. In humans some hantaviruses cause disease: haemorrhagic fever with renal syndrome (HFRS) in Eurasia. In Europe Puumala (PUUV) from bank voles and Saaremaa (SAAV) from field mice cause mild HFRS and Dobrava (DOBV) from yellow-necked mice severe HFRS. In Asia HFRS is caused mainly by Hantaan and Seoul viruses. In Americas some viruses cause hantavirus cardiopulmonary syndrome: Sin Nombre, Andes and other viruses carried by sigmodontine rodents, not found in Eurasia. In addition, in Europe the common vole carries Tula and rats Seoul virus. However, they have not been definitely associated with disease in Europe, although both can infect humans. We discuss the epidemiology, molecular genetics, detection of infection in carrier hosts and humans (including RT-PCR and 5-min serological tests), functions of hantaviral proteins, risk factors for humans to catch hantavirus infection (including smoking) and disease (including risk and protective HLA haplotypes), role and mapping of epitopes of cytotoxic T-cells, mechanisms of hantavirus-induced apoptosis, newly discovered clinical features (including hypophyseal haemorrhages in PUUV infection), and long-term consequences and pathogenesis of HFRS (endothelial permeability, thrombocytopenia, TNF-alpha and IL-6).
PUUV occurs widely in Europe except in the far north and Mediterranean regions, SAAV in northern, eastern and central Europe and DOBV mainly in the Balkans. The epidemiological patterns differ: in western and central Europe HFRS epidemics follow mast years with increased oak and beech seed production promoting rodent breeding. In the north, hantavirus infections and HFRS epidemics occur in 3–4 year cycles, driven by prey-predator interactions. The infections and HFRS are on the increase in Europe, partly because of better diagnostics and partly perhaps due to environmental changes. In several European countries hantavirus infections are notifiable and in some countries (e.g. Belgium, Finland, France, Germany, Scandinavian countries, Slovenia) their epidemiology is relatively well studied. In large areas of Europe, however, hantavirus infections and HFRS have not been studied systematically and they are still heavily under-diagnosed.
MRSA screening – will we ever agree?
S330 MRSA: universal screening!
L. Peterson*, A. Robicsek (Evanston, US)
The successful control of any outbreak or epidemic relies on detection of those harbouring the pathogen (infected and colonised persons) combined with eliminating spread to new individuals. The approach to containment and reduction of the global MRSA pandemic is now being discussed. A challenge for this infection is that most persons harbouring MRSA do not exhibit signs of disease and thus in order to detect all potential spreaders of this organism some surveillance must be done. The required level of detection (surveillance through screening) is not known and likely varies with the prevalence of colonisation and disease. For a given MRSA prevalence, the factor that seems most crucial in reducing spread is the percentage of potential isolation days captured. The operational processes that highly influence this are 1) the sensitivity of screening detection (including sites tested and laboratory methods used), 2) the speed at which results of newly detected positive patients are reported from the laboratory (assuming pre-emptive isolation is not employed), and 3) the selection of patient populations who are to undergo screening. Laboratory testing has a major impact on detecting MRSA colonised patients with real-time PCR having a sensitivity of 98% and a possible 2 hour reporting time compared to direct chromogenic agar cultures with a sensitivity of 80% and >24 hour reporting and enriched chromogenic agar testing with a sensitivity of 90% and >48 hour reporting (Am J Clin Pathol, 2009); both reduced sensitivity and prolonged reporting time negatively impacting the success of MRSA timely isolation. We have shown that capturing 33% of MRSA isolation days in a modest MRSA prevalence setting (9 infections/10,000 patient days) with a high sensitivity test having a >24 hour result reporting time did not reduce hospital-wide MRSA disease (Ann Int Med 148:209, 2008). Others have demonstrated that surveillance in an ICU with similar MRSA prevalence, again with a high sensitivity test having 1 day result reporting, did not reduce ICU disease until preemptive isolation was initiated (Crit Care 10:R25, 2006). Finally, we demonstrated that universal admission surveillance and decolonisation capturing 85% of possible MRSA isolation days had a dramatic impact by reducing 70% of all in-hospital infections from MRSA. Future research in this area should focus on better defining those patients that benefit from MRSA screening and the role of decolonisation in these programs.
Update on Clostridium difficile
S334 Update on Clostridium difficile pathogenesis
M. Rupnik* (Maribor, SI)
Clostridium difficile infection (CDI) is a toxin-mediated intestinal disease and extraintestinal manifestations are exceptional. Clinical outcomes can range from asymptomatic colonisation to mild diarrhoea and more severe disease characterised by inflammatory lesions and pseudomembranes in the colon, toxic megacolon or bowel perforation, sepsis, shock, and death.
The main clinical symptoms, secretory diarrhoea and inflammation of colonic mucosa, can be in great part explained by the actions of two large protein toxins, toxin A (TcdA) and toxin B (TcdB). Both toxins are cytotoxic, destroy the intestinal epithelium and decrease colonic barrier function by disruption of the actin cytoskeleton and tight junctions resulting in a decreased transepithelial resistance allowing fluid accumulation. In addition, C. difficile toxins also cause release of various inflammatory mediators which affect enteric nerves, sensory neurons and promote inflammatory cells, adding to the fluid secretion, inflammation and transmigration of neutrophils.
Some experimental evidence points also to possible extraintestinal action of C. difficile toxin B. In zebrafish embryos TcdB caused damage and edema in cardiac tissue and in hamsters the same toxin caused lung damage.
Only recently efficient systems have been developed to genetically manipulate C. difficile. Comparison of knock-out mutants producing only one of both toxins have shown that TcdB-positive-only mutants retain the ability to kill hamsters, whereas TcdA-positive-only mutants were not virulent for hamsters. These results are in concordance with epidemiological findings that naturally occurring A-B+ strains still cause the entire spectrum of CDI, but are not in concordance with effects observed after intragastric challenge of hamsters with purified toxins TcdA and TcdB.
The role of the third toxin produced by C. difficile, binary toxin CDT in the development of human disease is not well understood. CDT was shown to have enterotoxic effect in rabbit ileal loop assay, but natural strains producing CDT but neither TcdA nor TcdB colonised animals but were not lethal in hamsters.
Comparative genomic analysis will most likely reveal additional factors involved in pathogenesis and in increased virulence (including cell surface layer proteins, sporulation characteristics and antibiotic resistance). Additionally, the role of the host immune response in CDI has just started to be better understood.
S335 New developments in the laboratory diagnosis and epidemiology of Clostridium difficile infection
T. Riley* (Perth, AU)
Since 2002, there has been an escalation in rates of Clostridium difficile infection (CDI) with epidemic C. difficile (PCR ribotype 027/North American pulsed-field type 1 [NAP1]) responsible for outbreaks of severe infection in North America and Europe. While fluoroqinolone resistance and over-use are thought to be driving the epidemic, the ageing population and improved case ascertainment are contributing to the dramatic increase in cases. Other factors may also be important, such as the increase in prescription of proton pump inhibitors. In The Netherlands, since 2005, there has been an increase in prevalence of human CDI with ribotype 078 strains usually found in animals. These infections were in a younger population and more frequently community acquired. There was alarm when it was reported that 20% of retail beef samples in Canada contained C. difficile. The figure is higher in the USA where more than 40% of packaged meats (beef, pork and turkey) from 3 Arizona stores contained C. difficile. Most animal isolates of C. difficile produce binary toxin, and both pigs and cattle harbour PCR ribotype 078 a strain that, like ribotype 027, also produces more toxins A and B, and binary toxin. In the eastern part of The Netherlands where >90% of pig farms are located, >20% of human isolates are now ribotype 078, and human and pig strains of C. difficile are highly genetically related. It has been suggested that the overlap between the location of pig farms in The Netherlands and the occurrence of human ribotype 078 infections involves a common source. That source is likely to be the environment. The upsurge in CDI has prompted diagnostic companies to try to either improve current tests or develop new ones. Laboratory diagnostic methods can be divided into 3 groups; traditional faecal cytotoxin detection (with or without culture), enzyme immunoassays (EIAs) and molecular methods. Faecal cytotoxin detection is specific but lacks sensitivity, culture is sensitive but lacks specificity. New EIAs should find a niche in medium sized laboratories. Current in-house PCR methods have the potential for great sensitivity and specificity but have been available only in larger laboratories. New commercially-available platforms will make this methodology more accessible to smaller laboratories. Whatever method is chosen, it is necessary for the laboratory to have as fast a turn-around-time as possible, particularly in an outbreak situation.
HPV vaccine
S336 Why did France introduce the anti-HPV vaccine?
D. Lévy-Bruhl* (Saint-Maurice, FR)
In 2005, the Advisory Board on Immunisation (ABI) has been asked to make recommendations to the Ministry of Health regarding the inclusion or not in the French immunisation schedule of the soon to be licensed first HPV vaccine. The main elements considered in the establishment of the benefit-risk balance of routine HPV vaccination were:
On the benefit side:
-
–
the very significant potentially preventable burden of diseases;
-
–
the very high efficacy of the vaccine against persistent HPV 16/18 infections in naive subjects;
-
–
the expected additional impact on other HPV16/18 related lesions and cancers;
-
–
the fact that vaccination, by preventing the pre-cancerous lesions, has the advantage over screening to reduce the cost and anxiety related to their detection and management;
-
–
the available data in favour of a satisfactory safety profile;
-
–
the benefit of vaccination for the women not covered by the opportunistic screening program.
On the “risk” side:
-
–
the high cost of vaccination;
-
–
the unknown duration of protection;
-
–
the need for continuation of screening, even for vaccinated women;
-
–
the fact that the majority of residual cervical cancers could be prevented by the organisation of the screening program;
-
–
the risk of a decrease in compliance to screening for vaccinated women;
-
–
the low benefit if vaccinated and screened women were the same.
A cost effectiveness analysis, carried out on a multi cohort Markov model, showed that, over a 70 years period, the impact of vaccinating 80% of 14 years old girls or of organising the screening were comparable (reduction of cancer deaths close to 20%). However, the cost-effectiveness ratio of the vaccination was higher than that of the screening organisation, resp. 45,200 and 22,700 € per life year saved (at a 3% discount rate). On the basis of the economical analysis, the screening organisation was therefore the first priority. However, if both interventions were implemented, the overall reduction in cervical cancer deaths was estimated at 32%. The cost-effectiveness of the addition of vaccination on the top of the organisation of the screening appeared acceptable (55,000 € per life year saved).
Based on those results, the ABI issued in March 2007 a recommendation to include the HPV vaccination in the immunisation schedule for 14 years old girls, together with a catch up for 15 to 23 years old women not having started their sexual life more than one year ago. The vaccine cost has been reimbursed since July 2007.
Clinical microbiology – is outsourcing the way to go?
S338 The (r)evolution of clinical microbiology in Europe – is it good or bad?
G. Kahlmeter* (Växjö, SE)
Laboratory medicine in general and clinical microbiology in particular is presently subject to rapid (r)evolution. Are we aware? Are we in command? Do we know where we are going? Should we oppose or cooperate? Do we have a choice? Do we recognise a driving force other than money? Is it good, bad or just plain necessary? And are we gaining or losing?
It is not one evolutionary process – it is several parallel processes with varying emphasis in different areas. There are at least four distinctive major trends over the last 15 years; the gradual formation of bigger and bigger units (concentration), the amalgamation of many different laboratory services into one (Laboratory medicine), accreditation and an explosion of professional proficiencies and backgrounds of staff in microbiological laboratories. Personally I have withstood the first two, with pleasure succumbed to the latter. A recent 5th trend, outsourcing microbiology services to large private consortiums, is splitting clinical microbiology into a purely analytical high-throughput money-saving activity, often leaving the consultative, clinical part of microbiology and health care infection control adrift.
What is driving the evolution? Not only cost-saving but also our inability to recruit medically trained microbiologists, the need to broaden the knowledge base of microbiology laboratories, automation, the development of new techniques and apparatus common to many laboratory disciplines, computerised medicine, political trendiness, power struggles, and much more.
There is much to be gained by both concentration and amalgamation but much to be lost as well and many consider the heart and soul of clinical microbiology at risk.
Over a period of years, rational high-throughput production has won over consultation and personalised microbiology. That may be fine for the production of negative HIV-antibody/antigen analysis as for the screening of blood-donors but certainly not for the bacteriological cultures taken in conjunction with a hip replacement. Or when it comes to understand and advise on the intricacies of antimicrobial resistance development. In other cases “outsourcing” and/or “amalgamation” mean that blood cultures are sent to X-town, CMV-antibodies to Y-town and everything else to Z-ville. When that happens clinical microbiology is lost.
There are several instances where concentration, amalgamation and/or outsourcing of clinical microbiological services, alone or with other services, have meant that the tie between clinical microbiology and infection control has been severed and that many, both small and large hospitals have lost the personalised service so necessary to control outbreaks of multi-resistant bacteria and other health care related infections.
A good service requires a strong knowledgeable and enthusiastic champion. A service which encompasses too many branches of laboratory medicine cannot be expected to champion each and every one with equal strength and fervour. And when outsourced to “big companies”, there is no “clinical”, only “microbiology”.
In 2008 “medical microbiology” broke out from “laboratory medicine” in UEMS. We are now striving towards a strong “medical microbiology” service in Europe. It will have many facets, much strength, some weakness, great opportunities, but many threats. ESCMID certainly intends to help shape microbiology in Europe.
S339 One central laboratory is the best
M. Drancourt* (Marseille, FR)
The optimal organisation of microbiology laboratories in European metropolis is an evolutionary task, driven by the evolution in laboratory tasks, laboratory technologies, communication technologies, regulations and financial issues. In the past five-ten years, medical and societal query for a more rapid and refined detection and identification of pathogens and antimicrobial resistance determinants coincided with the expansion of internet-based and remote tools for communication, an unprecedented revolution in laboratory technologies and new financial constraints. The concentration of laboratory workforces into one unique laboratory is one way to address these apparently contradictory issues. The tertiary medical school hospital system in Marseille, a 2-million metropolitan area in France, comprises four hospitals for a total of 3,500 beds. The system had once four microbiology laboratories which have been progressively embedded into a unique, 600,000 acts per year, laboratory which deals with bacteriology, virology and environmental microbiology and hygiene. The medical staff comprises of 17, the ingenior staff of 11, technical staff of 88 and support staff of 13 persons for a total of 129 persons. This organisation allowed reducing labour time for routine microbiology, to develop prospective and sophisticated time-consuming diagnostic methods and to develop advanced diagnostic methods such as molecular methods (real-time PCR-based tests, sequencing, and mass spectrometry identification) and new generation serology. New, sophisticated technologies such as automated serology and mass spectrometry were corner-stones on which to base the constant diminution of routine labour time and the development of time-consuming tasks such as fastidious organisms' isolation. These evolutions paralleled the exponential increase in the ratio of ingeniors in the laboratory. This paradigm allowed for the constitution of large collections of biological specimens for retrospective analyses, the specialisation of every medical senior in one particular field of internationally recognized expertise and the increase in knowledge output in terms of peer-reviewed papers, patents and grants. Implantation of point-of-care in the emergency department, in permanent internet-based connection with the central laboratory, was the last, but not least, evolution of this system.
Update on tuberculosis
S342 Update on tuberculosis – epidemiology
S. Hoffner* (Stockholm, SE)
When tuberculosis epidemiology is seen in a global perspective, and the Millennium Development Goals are considered, it is clear that two regions of the world, Africa and Europe, are severely behind in the control of the disease. In Africa, especially sub-Saharan Africa, the TB problem is closely related to the endemic HIV/AIDS situation. In Europe, especially the eastern part and in parts of the former Soviet Union, the main obstacle to an effective TB control is related to drug resistant forms of M. tuberculosis. The prevalence of the most severe forms of resistance, MDR- and XDR-TB, is so high that it makes control efforts both extremely complicated and very expensive. Unfortunately, increasing levels of drug resistant TB are today also seen in many African countries, and HIV infection is spreading in Eastern Europe.
During the last ten-year period new tools, based on molecular fingerprinting of M. tuberculosis strains, have been increasingly adapted to study TB transmission. With such molecular methods to characterise clinical isolates of M. tuberculosis it is now possible to study the spread of individual strains of the bacteria in detail. The laboratory tools used, RFLP, MIRU/VNTR, spoligotyping and others, will be presented and their use exemplified. How molecular epidemiology contributed to the detection and characterisation of a major outbreak of drug resistant TB in the Stockholm area will be discussed.
Molecular characterisation of clinical isolates from different parts of the world has led to an increased recognition of the differences between different families of M. tuberculosis strains. To further describe and understand the role of these differences in the clinical field as well as for TB epidemiology is an ongoing and interesting field of research. An increased understanding of how TB is transmitted will hopefully help in the efforts to control this global health threat both on the local level and in a global perspective.
S343 Diagnosis and treatment
J.S. Friedland* (London, UK)
Living in the era of increasing tuberculosis drug resistance, the importance of making an early and accurate diagnosis with drug sensitivities has never been greater. The epidemiology of tuberculosis defines the extent of latent disease and the proportion which becomes active. Accurate diagnosis is vital if patients are to be treated in a timely manner and to reduce the amount of time infectious individuals go untreated in the community disseminating disease. In many areas of the world, DOTS programmes are at the forefront of tuberculosis control. However, as a diagnostic this currently relies on sputum smear microscopy which is known to miss 50% of cases of tuberculosis and provides no data on drug sensitivity. The second major issue around TB is the lack of worldwide diagnostic facilities. There is a need for a simple, low cost, easily implemented diagnostic test.
This talk will briefly consider the issues around the diagnosis of latent and active disease which are quite distinct. The focus will be on the diagnosis of active infection. In particular, the use of MODS (microscopic observation drug-susceptibility) assay in diagnosis of tuberculosis will be discussed. The potential for using this in resource poor countries will be reviewed as well as the way sophisticated technology maybe harnessed to improve reporting and allow translation to all parts of the world. The important issue of how to distinguish patients with latent and active disease will also be considered. Key issues and principles in diagnosis both now and in the future will be reviewed. In terms of treatment, there are 2 main issues. The first is that even short-course therapy is prolonged being a minimum of 6 months leading to issue of compliance. This may result in drug resistance. The massive rise of multi-drug resistant tuberculosis to approximately 500,000 cases world-wide with around 50 countries reporting extensively drug-resistant disease means that the need for new approaches to therapy are urgent. The second part of this talk will review different approaches to using current anti-mycobacterial drugs, the emergence of a small number of new drugs such as the diarylquinolones and entirely novel approaches to control and treat tuberculosis.
The year in infectious diseases
S345 The year in infectious diseases
V. Valtonen* (Helsinki, FI)
There has been great success and also many threats in the field of infectious diseases during the previous year.
The antimicrobial resistance, especially increasing carbapenem resistance among aerobic Gram-negative rods and XDR Mycobacterial tuberculosis strains are already big threats in some countries and they will probably spread to many other areas all over the world in the future and we will need new drugs for these indications but unfortunately very few new promising drugs seem to be in the pipeline at the moment for these purposes.
The virulent Clostridium difficile 027 strain spreads rapidly to many new countries and e.g. in Finland it killed many times more people compared with MRSA and ESBL strains in 2008. However, it is possible to stop its spreading but it needs new thinking in antibiotic use policy and infection control policy in hospitals. Clostridium difficile 027 infection has a high relapse rate after metronidazole or vancomycin therapy, but an experimental “stool exchange treatment” is a promising therapy although controlled studies are needed to prove this assumption.
An interesting research area during the last years has been the role of infections in the etiopathogenesis of chronic diseases like cancer, atherosclerosis, cardiovascular diseases and many autoimmune diseases. We can fight against many cancers like liver cancer and cervix cancer with virus vaccines and gastric cancer with antimicrobial drugs. Also the high incidence of malignant tumours seems to decrease during Haart treatment in HIV patients. The role of infections in the etiopathogenesis of cardiovascular diseases and atherosclerosis is complex. It is obvious that infections play a role in the etiopathogenesis of atherosclerosis, stroke and myocardial infarction but the undirected routine antimicrobial treatment is not recommended for these patients but there seems to be subgroups in patients with various cardiovascular diseases which may benefit from antimicrobial treatment. Recent studies seem to suggest that there are HLA types which protect or make people susceptible for coronary heart disease. The HLA type HLA-B*35 seems to be a risk factor for coronary heart disease but it is also a risk factor for chronic Chlamydia pneumoniae infection.
The feared pandemia due to H5N1 influenza A did not appear during the recent year and the world is now much more prepared to meet the next pandemia which, however, hopefully does not come during the next year.
Further spread of KPC-type carbapenemases
O348 Emergence of KPC-producing Klebsiella pneumoniae in Norway is associated with hospitalisation abroad, nosocomial transmission and sporadic urinary tract infections in outpatients without recent hospitalisation
Ø. Samuelsen*, C. Giske, U. Naseer, S. Tofteland, D.H. Skutlaberg, A. Onken, R. Hjetland, A. Sundsfjord (Tromsø, NO; Stockholm, SE; Kristiansand, Bergen, Oslo, Førde, NO)
Objectives: The worldwide dissemination of KPC-producing multidrug-resistant Enterobacteriaceae is worrisome. The first KPC-producing Klebsiella pneumoniae in Norway was isolated late 2007 from a patient after hospitalisation in Greece. Throughout the following year seven additional KPC-producing K. pneumoniae isolates have been detected in clinical samples from six new patients. The aim of this study was to perform molecular characterisation of the strains and examine their epidemiological relatedness.
Materials and Methods: Antimicrobial susceptibility was examined by Etest. Molecular characterisation was performed by MLST, PFGE and sequencing of the blaKPC genetic structure. Plasmid analysis was carried out by PFGE of S1 nuclease-digested total DNA and Southern blot hybridisation using a blaKPC probe. Relevant epidemiological data were collected retrospectively.
Results: Eight KPC-producing clinical isolates of K. pneumoniae have been identified from seven patients in two different regions of Norway from the following specimens: blood culture (n = 3), urine (n = 2), expectorate (n = 1), perineal swab (n = 1) and wound secretion (n = 1). Two blood culture isolates with clonally related but different PFGE-profiles were observed in one patient. The detection of KPC-producing K. pneumoniae isolates in Norwegian patients was associated with import in four cases after hospitalisation in Greece. Two patients had been hospitalised at the same hospital in Greece. Isolation of a KPC-producing isolate in a fifth patient was epidemiologically linked to one of these imported cases and was a case of nosocomial transmission in Norway. For the latter two cases no risk factors were identified with respect to recent hospitalisation or travel abroad. Molecular analysis of six isolates has shown genetically related PFGE-patterns and a common sequence type (ST258). ST258 has been associated with dissemination of CTX-M-15 in Hungary. The blaKPC gene was localised in Tn4401 on a ˜97 kb plasmid. The two most recent isolates are currently undergoing similar analysis.
Conclusion: The first seven cases of KPC-producing K. pneumoniae in Norway are associated with hospitalisation abroad, nosocomial transmission in Norway, or urinary tract infections in outpatients without obvious risk factors. The clonal relationship between isolates underlines the existence a biological fit genetic lineage of KPC-producing K. pneumoniae with an epidemic potential.
O349 Emerging infections due to KPC-2 producing Klebsiella pneumoniae in hospitals in Greece
P. Giakkoupi, H. Maltezou, M. Polemis, O. Pappa, G. Saroglou, A. Vatopoulos* on behalf of the National Surveillance System for Antimicrobial Resistance
Objectives: Two recent publications have reported the isolation of KPC producing K. pneumoniae from infections in two patients, one in France and one in Sweden, who originally had been hospitalised in Greece. Since this resistant mechanism had not been identified before in this country, the purpose of this report was to confirm the presence of blaKPC producing K. pneumoniae in Greece, to assess the extent of its spread and to study the genetic relatedness of the respective bacterial strains and the transferability of the blaKPC harbouring plasmids.
Methods: For a three month period (February to April 2008) 40 hospitals participating in the Greek System for Surveillance of Antibiotic Resistance (www.mednet.gr/whonet) were asked to seek for possible KPC producers among K pneumoniae isolates displaying reduced susceptibility to imipenem (equal or higher than 1 mg/L), a positive Hodge test for the presence of carbapenemase and a negative EDTA synergy test for the presence of metalloenzymes. The presence of blaKPC gene in these strains was confirmed by PCR and sequencing. MICs to carbapenems were determined by etest. Conjugation experiments were carried out both in broth and on agar. The possible absence of OmpK36 porin was detected by PCR. Molecular typing was performed by pulse-field gel electrophoresis of XbaI-restricted genomic DNA.
Results: Ninety two K. pneumoniae clinical isolates (one per patient) from 13 Hospitals all over Greece were found to harbour blaKPC-2 gene. Although colonies present in the inhibition zone made the exact determination of imipenem MIC difficult, the absence of OmpK36 porin was always associated with MIC of imipenem higher than 32 mg/L. All isolates exhibited resistance to all other drug classes except colistin, tetracycline and tigecycline. PFGE analysis revealed that 85 isolates from 12 Hospitals displayed more than 95% similarity and were classified into one pulsotype, whereas the remaining seven isolates belonged into four different pulsotypes. blaKPC-2 gene could not be transferred by conjugation from strains belonging to the main pulsotype. However, it was transferred from strains belonging to three out of the four remaining pulsotypes.
Conclusion: Production of KPC-2 betalactamase seems to be a new emerging resistance mechanism in Klebsiella pneumoniae in Greece. blaKPC-2 gene's possible clonal spread imposes the urgent need of implication of infection control practices in the affected hospitals.
O350 An outbreak of Klebsiella pneumoniae producing KPC-2 carbapenemase in a Greek universtity hospital
I. Galani, M. Souli, E. Papadomichelakis, F. Panayea, N. Mitchell, A. Antoniadou, G. Poulakou, F. Kontopidou, H. Giamarellou* (Athens, GR)
Background: Until now, carbapenem resistance among Klebsiella pneumoniae (Kp) clinical isolates in Greek hospitals has been attributed to the dissemination of VIM-1 metallo-beta-lactamase. We describe the first outbreak of KPC-producing Kp in Greece; the first to occur outside the USA or Israel. Setting: 21-bed ICU of Attikon University Hospital, Athens.
Methods: Kp isolates with an imipenem MIC > 1 mg/L and a negative EDTA-imipenem disk synergy test were submitted to boronic acid disk test, to PCR for a KPC gene with specific primers and sequencing. Records from patients colonised or infected with a KPC-producing Kp were retrospectively reviewed for clinical and epidemiological data. Environmental cultures for KPC-producers were performed. Clinical isolates were submitted to molecular typing using PFGE.
Results: From February to November 2008, 552 Kp were isolated from 95 patients, 132 (23.9%) of which were boronic acid positive and produced KPC-2. Most of them (126/132, 95.5%) were isolated since August. A total of 24 patients were identified as colonised or infected by a KPC producer which in 22 of them belonged to the same genetic clone. The source was faeces (73), bronchial secretions (26), blood (7), CVC tip (5), urine (15), pus (4) and throat (2). Among patients whose medical records were available, median age was 74, APACHE II score; 21, length of preceding hospital stay; 28 days, total length of stay; 50 days, immunosuppresion was identified in one and crude mortality was 71%. The KPC-producing Kp was more frequently ICU acquired whereas in a minority of patients it was already present on ICU admission. Seventy percent of the patients had previously received a carbapenem for a median of 15 days. Environmental colonisation was not identified. Ten (7.6%) of the KPC-producers from 8 (33.3%) patients were identified as the cause of an infection: bacteraemia (7), ventilator-associated pneumonia (2) and surgical site infection (1) and exhibited MIC90 (mg/L) for imipenem, >8; meropenem, >8; gentamicin, 4; ciprofloxacin, >2; fosfomycin, >128; colistin, 0.5 and tigecycline, 4. Most patients were successfully treated with a colistin-containing combination mostly with a beta-lactam. There was no attributed mortality.
Conclusions: The acquisition of KPC carbapenemase by Kp is an emerging threat for public health in Greek hospitals, which should be promptly recognized and confronted.
O351 Genetic evidence for KPC-encoding resistance among six Enterobacteriaceae species other than K. pneumoniae
M. Castanheira*, L. Deshpande, R. Mendes, R. Jones (North Liberty, US)
Objectives: To evaluate the genetic context and location of KPC-encoding genes among a large collection of Enterobacteriaceae isolates not K. pneumoniae.
Methods: 61 isolates belonging to six Enterobacteriaceae species (table ) recovered in the USA and Israel from 2000 through 2007 were evaluated. Isolates from the same bacterial species were typed by PFGE or automated ribotyping. KPC-encoding gene was fully sequenced. Plasmid preparations and I-Ceu digestion of total DNA were resolved in agarose gels, blotted and hybridised with a blaKPC probe. The blaKPC-carrying element (Tn4401) was amplified with various primer pairs, digested with Eag I and sequenced.
| Bacterial species (no.) | Location | KPC-types | Typing patterns/clones* |
|---|---|---|---|
| Enterobacter cloacae (25) | USA, Israel | KPC-2, KPC-3, KPC-4 | 11/4 |
| Klebsiella oxytoca (13) | USA | KPC-2 | 11/2 |
| Escherichia coli (10) | USA, Israel | KPC-2, KPC-3 | 8/1 |
| Citrobacter freundii (9) | USA | KPC-2, KPC-3 | 8/1 |
| Enterobacter gergoviae (2) | USA | KPC-2, KPC-3 | 2/0 |
| Serratia marcescens (2) | USA | KPC-3 | 2/0 |
Two or more isolates showing identical genotyping profiles.
Results: 30 strains each carried KPC-2 and KPC-3. One E. cloacae carried KPC-4. 13 K. oxytoca were KPC-2-producers and 2 S. marcescens harboured blaKPC-3, all from USA. Great genetic diversity was observed among the isolates (41 different types). One clone of 10 E. cloacae was detected in New York state (2006–2007). Small clusters of 2 and 3 strains were detected among E. coli, E. cloacae, K. oxytoca. Plasmids were present in all but 3 isolates. Persistence of clones throughout the years was not observed. In 35 isolates the KPC-encoding gene was located in high molecular weight plasmids (>54 Kb). blaKPC was located in the chromosome of 11 strains (E. cloacae, E. coli and K. oxytoca) and the location of this gene could not be determined in 15 strains. Small plasmids were present in several strains, but did not harbour blaKPC. Tn4401 carried blaKPC in 46 isolates, and the transposon element was conserved. This structure was not detected in 12 strains.
Conclusions: KPC-encoding genes were most often located in Tn4401 among several Enterobacteriaceae species collected in USA and Israel. This blaKPC-carrying element was located in plasmids and on the chromosome. This study highlights the importance of Tn4401 in the dissemination of blaKPC genes in several genetically diverse bacterial species. blaKPC was not associated with Tn4401 in only 12 of 61 strains. These strains are under further investigation.
O352 First description of KPC-2 in Raoultella planticola: report from the SENTRY Antimicrobial Surveillance Program
M. Castanheira*, L. Deshpande, J. Dipersio, R. Mendes, R. Jones (North Liberty, Akron, US)
Objective: To evaluate the carbapenem resistance mechanism in a Raoultella planticola bacteraemia isolate recovered from a patient hospitalised in Ohio, USA.
Methods: Species identification was performed by VITEK 2 and confirmed by 16S rRNA sequencing. Susceptibility testing used CLSI broth microdilution method. blaKPC was amplified and sequenced. The blaKPC genetic element (Tn4401) was amplified and sequenced. Plasmid extractions and conjugation experiments were carried out and the isolate was screened for ESBL-encoding genes, qnr and qepA.
Results: A 83 year old female patient was admitted to a hospital located in Akron with a diagnosis of CAP in May/2008. Sputum, paracentesis and blood cultures were negative. Urine culture grew E. coli and patient received courses of moxifloxacin, ceftriaxone, azithromycin and meropenem. The patient was discharged and returned after three weeks with respiratory problems. Tracheal aspirate grew a multidrug resistant A. baumannii and the blood culture grew the enteric-like Gram-negative bacillus. The isolate was identified as R. planticola by the VITEK 2, which was confirmed by 16S sequencing. R. planticola strain demonstrated resistance against most β-lactams, including carbapenems. Screening for KPC-encoding genes was positive and this strain carried blaKPC-2. Fluoroquinolone and aminoglycoside MIC values were elevated. KPC-2-encoding gene was located in Tn4401, but conjugation experiments failed. ESBL and qnr/qepA genes were not detected. Conclusions: KPC serine-carbapenemases have been detected in several Gram-negative species commonly isolated from clinical specimens. KPC genes are embedded in transposon-like structure usually harboured in conjugative plasmids carrying multiple antimicrobial resistance mechanisms.
This is the first report of KPC-producing R. planticola that is an environmental organism related to Klebsiella spp. The similarity between these organisms could facilitate the transfer of genetic material. KPC-producing isolates appear to be prevalent among different Enterobacteriaceae species in USA hospitals and was detected in an isolates of apparent environmental origin.
Immunology, host defences and immunotherapy
O353 Polymorphisms in the promoter region of TANK-binding kinase-1 are associated with Gram-positive bloodstream infections
P. Wolffs*, E. Beuken, S. Ouburg, S. Morré, F. Stassen (Maastricht, NL)
Objectives: It is long known that not all individuals with a specific disease present with the same clinical manifestations, nor do they have identical prognoses or responses to treatments. It has become clear that variations in the human genome are likely to have an impact on these aspects. TANK-binding kinase 1 (TBK1) is a central molecule in the induction of a.o. the type I interferon response to pathogens. Our goals for this study were 1) to investigate the frequency of single nucleotide polymorphisms (SNPs) in the promoter and coding region of TBK1 in a Dutch Caucasian population and 2) to search for potential associations between these SNPs and bloodstream infections.
Methods: Whole blood samples or samples of positive blood cultures were collected and after genomic DNA was isolated, PCR and sequencing were performed for SNP identification. Functional studies included promoter activity measurements using a luciferase assay as well as electrophoretic mobility shift assays (EMSA) to study binding of the transcription factor USF1 to the wt and mutant promoter. SNP incidences were studied in a case control study.
Results: In samples from Dutch Caucasian healthy volunteers, 4 SNPs were found with allele frequencies higher than 5% whereas 6 other known SNPs had frequencies lower than 5% in our cohort. Two SNPs (rs89208169 and rs89208163) located in the promoter region were studied in a larger cohort of 350 anonymised patients from the Maastricht University Medical Center with either Gram-positive or Gram-negative blood cultures. We found that the prevalence of rs89208169 was significantly increased in patients with positive blood cultures in comparison with those with negative blood cultures or healthy volunteers. Further investigation of this SNP showed that it is located just outside a USF1-binding site. Measuring the promoter activity using luciferase assays, the mutant promoter exhibited a decreased activity of <35%. This observation was confirmed by EMSA which showed that recombinant USF1 protein had a reduced binding affinity to the mutant promoter.
Conclusions: SNP rs89208169 in the promoter region of TBK1 has a significant association with Gram-positive infections. Our results demonstrate that this is likely due to a decreased expression of TBK1 due to reduced binding of the transcription factor USF1 to the mutant promoter. Our results support recent findings that TBK1 plays also an important role in the host response to Gram-positive infections.
O354 Evaluation of a novel small molecule caspase inhibitor, VX-166, as a potential therapy for sepsis
P. Weber*, P. Wang, P.S.H. Wang, R. Wu, M. Miksa, W. Dong, G. Ku, J.M.C. Golec, D. Dawson, P. Charlton (Abingdon, UK; Manhasset, Cambridge, US)
Objective: Lymphocyte apoptosis has been recognized as an important factor contributing to both the onset of sepsis post infection and to the progression into septic shock. Animal data suggest that prevention of lymphocyte apoptosis by caspase inhibition stabilises the immune system, improves bacterial clearance and decreases mortality in experimental sepsis. The present study evaluated the potential of VX-166, a novel broad caspase inhibitor, as a therapy for sepsis.
Methods and Results: Initial characterisation of VX-166 in a number of enzymatic and cellular assays clearly demonstrated that the compound is a broad caspase inhibitor with potent anti-apoptotic activity in vitro. In vivo, VX-166 was tested in a murine model of endotoxic shock and a clinically relevant model of peritonitis. In the endotoxic shock model, male CD-1 mice (n = 28 per group) were administered LPS (20 mg/kg IV) and survival was monitored for 96 h. VX-166 administered by repeat IV bolus (0, 4, 8 and 12 h post-LPS) significantly improved survival in a dose-dependent fashion (p < 0.0001). In the rat peritonitis model, adult male Sprague-Dawley rats (n = 12 per group) underwent caecal ligation and puncture (CLP) and survival was monitored over 10d. Continuous administration of VX-166 by mini-osmotic pump (0.9 mg/kg/h) immediately following surgery significantly improved survival (p < 0.01) from 38% in the control group to 88% in the compound-treated group. Mode of action studies in the rat CLP model confirmed that VX-166 reduced thymic atrophy and lymphocyte apoptosis (p < 0.01), supporting the anti-apoptotic activity of the compound in vivo. In addition, VX-166 reduced plasma endotoxin levels (p < 0.05), strongly suggesting an improved clearance of bacteria from the bloodstream.
Most importantly, we demonstrated that VX-166 fully retained its efficacy when dosed 3 hours after insult (p < 0.01) by improving survival to 92% versus 42% in control animals, further highlighting the potential of anti-apoptotic therapy in sepsis.
Conclusion: Overall these data demonstrate that VX-166 inhibits lymphocyte apoptosis, improves the clearance of bacterial endotoxin and improves survival in experimental sepsis. Importantly VX-166 improves survival in the CLP model when dosed post insult, and therefore represents significant progress in the development of therapeutically viable broad caspase inhibitors for the treatment of this disease.
O355 Activation of Toll-like receptor 2 and Toll-like receptor 2/6 by lactobacilli
V. Vankerckhoven*, S. Van Voorden, N. Hens, H. Goossens, G. Molenberghs, E. Wiertz (Wilrijk, BE; Leiden, NL; Hasselt, BE)
Objectives: Toll-like receptors function as key regulators of both innate and adaptive immunity. Lactobacilli modulate the immune system in different ways. The aim of this study was to examine Toll-like receptor (TLR2, TLR2/6 and TLR4) signalling induced by clinical and probiotic Lactobacillus strains.
Methods: A total of 45 Lactobacillus strains (19 L. paracasei and 26 L. rhamnosus) of different origin (22 probiotic, 2 faecal, and 21 clinical) were tested for TLR2, TLR2 in combination with TLR6, and TLR4. TLR signalling was measured as relative IL-8 promotor activation in transfected human embryonic kidney (HEK) 293 cells. IL-8 concentrations were measured using an enzyme-linked immunosorbent assay. Heat-killed Listeria monocytogenes (HKLM) was used as positive control in all assays, whereas PAM3, PAM2, and LPS were used as positive controls for, respectively, TLR2, TLR2/6, and TLR4. All assays were performed at least in duplicate. Linear mixed model analyses and stepwise model selection were used to identify the statistically significant effects. Random effects were used to account for heterogeneity across and homogeneity within isolates. P < 0.05 was considered statistically significant.
Results: HEK-TLR2 and HEK-TLR2/6, but not HEK-TLR4, cells released IL-8 upon stimulation with UV-inactivated lactobacilli, which was enhanced by co-transfection with CD-14. Interestingly, the production of IL-8 was shown to be variable for the different Lactobacillus isolates. Although similar results were seen for all isolates for TLR2 and TLR2/6, IL-8 production was significantly higher for TLR2 (8.4 log pg/ml) compared to TLR2/6 (6.05 log pg/ml) (P < 0.0001). No significant differences in IL-8 production were seen between clinical and probiotic isolates. However, L. rhamnosus isolates induced a significantly higher IL-8 production compared to L. paracasei isolates in both cell lines, 7.88 and 6.84 log pg/ml, respectively (P = 0.0004). Intra-isolate correlation was found significant (P < 0.0022).
Conclusions: Our study shows that lactobacilli activate both TLR2 and TLR2 in combination with TLR6. Our results also indicate that heterodimerisation of TLR2 with TLR6 does not lead to an improved recognition of lactobacilli. Furthermore, taking intra-isolate correlation into consideration proved to be important. Finally, our results suggest that differences in immunomodulation by lactobacilli may be related to differential signalling through TLRs, including TLR2 and TLR2/6.
O356 Mycobacteria affect group I CD1 expression and lipid-antigen presentation via p38 signalling in human DC precursor
M.C. Gagliardi, V. Sargentini, R. Teloni, M.E. Remoli, G. Federico, M. Videtta, G. De Libero, E. Coccia, R. Nisini* (Rome, IT; Basel, CH)
Objective: To gain insights into the mechanisms used by Mycobacterium tuberculosis and Bacillus Calmette Guérin to cause human monocytes differentiation into CD1 negative dendritic cells (My-MoDC), unable to present lipid antigens to specific T cells.
Methods: Human monocytes infected or not with mycobacteria were induced to differentiate into DC with GM-CSF and IL-4 in the presence or absence of p38 or ERK specific inhibitors. Kinases activation was detected by western blot using antibodies specific for phosphorylated and non phosphorylated isoforms. Differentiation of monocytes into DC and the CD1a, CD1b and CD1c expression was evaluated by flow cytometry and by real time PCR at different time points from infection. Functional expression of CD1 molecules was assessed by recognition of lipid antigens by CD1 restricted T cell clones.
Results: We show that mycobacteria trigger phosphorylation of ERK and p38 mitogen-activated protein kinase in human monocytes as well as of activating transcription factor (ATF)-2. Mycobacteria-infected monocytes treated with a specific p38 inhibitor, but not with a specific ERK inhibitor become insensitive to mycobacterial subversion and differentiate into CD1 positive My-MoDC, which are fully capable of presenting lipid antigens. Data indicate that phosphorylation of p38 is directly involved in CD1 inhibition.
Conclusions: We propose p38 signaling as a pathway exploited by mycobacteria to affect CD1 expression, thus representing a novel target of possible pharmacological intervention in the treatment of mycobacterial infections.
O357 Pro-inflammatory effect of activin A on microglial cells
S. Ebert*, S. Ribes, R. Nau, U. Michel (Gottingen, DE)
Objective: Activin A (Act A) is a multifunctional cytokine with roles in the immune system and the inflammatory response. Act A levels are elevated in the cerebrospinal fluid of patients with meningitis. Microglial cells, the major constituents of innate immunity within the brain, express Toll-like receptors (TLRs) recognising exogenous and endogenous ligands. Upon stimulation with TLR agonists, primary mouse microglial cells become activated and release nitric oxide (NO), cytokines, and also Act A, suggesting that they are a source of elevated Act A levels during central nervous system (CNS) infections. Both pro- and anti-inflammatory effects of Act A have been observed in vitro. We investigated whether Act A influences NO release from microglial cells stimulated with agonists of TLR2, 4, and 9.
Methods: Primary mouse microglial cells were kept in DMEM (+FCS+PS) either in presence or absence of Act A (1 µM). 24 hours after addition of Act A, cells were stimulated with the TLR2 agonist Pam3CSK4 (P3C), the TLR4 agonist endotoxin (LPS), and the TLR9 agonist cytosin-guanosin ODN 1668 (CpG) in the presence of interferon-gamma (IFN; 100 U/ml) for 48 hours. Control cultures were treated with IFN only. Concentrations of the TLR agonists evoking about 50% of the maximum NO release were used. NO release was quantified using the Griess reaction. Viability of microglial cells was determined using the WST-1 assay. Means+SD of NO release in % of maximum NO release are presented (n = 9). Data were analysed by one-way ANOVA followed by Bonferroni's multiple comparison test (p < 0.05 significant).
Results: ActA did not influence NO release from control microglial cells [10.03+2.90% (IFN), 9.13+2.69% (IFN+Act A); p > 0.05]. However, pretreatment with 1 µM Act A significantly enhanced NO release from microglial cells upon stimulation with 0.01 µg/ml P3C [60.16+4.54% (P3C), 76.84+5.58% (P3C+Act A); p < 0.001], 0.0003 µg/ml LPS [50.60+4.59% (LPS), 64.15+11.07% (LPS+Act A); p < 0.001], and 0.1 mg/ml CpG [44.48+4.14% (CpG), 57.17+8.90% (CpG+Act A); p < 0.001]. In none of the groups, cell viability was affected.
Conclusions: Pre-treatment with Act A enhances NO release from microglial cells activated by agonists of the principal TLRs involved in the recognition of bacteria. These findings provide further evidence for a role of Act A in the innate immune response and suggest that Act A acts as an pro-inflammatory modulator during infection and inflammatory processes in the CNS.
Bacterial genome plasticity – new insights into bacterial adaptation to the clinical environment (Symposium arranged with ESGEM)
S361 Role of insertion sequences in the mobility and expression of antibiotic resistance genes
L. Poirel* (Kremlin Bicetre, FR)
Insertion sequences (IS) are genetic tools that can mediate expression of previously silent genes or be responsible for the overexpression of certain genes (in each case by providing promoter sequences). In addition to be involved in gene transcription levels, IS elements also play a very important role for gene acquisition/mobilisation. An IS is usually made of of two inverted-repeat sequences (IRs) bracketing a gene encoding the transposase which activity enables this entity to replicate and target another sequence. The IS-related mechanisms at the origin of antibiotic resistance gene acquisition are diverse, including composite-transposition, rolling-circle transposition, one-ended transposition. IS elements may be also involved in gene acquisition by mediating co-integration processes, or recombination events as hypothetized for IS26 in relation with blaSHV extended-spectrum β-lactamase (ESBL) genes originating from the chromosome of Klebsiella pneumoniae. The blaCTX-M ESBL genes known to be extremely widespread worldwide are encoded on plasmids, and have been found in association with ISEcp1 (acting by one-ended transposition) or ISCR1 (acting by rolling-circle transposition). In that case, ISs have played a role in the mobilisation from the chromosome of Kluyvera spp. being the blaCTX-M progenitors and then in their expression. Also, genes encoding acquired AmpC β-lactamases, being of the blaACC, blaDHA, and blaCMY-types, are mostly found in association with ISCR1 or ISEcp1.
Sometimes antibiotic resistance genes are mobilised by composite transposons which are made of two copies of a given IS bracketing the mobilised fragment. In Acinetobacter baumannii, the worldwide disseminated blaOXA-23 carbapenemase gene is part of a composite transposon structure made of two copies of ISAba1, forming transposon Tn2006 which had mobilised a chromosomal fragment from Acinetobacter radioresistens that actually corresponds to the progenitor of blaOXA-23. Another possibility can be the forming of composite transposon structure bracketed by two different IS (sharing similar IRs) as observed with the blaPER-1 ESBL gene in Pseudomonas aeruginosa.
This diversity of ISs elements at the origin of mobilisation/acquisition of antibiotic resistance genes is therefore responsible for the very efficient dissemination of many of them.
S362 Resistance islands – their role in the accumulation and spread of antimicrobial resistance genes
K. Rajakumar* (Leicester, UK)
Historically, multi-antibiotic resistance in many bacterial species was largely attributed to the acquisition of resistance (R)-plasmids encoding one or more resistance determinants. However, over the last decade the R-plasmid paradigm has begun to be challenged. ‘Resistance islands’ comprising large, chromosomally-integrated spans of alien DNA harbouring multiple antibiotic resistance genes have been identified in the major hospital pathogens methicillin-resistant Staphylococcus aureus (MRSA) and multi-resistant Acinetobacter baumannii, and the food- and water-borne diarrhoeal pathogens Shigella, Salmonella and Vibrio cholerae. In addition, comparative genomics analysis of the archetypal Haemophilus influenzae conjugative resistance element that had spread worldwide revealed that it belonged to a large syntenic family of integrative islands, members of which could be found in at least 15 other β-and γ-Proteobacteria. With the exception of the A. baumannii island, these elements can be described as classic self-excising, -circularising and -integrative elements. All three functions are mediated by short island-flanking direct repeats and cognate integrase proteins encoded by the islands. In 2006 Fournier et al. described an 86kb A. baumannii island (AbaR1) which harboured 45 resistance genes packaged within a highly mosaic, integron-rich element that had almost certainly evolved via recombination, transposition and integron-mediated cassette capture from an ‘empty’ ancestral prototype. AbaR1 probably represents a new class of resistance island as it exhibits several features reminiscent of complex nested transposons, suggesting a distinct functional natute. However, despite the widespread distribution of resistance and genomic islands only a minority are known to code for part or all of the conjugative machinery necessary for their dissemination; others have been mobilised by helper plasmids or bacteriophages. Regardless, data on the mechanisms of mobilisation of the vast majority of similar nonresistance islands remain sparse. Importantly, resistance islands may not consists merely of packages of resistance genes. On the contrary, these diverse and frequently hybrid entities could potentially confer upon their hosts other advantageous traits relating to host-pathogen interaction, virulence, survival in the environment and/or transmissibility, truly justifying the label ‘selfish islands’ and further explaining their evolutionary success.
S363 Identification and characterisation of pathogenicity islands
L. Guy* (Uppsala, SE)
Due to the availability of new techniques, genome sequencing of bacteria has become fast and inexpensive. Furthermore, recent methods using paired-end reads located several kb apart in the genome eases the assembling process, even though no reference sequence is available. In a reasonably close future, it should be possible to obtain the fully assembled sequence of a bacterial isolate overnight.
The new sequencing techniques generate enormous amounts of genomic data and, thereby, a need for new tools. These should able to quickly analyze genomes and point to zones of interest, prompting further analysis on a reduced number of regions or genes, such as genomic islands.
Pathogenicity islands, a subset of genomic islands, carry genes such as toxins or resistance genes and have the particularity to be mobile, i.e. they may transfer to other species or strains. Thereby, they confer their new hosts a more resistant or infectious phenotype, making this phenomenon particularly important to study.
Nucleotide composition of genomes is fairly homogeneous inside bacterial genomes. In general, horizontally transferred regions can be spotted due to their particular nucleotide content, because they tend to retain the composition of their original host and don't share the one of their new hosts. To do an analogy with languages, genomes speak dialects, and as one would easily spot a paragraph in Finnish in an English text while not knowing Finnish, one can spot genomic and pathogenicity islands transfers in a given genome.
Several techniques relying on various compositional aspects and on different algorithmic methods have been recently developed to detect pathogenicity islands in bacterial genomes. Even very simple measures of the genome composition, such as the variation in T vs. A bias (TA skew) can lead to the identification of all known prophages in Streptococcus pyogenes. It can even trigger the discovery of a putative ancient genomic island carrying a large number of genes related to pathogenicity in all strains of that species.
In conclusion, with the rise of fast and inexpensive genome sequencing, new quick and simple methods are being developed. They take the advantage of the homogeneous nucleotide composition of bacterial genomes to uncover mobile genetic elements carrying genes involved in pathogenicity.
HBV resistance: a new frontier for antiviral therapy
S364 The new drugs and their resistance mechanisms
F. Zoulim* (Lyon, FR)
In the past 10 years, significant progress has been achieved in the management of chronic hepatitis B with the successive development of six potent antiviral medications (lamivudine, adefovir dipivoxil, pegylated interferon alpha, entecavir, telbivudine and tenofovir). However, the clinical results of antiviral therapy have been limited by the emergence of antiviral drug resistance especially with the first generation of nucleoside analogs (lamivudine, adefovir and telbivudine). Furthermore, the unique mechanism of viral genome replication and persistence within infected cells is responsible for viral persistence even after prolonged therapy with the newer antivirals (entecavir and tenofovir). This is the major reason why life-long treatment is envisaged in the majority of patients, which may expose them to long-term risk of developing resistance.
The use of in vitro phenotypic assays has been crucial for the characterisation of newly identified resistant mutants and determine their cross-resistance profile. Results allowed to understand the different mechanism of viral resistance to lamivudine and adefovir, the mechanism of primary failure to adefovir therapy, the unique mechanism of entecavir resistance, and to characterise the emergence of multi-drug-resistant strains in patients receiving sequential antiviral therapy. The cross-resistance profile for the main resistant mutants was determined which allowed to provide recommendation to clinicians for treatment adaptation based on molecular virology data.
The understanding of the development of HBV drug resistance has allowed to significantly improve the management of antiviral resistance and to design better treatment strategies to prevent resistance. The current standard of care relies on treatment initiation with antivirals combining a strong antiviral potency and a high barrier to resistance. A precise virologic monitoring is required to measure antiviral efficacy, and to diagnose partial response or viral breathrough at an early stage. This allows to adapt antiviral treatment preferrably using an add-on strategy with a drug having a complementary cross-resistance profile. This strategy has been shown to be efficient in controling viral replication and preventing liver disease progression in the majority of patients.
S366 Correlation between resistance and clinical progression
A. Dofferhoff* (Nijmegen, NL)
Treatment of chronic hepatitis B virus (HBV) infection is aimed at suppressing viral replication to the lowest possible level. In many prospective clinical trials it has been shown that a sustained HBV DNA response was correlated with serologic, histologic, or biochemical responses. Despite the recent progress in hepatitis B antiviral treatment, it is shown that antiviral drug resistance is inevitable against many of the nucleoside analogs. The emergence of antiviral-resistant strains of HBV leads to viral and subsequently biochemical breakthrough and may lead to disease progression and increased death. Most of the data on the clinical impact of antiviral resistant HBV came from the data derived from studies of lamivudine therapy. There is limited data on other HBV antiviral drugs like adefovir. It is shown in several studies that treatment of HBeAg-negative chronic hepatitis B with lamivudine effectively suppresses HBV replication and results in biochemical remission and histologic improvement in more than two thirds of patients. However, relapse has occurred in the majority of HBeAg-negative patients after the cessation of therapy. There are several studies to support the occurrence of severe hepatic flares, and liver failure after the emergence of lamivudine resistance. Several studies, where liver biopsies were taken, demonstrated that histological improvement was reduced in those patients experiencing lamivudine resistance. The clinical outcome for patients with antiviral resistance is related to their age, the severity of the underlying liver disease and the severity of the hepatic flares. On the other hand in a different study it was found that long-term lamuvidine treatment was associated with a reduced chance of developing cirrhosis and HCC in patients without advanced disease but, although resistant mutants reduced the benefits from lamivudine therapy, the outcome of these patients was still better than untreated patients. Results of several clinical trials have shown that the addition or substitution of newer antiviral agents can restore suppression of viral replication, normalisation of liver function and reverse histological progression in patients with antiviral resistance. Consequently, well-tolerated, potent therapies that offer a strong genetic barrier against the development of resistance are desirable, since antiviral resistance and poor adherence are key risk factors for treatment failure and subsequent reversal of clinical improvement.
Emerging resistances in Gram-negatives: update for 2009
S369 Salmonella and Campylobacter
T. Pál* (Al Ain, AE)
Resistance of enteric fever-causing and non-typhoid salmonella serovars to agents traditionally used to treat these infections in the past shows extensive geographical variation. Decreased susceptibility to ciprofloxacin is rapidly increasing all over the world with target alteration and increased efflux being the most important mechanisms behind. Infections with such strains often result in extended hospitalisation or even in therapeutic failures. Furthermore, it is likely that moderately increased MIC values facilitate the development of strains with higher level of resistance, i.e. a pattern described at various locations. Screening methods based on quinolone sensitivity testing may fail to indentify decreased fluoroquinolone susceptibility both in typhoid, as well as in non-typhoid salmonella. Plasmid mediated quinolone resistance genes are detected increasingly all around the world although neither the frequency nor the variety of genes identified has approached that seen in some other members of Enterobacteriaceae. Treatment with gatifloxacin or azithromycin are alternative options for invasive and systemic infections caused by strains with decreased susceptibility to ciprofloxacin.
At some parts of the World resistance to extended spectrum cephalosporins reached such incidence that may have therapeutic implications particularly when initial, empiric treatment of invasive infections is concerned. Resistance is due to plasmid coded AmpC type beta lactamases (particularly to CMY-2), and most often to ESBLs of which usually some of CTX-M types are the frequently encountered ones. Carbapenem resistance is still rare, albeit does occur, among salmonella isolates. The recent description of a non-typhoid salmonella strain with the blaIMP-4 gene co-located on a class-1 integron with several other resistance determinants on a conjugative plasmid is of particular concern.
Campylobacters exhibit natural resistance to a variety of antimicrobials. The drugs of choice used to be fluoroqunolones or macrolides. However, the current incidence of ciprofloxacin resistance made the former drugs already obsolete or seriously limited their use at several parts of the World. With the exception of few locations the incidence of macrolide resistance is still relatively low and is seen more frequently in C. coli than in C. jejuni. However, strains exhibiting resistance against both groups of drugs have been emerging, particularly in South-East Asia.
S371 Neisseria meningitidis and Neisseria gonorrhoeae
P. Mastrantonio*, P. Stefanelli (Rome, IT)
Neisseria meningitidis, the meningococcus, is a major cause of meningitis and septicaemia worldwide while Neisseria gonorrhoeae, the gonococcus, is responsible for one of the most widespread sexually trasmitted disease. The behaviour of these two species towards antibiotics is very different: resistance in N. gonorrhoeae is now widespread occuring as both chromosomally and plasmid mediated to a variety of drugs, whereas, besides resistance to sulphonamides, N. meningitidis remains largely susceptible to antibiotics used both for therapy and prophylaxis. However, as in the gonococcus, the resistance to antibiotics of N. meningitidis is also evolving, as documented by the ever higher frequency of strains with intermediate resistance to penicillin in many countries. Transformation has apparently provided both species with a mechanism by which they can increase resistance to penicillin by replacing part of their penA gene, which encodes PBP2, with part of the penA gene of related species that fortuitously produces forms of PBP2 less susceptible to the antibiotic. N. meningitidis is still at this step, whereas N. gonorrhoeae has acquired also mutation in the ponA gene that encodes PBP1, mutation in porin IB, increased expression of efflux pump and the TEM-1 β-lactamase plasmid. The emergence and the spread of gonococci fully resistant to penicillin since the second half of the 1980 s years led to the recommended use of fluoroquinolones as primary therapy. However, this class of antibiotics became rapidly unefficacious, mainly in Asia, due to the emergence of mutations in gyrA and parC which are able to block the activity of the quinolones on gyrase and topoisomerase IV. Since 2006, CDC no longer recommends their use for treatment of gonococcal diseases. Fortunately, the occurrence of quinolone resistant meningococci, due to mutations in gyrA, is still rare but even if cases are still few they are of great concern for the epidemic potential of this pathogen and the required prophylaxis of contacts.
Also for the other antibiotic, frequently used to this aim, rifampicin, some meningococci have showed to be resistant, again for the presence of mutations, in this case in the rpoB gene coding for the β-subunit of the meningococcal RNA polymerase.
The molecular epidemiological identification of clonal clusters for both Neisseria species with distinct resistance profiles is required to monitor ongoing trends that may pose problems both in therapy and prophylaxis.
Antibiotic use in primary care: new insights, better results? (Symposium arranged with ESPRIT)
S374 Attitudes and perceptions of doctors and patients to antibiotic use for LRTI in Europe
L. Brookes-Howell*, C. Butler, K. Hood, L. Cooper, H. Goossens (Cardiff, UK; Antwerp, BE)
Introduction: GRACE is a European Network of Excellence established to focus on antibiotic use for community-acquired lower respiratory tract infection (LRTI) and antimicrobial resistance across Europe. GRACE-02, the second study to begin within GRACE, is a large qualitative study that explores the attitudes of clinicians and patients to antibiotic use for LRTI and antibiotic resistance.
Aims: This presentation will focus on clinicians' accounts of the factors that contribute to variation in management of LRTI and patient views on when antibiotics are necessary.
Methods: Semi-structured interviews with 81 clinicians and 121 patients were conducted in primary care networks in nine European countries. Interviews were audio-recorded, transcribed and, where necessary, translated into English for analysis. Themes were identified, organised and compared using a Framework Approach.
Results: Analysis of clinician interviews shows that, beside clinical findings, factors which influence the management decision for patients can be divided into two main areas. Firstly, within each European network there is a group of country specific factors imposed by the system in which consultations take place. These factors include: near patient test usage, self-medication, patients' finances and lack of consistent, local prescribing guidelines. Secondly, there is a group of factors, similar across all networks, that relate to personal characteristics of certain groups of clinicians. These include clinicians' professional ethos, self-belief in decision making and attitude towards the doctor-patient relationship.
Analysis of patient interviews shows that beliefs about antibiotic use tend to draw on clinical factors, namely the severity of specific symptoms (fever and/or coughing). Many patients also implied a period of waiting or alternative action required before antibiotics are used – to identify whether the immune system would fight the infection or whether non-antibiotic management was effective before turning to antibiotics.
Discussion and Conclusion: With a greater understanding of the factors that contribute to the decision to prescribe, we discuss ideas to enhance appropriate prescribing. This analysis highlights the need for interventions to be sensitive to factors relating to the systems in which different European networks operate, to target the individual characteristics of specific groups of clinicians and to build on the clinical beliefs already held by patients.
Infectious diseases in animal models
O377 Pre-treatment with low-dose endotoxin prolongs survival from experimental lethal endotoxic shock
K. Kopanakis, I. Tzepi, E.J. Giamarellos-Bourboulis*, A. Macheras (Athens, GR)
Objective: Clinical trials of immunointervention with anti-endotoxin antibodies in patients with severe sepsis have failed to disclose survival benefit. These failures led us to the assumption that the opposite approach with a low endotoxin stimulus may result to low level immunoaralysis and subsequent survival benefit. This approach was tested in an experimental setting.
Methods: A total of 36 male C57B6 mice were studied divided into two groups: group A stimulated with the ip injection of sodium saline followed after one day by the ip injection of 30 mg/kg of lipopolysaccharide (LPS) of Escherichia coli O155:H5; and group B stimulated with the ip injection of 3 mg/kg of LPS of the same isolate followed after one day by the ip injection of 30 mg/kg LPS. LPS was diluted in sodium saline and the volume of each injection was 0.2 ml. Survival was recorded at six hour time intervals.
Results: Survival of group B was considerable prolonged compared with group A (log-rank: 5.435, p: 0.020) as shown in Figure 1 . Thirteen mice of group A died (72.2%) compared with seven mice of group B (38.9%, p: 0.044 between group).
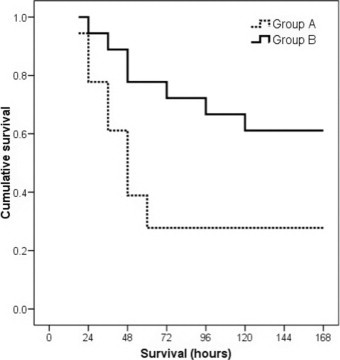
Conclusions: Administration of low doses of LPS prolongs survival after lethal endotoxic shock. This approach opens a promising novel pathway for immunointervention in sepsis.
O378 Efficacy of quinolones, mono versus combination therapy, in difficult-to-treat mixed infections caused by Escherichia coli and Bacteroides fragilis
M. Glenschek-Sieberth*, K. Merfort, S. Obertegger, R. Endermann (Wuppertal, DE)
Objective: Complicated intra-abdominal infections (cIAIs) are mostly polymicrobial infections caused by aerobic and anaerobic bacteria. A majority of these infections are dominated by Escherichia coli and Bacteroides fragilis. In this study, the antimicrobial efficacy of quinolones was evaluated using the murine pouch model infected concomitantly with E. coli and B. fragilis. This study tests the efficacy of moxifloxacin (MXF) monotherapy versus levofloxacin (LFX) and ciprofloxacin (CIP) monotherapies and LFX/metronidazole (MET) and CIP/MET combination therapies.
Methods: Clinical E. coli (n = 2) and B. fragilis (n = 2) isolates were used. MICs were determined by the broth microdilution method according to CLSI guidelines. Pouches for the murine model were created by injecting 5 mL of air and 0.5 mL of 0.1% croton oil in olive oil under the skin of the back. On day 3 the air was replaced with 1 mL soft agar. On day 5, the pouches were infected with a bacterial suspension of E. coli and B. fragilis. Mixed infected mice (n = 5/group) were treated for 2 days IV, b.i.d. with either MXF (100 mg/kg), or LFX (80 mg/kg) or CIP (90 mg/kg) alone or in combination with MET (100 mg/kg). These dosages simulate the AUC of the corresponding human IV therapy. Efficacy was assessed as the reduction in colony forming units (CFU) per mL pouch exudate 48 h post-infection compared with the infection control.
Results: According to CLSI breakpoints, the two B. fragilis isolates were categorised as intermediate susceptible (MIC = 4 mg/L) to MXF. One E. coli isolate was categorised as resistant (MIC = 8–16 mg/L) to MXF and one E. coli was categorised as susceptible (MIC = 0.016 mg/L) to MXF. In the murine pouch model mixed infected with the four different strains MXF, LFX/MET and CIP/MET demonstrated comparable activity. MXF monotherapy and LFX/MET or CIP/MET combination therapies achieved significant reductions in CFUs compared with the infection controls. LFX and CIP monotherapy failed to achieve significant CFU reductions compared with the infection control.
Conclusions: In the mixed infected murine pouch model, a model for cIAI abscess formation, LFX and CIP monotherapies exhibited only low efficacy. In contrast, MXF, LFX/MET and CIP/MET showed clear therapeutic efficacy, demonstrating the necessity of adequate anaerobic coverage when choosing antimicrobial treatment. MXF appears to be suitable for use as monotherapy in cIAIs.
O379 Efficacy of moxifloxacin in a murine granuloma pouch model caused by clinical Bacteroides fragilis isolates belonging to different breakpoint categories
M. Glenschek-Sieberth*, K. Merfort, S. Obertegger, R. Endermann (Wuppertal, DE)
Objectives: Moxifloxacin (MXF) is the only marketed fluoroquinolone with FDA approval for the monotherapy of complicated intra-abdominal infections (cIAIs). The obligate anaerobic bacterium Bacteroides fragilis is implicated in such infections. In this study, the antimicrobial efficacy of MXF against susceptible, intermediate and resistant clinical B. fragilis isolates was evaluated using the murine granuloma pouch (MGP) model, an animal model for infected intra-abdominal abscesses.
Methods: MXF MICs for clinical B. fragilis isolates were determined according to CLSI guidelines. FDA/CLSI MXF breakpoints for B. fragilis were defined as: susceptible ≤2 mg/mL, intermediate = 4 µg/mL, resistant ≥8 µg/mL. B. fragilis isolates with an MXF MIC of 2 µg/mL (n = 5), 4 mg/mL (n = 20) and 8 mg/mL (n = 8), which were virulent in the MGP model, were used to determine the efficacy of MXF. For the MGP model, pouches were created by injecting 5 mL of air and 0.5 mL of 0.1% croton oil in olive oil under the skin of the back. On day 3, the air was withdrawn and replaced by 1 mL soft agar. On day 5, a bacterial suspension was injected into the pouch. Infected mice (n = 6 mice/group) were treated with MXF 100 mg/kg IV, b.i.d. for 2 days. This dose simulates the AUC of the human 400 mg once-daily MXF IV dosage. Efficacy was assessed by the reduction in colony forming units (CFUs) in pouch exudates 48 hours post-infection compared with the untreated infection control.
Results: In the MGP model, MXF, 100 mg/kg b.i.d., displayed good efficacy in term of CFU reduction against all used strains in this study. There were no non-responders in terms of CFU reductions.
Table.
Efficacy distribution of strains (percent)
| Breakpoint categories of strains | CFU reduciion/mL pouch exudates |
||||
|---|---|---|---|---|---|
| ≥3 log10 | <3 log10 to ≥2 log10 | <2 log10 to ≥1 log10 | <1 log10 to ≥0 log10 | <0 log10 | |
| Susceptible (n = 5; MIC ≤ 2 μg/mL) | 100% | 0% | 0% | 0% | 0% |
| Intermediate (n = 20; MIC = 4 mg/mL) | 75% | 15% | 5% | 5% | 0% |
| Resistant (n = 8; MIC ≥ 8 μg/mL) | 50% | 25% | 12.5% | 12.5% | 0% |
Conclusions:
-
•
In a murine model of cIAIs, MXF demonstrated a high efficacy against clinical B. fragilis isolates with a MXF MIC ≤8 mg/mL.
-
•
MXF achieved a CFU reduction of ≥3 log10 against 100% of susceptible clinical B. fragilis isolates.
-
•
75% of the intermediate and 50% of the resistant clinical B. fragilis isolates displayed a ≥3 log10 CFU reduction by MXF.
O380 Impact of loss of major autolysin AtlE on activity of cloxacillin and vancomycin against Staphylococcus epidermidis
M. Hello, N. Caroff, C. Jacqueline, J. Caillon, G. Potel, E. Batard * (Nantes, FR)
Objective: To study the impact of the loss of major autolysin AtlE on the activity of cloxacillin and vancomycin against Staphylococcus epidermidis.
Methods: Wild-type (wt) atlE(+) O-47 and mutant atlE(−) O-47mut1 S. epidermidis strains were kind gifts from C Heilmann, Münster, Germany. Bactericidal activity in Mueller-Hinton broth was assessed by counting viable bacteria after a 24-h exposition to growing concentrations of cloxacillin or vancomycin. A sigmoidal dose-response model was used to estimate the maximal effect of bacterial killing, expressed as the decrease in bacterial counts. To compare virulence of both strains in the mouse peritonitis model, neutropenic mice were inoculated intraperitoneally with 3 to 8 log CFU. The median lethal dose (LD50) was assessed at Day 6. The efficacies of cloxacillin and vancomycin were assessed in the mouse peritonitis model. Mice were treated using various doses of antibiotics immediately after inoculation, and 4 and 8 h later. The median effective doses (ED50) were assessed at Day 6.
Results: MICs of cloxacillin and vancomycin were similar for both strains. The maximal bactericidal activity of cloxacillin and vancomycin were lower for the mutant atlE(−) strain in comparison with the wt atlE(+) strain. In the murine model, the LD50 s for wt atlE(+) and mutant atlE(−) strains were respectively 4.0 and 4.4log CFU/mL. The ED50 s of cloxacillin in the mouse peritonitis model were similar for both strains, as were ED50 s of vancomycin.
| Wild-type AtIE(+) strain | Mutant AtIE(−) strain | ||
|---|---|---|---|
| Cloxacillin | |||
| Susceptibility | MIC, mg/L | 0.25 | 0.5 |
| Bacterial killing in broth | Maximal effect, log CFU/mL (95% CI) | −3.048 (−3.541, −2.555) | −1.347 (−1.622, −1.072) |
| Mouse peritonitis model | ED50, mg/kg | 226 | 205 |
| Vancomycin | |||
| Susceptibility | MIC, mg/L | 1 | 1 |
| Bacterial killing in broth | Maximal effect, log CFU/mL (95% CI) | −3.936 (−4.446, −3.427) | 1 (−1.647, −0.9196) |
| Mouse peritonitis model | ED50, mg/kg | 9 | 6 |
Conclusion: The loss of atlE had no impact on the MICs of cloxacillin and vancomycin. Conversely, the mutant atlE(−) strain was less susceptible to bactericidal activity of both antibiotics, supporting the implication of AtlE in the tolerance of S. epidermidis to cell wall active antibiotics. The loss of AtlE did not alter the virulence of S. epidermidis in the mouse peritonitis model, whereas it decreased virulence in previously published experiments using an intravenous catheter infection model. Therefore, the mouse peritonitis model was suited to compare antibiotics efficacy against atlE(+) and atlE(−) strains. Our results showed that the loss of atlE did not alter significantly the activity of cloxacillin and vancomycin in the mouse peritonitis model. This study shows that the loss of atlE results in decreased susceptibility to bactericidal activity of cell wall active antibiotics, with no apparent impact on the activity of these antibiotics in the mouse peritonitis model.
O381 In infant rat pneumococcal meningitis, ceftriaxone plus daptomycin versus ceftriaxone attenuates brain damage and hearing loss while ceftriaxone plus rifampicin versus ceftriaxone does not
D. Grandgirard, M. Burri, K. Oberson, A. Bühlmann, F. Simon, S.L. Leib* (Berne, CH)
Objectives: Lytic antibiotics for therapy of bacterial meningitis (BM) increase the release of pro-inflammatory bacterial compounds which, in turns, induce inflammation. Exacerbation of the inflammatory response in cerebrospinal fluid (CSF) contributes to the development of neurological sequelae in survivors of BM. Daptomycin, a nonlytic antibiotic acting on Gram-positive bacteria has been shown to decrease inflammation and brain injury vs. ceftriaxone in experimental pneumococcal meningitis. With a view on the clinical application for empiric therapy of paediatric bacterial meningitis we investigated, whether therapies combining daptomycin or rifampicin with ceftriaxone are beneficial when compared to ceftriaxone monotherapy in infant rat pneumococcal meningitis.
Methods: Eleven day old Wistar rats were infected by intracisternal injection of S. pneumoniae and animals were treated with daptomycin (10 mg/kg, s.c., daily) plus ceftriaxone (100 mg/kg, s.c., bid), rifampicin (20 mg/kg, i.p., bid) plus ceftriaxone or ceftriaxone alone. CSF was sampled at 6 h and 22 h after the initiation of therapy and assessed for concentrations of chemo- and cytokines (MCP-1, MIP-1α, IL-1β, IL-6, IL-10; IL-18 and TNF-a). A subset of animals was sacrificed 40 h post infection (h pi) and brain damage quantified by histomorphometry. The remaining animals were treated for 3 d and were tested for hearing loss, by assessing the auditory brainstem response (ABR) at 3 weeks after infection.
Results: Compared to ceftriaxone alone, daptomycin plus ceftriaxone significantly (p < 0.04) lowered CSF concentrations of MCP-1, MIP-1alpha and IL-6 at 6 h and MIP-1α and IL-1β at 22 h after initiation of therapy, led to significantly (p < 0.01) less apoptosis assessed at 40 h pi, and significantly (p < 0.01) improved hearing capacity. While rifampicin plus ceftriaxone also led to lower CSF inflammation (p < 0.02 for IL-6 at 6 h), apoptosis and hearing loss were not significantly different from the ceftriaxone group.
Conclusion: Compared to ceftriaxone monotherapy, daptomycin plus ceftriaxone lowers the level of pro-inflammatory mediators in the CSF and reduces hippocampal apoptosis and hearing loss in infant rat pneumococcal meningitis.
O382 Ceftaroline vs. ceftriaxone in a highly penicillin-resistant pneumococcal pneumonia model
D. Croisier-Bertin*, L. Piroth, P.E. Charles, D. Biek, Y. Ge, P. Chavanet (Dijon, FR; Alameda, US)
Objectives: Ceftaroline (CPT) is a novel, parenteral, broad-spectrum cephalosporin exhibiting bactericidal activity against Gram-positive organisms, including methicillin-resistant S. aureus (MRSA) and multidrug-resistant S. pneumoniae, as well as common Gram-negative pathogens. The efficacy of simulated human dosing with CPT or ceftriaxone (CRO) was evaluated in a rabbit model of penicillin-resistant pneumococcal pneumonia.
Methods: 3 S. pneumoniae strains were used to induce pneumonia in rabbits: PSSP, PISP, and PRSP. MICs (mg/L) were 0.06/0.015, 1/0.125, and 4/0.25 for CRO and CPT, respectively. The animals were randomised to no treatment (controls), intravenous (IV) CPT human equivalent (HE) dosage (600 mg/12 h), IV CRO HE dosage (1 g/24 h), or intramuscular (IM) CPT (5 or 20 mg/kg) for PRSP-infected rabbits. Serum levels were measured by microbiological assay and PK data were obtained. Evaluation of efficacy was based on bacterial counts in lungs and spleen (per gram tissue).
Results: 5–7 animals/group were tested. For IV CPT/IV CRO, mean AUC0–24 was 155/938 mg.h/L, Cmax was 20/158 mg/L and Cmin was 1.3/6 mg/L, respectively. Bacterial counts in target tissues are listed in the Table .
| Group | Mean bacterial concentration ± SD (log10 CFU/g) |
|||||
|---|---|---|---|---|---|---|
| Lung |
Spleen |
|||||
| PSSP | PISP | PRSP | PSSP | PISP | PRSP | |
| Controls | 8.1 ±0.5 | 8.4±0.5 | 8.31±0.7 | 4.91±0.6 | 4±1.4 | 4.51 ±1.1 |
| CRO | 1±0b | 1±0b | 6.2±1.4 | 1±0b | 1±0b | 2.02±1.02a |
| CPT IV CPT IM | 1±0b | 1±0b | 1.1±0.2b,c | 1±0b | 1±0b | 1±0b |
| 5 mg/kg | − | − | 2.31±0.9a,d | − | − | 1.4±0.8a |
| 20 mg/kg | − | − | 1.08±0.16b,c | − | − | 1±0a |
p < 0.05 vs controls
p < 0.001 vs controls
p < 0.01 vs CRO
p < 0.05 vs CRO.
IV CPT and IV CRO were highly efficacious against PSSP and PISP. IV and IM CPT were superior to IV CRO against PRSP with a quasi sterilisation of lungs and spleen. Combined results from the IV and IM studies indicated that %T > MIC for CPT of 30% and 45% were associated with 50% and 100% bacterial count reductions, respectively.
Conclusion: In this rabbit model of penicillin-resistant pneumococcal pneumonia, CPT administered IV (with HE dosing) or by IM administration was more effective against PRSP than IV CRO.
O383 In vivo efficacy of humanised doses of moxifloxacin and piperacillin/tazobactam in animal models of complicated intra-abdominal infections
R. Endermann*, D. Hoepker, K. Merfort, M. Glenschek-Sieberth (Wuppertal, DE)
Objective: Moxifloxacin (MXF) is approved in the USA and other countries for the treatment of complicated intra-abdominal infections (cIAIs). We compared the efficacy of MXF with piperacillin/tazobactam (PIP/TAZ), a commonly used treatment for cIAIs, in three different models: (a) the murine granuloma pouch model with B. fragilis infection; (b) a chronic uterus infection with B. fragilis; and (c) an endogenous infection by normal bowel flora in a murine caecal ligation and puncture (CLP) model. The dosages of antimicrobials used were equivalent to the AUC of the human 400 mg MXF IV q.d. and the time above MIC of human 3.375 g PIP/TAZ IV q.d.s. therapy. Dosing was based on unbound concentrations in humans, neglecting higher Cmax values achieved in animals.
Methods:
-
a.
Granuloma pouch: pouches were formed by injecting air and 0.1% croton oil under the loose connective tissue on the back of mice (3 groups, n = 4–5/group). On day 3, the air was replaced by 0.25% agar in saline. On day 5, B. fragilis ATCC 25285 suspension was injected into the pouch. MXF 100 mg/kg or PIP/TAZ 400 mg/kg b.i.d. were given intravenously (IV) for 2 days. The efficacy endpoint was bacterial load in the pouch.
-
b.
Uterine infection: mice (3 groups, n = 15–28/group) received betaestradiol throughout the study. After 4 days the left uterine tube was surgically prepared and infected with B. fragilis 06688. Mice received IV treatment (MXF 100 mg/kg or PIP/TAZ 400 mg/kg b.i.d.) for 4 days starting on day 21 post-infection. The efficacy endpoint was bacterial load in the uterus.
-
c.
CLP model: the murine caecum was surgically prepared. A ligation was set at the proximal end of the caecum and the ligated part punctured. The caecum was then replaced into the peritoneum. After surgery, mice (3 groups, n = 8–9/group) were treated IV with MXF 100 mg/kg or PIP/TAZ 400 mg/kg for 2 days b.i.d. The efficacy endpoint was survival over 10 days.
Results:
-
a.
Granuloma pouch: MXF provided significantly greater reductions in CFUs than PIP/TAZ (Δ log CFU: MXF 6.78 units, PIP/TAZ 2.95 units; P = 0.029).
-
b.
Uterine infection: MXF provided significantly greater reductions in CFUs than PIP/TAZ (Δ log CFU: MXF 4.45 units; PIP/TAZ 1.16 units; P<0.0001).
-
c.
CLP model: survival over 10 days was significantly higher in the MXF group than in the PIP/TAZ group (P<0.0001).
Conclusions: Using humanised dosages, MXF had greater antimicrobial activity and provided higher survival rates that PIP/TAZ in three different models for cIAI.
O384 The haemochromatosis-associated Hfe mutation protects mice from Salmonella typhimurium infection via induction of lipocalin 2
M. Nairz, I. Theurl, A. Schroll, M. Theurl, S. Mair, T. Sonnweber, G. Fritsche, R. Bellmann-Weiler, G. Weiss* (Innsbruck, AT)
Mutations in HFE predispose to hereditary haemochromatosis type I, a frequent genetic disorder characterised by progressive parenchymal iron deposition and eventual organ failure. Since HFE mutations are associated with reduced iron levels within mononuclear phagocytes, we hypothesized that Hfe deficiency may be beneficial in infections with intramacrophage pathogens.
Using Hfe+/+, Hfe+/– and Hfe–/– mice in a model of typhoid fever, we found that animals lacking one or both Hfe alleles are protected from systemic infection with Salmonella typhimurium, displaying prolonged survival and improved bacterial control. This increased resistance can be referred to an enhanced production of the siderophore-binding peptide lipocalin 2 and the reduced availability of iron for Salmonella engulfed by Hfe deficient macrophages. This effect is mediated via stimulation of lipocalin 2-dependent iron export from infected cells since Hfe–/– macrophages concurrently knocked out for lipocalin 2 are unable to efficiently control the infection or to withhold iron from intracellular Salmonella. Correspondingly, infection of Hfe+/+ and Hfe–/– mice with siderophore deficient Salmonella abolishes the protection conferred by the Hfe defect.
Thus, by inducing the formation of the iron-capturing peptide lipocalin 2, the Hfe mutation harbours a genetically determined immunological advantage towards infections with intracellular pathogens such as Salmonella.
O385 Allogeneic transplantation of mononuclear cells as successful immunotherapy in experimental sepsis by multidrug-resistant Pseudomonas aeruginosa
I. Koutelidakis, A. Kotsaki, P.D. Carrer, K. Louis, A. Savva, E.J. Giamarellos-Bourboulis* (Thessaloniki, Athens, GR)
Objective: The majority of clinical trials of immunointervention in severe sepsis have failed to disclose survival benefit. A likely explanation may be administration of therapy when immunoparalysis of the septic host supervenes. In an attempt to reverse immunoparalysis, injection of mononuclear cells was attempted in experimental sepsis by multidrug-resistant Pseudomonas aeruginosa (MDRPA).
Methods: Peripheral blood mononuclear cells (PBMCs) diluted in RPMI were isolated from five healthy human volunteers after gradient centrifugation over Ficoll. 1 × 107/kg of one MDRPA live or heat-killed isolate from one patient with severe sepsis was injected intraperitoneally for bacterial challenge. A total of 72 male C57B6 mice were studied divided into four groups: group A (n = 26) pre-treated with RPMI and challenged after one hour with live isolate; group B (n = 26) pretreated with 5×107 PBMCs/kg and challenged after one hour with live isolate; group C (n = 10) pre-treated with RPMI and challenged after one hour with heat-killed isolate; group D (n = 10) pre-treated with 5 × 107 PBMCs/kg and challenged after one hour with heat-killed isolate. Survival was recorded for 20 mice of groups A and B and for all mice of groups C and D. Six mice of groups A and B were sacrificed six hours after challenge. Blood was collected from the lower vena cava and TNFalpha and IL-6 were estimated in serum by an enzyme immunoassay. Bacterial growth of liver and lung at the same time was assessed.
Results: Median survival of group A was 24 hours and of group B 88 hours (log-rank: 4.524, p: 0.033). Nineteen animals of group A died (95%) compared with eight animals of group B (40%, p: 0.038). Four animals of group C died (40%) compared with nil animals of group D (0%, log-rank: 4.274, p: 0.03). Median serum TNF-α of groups A and B at sacrifice was 31 and 184 pg/ml respectively (p: 0.048). Respective values for IL-6 were 2084 and 2231 pg/ml (pNS); for liver bacterial cells 3.63 and 4.99 log10 cfu/g (pNS); and for lung bacterial cells 2.56 and 4.22 log10 cfu/g (pNS).
Conclusions: Allogeneic transplantation with PBMCs prolonged survival in experimental sepsis by MDRPA. Its mechanism of action was related with a) blockade of cell wall structures as shown by survival experiments with heat killed isolate; and b) reversal of immunoparalysis as evidenced by increase of serum TNF-a. This approach creates a promising novel perspective for immunointervention in sepsis.
O386 Small-animal positron emission tomography in the mouse model of genital Chlamydia infection
A. Marangoni*, C. Nanni, M. Donati, R. Aldini, D. di Pierro, S. Trespidi, S. Accardo, S. Fanti, R. Cevenini (Bologna, IT)
Objectives: Chlamydia trachomatis is one of the world's major causes of sexually transmitted diseases of the cervix and urethra and it is a major agent of pelvic inflammatory disease.
Genital tract infection of female mice with Chlamydia muridarum closely mimics acute genital tract infection in women. Aim of this study was to assess the predictivity of 68Ga-chloride Small Animal Positron Emission Tomography (PET) for the identification of reactive animals and the follow-up of infection at various times after vaginal inoculation.
Methods: Chlamydiae elementary bodies were purified from LLC-MK2 cells by sucrose-gradients density centrifugation.
Animals used in this study were 23 female Balb/c mice, 6–8 weeks old. All the animals received 2.5 mg of medroxyprogesterone acetate i.m. 9 and 2 days prior the infection.
20 mice were infected by placing 15 µl of SPG containing 107 inclusion forming units (IFUs) of C. muridarum into the vaginal vault. Infection was induced under Ketamine anaesthesia. As control, 3 animals were challenged with 15 µl of SPG.
5 infected animals plus 1 control mouse underwent a 68Ga-chloride Small Animal PET. After 60 minutes of uptake, the animals were anaesthetized again and whole body images were acquired for 15 minutes in a single bed position using a Small Animal PET tomography. Images were reconstructed with iterative algorithm. This procedure was performed 5, 12 and 19 days after infection.
Infection was monitored by obtaining cervical-vaginal swabs from all the 20 infected animals 6, 13 and 20 days after infection. Moreover, 5 groups of 3 animals each were sacrificed at 6, 13, 20, 27 and 34 days after infection. Genital tracts were divided into the cervical-vaginal region, uterine horns, and oviducts. Individual wells of LLC-MK2 monolayers in 24-well plates were inoculated with 200 µl of the solution from vaginal swabs or homogenised tissues.
Inclusions were visualised by using fluorescein conjugated monoclonal antibody against Chlamydia group antigen.
Results: Results are summarised in the figure.
Conclusion: These preliminary data indicate that 68Ga-chloride PET is a promising technique to in vivo evaluates inflammatory response to genital C. muridarum infection. Further studies are required to test 68Ga-chloride PET's potential in the follow-up of animals with experimental genital infection after antibiotic treatment.
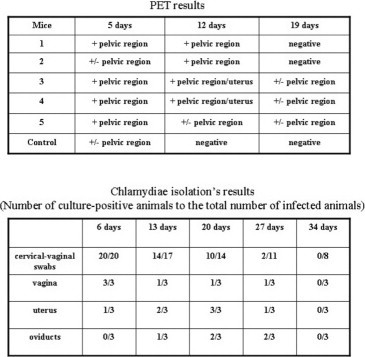
Nosocomial infections: a major clinical problem
O387 Inadequate statistical power of published comparative cohort studies on ventilator-associated pneumonia to detect mortality differences between the compared groups
M. Falagas*, V. Kouranos, A. Michalopoulos, S. Rodopoulou, A. Athanasoulia, D. Karageorgopoulos (Athens, GR)
Objective: Comparative cohort studies are often conducted to identify novel therapeutic strategies or prognostic factors for ventilator-associated pneumonia (VAP). We aimed to evaluate the statistical power of such studies to provide statistically and clinically significant conclusions.
Methods: We searched in PubMed and Scopus for comparative cohort studies evaluating the mortality of patients with VAP. We calculated for each of the included studies the statistical power to detect the observed difference in mortality between the compared groups (observed power), as well as 3 expected, clinically relevant, effect sizes (expected power).
Results: We identified 39 (20 prospective) comparative cohort studies on VAP as eligible for inclusion in this analysis. The median observed power of these studies was 17.9% [interquartile range (IQR), 9.8–52.4%]. The median expected power was 10.0% (IQR, 7.2–13.6%) for a risk ratio for mortality of 0.85 between the compared groups; 14.7% (IQR, 10.6–21.8%) for a risk ratio of 0.80; and 7.9% (IQR, 6.3–10.2%) for a reduction in mortality from 30% to 25%. All expected power measures were significantly lower than the observed power.
Conclusion: The statistical power of most cohort studies to detect the observed difference in mortality between compared groups of patients with VAP is low. The power is even lower when expected, clinically relevant, differences in mortality are considered. For a wiser utilisation of resources allocated to research, we favour the conduction of cohort studies with larger sample size so that potential differences between the compared groups are more likely to be shown.
O388 Frequency, prevention, outcome, and treatment of ventilator-associated tracheobronchitis: systematic review and meta-analysis
M. Agrafiotis*, I. Siempos, M. Falagas (Athens, GR)
Objective: To clarify issues regarding the frequency, prevention, outcome, and treatment of patients with ventilator-associated tracheobronchitis (VAT), which is a lower respiratory tract infection involving the tracheobronchial tree, while sparing the lung parenchyma.
Methods: We performed a systematic review and meta-analysis of relevant available data, gathered though searches of PubMed, Scopus, and reference lists, without time restrictions. A conservative random effects model was used to calculate pooled odds ratios (OR) and 95% confidence intervals (CI).
Results: Out of the 564 initially retrieved articles, 30 papers were included. Frequency of VAT was 10.2%. Selective digestive decontamination was proved an effective preventive strategy against VAT. Presence, as opposed to the absence, of VAT was not associated with higher mortality (OR: 1.18, 95% CI 0.90–1.53). Administration of systemic antimicrobials (with or without inhaled ones), as opposed to placebo or no treatment, in patients with VAT was not associated with lower mortality (OR: 0.56, 95% CI 0.27–1.14). Most of the studies providing relevant data noted that administration of antimicrobial agents, as opposed to placebo or no treatment, in patients with VAT was associated with more ventilator-free days and lower frequency of subsequent pneumonia, but without shorter length of intensive care unit stay or shorter duration of mechanical ventilation.
Conclusions: Approximately one tenth of mechanically ventilated patients suffer from VAT; an infection potentially prevented by the implementation of selective digestive decontamination. Antimicrobial treatment of patients with VAT may protect against the development of subsequent ventilator-associated pneumonia.
O389 Characteristics of elbow prosthetic joint infection: a 13-year retrospective analysis of 358 elbow prostheses
Y. Achermann*, C. Spormann, C. Kolling, C. Remschmidt, J. Wüst, B. Simmen, M. Vogt (Baar, Zurich, CH)
Objectives: Elbow arthroplasty is increasingly used for treatment of rheumatic or posttraumatic arthritis. Data on epidemiology, characteristics and treatment outcome of elbow prosthetic joint infection (PJI) is limited. Furthermore, no validated therapeutic algorithm exist as for hip or knee PJI. We analyzed all PJI, which occurred in a cohort of implanted elbow prostheses during a 13-year-period.
Methods: Between 01/1994 and 12/2007, all cases with implanted elbow prosthesis at our institution were retrospectively included. Elbow PJI was defined as visible purulence, acute inflammation on histopathology, sinus tract or microbial growth in periprosthetic tissue. Patients were regularly follow-up at outpatient orthopedic visits and were in addition recently contacted by phone. A Kaplan-Meier survival analysis was performed.
Results: During the study period, 358 elbow prostheses were implanted. Overall, 25 of 358 cases (7%) developed elbow PJI (median age 61y, range 41–82y, 40% males). Among them, 14 (56%) had a rheumatic disorder and 11 (44%) a posttraumatic arthritis. 12 infections were early (≤ 3 months), 3 were delayed (3–24 months) and 10 were late (≥ 24 months). More infections were acquired intraoperatively (n = 15, 60%) than haematogenously (n = 10, 40%). The following pathogens were cultured: Staphylococcus aureus (n = 11), coagulase-negative staphylococci (n = 7), Streptococcus agalactiae (n = 2), Corynebacterium sp. (n = 1), Enterococcus sp. (n = 1), Enterobacter cloacae (n = 1), mixed infections (n = 1) and culture-negative (n = 1). Treatment approaches included débridement with implant retention (n = 19), one-stage exchange (n = 2), two-stage exchange (n = 1), resection arthroplasty (1) and antibiotics only (n = 2). At follow-up, 16 (64%) patients were free of infection (median follow-up time 2.6 y, range 0.7–11.3 y) and 9 (36%) had a relapse (median time to infection 0.4 y, range 0.1–4.0 y). One patient died due to infectious endocarditis with secondary haematogenous elbow PJI. The relapse-free survival (95% confidence interval) was 75% (58%-93%) after 1 year, 70% (52%-89%) after 2 years, 62% (39%-85%) after 3 years and 52% (27%-78%) after 4 years.
Conclusions: The infection incidence after elbow arthroplasty was higher (7%) than reported after hip (<1%) or knee arthroplasty (<2%). Most infections (48%) manifested early (≤ 3 months). Underlying rheumatic disorder were common in elbow PJI (58%). The relapse-free survival after elbow PJI was 75%, 70%, 62% and 52% after 1, 2, 3 and 4 years.
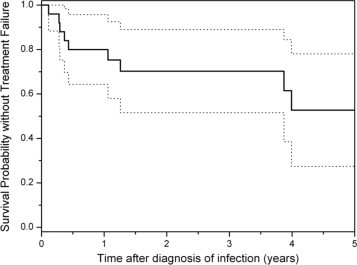
O390 Ecological effects of selective digestive tract decontamination and selective oropharyngeal decontamination on colonisation with antibiotic resistant Gram-negative bacteria
E.A.N. Oostdijk*, A.M.G.A. De Smet, H.E.M. Blok, E.S. Thieme Groen, J.A. J. W. Kluytmans, M.J.M. Bonten (Utrecht, Breda, NL)
Introduction: Selective Digestive tract Decontamination (SDD) and Selective Oropharyngeal Decontamination (SOD) aim to eradicate Gram-negative bacteria (GNB) from the intestinal en respiratory tract in intensive-care-unit (ICU) patients. We aimed to quantify effects of SDD and SOD on bacterial ecology in 13 ICUs that participated in a clustered group-randomised cross over study in the Netherlands, in which SDD, SOD or standard care (SC) was used during consecutive periods of 6 months (NEJM 2009;360:20). The order of periods was randomised per ICU.
Methods: Point prevalence surveys of rectal and respiratory samples were performed once monthly in all patients in ICU (receiving or not receiving SOD/SDD). Selective media were used to detect GNB and MIC testing was done for ceftazidime (CFT), ciprofloxacin (CIP) and tobramycin (TOB). Effects of SDD on rectal carriage were determined by comparing data from 6 SDD months in each ICU to data from all months preceding and following (in which SOD or SC was given). Combined effects of SDD/SOD on respiratory tract carriage were determined by comparing data from 12 months SDD/SOD (in any order) to data from the 6 SC months before and afterwards.
Results: 2583 rectal and 2023 respiratory tract samples were analysed. During SDD average proportions of patients colonised with GNB resistant to either CFT, TOB, CIP were 5%, 7% and 7% and these proportions were 15%, 13% and 13% during the post-intervention period (p < 0.05 in each case). This effect is most explicit for CFT with resistance levels increasing from 2.6% in the last month of SDD to 11.4% in the 1st month after SDD (p < 0.05). During SDD and SOD resistance levels in respiratory tract samples were <6% for all three antibiotics, but prevalence increased gradually (for CFT and TOB resistance; p < 0.05 for trend). After discontinuation of SDD and SOD average proportions increased to levels >10% for all three antibiotics (p < 0.05 in each case). CFT resistant isolates in rectal samples mainly included Enterobacteriaceae not being Escherichia coli and Klebsiella spp, whereas TOB and CIP resistant isolates mainly included E. Coli.
Conclusion: SOD and SDD have marked effects on the bacterial ecology in an ICU with a rapid and persistent increase in resistance after intervention. Antibiotic resistance remains a major concern associated with these infection control measures.
O391 Throwing caution to the winds? Three cases of anaphylaxis to chlorhexidine coated central venous catheters from a regional cardiac centre in northwestern England
A. Guleri*, M. Hartley (Blackpool, UK)
Background: Chlorhexidine, a bactericidal antiseptic chemical, is used in a wide variety of clinical settings within our institution. We report a cluster of 3-cases of anaphylaxis to chlorhexidine coated central venous catheters in patients scheduled for cardiac surgery in the Lancashire Cardiac Centre in northwest England during 2008.
Chlorhexidine based products include skin prep [2%] prior to venepuncture/insertion of vascular catheters, shampoo/bodywash [preop and MRSA decolonisation regime]; urinary catheter lubricant; contact lens solution; mouthwash; topical cream; chlorhexidine bonded medical devices.
Case study: All 3-patients suffered a severe systemic anaphylactoid reaction immediately after insertion of a central venous catheter impregnated with chlorhexidine acetate and silver sulfadiazine (ARROWgard Blue Catheter). Two of the patients responded to standard resuscitation and the surgery was postponed to a later date. The third patient failed resuscitation measures requiring cardiac massage until cardiopulmonary bypass was established and cardiac surgery was performed. In all 3 patients, tryptase levels were acutely elevated indicating mast cell degranulation. Subsequently, allergen specific IgE to chlorhexidine was demonstrated and skin prick/intradermal testing was positive to chlorhexidine, confirming the diagnosis of chlorhexidine-precipitated anaphylaxis in each patient.
A detailed review of the case-notes revealed that each patient had manifest evidence of minor cutaneous reactions to pre-operative chlorhexidine use that had not been ascribed to chlorhexidine at the time.
Discussion: FDA issued a public health notice [1998] following 1st description of anaphylaxis to chlorhexidine coated central venous catheter. A recent case cluster has also been reported from another cardiac centre in the UK [3-cases over a 9-month period]. References to be presented.
It is interesting that these reports of chlorhexidine anaphylaxis have all occurred in patients undergoing cardiac surgery. These patients receive multiple exposures to chlorhexidine during their pre-operative investigations and preparation. This has increased recently as a result of the drive to reduce the incidence of hospital-acquired infections. We wish to postulate that these patients have been sensitised by repeated topical exposure to chlorhexidine and have exhibited anaphylaxis when this allergen was presented to the patient in the form of the chlorhexidine coated central venous catheter.

O392 The effects of closed endotracheal suction systems on cross transmission with Pseudomonas aeruginosa in intensive care unit patients
I. Jongerden*, A. Buiting, J. Kesecioglu, S. Zeidler, M. Leverstein-van Hall, B. Speelberg, M. Bonten (Utrecht, Tilburg, NL)
Objectives: Closed endotracheal Suction Systems (CSS) are increasingly used in mechanically ventilated intensive care (ICU) patients. As compared to the traditional – and less expensive – Open Suction Systems (OSS), CSS are assumed to reduce bacterial cross-transmission, although this has not been studied extensively. We determined the effects of CSS, as compared to OSS, on the incidence of cross-transmission with Pseudomonas aeruginosa (PA) in a cluster-randomised cross-over study in four ICUs in two hospitals (between January 2007 and March 2008).
Methods: During two 6-month periods, all endotracheal suctioning procedures (ES) in a single unit were performed with either OSS or CSS, with the order of systems randomised. All patients with a length of ICU stay >24 hours were included and respiratory samples were collected for microbiological analysis on admission, and twice weekly thereafter. Samples were analyzed for growth of PA and representative isolates were genotyped with multiple-locus variable-number tandem-repeats analysis (MLVA). Cross-transmission was defined upon MLVA-type and overlapping times in ICU.
Results: In all, 1110 patients (11319 patientdays) were included and 68 (6.1%) patients were colonised with PA on admission. 107 Patients acquired colonisation with PA: 46 (8.4%) and 61 (12.6%) during CSS and OSS, respectively (p = 0.026). Acquisitions per 1000 patientdays at risk were 9.7 for CSS and 14.4 for OSS (p = 0.040). Yet, average daily PA prevalence in the ICUs was 12.4 and 14.5 during CSS and OSS, respectively (p = NS). In all, 4903 cultures were obtained (completeness of culture taking 96%). 228 PA strains from 158 patients were genotyped. During CSS, 38 of 70 patients (54%) carried a strain shared by at least one other patient, which was 40 of 88 patients (45%) during OSS. Within overlapping time intervals between positive PA cultures, there were 9 (22.5%) and 8 (14.5%) possible cases of cross-transmission during CSS and OSS, respectively (p = NS). Taking into account a timeframe of 9 days between positive PA cultures, 15 (37.5%) possible cases during CSS and 12 (21.4) during OSS were counted (p = NS).
Conclusion: In crude analysis, CSS was associated with a 4% lower acquisition rate with PA, which could not be explained by a lower incidence of cross-transmission and which yielded a slightly decreased average endemic prevalence in the ICU.
O393 Repeated prevalence surveys of healthcare-associated infections in Finnish neonatal intensive care units – preliminary results
E. Sarvikivi*, O. Lyytikäinen on behalf of the NICU Prevalence Survey Study Group
Objectives: To evaluate the burden of healthcare-associated infections and the distribution of infection types and causative agents in neonatal intensive care unit (NICU) patients.
Methods: NICUs of all secondary and tertiary care hospitals in Finland were invited to the prevalence study consisting of six monthly surveys, the first of which was conducted in November 2008. All infants present in the unit at the day of the study were included. A one-day training session for the study teams of the participating units was organised. The study protocol, a standardised case-record form, written definitions for all study variables, and CDC definitions (in Finnish) as well as practical case exercises were provided. Variables collected included gestational age, birth weight, type of delivery, severity of illness, preceding surgery, and contact isolation. For infections, type, origin and causative microbes were recorded. Indwelling devices (e.g., urinary catheter, central or peripheral line, ventilator) and antimicrobial agents were documented on the study day and retrospectively, for the preceding six days.
Results: All invited NICUs (N = 23) accepted the invitation. The first survey included 209 patients, 95 (45%) of whom from tertiary care NICUs. In total, 42 (20%) patients with 43 infections were detected. The most common type of infection was clinical sepsis, 52% of which had an onset during the first day of life. Positive cultures were obtained from 8 (19%) of the infections. The causative agents identified were Staphylococcus aureus, Corynebacterium diphtheriae, Staphylococcus capitis, Enterococcus faecalis, and coagulase-negative staphylococci. Table 1 summarises the characteristics of patients and infections stratified according to the level of care. Data on five surveys will be available and presented in May 2009.
Table 1.
Characteristics of patients and infections during the first point prevalence survey of healthcare-associated infections in 23 neonatal intensive care units (NICUs), Finland, November 2008
| NICUs |
|||
|---|---|---|---|
| Tertiary care (N = 5) | Secondary care (N = 18) | All (N = 23) | |
| Patients, N (%) | 95 (45) | 114 (55) | 209 (100) |
| Birth weight <1500 g | 41 (43) | 27 (23) | 68 (24) |
| Ventilator | 7 (7) | 1 (1) | 8 (4) |
| Nasal-CPAP | 29 (31) | 5 (4) | 34 (16) |
| Total parenteral nutrition | 13 (14) | 4 (4) | 17 (8) |
| Central venous catheter | 17 (18) | 1 (1) | 18 (16) |
| Patients with infection(s), N (%) | 25 (26) | 17 (15) | 42 (20) |
| Bloodstream infection | 4 | 0 | 4 |
| Clinical sepsis | 17 | 14 | 31 |
| Pneumonia | 4 | 0 | 4 |
| Urinary tract infection | 0 | 1 | 1 |
| Necrotising enterocolitis | 1 | 0 | 1 |
| Conjunctivitis | 0 | 2 | 2 |
Conclusions: The infection prevalence was high. However, most infections were classified as clinical sepsis, and the prevalence of this type of infection is likely to be overestimated due to the fact that empiric antimicrobial treatment is routinely started if maternal risk factors for neonatal infection exist. Repeated surveys can help to improve collaboration between the infection control team and ward staff, and thereby lead to improved surveillance and control of healthcare-associated infections.
O394 NA Antimicrobial prophylaxis in surgery: an international survey
V. Alexiou*, V. Ierodiakonou, G. Peppas, M. Falagas (Athens, GR)
Background: We sought to investigate current clinical practice of antimicrobial prophylaxis (AMP) in surgery.
Methods: Survey regarding the administration of AMP to patients, without comorbidity or allergy, undergoing surgery, among surgeons indexed as corresponding authors for articles published in general surgery, orthopedics, gynaecology and cardiac surgery journals.
Results: 1068 surgeons answered (response rate 68%). 26.1% of the respondents do not begin infusion of the first antimicrobial dose within 1 hour from incision, as suggested by guidelines, 27.2% continue administering AMP for 2 or more days after surgery, including 7.6% that continues for 4–7 days after surgery. There were significant differences in the selection of AMP regimens between participating surgeons from Europe and North America. Furthermore, 19% of Europeans order infusion of the first antimicrobial dose during incision compared to 3.9% of North Americans, 74.2% of Europeans discontinue AMP within 24 hours from surgery compared to 86% of North Americans. Finally, 31% of general surgeons originating from the North America administer supplementary oral prophylaxis for colectomy compared to only 5% of surgeons from Europe.
Conclusions: Even among experts, certain aspects of AMP are rather controversial. A uniform, evidenced-based practice is warranted especially in the era of increasing antimicrobial resistance.
O395 Inhaled colistin as adjunctive to intravenous colistin for the treatment of microbiologically documented VAP
I. Korbila, A. Michalopoulos, P. Rafailidis, D. Nikita, G. Samonis, M. Falagas* (Athens, Heraklion, GR)
Objective: Ventilator-associated pneumonia (VAP) due to multidrug-resistant Gram-negative bacteria contributed to the revival of intravenous (IV) colistin. However, the administration of inhaled colistin for VAP is controversial.
Methods: We performed a retrospective cohort study of patients with microbiologically documented VAP who received IV with or without inhaled colistin.
Results: 78 patients with VAP received IV plus inhaled colistin, while 43 patients received IV colistin alone, at an average daily IV colistin dose of 7.0±2.4 (mean±SD) and 6.4±2.3 million IU, respectively (P = 0.13); the average daily dose of inhaled colistin was 2.1 ±0.9 million IU. The outcome of infection was cure for 62/78 (79.5%) versus 26/43 (60.5%) patients who received IV plus inhaled colistin versus IV colistin alone, respectively (P = 0.025); all-cause in-hospital mortality was 31/78 (39.7%) versus 19/43 (44.2%), respectively (P = 0.63); all-cause ICU mortality was 28/78 (35.9%) versus 17/43 (39.5%), respectively (P = 0.92). The use of inhaled colistin was the only variable independently associated with cure of VAP in the multivariable analysis [odds ratio (OR) = 2.53, 95% confidence interval (CI) = 1.11–5.76]. The only independent predictors of mortality were a greater APACHE II score (OR = 1.12, 95% CI = 1.04–1.20), presence of malignancy (OR = 4.11, 95% CI = 1.18–14.23) and lower daily dosage of IV colistin (OR = 0.81, 95% CI = 0.68–0.96).
Conclusion: The outcome of VAP was better in patients who received inhaled colistin along with IV colistin than IV colistin alone. There was no statistically significant difference regarding all-cause in hospital and ICU mortality between the compared groups. Randomised controlled trials are warranted to further evaluate the role of inhaled colistin in VAP.
O396 Increased risk of common infections in hospitalised patients with type 2 diabetes mellitus
A. Zacharof* (Halandri, GR)
Objectives: Clinical data on the association of Diabetes Mellitus (DM) with common infections are lacking, are not conclusive, and are often biased. We try to determine the relative risk of common infections in patients with type 2 DM.
Methods: In a 21 year's prospective cohort study conducted as part of our Hospital epidemiological Survey, we compared 1797 adult patients who had DM type 2 with 4189 control patients who had hypertension without diabetes. We measured the number of attended episodes of infection in the respiratory tract, urinary tract, and skin and mucous membranes. We applied statistical multivariable and logistic regression analysis to determine independent risks of infections and their recurrences in patients with diabetes, compared with control patients.
Results: Upper respiratory infections were equally common among patients with diabetes and control patients. Patients with diabetes mellitus had a greater risk of lower respiratory tract infection (adjusted odds ratio: 1.32 [95% Confidence Interval, 1.13–1.53]), urinary tract infection (adjusted odds ratio 1.24 [95% CI, 1.10–1.39]), bacterial skin and mucous membrane infection (adjusted odds ratio 1.33 [95% CI, 1.15–1.54]), and mycotic skin and mucous membrane infection (adjusted odds ratio 1.44 [95% CI, 1.27–1.63]). Risks increased with recurrences of common infections.
Conclusion: Patients with Diabetes Mellitus type 2 are at increased risk for lower respiratory tract infection, urinary tract infection, and skin and mucous membrane infection. Studies are warranted into management of such infections in patients with diabetes.
Current management of Helicobacter pylori infections
S414 Epidemiology of H. pylori infection
H. Rautelin* (Uppsala, SE)
Helicobacter pylori causes a chronic infection in the human gastric mucosa (gastritis) worldwide. Man is the natural host of H. pylori. It has been estimated that about half of the world's population is infected. The critical period to obtain the infection is in childhood and early adolescense, although the precise person-to-person transmission routes are largely unclear. Low socioeconomic status and crowded living conditions are risk factors for H. pylori infection. In these conditions the child may easily obtain the infection from an infected mother or infected siblings. H. pylori usually causes a life-long infection, which only rarely disappears unless treated. However, since the early 1900 s, and particularly during the latter half of the century, the prevalence rates of H. pylori infection have clearly decreased in developed countries along with rapidly improving living standars. In elderly people the infection is still common and reflects the high prevalence rates of the infection in their childhood, whereas in the youngest age groups, the infection is rare due to a low rate of childhood infections. In developed countries the rate of new infections in adults is rare, about 1–2% per 10 years and thus, the low prevalence of H. pylori at present in the young age groups is not likely to increase during the coming years. In a recent study from Finland, the seroprevalence of H. pylori was about 3% among teenagers and among the 45-year-old subjects the seroprevalence was <30%. In addition to the natural decline of H. pylori infection, the active treatment of the infection in many developed countries has contributed to the rapid disappearance of H. pylori. The prevalence of H. pylori is much higher in developing than developed countries. This is also reflected in developed countries in the higher prevalence rates of H. pylori among children born to parents of foreign origin. H. pylori causes always gastritis and about 15–20% of the infected individuals will develop other sequelae such as peptic ulcer disease. However, the rapidly declining prevalence rate of the infection is reflected in the decreasing number of H. pylori positive peptic ulcers in many countries. About one third or even half of infected individuals develop atrophic gastritis, a risk factor for gastric cancer, during decades of the infection. The declining prevalence rates of H. pylori infection have been associated with the declining incidences of gastric cancer later on.
S415 Diagnosis of H. pylori in a high and low prevalence population
H.I. Maaroos* (Tartu, EE)
Detection of the H. pylori is based on the direct examination of the bacteria (bacteriology, morphology, cytology), on the production of urease by the bacteria (13 C urea breath test, rapid urease test), on the production of antibodies to H. pylori (several serological tests) or on the molecular genetics of the bacteria (PCR tests). Some of the tests require invasive procedures (endoscopy) and some others belong to group of noninvasive tests. Usually, the diagnosis of H. pylori infection must be proved at least by two positive tests. The sensitivity and the specificity of the tests is variable. The choice of the tests is dependent not only their invasive or nonivasive character or their sensitivity and specificity, but also on the aim of testing (screening of population, diagnosing of the disease, checkup of the results of treatment). Additional factor influencing the results of testing is the prevalence of H. pylori infection in studied target groups. The accuracy of the tests is lower in a primary health care setting than in a hospital setting owing to the lower prevalence of target disorders among patients consulting the family doctor. Estimation of the pre-test probabilities of the infection in individual patients is needed to achieve high accuracy of test results. Also validation of the tests is essential for different populations as the rate of H. pylori infection varies greatly among different European countries and different ethnic groups.
S416 Antimicrobial susceptibility and treatment strategies
F. Mégraud* (Bordeaux, FR)
Helicobacter pylori can become resistant to most of the drugs currently used for the eradication. As with Mycobacterium tuberculosis, this resistance occurs essentially via point mutations. Due to selection pressure the level of resistance is constantly evolving and necessitates setting up surveillance systems. At the European level, point prevalence evaluation is made every 10 years.
We will report on the last survey which began in April 2008 and is scheduled to last until March 2009. Thirty-seven centres from 23 countries supposedly culturing H. pylori routinely have been enrolled. The same protocol for susceptibility testing using Etest for 5 antibiotics (clarithromycin, levofloxacin, tetracycline, amoxicillin, rifabutin and metronidazole) kindly provided by AB BioMerieux are used on a defined Mueller Hinton blood agar. Only patients not having received previous H. pylori treatment have been included. An on-line report system has been designed.
At this stage the results for 1,000 patients and H. pylori strains are reported and indicate a global resistance rate of 19.9% to clarithromycin, 13.9% to levofloxacin and 35.4% to metronidazole. As expected, resistance to amoxicillin 2.1%, tetracycline 1.2% and rifabutin 0.7%, is low. Detailed results will be presented according to age, gender, country of residence and of birth, and endoscopic features.
According to the European Maastricht 3 guidelines (1995), susceptibility to clarithromycin should be tested or clarithromycin should not be used, if its resistance reaches 15–20%, which is the case in most European countries. An alternative is to use levofloxacin with amoxicillin and a proton pump inhibitor (PPI) for 10 days but resistance to levofloxacin is also increasing very quickly. Other possibilities include a combination of amoxicillin-metronidazole or tetracycline-metronidazole always with a PPI despite metronidazole resistance which can be overcome in vivo by increasing the treatment duration. Rifabutin can also be used with amoxicillin but must be kept as the last option because of its toxicity and impact on Mycobacteria.
Acknowledgement: The author is grateful to the steering committee of the European survey of antimicrobiol susceptiblility of H. pylori: Y. Glupczynski, A. Hirschl, M. Kist, M. Lopez Brea, L. Andersen as well as to the participants who made this study possible.
S417 CagA of Helicobacter pylori acts at the very early stage of differentiation of MDCK monolayers
L. Buti, R. Rappuoli, A. Covacci*, H. Ploegh (Siena, IT; Cambridge, US)
Type I strains of Helicobacter pylori possess the cag pathogenicity island to deliver virulence factors. cag is a specialised Type IV secretion machinery that is activated during infection and comprises 31 genes originated from a distant event of horizontal transfer. After translocation the effector protein CagA is phosphorylated on tyrosine residues restricted to a previously identified repeated sequence called D1. This sequence is located in the C-terminal half of the protein and contains the five amino acid motif EPIYA, which is amplified by duplications in a large fraction of clinical isolates. Tyrosine-phosphorylation of CagA is essential for the activation process that leads to dramatic changes in the morphology of cells growing in culture. In addition, we observed that two members of the Src kinases family, c-Src and Lyn, account for most of the CagA-specific kinase activity in AGS cell lysates. Translocated CagA interacts with the ZO-1 and Jam host-cell proteins causing disruption of the apical junctional complex. Transfection of the cagA gene into polarised epithelial cells induces disruption of cell-to-cell contacts and altered morphology. Strikingly CagA-expressing cells become migratory and invasive penetrating into collagen gel. The study of different portions of the molecule revealed the presence of two distinct functional domains and both are necessary to induce abnormal cell differentiation through interactions with host cell morphogens. Cell polarity and invasion have been suggested to contribute to both early and late stages of cancer formation. These results suggest a mechanism by which CagA may acts at the early stage of tumorigenic progression causing loss of cell polarity, increased cell motility and invasiveness of epithelial cells.
European perspective on mosquito- and rodent-borne viral diseases
S423 The spread of Chikungunya virus
P. Parola* (Marseille, FR)
After a period of 50 years of silence, a disease with an unpronouncable name, “chikungunya” (CHIK), has recently become a medical reality and reached the public throughout the world. In 2004, a large chikungunya virus (CHIKV) outbreak emerged in Eastern Africa, spread in West Indian Ocean islands with an unprecedented devastating outbreak in 2005–2006, then jumped to India and continued expansion into South-eastern Asia. In 2007, the virus reached Europe. Since the beginning of this outbreak, several million cases of chikungunya virus disease have occurred in autochthonous populations and in travelers who were diagnosed after they returned home from epidemic areas. New clinical entities, including severe to lethal presentations, were reported in complement to classical features, a febrile polyarthritis followed by long-lasting rheumatism. CHIKV which was usually transmitted by Aedes aegypti mosquitoes, has now been repeatedly associated with a new vector, Ae. albopictus (the “Asian Tiger Mosquito”) which has spread in tropical areas previously occupied predominantly by Ae. aegypti, and has dispersed worldwide. Within one year, a single new mutation (E1-A226V) was present in the CHIKV isolates in all places, providing selective advantage for CHIKV transmission by Ae. albopictus. Due to the globalisation of Ae. albopictus, this mutation increases the potential for CHIKV to permanently extend its range into Europe, Americas and other susceptible areas. As CHIKV could spread throughout the world, all physicians should be prepared to encounter this arboviral infection that represent a paradigm for emerging arboviral infections. We present here the different aspects of this reemerging and fascinating disease, focusing on the lessons from the recent large scale outbreaks.
Beyond antibiotics: the biologic basis and clinical utility of adjuvant therapy for severe pneumonia (Symposium arranged with the International Sepsis Forum)
S426 Low-monocyte human leucocyte antigen-DR expression is independently associated with nosocomial infections after septic shock
C. Landelle*, A. Lepape, N. Voirin, E. Tognet, J. Bohé, P. Vanhems, G. Monneret (Lyon, FR)
Objective: Sepsis-induced immunosuppression is hypothesized to contribute to a heightened risk of secondary nosocomial infection (NI). The main objective is to assess whether low monocyte human leucocyte antigen-DR (mHLA-DR) expression, proposed as a marker of immunosuppression, is associated with an increase of NI after septic shock.
Methods: A prospective observational study was conducted in 2 intensive care units (ICUs) in a French university hospital. The study included 209 septic shock patients during the period December 1, 2001 through April 30, 2005. mHLA-DR was measured by standardised flow cytometry at days 3–4 and 6–9 after the onset of septic shock. All patients were screened daily for 4 NI sites after septic shock onset during ICU stay: microbiologically-documented pulmonary, urinary tract, bloodstream and catheter-related infections. A multivariate Cox model was used to identify the variable independently associated with the risk of NI, based on their adjusted hazard ratios (aHR) and their 95% confidence interval (95% CI).
Results: At days 3–4, we obtained measurements in 153 patients of whom 42 developed NI. The latter exhibited lower mHLA-DR values than those without NI (28% vs 39%, p = 0.03). Multivariate Cox model analysis revealed that mHLA-DR <25% was the sole factor independently associated with NI occurrence after adjustment for clinical parameters (age, gender, Simplified Acute Physiology Score II, Sepsis-related Organ Failure Assessment, and intubation) with an aHR of 1.92 (95% CI: 1.04–3.57; p = 0.04). Similarly, at days 6–9, mHLA-DR <40% remained the sole parameter predicting NI with an aHR of 2.28 (95% CI: 1.19–4.36; p = 0.01).
Conclusion: Low mHLA-DR expression after septic shock independently predicts NI. This promising biomarker may be of major interest in identifying patients at increased NI risk who could benefit from targeted and tailored therapy aimed at restoring immune functions.
S427 The cytokine response in severe pneumonia: insights from preclinical studies
T. van der Poll* (Amsterdam, NL)
Pneumonia, the leading infectious cause of death in the US, kills more people annually than AIDS, tuberculosis, meningitis and endocarditis combined. From a wide range of observational studies of community-acquired pneumonia (CAP), only half of the cases had an aetiologic agent identified. Streptococcus pneumoniae was consistently the predominant bacterial aetiology. This lecture will primarily focus on the innate immune response to pneumococcal pneumonia.
Toll-like receptors (TLRs) are key molecules that recognize pathogen associated molecular patterns (PAMPs) and induce an inflammatory response. Pneumolysin, an intracellular toxin found in all S. pneumoniae clinical isolates, is an important virulence factor of the pneumococcus that is recognized by TLR4. Although TLR2 is considered the most important receptor for Gram-positive bacteria, TLR2 does not play a decisive role in host defence against S. pneumoniae pneumonia; likely, pneumolysin-induced TLR4 signalling can compensate for TLR2 deficiency during respiratory tract infection with S. pneumoniae. Besides TLR2 and TLR4, TLR9 contributes to an effective host defence against S. pneumoniae in the airways. The importance of TLR signaling for host defence against pneumococcal pneumonia is illustrated by the fact that mice lacking the common TLR adaptor protein MyD88 are highly susceptible to this infection.
Activation of TLRs results in the production of proinflammatory cytokines. There is ample evidence that underlines the importance of tumour necrosis factor (TNF) and interleukin (IL)-1 in host defence in bacterial pneumonia: In a murine S. pneumoniae pneumonia model, treatment with a neutralising anti-TNF mAb strongly impaired antibacterial defence. In addition, IL-1a receptor type I deficient mice infected with S. pneumoniae displayed an increased bacterial outgrowth. Of considerable interest, treating IL-1 receptor deficient mice with a neutralising anti-TNF antibody made them extremely susceptible to pneumococcal pneumonia.
Infection of the lower airways by S. pneumoniae is associated with complex interaction between the pathogen (e.g. cell wall components, pneumolysin) and the host (e.g. TLRs, cytokines). These interactions play a crucial role in the outcome of this clinically important infection.
S428 The role of microbial virulence factors in the pathogenesis of bacterial pneumonia
S. Opal* (Pawtucket, US)
Severe bacterial pneumonia remains uncommon unless specific conditions exist that tip the balance between the host and pathogen in favour of the microorganism. Such conditions include: persons at the extremes of age; exposure to especially virulent organisms; patients with concomitant illness impairing pulmonary clearance mechanisms; and immunocompromised hosts. Pathogens overcome an array of innate and acquired host defences to successfully invade the host. The known virulence traits of three common respiratory pathogens (Streptococcus pneumoniae, Staphylococcus aureus, and Pseudomonas aeruginosa) will be briefly reviewed. The capsular polysaccharide of pneumococci is the major anti-phagocytic virulence trait but many other factors contribute to disease pathogenesis including the critically important exotoxin known as pneumolysin, bacteriocins, adherence factors, choline binding proteins, lipoteichoic acid, iron, manganese and magnesium transporters, pili, competence and biofilm capacity, and virulence genes that promote invasion and impair clearance once the organism has entered the blood stream. S. aureus is notorious for the numerous A/B type toxins, cytotoxins, and superantigens it generates during the course of invasion. Staphylococci deploy a complex series of quorum sensing signals that coordinate adhesin and invasion genes within biofilms or between planktonic organisms and likely contribute to the success of this pathogen. P. aeruginosa produces an array of extracellular exotoxins and cytotoxins delivered by type III secretion systems. These include elastase, phospholipases C, a series of apoptotic and anti-phagocytic exotoxins, along with an alginate capsule and an unusual and variable LPS structure that participate in microbial invasion. The pathogen expresses at least three interacting, quorum sensing systems to coordinate virulence and biofilm formation. A detailed understanding of these virulence factors is now providing therapeutic options to control these respiratory pathogens. Surface expressed and extracellular toxins of pneumococci have been selected as new vaccine targets. Inhibitory peptides and small molecule inhibitors of quorum sensing and biofilm formation are under investigation for staphylococcal and P. aeruginosa infections. These innovative and non-antibiotic treatment strategies are gaining greater importance as progressive antibiotic resistance threatens the management of these severe bacterial infections in the future.
An update on infections you would be surprised to see
S431 Brucellosis
G. Pappas* (Ioannina, GR)
Brucellosis, possibly the commonest zoonotic infection worldwide, has troubled humans since antiquity. Recent years have seen the expansion of the animal reservoir of the disease to a wide spectrum of wildlife species, extending to marine mammals, and the recognition of novel Brucella species. Furthermore, animal and human disease has re-emerged in numerous countries which were brucellosis-free, and currently the most important endemic foci include Near East and Central Asia. Complex socioeconomic and political factors may be incriminated for these alterations in endemicity. The complex mechanisms by which Brucella evades immune response and survives intracellularly are progressively clarified. Novel diagnostic techniques as real time PCR may shed light in the life cycle of Brucella inside the human host; preliminary studies have indicated that the pathogen may persist in latent form for years after apparent clinical cure, in asymptomatic individuals. Treatment principles have not evolved significantly. The expert guidelines issued recently under the name of “Ioannina Recommendations” support the need for a six-week combined treatment that includes traditional antibacterials and is modified accordingly in serious complications as spondylitis and central nervous system involvement. The road to the development of a vaccine for humans seems long though.
S433 Anthrax
M. Doganay* (Kayseri, TR)
Anthrax is ancient diseases and relatively a forgotten disease in western world until 2001 when spores were mailed in USA causing five deaths. Currently, human anthrax is seen most commonly in agricultural regions of the world where anthrax in animals is prevalent, in which countries of Middle East, in Africa, Central Asia and South America. It is also an endemic disease in Turkey.
Human cases may occur in an agricultural or an industrial environment. The infection is an occupational hazard of workers who process hides, hair, bone and bone products, and wool and of veterinarians and agricultural workers who handle infected animals. The main route of transmission is contact with or ingestion of contaminated meal with or inhalation of Bacillus anthracis spores. The aim of the present study was to review human anthrax in Turkey during the last decade.
Papers on anthrax published from Turkey between 1990 and 2007 were collected and reviewed. Most cases were recorded from the central and eastern parts of Turkey. Three of the reports appeared in international journals prior to 1990, 10 reports appeared in the 1990 s, and 24 reports appeared after the anthrax events of 2001 in the USA. These reports included 926 cases, 426 of which could be reviewed: 413 (96.9%) cases of cutaneous anthrax, 8 (1.9%) cases of gastrointestinal anthrax, and 5 (1.2%) cases of anthrax meningitis. Of all the affected patients, 95.2% had contact with contaminated materials. A Nosocomial spread from a 20 day-old baby who developed a cutaneous anthrax lesion on the periumbilical region to two nurses and one cleaner was reported. Most of the patients (88.7%) had received penicillin G. Total mortality was 2.8%.
A total of 138 clinical isolates from human cases were evaluated in five studies. All isolates tested against Penicillin G were susceptible. None of the strains produced beta-lactamase. Doxcycline, tetracycline, erythromycin, aminoglycosides and ciprofloxacin were highly active against all strains.
Anthrax is an endemic disease in Turkey, and acquisition of infection is generally through contact with ill or dying animals or animal products. Sheep and cattle are generally involved. Most clinical disease in humans is cutaneous anthrax, although other clinical forms are seen and have a greater mortality. Penicillin remains the drug of choice in treating the disease. Controlling anthrax in humans depends on controlling the infection in animals.
S434 Leptospirosis
P.A. Tambyah* (Singapore, SG)
Leptospirosis is a very old disease that has been known for more than a hundred years and possibly even longer since the time of Hippocrates. It remains a major cause of illness in many tropical and subtropical countries and thus in travellers. It has also been identified as a zoonosis in Europe and North America. It is a disease that can surprise us because the clinical presentations are not always typical. In recent years, pulmonary and other atypical presentations have been more widely recognised. There is no effective vaccine but chemoprophylaxis is effective in selected populations. Prompt recognition and early institution of appropriate treatment as with most other infectious diseases appear to be critical in ensuring a good outcome for our patients. There are interesting new developments in diagnostics and molecular epidemiology but clearly there are many challenges remaining in this field.
Acinetobacter baumannii antibiotic resistance and virulence genes
O435 Worldwide dissemination of the blaOXA-23 carbapenemase gene associated to different genetic structures in Acinetobacter baumannii
P. Mugnier*, L. Poirel, T. Naas, P. Nordmann (Le Kremlin-Bicêtre, FR)
Objectives: Carbapenem-resistant Acinetobacter baumannii are increasingly reported worldwide. One of the main carbapenem resistance determinant corresponds to the carbapenem-hydrolysing oxacillinase OXA-23. The blaOXA-23 gene had been previously reported to be located in a composite transposon structure Tn2006 (flanked by two copies of insertion sequence ISAba1), or in the transposon structure Tn2007 made of one copy of ISAba4. Our objective was to determine the genetics associated with the blaOXA-23 gene among A. baumannii isolates from worldwide origin.
Methods: Twenty carbapenem-resistant clinical A. baumannii isolates harbouring the blaOXA-23 gene were collected from different sources worldwide. Detection of the blaOXA-23 gene was performed by PCR followed by sequence analysis. The plasmid/chromosomal location of the blaOXA-23 gene was determined by using the I-CeuI technique. Genetic structures surrounding the blaOXA-23 gene in A. baumannii were investigated by cloning and sequencing. Genotyping of the isolates was performed by PFGE and MLST.
Results: The collection was made of isolates recovered from France, Belgium, Vietnam, Saoudi Arabia, New Caledonia, South Africa, Australia, Lybia, Egypt, Kingdom of Bahrain. Among these 20 isolates, 15 clones were identified. Several isolates recovered from very different locations were corresponded to a same clone (i.e. South Africa and New Caledonia). Ten isolates possessed the blaOXA-23 gene on a chromosomal location and the 10 others on a plasmid location. The 10 isolates in which the blaOXA-23 gene was chromosome-borne harboured the entire Tn2006 composite transposon that was always bracketed by a 9-bp long target site duplication (differing among the different clones), as a signature of transposition events. Among the 10 isolates in which the blaOXA-23 gene was plasmid-borne, different structures were identified. One isolate harboured the entire Tn2006 transposon. The blaOXA-23 gene was associated to an upstream-located ISAba1 element (like with Tn2006), but lacked the second downstream-located ISAba1 copy for 6 isolates, and was located inside transposon Tn2007 for 3 isolates.
Conclusion: This study shows that dissemination of blaOXA-23 is related to diverse genetic structures. However, transposon Tn2006 corresponds to the main structure disseminating blaOXA-23 in A. baumannii. The blaOXA-23 gene was either plasmid- or chromosome-located, that may suggest frequent mobilisation events of those structures.
O436 blaOXA-58-carrying Acinetobacter baumannii in Portugal: more ancient and prevalent than initially imagined
S. Quinteira*, F. Grosso, A. Gomes, H. Ramos, L. Peixe (Famalicão, Porto, PT)
Objectives: Although OXA-58 has been reported from many countries, in Portugal only a previous description of a single isolate was made till now. We aimed to analyse the spread of blaOXA-58 among imipenem-resistant A. baumannii (IRAb), within a university hospital, throughout a period of 6 years.
Methods: From 2001–2006, 181 IRAb were collected from several specimens and different wards. Isolates were identified by API32GN and 16SrDNA sequencing. MICs were determined for b-lactam antibiotics by the Etest and for colistin and tigecycline by the agar dilution method. Susceptibility to aminoglycosides and ciprofloxacin was tested by disk diffusion method. Carbapenemase activity was detected by a bioassay. PFGE (ApaI) was done in representative isolates. blaOXA-23-like, blaOXA-24-like, blaOXA-51-like and blaOXA-58 genes were sought by multiplex PCR. The presence of ISAba2 and ISASba3 surrounding the blaOXA-58 gene was investigated. Hybridisation assays were performed using blaOXA-58 probe after ICeuI digestion to ascertain the genetic location of the gene. Sequencing of blaOXA-58 flanking regions was conducted in plamidic extract from a representative strain.
Results: blaOXA-58, found in 22 A. baumannii isolates, all belonging to the same pulsotype, was first recovered in 2001, thus preceding the original description from Poirel et al. (2005). The remaining positive isolates were collected during the 2001–2004 period and were found not to be clonally related to the endemic OXA-40 carrying Iberian clone. This blaOXA-58-producing clone showed resistance to several b-lactams (including imipemem), susceptibility to ceftazidime, netilmicin and minocycline, and variable susceptibility to meropenem, cefepime, and aztreonam.
MICs for colistin and tigecycline ranged from >16 mg/L and from 0.25–4 mg/L, respectively.
All OXA-58-producing isolates presented the ISAba3 downstream of the blaOXA-58 gene. Hybridisation assays revealed a plasmidic location for the blaOXA-58 gene with ca 90Kb. Plasmid sequencing showed an ISAba3-like truncated at the 3’ end upstream of the blaOXA-58 gene, a fact that may explain the observed negative carbapenemase-production bioassay.
Conclusion: blaOXA-58-carrying A. baumannii is, apparently, more ancient than initially imagined. Although undetected from 2004 onwards, the fact that it possessed a non-expressible gene, due to alterations in the promoter region, suggests that this information might have been incorporated from a still unidentified source.
O437 Outbreak of OXA-23-producing carbapenem-resistant Acinetobacter baumannii/calcoaceticus in an intensive care unit in Brazil
C.G. Prates, A.F. Martins, S.V. Superti, L. Lutz, F.S. Lopes, F. Ramos, A.P. Zavascki* (Porto Alegre, BR)
Objective: To describe an outbreak caused by OXA-23-producing Acinetobacter baumannii/calcoaceticus (AB) in an intensive care unit (ICU) from a tertiary-care hospital from Brazil.
Methods: All patients admitted to the 22-bed ICU of Hospital Ernesto Dornelles from March 2006 (detection of the index case) up to November 2008 were assessed. Univariate analysis of potential predictors of 30-day mortality was performed. Variables with a p≤0.10 were included in a Cox regression model. A p≤0.05 was significant.
A sample of 25 CRAB was submitted to PCR for blaoxa-23 gene. Susceptibility tests were performed by disc-diffusion method (CLSI guidelines). MICs for polymyxin B were determined by agar dilution and for tigecycline by E-test in isolates submitted to PCR.
Results: A total of 2879 patients were admitted to ICU during the study period, 60 (2.1%) presented the recovered of at least one CRAB. The incidence rate of CRAB was 3.2 per 1000-patient/day: 1.3 per 1000-patient/day in 2006, 3.2 in 2007 and 5.4 in 2008. The prevalence of CRAB among all AB isolates was 29.0% in 2006, 70.0% in 2007 and 88.1% in 2008. The mean±SD age of patients was 69.4±14.3 years. Twenty-seven (45%) were male. Isolates were recovered from respiratory secretions (33 isolates, 55.0%), blood (11, 18.3%), urine (7, 11.7%), catheter (5, 8.3%) and other secretions (4, 6.7%). Only 24 (40.0%) of 60 patients received appropriate antimicrobial therapy either with polymyxin B (79.2%), ampicillin-sulbactam (12.5%) or tigecycline (8.3%). Overall 30-day mortality of patients with CRAB was 50%. Mortality rates were 3.2 per 1000-patient/day. These rates were significantly higher among patients who have not received appropriate therapy (1.2 per 1000-patient/day) compared with those who have received it (0.3 per 1000-patient/day; p = 0.001; figure 1 ). In the Cox regression model only receiving appropriate treatment (hazard ratio [HR] 3.29; 95% Confidence Interval [CI] 1.35–8.02); p = 0.009) was independently associated with 30-mortality. Positive blood culture for CRAB remained in the final model (HR 1.85; 95% CI 0.86–4.00; p = 0.12). All 25 isolates submitted to PCR were positive for blaoxa-23. All these isolates were susceptible to polymyxin B and tigecycline.
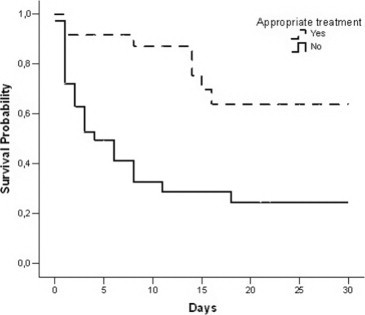
Conclusion: High 30-day mortality occurred in this ICU outbreak. Many patients did not receive appropriate therapy, which significantly increased mortality. Other clinical risk factors for mortality in this outbreak are currently under investigation.
O438 Molecular identification and characterisation of Acinetobacter baumannii in Norwegian strain collections reveal major discrepancies to phenotypic identification and the presence of carbapenemase-producing clonal lineages
N. Karah*, B. Haldorsen, K. Hegstad, A. Sundsfjord, Ø. Samuelsen on behalf of the Norwegian Study Group on Acinetobacter
Objectives: Acinetobacter baumannii is an important opportunistic pathogen that mainly affects critically ill patients in intensive care units. The aim of this project was to analyse two national strain collections of Acinetobacter spp. from Norway with respect to precise species identification of A. baumannii and further characterisation of confirmed A. baumannii isolates with regard to antimicrobial susceptibility, presence of carbapenemases and clonal lineages.
Materials and Methods: A total of 31 multidrug-resistant isolates of Acinetobacter spp. submitted to the Reference Centre year 2003–2008 from various clinical specimens and 118 blood culture isolates of Acinetobacter spp. from all Norwegian clinical laboratories year 2005 to 2007 were included. Identification of A. baumannii was performed by VITEK2, blaOXA-51 PCR, and 16S-23S rRNA intergenic spacer PCR. Sequencing of 16S rRNA and rpoB was used to confirm the results. Susceptibility testing was examined by Etest. The presence of defined blaOXA-enzymes related to carbapenem resistance and epidemic clonal lineages were examined by multiplex PCRs.
Results: In total 100 out of 149 isolates were identified as A. baumannii by VITEK2. However, only 17 isolates were confirmed as A. baumannii by molecular methods. Molecular identification methods showed consistent results with only one exception: one isolate was identified as A. baumannii by the 16S-23S rRNA intergenic spacer PCR and A. radioresistens by sequencing of 16S rRNA/rpoB. Among the 17 isolates identified as A. baumannii, 7 isolates were from the multidrug-resistant strain collection and 10 from the national blood culture collection. Five of the A. baumannii isolates detected were intermediate susceptible or resistant to carbapenems and were PCR-positive for blaOXA-23-like (n = 4) and blaOXA-58-like (n = 1). BlaOXA-24-like was not identified. Six isolates were found to belong to European clones I (n = 3) and II (n = 3).
Conclusion: Automated phenotypic identification of A. baumannii show major discrepancies compared to molecular methods which showed consistent results. A. baumannii represents only 8.5% of the blood culture isolates phenotypically identified as Acinetobacter spp. indicating that other Acinetobacter species are important causes of bacteraemia. The presence of blaOXA-23-like and blaOXA-58-like genes was related to carbapenem resistance and isolates belonging to European clones I and II have emerged in Norway.
O439 Novel genetic context of multiple blaOXA-58-like genes in Acinetobacter genospecies 3
B. Evans*, A. Hamouda, K. Towner, S. Amyes (Edinburgh, Nottingham, UK)
Objectives: The spread of carbapenemase genes within Gram negative bacteria is of great cause for concern. In 2008, the first report of a blaOXA-58 gene outwith Acinetobacter baumannii was reported in Acinetobacter genospecies 3. We had also identified a genospecies 3 isolate encoding a blaOXA-58-like gene, and the aim of this study was to examine the genetic environment of the gene to investigate the mobilisation between species.
Methods: Restriction analysis of rRNA was used to confirm identity to the species level. Susceptibility to imipenem and meropenem was determined through the plate doubling dilution method. Screening by PCR for blaOXA-51-like, blaOXA-23-like, blaOXA-40-like and blaOXA-58-like genes was carried out. Analysis of the genetic environment surrounding the blaOXA-58-like gene was conducted by sequencing inverse PCR products and gene-walking fragments. The structure of the surrounding sequence was confirmed using internal primers, which were also used to screen other blaOXA-58-like positive isolates in our collection.
Results: Restriction analysis confirmed the isolate belonged to Acinetobacter genospecies 3. The isolate showed reduced susceptibility to imipenem and meropenem with MICs of 2 mg/L for both antibiotics. The isolate was negative for a blaOXA-51-like, blaOXA-23-like or blaOXA-40-like gene, but positive for a blaOXA-58-like gene. Analysis of the genetic environment of the blaOXA-58-like gene revealed the gene was within a novel genetic structure. Upstream of the blaOXA-58-like gene was the left-hand end of an ISAba3 element, interrupted by an ISAba125 element. The elements contained putative promoter sequences. Downstream was an araC1 and a lysE gene, followed by a sequence similar to the Re27 element described previously. Following this was a complex region containing the right-hand end of an ISAba3 tnpA gene, interrupted by an incomplete tnpA gene with 99% similarity to ISAba3, itself interrupted by an ISAba125 sequence. This region was followed by a second blaOXA-58-like gene. All other blaOXA-58-like positive isolates in our collection were negative for ISAba125 upstream of blaOXA-58.
Conclusion: This study is the first to report multiple copies of a blaOXA-58-like gene in an Acinetobacter genospecies 3 isolate, and has identified a novel structure containing two blaOXA-58-like genes and two ISAba125 sequences. The ISAba125 elements may be responsible for the duplication of the blaOXA-58-like gene.
O440 Three major A. baumannii clones account for all carbapenem-resistant strains
M.L. Mezzatesta*, M. D'Andrea, R. Migliavacca, T. Giani, F. Gona, G. Marchese, E. Nucleo, L. Pagani, G. Rossolini, S. Stefani (Catania, Siena, Pavia, IT)
Objective: Acinetobacter baumannii is a significant nosocomial pathogen that has the potential to spread among hospitalised patients especially in intensive care units. Clinical isolates of A. baumannii are often characterised by a multiple antimicrobial resistance phenotype, including major therapeutic options such as carbapenems.
To trace the diffusion of carbapenem-resistant A. baumannii in Italy, a Sequence Typing (ST) scheme was compared with typing results generated by PFGE.
Methods: 119 A. baumannii isolates were collected during 2004–2005 in 8 Italian regions. All strains were non susceptible to carbapenems and antibiotic resistance determinants were investigated by PCR. PFGE was routinely performed and the MLST scheme used was based on fragments of the six genes as published in the MLST Pasteur web site http://www.pasteur.fr/recherche/genopole/PF8/mlst/, while primers used for the amplification of rpoB were designed using Vector NTI on the basis of the published sequence (CU459141).
Representatives of major European clones I (RUH875) and II (RUH134) were used as controls.
Results: Our results confirm the particular propensity of A. baumannii for nosocomial cross-transmission in vast geographical areas.
All isolates, belonging to three MDR clones, were characterised by the presence of blaOXA-58 determinant. Six isolates, belonging to PFGE type C, were also positive for the blaOXA-23 allele. No isolates were positive for the blaOXA-24 allele.
Conclusions: PFGE and MLST possess the same discriminatory power, the same reproducibility, and are epidemiologically concordant in defining the three clones circulating in Italy, two of them belonging to the 2 pan European clones; the third clone was isolated only in 1 centre.
| N. strains | PFGE |
ST | Allelic profile |
OXAs content | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| type | subtype | cpn60 | fusA | gltA | pyrG | recA | rplB | rpoB | |||
| 109 | A | 3 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | OXA51-like, 58 |
| 4 | B | 0 | 1 | 1 | 1 | 1 | 1 | 5 | 1 | 1 | OXA51-like, 58 |
| 6 | C | 2 | 20 | 3 | 1 | 1 | 1 | 5 | 1 | 1 | OXA51-like, 58, 23 |
| RUH 134 | A | − | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | − |
| RUH 875 | B | − | 1 | 1 | 1 | 1 | 1 | 5 | 1 | 1 | − |
O441 Detection of extended-spectrum beta-lactamase type PER-1 in Acinetobacter baumannii species isolated from bloodstream infections and investigation of clonal relationship
M. Cosar, I. Tuncer, U. Arslan*, A. Mansur, B. Otlu, R. Durmaz, D. Findik (Konya, Malatya, TR)
Objective: Acinetobacter baumannii is an important nosocomial pathogen with wide intrinsic resistance. However, due to the dissemination of the acquired resistance mechanisms; such as extended-spectrum beta-lactamase (ESBL) and metallo betalactamase (MBL) production, multidrug resistant strains have been isolated more often. PER-1 was first detected in Turkey and was found to be widespread among Acinetobacter spp. and P. aeruginosa. Since then, PER-1 has been discovered in other countries, and most recently found in northern Italy and in Korea. In this study, the presence of PER-1 type ESBL was investigated in caftazidime resistant A. baumannii strains isolated from bloodstream infections by PCR and also the clonal relatedness of the isolates were investigated by Random Amplified Polymorphic DNA (RAPD) and Pulsed Field Gel Electrophoresis (PFGE) in all PER-1 producing A. baumannii strains.
Methods: A. baumannii strains isolated from bloodstream infections was included in this study. The isolates were identified as A. baumannii by conventional methods and Phoenix 100 BD automated System system (Becton Dickinson Diagnostic Systems, Sparks). Ceftazidime resistance was determined by E-test. PER-1 genes were screened by PCR. The clonal relationship of PER producing A. baumannii isolates were analyzed by RAPD and PFGE. Data analyses were performed using Gel Compar II (Applied Maths, Sint-Martens-Latem, Belgium).
Results: Of the 100 A. baumannii isolates; 78 (78%) were determined as ceftazidime-resistant by E-test. Among the 78 ceftazidime-resistant A. baumannii isolates the PER-1 gene was identified in 18 (23%). The similarity of the bands were calculated according to “dice smilarity coefficients” and all PER-1 positive isolates were found as clonally related.
Conclusion: In our study the prevalence of PER-1 was lower than the previous studies. But the presence of high ceftazidime resistance rates among these isolates may indicate the presence of other beta-lactamases. DNA analysis by PFGE and RAPD revealed an outbreak caused by a unique clone. Detection of clonal related isolates among different services may be because of the treatment of these patients at the same services before and this may explain the spread of PER-1 positive strains.
O442 Resistance genomic islands related to AbaR1 are common in Acinetobacter baumannii strains belonging to European clone I
L. Krizova*, M. Maixnerova, L. Dijkshoorn, A. Nemec (Prague, CZ; Leiden, NL)
Objective: Acinetobacter baumannii strains belonging to European (EU) clone I are commonly resistant to multiple antimicrobial agents. A number of resistance genes were recently detected on an 86-kb genomic resistance island (AbaR1) inserted in the ATPase gene of EU clone I strain AYE. The aim of this study was to assess the presence of AbaR1-related structures in epidemiologically unrelated strains of EU clone I.
Methods: The study set included 25 multi-drug resistant (MDR) strains of EU clone I collected in 19 European countries in 1978–2004 and 10 genotypically unique, fully susceptible strains. Using PCR, all strains were investigated for the presence of the ATPase gene and for nine genes found to be associated with AbaR1. Furthermore, the strains were tested for the disruption of the ATPase gene using PCR primers directed against the 3’ and 5’ ends of this gene. Strains with the disrupted gene were investigated for the presence and structure of the ATPase gene-AbaR1 connecting regions using PCR mapping and RFLP. PCR primers were derived from the known sequence of strain AYE.
Results: All strains were positive for the ATPase gene. The 10 susceptible strains had an intact ATPase gene whereas all MDR strains failed to produce the expected amplicon in the ATPase disruption test. All EU clone I strains yielded positive results for the ATPase gene-AbaR1 connecting regions, the structure of which corresponded to those of AYE. These findings suggest the presence of ATPase integrated elements in clone I strains, the integration of which had invariably taken place at the same locus site. None of the AbaR1-associated resistance genes were found in any of the susceptible strains. In contrast, the MDR strains harboured the following AbaR1-associated genes (% positive strains): aacC1 (21), aadA1 (21), aadB (4), aphA1 (21) strA (3), merA (20), tetA (18), cat (23), the gene encoding heavy metal detoxification protein (25). Individual MDR strains carried from one to nine AbaR1-associated genes in 11 different combinations. There was a good correlation between the content of resistance genes and resistance phenotypes.
Conclusion: Genetic structures related to AbaR1 are common in strains belonging to EU clone I. The heterogeneity of resistance patterns in this clone is likely to result from the variations in the content of AbaR1-related structures.
Supported by grant 310/08/1747 of the Grant Agency of the Czech Republic.
O443 Mutation frequency of rifampicin resistance in Acinetobacter baumannii clinical isolates
P. Komp Lindgren*, H. Seifert, O. Cars (Uppsala, SE; Cologne, DE)
Objectives: To study the differences in mutation frequency and evaluate the possible correlations between drug resistance development and mutation rate in Acinetobacter baumannii (AB).
Methods: The mutation frequency (MF) of rifampicin (RIF) resistance was used as a surrogate measure of differences in mutation rate and for detection of the presence of mutator phenotype. The MF of RIF resistance was measured in 100 clinical isolates collected from different AB infections over a 20 year period in Europe and USA and two reference strains (AB ATCC 19606 and 17978). MF of RIF in AB isolates was compared with E. coli control strains with altered mutation rates. 10–20 cultures of each isolate were grown over night and plated onto RIF containing Mueller-Hinton agar plates and non RIF containing plates to determine the MF of rifampicin resistance. After 24 hour incubation colonies were counted and the frequency was calculated. The MF was compared to each individual strain's resistance profile (resistant vs multidrug resistant, MDR) and infection specific history (sporadic vs outbreak isolate).
Results: The MF of RIF resistance ranged between ˜2.2×10−10 to 7.8×10−8. None of the isolates displayed any MF near the mismatch-(mutS, 3.0 × 10−6) or dam-mutant (3.9 × 10−7) of E. coli. Still, many of the AB isolates, 66 of 102, displayed a MF of rifampicin lower (< 10 9) then wild type E. coli. There were no significant mean differences between sporadic (1.3 × 10−8) and outbreak (1.2×10−8) isolates. In the comparison of resistance profile and MF, the MIC values of 5 different antibiotic classes were used. The isolates were classified as resistant (resistant to <2 antibiotics) and MDR (resistant to ≥3) by the MIC values according to EUCAST breakpoints. The mean MF of resistant versus MDR isolates were 8.8×10−9 and 1.2×10−8, respectively.
Conclusion: Although no A. baumannii isolates displayed a strong mutator phenotype, the diverse mutation frequencies reflect the past evolutionary history of these isolates. The existence of a significant number of possible ‘weak-mutators’ (≤10 times increased MF) among clinical isolates presents a hidden potential for the rapid evolution of resistant isolates. It was previously shown in E. coli that a slightly increased mutation rate (4–20 fold) can drive the evolution of antibiotic resistance. Our finding that MDR A. baumannii isolates had increased mutation rates can have an impact on future development of resistance in these isolates.
O444 Genome comparison of Acinetobacter baumannii: evaluation of drug resistance, adherence, haemolysis and other potential virulence factors
F. Imperi, M. Iacono, L. Antunes, L. Villa, P. Visca, G. De Bellis, A. Cassone, A. Carattoli* (Rome, Segrate, IT)
Objectives: despite the importance of Acinetobacter baumannii as emerging pathogen worldwide, studies on the mechanisms underlying its pathogenesis are lacking. Multidrug resistant strains are emerging throughout many geographic areas and two pan-epidemic European clones (I and II) have been documented, endowed with a broad range of antibiotic resistance. In this study, the genome sequences of the multidrug resistant A. baumannii ACICU (European clone II; Iacono et al. AAC 2008) and AYE (European clone I, Vallenet et al. PLOS One 2008) strains were compared with the genome of the antibiotic susceptible, not pathogenic SDF strain, and with that one of the reference ATCC17978 strain (Smith et al. Genes Dev 2007) with the aim of identifying genomic regions implied in pathogenesis and drug resistance.
Methods: protein similarities were searched by the BLASTp algorithm. Pathogenicity studies were performed using the Galleria mellonella model of infection. Haemolysis was evaluated on defibrinated horse blood.
Results: in this study, we used larvae of the insect G. mellonella (greater wax moth) as infection model to compare the virulence of the A. baumannii strains ATCC17978, AYE, ACICU and SDF. The 50% lethal dose (LD50) was comparable for AYE and ACICU, while it was ca. 10- and 100-fold higher when larvae were infected with ATCC17978 and SDF, respectively. Thus, the SDF genome was used as reference genome to identify functions acquired by pathogenic strains with a possible role in antibiotic resistance and pathogenicity. Sixty-two clusters, corresponding to almost 870 CDSs, were identified in the ACICU and AYE genomes (and partially in ATCC17978) that were absent in SDF. These clusters encode: (i) resistance genes and transporters plausibly involved in drug efflux (30 transporters of the MFS, DMT, ABC, RND, MOP and ACR3 families were unique of drug resistant strains and absent in the susceptible SDF strain); (ii) pili and fimbriae systems related to biofilm formation and motility; (iii) haemolysin- and haemagglutinin-related proteins differently distributed among the four genomes, (iv) iron uptake and other metabolic genes.
Conclusion: Genome comparison identified unique features of A. baumannii epidemic clones and provided novel insights into the genetic basis of multidrug resistance and pathogenesis in this species. This study may contribute to understand the concept of infection, invasiveness and colonisation in the emergent pathogen A. baumannii.
Hard to swallow – emerging and re-emerging issues in food-borne infection (Symposium arranged with EFWISG)
S460 MRSA in food products: cause for concern or case for complacency?
J. Kluytmans* (Breda, NL)
In 2003 a new MRSA strain was found in The Netherlands that could not be typed with Sma1 Pulsed Field Gel Electrophoresis due to the presence of a novel methylation enzyme. The initial observations on this strain were related to persons, who had contact with pigs. Using MLST analysis it was shown that all non-typable strains belonged to one clonal compex, ST-398. Subsequently a study was performed which confirmed the association of ST-398 in humans and a reservoir in pigs and veal calves. Meanwhile, this clone has been found in horses and chicken as well. In geographic areas with a high density of pig- or cattle-farming the prevalence of MRSA has increased dramatically since an active screening was recommended by the Dutch Working Party on Infection Control (WIP) in June 2006 (WWW.WIP.NL). At present, approximatelty 30% of ll new cases of MRSA in The Netherlands are ST-398. Some case reports show that this strain can cause serious infections. On the other hand there are indications that ST-398 is less virulent and less transmissible among humans than other MRSA strains. At this time ST-398 has been found all over the world, nearly always in relation to animal husbandry.
The findings above prompted investigations into the presence of MRSA in food. A large survey in The Netherlands showed that 145 out of 1293 pieces of retail meat harboured MRSA (11.2%). The quantity of MRSA per piece of meat was low. This raises concern over the potential spread of MRSA or the resistance genes into the general population. The presence of low amounts of ST-398 is not considered to be a risk if the meat is prepared properly. There is a theoratical risk for tansmission related to handling of meat. At present there are no indications that the presence of ST-398 in food is causing further spread into the community.
Interventions in the use of antimicrobials: do they affect antimicrobial resistance?
O463 Reduction of the use of macrolides does not decrease macrolide resistance in Streptococcus pneumoniae
M. Bergman*, S.T. Nyberg, P. Huovinen, A.J. Hakanen and The Finnish Study Group for Antimicrobial Resistance (FiRe Network)
Objectives: Macrolide resistance in Streptococcus pneumoniae and marolide usage in Finland was evaluated.
Methods: 29,535 S. pneumoniae isolates were tested during 2001 – 2007 for macrolide resistance in the laboratories of 20 central hospital districts, covering the whole of Finland. The susceptibility testing was performed according to the guidelines of CLSI. Data concerning outpatient macrolide sales were obtained from the National Agency of Medicines. The macrolide (erythromycin) resistance trends were statistically evaluated, as well as the consumption figures of azithromycin, roxithromycin, clarithromycin, and all macrolides pooled. The effect of age was also evaluated.
Results: Results show that in spite of a notable decrease in total macrolide usage from 2.06 to 1.43 Defined Daily Doses/1000 inhabitants/day (p = 0.008), macrolide resistance in S. pneumoniae increased significantly (p < 0.001). The result was similar when different macrolide compounds were analysed separately. The increase in resistance could especially be seen in the age group of children under 5 years old. In 2007, macrolide resistance in this age group was 29.2%, whereas patients over 5 years old had a resistance rate of only 17.2%.
Conclusion: In conclusion, despite a reduction in macrolide usage, macrolide resistance in S. pneumoniae in Finland did not decrease. Instead, macrolide resistance increased statistically significantly during the study period. The increase was the most striking among isolates from children under 5 years old. This implies that antimicrobial usage is not the only factor that affects resistance.
O464 Effect of reduced use of quinolones on the observed resistance rates in E. coli
I. Willemsen*, B. Cooper, C. van Buitenen, M. Winter, J. Kluytmans (Breda, Amsterdam, NL; London, UK)
Objectives: To determine the effects of multiple interventions that reduced the use of Quinolones, on the observed resistance of E. coli in a teaching hospital.
Methods: During a prospective study, from 2005 through 2007, 4 interventions to improve the use of quinolones (QUIN) were executed. First, a switch from intravenous- to oral medication (01–2006); second, education programs for interns/residents and physicians and the release of a new antimicrobial formulary (05–2006); third, a restriction note was printed on all laboratory rapports (10–2006) and fourth, active monitoring and giving feedback on prescriptions (01–2007). Susceptibility patterns for E. coli including ciprofloxacin, cefuroxim, ceftazidim, co-trimoxazole and tobramycin from hospitalised patients were analyzed starting in 2004. Statistical analyses were performed using segmented Poisson regression models to look at effect of interventions on resistance (both sudden stepwise changes and changes in trends). Bayesian model averaging was used to account for model uncertainty.
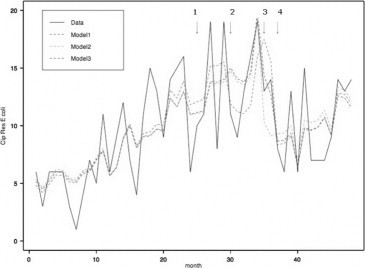
Results: Before the start of the interventions the resistance rate was increasing by an average of 2.6% per year. The interventions resulted in a significant reduction of QUIN use from on average 550 Prescribed Daily Doses to 350 PDD per month. In the best fitting Poisson model for the resistance data, a significant stepwise decrease was found to be associated with interventions 2 and 4. However, there was substantial uncertainty in the model choice, and after accounting for this there was no conclusive evidence in support of any particular intervention, although there was evidence that at least one of the interventions was associated with the observed reduction in resistance. There were no stepwise decreases or decreasing trends in resistance rates to other antimicrobials during the study period.
Conclusions: This study found that targeted interventions that reduce the use of QUIN were associated with a decrease of the QUIN resistance rate in E. coli.
O465 Antibiotic therapy and resistance in Germany: influence and intervention
E. Velasco*, W. Espelage, I. Noll, A. Barger, T. Eckmanns (Berlin, DE)
Objectives: Growing populations of older and immunocompromised patients, changes in epidemiology and unchecked use of antibiotics can led to a rise in consumption as well as resistance to certain treatments. Medical doctors (MDs) often have an important role alongside contributing factors. We conducted a national survey of MDs in Germany on their behaviours and expectations for intervention. We aimed to assess MD behaviours with and influences on antibiotic prescribing and the potential for related interventions that address antibiotic resistance.
Methods: A representative sample comprised 10,610 MDs with differing practice specialties, from both stationary and ambulatory settings (respectively: 36% and 0% internists, 0% and 54% general practitioners, 32% and 11% surgery, 3% and 4% ear/nose/throat, 10% and 10% paediatrics, 5% and 3% urology, 9% and 13% gynaecology, 2% and 4% dermatology, 3% and <1% other) in 15 federal states. We developed study questions to capture baseline information on MDs and their practice with antibiotics. Questions also focused on selected influences that may affect behaviour in practice. Other questions solicited opinions about interventions that may improve practice. Mailed questionnaires were distributed to participants via state medical associations.
Results: Among survey respondents (n = 3,613; response rate = 34%), 66% reported that they prescribe antibiotics daily, and 90% indicated they do so at least weekly. Of all surveyed MDs, 60% reported that they think their own prescribing practice has an influence on antibiotic resistance in their region. Of all MDs, 83% found it “important” to continually improve use of antibiotics through industry independent experts providing consultation, audits and feedback. Of all MDs, 96% found it “important” to have provision of regional coverage of antibiotic resistance with appropriate feedback for practicing MDs, and 82% found it “important” to have provision of antibiotic regulations of prescriptions with appropriate feedback for practicing MDs. (Results in Table 1 .)
Table 1.
Selected questions from survey
| Question | n = | Responsesa |
||
|---|---|---|---|---|
| % Stationary | % Ambulatory | % Combined | ||
| Do you use some form of guidelines for antibiotic | 3442 | 84 yes | 78 yes | 81 yes |
| therapy? | 13 no | 16 no | 15 no | |
| How often do you consult other colleagues about | 3547 | 49 daily | 5 daily | 26 daily |
| starting a patient on antibiotic therapy? | 2 never | 30 never | 16 never | |
| Do you think your own prescribing practice has an | 3529 | 70 yes | 51 yes | 60 yes |
| influence on antibiotic resistance in your region? | 21 no | 36 no | 29 no | |
| Do you think antibiotic resistance is a relevant | 3527 | 88 yes | 67 yes | 77 yes |
| problem in your work position? | 11 no | 29 no | 21 no | |
| “I would rather prescribe antibiotics than not when a patient wants to work” | 1839 | − | 18 agree | − |
| 35 disagree | ||||
| 25 disagree strongly | ||||
| “I would rather prescribe antibiotics than not when treating immunosuppressed patients” | 1702 | 25 agree strongly | − | − |
| 60 agree | ||||
| 3 disagree | ||||
| Do you find guidelines for diagnostics and therapy for antibiotic infections for MDs in ambulatory settings important? | 1844 | − | 48 “very important” | − |
| 92 “important” | ||||
| Do you find clinic-internal guidelines for diagnostics and therapy for antibiotic infections with consideration of local resistance data important? | 1690 | 65 “very important” | − | − |
| 95 “important” | ||||
Not all results shown and remaining percentages are as follows: A closed three category scale was used for options “yes”, “no”, “do not know”. A closed four category scale was used with options “very important”, “important”, “less important” and “not important”. A closed five category scale was used for options “daily”, “weekly”, “monthly”, “seldom” and “never”. A closed five category scale was used for options “strongly agree”, “agree”, “neutral”, “disagree” and “strongly disagree”.
Conclusion: Many MDs prescribe antibiotics often and believe their practice may have an effect on antibiotic resistance. Results indicate that MDs value information, interventions and surveillance in order to support responsible use of antibiotics. There is an ongoing effort in Germany to address these findings at the national level e.g. by establishing a surveillance system for antibiotic resistance and antibiotic usage.
O466 Two years after introduction of ertapenem in the antibiotic formulary of an intensive therapy unit in a large teaching hospital: effect on antibiotic resistance patterns of Pseudomonas species and Enterobacteriaceae
P. Lal*, T. Neal (Liverpool, UK)
Objectives: Ertapenem, a parenteral carbapenem licensed for once daily use in April 2002 in Europe is increasingly being used as monotherapy for treatment of serious infection caused by Enterobacteriaceae. In two international randomised trials its use was not associated with increase in bowel colonisation of extended-spectrum β-lactamase/Amp C β-lactamase (Amp C) producing Enterobacteriacae or imipenem-resistant Pseudomonas species, a major issue in infection control. Ertapenem was introduced in our intensive therapy unit in January 2007. We carried out this study to determine changes in antibiotic resistance patterns amongst Pseudomonas species and Enterobacteriaceae between the periods before [January 2005 to December 2006] and after [January 2007 to December 2008] its introduction.
Methods: The antimicrobial susceptibility data was collected from an online database maintained in the department and percentage resistance (% resistance) for all antimicrobials was compared between the two periods separately for Pseudomonas species and Enterobacteriaceae. The p values were calculated using Fisher's exact test.
Results: The % resistance amongst Pseudomonas species in the two periods was: amikacin (3%, 0.6% *), ciprofloxacin (23%, 22%), ceftazidime (6%,7%), gentamicin (4%, 0.8%*), piperacillin/tazobactam (4%, 3%), carbapenems (19%, 20%) respectively. That for Enterobacteriaceae was: co-amoxiclav (44%, 39%), amoxicillin (85%, 89%), 2nd & 3rd generation cephalosporins combined (40%, 38%), cefpodoxime (46%, 42%), ceftazidime (30%, 32%), cefoxitin (42%, 36%*), ciprofloxacin (32%, 34%), gentamicin (15%, 11.5%*), amikacin (1.9%, 1.7%), piperacillin/tazobactam (23%, 22%), trimethoprim (45%,43%) and carbapenems (0.6%, 2.2%*) respectively. (* denotes significant p values <0.05, see Table ).
Table.
The percentage antibiotic resistance amongst Pseudomonas species and Enterobacteriaceae between the periods 01/05–12/06 and 01/07–12/08
| Antimicrobials | % Resistance |
p value (Fisher's exact test) | |
|---|---|---|---|
| 01/05–12/06 | 01/07–12/08 | ||
| Enterobacteriaceae | |||
| Co-amoxiclav | 44 | 39 | 0.018 |
| Amoxicillin | 85 | 89 | 0.740 |
| 2nd &3rd cepahalosporins (total) | 40 | 38 | 0.07 |
| Cefpodoxime | 46 | 42 | 0.14 |
| Ceftazidime | 30 | 32 | 0.26 |
| Cefoxitin | 42 | 36 | 0.004 |
| Ciprofloxacin | 32 | 34 | 0.18 |
| Gentamicin | 15 | 11.5 | 0.0094 |
| Amikacin | 1.9 | 1.7 | 0.10 |
| Trimethoprim | 45 | 43 | 0.31 |
| Piperacillin/tazobactam | 23 | 22 | 0.64 |
| Carbapenems (imipenem, meropenem) | 0.6 | 2.2 | 0.0042 |
| Pseudomonas species | |||
| Amikacin | 3 | 0.6 | 0.02 |
| Ciprofloxacin | 23 | 22 | 0.74 |
| Ceftazidime | 6 | 7 | 0.77 |
| Gentamicin | 4 | 0.8 | 0.005 |
| Piperacillin/tazobactam | 4 | 3 | 0.43 |
| Carbapenems (imipenem, meropenem) | 18.7 | 19.7 | 0.26 |
Conclusions: This study shows significant increases in resistance of Enterobacteriaceae to carbapenems in the period after introduction of ertapenem. However there was no significant change in resistance of Pseudomonas species to carbapenems. The resistance to co-amoxiclav and cefoxitin decreased significantly in Enterobacteriaceae in the latter period suggesting a reduction in Amp C producing organisms. The aminoglycoside resistance decreased significantly in the latter period in both Enterobacteriaceae and Pseudomonas species. These findings which are important for treatment and infection control demonstrate the need for resistance surveillance after introduction of a new antimicrobial to detect any collateral changes.
O467 Survey of antibiotic resistance in Streptococcus pneumoniae collected in Belgium during winter 2008. Follow-up of resistance since 1995 and possible effect of antibiotic campaigns
R.L.M. Vanhoof*, E. Van Bossuyt, S. De Craeye, J. Van Eldere, J. Verhaegen, L. Kaufman on behalf of the Belgian SP Study Group
Objectives: S. pneumoniae remains an important pathogen with high rates of antibiotic non-susceptibility being reported worldwide. There remains a need for continuous national surveillance of resistance. Here, we compare the 2008 data with those obtained since 1995.
Methods: Strains were collected by 15 centres. MIC to Penicillin (PN), Amoxicillin (AM), Cefuroxime (CR), Cefotaxime (CT), Ciprofloxacin (CI), Levofloxacin (LV), Moxifloxacin (MO), Erythromycin (ER), Telithromycin (TL) and Tetracycline (TT) was determined by the NCCLS microdilution test. Data on antibiotic use were obtained from ESAC.
Results: In the 2008 survey, 448 strains were tested. Non-susceptibility rates (%I+R) were as follows: PN: 11.6, AM: 0, CR: 9.2, CT: 2.0, CI: 5.1, LV: 0.7, MO: 0.4, ER: 29.7, TL: 0 and TT: 21.9. ER-TT (12.7%) was the commonest IR profile. MDR was 22.5%. In the period 1995–2008, 3262 strains were collected. PN-IR increased significantly from 12.5 (1995) to 21.0 (2001) and decreased to 11.6 in 2008. AM, CR and CT had a similar evolution. AM peaked at 3.1 in 2003 and decreased to 0 in 2008. CP-IR decreased significantly from 1999 (15.1) to 2008 (5.1). ER-NS (21.6–37.7) increased over the years and TT-IR (22.8–38.5) stayed high. IR for LV, MO and TL were always low (0.5–3.3; 0–0.6; 0–1 resp.). B-lactam distributions were bimodal. PN MIC50 shifted to the right from 1995 (0.008) to 2003 (0.06) and returned to 0.015 (2008). FQs had one-modal distributions; MIC50 remained stable (CP, LV: 0.5–1, MO 0.06). IR for PN, ER and TT were always higher in children (CH) than in adults (AD). Significant differences were found for PN (1995), ER (1997, 2004, 2006, 2007, 2008), TT (2004, 2006). Generally, CP-IR was higher in AD than in CH. IR was lower in the North (N) than in the South (S). Significant differences: PN (2005, 2006), ER (2003, 2004, 2005), TT (2005). Both N and S knew a deceasing IR tendency: PN = N (12.1–8.1), S (18.8–13.2); CP = N (11.6–5.9), S (18.9–5.9); TT = N (27.4–21.5), S (35.9–23.5). ER increased in the N (20.9–29.7). Total outpatient antibiotic use (DID) decreased from 26.2 (1999) to 22.7 (2004) and increased to 24.2 (2006). DID for PN and FQ increased, MLS stabilised and TT decreased.
Conclusions: Since 2001–2003 an IR decrease was noted for PN, CP and TT. ER-IR increased further over the years. The decrease paralleled the start of public campaigns on antibiotic use. IR rates remain higher in CH than in AD. The N/S difference became less marked.
Paediatric infections: new bugs and emerging roles for the older ones
O468 Parachlamydia and Rhabdochlamydia in respiratory secretions of premature newborns: prevalence and clinical impact
F. Lamoth*, A. Schneider, S. Aeby, K. Jaton, B. Vaudaux, G. Greub (Lausanne, CH)
Objectives: Parachlamydia acanthamoebae is a new recognized member of the order Chlamydiales. Growing evidences suggest that this bacteria may have a pathogenic role in humans causing respiratory diseases. It has also been recently identified as an agent of bovine abortion and may be a cause of miscarriage in women. In contrast, little is known about the pathogenic role of Rhabdochlamydia crassificans, another related Chlamydiales. Molecular diagnostic tools are useful to detect these obligate intracellular bacteria because of their inability to grow on conventional culture media. The aim of this work was (i) to develop a real-time PCR for the diagnosis of Rhabdochlamydia infection and (ii) to study respiratory secretions of newborns for the presence of Parachlamydia and Rhabdochlamydia DNA.
Methods: A new quantitative real-time TaqMan PCR (q-PCR) to be used on ABI Prism 7900 was developed. The q-PCR was then blindly applied to 41 consecutive respiratory samples (endotracheal or nasopharyngeal secretions) taken from 29 critically-ill newborns admitted in the neonatology ward of our university hospital. These samples were also tested using a previously developed Parachlamydia-specific PCR.
Results: Most newborns (28/29) were premature (median gestational age: 28.6 weeks; range: 24.6–41.2). Initial respiratory distress syndrome was present in 86% of them. Positive PCR results were obtained in 12/29 (41%) patients (8 Parachlamydia, 3 Rhabdochlamydia, 1 both species) at a median of 17.5 days (range: 2–230) after birth. When compared to the control group (17 patients with negative PCR), these 12 newborns had a significantly worse primary adaptation and a higher incidence of resuscitation maneuvers at birth (Table). Duration of noninvasive mechanical ventilation and stay in neonatology ward were also significantly longer. A fatal issue was observed in 3 infected cases, as compared to no death in controls (p = 0.06). Gestational age at birth as well as the incidence of pulmonary or systemic infections did not differ between cases and controls.
Conclusion: A high prevalence of Parachlamydia and Rhabdochlamydia DNA was observed in respiratory secretions of premature critically-ill newborns. The presence of DNA of these microorganisms was associated with a worse primary adaptation, a more severe respiratory distress syndrome and a trend towards a higher mortality. Their pathogenic role should be further investigated.
Table.
Newborns with positive PCR for Parachlamydia and/or Rhabdochlamydia in respiratory secretions compared with control group
| Positive results (n = 12) | Negative results (n = 17) | P value | |
|---|---|---|---|
| Primary adaptation (Apgar score) | |||
| First score (1 min)* | 2.5 (0–7) | 8 (2–9) | 0.002 |
| Sum of 3 scores (1, 5, 10 min)* | 18.5 (8–27) | 27 (17–29) | 0.002 |
| Cardiac resuscitation (first 48 h)** | 6 (50) | 0 (0) | 0.002 |
| Invasive mechanical ventilation (first 48 h)** | 11 (92) | 8 (47) | 0.019 |
median (range)
total number (percent).
O469 Superior detection of Kingella kingae and Staphylococcus aureus in paediatric osteoarticular infections using molecular assays
S. Juretschko*, T. Beavers-May, C. Hemphill, J. Romero, S. Stovall (Little Rock, US)
Objectives: Delayed diagnosis and treatment may worsen the outcome of paediatric osteoarticular infections. Epidemiological data show Staphylococcus aureus as the predominant pathogen. Recently increased prevalence of Kingella kingae infections has been reported in young children.
The genus Kingella consists of 3 species, K. kingae, K. oralis and K. denitrificans. All are Gram negative, sometimes difficult to stain, rod shaped bacteria that are normal respiratory and genitourinary flora. They are slow-growing and fastidious. Although improved recovery was shown when using Fan or PEDs-F blood culture bottles, the majority of these infections remain undetected, especially in pre-treated patients. We report the use of real time polymerase chain reaction (rt-PCR) assays for detection of K. kingae and S. aureus in paediatric osteoarticular infections.
Methods: 116 synovial fluid samples from 97 patients, 1 month and 17 years of age, were collected over 19 months (03/2006 to 10/2007). The samples were from 54 knees, 39 hips, 9 ankles, 6 elbows, 4 shoulders, 2 wrists and 2 femur abscesses. After automated DNA/RNA extraction, specimens were subjected to 4 hour pathogen-specific rt-PCR. Samples were inoculated onto sheep blood and chocolate agar as well as a Peds-F bottle. Final species identification and antimicrobial susceptibilities were determined by Phoenix (TM).
Results: 45 patients (56 specimens) had positive culture and/or rt-PCR, resulting in an overall positivity rate of 46%. S. aureus was the predominant pathogen accounting for 31 specimens of 23 patients (12 MRSA, 11 MSSA) and. 37% of positive specimens (18 patients) were due to K. kingae (n = 21). Among children 0–2 years (n = 35), K. kingae was the predominant pathogen accounting for 16 positive patients (46%), followed by MSSA in 4 patients (11%). The positivity rate for this age group was 57%. Only 2 children >2 years (5 and 9 years) were positive for K. kingae. MRSA was the predominant pathogen in 6–12 year olds, and MSSA was evenly distributed among children 3–17 years old. Culture detected only 5 of 21 specimens positive for K. kingae and 25 of 31 S. aureus. 4 other pathogens were detected by culture only.
Conclusion: The use of these molecular assays enhances detection of organisms, especially for K. kingae (19% vs. 5% for culture). Additionally, faster identification (TAT 4 hrs) allows for rapid targeted therapy. This improvement in TAT could lead to shorter hospital stays in about 54% of cases.
O470 Population dynamics and geographical diversity of Moraxella catarrhalis in the Generation R study
S.J.C. Verhaegh*, M.L. Snippe, H.A. Moll, A. van Belkum, J.P. Hays (Rotterdam, NL)
Objectives: Moraxella catarrhalis is often found in the nasopharynx of children having the capacity to cause respiratory infections. Several virulence-associated genes have been identified in M. catarrhalis, though relatively little is known about the frequency of these genes. In this study, genotyping, virulence gene screening, and virulence gene PCR-RFLP studies were used to investigate isolate variation in chronologically distinct, and serial, isolates of M. catarrhalis colonising young children.
Methods: Nasopharyngeal swabs were taken from children enrolled in the Generation R focus cohort group, a study based in Rotterdam, The Netherlands, comprising 1,079 children, born between February 2003 and August 2005. Nasopharyngeal swabs were taken at 1.5, 6 and 14 months of age. Of the 732 M. catarrhalis isolates cultured, 48 single and 82 serial isolates were further investigated for genotype (PFGE or MLST), virulence gene frequency (PCR screening), and virulence gene diversity (PCR-RFLP).
Results: Genotyping revealed a high degree of diversity, indicative of a panmictic bacterial population. Further, there was no association between genotype and colonisation frequency, or year of isolation. PCR screening for virulence genes revealed an incidence of 98% for uspA1, 81% for hag, 82% for uspA2 and 18% for uspA2H. No significant difference was observed in the prevalence of virulence-associated genes between isolates originating from children who were colonised only once or children colonised on all 3 occasions (P = 1). PCR-RFLP analysis of uspA1, hag and uspA2 showed many gene variants, with no association between PCR-RFLP patterns and colonisation frequency, or year of isolation.
Conclusion: Even in relatively localised geographical settings, the genotypic diversity of M. catarrhalis isolates colonising children is large, with no yearly pattern of genotype predominance. Children serially colonised with M. catarrhalis isolates appear to clear a particular genotype only to become subsequently colonised with a different genotype. The incidence of virulence genes in this relatively localised study group is remarkably similar to that reported in global M. catarrhalis isolates, possibly indicating that similar selection pressure exists for M. catarrhalis at both the local and global level. Virulence gene variation appears to be high, even in this relatively restricted geographical group. These results could have consequences for vaccines designed against virulence genes.
O471 Epidemiology of cytomegalovirus in pregnancy and risk evaluation for delivering a child with congenital CMV infection
A. Naessens*, I. Foulon, A. Casteels, W. Foulon (Brussels, BE)
Objectives: To evaluate the epidemiology of cytomegalovirus in pregnancy and to evaluate the risk for delivering a child with congenital CMV (cCMV).
Methods: Between 1996–2006, 11825 unselected mother-infant pairs were included. In the mother a serological screening was performed consisting in the detection of CMV IgG and IgM antibodies at the first prenatal visit and at birth. In the neonate CMV urine culture was performed to diagnose congenital infection. When a pregnant woman was found to have a second trimester spontaneous abortion or a death in utero, an investigation for possible congenital CMV infection was carried out.
Results: Serological screening at the first prenatal visit showed no immunity in 4701 women, evidence of past infection (IgG positive IgM negative) in 6877 women (58.2%) and in 250 women (2.0%) both IgG and IgM antibodies were detected. After investigation of stored and follow up samples from these 250 patients, 14 could be classified as having a primary CMV infection during pregnancy, 99 patients had previous immunity before the current pregnancy and from 137 patients the type of the maternal CMV infection could not be determined. Follow-up serology of the 4701 women without immunity revealed a seroconversion in 58 of them (1.2%).
A total of 61 (0.52%) congenital infections (cCMV) were diagnosed. The incidence of the cCMV among the different groups of women are summarised in the table.
Conclusion: cCMV infection occurs in 0.52% of our population of pregnant women. cCMV was considered to be due to a primary maternal CMV infection in 54% of the infants; 33% due to a recurrent maternal CMV infection and in 13% the type of maternal infection could not be determined.
The risk for a seronegative pregnant woman of acquiring CMV during pregnancy is 1.2%. The transmission risk after a maternal primary infection is 45%. Women with prior immunity have a very low risk (0.20%) for cCMV, this risk increases to 3% when IgM are find in women with know prior immunity. The risk for women with undetermined infectious status in early pregnancy to give birth to a congenitally infected neonate is 5.8%.
| Pregnant women | N | N cCMV | risk of cCMV |
|---|---|---|---|
| IgG pos/IgM neg. at first prenatal visit | 6877 | 17 | 0.20% |
| Seroconversion during pregnancy | 58 | 26 | 45% |
| IgM positive at first prenatal visit | 250 | 18 | 7.2% |
| Primary infection | 14 | 7 | 50% |
| Prior immunity | 99 | 3 | 3% |
| Undetermined maternal infection | 137 | 8 | 5.8% |
| Total population | 11825 | 61 | 0.52% |
O472 Rotavirus gastroenteritis in Norway: analysis of prospective surveillance and hospital registry data
E. Flem*, K. Vainio, H. Døllner, C. Midgaard, F.J. Bosse, A.G. Wesenberg Rognlien, A. Rojahn, S. Nordbo, G. Størvold, G. Njølstad, K.O. Wathne, K. Konsmo, P. Aavitsland (Oslo, Trondheim, Bergen, NO)
Objectives: We examined the epidemiology and burden of rotavirus gastroenteritis in Norway to inform the national decision on introducing new rotavirus vaccines into routine immunisation.
Methods: We reviewed the national hospital registry data on children <5 years of age hospitalised with acute gastroenteritis (AGE) during January 1995–December 2004. We also conducted sentinel rotavirus surveillance among children <5 years of age admitted with AGE to three large hospitals during 2006–2008, and examined the numbers of rotavirus-positive tests reported to the national laboratory surveillance system in 1995–2004.
Results: During 1995–2004, 14973 gastroenteritis hospitalisations were reported for an annual rate of 4.9 (95% confidence interval (CI) 4.6–5.3) hospitalisations per 1000 children. The proportion of AGE hospitalisations with rotavirus-specific code on the discharge records was 14%. However, sentinel surveillance determined that 63% (95% CI 57.4–68.3) of these hospitalisations were associated with rotavirus, yielding an estimated annual incidence of 3 (95% CI 2.6–3.5) rotavirus hospitalisations per 1000 children, corresponding to ˜906 (range 735–1092) hospitalisations annually. Children aged 6–23 months accounted for 61% of all confirmed rotavirus cases. Rotavirus hospitalisations demonstrated distinct spring seasonality. No rotavirus-associated deaths were reported during sentinel surveillance or in the hospital registry data.
Conclusions: Estimated two thirds of all gastroenteritis hospitalisations in children <5 years of age in Norway are attributable to rotavirus. This report provides the first data on rotavirus epidemiology and disease burden in Norway. Further studies are needed to assess the economic impact of rotavirus disease and the cost-effectiveness of vaccination to inform decisions on introduction of rotavirus vaccines into the national program of childhood immunisation.
Pseudomonas aeruginosa and its relatives
S473 Dynamics of antibiotic resistance and virulence in Pseudomonas aeruginosa
T. Köhler* (Geneva, CH)
Pseudomonas aeruginosa may colonise the lungs of cystic fibrosis patients over years but may also cause acute infections in mechanically ventilated patients and immuno-compromised hosts within a matter of days. Despite aggressive antibiotic treatments the organism is rarely eradicated. Instead P. aeruginosa adapts to its host environment by developing resistance mechanisms and changing its lifestyle and virulence properties. Focusing on mechanically ventilated patients, we will detail the dynamics of resistance emergence and persistence of P. aeruginosa lung populations during antibiotic therapy. We further discuss how P. aeruginosa populations evolve naturally in the absence of any antimicrobial treatment within the lungs of intubated patients by changing their virulence properties. The relevance of these findings both with respect to concepts of social evolution and the development of novel anti-infective strategies will be highlighted.
S474 Drug efflux in intrinsic and acquired resistance in P. aeruginosa
C. Llanes, K. Jeannot, D. Hocquet, L. Vettoretti, P. Plésiat* (Besançon, FR)
The genome of P. aeruginosa encodes many potential efflux systems. However, only a few of them appear to play a significant role in antibiotic resistance. In this respect, the Mex (for Multiple efflux) systems are of particular interest because of their ability to extrude a wide range of antimicrobials. These polyspecific machineries result from the assembly of (i) a drug/proton antiporter, (ii) a periplasmic adaptor protein, and (iii) an outer membrane gated channel. It is now well established that the constitutive expression of the tripartite pump MexAB-OprM provides P. aeruginosa with a relatively high intrinsic resistance to quinolones, β-lactams (except imipenem), tetracyclines, macrolides, chloramphenicol, trimethoprim, and novobiocin. This protective mechanism is potentiated by the poor permeability of the outer membrane and activity of another pump, MexXY/OprM, whose expression is induced by substrates targeting the ribosome (e.g., tetracyclines, macrolides, aminoglycosides). Accumulating reports indicate that multidrug resistant mutants up-regulating one or both of these systems are quite common in the clinical setting. Such mutants, which are readily selected by sub-optimal treatments with fluoroquinolones, β-lactams or aminoglycosides, tend to accumulate various resistance mechanisms without loosing the wildtype pathogenicity of P. aeruginosa. Whether the low resistance levels (MIC × 2- to 8-fold) conferred by efflux may promote second-step mutants with altered drug targets (GyrA, GyrB, ParC) or derepressed AmpC β-lactamase has not been confirmed in vitro. In the specific context of cystic fibrosis (CF), a recent study from our laboratory showed that the MexXY/OprM pump can be responsible for much higher resistance levels to aminoglycosides (64- to 128-fold). This increased efficacy of the system partially results from adaptive mutations in the mexY gene. In contrast, subpopulations deficient in MexAB-OprM tend to emerge during long-term colonisation of CF airways. While easily selected in vitro on selective media, mutants overexpressing other Mex systems (MexCD-OprJ, MexEF-OprN, MexGHI-OpmD, MexJK/OprM, MexVW/OprM) have been rarely described in CF and non-CF patients. Some data support the notion that up-regulation of MexCD-OprJ or MexEF-OprN might be detrimental to the virulence of P. aeruginosa. In conclusion, therapeutic strategies based on efflux inhibitors should target the MexAB-OprM and the MexXY/OprM systems in priority.
European aspects of malaria
S478 Rapid diagnostic tests for malaria: twenty years to convince …
B. Genton* (Lausanne, CH)
Prompt diagnosis and treatment of malaria are critical factors in reducing morbidity and mortality. Microscopy has long been the gold standard for malaria diagnosis, but the newer rapid diagnostic tests (RDTs) now offer considerable advantages, especially so in endemic countries. After close to twenty years of development and operational research, the diagnostic performance of RDTs is now established in all settings. Meta-analyses have clearly demonstrated equivalence of RDTs over expert microscopy to detect parasites, and clear superiority over routine microscopy. Actually, one of the major reasons that have delayed successful implementation of RDT in endemic areas was the use of poor quality microscopy that has impeded reliable measurement of sensitivity and specificity and undermined confidence of health workers in RDTs. Other factors were poor product performance, inadequate methods to determine the quality of products and a lack of emphasis and capacity to deal with these issues. For the potential of RDTs to be realised, it is crucial that high-quality products that perform reliably and accurately under field conditions are made available and that quality insurance is performed on all steps of the procedure. In achieving this goal, the shift from symptom-based diagnosis to parasite-based management of malaria can bring significant improvement for the management of fever in endemic areas.
For travelers returning in temperate climates with fever, RDTs have also the potential to improve diagnostic procedures, especially so in hospitals where reliable microscopy is not available out of hours. In patients with no danger sign or significant thrombopenia, a negative RDT is sufficient to exclude malaria and allows waiting 12–24 hours for performing or reading the microscopy slide. RDTs should be repeated every 12–24 hours for three consecutive days if fever persists and in the absence of alternative diagnosis.
RDTs represent a revolution in the fight against malaria and will tremendously help to manage appropriately patients with fever, especially so when malaria is declining and hence other causes of fever increasing. The ambitious deployment that is foreseen in the coming years in Africa through large grants from the Global Fund should contribute to achieving the millennium goals.
S479 Clinical aspects of imported malaria
C. Hatz* (Basel, CH)
Fever is the key symptom of malaria among returning travellers (97%). Headache, chills, myalgia, sweating and lack of a focus are frequently recorded, but non-specific. Nausea and vomiting are often seen in children. The differential diagnosis of other infections, mainly of viral origin, is further difficult because (dry) cough and (mild) diarrhoea are often present. Laboratory findings (thrombocytopenia, low or normal leucocyte count) can be helpful in the assessment of mild to moderate malaria.
Clinical signs and symptoms, e.g. fever, may be mitigated in semiimmune patients (visiting friends and relatives, foreign visitors) seen in non-endemic countries who represent the majority of cases diagnosed in industrialised countries. Caution is warranted in assessing such patients as many of them may no longer be exposed to malaria in their countries of origin, thus no longer partially protected and also at risk of suffering from severe complications.
Up to 10% of all imported malaria cases may be severe, presenting with jaundice, impaired consciousness to coma, acute renal failure, and, in the course of events, acute respiratory failure. Delay in diagnosis and start of treatment is partly responsible for fatality rates of 1% and more in some countries.
If you don't look for them, you won't find them: anaerobes revisited
S481 Anaerobic microbiota of the mouth – friend or foe?
E. Könönen* (Turku, FI)
Anaerobes form a major part of the commensal microbiota in the digestive tract where they constitute an integral component of the function on mucosal surfaces. In the mouth, teeth create a unique, non-shedding environment for bacteria to attach and to form biofilms. There is an age-related succession order of species in bacterial colonisation of the mouth, and once established, individual anaerobic species tend to remain as members of the oral microbiota. The age-related pattern of the colonisation of anaerobic bacteria is partly connected with the development (or loss) of the dentition. Interactions between different bacteria residing in the same microenvironment influence the composition of the microbiota – or the development of pathologic conditions. Although commensal bacteria are regarded beneficial to the host, some anaerobic members of the oral microbiota contain characteristics potentially detrimental for the health status of an individual. Molecular means of characterisation have resulted in increased knowledge about the “normal” microbiota of the mouth and in detection of new species and genera as well as phylotypes, which can be associated with infectious situations in the mouth. Oral infections are multifactorial and polymicrobial in nature, and their aetiologic organisms originate mainly from the oral resident microbiota. The involvement of anaerobes is most obvious in infections of root canals, periodontal tissues, and tissues surrounding erupting wisdom teeth where typical anaerobic findings are Gram-negative rods. In addition, Gram-positive anaerobic cocci and non-spore-forming Gram-positive anaerobic rods are common in odontogenic infections. On some occasions, anaerobes of localised dentoalveolar infections can spread to adjacent tissues and even to the bloodstream, resulting in severe complications in extraoral sites. Interestingly, a relatively limited number of anaerobic species are involved in clinically severe infections, however, microbial findings seem to vary depending on geography. Concomitant with the increase in the number of immunosuppressed patients, the number of opportunistic infections caused by commensal anaerobes may increase. Identification to the species level will help to establish associations between individual anaerobic species and specific disease states.
S482 The hidden villains in severe diabetic foot infections
D.M. Citron* (Culver City, US)
Studies on the bacteriology of diabetic foot infections (DFI) have yielded varied and often contradictory results. The role of anaerobes is particularly unclear, often because the type and severity of the infection is poorly defined, recent antibiotic therapy is unknown, and specimen collection and culture techniques are inadequate. When optimal collection, transport, and culture techniques are used, multiple organisms including aerobes and anaerobes are usually recovered from severe DFI. Interactions within these polymicrobial soups lead to production of virulence factors, such as haemolysins, proteases, collagenases, and short chain fatty acids, which promote inflammation, impede healing and contribute to the chronicity of the infection. To better define the bacteriology of diabetic foot infections, we analyzed our data from a large prospective U.S. multicentre trial of patients with moderate to severe infection that required initial parenteral antibiotic therapy and used optimal post-debridement sample collection, transport and culture procedures. Of the 427 culture-positive specimens (of 454 total), only 16.2% were pure cultures while 30.4% yielded 5 or more organisms. A total of 462 anaerobes (range 0–9, average 2.3, per specimen) were recovered from 49% of patients, with Gram-positive cocci (GPC) accounting for 45.5% of all anaerobic strains. Finegoldia magna was the predominant species, recovered from 24.4% of patients (99/406) with Prevotella spp. the second most common (12.3% of patients), followed closely by Porphyromonas spp. (10.3%) and the Bacteroides fragilis group (10.2%). B. fragilis was the predominant species (40.4%, 19 of 47) within the group. A greater proportion of anaerobes were cultured from tissue than from ‘deep swab’ specimens (5.5 vs. 2.1), especially for Porphyromonas spp. (70% vs. 23%), and Prevotella spp. (72% vs. 23%). GPC and B. fragilis group species appeared more evenly distributed among the 4 specimen types. GPC were present in 37.4% of patients, but are often under-reported in studies, possibly because of the selective media used. LKV agar grows B. fragilis group and Prevotella spp, but not Gram-positive anaerobes or Porphyromonas spp., which could explain why many studies find the B. fragilis group to be the predominant anaerobe. Clostridia were present in 4.9% of our patients. If you look closely, the hidden villains are lurking just beneath the inflamed surface and are not so difficult to find.
Shifting from cultures to direct detection of bacterial components
S485 Is culture still the gold standard, really?
M. Struelens* (Brussels, BE)
Tremendous technological advances are made in culture-independent methods of detection and identification of human bacterial pathogens, such as PCR or hybridisation of their genomic DNA. Yet, time honoured Pastorian bacterial culture in liquid and solid nutritive media still remains the gold standard for the laboratory diagnosis of a majority of bacterial infections. This unusual robustness of a 19th century technology stems from its unmatched operational characteristics:
-
1.
broad range of detected agents, depending on adequate combination of media/incubation conditions;
-
2.
unlimited source of clonal population for individual isolate, allowing versatile characterisation of antibiotic susceptibility and/or pathogenic factor production and/or epidemiological subtyping;
-
3.
possibility of storage/bio-banking of cells for complementary clinical testing, research and diseases surveillance collections;
-
4.
proof of pathogenic role of agent at the time of viable cell isolation from the site of infection, in contrast to false-positive results with molecular tests (tissue translocation or persistence of bacterial DNA, soluble antigen, …).
Major drawbacks of bacteriological culture include long turn-around time, cost and labour/skill intensity. These are partly alleviated by new technologies, including automated processing, physical/chemical growth detection and rapid molecular fingerprinting (MALDI-TOF, Raman spectrometry, 16S rDNA SNP detection). It is likely that the next decade will see a complete redefinition of the place of direct detection methods and culture-based confirmation methods in clinical bacteriology, enabling a rejuvenation rather than elimination of culture as a daily diagnostic tool.
S486 Detection of nucleic acids, is there a future after PCR?
J. Schrenzel* (Geneva, CH)
The advent of real-time PCR revealed instrumental to the successful implementation of molecular methods in routine clinical microbiology laboratories. Automated nucleic extraction platforms can now be coupled to robotic handling for large-scale detection and quantification purposes, mostly in virology. I will review here the attempts of implementing home-brew and commercial nucleic-acid based detection methods directly from blood samples and highlight hopes and pitfalls. I will then expand on two promising nucleic acid amplification methods: LAMP (loop mediated isothermal amplification) and a protein-free method called DNAzyme. These isothermal amplification methods share several strengths: robustness across highly diversified physico-chemical conditions, versatility in assay development and minimal requirements (if any) for sample preparation. They will definitely compete against current real-time PCR assays and might become a novel standard, due to lower costs and improved performances.
S487 Single-cell identification by improved fluorescence in situ hybridisation techniques
R.I. Amann*, B.M. Fuchs (Bremen, DE)
The ribosomal RNA (rRNA) approach to microbial evolution and ecology has become an integral part of microbiology. Rapidly growing databases exist that encompass besides the 16S rRNA sequences of almost all validly described Bacteria and Archaea also numerous 16S rRNA sequences of so far uncultivated microbes, directly retrieved from the environment by PCR or metagenomics. Based on the patchy evolutionary conservation of rRNA genes oligonucleotide probes can be designed in a directed way with specificities ranging from species up to large evolutionary entities like phyla or even domains.
When such probes are labeled with fluorescent dyes or the enzyme horseradish peroxidase they can be used to identify single microbial cells by fluorescence in situ hybridisation (FISH) directly in complex environmental samples. An update on recent applications and methodological improvements will be given which includes the identification of small bacterial cells by catalyzed reporter deposition (CARD)-FISH. With optimised methods and proper controls FISH yields exact cell numbers and spatial distributions for defined bacterial populations also in highly complex mixed microbial communities.
S488 Protein pattern matching – identification of microorganisms using matrix-assisted laser desorption/ionisation time-of-flight (MALDI-TOF) mass spectrometry
A. Mellmann* (Münster, DE)
Quick and reliable species identification of microorganisms is of great importance in medical microbiology. Several bacterial and fungal species can be identified only using laborious and time-consuming methods. Furthermore, in many cases misidentification occurs due to e.g. limited biochemical reactivity, different morphotypes or limited information in reference panels. In this talk, matrix-assisted laser desorption/ionisation time-of-flight (MALDI-TOF) mass spectrometry will be presented as a method for species identification. This technology applies protein pattern matching based on mass spectrometry. During the identification process, a mass pattern is generated for each organism. The subsequent comparison of this pattern with a database comprising reference patterns derived from well-characterised reference strains leads to species identification. As examples, the identification of various nonfermenting bacterial strains isolated from clinical specimens in comparison to partial 16S rDNA sequencing will be shown. Moreover, speed, accuracy in comparison to other methods, and inter- and intra-laboratory reproducibility of MALDI-TOF MS-based species identification will be discussed.
Streptococci: mechanisms of resistance and epidemiology
O489 Trends in invasive Streptococcus pneumoniae serogroup 1 sequence types in Belgium
T. Goegebuer, K. Van Pelt, J. Verhaegen, J. Van Eldere* (Leuven, BE)
Objectives: S. pneumoniae serogroup 1 (SG1) isolates frequently cause invasive pneumococcal disease, particularly in children. From 2003 onwards a marked increase in SG1 isolates was observed; overall prevalence increased from 8.2% (1998–2002) to 13.6% (2003–2006). We determined the sequence types (ST) in SG1 isolates in order to better understand trends in SG1 resistance and spread.
Methods: As national reference centre, we receive all invasive isolates from more than 100 of 182 laboratories in Belgium. 124 randomly chosen SG1 isolates from all ages from 1998 to 2006 were analysed via multi-locus sequence typing (MLST) as described by Enright & Spratt (Microbiol. 1998; 144: 3049–60). We also included data on strain characteristics and patient characteristics.
Results: 10 different sequence types (ST) were identified: ST350 (n = 66), ST306 (n = 24), ST304 (n = 13), ST227 (n = 10), ST228 (n = 5), ST2915 (n = 2), ST305 (n = 2), ST612 (n = 1), and ST217 (n = 1). All ST are known to circulate in Europe, US and Canada, but not in South-America or Asia. During 1998–2002 the predominant ST's were ST350 (46%), ST227 (17%) and ST304 (15%). For 2003–2006, ST350 (59%) and ST306 (33%) were most prevalent.
The prevalence of ST350 has stabilised around 60% of SG1 isolates since 2000. It was observed in all Belgian provinces, but it was significantly more prevalent in the Northern part of Belgium. Only 22% of ST350 strains were susceptible to macrolides, tetracycline and b-lactams. Resistance to macrolide and/or tetracycline increased from 33% in 2000 to 86% in 2006. This increase was almost entirely due to multi-drug resistance (macrolides plus tetracycline).
ST306 is known to be highly invasive and was not present in Belgium before 2001, but increased to 30% of SG1 isolates in 2006. All ST306 isolates have remained drug-susceptible.
ST227 is the most common ST in England, the US and Canada and was present during the period 1998–2002, but wasn't observed after 2003.
Conclusion: The increase in SG1 invasive S. pneumoniae in the period 1998–2006 was predominantly linked to the increase in ST350 and ST306. While ST350 was already present in 1998, ST306 emerged only recently. Resistance development was very prominent in ST350 but was not yet observed in ST306.
O490 Clonal diversity of penicillin non-susceptible Streptococcus pneumoniae isolates in Moscow, Russia
T. Savinova, E. Ilina, A. Borovskaya, S. Sidorenko* (Moscow, RU)
Objectives: Russia is in a favourable position regarding prevalence of penicillin-resistance among Streptococcus pneumoniae, not more than 15–20% of isolates demonstrated reduced susceptibility during last 10 years. Since epidemiological studies of pneumococcal resistance have revealed the worldwide dissemination of epidemic clones, the aim of the present study was to evaluate genetic heterogeneity of Russian isolates.
Methods: Thirty nine penicillin non-susceptible isolates of S. pneumoniae collected in 2005 – 2007 during nationwide survey were included in the study. Multilocus sequence typing (MLST) was performed as described by Enright, M. C., et al. The sequence types (STs) were obtained by using the MLST database (http://www.mlst.net). Clonal relationships in the strain collection were visualised using eBURST (http://eburst.mlst.net). Groups of isolates sharing six of seven alleles were assigned to clonal complexes (CCs).
Results: A total 17 different ST and 16 different CC were detected. Only five CC were represented by multiple isolates. CC81 was predominant and represented by 12 isolates (30.8%), all of them were ST81. These isolates demonstrated similar multidrug resistance phenotypes; besides non-susceptibility to penicillin all of them were resistant to macrolides, tetracycline and chloramphenicol, six isolates were also resistant to levofloxacin. Four isolates belongs to CC271 (three ST236 and one ST651) and demonstrated different resistance phenotypes. Three isolates belongs to CC315 (all ST315) and demonstrated resistance to macrolides and chloramphenicol. Each of CC280 (all ST239) and CC414 (all ST1500) were represented by two isolates and were susceptible to all antibiotics except penicillin. 16 different ST (five of them new) were represented by a single isolate
Conclusion: Penicillin non-susceptible S. pneumoniae in Russia are represented by multidrug resistant CC81 isolates related to international Spain23F-1 clone and heterogeneous group of isolates of different CC with low level of associated resistance to other antimicrobials.
O491 Macrolide resistance of invasive Streptococcus pneumoniae in Slovenia, 1998 – 2007
T. Kastrin*, M. Paragi, J. Kolman, M. Cizman, M. Bezenšek, M. Culafic, V. Mioc (Ljubljana, SI)
Objectives: The surveillance of invasive pneumococcal diseases is a part of slovene National Public Health program since 1993. In the present study we investigated the genetic basis of macrolide resistance.
Methods: Isolates of Streptococcus pneumoniae (SP), isolated from sterile body sites were nationally collected. All isolates were typed with capsular swelling reaction. Antibiotic susceptibility was determined by disc diffusion test and E-test following the CLSI recommendations. The presence of erm(B), mef(E), mef(A) and erm(TR) genes were determined by PCR. Clonality of the selected isolates was studied by PFGE of SmaI-digested bacterial DNA.
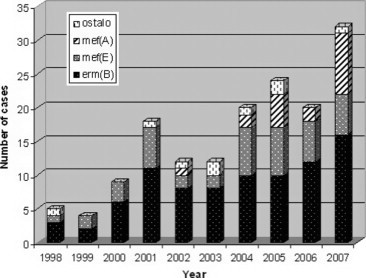
Results: A total of 1448 invasive isolates of SP were collected in Slovenia from 1998 to 2007. Of these, 156 isolates (10.8%) were resistant to erithromycin. We observed a rise of macrolide resistance in invasive S. pneumoniae from 4.7% in 1998 to 16.8% in 2007. The most prevalent determinant of macrolide resistance in the observed period was the erm(B) gene (55%), followed by the mef(E) (27%) and mef(A) gene (12%). The erm(TR) gene was not found. The most prevalent serotypes among macrolide resistant isolates were 14 (35%), 6B (18%), 19F (9%), 9V (9%), 19A (8%) and 6A (4%). Multiple antimicrobial resistance was demonstrated in 53.8% of macrolide-resistant clinical isolates. The strains carrying the erm(B) gene were multiple resistant in 72.1% of cases, whereas the strains with the mef(E) gene were associated with multiple resistance in 52.3% of cases. Strains with mef(A) gene were susceptible to all other antibiotics. During the observed period the number of isolates with erm(B) gene was constantly increasing, on the other hand the number of isolates with mef(E) gene was constant for the last four years. The first isolate with mef(A) was demonstrated in 2002 and in 2007 they were more common than isolates with mef(E) gene. We demonstrated that all except two isolates with mef(A) gene were genetically closely related and belonged to international clone England14–9. In conclusion, the main reason for the increase of serotype 14, mef(A) positive isolates was the spread of the England14–9 clonal cluster.
Conclusions: Due to the increase of the incidence and resistance of pneumococcal isolates the epidemiological surveillance, sero- and molecular typing of invasive pneumococci is an important issue of Public Health institutions.
O492 Resistance among invasive Streptococcus pyogenes in France, 2006–2008
A. Ergani*, A. Doloy, C. Plainvert, G. Collobert, C. Poyart, A. Bouvet (Paris, FR)
Objectives: To investigate the MLSB and tetracycline resistance and the emm gene distribution among the invasive Streptococcus pyogenes (GAS) strains.
Methods: Between January 2006 and December 2008, a total of 991 strains responsible for invasive infections for adult patients were sent to the French National Reference Center for Streptococci to be studied. Antibiotic susceptibility testing was done by disk diffusion method according to the CA-SFM guidelines. MICs were determined by E-test method. Streptococcal emm sequence was done according to the CDC protocol. Detection of macrolide and tetracycline resistance genes: erm(B), erm(TR), mef(A), tet(M), tet(O), tet(K), and tet(L) was performed by PCR.
Results: Among the 991 Streptococcus pyogenes invasive strains; more than ten different emm-types were identified. The most frequent emm sequence types were emm1, emm28 and emm89. A total of 80 strains (8%) were resistant to erythromycin. Erythromycin resistance prevalence had decreased during the three years period (12.2%-2006, 7.6%-2007, 5.5%-2008). 69 had an MLSB constitutive (65 strains) or inducible (4 strains) phenotype due to erm(B) or erm(TR) resistance gene. 11 with the M phenotype and mef(A) gene were susceptible to clindamycin. Among the 132 (13.3%) tetracycline resistant isolates tet(M), tet(O) and tet(L) genes were detected in 86, 27 and 19 strains, respectively. Tetracycline resistance prevalence had also decreased during the three years period (16.8%-2006, 14%-2007, 8.7%-2008).
Conclusion: Most of the invasive French GAS isolates remained erythromycin and tetracycline susceptiple during three years. Nontheless, the resistance rates have had the tendency to decrease slightly. Taking into account the resistance trends helps to guide the therapy for penicillin-allergic patients.
O493 Molecular characterisation of macrolide resistance in Streptococcus dysgalactiae subsp. equisimilis isolates from Portugal
M.D. Pinho*, J. Melo-Cristino, M. Ramirez on behalf of the Portuguese Group for the Study of Streptococcal Infections
Objectives: During a survey on antimicrobial susceptibility in beta-haemolytic group C and G streptococci (GCGS) from Portugal, a macrolide resistance rate higher than previously reported in other European countries was found (22%) among S. dysgalactiae subsp. equisimilis isolates. To gain further insights into the resistance mechanisms involved and the clonal structure of the resistant population, we undertook the phenotypic and molecular characterisation of macrolide resistant S. dysgalactiae subsp. equisimilis isolates and compared it with the susceptible population.
Methods: Antimicrobial susceptibility testing and macrolide resistance phenotype were determined by disk diffusion. All the macrolide-resistant isolates were further characterised by MIC testing and genotype determination by PCR. A combination of emm typing and pulsed-field gel electrophoresis (PFGE) was used to type the population and the Simpson's index of diversity (SID) with 95% confidence intervals was calculated as previously described.
Results: A total of 69 isolates were resistant to erythromycin (MIC range, 4 to >256 ug/ml). The vast majority of isolates presented a MLSB phenotype (n = 64) and carried the erm(A) gene (n = 55), while the mef-encoded M-phenotype was expressed by only 5 isolates. Among resistant isolates, 13 distinct emm types were found distributed by 10 PFGE clusters that overlapped with the main clusters detected in the susceptible population. The emm types stG480, stG6, stG485 and stG2078 accounted for approximately two thirds of the resistant isolates. PFGE did not always separate neither macrolide-resistant from susceptible isolates nor erm(B) and mef(A) from the prevailing erm(A) isolates. The SIDs of emm and PFGE calculated for resistant isolates were not statistical different from the overall population. The two most prominent MLS resistant lineages were one with stG480/erm(A) isolates (n = 8) and stG485/mef(A) (n = 3), and another including stG2078/erm(A) (n = 8).
Conclusion: Although most of the resistant isolates presented a MLSB phenotype and carried an erm(A) gene, molecular typing revealed extensive diversity in both emm types and PFGE clones. Macrolide resistance had a polyclonal origin, with resistance emerging among most susceptible clones. Monitoring of macrolide resistance patterns in S. dysgalactiae subsp. equisimilis is essential as this pathogen is increasingly recognised as an important human pathogen.
O494 Penicillin resistance caused by dissemination of serotype 14 – clone Spain9V ST156 in the vaccine era
A.S. Simões*, R. Sá-Leão, S. Nunes, N. Frazão, A. Tavares, H. de Lencastre (Oeiras, PT)
While performing pneumococcal nasopharyngeal colonisation surveillance studies among children attending day care centres (DCC) in Portugal, we observed that the rate of strains with penicillin MIC ≥2 ug/mL more than tripled from 1.8% in 2006 to 6% in 2007 (p = 0.002). The aim of this study was to characterise the 20 isolates recovered in 2007 which had a MIC to penicillin ≥ 2 ug/mL.
Methods: Pneumococci were isolated and identified on the basis of selective growth on gentamycin blood agar plates, optochin susceptibility, colony morphology, and alfa-haemolysis. Susceptibility to antimicrobials agents was performed according to the CLSI recommendations and definitions. Strains were serotyped by the Quellung reaction and/or multiplex PCR using specific primers for each serotype. Pulsed-Field Gel Electrophoresis (PFGE), after restriction of the total DNA with SmaI, was performed to compare genetic backgrounds.
Results: Sixteen of the 20 isolates belonged to serotype 14, three were serotype 19A and one was of serotype 15A. Strains of serotype 14 were also resistant to sulfamethoxazole-trimethoprim and belonged to a single PFGE cluster identified as clone Spain9V ST156. The penicillin resistant serotype 14 strains were isolated in two DCC, from nine children vaccinated with the 7-valent pneumococcal conjugate vaccine (PCV7), four non-vaccinated children and three children with unknown vaccination status. Five of these carriers had received antibiotics recently. In these two DCC the overall proportion of children vaccinated with PCV7 was 64%; 27% of the children had received antibiotics within the previous month and 16% had received three or more courses of antibiotics in the last six months.
Conclusions: Since the introduction of the PCV7 in Portugal, in June 2001, the proportion of penicillin resistant pneumococci recovered from colonisation has been stable (c.a. 2%). The sudden increase in the levels of penicillin resistance observed in the 2007 surveillance study was found to be largely due to the dissemination of clone Spain9V ST156 serotype 14 variant in two DCC with high consumption of antibiotics. The observations suggest a combination of high antibiotic selective pressure and transmission rates resulting in an outbreak-like situation with a penicillin resistant vaccine type clone being disseminated among children in day care despite use of PCV7.
O495 Inducibility of PatA/PatB efflux pumps by fluoroquinolones in Streptococcus pneumoniae
F. El Garch, A. Lismond, F. Van Bambeke*, P.M. Tulkens (Brussels, BE)
Background: Beside target mutation, active efflux is another common resistance mechanism to fluoroquinolones (FQ) in S. pneumoniae. Two main efflux systems have been described so far, namely PmrA (member of the MFS superfamily) and the two ABC transporters PatA/PatB. We have studied the inducibility of pmrA, patA and patB genes expression when bacteria are exposed to subinhibitory concentrations of FQ.
Methods: We used a wild-type sensitive strain (ATCC49619), two clinical strains resistant to FQ (SP13 and SP295), and two efflux mutants (SP334 and SP335; selected in vitro after exposure to ciprofloxacin [JAC 2007, 60:965–972]). MIC were determined according to CLSI. Induction was obtained by growing bacteria in Todd-Hewitt broth added by half the MIC of each FQ (CIP, NOR, LVX, MXF, GMF) for 4 h at 37°C in 5% CO2 atmosphere. Expression levels of pmrA, patA and patB genes were determined by real-time PCR. Reversibility of induction was tested by re-cultivating bacteria for 4 h in drug-free medium.
Results: Antimicrobial susceptibilities for CIP and MXF and gene expression at basal level and after exposure to these FQ are shown in the Table. At the basal level, the 4 resistant strains harboured efflux mechanisms (MIC of NOR [not shown] and CIP reduced of at least 2 dilutions by reserpine) that did not affect MXF, LVX and GMF. PmrA gene was not or only modestly overexpressed in all strains, with no overexpression after induction. In contrast, PatA/B genes were markedly overexpressed in the 4 resistant strains and were further induced to higher levels after exposure to CIP or MXF. Similar results were obtained with LVX, NOR and GMF [not shown]. Induction was however reversible upon drug removal.
Conclusion: The ABC efflux system PatA/PatB is reversibly induced upon exposure of S. pneumoniae to sub-MIC concentrations of FQ, whether good substrates (CIP, NOR) or not (MXF, LVX, GMF). This effect is particularly marked in strains showing a high basal expression level, suggesting it contributes to resistance.
| Strains and MIC (mg/L)a | Inducer antibiotics | Gene expression levelsb,c |
||
|---|---|---|---|---|
| pmrA | patA | patB | ||
| ATCC 49619 | Basal | 1 | 1 | 1 |
| CIP: 1/0.5 | + CIP | 1.24±0.03 | 3.46±0.02 | 3.14±0.01 |
| MXF: 0.25/0.25 | + MXF | 1.03±0.01 | 3.05±0.03 | 3.07±0.32 |
| SP13 | Basal | 1.90±0.16 | 12.66±0.24 | 11.98±0.58 |
| CIP: 16/2 | + CIP | 1.65 ±0.02 | 22.11±0.32 | 20.51±2.81 |
| MXF: 0.25/0.25 | + MXF | 1.52±0.03 | 20.74±3.54 | 22.4±3.06 |
| SP295 | Basal | 1.24±0.05 | 4.90±1.11 | 4.83±0.65 |
| CIP: 2/0.5 | + CIP | 1.16±0.07 | 25.78±2.71 | 13.86±4.18 |
| MXF: 0.125/0.125 | + MXF | 1.10±0.03 | 27.03±0.67 | 19.21±1.50 |
| SP334 | Basal | 0.84±0.06 | 3.54±0.16 | 4.40±0.17 |
| CIP: 4/1 | + CIP | 1.25±0.01 | 14.47±1.22 | 13.82±0.93 |
| MXF: 0.5/0.5 | + MXF | 1.14±0.04 | 10.56±0.43 | 10.97±0.57 |
| SP335 | Basal | 2.33±0.31 | 10.71±1.75 | 7.44±0.71 |
| CIP: 32/2 | + CIP | 1.95±0.05 | 113.80±48.8 | 97.94±9.35 |
| MXF: 0.5/0.25 | + MXF | 2.56±0.03 | 145.88±1.75 | 81.62±6.57 |
MIC determined without/with the efflux pump inhibitor reserpine (10 mg/L)
expressed as the ratio to the basal expression level measured in ATCC 49619
gene expression level in boldface indicates an increase compared to the basal level without inducers.
O496 Efflux increases QRDR (quinolone resistance determining region) mutation frequency in fluoroquinolone-susceptible pneumococci
N. Mihaylov, C.B. Duesberg*, D. Rudolf, T. Fuehner, T. Welte, M.W. Pletz (Hanover, DE)
Objectives: Resistance to fluoroquinolones requires sequential mutations in both target enzymes DNA gyrase and topoisomerase IV. Single mutations usually increase the MIC slightly, but enhance the probability of further mutations. Efflux pumps like PmrA reduce antibiotic concentrations in the bacterial cell, enabling longer survival. We hypothesised that efflux positive bacteria are more likely to develop resistance than efflux negative bacteria.
The following questions were addressed:
-
1.
Do the efflux pump inhibitors reserpine and verapamil reduce the mutation frequency?
-
2.
Do fluoroquinolone-susceptible efflux positive pneumococci exhibit higher parC or gyrA QRDR mutation frequencies than efflux negative isolates?
-
3.
Does efflux phenotype impose a fitness cost?
Methods: Matched efflux positive and negative pneumococcal isolates with identical or similar genotype according to multi-locus sequence typing collected by the German community acquired pneumonia network CAPNETZ were analysed (n = 17). Strains TIGR4 and R6 were included as efflux negative controls.
Ciprofloxacin (CIP) MICs and efflux phenotype were measured by agar dilution method, for efflux detection reserpine (10 mg/l) was added and a fourfold decrease in MIC was considered as efflux positive.
Mutation frequencies were determined by plating bacterial suspensions onto agar with and without CIP. After incubation colonies were counted and the ratio of CFU/ml yielded the mutation frequency. Equally, the mutation frequency was determined adding different concentrations of verapamil (10, 25, 50, 100, 500 mg/l) or reserpine (0.01, 0.1, 1, 5, 10 mg/l).
Biological fitness was calculated as the maximum slope of growth curves recorded in a microtitre plate reader.
Results: 1) Even at low concentrations, reserpine clearly reduced the mutation frequency of efflux positive and, to a lesser extent, efflux negative pneumococci when exposed to CIP (figure 1 ); verapamil exhibited this effect merely at high concentrations. 2) Efflux positive isolates produced more frequently mutants (8/9) than efflux negative isolates (2/10) (p = 0.005, Fisher's exact test). 3) Efflux phenotype had no measurable impact on the biological fitness.
Figure 1.
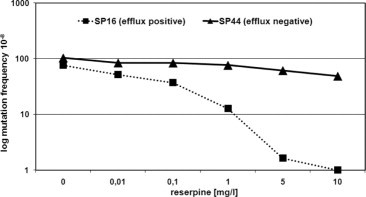
Effect of reserpine on the mutation frequency of pneumococcal isolates with identical MLST sequence type.
Conclusion: A positive efflux phenotype increases the QRDR mutation frequencies in the presence of fluoroquinolones and this effect can be inhibited by very low concentrations of reserpine. As a matter of concern, efflux is not associated with decreased biological fitness.
O497 Lack of emergence of fluoroquinolone resistance and gyrA mutatios in S. pneumoniae despite increased fluoroquinolone use
R. Melano, S.N. Patel, A. McGeer*, K.A. Green, D.R. Pillai, S. M. Poutanen, D. Low on behalf of the Canadian Bacterial Surveillance Network (CBSN)
Background: Use of fluoroquinolone (FQ) has been associated with increasing FQ resistance in S. pneumoniae. Because respiratory FQs (levofloxacin (Levo) and moxifloxacin (Moxi)) are first line therapy for serious respiratory infections, increasing FQ resistance (FQR) in SP is a concern. Levo targets parC, and Moxi targets gyrA, which may permit differentiation of degree of selective pressure. We examined FQ use, and changes in the prevalence of FQR and QRDR mutations in Canadian isolates of SP.
Methods: CBSN is a Canadian collaborative network of microbiology laboratories that has performed surveillance for antibiotic resistance in SP since 1988. Antimicrobial resistance is performed in a central lab to CLSI standards. We sequenced QRDR regions of all FQR isolates and a stratified sample of FQ susceptible isolates. Population FQ use was obtained from IMS Canada.
Results: From 1995 to 2007, FQ use increased from 53 to 97 Rx/1000pop/yr; Levo use from 0 to 10 Rx/1000pop/yr, and Moxi use from 0 to 17 Rx/1000pop/yr. 31081 isolates were available for testing. Levo R rates increased from 0 in 1993 to 1.8% in 2002 then remained stable until 2008 (1.6% in 2008). Moxi R rates increased to 0.6% in 2004, then stabilised (0.7% in 2008). The prevalence of parC only mutations has not increased significantly in the last decade (see Table ). The prevalence of isolates with both parC and gyrA mutations increased until 2002, but has decreased in 2008. The first gyrA only mutant was detected in 2000; the prevalence of gyrA only mutants since then has increased, but remains very low (7/2044, 0.34% in 2007).
| Year | Rates of mutations in QRDR regions |
|||
|---|---|---|---|---|
| N | parC only | parC & gyrA | gyrA only | |
| 1997 | 1409 | 1.72 | 0.40 | 0 |
| 1998 | 1426 | 1.89 | 0.21 | 0 |
| 1999 | 2086 | 1.52 | 0.28 | 0 |
| 2000 | 2191 | 1.46 | 0.64 | 0.14 |
| 2001 | 2240 | 1.74 | 0.85 | 0.04 |
| 2002 | 2504 | 1.11 | 1.55 | 0.04 |
| 2003 | 2419 | 0.83 | 0.87 | 0.12 |
| 2004 | 2548 | 0.63 | 1.35 | 0.12 |
| 2005 | 2662 | 1.05 | 1.24 | 0.08 |
| 2006 | 2224 | 1.88 | 1.27 | 0.39 |
| 2007 | 2044 | 1.03 | 0.68 | 0.34 |
Conclusion: Despite increasing use of respiratory FQs, FQR in pneumococci is very low and not increasing in Canada. The prevalence of isolates with parC mutations is decreasing. Isolates with mutations in gyrA alone remain extremely rare, suggesting that Moxi exerts minimal selective pressure for resistance.
O498 Characterisation of a chimeric mosaic structure carrying erm(B) and tet(O) genes in S. agalactiae
A. Lupo*, M. Scillato, O. Tomasello, T. Triscari Barberi, S. Stefani, J. Blackman Northwood, D.J. Farrell, M. Santagati (Catania, IT; Cambridgeshire, UK)
In Streptococci, two well characterised macrolide resistance have been described: target modification and active drug efflux. Target site modification is mediated by the erm genes – erm(B), erm(A), erm(C) – which confers the MLSB phenotype. Target modification by mutations in 23S rRNA as well as mutation in L4 and L22 ribosomal proteins have also been reported. Expression of mef(A) genes activate an efflux mechanism responsible for M-type resistance
We characterised a clinical isolate of S. agalactiae MB56GBS022 exhibiting the MLSB phenotype and tetracycline resistance. In this study, we determined the resistance genes, their association, and their localisation and mobility by conjugation.
Methods: The macrolide and tetracycline resistance genes were confirmed by PCR. The association between macrolide and tetracycline genes was investigated by Long-PCR and sequencing. Conjugation experiments were performed by filter matings. The genetic localisation of resistance genes was determined by endonuclease I CeuI – followed by PFGE and Southern blot. The hybridisation study was performed using three specific probes for the 16S and 23S rRNA genes, for erm(B) and tet(O) genes.
Results: S. agalactiae MB56GBS022 carried erm(B) and tet(O) genes on the same amplicon of 7 kb in size. The nucleotide sequence analysis of the entire product was identical to the pEOC01 of 11 kb from Pediococcus acidilactici that contains four orfs, of which orf2 and orf3 encode a putative resolvase and topoisomerase type I, respectively.
The endonuclease I CeuI method, that easily distinguishes between plasmid and chromosomal localisations as I-CeuI only cuts chromosomal DNA, revealed the localisation of resistance genes on the plasmid.
All attempts to transfer erm(B)-tet(O) structure by conjugation from S. agalactiae MB56GBS022 to OG1SS E. faecalis as recipient failed.
Conclusion: Our results show the first case of the association between erm(B) and tet(O) genes on the unique mosaic structure in S. agalactiae, probably on the plasmid, as demonstrated by the I CeuI-assay. Further studies are on going to characterise the entire genetic element carrying resistance genes.
Clinical virology
O499 Improving influenza pre-analytic collection systems: alternative collection systems to inactivate, preserve, or extract influenza for rapid testing
S. Castriciano*, K. Luinstra, M. Ackerman, A. Petrich, M. Smieja (Brescia, IT; Hamilton, CA)
Objectives: In this study, 3 alternative influenza sample collection systems were evaluated for potential use in a pandemic situation. The objectives were to develop: 1) a non-temperature dependent swab collection and transport system, that inactivates influenza virus infectivity but preserves cell morphology and nucleic acid (NA) for the detection of suspected influenza infections and/or 2) a system compatible with direct NA testing without the need for purification prior to detection by a rapid real-time RT-PCR.
Methods: Flocked nasopharyngeal swabs (NPS) collected in UTM (U) were compared to NPS collected in a CyMol (C), M-swab (M) or Dry (D) Flocked Swab collection system (Copan, Italia). CyMol is an alcohol-based medium that preserves cells for DFA testing. The M-swab contains 600 uL of medium and 150 uL of glass beads, and requires no NA purification step. Shell vial culture was used to assess influenza virus inactivation after 30 minutes exposure to the collection media. A mock-infected Influenza A virus sample was absorbed to duplicate swabs then placed into the 4 collection systems. The infected collection media were held at RT for 30 minutes and then inoculated in duplicate into shell vial culture and stained after 48 hours. Influenza A stability and NA recovery after mock infection of each collection system was assessed after 1, 7, 14 and 21 days (d) at 4°C, −20°C, room temperature (RT) and 37°C. Aliquots of infected collection media were extracted by easyMag and 5 uL of purified NA tested by a quantitative influenza A RT-PCR on the Roche LightCycler. M-Swab collected samples were also tested directly or after boiling, without NA purification.
Results: Shell vial culture found that Influenza A virus was inactivated after 30 minutes exposure to the C medium but not when exposed to the U and M media. Influenza A was detected by DFA from the U and C cell smears. Quantitation of Influenza A RNA was constant after 1, 7 and 14 d in U, C, M and D collection systems at −20, 4°C and RT. The quantity of RNA recovered declined significantly after 14 d at 37°C in all 4 collection systems. M with boiling yielded data comparable to the easyMag extraction.
Conclusions: The Copan CyMol medium inactivates influenza infectivity, preserves cells and stabilises RNA up to 14 days at −20, 4°C and RT. CyMol medium is a potential alternative for safe sample collection during a pandemic influenza situation. The M-swab presents a rapid testing alternative.
O500 Molecular detection of 12 viruses and subtypes by Luminex respiratory viral panel in respiratory specimens from children
R. Selvarangan*, S. Selvaraju, D. Baker, K. Estes, L. Hays, D. Abel, S. Hiraki (Kansas City, US)
Objective: Luminex respiratory viral panel (RVP) is a multiplex PCR capable of detecting and differentiating twelve different respiratory viruses and their subtypes; influenza A (Flu A) (subtypes H1 and H3), influenza B (Flu B), Respiratory syncytial virus (RSV) (subtypes A and B), Adenovirus (AdV), Parainfluenza 1 (PIV 1), Parainfluenza 2 (PIV 2), Parainfluenza 3 (PIV 3), human metapneumovirus (hMPV) and Rhinovirus (RhV). The aim of this study was to evaluate the analytical performance characteristics of RVP assay and to evaluate its ability to detect respiratory viruses from nasopharyngeal aspirates obtained from children.
Method: Analytical sensitivity, specificity, accuracy and precision of the Luminex RVP assay were determined using control viral stocks and respiratory specimens previously tested by Rmix shell vial culture. Result: Luminex RVP assay reliably detected ATCC viral stocks of Flu A, Flu B, RSVB, RhV and PIV3 in the range of 10e-2 to 10e-4 TCID50/ml. No cross reactivity was noted with CMV, HSV, HHV6, EBV, VZV, PIV4, cornoavirus 229E and OC43. Among 146 respiratory specimens previously characterised by culture 138 specimens were accurately detected with overall accuracy of 95%. The median coefficient of variation in mean fluorescent index values of signals from replicate analyses of influenza A, B and RSV was 9% (7% to 25%). The 146 clinical specimens tested by RVP assay included 109 culture positive and 37 culture negative specimens. Respiratory viruses isolated from the culture positive specimens include the following; 19 AdV, 11 Flu A, 10 Flu B, 19 RSV, 9 PIV1, 6 PIV2, 5 PIV3, 19hMPV and 14 RhV. RVP assay detected all of the respiratory viruses except one each of RSV, PIV1 and PIV2 virus with overall sensitivity ranging from 88% to 100% for the different respiratory viral groups. Among the 37 culture negative specimens 20 respiratory viruses were detected by RVP of which 15 were subsequently confirmed by repeat analyses.
Conclusion: Luminex RVP assay is a highly sensitive and specific test useful in the detection of commonly encountered respiratory viruses in respiratory specimens. The addition of RVP assay to the viral testing algorithm of respiratory infections in children provides rapid results, improves diagnostic yield and may result in decreased antibiotic usage, reduced diagnostic testing and reduced hospital stay.
O501 Aetiological role of viruses in hospitalised patients with acute gastroenteritis in Greece
M. Savvala, I. Daniil, I. Berberidou, A. Koutsibiri, A. Stambolidi, M. Papachristodoulou, N. Spanakis, D. Petropoulou*, A. Tsakris (Athens, GR)
Objective: In developed countries, viruses, particularly noroviruses, are recognized as the leading cause of acute gastroenteritis. We determined the aetiology, prevalence and seasonal distribution of viral gastrointestinal infections in hospitalised patients with acute diarrhoea.
Methods: During one-year period (November 2007-November 2008), a total of 201 faecal specimens were collected from 165 children, 21 premature neonates and 15 adults who were hospitalised with symptoms and signs of acute gastroenteritis. Stool samples were tested for the presence of rotavirus, adenovirus, astrovirus and norovirus. Rotavirus, adenovirus and astrovirus antigen detection was performed by chromatographic immunoassays (Rotavirus and Adenovirus, VIKIA®-bioMerieux, France; H&R Astrovirus-Vegal Farmaceutica, Spain). Noroviruses were detected by an enzyme immunoassay (Ridascreen®r-biopharm, Germany) and confirmed by reverse transcription-PCR. Data were analyzed for seasonality of infection and possible transmission mode.
Results: The overall incidence of viral identification in acute diarrhoeal stool was 24% (48 of 201 patients). Fifty one viral antigens were detected and the overall prevalence rates for rotavirus, adenovirus, norovirus and astrovirus were 14.9% (30/201), 7.0% (14/201), 3.0% (6/201) and 0.5% (1/201), respectively. Noroviruses were detected in 3 patients during an epidemic in December 2007, in one patient while he was in cruise and in 2 premature neonates hospitalised in the neonatal unit. Mixed viral infection by norovirus and astrovirus was detected in an adult and by rotavirus and adenovirus in 2 adults. The majority of cases of viral gastroenteritis occurred in spring (37.5%) and in summer (27.1%), caused mainly by rotavirus, while norovirus infections occurred during early autumn and winter.
Conclusions: Rotaviruses followed by adenoviruses were the main causative agents of viral gastrointestinal infections in our hospitalised population, which was mostly consisted of infants and young children. The aetiological diagnosis of gastroenteritis allows the isolation of infected patients, the prevention of epidemics and the avoidance of unnecessary use of antibiotics.
O502 Presence of oncogenic human papillomavirus infections in female population from southern Italy, correlation with cyto-histological abnormalities and implications in vaccine campaign
L. Tagliaferro*, P. Menegazzi, E. Reho, L. Barzon, G. Palù (Lecce, Padua, IT)
Objectives: The advent of some HPV prophylactic vaccines increased the necessity to improve the knowledge of local viral type distribution to survey the impact of vaccination on HPV-related diseases. Actually, few epidemiological data are available in Italy, so we evaluated the presence of oncogenic HPVs in female population from South of Italy and their correlation with cervical cyto-histological abnormalities.
Methods: 654 genital samples, collected from 2003 to 2008, were investigated for HPV presence and matched with PAP test results and histological data, when available.
HPV typing was performed by a commercial assay, able to detect up to 28 genotypes.
Results: HPV DNA was detected in 45.9% of samples, 41.7% of which had multiple infection. In women with single infection, the most common HPV types were HPV-6 and HPV-16, followed by HPV-51, HPV-31, HPV-53 and HPV-66, whereas in women with multiple infections HPV-6 was the most commonly detected type, followed by HPV-66, HPV-31, HPV-16 and HPV-51.
A different distribution of HPV types and a higher rate of multiple infections were observed in young vs. older women, suggesting the existence of a natural selection of HPVs which preserve a better fitness. High-risk HPVs were detected in all high-grade cervical intraepithelial lesions, with HPV-16, HPV-18, HPV-31, and HPV-51 as the most frequent types. However, HR-HPV types were detected also in a high rate of women with a negative Pap test as well as in women with a negative cervical biopsy, suggesting the need to improve the accuracy of available cervical cancer screening tests.
Conclusion: The results of this study, which provide information on the epidemiology of HPV infection and type distribution in women from South Italy, should be taken into consideration in the implementation of local vaccination programs.
O503 HPV infection in HIV-infected men who have sex with men and correlation with HHV8 shedding
S. Parisi*, C. Boldrin, R. Scaggiante, M. Cruciani, S. Andreis, A. Barelli, S. Pagni, F. Dal Bello, G. Palù (Padua, Verona, Venice, IT)
Objectives: To evaluate HPV genotypes circulation and persistence over time in different sampling sites among HIV(+) men who have sex with men (MSM) (pts) and correlations with HHV8 oral shedding.
Methods: Samples obtained from rectal mucosa- (RS), pharyngeal-swabs (PhS) and saliva of 118 pts from December 2007 to December 2008 were studied. After 6 mo, samples were collected again. Amplification products were sequenced by in-house method using ABI PRISM 3130 XL. HHV8 oral shedding was tested by Real-Time in-house method.
Results: HPV was found in 97 (82%) of RS: 9 pts had multiple HPV-genotypes, and 82 pts a single genotype or an identified type with a co-infection with other not-identified types [32 (39%) High-Risk genotypes (HR) – 11 HPV-16, 1 HPV-18, 2 HPV-33, 1 HPV-53, 6 HPV-58, 11 HPV-66-; 42 Low Risk genotypes (LR) – 12 HPV-6, 6 HPV-11, 1 HPV-40, 7 HPV-61, 5 HPV-70, 2 HPV-72, 4 HPV-81, 5 HPV-83, and 8 other types]. 2 pts had amplification products not further analysable, 4 typing are ongoing and 21 pts were negative.
After 6 mo, 56/58 RS (+) re-tested were found still positive; 27 pts with LR/HR-RS still harboured the same genotype; 2 LR became negative; 5/9 RS-negative became positive, 3 with HR-HPV.
Among 71 PhS evaluated, 17 (24%) were positive (5 HR-HPV), 15 with concurrent RS (+), often with a different genotype.
81% of pts receiving antiretroviral therapy (66% of total) and 90% of naive pts (34% of total) were found RS(+). No significant differences were observed in HR-HPV prevalence among these groups.
92 pts were evaluated for oral HHV8 shedding. 12 pts were HHV8(−)/RS-HPV-neg, 55 HHV8(−)/RS-HPV(+) and 25 (27%) HHV8(+)/RS-HPV(+); 12 associated with HR/LR-HPV. 66% of HHV8-pos were HIV treated.
Conclusions: A high prevalence of HPV infection was found in RS from HIV(+) MSM, with HR/LR types in at least 76% of positive RS and in 61% in the entire cohort, irrespective of HAART treatment. Moreover, the persistence over 6 mo of the same HPV-types in RS was commonly observed, together with HPV infection in pharynx. HHV8 oral shedding was correlated with HPV infection. These findings suggest a possible multiple source of acquisition and spreading of HPV to sexual and non-sexual contacts. Careful survey for HPV and HHV8 infection should be carry out in HIV-MSM, a population at high risk of developing HPV- and HHV8-related cancers. These co-infections suggest repeated sexual unprotected contacts.
O504 Viral antigen expression in individuals with chromosomal integrated HHV-6
V. Strenger*, W. Schwinger, W. Zenz, I. Lautenschlager, S.W. Aberle, T. Popow-Kraupp, E.P. Nacheva, A. Virgili, G. Zobel, C. Urban (Graz, AT; Helsinki, FI; London, UK)
Objectives: Chromosomal integration of the HHV-6 genome (CIHHV-6) into the human genome occurs in 1–2% of healthy individuals and leads to persistently high levels of HHV-6 PCR copy numbers in blood and tissue. Consequently, this may be interpreted as persistent active HHV-6 infection.
Although HHV-6mRNA has been detected in a few individuals with CIHHV-6, there is no evidence of replication of viral particles up to now. Viral cultures have shown negative results. So, CIHHV-6 is thought not to be linked to any disease.
Methods: We performed HHV-6 antigen detection in PBMCs of 4 individuals with FISH proven CIHHV-6 by means of antibodies directed against HHV-6 variant A and B (indirect immunoperoxidase staining).
Results: In 2 unrelated female adolescents (both with CIHHV-6 variant A) we detected HHV-6 antigen. One patient is suffering from recurrent parotitis since 5 years and from hypoimmunoglobulinaemia. The other patient (15a) was treated with allogeneic bone marrow transplantation (BMT) for acute myeloid leukaemia (AML) and acquired CIHHV-6 from the healthy donor. So, CIHHV-6 is only found in blood cells. In the latter patient only symptoms attributable to the post BMT course have been observed (prolonged mixed haematological chimerism, protracted mucositis, transient hypertension and transient neuropathy). At the time of antigen detection 5 years after BMT the patient was clinically well. In 2 individuals (a girl after fatal myocarditis and her healthy father – both with variant B) no HHV-6 antigen has been detected.
Discussion: Up to now CIHHV-6 is considered not to cause any disease. For the first time we show the expression of HHV-6 antigen, which indicates the replication of viral particles. This might have a pathophysiological impact.
One patient with positive antigen detection is suffering from a disease of unclear aetiology. So, an association of replication of CIHHV-6 with the disease might be considered.
In contrast, the other patient did not show any symptoms at the time of antigen detection. This patient shows a special mode of acquisition of CIHHV-6 (by BMT) possibly resulting in differences in the immunological priming and response. In addition, in the latter patient CIHHV-6 is restricted to blood cells.
Two other patients did not show antigen expression. So, it is unclear how the transcription and translation of viral genes is influenced? Furthermore, is there a pathophysiological impact of viral replication in individuals with CIHHV-6?
| 1 | 2 | 3 | 4 | |
|---|---|---|---|---|
| Age | 5a | 43a | 15a | 18a |
| Gender | female | male | female | female |
| Underlying disease, symptoms at the time of antigen detection | minimally conscious state after resuscitation due to severe myocarditis | healthy, father of patient 1 | AML, BMT 5 years ago, transmission of CIHHV-6 by BMT, no symptoms | chron. parotitis for the last 5 years, hypoimmunoglobulinaemia |
| HHV-6 variant | B | B | A | A |
| Antigen detection | neg. | neg. | pos. | pos. |
| Chromosome site | 9p ter | 9p ter | 17p ter | 17p ter |
O505 Cellular inflammation and viral loads in primary Epstein-Barr viral meningo-encephalitis
E. Bathoorn*, B.J. Vlaminckx, R. Donders, S.A. Schoondermark-Stolk, S.F. Thijsen (Utrecht, Nieuwegein, NL)
Objectives: Several case studies have reported on meningo-encephalitis caused by a primary Epstein-Barr virus (EBV) infection. We aimed to investigate the viral loads, and the inflammatory characteristics of this thus far poorly defined disease entity.
Methods: We evaluated all cases from 2003–2008, in which an EBV polymerase chain reaction test (PCR) was requested on a cerebro spinal fluid (CSF) sample. Primary infection was defined as a clinical presentation with sore throat/pharyngitis/malaise in combination with lymphocytosis, and detectable heterophile antibodies or positive EBV IgM antibodies. Patients with proven neuroborreliosis served as control group. Leukocyte response and EBV viral loads in CSF, and serum were compared between primary EBV and neuroborreliosis cases.
Results: We identified six cases with a primary EBV infection (median age: 22, male: 4) with neurological symptoms ranging from meningeal signs to encephalitis. These were compared to 14 patients with neuroborreliosis (median age: 27, male: 6). In four out of six patients with a primary EBV infection with neurological symptoms EBV DNA was detected in CSF and in serum, whereas all neuroborreliosis cases were EBV PCR negative in both compartments. Viral loads were lower in CSF as compared to serum. In blood, leukocytes, lymphocyte, and monocyte counts were significantly increased as compared to the neuroborreliosis cases (see table 1 ).
Table 1.
| EBV-meningitis (n = 6) | Neuroborreliosis (n = 14) | |
|---|---|---|
| Leukocytes in blood (×109/L) | 13.5 (10.3–18.5)* | 7.2 (5.9–10.5) |
| Neutrophils in blood (×109/L) | 5.8 (4.7–10.5) | 4.4 (3.4–8.0) |
| Lymphocytes in blood (×109/L) | 7.6 (2.9–12.8)† | 1.7 (1.2–2.2) |
| Monocytes in blood (×109/L) | 1.3 (1.2–1.7)† | 0.7 (0.6–0.9) |
| EBV PCR in CSF (DNA copies) | 226 (<50–1461)†; n = 2 <DL | All <DL |
| EBV PCR in serum (DNA copies) | 1507 (<50–14127)†; n = 2 <DL | All <DL |
CSF: cerebrospinal fluid. EBV: Epstein-Barr virus. DL: detection limit (50 DNA copies).
p < 0.05
p < 0.01; comparison by Mann-Whitney U-test.
Data presented as median (interquartile range).
Conclusion: Sixty-seven % of cases with EBV meningo-encephalitis have detectable viral DNA amounts in CSF and serum, whereas neuroborreliosis patients do not. Cases with primary EBV meningoencephalitis have increased systemic leukocytosis, with higher lymphocyte, and monocyte levels compared to neuroborreliosis patients.
O506 Incidence of post-herpetic neuralgia in treated and untreated patients with herpes zoster followed for 1 year in an Italian prospective cohort: preliminary results
G. Parruti*, F. Sozio, C. Rebuzzi, M. Tontodonati, E. Polilli, A. Agostinone, A. Manna, F. Di Masi, A. Consorte, G. Congedo, L. Cosentino, D. D'Antonio, L. Pippa, L. Manzoli, C. Granchelli (Pescara, Chieti, IT)
Objectives: A large prospective cohort of patients with herpes zoster (HZ) was enrolled between May 2006 and June 2008 in Pescara, Italy, with a planned 1-year follow-up after clinically and/or molecularly assessed diagnosis. Aim of the study was to evaluate predictors of prolonged acute course and/or incidence of Post-Herpetic Nevralgia (PHN).
Methods: Data from all enrolled patients were collected by a network of 51 general practitioners. Suspected cases and patients with intense acute pain were referred to our institution for immediate evaluation. Clinical and demographic information was mandatory at baseline, as photographs of enrolled patients. For uncertain cases, varicella-zoster virus (VZV) antibodies and VZV DNA PCR on plasma and/or vesicular eluates (whenever available) were performed. Follow-up data were collected at outpatient control visits or by phone calls at 1, 3, 6 and 12 months after onset of HZ. PHN was diagnosed when pain persisted or relapsed at least one month after complete clearing of dermatomeric lesions. Adverse events other than pain were classified according to WHO grading scale and reported if ≥2. All statistical calculations were performed by Stata 8.0 software package.
Results: 523 patients were enrolled, 306 (58.5%) females, with a mean age of 57.7 years, 1-year follow-up data being now available for 489. HZ was localised at thorax in 45.4% and head in 20.7%; pain in the acute phase was reported as intense or very intense by 127 (25.97%) patients; 54 (11.04%) patients were referred for molecular diagnosis as clinically uncertain, 37 (68.5%) being confirmed as VZV-related cases. Forty eight (9.82%) patients were not prescribed any antiviral drug at diagnosis by referring physicians, in spite of extensive support in the study plan. During follow-up, 163 (33.3%) patients reported any type of adverse event (at a mean of 91.2±74.8 days), including 93 (19.02%) patients reporting PHN. PHN was significantly more frequent in untreated vs treated patients (37.5% vs 17.0%, p = 0.001), as were total adverse events (54.2% vs 31.1%, p = 0.001). Untreated patients did not significantly differ from those treated by age (56.3% vs 57.7%, p = 0.66) and sex (females vs males 11.9% vs 6.9%, p = 0.056), whereas they complained for more intense pain (15.0% vs 8.0%, p = 0.024) at presentation.
Conclusion: Our study confirms the importance of early diagnosis and prompt antiviral treatment at the onset of HZ in order to minimise the risk of PHN.
O507 Emergence of an unusual group A rotavirus VP4 genotype among bovine population in India
A.B. Kolpe, R. Arora, M.M. Yadav, C.G. Raut, S.D. Chitambar* (Pune, IN)
Objective: To perform the molecular characterisation and the phylogenetic analysis of unusual G8P[14] bovine group A rotavirus (BoRV-A) strains identified in Pune, western India, during a 2007–2008 rotavirus (RV) epidemiological surveillance.
Methods: Faecal specimens (n = 78) from apparently healthy and diarrheic calves (aged <1 year) were collected per-rectally and investigated for detection of group A rotavirus by antigen capture ELISA (Generic Assay, Germany). ELISA positive specimens (n = 3) were investigated further for molecular characterisation.
Genotyping of BoRV-A strains was carried out on dsRNA extracted from 10% PBS faecal suspensions by a nested and/or heminested RT-PCR specific for VP7 and VP4 genes, using pools of G and P type specific primers. All strains (NIV/BRV/68, NIV/BRV/79, and NIV/BRV/86) were not typeable for the VP4 and VP7 genes.
After purification by “Qiaquick Gel Extraction Kit” (QIAGEN, Germany), the VP4, VP6, VP7, and NSP4 first amplicons of the BoRV-A strains were subjected to sequence analysis with automated sequencer ABI 3130 XL DNA Analyzer (Applied Biosystems, USA). Phylogenetic analysis was performed using MEGA version 4.0.
Results: The NIV/BRV/68, NIV/BRV/79, and NIV/BRV/86 strains exhibited long e-type, G8 and P[14] specificities for VP7 and VP4 genes respectively. By sequence analysis, the VP7 genes displayed high nucleotide (nt) and amino acid (aa) identities to Indian bovine B17 (nt-94.5–98.2% and aa-97.5–99.2%) and Egyptian human EGY2295 (nt-94.2–95.1% and aa-96.8–97.9%) strains, while the VP4 sequences were closely related to the Hungarian human Hun5 strain (nt-94.7–95.4% and aa-97.8–98.2%). The VP6 sequences were found to contain subgroup-I specificity and showed maximum identity with Indian porcine HP140 strain, while NSP4 belonged to genotype-A.
Phylogenetic analysis revealed human and porcine origin of VP4 and VP6 genes respectively, while bovine origin was confirmed by VP7 and NSP4 sequence analysis.
Conclusion: The Indian NIV/BRV/68, NIV/BRV/79, and NIV/BRV/86 strains could be the result of a reassortment between a Hun5-like human strain with P[14] specificity, long e-type and subgroup I, already circulating in Hungary, Italy, and a G8 bovine strain. The genetic relatedness of NIV/BRV strains to Hun5 provides direct evidence for the bovine origin of the VP4 and VP7 genes of human G8P[14] strains.
O508 Prolonged survival of dengue virus in blood and excretion in urine after clinical recovery
C. Laosakul*, M. Sriprapun, K. Chaiyo, S. Krajiw, D. Chansinghakul, G. Suwanpimolkul, J. Pupaibool, K. Arunyingmongkol, C. Pancharoen, U. Thisyakorn, W. Kulwichit (Bangkok, TH)
Objectives: Dengue is a flavivirus and is among the most widely-spread viral diseases. Our previous report demonstrates existence of live dengue virus in blood and urine even in the convalescent postfebrile period. In some cases, excretion in the patient's urine can be detected as late as 28 days after the onset of illness. This goes along with the model of West Nile virus, another type of flavivirus, which can be excreted in the urine for months after acute infection in both animal studies and human case report. Here we report a pilot study to address a magnitude of such findings.
Methods: Between April 2007 and October 2008, paediatric and adult febrile patients suspected of dengue infection were enrolled. Diagnosis of dengue was based on standard specific serology on paired sera. Patients with negative serology served as controls. Blood and urine specimens were collected at several time points. Whole blood was separated into plasma and peripheral blood mononuclear cells (PBMC). These have been aliquoted and used for earlier studies and some stored in freezers. Available plasma, PBMC, and urine were processed and inoculated into Aedes aegypti. Surviving mosquitoes at 14 days after inoculation were employed for viral detection by dengue-specific RT-PCR. Indirect fluorescence antibody (IFA) staining of mosquito heads was performed on all positive RT-PCR specimens, except for the one from PBMC (awaiting IFA result).
Results: 5 and 45 cases of primary and secondary infections, respectively, and 4 negative controls were included. These translated into 55 and 59 early and late dengue specimens, and 6 and 4 early and late negative-control counterparts, respectively. Dengue virus were isolated in some blood and urine specimens as late as 46 days after the onset of illness. No virus was isolated from control specimens. All but 5 positive RT-PCR specimens also demonstrated positive IFA. 4 out of 5 negatives were from early-phase specimens.
Conclusion: Our study demonstrates prolonged survival of dengue virus after clinical recovery. This finding has pathologic and epidemiologic significance, adding a potential role of urine in the transmission of the disease. Spread of the virus to humans might occur through infectious urine with help from arthropod vectors. This research could provide new insights into our understanding of the pathogenesis of DENV infection.
Isolation of dengue virus from blood and urine specimens during early (days 1–7 after onset of illness) and late (days 8–46) phases of infection (specimens with dengue isolated/total specimens for mosquito inoculation)
| Early phase | Late phase | |
|---|---|---|
| Plasma | 16/25 (64%) | 0/13 (0%) |
| PBMC | not performed | 1/2 (50%) |
| Urine | 8/29 (28%) | 12/44 (27%) |
| All specimens | 24/54 (44%) | 13/59 (22%) |
Reference(s)
- 1.Geha RS, Notarangelo LD, Casanova JL, Chapel H, Conley ME, Fischer A. Primary immunodeficiency diseases: an update from the International Union of Immunological Societies Primary Immunodeficiency Diseases Classification. J Allergy Clin Immunol. 2007 Oct;120:776–794. doi: 10.1016/j.jaci.2007.08.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Casanova JL, Fieschi C, Bustamante J, Reichenbach J, Remus N, von Bernuth H, Picard C. From idiopathic infectious diseases to novel primary immunodeficiencies. J Allergy Clin Immunol. 2005 Aug;116(2):426–430. doi: 10.1016/j.jaci.2005.03.053. [DOI] [PubMed] [Google Scholar]
- 1.WA Krueger et al., AAC 2005.
- 2.E Boselli et al., ICM 2004.
- 1.Van den Broek et al. Methicillin-resistant Staphylococcus aureus in people living and working in pig farms. Epidemiol. Infect., published online 24 October 2008 (doi:10.1017/S0950268808001507). [DOI] [PubMed]
- 1.Toté K. Letters in Applied Microbiology. 2008;46:249–254. doi: 10.1111/j.1472-765X.2007.02298.x. [DOI] [PubMed] [Google Scholar]
- 1.Buising K, Thursky K, Robertson M, Black J, Street A, Richards M, Brown G. Electronic antibiotic stewardship–reduced consumption of broad-spectrum antibiotics using a computerised antimicrobial approval system in a hospital setting. J Antimicrob Chemother. 2008 doi: 10.1093/jac/dkn218. [DOI] [PubMed] [Google Scholar]
Uncited References
- 1.Baldwin NS. Clinical Microbiology and Infection. 2008;14:S416. [Google Scholar]
- 1.Ciofu O., Høiby N. Cystic fibrosis – coping with resistance. In: Gould I., van der Meer J., editors. Antibiotic Policies – figthing resistance. Springer Verlag; 2007. pp. 149–174. [Google Scholar]
- 2.Yang L., Haagensen J.A.J., Jelsbak L., Johansen H.K., Sternberg C., Høiby N., Molin S. In situ growth rates and biofilm development of Pseudomonas aeruginosa populations in chronic lung infection. J. Bacteriol. 2008;190:2767–2776. doi: 10.1128/JB.01581-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pamp S.J., Gjermansen M., Johansen H.K., Tolker-Nielsen T. Tolerance to the antimicrobiakl peptide colistin in Pseudomonas aeruginosa biofilms is linked to metabolically active cells, and depends on the pmr and mexAB-oprM genes. Mol. Microbiol. 2008;68:223–240. doi: 10.1111/j.1365-2958.2008.06152.x. [DOI] [PubMed] [Google Scholar]
- Amann R., Fuchs B.M. Nature Reviews Microbiology. 2008;6:339–348. doi: 10.1038/nrmicro1888. [DOI] [PubMed] [Google Scholar]
- de Vries E., for the Clinical Working Party of the European Society for Immunodeficiencies ESID Patient-centred screening for primary immunodeficiency: a multi-stage diagnostic protocol designed for non-immunologists. Clinical and Experimental Immunology. 2006;145:204–214. doi: 10.1111/j.1365-2249.2006.03138.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 1.Doi Y, Wachino J, Arakawa Y. Nomenclature of plasmid-mediated 16S rRNA methylases responsible for panaminoglycoside resistance. Antimicrob Agents Chemother. 2008;52:2287–2288. doi: 10.1128/AAC.00022-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wachino J, Shibayama K, Kurokawa H, Kimura K, Yamane K, Suzuki S, Shibata N, Ike Y, Arakawa Y. Novel plasmid-mediated 16S rRNA m1A1408 methyltransferase, NpmA, found in a clinically isolated Escherichia coli strain resistant to structurally diverse aminoglycosides. Antimicrob Agents Chemother. 2007;51:4401–4409. doi: 10.1128/AAC.00926-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Doi Y, Arakawa Y. 16S ribosomal RNA methylation: emerging resistance mechanism against aminoglycosides. Clin Infect Dis. 2007;45:88–94. doi: 10.1086/518605. [DOI] [PubMed] [Google Scholar]
- 4.Yamane K, Wachino J, Suzuki S, Shibata N, Kato H, Shibayama K, Kimura K, Kai K, Ishikawa S, Ozawa Y, Konda T, Arakawa Y. 16S rRNA methylase-producing, Gram-negative pathogens, Japan. Emerg Infect Dis. 2007;13:642–646. doi: 10.3201/eid1304.060501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Park YJ, Lee S, Yu JK, Woo GJ, Lee K, Arakawa Y. Co-production of 16S rRNA methylases and extended-spectrum b-lactamases in AmpC-producing Enterobacter cloacae, Citrobacter freundii and Serratia marcescens in Korea. J Antimicrob Chemother. 2006;58:907–908. doi: 10.1093/jac/dkl317. [DOI] [PubMed] [Google Scholar]
- 6.Lee H, Yong D, Yum JH, Roh KH, Lee K, Yamane K, Arakawa Y, Chong Y. Dissemination of 16S rRNA methylase-mediated highly amikacin-resistant isolates of Klebsiella pneumoniae and Acinetobacter baumannii in Korea. Diagn Microbiol Infect Dis. 2006;56:305–312. doi: 10.1016/j.diagmicrobio.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 7.Wachino J, Yamane K, Shibayama K, Kurokawa H, Shibata N, Suzuki S, Doi Y, Kimura K, Ike Y, Arakawa Y. Novel plasmid-mediated 16S rRNA methylase, RmtC, found in a Proteus mirabilis isolate demonstrating extraordinary high-level resistance against various aminoglycosides. Antimicrob Agents Chemother. 2006;50:178–184. doi: 10.1128/AAC.50.1.178-184.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yamane K, Wachino J, Doi Y, Kurokawa H, Arakawa Y. Global spread of multiple aminoglycoside resistance genes. Emerg Infect Dis. 2005;11:951–953. doi: 10.3201/eid1106.040924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yamane K, Doi Y, Yokoyama K, Yagi T, Kurokawa H, Shibata N, Shibayama K, Kato H, Arakawa Y. Genetic environments of the rmtA gene in Pseudomonas aeruginosa clinical isolates. Antimicrob Agents Chemother. 2004;48:2069–2074. doi: 10.1128/AAC.48.6.2069-2074.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Doi Y, Yokoyama K, Yamane K, Wachino J, Shibata N, Yagi T, Shibayama K, Kato H, Arakawa Y. Plasmid-mediated 16S rRNA methylase in Serratia marcescens conferring high-level resistance to aminoglycosides. Antimicrob Agents Chemother. 2004;48:491–496. doi: 10.1128/AAC.48.2.491-496.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yokoyama K, Doi Y, Yamane K, Kurokawa H, Shibata N, Shibayama K, Yagi T, Kato H, Arakawa Y. Acquisition of 16S rRNA methylase gene in Pseudomonas aeruginosa. Lancet. 2003;362(9399):1888–1893. doi: 10.1016/S0140-6736(03)14959-8. [DOI] [PubMed] [Google Scholar]


