Abstract
Objective The recent worldwide epidemic of Severe Acute Respiratory Disease (SARS) caused over 800 deaths and had a major impact on the health services in affected communities. The impact of SARS on colorectal surgery, particularly service provision and training, is unknown. This paper reports these changes from a single colorectal unit at the centre of the outbreak.
Patients and methods Hospital databases and electronic patient records covering the 4 months duration of the SARS epidemic and an equivalent period preceding SARS were compared. Data was collected for inpatient admissions, outpatient consultations, operative surgery, colonoscopy and waiting times for appointments or surgery.
Results The SARS epidemic resulted in reductions of 52% for new outpatient attendances, 59% for review attendances, 51% for admissions, 32% for surgical procedures and 48% for colonoscopies. Major emergency procedures, cancer resections and complex major procedures were unaffected. Operative procedures by trainees reduced by 48% and procedures by specialists reduced by 21%. Patients awaiting early or urgent outpatient appointments rose by 200% with waiting times for colonoscopy increased by a median 3, 5 or 9 weeks for outpatient, inpatient or non‐urgent cases, respectively. The waiting time for minor elective colorectal surgery was extended by 5 months.
Conclusion SARS resulted in a major reduction in the colorectal surgical caseload. The consequences were evidenced by a detrimental effect on waiting times and colorectal training. However, serious pathology requiring emergency or complex surgery was still possible within these constraints.
Keywords: SARS, epidemic, colorectal training
Introduction
A respiratory epidemic defined as Severe Acute Respiratory Syndrome (SARS) emerged in the South‐east Asia region in March 2003 [1, 2, 3]. The rapid transmission of the causal organism, a coronavirus named SARS Corona Virus [4, 5], led to 8439 cases in 32 countries worldwide with over 800 fatalities. Although most patients presented with respiratory symptoms or fever, isolated or coexisting abdominal and gastrointestinal symptoms were not uncommon. The epidemic resulted in the implementation of stringent precautionary measures for patients and particularly hospital staff who were at greatest risk from the contaminated droplets and bodily fluids of their patients.
Our hospital treated the index case in Hong Kong and found itself at the epicentre of the outbreak in the region. The epidemic was recognized in the first week of March and resulted in profound changes to the colorectal surgical service. Hong Kong was officially declared SARS‐free by the World Health Organization on 23 June 2003, but the effects on the colorectal service persist. This paper describes the effects of a SARS epidemic on a single colorectal surgical unit.
Patients and methods
The Colorectal Unit serves as a tertiary referral unit for a cluster of local hospitals, but also provides specialist services for colorectal and general surgical diseases. An electronic record system in use throughout the public health service in Hong Kong provided data on out‐patient attendance and in‐patient admissions. Further information was obtained from the Clinical Management System electronic patient records, operating theatre records and the Endoscopy Unit logbooks. For simplicity, we defined the ‘SARS’ period as occurring between 01.03.2003 and 30.06.2003. Data for this period was compared with a similar preceding 4‐month period between 01.11.2002 and 28.02.2003 which we termed ‘Pre‐SARS’.
Outpatient data included new referrals, review consultations and default rates. Waiting times for outpatients were determined on 01.03.2003 (approximately the start of the SARS period) and on 01.07.2003 (at the end of SARS).
Ward occupancy was divided into emergency, elective and daycase admissions. These patients are admitted for either investigation (e.g. colonoscopy) or treatment (conservative or operative) under the care of the colorectal team.
Operative procedures were subdivided into emergency and elective cases. Descriptive terms are used for all operative procedures, but these were additionally classified into minor, intermediate, major, major + or complex major 1–3 according to the British United Provident Association (BUPA) Schedule of Procedures [6]. An operative episode is defined as the performance of, or the assistance with, a surgical operation.
Results
Pre‐SARS, admissions to the colorectal unit totalled 784 cases (214 day cases, 291 emergencies, 279 electives) over the 4‐month period. During the equivalent period of SARS, the total dropped by 51% to 384 admissions of which 109 were day cases (a 49% reduction), 159 were emergencies (a 45% reduction) and 116 were elective admissions (a 58% reduction).
The number of colonoscopies fell by 48% from 178 (Pre‐SARS) to 92 (SARS). In contrast, the waiting times for an urgent colonoscopy increased by 3 weeks for outpatients, by 5 weeks for cases requiring in‐patient colonoscopy and by 9 weeks for nonurgent cases. Total operative procedures reduced from 182 to 112 (32%), mainly due to a reduction in minor, intermediate and major cases (Fig. 1). Of the 182 operations performed Pre‐SARS, 82 (45%) were emergency procedures compared to 63 of 112 operations (56%) during SARS. Cancer resections reduced only from 49 to 41 (16%) during the respective periods. Laparoscopic resection rates were similar (13/49 Pre‐SARS vs 7/41 SARS). Before SARS emerged, there were 181 specialist operative episodes and 152 trainee operative episodes. These operative episodes reduced to 143 for specialists and 73 for trainees during SARS, reductions of 21% and 52%, respectively. Operations performed by trainees were supervised by a specialist in 7 of 97 cases (7%) Pre‐SARS and in 7 of 39 cases (18%) during SARS. Waiting times for elective minor colorectal operations increased from 11 months to 18 months.
Figure 1.
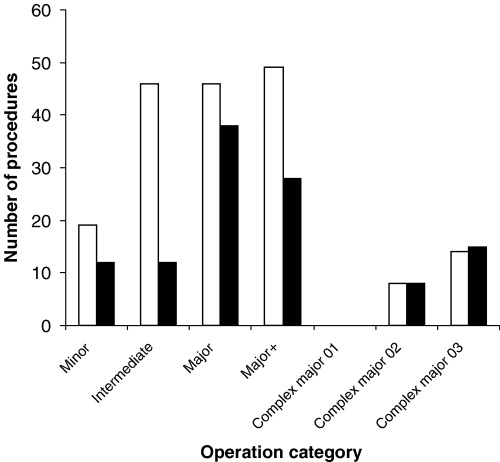
Operations performed according to the BUPA Schedule of Procedures [6]. □ Pre‐SARS; ▮ SARS.
The number of new outpatient referrals awaiting urgent or early appointments (up to 12 weeks) in the colorectal clinic increased from 10 patients before SARS to 32 patients at the end of the epidemic. The overall figures for general surgery however, were 190 and 269 patients for the two periods, respectively. The colorectal unit saw 315 new outpatients and 1721 review cases Pre‐SARS. During SARS these figures dropped to 152 and 702, respectively. Default rates from clinic appointments climbed from 20% to 80% across the general surgery specialty.
Staff shortages and the burden of managing the SARS cases, most notably in medical wards, the intensive care unit and the emergency department necessitated the redeployment of personnel to these units. Fourteen of 40 surgical ward nurses, 8 of 18 endoscopy nurses and 2 junior doctors were temporarily absent from the colorectal unit for varying periods. This amounted to a loss of approximately 800 person working days for the unit.
Discussion
The workload of our colorectal service was severely curtailed in almost all aspects of patient care. The dramatic reductions in throughput of cases, with the notable exceptions of cancer resections and major emergency surgery, have had profound effects on the service. The figures for patients awaiting a colorectal clinic appointment do not appear to be dramatic because a preplanned reconfiguration of outpatient services occurred during SARS which saw new routine colorectal cases deflected to another hospital in the region. In many cases, nonurgent surgery was postponed indefinitely to ensure priority was given to those with life‐threatening diseases. Consequently, most patients requiring minor or intermediate elective procedures such as haemorrhoidectomy and fistulotomy will wait more than 18 months for surgery.
Colorectal trainees suffered a reduction in exposure to cases, affecting both clinical and operative experience. The latter was not reciprocated by an increase in supervision by seniors despite the reduction in the workload for the unit. Basic surgical trainees suffered most by a drastic reduction in the minor, intermediate and elective cases. Participation in the major cases was discouraged due to the high risk of contracting SARS during operative or endoscopic procedures, while instruction was further hampered by the self‐contained ventilation systems used for surgical or endoscopic attire (see Fig. 2). Colonoscopy turnover was further hampered by non–attendance, barrier precautions and prolonged endoscope cycling times, but we have not measured these factors.
Figure 2.
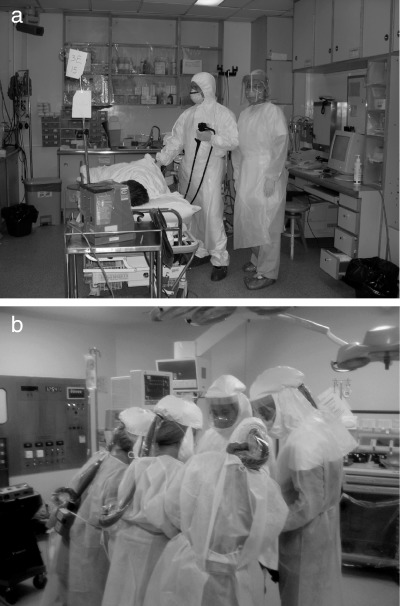
Barrier protective clothing and personal ventilation systems used for (a) colonoscopy and (b) operative surgery during the SARS epidemic.
Indirect effects of SARS on the colorectal service such as cancellations of tutorials, journal clubs, grand rounds or weekly meetings such as radiology, pathology, oncology or morbidity and mortality are unknown. Similarly, we have not studied the effects of SARS on specialists such as their incomes from private practice, the disruption to clinical trials and studies, the effect on their education of undergraduates or their own Continuing Medical Education (CME) accreditation.
No data is available yet on the impact of SARS (if any) on the waiting times for staging investigations, oncology referral or administration of adjuvant therapy of colorectal cancer patients. The full impact of SARS on surgery is still unknown, since its effects on regional economics, politics, hospital infrastructure, health strategy and personnel may only become evident in the long term. The financial consequences of SARS to the economy, and hence the funding of the health service in the next budget, are likely to impact significantly on the colorectal services we can provide.
It is anticipated by some authorities on SARS that more virulent strains will emerge and that epidemics will re‐emerge sporadically [7]. Our own experience with SARS in colorectal surgery has hopefully provided an opportunity for colleagues and managers to reflect on their own service and any contingency plans they have to tackle a similar crisis.
References
- 1. Centre for Disease Control. Outbreak of severe acute respiratory syndrome – worldwide 2003. Morb Mort Week Rev 2003; 52: 226–8. [PubMed] [Google Scholar]
- 2. Lee N, Hui D, Wu A, et al. A major outbreak of severe acute respiratory syndrome in Hong Kong. N Engl J Med 2003; 348: 1986–94. [DOI] [PubMed] [Google Scholar]
- 3. Tsang KW, Ho PL, Ooi GC, et al. A cluster of cases of severe acute respiratory syndrome in Hong Kong. N Engl J Med 2003; 348: 1977–85. [DOI] [PubMed] [Google Scholar]
- 4. Peiris JS, Lai ST, Poon LL, et al. SARS Study Group. Coronavirus as a possible cause of severe acute respiratory syndrome. Lancet 2003; 361: 1319–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Drosten C, Gunther S, Preiser W, et al. Identification of a novel coronavirus in patients with severe acute respiratory syndrome. N Engl J Med 2003; 348: 1967–76. [DOI] [PubMed] [Google Scholar]
- 6. BUPA. (2003). BUPA Schedule of Procedures. [WWW document]. URL http://www.bupa.org.uk [Google Scholar]
- 7. World Health Organization. (2003) Severe acute respiratory syndrome (SARS). Status of the Outbreak and Lessons for the Immediate Future. Communicable Disease Surveillance and Response. WHO, Geneva. [Google Scholar]


