Abstract
A seizuring cat can be a challenging case for every veterinarian and, therefore, the correct diagnosis and the appropriate management of such a case requires understanding of the most common causes of feline seizures. The underlying cause of the seizures should be investigated by a thorough questioning of the diagnostic approach and most likely diagnoses. If the cause of the seizures can be found then the appropriate therapeutic approach may improve the prognosis. The treatment of the feline seizures is similar to the canine patients; however, the differences should be kept in mind. This article is tailored to answer the most common questions that veterinary surgeons should ask themselves when dealing with a seizuring cat.
Keywords: Cats, Seizure, Anti‐epileptic drugs
Seizures, although occurring less commonly than in dogs, are the most common form of neurological diseases in cats (Boothe et al, 2002). Sometimes the first question the clinician has to answer is whether the cat is suffering from seizure or other paroxysmal episodes, before planning further diagnostic and therapeutic plan.
It is very rare to see potentially epileptic cats seize in the consult room. And, without any doubt, a mobile phone with an installed camera is the best invention for the veterinarian interested in neurology or dealing with neurological patients. To have short movie footage of the episode capture by the owner is the most helpful tool in assessing the nature of the described episode. In fact, it is not difficult for the owners to distinguish the generalised seizure as they often manifest as generalised tonic‐clonic episodes, loss of consciousness, opisthotonus, claw clenching, paddling movements, vomiting, urination and defecation (Kline, 1998). However, most cats may also experience focal or partial complex seizures that can remain as isolated incidents or occur multiple times in a day; in such cases, the owner can report that the cat may hypersalivate, have an orofacial automatism such as lip smacking, dilated pupils, rhythmical movements of one limb or excessive vocalisation (Kline, 1998; Schriefl et al, 2008).
Does idiopathic epilepsy exist in cats?
Seizuring in cats is mainly a neurological manifestation of underlying diseases (Boothe et al, 2002). However, cats can suffer from primary epilepsy, also known as probably symptomatic epilepsy or idiopathic epilepsy. The true incidence of the primary epilepsy in cats is unknown but it has been estimated to be as high as 20–60% of all seizuring cats (Quesnel et al, 1997; Schriefl et al, 2008). The increasing access to magnetic resonance imaging (MRI) facilities and cerebrospinal fluid (CSF) analysis confirms that there are a substantial number of cases without a diagnosed underlying cause. Affected cats vary from 1–12 years of age with presentation of generalised and/or partial seizures, and have normal interictal neurological examination (Schriefl et al, 2008).
Why is the cat's age so important?
The age of the cat is important information in drawing up the differential list. As some diseases more commonly affect younger cats and others, older cats. The diseases of the young animals are mainly the anomalous, congenital or infectious diseases. Multiple littermates can be affected and the only complaint is the seizure activity in many cases. The adult and old cats suffer more common inflammatory or neoplastic disease. The classical examples are anomalous/congenital diseases, usually diagnosed in kittens, that should not be firstly considered as a differential diagnosis for older cats with seizures. A number of different congenital brain malformations can cause seizures in young kittens; these include hydrocephalus, porencephaly, lissencephaly and others. Cats with porencephaly have cystic cavities within their cerebrum, and intrauterine feline parvovirus infection of the queen has been postulated as a possible cause for this (Summers et al, 1995) ( Figure 1 ). Treatment is aimed at controlling the seizures, and the prognosis will depend on the response to treatment. Cats with an obstructive hydrocephalus may require surgical placement of a shunt to drain the excess cerebrospinal fluid from the ventricular system to the peritoneum (ventriculoperitoneal shunt). Although this is preferential treatment in cats with congenital hydrocephalus, it is not treating the primary condition and is only palliative. However, the outcome is good if no complications of the shunt device do occur. Some patients can be managed conservatively, mainly with the drugs decreasing the production of cerebrospinal fluid (CSF).
Figure 1.
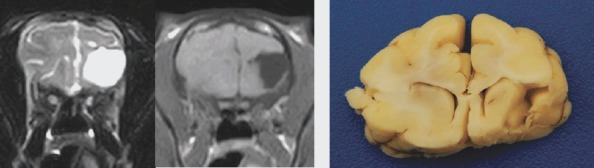
(From left to right) T2 weighted and T1 weighted transverse MRI images of a cat with porencephaly (PCR cerebrospinal fluid was positive for feline parvovirus). Gross post‐mortem ventral view of the brain of a cat with porencephaly
What is the breed of the cat?
Pure breed cats generally suffer more from inherited diseases caused by close inbreeding when compared with mongrels. If the cat is pure breed, the owners should be asked other questions regarding the siblings and ancestors. Various lysosomal storage diseases can cause seizures through interference of neuronal metabolism or accumulation of intracellular by‐products, although seizure activity usually manifests as a late event in the course of the disease. The identification of the affected enzyme and/or the affected gene is usually not possible and the intracellular by‐product may be found in whole blood, leucocytes, skin or liver biopsies. In some cases, accumulated storage product can be found in the urine. The prognosis for confirmed lysosomal storage diseases is poor and no specific treatment is available (Dewey, 2008).
Has the cat changed their behaviour or turned aggressive?
Seizuring cats can start displaying the behavioural changes characterised by aggression and/or depression. This is important add‐on information from the owners because the underlying brain pathology should be considered more likely if the cat presents with such symptoms. If the aggression, along with the partial seizures, is a primary problem then hippocampal necrosis or temporal epilepsy should be considered. Hippocampal necrosis affects the hippocampus and the piriform lobes and is a potential cause of seizure activity. However, it is debatable as to whether this develops as a consequence of inappropriately treated seizure activity or if it is an underlying cause of the seizures. Some authors suggest that seizure activity caused by degenerative, metabolic or toxic disorders can cause bilateral destruction of the hippocampus or of the piriform lobes. Diagnosis is usually made by characteristic MRI features of bilaterally hyperintense lesions on T2 weighted and hypointense lesions on T1 weighted images without a mass effect, and variable contrast uptake in the hippocampus (Schmied et al, 2008).
Is there any history of trauma?
Road traffic accidents, falls or other blunt trauma can commonly lead to traumatic brain injury; cats with a history of head trauma have almost a 12‐fold higher risk of developing epilepsy compared to cats without head trauma (Steinmetz et al, 2010). In this case, the first target is to stop the seizures but the clinician should not forget to rule out other life‐threatening conditions, such as haemo‐ or uro‐abdomen.
Suspect brain trauma: take radiographs or not?
Skull radiographs very rarely yield valuable information. Computer tomography (CT) and MRI can reveal large cerebral haematomas, which may require decompressive surgery in many cases ( Figure 2 ). However, CT and even MRI can also be unremarkable in the cases with severe neurological deficits. The prognosis depends on the presenting clinical signs and response to treatment. Serial monitoring using the Modified Glasgow Coma Scale is commonly used in monitoring the neurological status of dogs, and might also be useful in cats.
Figure 2.

T2 weighted gradient echo dorsal view of the brain of a cat showing a haematoma after a road traffic accident
Is there any known toxin in the cat's environment? Has the cat been treated with an over‐the‐counter flea product?
Many toxins can cause the seizure activity in cats, and knowing the cause of the seizure in case of intoxication is rarely possible. However, the owners are usually aware of applying the pyrethrines and pyrethroids. These are insecticides sold over the counter (OTC) for the treatment of flea and tick infestations, and cats appear to be highly sensitive to these drugs. The incidence of seizures in cats with permethrine intoxication is about 30%, and other neurological signs, such as tremors, twitching, ataxia, ptyalism and mydriasis, are also very common (Boland and Angles, 2010). Clinical sings are usually noticed immediately after exposure or may be delayed for up to 72 hours. Dermal decontamination should be instituted as soon as possible. Diazepam, methacarbamol and phenobarbitone can be used in case of seizures. Other toxins, such as organophosphates, carbamates, ethylene glycol or lead should also be considered if there is a history of exposure.
What is the cat fed on?
Food plays an important role in the life of any animal and particularly vitamin deficiency due to unbalanced diet can be a triggering factor for seizures. Thiamine (Vitamin B1) deficiency is a common cause of seizures in the areas where cats eat primarily a raw fish diet that contains thiaminase, which destroys thiamine. Nowadays, it is more commonly seen secondary to reduced food intake. Characteristic MRI features associated with thiamine deficiency have been described and are reversible if appropriate thiamine administration is instituted (Palus et al, 2010).
Why do I need to do a proper physical examination?
The physical examination can provide several hints in diagnosing the underlying cause of the seizures. Taking the cat's temperature, palpating lymph nodes and thyroid glands, performing abdominal palpation and thoracic auscultation with measurement of blood pressure are basic examinations. When dealing with a seizuring cat, this information will be immensely helpful in constructing the differential diagnoses list and deciding on diagnostic work‐up for the most likely causes of seizures, or seizure‐mimicking episodes in that particular cat. Disorders causing cerebral hypoxia (e.g. polycythaemia, anaemia, cardiomyopathies) can lead to development of the seizures or episodes mimicking seizures. Hyperthyroidism can cause seizures but more commonly causes encephalopathic signs, such as behavioural change and irritability. The increased circulating thyroid hormone concentration is proposed to cause an alteration in brain neurotransmitter balance and to increase the excitability of the brain parenchyma (Dewey, 2008). Systemic hypertension can arise from hyperglucorticoidaemia (hyperadrenocorticism, iatrogenic), renal disease, hyperthyroidism or diabetes mellitus. Systemic hypertension leads to interstitial cerebral oedema, which increases intracranial pressure, resulting in subsequent neurological signs, and is referred to as hypertensive encephalopathy (Brown, 2005). Hypertension is also a potential risk factor for developing haemorrhagic or thrombotic infarctions within the brain, which predispose to seizure activity (Brown, 2005).
Do I have to listen to the heart?
A thorough auscultation of the heart and multiple heart rate measurements should be performed when dealing with the cat a the history of seizures. Paroxysmal episodes associated with high‐grade atrio‐ventricular blocks or other cardiomyopathies can mimic the clinical signs associated with complex partial seizures, and it is, again, important to have a video of the cat from the owner for a better understanding of the clinical signs.
The ophthalmological examination: do I bother in a seizuring cat?
Fundic examination in a seizuring cat is important, as the optic nerve is the only visible part of the brain. The signs of hypertension or other systemic diseases can also be recognised, such as inflammatory or infectious diseases or lymphoma. Feline coronavirus associated meningoencephalitis is one of the most common feline infectious neurological diseases. Cats will often show other systemic signs including pyrexia, lethargy, chorioretinitis and uveitis. The affected cats develop clinical signs when usually under 2 years or later in their life when they are older than 9 years of age. Cerebellar and vestibular signs are the most common presentations, with seizures seen in approximately 25% of cases (Timmann et al., 2008). Characteristic abnormalities on MRI are: obstructive hydrocephalus; ependymitis; and meningitis. Elevated protein and neutrophilic pleocytosis in CSF together with the clinical signs, age, MRI findings and positive coronavirus antibodies or PCR in the CSF are suggestive of the in vivo diagnosis of feline coronavirus infection ( Figure 3 ).
Figure 3.

(Top to botton) T1 weighted and T1 weighted post contrast of a kitten with CNS FIP. CSF of the same kitten with FIP with neutrophilic pleocytosis
Why do I have to do a proper neurological examination?
The seizure is the presentation of forebrain dysfunction. Because forebrain dysfunction is sometimes difficult to assess on the neurological examination in animals, it is important to realise that the seizure can be the only neurological sign. The neurological examination can be completely normal in the interictal period, even in cases with very significant underlying pathology. It is, however, very important to perform the neurological examination, which can reveal symmetrical or asymmetrical neurological deficits. When we are dealing with the cat with symmetrical signs, metabolic or toxic causes should be considered as the most likely differential diagnosis. If asymmetric signs are noted (for example obtundation, aimless pacing, circling, absent or reduced menace response, central blindness or other cranial nerve deficits), intracranial lesions, such as tumours, or a vascular event must be at the top of your differentials list. The incidence of seizures in cats with intracranial tumours is about 20%, and generalised tonic‐clonic seizures are commonly seen (Tomek et al, 2006). Meningiomas are the most common intracranial tumours in cats, and seizure activity is reported in approximately 15–25% of the cases (Troxel et al, 2003; Tomek et al, 2006). They are usually solitary, well‐circumscribed masses, and surgical removal is the treatment of choice with disease‐free survival times reported as 2 years ( Figures 4 and 5). Lymphoma is very common in cats and, in fact, is the second most common tumour affecting cats’ brains (Troxel et al, 2003). The seizures are seen in about 25% of cases with lymphoma affecting brain (Tomek et al, 2006). Lymphoma can be diagnosed by finding lymphoblasts in the CSF ( Figure 6 ). It can affect any part of the CNS, and may be part of a multicentric disease process. Other primary or metastatic intracranial tumours can also infrequently cause seizures.
Figure 4.

T1 weighted transverse post contrast MR image of a cerebrocortical meningioma
Figure 5.
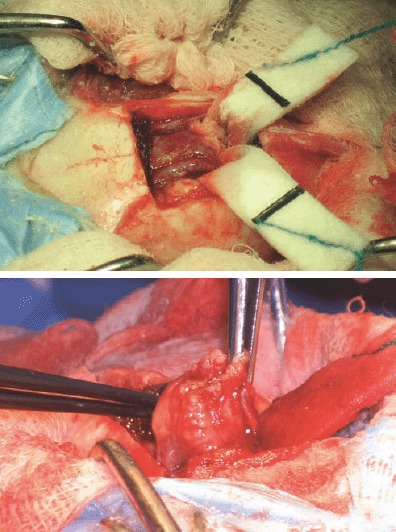
Intraoperative images – removal of the meningioma
Figure 6.

Lymphoblasts in the CSF in a cat with CNS lymphoma
What blood tests would help me?
Haematology should be performed in order to rule out the signs of polycythemia and to look for a possible inflammatory changes in the leucogram. Minimum biochemical database (ALT, albumin, total protein, Glucose, BUN, Creatinine) and electrolyte tests (Na, K, P, Ca) should be performed in order to rule out a possible metabolic cause of the seizures. Metabolic causes of seizure activity include hepatic, renal and electrolyte‐associated encephalopathy, hypoglycaemia, hyperglycaemia and hypocalcaemia (Dewey, 2008). The majority of cases of hepatic encephalopathy are due to underlying liver dysfunction, such as hepatic lipidosis, or from structural abnormalities, such as a portosystemic shunt ( Figure 7 ). Ptyalism is extremely common in cats with hepatic encephalopathy with stunted growth and copper‐coloured eyes also being common presenting features of cats with portosystemic shunts ( Figure 8 ). Hypoglycaemia can result from severe liver disease, insulin overdose, sepsis or an insulinoma; the latter is very rare in the cat. The investigation for metabolic causes of seizure activity may require a bile acid stimulation test, endocrine testing and urine analysis, with abdominal ultrasonography and histopathology as required. Hyperthyroidism is common in older cats and can cause the seizures (Dewey, 2008). So, to run a total feline T4 test in older cats with seizures is also recommended.
Figure 7.

Ultrasound of the cat with the history of partial complex seizures is showing an anomalous vessel entering the caudal vena cava in an unusual angle and causing turbulence
Figure 8.

Copper‐colored eyes of a cat with portosystemic shunt
Do I have to perform urinalysis?
Generally, the urinalysis should always be performed when dealing with neurological feline patient. The main reason for doing so in seizuring cats is to rule out extracranial causes of the seizures. Decreased ability to concentrate urine, proteinuria and glycosuria might be suggesting of a renal disease or systemic hypertension, which was mentioned previously. Also, the presence of urate crystals can be suggestive of a liver disorder. This examination is certainly complementary rather than diagnostic but should not be omitted in a diagnostic work‐up.
Do I perform any diagnostic imaging?
If there is any suspicion (from the history, clinical signs, blood works) of the disease affecting extracranial organs then radiographs and ultrasound can be helpful (e.g. in the cases with portosystemic shunt, FIP, lymphoma) in identifying the primary cause of seizures. However, if these extracranial causes of the seizures are ruled out then MR imaging of the brain is the most useful in identifying or ruling out the intracranial condition causing the seizures.
Do I prescribe steroids or not?
Glucocorticosteroids should not be misused and should only be administered to cases where it is indicated. It can have otherwise catastrophic consequences. An example in which glucocorticosteroids are indicated is non‐suppurative meningoencephalitis of unknown aetiology (MUA). Cats with this disease can develop multifocal intracranial signs, which may include seizures (Quesnel et al, 1997). Other neurological deficits, cervical hyperaesthesia and pyrexia are often accompanying signs. Routine haematology and biochemistry can be unremarkable or may shown signs of a systemic inflammatory response. MRI of the brain can reveal multifocal ill‐defined areas of hyperintensity on T2‐weighted and FLAIR images, with no or minimal contrast enhancement on T1 weighted images. CSF analysis often reveals pleocytosis with elevated protein level (Figure 10). Treatment with immunosuppressive medication (e.g. glucocorticosteroids) can achieve remission of signs. Concurrent anti‐epileptic medication is needed for cases presenting with seizures.
Glucocorticosteroids are contraindicated in cases of suspected infective disease, i.e. toxoplasmosis, a common infectious CNS disease. Toxoplasma gondii is an intracellular coccidian parasite and the cat is the definitive host. Cats can become infected transplacentally, via milk, or through ingestion of sporulated cysts in contaminated food/water or tissue cysts in rodents. Clinical signs are variable and include non‐specific findings such as pyrexia, anorexia and lethargy. Neurological signs of the toxoplasmosis may include seizures, cerebellar and vestibular signs or multifocal CNS signs. Haematology can show an inflammatory leucogram with neutrophilia, lymphocytosis, monocytosis or eosinophilia. Biochemical findings depend on the involved organs during the infection (e.g. muscle, liver.). An elevated Toxoplasma IgM antibody titre indicates recent or active infection, which can be supported by demonstrating a four‐fold increase in the Toxoplasma IgG antibody titre over 2 to 3 weeks. An MRI finding of a mass lesion with contrast enhancement consistent of granuloma, in connection with CSF analysis, serology and PCR can help reaching the in vivo diagnosis. Treatment consists of a course of Clindamycin at a dose of approximately 20–25 mg/kg twice daily; pyrimethamine in combination with trimethropim sulfanamide can also be used. Repeated serology and PCR on CSF and/or blood are necessary to monitor the response to treatment. Treatment needs to be continued until the Toxoplasma IgM antibody titre drops to below that of the IgG titre or becomes negative.
Do I need to refer this cat?
The need for referral does always depend on the facilities of the practice, or the owner's wishes and expectations. Cats with uncontrollable seizures should be referred to specialist neurologists for further investigations. Numerous diseases cause seizures in cats, and some of them cannot be easily diagnosed without advanced investigations (abdominal ultrasound, CT, MRI and/or CSF analysis) and expertise. If the underlying cause is found, treatment should be always aimed at this. Therefore, it is a paramount to investigate these cases thoroughly and diagnose the underlying pathology if present.
When and how to treat seizures in cats?
The aim of any anti‐epileptic treatment is to reduce the frequency and severity of the seizures as well as prevent further increase of epileptogenic foci. Positive response to anti‐epileptic drugs is considered if seizure frequency decreases by at least 50%; however, most cats will still continue to have the occasional seizure despite adequate treatment. Specific treatment targeting underlying cause of the seizures is the first step. However, the majority of cases also require concurrent anti‐epileptic treatment. Any cat presenting in status epilepticus or with cluster seizures has to be considered as an emergency and should receive immediate treatment to stop the seizures, followed by a thorough investigation into the underlying cause. Maintenance therapy is usually indicated in patients experiencing more than one single seizure or cluster seizures, status epilepticus, post‐traumatic seizure and seizures associated with structural intracranial disease.
Phenobarbitone is the first‐line drug for seizuring cats. Although cats are generally less susceptible to the ‘classical’ side effects compared with dogs, sedation, ataxia, polyuria, polydipsia and polyphagia are still the most common side effects, as in dogs. There are also reports of cerebellar signs, reversible leucopenia, thrombocytopenia, coagulopathies, facial or generalised pruritus, limb oedema and hypersensitivity dermatitis (Ducote et al, 1999). Peculiar side effect with generalised lymphadenopathy, and called pseudolymphoma, has been reported recently in the literature; in this study. the lymphadenopathy resolved a few days after changing to another anti‐epileptic drug (Baho et al, 2011). The recommended dose is 1–3 mg/kg once or twice daily. Serum levels are checked after 2 weeks and the dose adjusted accordingly. Therapeutic levels are similar to those reported for dogs at 65–170 μmol/l (15–40 μg/ml) with the ideal range being between 90–130 μmol/l (20–30 μg/ml) (Smith‐Bailey and Dewey, 2009). The phenobarbitone levels should be measured ideally every 3–6 months if the seizure control is adequate. If the seizure control is not adequate or the frequency of dosing increased, the measurement of phenobarbitone level should be performed more frequently. Regular monitoring of haematology and serum biochemistry is important. Phenobarbitone cannot be withdrawn abruptly as ‘withdrawal seizures’ can occur, but patients can develop a physical dependence on phenobarbitone (Podell, 2004).
Levetiracetam is a new generation of anti‐epileptic drug. It has been associated with very infrequent and only mild side effects in people, dogs and cats. The dose is 10–20mg/kg three times daily. The rare side effects reported are salivation, transient sedation and inappetence. The majority of the levetiracetam is excreted in the urine, and dose should be adjusted in the patient with impaired renal function. A recent study has shown that levetiracetam is a useful adjunctive treatment to phenobarbitone in reduction of seizure frequency (Smith Bailey and Dewey, 2009).
(9)
[ T2 weighted transverse MR image of the brain of a cat with MUA. CSF of the same cat with MUA with mononuclear pleocytosis ]
Gabapentin is another novel anti‐epileptic drug and can be used as both monotherapy and add‐on therapy. In dogs, gabapentin undergoes partial (approximately 30%) metabolism in the liver and is eliminated through the kidneys (Vollmer et al, 1986). Even if no specific data are available in cats, monitoring of renal function is recommended. The dose is 5–10 mg/kg two to three times a day. The most common adverse effect in cats is excessive sedation and ataxia (Podell, 2004).
Despite being used historically, diazepam should not be prescribed to cats due to the risk of potentially fatal idiosyncratic hepatotoxicity (Center et al, 1996). Instead, diazepam is the drug of choice in emergency seizuring cats. Intravenous and rectal diazepam has not been associated with this reaction and so can be used safely in the emergency treatment of seizures.
Bromide is generally not recommended in the treatment of feline seizures.
How do I monitor the effectiveness of the treatment?
It is important to monitor the response to treatment, and owners should be advised to keep an accurate seizure diary. In case of inadequate response to the treatment dose, owner's/cats compliance or the diagnosis should be re‐visited and additional investigation and treatment should be advised to the owners.
Despite appropriate treatment, some cats may experience occasional cluster seizures or even status epilepticus, which can be very distressing for the owners. Rectal administration of diazepam at the dose of 1–2 mg/kg as soon as seizures are noticed, or immediately after, is recommended as home treatment. If seizures continue or the cat is excessively sedated, emergency veterinary care should be sought (Dewey, 2008).
What is the prognosis for a seizuring cat?
In conclusion, prognosis for the seizuring cat depends on the final diagnosis, and, generally, cats with primary idiopathic epilepsy have a longer survival time than cats with the epilepsy with an underlying severe pathology (symptomatic epilepsy) (Schriefl et al, 2008).
KEY POINTS
-
•
Even if primary epilepsy exists in the cat, the underlying cause of the seizures should be always ruled out
-
•
If identified, the underlying disease of the seizure should be treated as soon as possible
-
•
The logical clinical approach in identifying the underlying cause in the seizuring cats can be very rewarding, even without any advanced tools and a need for referral
-
•
The first line anti‐epileptic drug for cats is phenobarbitone
-
•
Anti‐epileptic treatment only controls the seizures—it does not address the underlying cause. The thorough neurological work‐up should be performed prior to the to commencement of the anti‐epileptic treatment
-
•
If the primary epilepsy is diagnosed in cats, the prognosis is generally good with appropriate anti‐epileptic management.
Continuing Professional Development
In order to test your understanding of this article, answer these multiple choice questions, or if you are a subscriber, go online at http://www.ukvet.co.uk, and find many more multiple choice questions to test your understanding.
Adjunctive tests
-
1)
What is the one of the side effects reported with Phenobarbitone in cats:
a. Trombocytopenia
b. Excessive salivation
c. Allergic asthma
d. Hypertension
-
2)
The most common infectious cause of feline seizures is:
a. Toxoplasmosis
b. Bartonellosis
c. Feline parvovirus
d. Feline infectious peritonitis
-
3)
The first line AED treatment is:
a. Potassium bromide
b. Gabapentin
c. Phenobarbitone
d. Levetiracetam
For answers please see page 354
Supporting Information
Additional Supporting Information may be found in the online version of this article:
S1: Continuing Professional Development – Answers.
Supporting information
Please note: Wiley‐Blackwell are not responsible for the content or functionality of any supporting information supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
Supporting info item
References
- Baho MJ, Hostutler R, Fenner W et al (2011) J Am Vet Med Assoc 238(3): 353–5. [DOI] [PubMed] [Google Scholar]
- Boland LA, Angles JM (2010) Feline permethrin toxicity: retrospective study of 42 cases. J Feline Med Surg 12(2): 61–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown SC (2005) Pathophysiology of systemic hypertension In: Ettinger SJ, Feldman EC. Eds, Textbook of Veterinary Internal Medicine. Saunders Elsevier, St. Louis : : 472–9. [Google Scholar]
- Boothe DM, George KL, Couch P (2002) Disposition and clinical use of bromide in cats. J Am Vet Med Assoc 221(8): 1131–5. [DOI] [PubMed] [Google Scholar]
- Center SA, Elston TH, Rowland PH et al (1996) Fulminant hepatic failure associated with oral administration of diazepam in 11 cats. J Am Vet Med Assoc 209(3): 618–25. [PubMed] [Google Scholar]
- Dewey CW (2008) Encephalopathies: Disorders of the Brain In: Dewey CW. Ed, A Practical Guide to Canine and Feline Neurology. Wiley‐Blackwell, Iowa : 115–220. [Google Scholar]
- Ducote JM, Coates JR, Dewey CW (1999) Suspected hypersensitivity to phenobarbital in a cat. J Feline Med Surg 1(2): 123–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline K (1998) Feline Epilepsy. Clin Tech Small Anim Pract 13(3): 152–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palus V, Penderis J, Jakovljevic S et al (2010) Thiamine deficiency in a cat: resolution of MRI abnormalities following thiamine supplementation. J Feline Med Surg 12(10): 807–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Podell M (2004) Seizures In: Platt SR, Olby NJ. eds, BSAVA Manual of Canine and Feline Neurology. British Small Animal Veterinary Association, Quedgeley : 97–112. [Google Scholar]
- Quesnel AD, Parent JM, McDonell W et al (1997) Diagnostic evaluation of cats with seizure disorders: 30 cases (1991–1993). J Am Vet Med Assoc 210(1): 65–71. [PubMed] [Google Scholar]
- Schmied O, Scharf G, Hilbe M et al (2008) Magnetic resonance imaging of feline hippocampal necrosis. Vet Radiol Ultrasound 49(4): 343–9. [DOI] [PubMed] [Google Scholar]
- Schriefl S, Steinberg TA, Matiasek K et al (2008) Etiologic classification of seizures, signalment, clinical signs, and outcome in cats with seizure disorders: 91 cases (2000–2004). J Am Vet Med Assoc 233(10): 1591–7. [DOI] [PubMed] [Google Scholar]
- Smith Bailey K, Dewey CW (2009) The seizuring cat. Diagnostic work‐up and therapy. J Feline Med Surg 11(5): 385–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinmetz S, Brauer C, Rohn K et al (2010) Posttraumatic epilepsy in dogs and cats: Proceedings of ECVN‐ESVN Annual Symposium 2010. European Society of Veterinary Neurology‐European College of Veterinary Neurology. [Google Scholar]
- Summers BA, Cummings JF, DeLahunta A (1995) Malformations of the Central Nervous System In: Summers BA, Cummings JF, DeLahunata A. eds, Veterinary Neuropathology. Mosby‐Year Book, St Louis : 68–94. [Google Scholar]
- Timmann D, Cizinauskas S, Tomek A et al (2008) Retrospective analysis of seizures associated with feline infectious peritonitis in cats. J Feline Med Surg 10(1): 9–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomek A, Cizinauskas S, Doherr M et al (2006) Intracranial neoplasia in 61 cats: localisation, tumour type and seziure patterns. J Feline Med Surg 8(4): 243–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troxel MT, Vite CH, Van Winkle TJ et al (2003) Feline Intracranial Neoplasia: Retrospective Review of 160 Cases (1985–2001). J Vet Intern Med 17(6): 850–9. [DOI] [PubMed] [Google Scholar]
- Vollmer KO, von Hodenberg A, Kölle EU (1986) Pharmacokinetics and metabolism of gabapentin in rat, dog and man. Arzneimittelforschung 36(5): 830–9. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Please note: Wiley‐Blackwell are not responsible for the content or functionality of any supporting information supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
Supporting info item



