Abstract
Purpose
To investigate whether microsurgical excision of trabecular meshwork (TM) in an ex vivo pigmentary glaucoma model can normalize the hypertensive phenotype.
Methods
Eight eyes of a porcine pigmentary glaucoma model underwent 90° of microsurgical TM excision with an aspirating dual-blade (Goniotome (G)). 24 hours later, additional 90° of TM were removed. Anterior segments with sham surgeries served as the control (C). Outflow facility and intraocular pressure (IOP) were analyzed. Histology with hematoxylin and eosin (H&E) was obtained.
Results
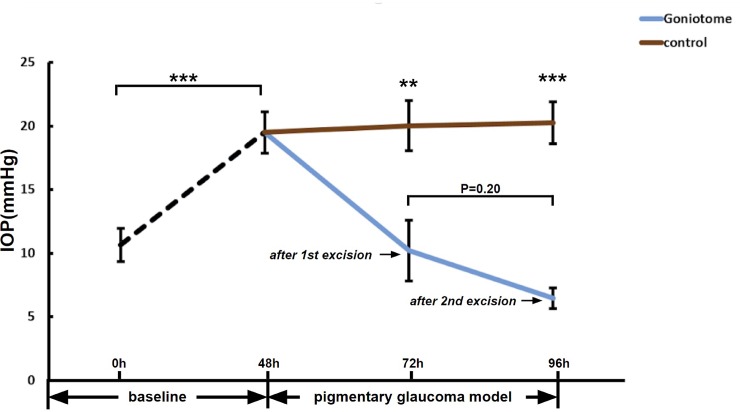
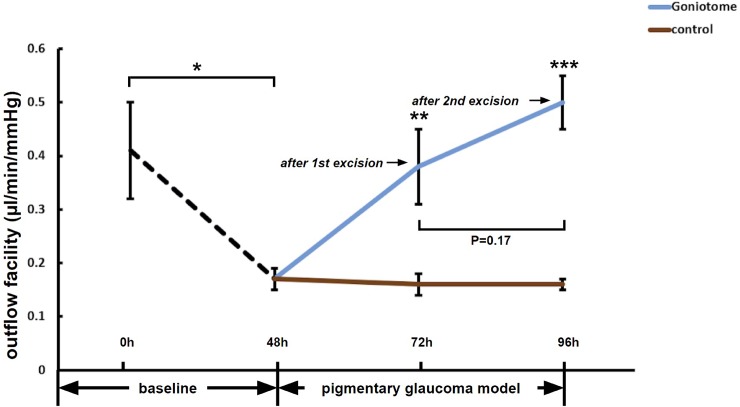
After the first 90° TM excision, IOP was significantly lower in G (10.2±2.4 mmHg, n = 7) than C (20.0±2.0mmHg, n = 8, P<0.01). Outflow facility in G (0.38±0.07 μl/min/mmHg) was higher than C (0.16±0.02 μl/min/mmHg, P<0.01). After the second 90° TM excision, IOP in G (6.46±0.81 mmHg, n = 7) was significantly lower than C (20.3±1.7 mmHg, n = 8, P<0.001), while the outflow facility in G (0.50±0.05 μl/min/mmHg, n = 7) was higher than C (0.16±0.01 μl/min/mmHg, n = 8, P<0.001). Compared to the first excision, excision of an additional 90° did not change of IOP (P = 0.20) or outflow facility (P = 0.17) further.
Conclusions
Excision of 90° of TM in a pigmentary glaucoma model using an aspirating dual-blade decreased IOP and increased outflow facility.
Introduction
Pigment dispersion syndrome (PDS) can lead to pigmentary glaucoma (PG), a form of secondary open-angle glaucoma, which often affects nearsighted individuals in their 30s to 40s [1, 2]. The prevalence of PDS is as high as 2.5% in the general population and incurs a risk of 15% of PG within 15 years [3]. In PDS, the iris releases cellular debris that contains pigment granules which accumulate in the trabecular meshwork (TM), on the corneal endothelium in the form of the Krukenberg spindle, on the lens surface, and elsewhere [4]. The pathogenesis of PDS is poorly understood, but several mutations or variants of more than one gene seem to contribute with a susceptibility locus at 7q35–q36 [5]. Cytoskeletal and structural TM changes [6] can make PG more challenging to treat medically or by laser [2]. These challenges include IOP spikes and a reduced success rate after trabeculoplasty in heavily pigmented eyes [7, 8]. After a first trabeculoplasty, the need for a second laser or operating room procedure is twice as high in eyes with pigmentary glaucoma [9]. Mid-peripheral iris transillumination defects can be seen early in the course of the disease, which can progress to more extensive iris atrophy.
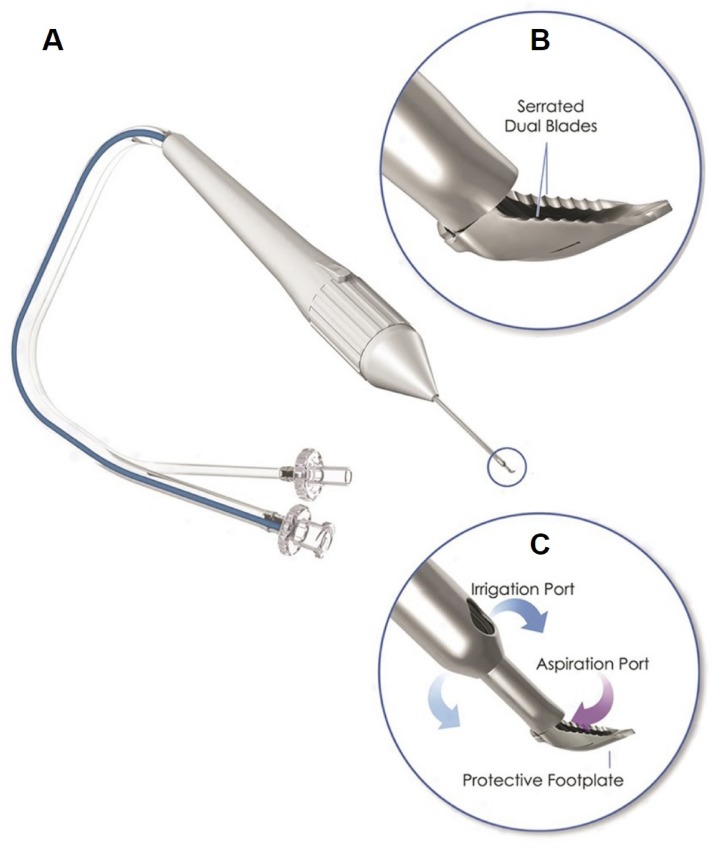
Trabecular ablation, for instance, by Trabectome surgery (Neomedix Corp., Tustin, California, United States), can be effective in a range of glaucoma disease stages [10–15] which makes it well suited for PG. Ab interno angle surgeries rely on maintaining the anterior chamber either passively with a viscoelastic device [16, 17] or actively, using an irrigation and aspiration (I&A) system [18, 19]. The advantages of a clear angle view and anterior chamber stability have recently become more readily available with an I&A-equipped dual-blade (Goniotome, Neomedix Corp., Tustin, California, United States). This device does not require a high-frequency generator to molecularize the TM and instead excises a strip of TM tissue [16, 20]. These features and its ability to excise TM in a controlled environment and to harvest it non-destructively make it also useful for glaucoma research.
In the present study, we hypothesized that trabecular excision with an I&A-equipped dual-blade device could also restore outflow by removing the pathology. We have extensive experience studying outflow in experimental systems [21, 22], including gene transfer [23–29], disease modeling [6, 30, 31] and surgical outflow enhancement [16, 17, 20, 32–35], but this is the first study of a microsurgical intervention for glaucoma in an ex vivo model of glaucoma.
Materials and methods
Pig eye perfusion culture and pigmentary dispersion glaucoma model
Sixteen porcine eyes were obtained from a local abattoir (Thoma Meat Market, Saxonburg, PA) as left-right matched pairs and were processed within two hours of sacrifice. Our Institutional Animal Care and Use Committee (IACUC) assessed that an IACUC protocol, approval or waiver was not required because no animals were sacrificed for the purpose of doing research. After the removal of extraocular tissues, the eyes were decontaminated in 5% povidone-iodine solution (3955–16, Ricca Chemical Company, Arlington, TX 786012) for two minutes and irrigated three times with phosphate-buffered saline (PBS). The posterior segment, lens, iris, and ciliary body were carefully removed. Anterior segments with intact TM were mounted in perfusion dishes as described before [36]. The perfusion media consisted of Dulbecco's modified Eagle media (DMEM, SH30284, HyClone, GE Healthcare, UK) supplemented with 1% fetal bovine serum (FBS, 10438026, Thermo Fisher Scientific, Waltham, MA) and 1% antibiotic/antimycotic (15240062, Thermo Fisher Scientific, Waltham, MA) at a constant rate of 3 μl/min using a microinfusion pump (PHD 22/2000; Harvard Apparatus, Holliston, MA).
A suspension of pigment granules was generated with freeze-thaw cycles, as described previously [6]. In brief, the irises of 10 decontaminated porcine eyes were isolated, frozen at -80C° for two hours, and thawed at room temperature for 2 hours. This process was performed twice to lyse cells and release pigment granules. The lysate was suspended in 15 mL PBS and aspirated and expelled 20 times to promote further pigment release. After filtering through a 70-μm cell strainer (431751, Corning Incorporated, Durham, NC), the suspension was centrifuged at 3000 rpm for 15 minutes. The supernatant was discarded, and the pigment was resuspended in 15 ml PBS. The centrifugation and resuspension steps were repeated four times. The pigment pellet was resuspended in 4 mL PBS for pigment stock solution. The stock solution was diluted 1000-fold, and concentration was determined with a hemocytometer, using 600x magnification (Eclipse TE200-E, Nikon Instruments Inc., Melville, NY). Pigment granules were added to perfusion media after 48h of IOP stabilization, at a concentration of 1.67×107 particles/mL. The IOP was measured with pressure transducers (SP844; MEMSCAP, Skoppum, Norway) and recorded every two minutes (LabChart, ADInstruments, Colorado Springs, CO).
Trabecular meshwork excision
When the hypertensive plateau was established, the TM in experimental group G was excised with the Goniotome (Neomedix Corp., Tustin, CA, United States, Fig 1). A single surgeon (NAL) with comprehensive experience in ab interno trabeculectomy performed the procedures. The inverted anterior segments were positioned under a surgical microscope (S4, Carl Zeiss Meditec, Jena, Germany). The tip of the instrument was inserted into the TM, and aspiration was started, causing the serrated dual-blades to engage and excise the TM. The excision was continued 90° to the left, and the excised TM strip was cut by angulating the tip of the Goniotome. After 24 hours, an additional 90° of the TM was removed using the same procedure with an excision path in the opposite direction. Control eyes in group C underwent a sham procedure meant to mimic irrigation and aspiration. Irrigation and aspiration are part of a procedure termed “trabecular aspiration” that has been observed to remove pigmentary debris and induce trabecular meshwork remodeling with a small and transient IOP reduction [37]. As in group G, the Goniotome was placed into the inverted anterior segment under the microscope. Irrigation and aspiration were started, and movements along the TM 90 degrees into each direction were made but without touching the TM.
Fig 1. Goniotome surgical system.
The Goniotome has two irrigation ports that maintain the chamber (C, blue arrows). The TM is put under stretch by a ramp and excised. TM, blood, and debris are aspirated into the tip (C, red arrow).
Histology
After the perfusion culture experiments, the anterior segments were fixed with 4% paraformaldehyde for 24 hours, rinsed, embedded in paraffin, and sectioned at a thickness of 6 microns. Hematoxylin and eosin staining was performed for gross histological evaluation.
Statistics
Data were reported as the mean ± standard error unless stated otherwise. A one-way ANOVA was used to compare the data for different groups at individual time points. Paired t-tests were used for an in-group comparison of IOP and outflow facility before and after treatment (PASW 18.0, SPSS, Armonk, New York, United States). Differences were considered statistically significant for P<0.05. IOPs were averaged over 6 hours following excision. Media and dish handling were scheduled to occur outside of these periods to avoid artifacts. The outflow facility was computed using the Goldmann equation, assuming that the episcleral venous pressure is near zero, Po = (F/C) + Pv (Po: IOP, F: rate of aqueous formation, C: outflow facility, Pv: episcleral venous pressure).
The minimum number of eyes for an adequate testing power was determined with a sample size calculator. A minimum sample size of three was required to detect at least an 18% IOP reduction [38] with an alpha of 0.05 and a power of 0.80, given the historical baseline facility of 0.25+/- 0.06 [6]. Our perfusion system allows us to run eight eyes in parallel, and this number was chosen for sufficient redundancy.
Results
Sixteen porcine eyes were used (eight eyes in C, and eight eyes in G). One eye in G was excluded due to a transducer error. After 48h of perfusion, a stable baseline IOP of 10.7±1.3 mmHg (all eyes) was achieved without a significant difference in IOP between C (11.4±0.6) mmHg and G (9.8±2.7 mmHg; C versus G: P = 0.54). After 48h of pigment perfusion to establish the pigmentary glaucoma model, IOP increased by 82% to a plateau at 19.5±1.6 mmHg (all eyes, P<0.001). At this point, pretreatment IOP in C (21.6±2.6 mmHg) was similar to G (17.7±2.0 mmHg, P = 0.24). The first TM excision in G reduced the IOP to 10.2±2.4 mmHg (n = 7) 24 hours later compared to 20.0±2.0 mmHg in C (n = 8, P<0.01). The second TM excision, now had an average in G of only 6.5±0.8 mmHg, (n = 7, P = 0.20) compared to 20.3±1.7 mmHg (n = 8, P<0.001) in C (Fig 2). The first excision resulted in an IOP reduction of 48% and the second one in an IOP reduction of 67% compared to the hypertensive baseline.
Fig 2. IOP reduction after TM excision.
After 48h perfusion with pigment, IOP in PG was significantly higher compared to baseline (n = 15, ***P<0.001). Twenty-four hours after a 90° excision of TM (G), IOP in G (n = 7) was lower than in C (n = 8, **P<0.01). Twenty-four hours after a second, adjacent excision of 90° TM, IOP in G appeared to slightly reduce further (n = 7, P>0.05) remaining lower than C (n = 8, ***P<0.001).
After 48h of perfusion, the baseline outflow facility was stable (0.41±0.09, n = 15). After 48h of pigment perfusion, the outflow facility of PG (0.17±0.02, n = 15, P<0.05) was significantly decreased from baseline. 24 hours after the first 90° of TM excision, outflow facility in G (0.38±0.07 μl/min/mmHg, n = 7) was higher than C (0.16±0.02 μl/min/mmHg, n = 8, P<0.01). Twenty-four hours after the second TM excision, outflow facility in G (0.50±0.05 μl/min/mmHg, n = 7) was higher than C (0.16±0.01 μl/min/mmHg, n = 8, P<0.001), but there was no significant further increase in outflow facility after second TM excision (Fig 3), compared with the outflow facility after first TM excision (P = 0.17).
Fig 3. Increased outflow facility after TM excision.
The outflow facility of PG was decreased from baseline (n = 15,*P<0.05) after 48 hours of perfusion with pigment. Twenty-four hours after the first 90° TM excision, the outflow facility in G (n = 7) increased compared to C (n = 8, **P<0.01). Twenty-four hours after the second 90° excision, the outflow facility in G (n = 7) remained significantly higher than C (n = 8, ***P<0.001).
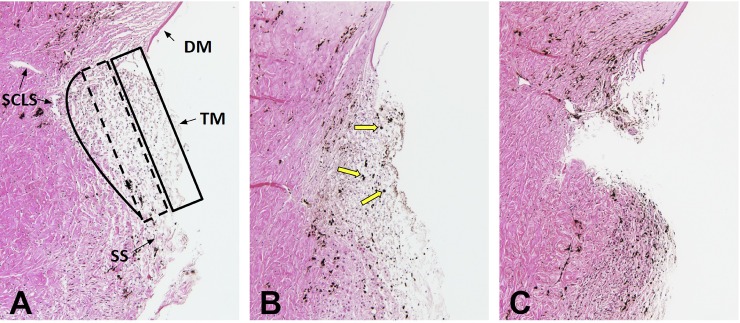
The control TM appeared as a thick, multilayered structure consisting of the uveal, the corneoscleral, and the juxtacanalicular meshwork (Fig 4A). Pigs have an angular aqueous plexus without a single lumen Schlemm’s canal characteristic for primate eyes. Instead, smaller, Schlemm’s canal-like segments (SCLS) adjacent to the juxtacanalicular meshwork could be made out. The normal TM was lightly pigmented (Fig 4A). After perfusion with pigment-supplemented media for 48 hours, pigment granules were present in the TM at a density of approximately 10,000-fold below the amount expected to cause a physical obstruction [39]. The pigment granules were seen throughout the TM (Fig 4B, yellow arrows). After the TM excision with the Goniotome, a full-thickness portion of TM appeared removed without damage to the adjacent sclera or corneal endothelium (Fig 4C). In comparison to the smaller human TM that can be removed in its entirety, remnants of adjacent TM remained.
Fig 4. Histology.
Normal TM was lightly pigmented and consisted of three areas with different compactness and cell densities: the uveal meshwork (box with solid line, A), the corneoscleral meshwork (box with dashed line, Fig 4A), and the juxtacanalicular meshwork (solid line, A) adjacent to small canal-like segments characteristic of the porcine angular aqueous plexus (SCLS). Pigment granules were observed in all layers of TM (B, yellow arrows) after perfusion with pigment-supplemented media. After TM excision, a large, full-thickness portion of TM was removed (C). Trabecular meshwork: TM, Schlemm’s canal-like segments (SCLS) of the porcine angular aqueous plexus, scleral spur (SS), Descemet's membrane (DM).
Discussion
This is the first study of a microincisional intervention in an ex vivo model of glaucoma. We found that trabecular excision with a novel dual-blade device, the Goniotome, induces a 52.5% IOP reduction after only 90° of TM are removed. Additional TM excision did not significantly lower the IOP. This finding is concurrent with the clinical observation in human eyes that the length of TM ablation beyond 90° does not lower IOP more even though it might improve the chances of successfully connecting to working collector channels [40, 41]. Pig eyes do not have a single, contiguous Schlemm’s canal, yet a circumferential flow pattern can be observed here as well [22, 32].
The trabecular meshwork and the inner wall of Schlemm’s canal are primary sites of outflow resistance in primary open angle glaucoma [42], but distal outflow resistance also appears to play a role [43, 44]. In contrast, secondary open angle glaucomas are caused by pathologies mostly limited to the TM and respond well to ab interno trabeculectomy [45–48]. Pigmentary glaucoma is such a secondary glaucoma and tends to present with a relatively high mean IOP of 30 mmHg with a range from 24 to 56 mmHg [3, 49]. The mechanism of outflow compromise in PG is not a simple mechanical obstruction but seems due to a rearrangement and contraction of the TM actin cytoskeleton [30]. The phagocytic overload eventually leads to TM cell death, and collapse and fusion of denuded trabecular beams [50, 51].
Recent evidence points towards a central role of RhoA in regulating the cytoskeleton, motility, and phagocytosis of TM cells in PG [6, 52]. Ocular hypertension emerges as soon as cytoskeletal changes occur, and before phagocytosis declines [30]. We found that a Rho-kinase inhibitor can relax the contracted cytoskeleton and normalize outflow in an ex vivo PG model [31]. In a separate study, we observed that Rho-kinase inhibitors could cause an IOP reduction independent of the TM by dilating the distal outflow vessels. Gottanka et al. described downstream changes in PG that included star-shaped cells migrated away from the TM with an accompanying loss of connecting fibrils [51]. Neither we nor Gottanka et al. nor Alvarado et al. in an earlier study [50] found pigment downstream of the TM. The fact that TM excision in our study increases the facility to a supraphysiological level points again to the TM as the principal pathology.
Non-surgical treatment of PG is challenging [2, 53], and in the past, about 35% of all PG patients needed traditional filtering surgery to control IOP [54]. The safety and efficacy of ab interno trabeculectomy are especially attractive for younger patients, including ones affected by PG. As seen in this model, the continued pigment dispersion does not appear to block exposed collector channel orifices or cause a subsequent IOP rise.
There are several limitations to our study. We used an ex vivo model, so immunologic responses, changes of the distal outflow tract distal, and wound healing processes that could affect the IOP, are not taken into account. The observation time as relatively brief. Moreover, there are anatomical differences between human and porcine eyes that may result in a different IOP response.
In conclusion, in this porcine ex vivo PG model, Goniotome surgery caused a 52.5% IOP reduction after removal of 90° of TM.
Supporting information
(PDF)
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
This work was supported by NIH grant K08-EY022737 (NAL), NIH CORE Grant P30 EY08098 to the Department of Ophthalmology, the Initiative to Cure Glaucoma of the Eye and Ear Foundation of Pittsburgh (NAL), the Wiegand Fellowship (YD), an unrestricted grant from Research to Prevent Blindness, New York, NY and an unrestricted fellowship grant from the Third Xiangya Hospital of Central South University (CW)
References
- 1.De Moraes CG, Susanna R Jr (2016) Glaucomas: Pigment Dispersion Syndrome, Pigmentary Glaucoma, and Angle Recession Glaucoma. In: Giaconi JA, Law SK, Nouri-Mahdavi K, et al. (eds) Pearls of Glaucoma Management Springer Berlin Heidelberg, pp 419–430 [Google Scholar]
- 2.Niyadurupola N, Broadway DC (2008) Pigment dispersion syndrome and pigmentary glaucoma—a major review. Clin Experiment Ophthalmol 36:868–882 10.1111/j.1442-9071.2009.01920.x [DOI] [PubMed] [Google Scholar]
- 3.Siddiqui Y, Ten Hulzen RD, Cameron JD, et al. (2003) What is the risk of developing pigmentary glaucoma from pigment dispersion syndrome? Am J Ophthalmol 135:794–799 10.1016/s0002-9394(02)02289-4 [DOI] [PubMed] [Google Scholar]
- 4.Ritch R, Steinberger D, Liebmann JM (1993) Prevalence of pigment dispersion syndrome in a population undergoing glaucoma screening. Am J Ophthalmol 115:707–710 10.1016/s0002-9394(14)73635-9 [DOI] [PubMed] [Google Scholar]
- 5.Andersen JS, Pralea AM, DelBono EA, et al. (1997) A gene responsible for the pigment dispersion syndrome maps to chromosome 7q35-q36. Arch Ophthalmol 115:384–388 10.1001/archopht.1997.01100150386012 [DOI] [PubMed] [Google Scholar]
- 6.Dang Y, Waxman S, Wang C, et al. (2018) A porcine ex vivo model of pigmentary glaucoma. Sci Rep 8:5468 10.1038/s41598-018-23861-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Damji KF, Bovell AM, Hodge WG, et al. (2006) Selective laser trabeculoplasty versus argon laser trabeculoplasty: results from a 1-year randomised clinical trial. Br J Ophthalmol 90:1490–1494 10.1136/bjo.2006.098855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harasymowycz PJ, Papamatheakis DG, Latina M, et al. (2005) Selective laser trabeculoplasty (SLT) complicated by intraocular pressure elevation in eyes with heavily pigmented trabecular meshworks. Am J Ophthalmol 139:1110–1113 10.1016/j.ajo.2004.11.038 [DOI] [PubMed] [Google Scholar]
- 9.Koucheki B, Hashemi H (2012) Selective laser trabeculoplasty in the treatment of open-angle glaucoma. J Glaucoma 21:65–70 10.1097/IJG.0b013e3182027596 [DOI] [PubMed] [Google Scholar]
- 10.Bussel II, Kaplowitz K, Schuman JS, et al. (2015) Outcomes of ab interno trabeculectomy with the trabectome after failed trabeculectomy. Br J Ophthalmol 99:258–262 10.1136/bjophthalmol-2013-304717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Parikh HA, Bussel II, Schuman JS, et al. (2016) Coarsened Exact Matching of Phaco-Trabectome to Trabectome in Phakic Patients: Lack of Additional Pressure Reduction from Phacoemulsification. PLoS One 11:e0149384 10.1371/journal.pone.0149384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Neiweem AE, Bussel II, Schuman JS, et al. (2016) Glaucoma Surgery Calculator: Limited Additive Effect of Phacoemulsification on Intraocular Pressure in Ab Interno Trabeculectomy. PLoS One 11:e0153585 10.1371/journal.pone.0153585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roy P, Loewen RT, Dang Y, et al. (2017) Stratification of phaco-trabectome surgery results using a glaucoma severity index in a retrospective analysis. BMC Ophthalmol 17:30 10.1186/s12886-017-0421-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Loewen RT, Roy P, Parikh HA, et al. (2016) Impact of a Glaucoma Severity Index on Results of Trabectome Surgery: Larger Pressure Reduction in More Severe Glaucoma. PLoS One 11:e0151926 10.1371/journal.pone.0151926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dang Y, Roy P, Bussel II, et al. (2016) Combined analysis of trabectome and phaco-trabectome outcomes by glaucoma severity. F1000Res 5:762 10.12688/f1000research.8448.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang C, Dang Y, Waxman S, et al. (2017) Angle stability and outflow in dual blade ab interno trabeculectomy with active versus passive chamber management. PLoS One 12:e0177238 10.1371/journal.pone.0177238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Parikh HA, Loewen RT, Roy P, et al. (2016) Differential Canalograms Detect Outflow Changes from Trabecular Micro-Bypass Stents and Ab Interno Trabeculectomy. Sci Rep 6:34705 10.1038/srep34705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kaplowitz K, Schuman JS, Loewen NA (2014) Techniques and outcomes of minimally invasive trabecular ablation and bypass surgery. Br J Ophthalmol 98:579–585 10.1136/bjophthalmol-2013-304256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kaplowitz K, Bussel I, Loewen NA (2013) Minimally Invasive and Nonpenetrating Glaucoma Surgeries. In: Yanoff M, Duker JS (eds) Ophthalmology: Expert Consult: Online and Print. Elsevier—Health Sciences Division, pp 1133–1146 [Google Scholar]
- 20.Dang Y, Wang C, Shah P, et al. (2018) Outflow enhancement by three different ab interno trabeculectomy procedures in a porcine anterior segment model. Graefes Arch Clin Exp Ophthalmol. 10.1007/s00417-018-3990-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fautsch MP, Bahler CK, Vrabel AM, et al. (2006) Perfusion of his-tagged eukaryotic myocilin increases outflow resistance in human anterior segments in the presence of aqueous humor. Invest Ophthalmol Vis Sci 47:213–221 10.1167/iovs.05-0334 [DOI] [PubMed] [Google Scholar]
- 22.Loewen RT, Brown EN, Roy P, et al. (2016) Regionally Discrete Aqueous Humor Outflow Quantification Using Fluorescein Canalograms. PLoS One 11:e0151754 10.1371/journal.pone.0151754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Loewen RT, Roy P, Park DB, et al. (2016) A Porcine Anterior Segment Perfusion and Transduction Model With Direct Visualization of the Trabecular Meshwork. Invest Ophthalmol Vis Sci 57:1338–1344 10.1167/iovs.15-18125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dang Y, Loewen R, Parikh HA, et al. (2016) Gene transfer to the outflow tract. Exp Eye Res 044396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang Z, Dhaliwal AS, Tseng H, et al. (2014) Outflow tract ablation using a conditionally cytotoxic feline immunodeficiency viral vector. Invest Ophthalmol Vis Sci 55:935–940 10.1167/iovs.13-12890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Loewen N, Fautsch MP, Peretz M, et al. (2001) Genetic modification of human trabecular meshwork with lentiviral vectors. Hum Gene Ther 12:2109–2119 10.1089/10430340152677449 [DOI] [PubMed] [Google Scholar]
- 27.Loewen N, Bahler C, Teo W-L, et al. (2002) Preservation of aqueous outflow facility after second-generation FIV vector-mediated expression of marker genes in anterior segments of human eyes. Invest Ophthalmol Vis Sci 43:3686–3690 [PubMed] [Google Scholar]
- 28.Khare PD, Loewen N, Teo W, et al. (2008) Durable, safe, multi-gene lentiviral vector expression in feline trabecular meshwork. Mol Ther 16:97–106 10.1038/sj.mt.6300318 [DOI] [PubMed] [Google Scholar]
- 29.Loewen N, Fautsch MP, Teo W-L, et al. (2004) Long-term, targeted genetic modification of the aqueous humor outflow tract coupled with noninvasive imaging of gene expression in vivo. Invest Ophthalmol Vis Sci 45:3091–3098 10.1167/iovs.04-0366 [DOI] [PubMed] [Google Scholar]
- 30.Dang Y, Waxman S, Wang C, et al. (2018) Intraocular pressure elevation precedes a phagocytosis decline in a model of pigmentary glaucoma. F1000Res 7.: 10.12688/f1000research.13797.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dang Y, Wang C, Shah P, et al. (2018) RKI-1447, a Rho-Kinase Inhibitor Causes Ocular Hypotension, Actin Stress Fiber Disruption and Increased Phagocytosis. Graefes Arch Clin Exp Ophthalmol (in press) 1–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Loewen RT, Brown EN, Scott G, et al. (2016) Quantification of Focal Outflow Enhancement Using Differential Canalograms. Invest Ophthalmol Vis Sci 57:2831–2838 10.1167/iovs.16-19541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fallano K, Bussel I, Kagemann L, et al. (2017) Training strategies and outcomes of ab interno trabeculectomy with the trabectome. F1000Res 6:67 10.12688/f1000research.10236.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dang Y, Waxman S, Wang C, et al. (2017) Rapid learning curve assessment in an ex vivo training system for microincisional glaucoma surgery. Sci Rep 7:1605 10.1038/s41598-017-01815-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Oatts JT, Zhang Z, Tseng H, et al. (2013) In vitro and in vivo comparison of two suprachoroidal shunts. Invest Ophthalmol Vis Sci 54:5416–5423 10.1167/iovs.13-11853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dang Y, Waxman S, Wang C, et al. (2017) Freeze-thaw decellularization of the trabecular meshwork in an ex vivo eye perfusion model. PeerJ 5:e3629 10.7717/peerj.3629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jacobi PC, Dietlein TS, Krieglstein GK (2000) Effect of trabecular aspiration on intraocular pressure in pigment dispersion syndrome and pigmentary glaucoma. Ophthalmology 107:417–421 10.1016/s0161-6420(99)00091-3 [DOI] [PubMed] [Google Scholar]
- 38.Kaplowitz K, Bussel II, Honkanen R, et al. (2016) Review and meta-analysis of ab-interno trabeculectomy outcomes. Br J Ophthalmol 100:594–600 10.1136/bjophthalmol-2015-307131 [DOI] [PubMed] [Google Scholar]
- 39.Epstein DL, Freddo TF, Anderson PJ, et al. (1986) Experimental obstruction to aqueous outflow by pigment particles in living monkeys. Invest Ophthalmol Vis Sci 27:387–395 [PubMed] [Google Scholar]
- 40.Khaja HA, Hodge DO, Sit AJ (2008) Trabectome Ablation Arc Clinical Results and Relation to Intraocular Pressure. Invest Ophthalmol Vis Sci 49:4191–4191 [Google Scholar]
- 41.Hunter KS, Fjield T, Heitzmann H, et al. (2014) Characterization of micro-invasive trabecular bypass stents by ex vivo perfusion and computational flow modeling. Clin Ophthalmol 8:499–506 10.2147/OPTH.S56245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tamm ER, Ethier CR (2009) Current aspects of aqueous humor dynamics and glaucoma. Exp Eye Res 88:618–619 [DOI] [PubMed] [Google Scholar]
- 43.McDonnell F, Dismuke WM, Overby DR, Stamer WD (2018) Pharmacological regulation of outflow resistance distal to Schlemm’s canal. Am J Physiol Cell Physiol 315:C44–C51 10.1152/ajpcell.00024.2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Waxman S, Wang C, Dang Y, et al. (2018) Structure–Function Changes of the Porcine Distal Outflow Tract in Response to Nitric Oxide. Invest Ophthalmol Vis Sci 59:4886–4895 10.1167/iovs.18-24943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ting JLM, Damji KF, Stiles MC, Trabectome Study Group (2012) Ab interno trabeculectomy: outcomes in exfoliation versus primary open-angle glaucoma. J Cataract Refract Surg 38:315–323 10.1016/j.jcrs.2011.08.043 [DOI] [PubMed] [Google Scholar]
- 46.Kaplowitz K, Loewen NA (2015) Trabectome-Mediated Ab Interno Trabeculectomy for Secondary Glaucoma or as a Secondary Procedure. In: Advanced Glaucoma Surgery Springer, Cham, pp 15–29 [Google Scholar]
- 47.Ngai P, Kim G, Chak G, et al. (2016) Outcome of primary trabeculotomy ab interno (Trabectome) surgery in patients with steroid-induced glaucoma. Medicine 95:e5383 10.1097/MD.0000000000005383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dang Y, Kaplowitz K, Parikh HA, et al. (2016) Steroid-induced glaucoma treated with trabecular ablation in a matched comparison with primary open-angle glaucoma. Clin Experiment Ophthalmol 44:783–788 10.1111/ceo.12796 [DOI] [PubMed] [Google Scholar]
- 49.Sugar HS (1966) Pigmentary glaucoma. A 25-year review. Am J Ophthalmol 62:499–507 10.1016/0002-9394(66)91330-4 [DOI] [PubMed] [Google Scholar]
- 50.Alvarado JA, Murphy CG (1992) Outflow obstruction in pigmentary and primary open angle glaucoma. Arch Ophthalmol 110:1769–1778 10.1001/archopht.1992.01080240109042 [DOI] [PubMed] [Google Scholar]
- 51.Gottanka J, Johnson DH, Grehn F, Lütjen-Drecoll E (2006) Histologic findings in pigment dispersion syndrome and pigmentary glaucoma. J Glaucoma 15:142–151 10.1097/00061198-200604000-00011 [DOI] [PubMed] [Google Scholar]
- 52.Wang C, Dang Y, Loewen RT, et al. (2018) Impact of Pigment Dispersion on Trabecular Meshwork Cells. In press: Graefes Arch Clin Exp Ophthalmol. 1–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ritch R, Campbell DG, Camras C (1993) Initial treatment of pigmentary glaucoma. J Glaucoma 2:44–49 [PubMed] [Google Scholar]
- 54.Lehto I (1992) Long-term follow up of argon laser trabeculoplasty in pigmentary glaucoma. Ophthalmic Surg 23:614–617 [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.