We would like to express our concern about kidney transplant programmes during the coronavirus disease 2019 (COVID-19) pandemic. Although we recognise the importance of kidney transplants for dialysis patients, we cannot ignore the potential safety issues during this pandemic.
The limited accuracy of the RT-PCR test might lead to underdiagnosis of infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Weaknesses in the detection of SARS-CoV-2 infection have been identified in the pre-analytical phase (ie, collection, handling, transport and storage, and timing of the test) and in the analytical phase (ie, viral recombination, assay quality, harmonisation, and instrument performance).1 All these issues could result in a high risk of false-negative test results.2 Additionally, a Chinese study of chest CT in the diagnosis of COVID-19 infection reported positive RT-PCR assays in only 601 (59·3%) of 1014 patients with suspected infection.3 Among the 308 patients with baseline negative RT-PCR, 147 (47·7%) were reconsidered after the test as highly probable cases, and 103 (33·4%) as probable cases (based on symptoms, CT scan, and subsequent swab test), whereas only 58 (18·8%) patients were regarded as true negative cases. This high rate of negative results from RT-PCR in patients with radiological features typical of SARS-CoV-2 pulmonary infection raises doubts about test sensitivity in patients with no symptoms. Furthermore, the greatest likelihood of false-negative results was reported to be 5–7 days before onset of symptoms.1
With regard to transplant procedures, SARS-CoV-2 infection could be missed in both donors and recipients who are asymptomatic owing to the sensitivity issues with the RT-PCR test. RT-PCR with bronchoalveolar lavage in the donor might improve the accuracy of the test; however, this procedure would not be applicable to the recipient. The short time interval from notification that a kidney transplant can take place to the surgical procedure does not permit a test in the recipient. Furthermore, we do not have data on the sensitivity of multiple RT-PCR tests or RT-PCR tests with bronchoalveolar lavage in asymptomatic individuals. Additionally, in the immediate postoperative period and after hospital discharge, transplanted patients have increased susceptibility to SARS-CoV-2 infection owing to induction therapy and immunosuppressive treatment.
Scarce resources (eg, beds, operating theatres, medics, and nurses) might be an additional challenge for transplant services during this pandemic, in which many teams are deployed in the care of patients with COVID-19 patients; a logistical difficulty also exists in ensuring clean and microbiologically safe pathways within hospitals for transplant patients.
In our opinion, insufficient evidence is available to consider kidney transplantation as a safe procedure in COVID-19 pandemic areas. In emergency situations—eg, in cases of no vascular access, unfeasible dialysis, or a hyperimmune state—the benefits might outweigh the risks of a kidney transplant. Therefore, decisions should be made on a case-by-case basis, with concerns shared among the transplant team and patient after careful assessment of the risks and benefits. A pressing need exists to evaluate possible solutions to reduce the risk of kidney transplantation procedures during the COVID-19 pandemic, and for research to address the sensitivity issues of diagnostic tests for COVID-19. In the meantime, each case should be carefully discussed and scrutinised by the entire transplant team, and a dedicated consent form would help patients to make well informed decisions.
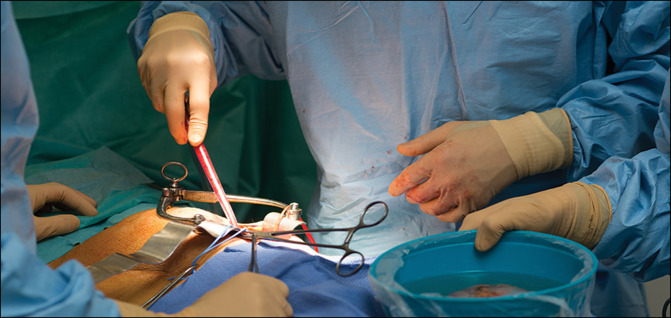
© 2020 A Noor/BSIP/Science Photo Library
Acknowledgments
We declare no competing interests.
References
- 1.Lippi G, Simundic AM, Plebani M. Potential preanalytical and analytical vulnerabilities in the laboratory diagnosis of coronavirus disease 2019 (COVID-19) Clin Chem Lab Med. 2020 doi: 10.1515/cclm-2020-0285. published online March 16. [DOI] [PubMed] [Google Scholar]
- 2.Wang W, Xu Y, Gao R. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. 2020 doi: 10.1001/jama.2020.3786. published online March 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ai T, Yang Z, Hou H. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020 doi: 10.1148/radiol.2020200642. published online Feb 26. [DOI] [PMC free article] [PubMed] [Google Scholar]