Highlights
-
•
HLH in adults can result in acute necrotizing encephalitis and severe hemorrhagic brain disease due to disseminated intravascular coagulation (DIC).
-
•
Observation of DIC in patients with HLH should prompt neuroimaging evaluation as brain hemorrhage is a potentialcomplication.
-
•
HLH (or CSS in COVID-19 patients) -related brain injury should be considered in patients with appropriate systemic manifestations as early diagnosis and treatment are crucial.
Keywords: Hemophagocytic syndrome, Adult onset Still’s disease, Acute necrotizing encephalopathy, Diffuse hemorrhagic encephalopathy, Disseminated intravascular coagulation
Abstract
The diagnosis of hemophagocytic lymphohistiocytosis (HLH) with cerebral involvement is challenging given the rarity of HLH and its resemblance to the much more common severe sepsis. Timely diagnosis and treatment may be lifesaving. We report two cases demonstrating different and rare forms of severe brain involvement in adult patients with HLH: acute necrotizing encephalopathy, and diffuse hemorrhagic disease due to disseminated intravascular coagulation. Severe HLH with brain involvement in adults is rare. HLH with cerebral involvement should be considered in patients presenting with severe systemic inflammatory response syndrome (SIRS) but negative cultures and unusual or unexpectedly severe clinical and/or radiologic signs of cerebral dysfunction. Similar brain injury may occur in patients with cytokine storm syndrome due to COVID-19.
Background
Hemophagocytic lymphohistiocytosis (HLH) presents with fevers, rash, organomegaly, cytopenia, and increased triglycerides and ferritin (Ramos-Casals et al., 2014) [1]. Neurologic abnormalities are reported in about one-third of patients (Cai et al., 2017), including a few cases of acute necrotizing encephalopathy (ANE) (Xiujuan et al., 2015). Coagulation abnormalities are frequent in HLH patients (Valade et al., 2015).
Objective
To raise awareness about the importance of early diagnosis and treatment of HLH with neurological involvement to prevent serious complications and demise.
1. Case report
1.1. Patient 1
A 46-year-old woman was admitted with a 3-month history of dyspnea, dysphagia and a generalized, maculopapular, and pruritic rash. She was febrile, tachycardic, and tachypneic. Neurological examination was normal.
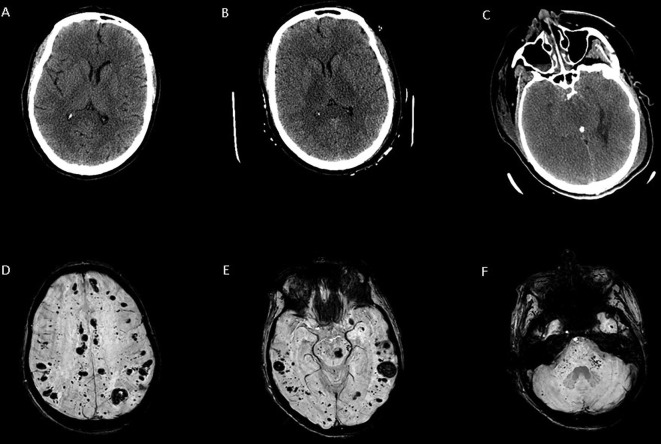
Her neurological status progressively worsened, and within 48 h she was alert, but followed no commands, anarthric, had significant spasticity, hyperreflexia and myoclonus. CT head (Fig. 1 A) and cerebrospinal fluid (CSF) analysis were unremarkable.
Fig. 1.
Axial CT images of the brain from Patient 1 (A–C) and susceptibility-weighted MR images of the brain from patient 2 (D–F). Panel A, (admission) is normal. Panel B (HD 3) shows prominent, bilaterally symmetric thalamic hypodensities. Panel C (HD 5) shows diffuse, severe cerebral edema. Panels D-F (HD 5) demonstrate innumerable microscopic and small hemorrhages involving nearly all brain regions, with a predilection for subcortical white matter and the middle cerebellar peduncles.
On hospital day (HD) 3, she developed coma with conjugate depressed gaze, intact brainstem reflexes and flexor posturing to pain. She was intubated and developed distributive shock. CT head showed bilateral symmetric thalamic hypodensities (Fig. 1B), consistent with ANE. Labs were markedly abnormal with thrombocytopenia, elevated creatinine, transaminitis, triglycerides of 1440 mg/dL, LDH of 1270 IU/L and ferritin of 40,000 ng/mL. Still’s disease with HLH was diagnosed based on Fautrel, Yamaguchi, and Henter criteria [5]. Bone marrow biopsy was consistent with HLH. Etoposide and high-dose dexamethasone were initiated.
On HD 5 she developed severe hypotension; bradycardia; fixed, dilated pupils; and absent lower brainstem reflexes and motor responses. CT head revealed diffuse, severe cerebral edema with central transtentorial and transforaminal herniation (Fig. 1C). Life support was discontinued. Posthumously, elevated soluble CD25 (5950 pg/mL, Ref <=1033) and phagocytic histiocytes on bone marrow biopsy (H-score 98%) confirmed HLH. Post-mortem brain examination revealed diffuse edema, normal vessels, and early softening and discoloration of the bilateral thalami with prominent eosinophilic and pyknotic neurons.
1.2. Patient 2
A 44-year old woman presented after a 5-day outside hospitalization for fever, right upper quadrant abdominal pain, and transaminitis that rapidly progressed to altered consciousness, hypoxia, acute respiratory distress syndrome (ARDS), distributive shock, anuric renal failure, and disseminated intravascular coagulation (DIC). She required intubation and received empiric antibiotics for presumed cholecystitis and septic shock and was transferred to our hospital.
Neurologic examination on arrival revealed coma, intact brainstem reflexes, flaccid quadriplegia, and diffuse hyperreflexia. Innumerable punctate hemorrhages throughout the cerebral hemispheres were seen in the CT head and brain MRI (Fig. 1D–F). Labs revealed anemia, thrombocytopenia, elevated creatinine of 5.2 mg/dL, transaminitis, triglycerides of 559 mg/dL, CK of 555 IU/L, LDH of 697 IU/L and ferritin of 4,921 ng/mL. Blood cultures were negative. High-dose dexamethasone was started for suspected HLH. Etoposide was added after bone marrow biopsy was consistent with HLH. She slowly improved, was extubated on HD 19 and at 2 months was living at home with a modified Rankin score of 2.
2. Discussion
We report two cases demonstrating different and rare forms of severe brain involvement in adult patients with HLH: ANE, and diffuse hemorrhagic disease due to DIC.
Severe HLH with brain involvement in adults is rare. A retrospective study found that 10% of 289 adult patients with HLH had central nervous system (CNS) involvement [2]. CSF and neuroimaging findings are typically unspecific [2].
ANE is an uncommon but distinctive type of acute, severe brain injury. ANE in children but not in adults with HLH has been reported [3]. Therefore, we herein describe the first case of an adult patient with HLH presenting with fulminant ANE.
DIC has been described in 50% of the patients in a series of critically ill HLH patients admitted to intensive care unit [4]. Brain hemorrhage in adult patients with HLH was found in only 1 out of 289 adult patients with HLH [2]. Our patient presented with DIC resulting in rapid progression to multiple intracerebral hemorrhages with coma. Early suspicion of the underlying diagnosis prompted us to start timely treatment, which resulted in functional neurological recovery of the patient.
Clinical manifestations, labs and imaging findings of HLH with CNS involvement are non-specific [1]. Early diagnosis and treatment is important to prevent serious complications and demise. Such diagnosis should be considered in patients with sepsis-like illness in the absence of an identifiable infection and disproportionately severe neurological manifestations. The existence of the HLH-like cytokine storm syndrome in adult patients with COVID-19 infection [6] which has, in at least one published case led to ANE [7], elevates the importance of a raised index of suspicion for these forms of severe cerebral injury in patients with COVID-19 infection.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jocn.2020.04.054.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Ramos-Casals M., Brito-Zerón P., López-Guillermo A., Khamashta M.A., Bosch X. Adult haemophagocytic syndrome. Lancet. 2014;383(9927):1503–1516. doi: 10.1016/S0140-6736(13)61048-X. [DOI] [PubMed] [Google Scholar]
- 2.Cai G., Wang Y., Liu X., Han Y., Wang Z. Central nervous system involvement in adults with haemophagocytic lympohistiocytosis: a single-center study. Ann Hematol. 2017;96(8):1279–1285. doi: 10.1007/s00277-017-3035-5. [DOI] [PubMed] [Google Scholar]
- 3.Xiujuan W., Wei W., Wei P., Limin W., Kangding L., Hong-Liang Z. Acute necrotizing encephalopathy: an underrecognized clinicoradiologic disorder. Mediators Inflamm. 2015;2015 doi: 10.1155/2015/792578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Valade S., Azoulay E., Galicier L., Boutboul D., Zafrani L., Stepanian A. Coagulation disorders and bleedings in critically ill patients with hemophagocytic lymphohistiocytosis. Medicine. 2015;94(40):1–6. doi: 10.1097/MD.0000000000001692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Henter J.I., Home A., Arico M., Egeler R.M., Filipovich A.H., Imashuku S. HLH-2004: Diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2007;48(2):124–131. doi: 10.1002/pbc.21039. [DOI] [PubMed] [Google Scholar]
- 6.Mehta Puja, McAuley Daniel F, Brown M, Sanchez Emilie, Tattersall Rachel S, Manson Jessica J. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395(10229):1033–1034. doi: 10.1016/S0140-6736(20)30628-0. (In press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Poyiadji Neo, Shahin Gassan, Noujaim Daniel, Stone Michael, Patel Suresh, Griffith Brent. COVID-19-associated Acute Hemorrhagic Necrotizing Encephalopathy: CT and MRI Features. Radiology. 2020 doi: 10.1148/radiol.2020201187. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.