Abstract
Owing to the COVID-19 outbreak in Lombardy, Italy) there is an urgent need to manage cardiovascular emergencies, including acute coronary syndrome (ACS), with appropriate standards of care and dedicated preventive measures and pathways against the risk of SARS-CoV-2 infection. For this reason, the Government of Lombardy decided to centralize the treatment of ACS patients in a limited number of centers, including our university cardiology institute, which in the past 4 weeks became a cardiovascular emergency referral center in a regional hub-and-spoke system. Therefore, we rapidly developed a customized pathway to allocate patients to the appropriate hospital ward, and treat them according to ACS severity and risk of suspected SARS-CoV-2 infection. We present here the protocol dedicated to ACS patients adopted in our center since March 13, 2020, and our initial experience in the management of ACS patients during the first 4 weeks of its use. Certainly, the protocol has room for further improvement as everyone’s experience grows, but we hope that it could be a starting point, adaptable to different realities and local resources.
Résumé
En raison de l'épidémie de COVID-19 en Lombardie (Italie), il est impératif de gérer les urgences cardiovasculaires, y compris les syndromes coronariens aigus (SCA), en suivant des normes de soins appropriées ainsi que des modes d’action et mesures préventives spécifiques contre le risque d'infection par le SARS-CoV-2. C'est pourquoi le Gouvernement de Lombardie a décidé de centraliser le traitement des patients atteints de SCA dans un nombre limité de centres, dont notre institut universitaire de cardiologie, qui est devenu au cours des quatre dernières semaines un centre de référence pour les urgences cardiovasculaires au sein d’un système régional en étoile. Par conséquent, nous avons rapidement mis au point une méthode personnalisée pour affecter les patients au service hospitalier approprié afin de les traiter en fonction de la gravité du SCA et du risque d'infection au SARS-CoV-2 suspectée. Nous présentons ici le protocole dédié aux patients atteints de SCA qui a été adopté dans notre centre depuis le 13 mars 2020, et notre premier bilan de la prise en charge des patients atteints de SCA durant les quatre premières semaines de son application. Certes, le protocole peut encore être amélioré au fur et à mesure que l'expérience de chacun se développe, mais nous espérons qu'il pourra constituer un point de départ, adaptable aux différentes réalités et ressources locales.
The uncontained outbreak of coronavirus disease 2019 (COVID-19) has already taken on pandemic proportions. Owing to increased demand in Lombardy, Italy, most of the intensive therapy beds, including those of intensive cardiac care units (ICCUs), have been dedicated to the treatment of patients with pneumonia and severe acute respiratory syndrome.1 At the same time, there is an urgent need to manage cardiovascular emergencies, including acute coronary syndrome (ACS), with appropriate standards of care and dedicated preventive measures and pathways against the risk of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection.
For this reason, the government of Lombardy and local health authorities decided to centralize the treatment of cardiovascular emergencies in a limited number of centers, including our university cardiology institute, which, 4 weeks before the writing of this report, became a referral center for cardiovascular emergencies in a regional hub-and-spoke system. Therefore, we rapidly developed a local protocol for the triage and management of ACS patients. In particular, we conceived a customized pathway to allocate patients to the appropriate hospital ward and to treat them according to ACS severity and the risk of suspected SARS-CoV-2 infection. Initially, we significantly reduced, and in the past 4 weeks suspended, truly elective procedures in the catheterization laboratories and cardiovascular operating rooms to preserve resources and avoid patient exposure to SARS-CoV-2. Two interventional teams have been dedicated to ACS patients: one working in turn to provide in-hospital 24-hour coverage, and the other one being 24-hour on call. Thus, in the case of an excessive volume of patients, it has been planned to use 2 catheterization laboratories at the same time and, eventually, additional beds outside the ICCU located in the adjacent postoperative intensive care unit.
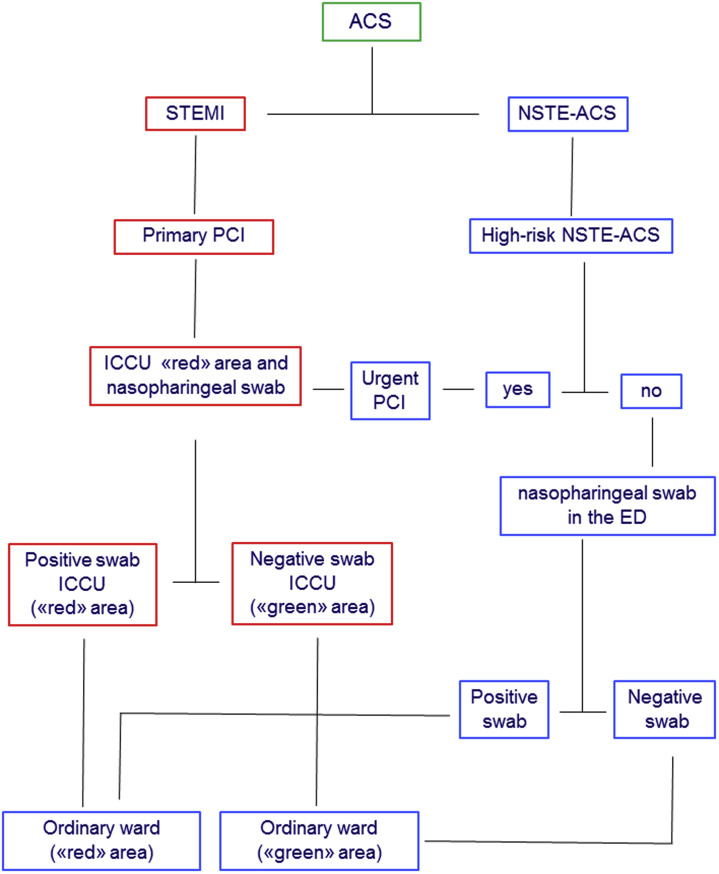
We are not sure whether we will be able to keep all protective measures in place while providing the best treatment strategies for ACS patients during the uncontained COVID-19 outbreak in Lombardy. However, we think that our pilot effort may help other hospitals that are already involved with or will have to face the same critical pandemic in the near future. The goal is to guarantee the best and safest treatment to all ACS patients based on the recommendations of the published guidelines, while ensuring in-hospital safety of health care personnel. Figure 1 shows the flow-chart of the ACS protocol currently adopted in our center and we report in Table 1 the initial clinical experience in the management of ACS patients during the first 4 weeks of using the protocol. We do not provide a detailed description of the recommendations regarding personal protective equipment (PPE) for health care personnel dealing with patient care, because they have been recently provided by the American College of Cardiology Interventional Council, the Society of Cardiovascular Angiography and Intervention, and the Canadian Association of Interventional Cardiology.2 , 3- However, our mandatory recommendations for health care personnel taking care of patients with confirmed, probable, or suspected SARS-CoV-2 infection include correct donning and doffing of PPE (gown, gloves, goggles/shields), limiting the number of people providing care, changing scrubs between cases, social distancing inside the hospital, and changing civilian clothes and footwear on entering and leaving the hospital. Moreover, all patients are required to wear a medical surgical mask throughout their hospitalization.
Figure 1.
Flowchart of the customized pathway for patients with acute coronary syndrome. ACS, acute coronary syndrome; ED, emergency department; ICCU, intensive cardiac care unit; NSTE-ACS, non–ST-segment-elevation acute coronary syndrome; PCI, percutaneous coronary intervention; STEMI, ST-segment-elevation myocardial infarction.
Table 1.
Patients with acute coronary syndrome admitted to our centre from March 13 to April 9, 2020, compared with the same time period in 2019
| Variable | 2020 | 2019 | P value |
|---|---|---|---|
| Patients admitted with ACS, n | 92 | 45 | – |
| Patients transferred from spoke centers | 56 (61%) | 9 (20%) | < 0.001 |
| Age, y, mean ± SD | 65 ± 13 | 66 ± 13 | 0.67 |
| Males | 70 (76%) | 35 (78%) | 0.83 |
| STEMI | 57 (62%) | 23 (51%) | 0.23 |
| NSTE-ACS | 35 (38%) | 22 (49%) | 0.23 |
| High-risk NSTE-ACS | 7 (8%) | 4 (9%) | 0.80∗ |
| Coronary angiography/PCI | 86 (93%) | 43 (96%) | 0.99∗ |
| Positive COVID-19 swab at admission | 9 (10%) | – | – |
| Cardiogenic shock | 12 (13%) | 3 (7%) | 0.38∗ |
| Cardiogenic shock in COVID-19 patients | 1 (1.1%) | – | – |
| In-hospital cardiac death | 9 (10%) | 2 (4%) | 0.33∗ |
| In-hospital cardiac death in COVID-19 patients | 1 (1.1%) | – | – |
| In-hospital death due to COVID-19 | 0 (0%) | – | – |
Results are presented as n (%) unless otherwise specified.
ACS, acute coronary syndrome; COVID-19, Coronavirus disease 2019; NSTE-ACS, Non-ST-elevation acute coronary syndrome; PCI, percutaneous coronary intervention; STEMI, ST-elevation acute myocardial infarction.
Fisher exact test.
STEMI
In patients with ST-segment-elevation acute myocardial infarction (STEMI) who are referred to our emergency department (ED), conservative care cannot be considered as an option in the majority of the cases, and primary percutaneous coronary intervention (PCI) is still our standard of care. Patients in whom for obvious reasons there is not time to wait for nasopharyngeal swab result are immediately transferred to a catheterization laboratory dedicated only to those potentially infected with SARS-CoV-2 and are subjected to coronary angiography and primary PCI. Notably, despite our catheterization laboratory having ∼ 20 air exchanges per hour, it is not under negative pressure. Therefore, it is sanitized after each procedure by a dry and nontoxic environment micronized disinfecting treatment (PoliDisin Air; Biosteril, Treviso, Italy). After primary PCI, patients are admitted to our 13-bed ICCU, where 5 beds (“red” area) are dedicated to patients who are considered to be potentially infected until the result of the diagnostic test. The swab is performed, observing safety rules during specimen collection, as soon as they enter the ICCU, and the result is available within 3-4 hours (GeneFinder COVID-19 RealAmp Kit; ELITechGroup, Torino, Italy). In case of a negative swab result and in the absence of suspicious symptoms of virus infection, the patients are moved from the “red” to the “green” ICCU area and, when the acute phase is over, they are transferred to the ordinary ward where only SARS-CoV-2–negative patients are hospitalized. If the clinical suspicion is high and a second swab remains negative, a chest computed tomographic (CT) scan is performed. Conversely, in case of a positive test, they remain in the “red” ICCU area through the acute phase and then are transferred to the ward dedicated to SARS-CoV-2-positive patients (Fig. 1). Separate staffs of nurses and doctors take care of patients in the “red” and “green” ICCU areas. To minimize the infection risk within the ICCU “red” area, the following preventive measures are adopted: 1) a single patient room is reserved for patients requiring mechanical ventilation or admitted with an already known SARS-CoV-2 infection, 2) distance of at least 2 metres between patients, separated by a plastic sheet divider, and 3) a 1:1 nursing-patient ratio until the swab result is available. Finally, a more rapid (20 min) SARS-CoV-2 testing strategy will be available within the next 2 weeks for early identification of SARS-CoV-2–positive patients, to further minimize their stay in the “red” area. As in the catheterization laboratories, ICCU and ordinary ward beds are not under negative pressure. However, they undergo a rapid (30 min/100 m3) sanitization after each patient discharge, with the same technology used in the catheterization laboratories.
Non–ST-Segment-Elevation ACS
High-risk non–ST-segment-elevation (NSTE) ACS, as defined by hemodynamic or electrical (life-threatening arrhythmias or cardiac arrest) instability, recurrent or ongoing chest pain refractory to medical treatment, or relevant ST-T-wave changes, follow the STEMI protocol. Patients with NSTE-ACS without the characteristics mentioned above are evaluated in the ED in a dedicated and monitored “red” area and undergo nasopharyngeal swab, and eventually chest CT scan, immediately after ACS diagnosis. The rationale to perform a swab at hospital admission in all patients derives from the high prevalence of asymptomatic patients with SARS-CoV-2 infection in Lombardy who must be isolated. The aim is to reduce the risk of infection spreading within the hospital by maintaining separate clinical pathways between SARS-CoV-2–positive and –negative patients. In case of a negative test result and absence of suspicious symptoms of virus infection, the patient is transferred to an ordinary monitored ward where only SARS-CoV-2–negative patients are hospitalized. Coronary angiography and possibly a PCI are performed within 24 hours in the catheterization laboratory reserved for these patients. On the other hand, when the swab result is positive, the patient is admitted to an ordinary monitored ward dedicated only to SARS-CoV-2–positive patients with a view of deferring the invasive procedure provided she/he has hemodynamic stability. If the invasive approach is considered to be clinically indicated, the procedure is performed in the catheterization laboratory dedicated to SARS-CoV-2–positive patients.
Initial Clinical Experience
Ninety-two ACS patients were admitted to our center from March 13 to April 9, 2020 (Table 1). Of them, 9 (10%) had a positive SARS-CoV-2 swab at hospital admission or soon after primary PCI, without overt infection symptoms. Only 1 patient among those with an initial negative swab developed symptoms suggestive of COVID-19 during hospitalization and underwent a second swab and CT scan, both of which returned positive. Of note, no death due to COVID-19 occurred during this preliminary experience. The short duration of the observation period prevents conclusions being drawn about the ability of our protocol to reduce the spread of SARS-CoV-2 infection within the hospital. This will need a much larger sample size with a meticulous nosocomial infection tracking. Similarly, it is premature to make assumptions regarding the cardiac outcome of these patients during the COVID-19 outbreak. However, preliminary experience indicates an overall reduction in the number of patients hospitalized for ACS and delayed hospital presentation, a phenomenon that is also being observed in other European countries4 and the United States.5 A possible and concerning explanation may be that ACS patients decide to stay at home instead of going to the hospital because COVID-19 has created the fear of being infected in the hospital environment. Unfortunately, when they finally seek medical attention it is often late in the course of the ACS when their condition has worsened. Supporting this alarming theory is our observation of a higher rate of cardiogenic shock and in-hospital cardiac mortality in the past 4 weeks when compared with the same time interval of the previous year (Table 1). If patients delay or avoid care for life-threatening conditions such as ACS because of the pandemic fear, then the death rate may extend far beyond that directly associated with SARS-CoV-2 infection.
The use of this in-hospital pathway focused on ACS patients is ongoing in our centre, and we still have no firm data on its effectiveness in containing the spread of the virus within the hospital and ensuring optimal clinical management of ACS patients. In this regard, we acknowledge that our protocol could be considered suboptimal because it suffers from several physical and technical limitations. An ideal approach would be to have negative-pressure facilities and physically separated ICCU beds for SARS-CoV-2–infected and –noninfected patients. However, such structural changes cannot be achievable in the short term in most hospitals. Indeed, it is noteworthy that, concerning negative pressure in the catheterization laboratories, the vast number in the United States have either normal- or positive-pressure ventilation systems, because they are not designed for infection isolation.2 Moreover, we currently lack data comparing our ongoing in-hospital organization for ACS patients with a theoretically optimal one with separated facilities. It is to be hoped that such data can be obtained to determine whether and to what extent major investments are justified.
In conclusion, our protocol certainly has room for significant improvement, also as everyone’s experience grows, but we hope that it could be a starting point, adaptable to different realities and local resources. The ultimate goal is to maintain a high level of care for these patients even at a time of dynamic global crisis that is placing an unprecedented strain on health care systems.
Funding Sources
No funding sources were obtained for this article.
Disclosures
The authors have no conflicts of interest to disclose.
Footnotes
See page 964 for disclosure information.
References
- 1.Grasselli G., Pesenti A., Cecconi M. Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: early experience and forecast during an emergency response [e-pub ahead of print]. JAMA. [DOI] [PubMed]
- 2.Welt F.G.P., Shah P.B., Aronow H.D. American College of Cardiology’s Interventional Council and the Society of Cardiovascular Angiography and Intervention. Catheterization laboratory considerations during the coronavirus (COVID-19) pandemic: from ACC’s Interventional Council and SCAI [e-pub ahead of print]. J Am Coll Cardiol. [DOI] [PMC free article] [PubMed]
- 3.Wood D.A., Sathananthan J., Gin K. Precautions and procedures for coronary and structural cardiac interventions during the COVID-19 pandemic: guidance from Canadian Association of Interventional Cardiology [e-pub ahead of print]. Can J Cardiol. [DOI] [PMC free article] [PubMed]
- 4.Rodríguez-Leora O., Cid-Álvarezd B., Ojedae S. Impacto de la pandemia de COVID-19 sobre la actividad asistencial en cardiología intervencionista en España [e-pub ahead of print]. REC Interv Cardiol. [DOI]
- 5.Garcia S., Albaghdadi M.S., Meraj P.M. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic [e-pub ahead of print]. J Am Coll Cardiol. [DOI] [PMC free article] [PubMed]