Introduction
We present a patient with recurrent NSCLC in whom asymptomatic coronavirus disease 2019 (COVID-19) was detected after abnormal volumetric computed tomography (CT) image guidance was performed as part of the routine setup and delivery of curative stereotactic ablative radiotherapy (SABR).
In January 2020, a 63-year-old woman was diagnosed with a left upper lobe recurrence of pulmonary adenocarcinoma. The patient was referred for stereotactic ablative radiotherapy and enrolled on a phase II protocol investigating the addition of nivolumab to SABR in the definitive management of NSCLC (clinical trial number NCT03110978).1
Case Report
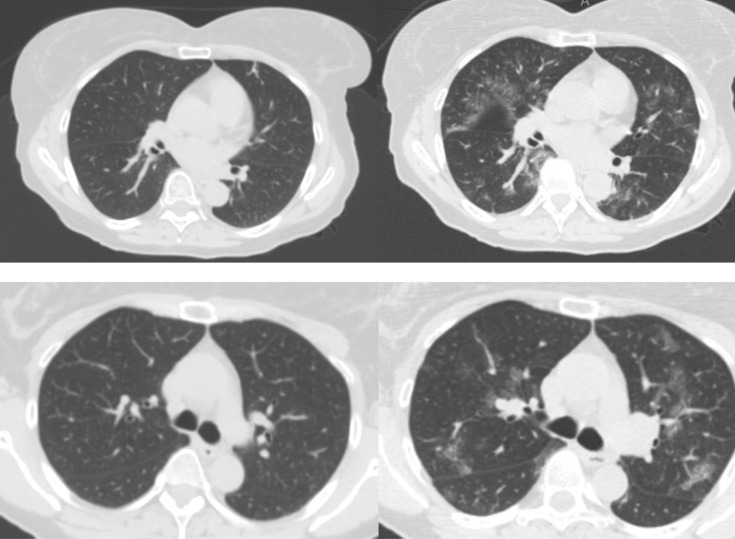
On arrival for her first SABR treatment, the patient was screened per COVID-19 pandemic policies and was deemed low-risk for infection (no new respiratory symptoms, normal body temperature, no recent travel). As per standard SABR protocol, volumetric imaging of the patient’s thorax was obtained through CT-on-rails for patient setup and tumor localization. A comparison was done with her initial CT simulation scan (performed 20 days earlier), which revealed interval development of new multifocal ground-glass opacities of the lungs (Fig. 1 ). The treatment was deferred. Within 12 hours, the nasopharyngeal swab reverse transcription–polymerase chain reaction (RT-PCR) test detected COVID-19. The patient was advised on strict home quarantine and return precautions; all personnel involved were rapidly notified, screened, and cleared accordingly. The patient’s radiation treatments were deferred until she had a subsequent negative test for COVID-19 in accordance with the department policy. The patient remained asymptomatic but her household contacts subsequently became ill and were confirmed to have COVID-19.
Figure 1.
Initial CT simulation images for treatment planning (left), compared with CT image guidance before the first fraction of stereotactic ablative radiotherapy, which was scheduled 20 days later (right). CT, computed tomography.
Discussion
As the COVID-19 pandemic spreads, health care systems must quickly adapt to minimize its global impact. Of the 429,052 confirmed cases within the United States, many have been linked to asymptomatic community spread.2 Early recognition of patients with COVID-19 could streamline isolation protocols, and thus, mitigate its adverse outcomes, particularly among our vulnerable oncologic patient population.3 However, standard screening and testing measures have been insufficient owing to limitations in access and speed. Characteristic radiographic findings have been reported on diagnostic chest CTs of patients with COVID-19. Typical CT findings include bilateral parenchymal ground-glass and consolidative pulmonary opacities with frequent rounded shape and peripheral lung distribution (Table 1 ).4 Data support the utility of chest CTs for primary detection in epidemic areas; and in some cases, chest CT was reported to be more sensitive than RT-PCR, particularly in the earliest (likely asymptomatic) phases of the infection.4
Table 1.
Typical Pulmonary Computed Tomography Image Presentation for Each Stage of COVID-19
| Early Stage | Severe Stage | Resolving Stage |
|---|---|---|
| Multifocal ground-glass opacities with or without consolidation | Increased extent and density of opacities | Resolution of nodular opacities |
| Rounded shape Most commonly involving ≥2 lobes |
Frequent progression to multifocal organizing consolidation or pneumonia | Absorption of bilateral ground-glass opacities Absorption of consolidation |
| Often bilateral, peripheral |
Suppli et al.5 reported a similar case with detectable cone-beam CT (CBCT) abnormalities 36 hours in advance of COVID-19 diagnosis and the manifestation of clinical symptoms. In our case, the patient remained asymptomatic, thus increasing the risk of potential silent spread in our department. Note the superior image resolution of CT-on-rails (in the current report) compared with that of CBCT. Owing to streak artifacts, subtle ground-glass opacities are difficult to detect on CBCT, particularly when obtained on free-breathing, although CBCT benefits from ubiquity across radiation oncology departments. However, both cases advocate for staff in radiotherapy departments to remain vigilant for unexpected ground-glass changes on both initial CT simulation and daily CT image guidance, which can serve as rapid assessment tools during the COVID-19 pandemic, permitting early isolation procedures and providing valuable clinical input toward diagnosis while awaiting RT-PCR confirmation.
Footnotes
Disclosure: Dr. Chang reports receiving grants from Bristol-Meyers Squibb, personal fees from Varian, AstraZeneca, and is a shareholder in Global Oncology One outside the submitted work. Dr. Koong reports being a shareholder in Aravive, Inc. outside the submitted work. The remaining authors declare no conflict of interest.
References
- 1.Bernstein MB, Krishnan S, Hodge JW, Chang JY Immunotherapy and stereotactic ablative radiotherapy (ISABR): a curative approach? Nat Rev Clin Oncol. 2016;13:516–524. doi: 10.1038/nrclinonc.2016.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bhatraju PK, Ghassemieh BJ, Nichols M, et al. Covid-19 in critically ill patients in the Seattle region - case series [e-pub ahead of print]. N Engl J Med. https://doi.org/10.1056/NEJMoa2004500, accessed March 30, 2020. [DOI] [PMC free article] [PubMed]
- 3.Liang W., Guan W., Chen R. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21:335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ai T, Yang Z, Hou H, et al. Correlation of chest CT and RT-PCR testing in coronavirus Disease 2019 (COVID-19) in China: A report of 1014 cases [e-pub ahead of print]. Radiology. https://doi.org/10.1148/radiol.2020200642, accessed March 30, 2020. [DOI] [PMC free article] [PubMed]
- 5.Suppli MH, Riisgaard de Blanck S, Elgaard T, Josipovic M, Pøhl M. Early appearance of coronavirus disease 2019 associated pulmonary infiltrates during daily radiotherapy imaging for lung cancer. J Thorac Oncol. 2020;17:1081-1084. [DOI] [PMC free article] [PubMed]