Abstract
This case report describes a 57-year-old man who presented to the emergency department with right upper extremity swelling and redness. He was diagnosed with right upper extremity deep venous thrombosis extending from the brachial vein to the subclavian vein. The patient underwent successful mechanical thrombectomy with the ClotTriever system (Inari Medical, Irvine, Calif).
Keywords: Thrombosis, Peripheral edema, Peripheral circulation
A 57-year-old man presented to the emergency department with right upper extremity swelling and redness. Two days before arrival, the patient had a peripherally inserted central catheter (PICC) line removed, which was originally placed for prolonged antibiotic therapy because of a history of diverticulitis and a recent gastrointestinal abscess. His past medical history included hypertension and former tobacco use. The patient's home medications included amlodipine (5 mg daily), clonidine (0.2 mg twice per day), lisinopril (20 mg daily), ciprofloxacin (500 mg twice per day), and metronidazole (500 mg every 8 hours). The patient was hemodynamically stable, without any evidence of cardiac or respiratory compromise. Findings on physical examination were normal, except for right upper extremity erythema and mild swelling. Sensation, strength, and pulses were intact throughout the right upper extremity.
The patient agreed to publish this report and all included information and figures.
Case report
Ultrasound of the right upper extremity demonstrated acute deep venous thrombosis (DVT) in the subclavian, axillary, and brachial veins. Computed tomography angiography of the chest showed multiple pulmonary emboli in all lobes of both lungs and a right ventricular/left ventricular ratio of 1.0. Echocardiography was performed to assess for possible right ventricle dysfunction, which proved to be mild. The patient was determined to have an intermediate risk for a massive pulmonary embolism (PE) and thus was treated medically. A heparin drip was maintained throughout hospitalization. The cardiology service was consulted in the evening on the second day of admission. Because of the large upper extremity clot burden, the patient's worsening symptoms, and a concern for further embolization resulting in more strain on the right ventricle, thrombectomy of the upper extremity DVT was pursued on the morning of the third day of admission. Ultrasound-guided access of the right brachial vein was achieved with a micropuncture technique. Extensive thrombus was noted on venography, extending from the distal right brachial vein through the right subclavian veins (Fig 1); thus, a 0.035-inch × 260-cm Glidewire (Terumo, Somerset, NJ) was advanced past the thrombus into the inferior vena cava. The ClotTriever system (Inari Medical, Irvine, Calif), consisting of a 13F specialty sheath with an integrated funnel for optimal thrombus capture and the ClotTriever catheter (Fig 2), was inserted. Once it was inserted through the sheath and positioned beyond the thrombus, the catheter was deployed, unveiling a coring element that separates thrombus from the vessel wall and an integrated collection bag that collects thrombus as the catheter is slowly pulled back toward the sheath (Fig 3). For the entire thrombus to be extracted, it was imperative to advance the device to the inferior vena cava. Successful mechanical thrombectomy was achieved after one complete pass. Comparison of the venogram before and after the procedure signified a >90% reduction in thrombus burden (Fig 4). Fig 5 depicts the large amount of thrombus removed with the single pass of the ClotTriever catheter. There were no complications, and the patient was monitored on the cardiac telemetry unit. The following day, the patient was discharged home on his home medications as well as apixaban 5 mg twice a day and was instructed to follow up in the office in 1 week.
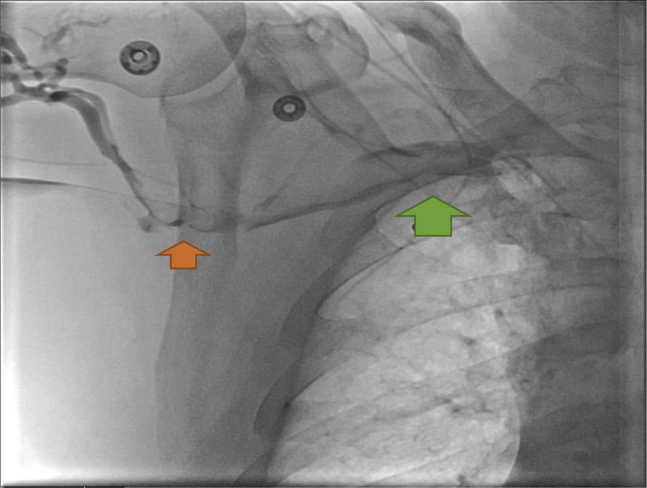
Fig 1.
Venogram before thrombectomy signifying decreased venous flow through the right axillary vein (orange arrow) and the right subclavian vein (green arrow).
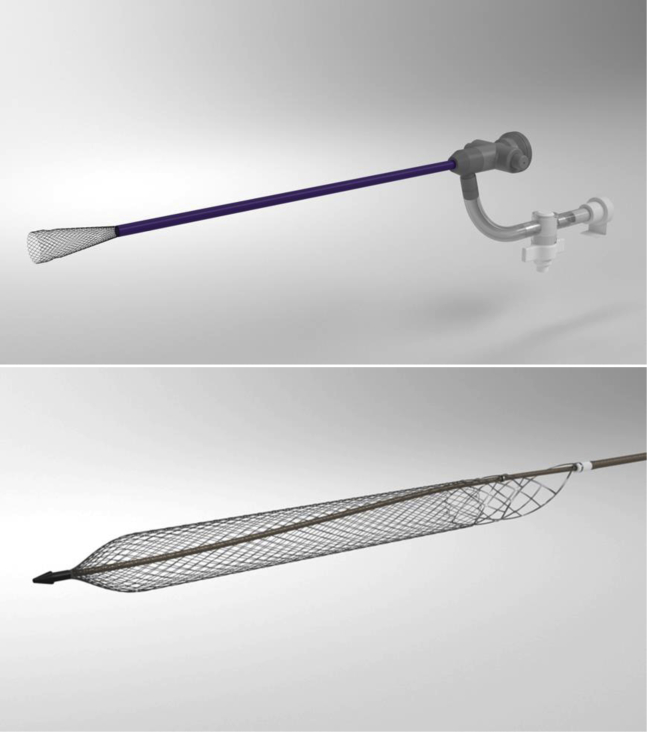
Fig 2.
Schematic of the ClotTriever device. (Courtesy Inari Medical, Irvine, Calif).
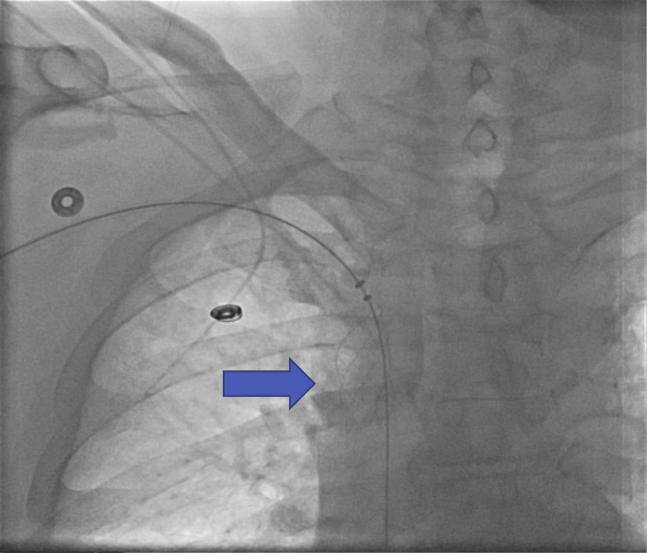
Fig 3.
Confirming placement of ClotTriever catheter at the junction of the right subclavian vein and superior vena cava (arrow).
Fig 4.
Venogram after thrombectomy shows vastly improved flow through the right axillary vein (black arrow) and the right subclavian vein (yellow arrow).
Fig 5.
Large amount of thrombus removed from the right subclavian and axillary veins after one pass with the ClotTriever catheter.
At the 1-week follow-up visit, the patient's right upper extremity edema and erythema were fully resolved, and he was tolerating the apixaban without any sign of bleeding. The patient was further evaluated at 3-month follow-up and continued to be without swelling or pain. He had full function of his upper extremity without limitations. Apixaban was discontinued after completion of the 3-month course for provoked DVT or PE, and he is awaiting follow-up right upper extremity ultrasound to evaluate for complete thrombus resolution.
Discussion
We successfully performed mechanical thrombectomy using the ClotTriever system on a patient with an upper extremity DVT that developed after removal of a PICC line. The risk of DVT brought on by PICC lines is high, with a frequency of up to 38.5%, regardless of whether the patient has a history of venous thrombosis.1,2 Therefore, it is imperative that these patients are closely monitored during hospitalization for symptoms indicating a possible DVT. If a DVT or PE is diagnosed, the first 10 days have the highest risk for recurrent thrombosis and embolization.3 This time period makes early anticoagulation and possible intervention crucial in these patients.
Approximately 5% to 10% of all DVT cases occur in the upper extremities.4 Whereas the clinical presentation of this patient was typical of an upper extremity DVT, the minimally invasive treatment, although indicated for the nonsurgical removal of soft emboli and thrombi from the peripheral vasculature, was unique. Publications on the ClotTriever system's effective use in lower extremity and inferior vena cava thrombosis exist, but to the best of our knowledge, this is the first report of its use in upper extremity DVT.5 The American College of Chest Physicians recommends treatment of DVT with anticoagulation for a minimum of 3 months with low-molecular-weight heparin, vitamin K antagonists, or direct oral anticoagulant.6 However, catheter-directed thrombolysis can be considered in patients with severe symptoms, thrombus extending from subclavian to axillary vein, symptoms of <2 weeks, good performance status, life expectancy >1 year, and low bleeding risk.6 We thought the patient fit into those criteria and was a good interventional candidate. Although there was some mild flow around the DVT (as noted on preintervention venography), intervention was believed to be best with the persistent symptoms and acute presentation. Based on the operator's clinical experience, it was thought that this patient would have better symptomatic relief, better overall outcome, and decreased length of stay with the ClotTriever system compared with catheter-directed thrombolysis or medical therapy alone. In this case, it was estimated that the length of stay decreased by roughly 2 days, which justified the expense of the device.
Conclusions
Other thrombectomy systems, such as AngioJet (Boston Scientific, Marlborough, Mass) or Indigo (Penumbra Inc, Alameda, Calif), are available on the market; however, the operator's preference and availability at the facility led the authors to use the ClotTriever system. The successful outcome warrants evaluation of future patients for mechanical thrombectomy suitability, which might prove beneficial as a single-session treatment option for upper extremity DVTs or occlusive subclavian lesions if they are associated with acute or subacute thrombosis.
Footnotes
Author conflict of interest: none.
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Abdullah B.J., Mohammad N., Sangkar J.V., Abd Aziz Y.F., Gan G.G., Goh K.Y. Incidence of upper limb venous thrombosis associated with peripherally inserted central catheters (PICC) Br J Radiol. 2005;78:596–600. doi: 10.1259/bjr/32639616. [DOI] [PubMed] [Google Scholar]
- 2.Heit J.A. The epidemiology of venous thromboembolism in the community: implications for prevention and management. In: Bergen J.J., editor. The vein book. Academic Press; New York: 2007. pp. 323–330. [Google Scholar]
- 3.Smith S.B., Geske J.B., Maguire J.M., Zane N.A., Carter R.E., Morgenthaler T.I. Early anticoagulation is associated with reduced mortality for acute pulmonary embolism. Chest. 2010;137:1382–1390. doi: 10.1378/chest.09-0959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mintz A., Levy M.S. Upper extremity deep vein thrombosis. https://www.acc.org/latest-in-cardiology/articles/2017/11/09/13/30/upper-extremity-deep-vein-thrombosis Available at: Accessed October 5, 2019.
- 5.Crowner J., Marston W. Percutaneous thrombectomy using a novel single-session device for acute iliocaval deep venous thrombosis. J Vasc Surg Venous Lymphat Disord. 2018;6:300–301. [Google Scholar]
- 6.Munoz F.J., Mismetti P., Poggio R., Valle R., Barron M., Guil M. Clinical outcome of patients with upper-extremity deep vein thrombosis: results from the RIETE Registry. Chest. 2008;133:143–148. doi: 10.1378/chest.07-1432. [DOI] [PubMed] [Google Scholar]