Abstract
Phlegmasia cerulea dolens can be a potentially devastating complication of severe deep venous thrombosis leading to limb ischemia and tissue necrosis. This report describes a patient presenting with phlegmasia cerulea dolens of the right lower extremity. Because of the urgent nature of the condition, percutaneous nonpharmacologic mechanical thrombectomy in a single session was pursued. Extensive thrombus burden was removed from the patient, and vessel patency was restored after balloon venoplasty. The patient's symptoms rapidly resolved, and the targeted vessels remain patent at 3-month follow-up.
Keywords: DVT, Phlegmasia, Inari, Thrombectomy
Phlegmasia cerulea dolens can be a potentially devastating complication of severe deep venous thrombosis (DVT) leading to limb ischemia and tissue necrosis. It is characterized by limb swelling, acute ischemic pain, and discoloration and is complicated by risk factors including malignant disease, hypercoagulable state, and venous stasis.1 If it is left untreated, phlegmasia cerulea dolens carries a 25% to 40% mortality rate, and even survivors may require amputation in 20% to 50% of cases.2, 3, 4 Intervention is indicated, and options range from open venous thrombectomy to percutaneous methods, although duration of thrombolytics and associated bleeding risks may complicate percutaneous intervention.5 With the patient's consent, this case of phlegmasia cerulea dolens successfully treated with single-session percutaneous nonpharmacologic mechanical thrombectomy is presented.
Case report
A 29-year-old white woman with Down syndrome and mild cognitive impairment presented to her primary care physician with a 1-day history of acute right lower extremity edema extending from the proximal thigh to the level of the foot and associated pain described as continuous, severe, and throbbing. Venous duplex ultrasound examination demonstrated extensive occlusive thrombus extending from the right external iliac vein to the infrapopliteal veins. She was then transferred to our emergency department, where vascular surgical consultation was requested and systemic anticoagulation with intravenous heparin was initiated and titrated per heparin nomogram.
Before her presentation, the patient had no episodes of lower extremity discomfort. She is ambulatory and denies intermittent claudication, rest pain, or tissue loss. Her mother did note some subjective intermittent right lower extremity edema that was insignificant. The patient does not smoke. She has been taking the Depo-Provera contraceptive for 15 years, progesterone only; however, she was converted to an estrogen-progesterone combination pill 6 weeks earlier. She did not have any long-haul travel.
Physical examination in the presence of her parents demonstrated a well-developed woman with Down facies who was alert and oriented. She did engage when prompted. Cardiorespiratory examination was within normal limits. Peripheral vascular examination identified normal femoral, popliteal, posterior tibial, and dorsalis pedis pulses bilaterally. Extremity evaluation identified phlegmasia cerulea dolens of the right lower extremity with 4+ pitting edema with erythema and bluish discoloration (Fig 1). She had satisfactory sensory and motor function of the legs.
Fig 1.
Acute extensive right lower extremity edema and phlegmasia cerulea.
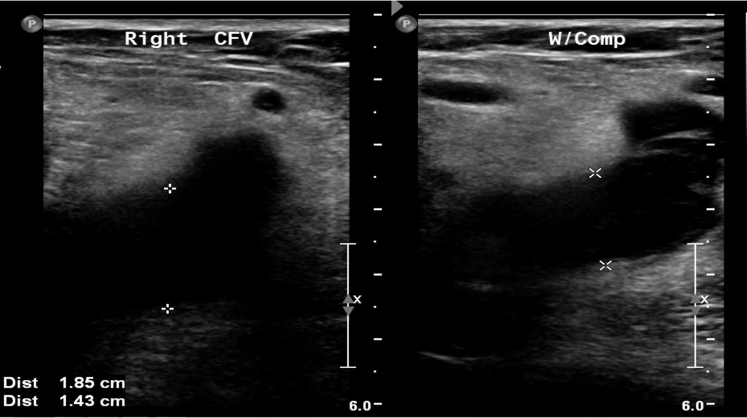
Laboratory evaluation was within normal limits. Diagnostic imaging with venous duplex ultrasound identified extensive occlusive thrombus extending from the right external iliac vein to the infrapopliteal deep veins (Figs 2 and 3).
Fig 2.
Venous duplex ultrasound image of right common femoral vein (CFV) depicting acute dilation, noncompressibility, and hypoechoism. W/Comp, With compression.
Fig 3.
Venous duplex ultrasound image of thrombosed saphenofemoral junction (SF Junc) and popliteal vein (Pop V). W/Comp, With compression.
A comprehensive discussion was conducted with the patient and her family. Given the significant thrombus burden, proximal extension, and acute edema, urgent surgical intervention was recommended.
The patient was brought to the operating room, and general anesthesia was induced before she was placed in the prone position. General anesthesia was selected for concern of cooperation with conscious sedation because of her cognition. With ultrasound guidance, the right popliteal vein was identified and noted to be severely dilated and completely thrombosed; the lumen was hypoechoic. Following modified Seldinger technique with a micropuncture access kit, the vessel was accessed as distal as possible, and there was no aspiration of blood. A microsheath was placed, and right lower extremity venography was performed, demonstrating complete thrombosis of the femoropopliteal and iliofemoral segments. The patient was then systemically anticoagulated with heparin with a target activated clotting time of >250 seconds.
A 0.035-inch wire was then placed and advanced into the inferior vena cava with injection of contrast material, confirming true lumen position and a patent iliocaval segment and inferior vena cava without evidence of anatomic duplication or abnormality. Serial dilation of the access site was performed for insertion of the 13F ClotTriever specialty sheath (Inari Medical, Irvine, Calif). The ClotTriever catheter, consisting of a coring element that separates thrombus from the vessel walls and an integrated nitinol collection bag for distal protection, was then brought to the field. Primary percutaneous mechanical venous thrombectomy of the right lower extremity was performed by pullback technique from the inferior vena cava to the popliteal access site. Four passes of the device were conducted in total, with the coring element rotated 90 degrees for each pass, extracting a significant amount of acute and subacute thrombus. Thrombus was cleared off on the back table after each pass until there was a clean pass of the device (Fig 4).
Fig 4.
Ascending venogram of right lower extremity (prone position) before and after percutaneous thrombectomy with demonstrated thrombus burden.
Ascending venography through the introducer sheath demonstrated cephalad flow with several areas of stenosis and trabecular synechiae. Intravascular ultrasound (IVUS) was then performed with a 0.035-inch IVUS catheter (Philips, Amsterdam, The Netherlands) by pullback technique. Interestingly, there was no evidence of compressive phenomena other than trabecular synechiae in the right external iliac vein identifying a 35% stenosis as well as in the right common femoral vein, femoral vein, and popliteal veins. Given her young age and minimal stenosis confirmed on IVUS, it was decided against primary stent implantation. Balloon venoplasty of the iliofemoral segment was then conducted with a 14-mm high-pressure balloon and of the femoropopliteal segment with an 8-mm noncompliant balloon. Completion venography demonstrated brisk cephalad flow toward the inferior vena cava with no evidence of contrast material delay; completion IVUS confirmed complete resolution of any stenosis or abnormality.
The patient's leg was wrapped with an elastic bandage from the foot to the proximal thigh, and she returned to systemic anticoagulation. The next day, the wrap was removed, and she was discharged home on a direct oral anticoagulant. The pain and edema had resolved significantly, and at 1- and 3-month follow up, she was completely asymptomatic with normal findings on venous duplex ultrasound (Fig 5).
Fig 5.
Postoperative clinical image of patient with resolution of acute edema and phlegmasia.
Discussion
The treatment of proximal iliofemoral DVT ranges from medical management to endovascular interventions. Although open venous thrombectomy has been historically described, new technologies allow minimally invasive percutaneous techniques with satisfactory results.
Endovascular intervention generally employs the administration and infusion of thrombolytic agents, such as tissue plasminogen activator.6,7 Although it is effective, there are inherent contraindications to its use, such as recent surgery or the patient's noncompliance. Furthermore, the use of lytic agents predisposes the patient to bleeding risks, such as intracerebral hemorrhage or bleeding from the access site, and increases the use of important hospital resources, such as the intensive care unit and critical care nursing.8
In addition, thrombolytic therapy can have long infusion times ranging from 24 to 72 hours.9, 10, 11 Distinctly, however, phlegmasia cerulea dolens requires urgent action in an effort to avoid the concern for associated venous gangrene and major limb loss. To this end, single-session percutaneous thrombectomy for immediate extirpation of the significant thrombus burden was pursued. This approach using the ClotTriever system has recently been described for acute proximal iliofemoral DVT.9 Given the urgent nature of the patient's diagnosis, the duration of treatment necessary for thrombolytic therapy was not appropriate as she required more immediate intervention. Moreover, her cognitive impairment necessitated general anesthesia for the procedure, and it was believed that she would not be able to tolerate lying flat for the duration of thrombolysis therapy in the intensive care unit.
Conclusions
The use of the Inari ClotTriever system is an effective percutaneous nonpharmacologic solution allowing treatment in a single session without the risks associated with thrombolytic therapy. It should be considered for urgent thrombus extirpation in phlegmasia cerulea dolens.
Footnotes
Author conflict of interest: none.
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Chinsakchai K., Ten Duis K., Moll F.L., de Borst G.J. Trends in management of phlegmasia cerulea dolens. Vasc Endovascular Surg. 2011;45:5–14. doi: 10.1177/1538574410388309. [DOI] [PubMed] [Google Scholar]
- 2.Perkins J.M., Magee T.R., Galland R.B. Phlegmasia caerulea dolens and venous gangrene. Br J Surg. 1996;83:19–23. doi: 10.1002/bjs.1800830106. [DOI] [PubMed] [Google Scholar]
- 3.Stallworth J.M., Bradham G.B., Kletke R.R., Price R.G., Jr. Phlegmasia cerulea dolens: a 10-year review. Ann Surg. 1965;161:802–811. doi: 10.1097/00000658-196505000-00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bhatt S., Wehbe C., Dogra V.S. Phlegmasia cerulea dolens. J Clin Ultrasound. 2007;35:401–404. doi: 10.1002/jcu.20317. [DOI] [PubMed] [Google Scholar]
- 5.Wang C.N., Deng H.R. Percutaneous endovenous intervention plus anticoagulation versus anticoagulation alone for treating patients with proximal deep vein thrombosis: a meta-analysis and systematic review. Ann Vasc Surg. 2018;49:39–48. doi: 10.1016/j.avsg.2017.09.027. [DOI] [PubMed] [Google Scholar]
- 6.Meissner H., Gloviczki P., Comerota A.J., Dalsing M.C., Eklof B.G., Gillespie D.L. Early thrombus removal strategies for acute deep venous thrombosis: clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. J Vasc Surg. 2012;55:1449–1462. doi: 10.1016/j.jvs.2011.12.081. [DOI] [PubMed] [Google Scholar]
- 7.Lin P.H., Ochoa L.N., Duffy P. Catheter-directed thrombectomy and thrombolysis for symptomatic lower-extremity deep vein thrombosis: review of current interventional treatment strategies. Perspect Vasc Surg Endovasc Ther. 2010;22:152–163. doi: 10.1177/1531003510378756. [DOI] [PubMed] [Google Scholar]
- 8.Ng T.T., Sigman M., Weaver F.A. Basic data related to thrombolytic therapy for acute venous thrombosis. Ann Vasc Surg. 2014;28:1039–1044. doi: 10.1016/j.avsg.2013.12.002. [DOI] [PubMed] [Google Scholar]
- 9.Crowner J., Marston W. Percutaneous thrombectomy using a novel single-session device for acute ilio-caval deep vein thrombosis. J Vasc Surg Cases Innov Tech. 2019;5:302–304. doi: 10.1016/j.jvscit.2019.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vedantham S., Goldhaber S.Z., Julian J.A., Kahn S.R., Jaff M.R., Cohen D.J., ATTRACT Trial Investigators Pharmacomechanical catheter-directed thrombolysis for deep-vein thrombosis. N Engl J Med. 2017;377:2240–2252. doi: 10.1056/NEJMoa1615066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Enden T., Haig Y., Enden T., Grøtta O., Kløw N.E., Slagsvold C.E., CaVenT Study Group Catheter-directed thrombolysis vs. anticoagulant therapy alone in deep vein thrombosis: results of an open randomized, controlled trial reporting on short-term patency. J Thromb Haemost. 2009;7:1268–1275. doi: 10.1111/j.1538-7836.2009.03464.x. [DOI] [PubMed] [Google Scholar]