Abstract
Purpose
To present a case of central retinal artery occlusion as the first symptomatic manifestation of Moyamoya disease in a middle-aged patient.
Observations
Case report of a 48-year-old female Chinese-American patient who presented with sudden onset painless unilateral vision loss. Fundus photos, optical coherence tomography, fluorescein angiography, magnetic resonance angiography, computed tomography angiography, and catheter cerebral angiogram were performed. The patient's dilated fundus examination showed classic findings of a central retinal artery occlusion. Diagnostic brain imaging demonstrated extensive stenosis of the cerebrovascular network, with almost complete unilateral occlusion of the internal carotid artery along with compensatory collateral vessels. This led to a new diagnosis of Moyamoya disease. The patient was treated with extracranial-intracranial bypass surgery.
Conclusions and importance
Arterial abnormalities in patients with Moyamoya disease are uncommon and have previously only been reported in younger patients in their teens and 20s. Young and middle-aged patients presenting with central retinal artery occlusions should undergo complete neurologic workup including stroke evaluation; in this case, revealing Moyamoya disease, a rare yet life-threatening condition, as the underlying etiology.
Keywords: Central retinal artery occlusion, Cerebrovascular disease, Moyamoya disease, Optical coherence tomography, Retina, Vascular occlusion
1. Introduction
Moyamoya disease is a rare cerebrovascular disorder associated with progressive stenosis of the terminal internal carotid artery and its branches.1 In Japanese, Moyamoya means “a hazy puff of smoke,” which describes the tangle of abnormally dilated collateral vessels formed to compensate for the occlusion. We report a case of a middle-aged woman who presented with acute painless unilateral vision loss and was found to have a central retinal artery occlusion. Systemic evaluation led to the diagnosis of Moyamoya disease.
2. Case report
We report a 48-year-old Chinese-American woman who presented to the Emergency Department (ED) 8 hours after awakening with painless vision loss in the right eye. She denied other associated ocular or neurologic symptoms. Her past medical history was notable for prior smoking and hypertension well-controlled on medication.
At initial evaluation by our Ophthalmology Consult Service in the ED, her visual acuity was hand motion in the right eye and 20/40 in the left eye. Dilated fundus exam of the right eye showed a “cherry red spot” with extensive retinal whitening consistent with central retinal artery occlusion (CRAO). Her neurologic examination was otherwise normal.
The patient was admitted to the hospital for a complete neurologic work-up including stroke evaluation. Laboratory testing was nonrevealing. Transthoracic echocardiogram was unremarkable. Magnetic resonance angiography (MRA) and computed tomography angiography (CTA) demonstrated high-grade stenosis throughout the cervical segment of the right internal carotid artery (ICA), concerning for Moyamoya disease [Fig. 2A]. The patient was discharged on aspirin and statin therapy.
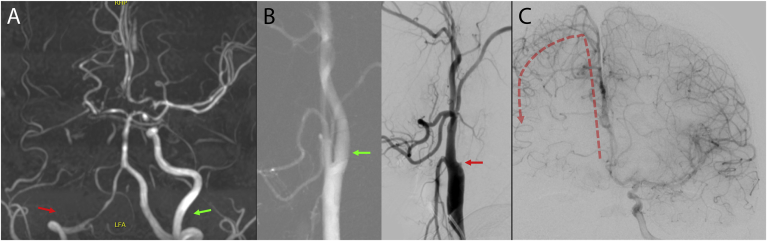
Fig. 2.
Neuroimaging
A. Magnetic resonance angiogram of the brain (axial view) shows complete occlusion of the right ICA (red arrow) and middle cerebral artery (MCA) along with mild segmental stenosis of the distal left supraclinoid ICA and proximal left MCA. Severe Moyamoya disease was present on the right and mild disease on the left (green arrow pointing to non-occluded left proximal ICA). B. Catheter cerebral angiogram of the neck (lateral view) demonstrates complete occlusion of right ICA (right panel, red arrow) compared to the non-occluded left ICA (left panel, green arrow). C. Catheter cerebral angiogram of the head (anteroposterior view) following left ICA injection shows formation of abnormal right-sided collateral arterial supply (red arrow) with R anterior cerebral artery supplying pial collaterals. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
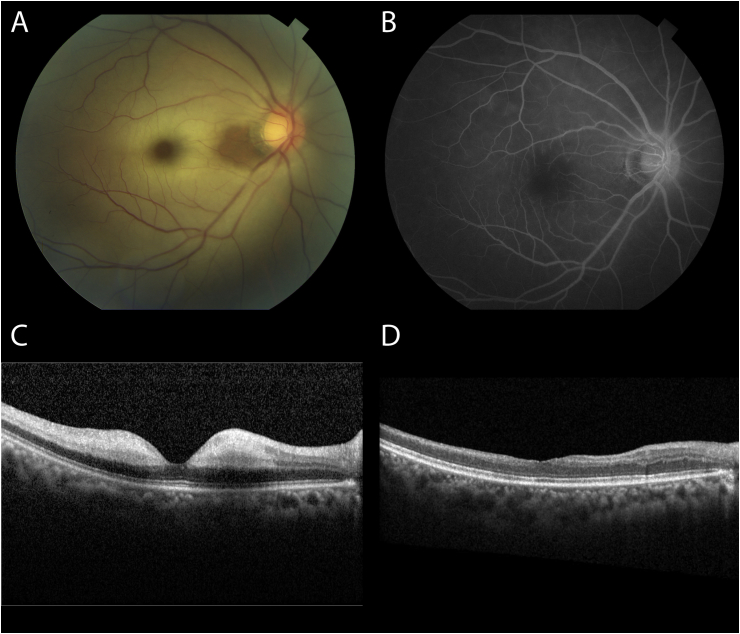
The patient was re-evaluated in Ophthalmology clinic 4 days after onset of vision loss. Her visual acuity in the right eye was stable at hand motion. Repeat dilated fundus exam is shown in Fig. 1A. Optical coherence tomography (OCT) of the right eye demonstrated marked retinal nerve fiber layer edema with sparing temporal to the optic disc [Fig. 1C]. Fluorescein angiogram (FA) of the right eye showed reperfusion of the posterior pole [Fig. 1B]. Indocyanine green angiography showed patchy choroidal filling in the right eye. Ophthalmic imaging of the left eye was unremarkable.
Fig. 1.
Ophthalmic imaging
A. Color fundus photograph of the right eye 4 days after symptom onset shows diffuse retinal whitening with a “cherry red spot,” and local preservation of perfusion temporal to the optic disc. B. Mid-stage FA of the right eye shows reperfusion of the retina. C. Initial OCT through the right fovea shows marked retinal nerve fiber layer edema with some nasal sparing. D. OCT of the right eye 2 months after symptom onset shows inner retinal thinning with sparing temporal to the optic disc. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
The patient underwent a diagnostic catheter cerebral angiogram which confirmed occlusion of the right ICA at the cervical level and a constellation of collateral arterial supply indicative of Moyamoya disease [Fig. 2B and C]. At 2 month follow-up evaluation, her vision in the right eye had improved slightly to counting fingers at 2 feet. OCT at that time showed thinning of the inner retina with some sparing temporal to the optic disc [Fig. 1D]. Five months after initial presentation, the patient underwent right-sided extracranial to intracranial bypass surgery as recommended by Neurosurgery.
3. Discussion
The epidemiology of Moyamoya varies geographically, with a higher prevalence of 3/100,000 in Japan to a lower prevalence of 0.086/100, 000 in America. Women are twice as likely to be affected as men, with a bimodal age distribution of onset peaking in the first decade of life with a second peak in the later 20s–30s. There have been only rare case reports of arterial abnormalities of the eye in Moyamoya patients, primarily in young patients in their teens or 20s.2, 3, 4, 5, 6 Our case demonstrates CRAO as the first symptomatic manifestation that ultimately led to a new diagnosis of Moyamoya disease in a woman in her late 40s. Adults with Moyamoya often present with symptoms of ischemic or hemorrhagic strokes with high risk of recurrences. Up to two-thirds of Moyamoya disease patients will have symptomatic progression over a 5-year period, but after surgery the rate of progression decreases to 2.3%.1 Though there is no curative treatment for Moyamoya disease, options for direct or indirect surgical revascularization exist. Fortunately, our patient had not suffered any other neurologic damage from her underlying disease, which is a good prognostic indicator,1 and she has undergone direct revascularization via bypass surgery. Patients who present with a symptomatic CRAO warrant a thorough neurologic workup to evaluate for risk of stroke. In our case, evaluation revealed Moyamoya disease, a rare yet life-threatening condition, as the underlying etiology for which therapeutic intervention may be indicated.
Patient consent
Explicit consent was not obtained from the patient, given that this report does not contain any identifying information.
Funding
The authors have no funding or grant sources to report.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Declaration of competing interest
None of the authors have financial disclosures.
Acknowledgments
None.
References
- 1.Scott R.M., Smith E.R. Moyamoya disease and moyamoya syndrome. N Engl J Med. 2009;360(12):1226–1237. doi: 10.1056/NEJMra0804622. [DOI] [PubMed] [Google Scholar]
- 2.Kumar M.A., Ganesh B.A. CRAO in moyamoya disease. J Clin Diagn Res : J Clin Diagn Res. 2013;7(3):545–547. doi: 10.7860/JCDR/2013/4579.2819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chace R., Hedges T.R., 3rd Retinal artery occlusion due to moyamoya disease. J Clin Neuro Ophthalmol. 1984;4(1):31–34. [PubMed] [Google Scholar]
- 4.Akkoyun I., Baskin E., Caner H., Agildere M.A., Boyvat F., Akova Y.A. [Hemicentral retinal artery occlusion associated with moyamoya syndrome] Ophthalmologe : Zeitschrift der Deutschen Ophthalmologischen Gesellschaft. 2006;103(10):888–891. doi: 10.1007/s00347-006-1401-0. [DOI] [PubMed] [Google Scholar]
- 5.Ebert J.J., Sisk R.A. CRAO in moyamoya syndrome associated with Southampton hemoglobinopathy. Ophthalmic Surg Laser Imag Retina. 2019;50(5):e166–e170. doi: 10.3928/23258160-20190503-17. [DOI] [PubMed] [Google Scholar]
- 6.Ushimura S., Mochizuki K., Ohashi M., Ito S., Hosokawa H. Sudden blindness in the fourth month of pregnancy led to diagnosis of moyamoya disease. Ophthalmologica Journal international d'ophtalmologie International journal of ophthalmology Zeitschrift fur Augenheilkunde. 1993;207(4):169–173. doi: 10.1159/000310428. [DOI] [PubMed] [Google Scholar]