Ebola outbreaks result in significant morbidity and mortality in affected countries. Although several leading candidate Ebola vaccines have been developed and advanced in clinical testing, additional vaccine candidates may be needed to provide protection against different Ebola species and to extend the durability of protection. A novel approach demonstrated here is to express two genetically diverse glycoproteins on a spherical core, generating a vaccine that can broaden immune responses against known pathogenic Ebola viruses. This approach provides a new method to broaden and potentially extend protective immune responses against Ebola viruses.
KEYWORDS: Ebola virus, Ebola virus disease, Ebola glycoprotein, Ebola vaccine, Sudan virus, Bundibugyo virus, Tai Forest virus, Marburg virus, virus-like particles
ABSTRACT
The 2013–2016 Ebola outbreak in West Africa led to accelerated efforts to develop vaccines against these highly virulent viruses. A live, recombinant vesicular stomatitis virus-based vaccine has been deployed in outbreak settings and appears highly effective. Vaccines based on replication-deficient adenovirus vectors either alone or in combination with a multivalent modified vaccinia Ankara (MVA) Ebola vaccine also appear promising and are progressing in clinical evaluation. However, the ability of current live vector-based approaches to protect against multiple pathogenic species of Ebola is not yet established, and eliciting durable responses may require additional booster vaccinations. Here, we report the development of a bivalent, spherical Ebola virus-like particle (VLP) vaccine that incorporates glycoproteins (GPs) from Zaire Ebola virus (EBOV) and Sudan Ebola virus (SUDV) and is designed to extend the breadth of immunity beyond EBOV. Immunization of rabbits with bivalent Ebola VLPs produced antibodies that neutralized all four pathogenic species of Ebola viruses and elicited antibody-dependent cell-mediated cytotoxicity (ADCC) responses against EBOV and SUDV. Vaccination of rhesus macaques with bivalent VLPs generated strong humoral immune responses, including high titers of binding, as well as neutralizing antibodies and ADCC responses. VLP vaccination led to a significant increase in the frequency of Ebola GP-specific CD4 and CD8 T cell responses. These results demonstrate that a novel bivalent Ebola VLP vaccine elicits strong humoral and cellular immune responses against pathogenic Ebola viruses and support further evaluation of this approach as a potential addition to Ebola vaccine development efforts.
IMPORTANCE Ebola outbreaks result in significant morbidity and mortality in affected countries. Although several leading candidate Ebola vaccines have been developed and advanced in clinical testing, additional vaccine candidates may be needed to provide protection against different Ebola species and to extend the durability of protection. A novel approach demonstrated here is to express two genetically diverse glycoproteins on a spherical core, generating a vaccine that can broaden immune responses against known pathogenic Ebola viruses. This approach provides a new method to broaden and potentially extend protective immune responses against Ebola viruses.
INTRODUCTION
The 2013–2016 outbreak of Ebola virus disease (EVD) in West Africa resulted in over 28,000 infections and 11,300 deaths (1). The extent of the outbreak, the high rate of mortality, and the devastating effects on public health systems of the affected nations emphasized the importance of developing new vaccines and therapeutics against Ebola viruses. The development of several experimental Ebola vaccines that had shown promise in nonhuman primate (NHP) models of EVD was subsequently accelerated, and these vaccines advanced into clinical trials (2–11). A recombinant vesicular stomatitis virus-based replication-competent vaccine (VSV-ZEBOV) was deployed in a ring vaccination strategy in Guinea during the 2013–2016 outbreak and demonstrated 100% protection (2). VSV-ZEBOV again is being deployed to help contain the current Ebola outbreak in the Democratic Republic of the Congo (DRC) (12). Another leading approach utilizes replication-deficient adenovirus-based Ebola vaccines. Clinical trials conducted using recombinant adenovirus vectors based on adenovirus type 5 (Ad5), adenovirus type 26 (Ad26), and chimpanzee adenovirus type 3 (ChAd3) have shown these vaccines to be safe and immunogenic (3–5, 7, 9, 10). Adenovirus-based vaccines have been shown to protect against lethal doses of Ebola virus in the NHP model (13–15) but have not yet been proven protective in the setting of a human epidemic. While no Ebola vaccine is licensed in the United States or in any Western country, the current live vector vaccines represent a very promising response to an urgent health need.
Despite the substantial progress in the development of Ebola vaccines, additional work is needed. For an Ebola vaccine to be effective in outbreak settings as well as in providing long-term protection, it should be able to elicit rapid and durable protective immune responses. The leading Ebola vaccine candidates may be limited in their potential to provide durable immunity (4, 16, 17). These limitations may be addressed through heterologous boosting, as has been shown when adenovirus vector-based vaccines are combined with a booster dose of a heterologous modified vaccinia Ankara (MVA) vaccine (5, 7, 9, 11, 14). Vaccines based on human adenovirus vectors are limited by the presence of preexisting immunity against the vector backbone in areas where Ebola outbreaks have been reported in the past (4, 13, 14, 18–20). VSV-ZEBOV has an acceptable safety profile for the outbreak setting, but tolerability in lower-risk settings may be an issue due to adverse events, such as arthritis and skin rash (21). Another consideration is the inability of monovalent vaccines to elicit broad protection against Ebola virus species other than EBOV, should an epidemic with a non-EBOV species occur. Therefore, it will be advantageous to develop additional Ebola vaccine approaches that may extend durability, enhance breadth, and provide an acceptable safety and tolerability profile for those who are not at immediate risk of developing EVD.
Data from NHP models and from survivors of EVD indicate that effective humoral and cell-mediated immune responses are mounted against Ebola virus antigens during infection (15, 22–30). Anti-Ebola antibody responses generally are detected between weeks 2 and 4 following the onset of symptoms and reported to be absent or diminished in fatal cases of EVD (31–33). The role of anti-Ebola antibodies in protection against EVD has been demonstrated by the successful protection of NHPs administered anti-Ebola GP antibodies in a challenge model (34) and by data from NHP studies (35) and clinical trials evaluating VSV-ZEBOV Ebola vaccine (2, 28, 29, 36–38). Ebola-specific antibodies likely mediate protection through neutralization of the virus as well as through ADCC (19, 25, 39–46). Although some reports have indicated that fatal outcomes in EVD patients are associated with acute T cell deficiencies, as represented by decreased CD4 and CD8 T cell numbers, aberrant cytokine secretion, and T cell apoptosis (33, 47–49), recent studies have reported that there is a substantial activation of Ebola-specific CD4 and CD8 T cells during the acute phase of Ebola infection (23, 30). Preclinical data from studies evaluating adenovirus-based Ebola vaccines have also suggested an integral role for T cells in immune protection against EVD (3, 5, 7, 9, 11, 13–15, 40).
Ebola VLP vaccines incorporating EBOV GP and/or EBOV nucleoprotein (NP) on a filamentous EBOV VP40 core have been shown to be protective in rodent and NHP models of EVD (22, 26, 50, 51). These VLPs incorporate a substantial amount of GP, and, like the virus itself, are filamentous and widely heterogeneous in shape and size. VLP heterogeneity and large size can present problems in VLP production, purification, sterilization, and analysis, potentially limiting the feasibility of this VLP vaccine approach (52). Optimal shape and size are important factors in the design of nanoparticle-based vaccines. Smaller and spherical particles are more efficiently targeted by the lymphatic system to the draining lymph nodes and may be more efficiently taken up by lymph node antigen-presenting cells (53, 54). Therefore, we sought to develop a more uniform nanoparticle Ebola VLP for vaccine purposes. Here, we describe the development and immunogenicity of monovalent and bivalent VLP-based Ebola vaccines that incorporate GP(s) on a spherical Gag core and are readily produced as a homogeneous product from stable and scalable producer cells. Gag-based Ebola VLPs elicited strong humoral and cellular immune responses in rabbits and rhesus macaques. The incorporation of both EBOV GP and SUDV GP significantly extended the breadth of both neutralizing antibody and ADCC responses compared with those of EBOV GP alone. These results support the use of bivalent VLPs to expand the breadth and enhance the durability of responses elicited by current live vector-based Ebola vaccines.
RESULTS
Generation of stable cell lines secreting monovalent and bivalent Ebola VLPs.
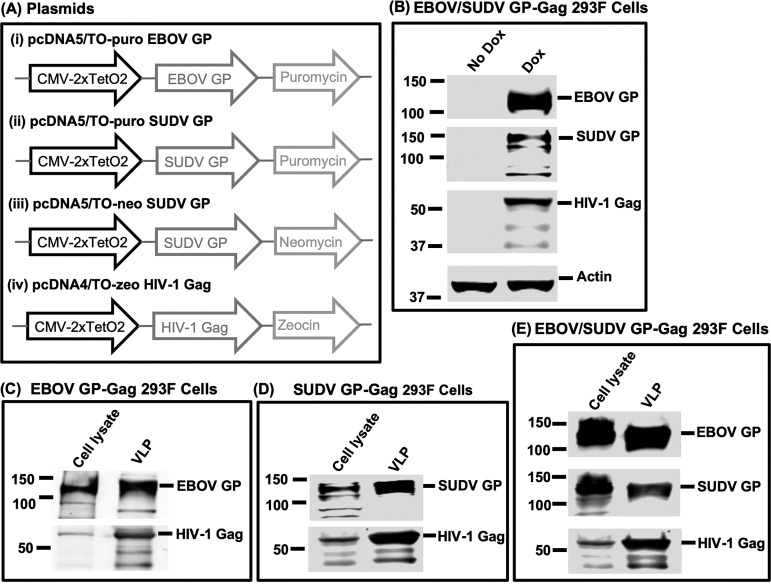
To generate a scalable production system for VLPs, 293F cells (ThermoFisher Scientific, Waltham, MA) were stably transfected with plasmids expressing codon-optimized human immunodeficiency virus type 1 (HIV-1) gag gene together with GP from EBOV or SUDV under a tetracycline-inducible promoter (Fig. 1A). A third cell line capable of secreting bivalent VLPs was generated by stable transfection with three plasmids under individual antibiotic selection to generate the EBOV/SUDV GP-Gag 293F bivalent VLP production line (Fig. 1A and B). Upon induction with doxycycline, EBOV GP-Gag 293F cells secreted VLPs that expressed EBOV GP and HIV-1 Gag (Fig. 1C). Similarly, SUDV GP-Gag 293F cells, upon doxycycline induction, secreted VLPs expressing SUDV GP and HIV-1 Gag (Fig. 1D). VLPs obtained from EBOV/SUDV GP-Gag 293F cells expressed EBOV GP, SUDV GP, and HIV-1 Gag (Fig. 1E).
FIG 1.
Generation of stable cell lines secreting EBOV GP-Gag, SUDV GP-Gag, and bivalent EBOV/SUDV GP-Gag VLPs. (A) Schematics of pcDNA5/TO-puro EBOV GP, pcDNA5/TO-puro SUDV GP, pcDNA5/TO-neo SUDV GP, and pcDNA4/TO zeo HIV-1 Gag plasmids generated to develop different stable cell lines used in this study. (B) 293F cells selected after stable transfections with EBOV GP, SUDV GP, or both and HIV-1 Gag plasmids were cultured as such or induced with doxycycline for 24 h, and cell lysates were probed by Western blotting for EBOV GP, SUDV GP, HIV-1 Gag, and actin using specific antibodies. A representative Western blot from EBOV/SUDV GP-Gag 293F cells is shown. Similar results were obtained with EBOV GP-Gag and SUDV GP-Gag 293F cells. (C to E) Stable cells were induced with doxycycline for 40 h, and cleared supernatants were loaded on 20% sucrose cushions and subjected to ultracentrifugation. VLP pellets so obtained and the corresponding cell lysates were probed by Western blotting using anti-EBOV GP-, anti-SUDV GP-, and anti-HIV-1 Gag-specific antibodies.
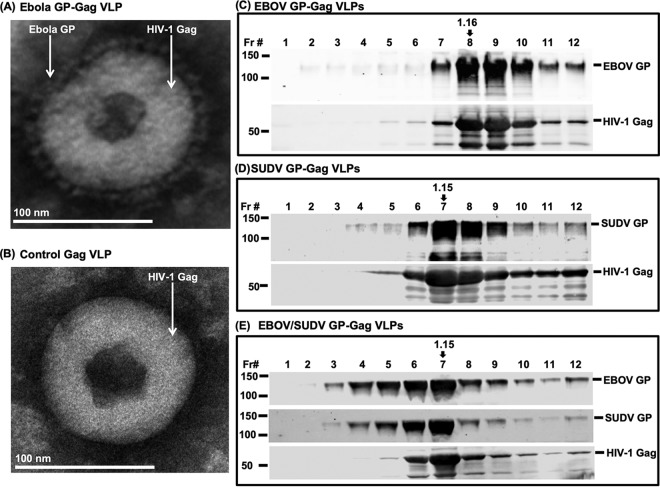
Characterization of Ebola VLPs with a Gag core.
HIV virions incorporate only a limited number of HIV-1 Env trimers on their surfaces (55), a characteristic that would not be desirable in a VLP vaccine construct. To document the density of Ebola GP incorporation onto Gag VLPs and to assess particle morphology, we purified VLPs from producer cell supernatants and pelleted VLPs for examination by negative staining electron microscopy. VLPs were found to be spherical, ∼110 to 130 nm in diameter, with particle cores abundantly covered with Ebola GP spikes (Fig. 2A). The relative amounts of EBOV GP and SUDV GP on the bivalent EBOV/SUDV GP-Gag VLPs were determined by semiquantitative Western blotting using EBOV GP- and SUDV GP-specific antibodies and known amounts of recombinant EBOV GP and SUDV GP. The Gag content of VLPs was quantified using a Gag enzyme-linked immunosorbent assay (ELISA) as previously established (56). The Gag content in different VLP lots varied between 4.2 and 14.8 μg/ml. For every 1 μg of Gag, there was approximately 3.5 μg of EBOV GP and 0.7 μg of SUDV GP present on the bivalent EBOV/SUDV GP-Gag VLPs. Note that for immunizations described below, doses were standardized based on the Ebola GP content. The buoyant density of the VLPs next was determined by ultracentrifugation over 20 to 60% sucrose gradients, followed by analysis of GP and Gag content of each fraction. Ebola VLPs demonstrated peak buoyant densities between 1.14 and 1.16 g/ml, as expected for the density of Gag particles (Fig. 2C to E).
FIG 2.
Characterization of Ebola VLPs by electron microscopy and buoyant density. Ebola VLPs harvested from culture supernatants were analyzed by negative stain electron microscopy. (A and B) The analysis showed spherical particles abundantly covered with spikes of glycoproteins on their surface. (C to E) Equilibrium sucrose density gradient analysis of monovalent and bivalent Ebola VLPs. VLPs harvested from culture supernatants were fractionated by ultracentrifugation on 20 to 60% sucrose gradient. Fractions were analyzed by Western blotting for the presence of EBOV GP, SUDV GP, and HIV-1 Gag using specific antibodies. The refractive index of each fraction was measured and their buoyance density calculated. Densities of the fractions with largest amount of EBOV GP, SUDV GP, and HIV-1 Gag are shown with arrows above each fraction.
Ebola VLPs are immunogenic and induce functional antibodies in rabbits.
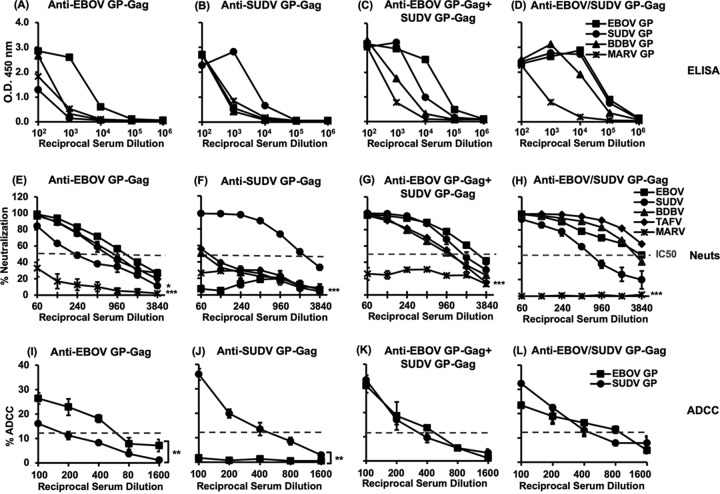
The ability of monovalent and bivalent Ebola VLPs to induce antibody responses in rabbits was evaluated next. Rabbits received four inoculations with VLPs adjuvanted with CpG and poly(I:C), followed by measurement of binding antibodies and functional activity in sera collected 2 weeks following the final booster immunization. Poly(I:C) and CpG were selected as adjuvants based on their strong ability to trigger innate immune signaling pathways downstream of toll-like receptor 3 (TLR3) and TLR9, respectively, which have been shown to trigger the production of type I interferons (IFN-α and IFN-β) and to enhance B and T cell activation and maturation of antigen-presenting cells (57, 58). These adjuvants have been reported to significantly enhance the protective ability of VLP-based vaccines against influenza and Ebola viruses (59–61). Immunization with EBOV GP-Gag VLPs induced anti-EBOV GP binding antibody responses with endpoint antibody titers of 1 × 105 (Fig. 3A). EBOV VLP-induced binding antibodies were cross-reactive with heterologous SUDV GP, Bundibugyo virus (BDBV) GP, and Marburg virus (MARV) GP but at much lower titers (Fig. 3A). Similarly, SUDV GP-Gag VLPs induced strong anti-SUDV GP antibody responses with titers of 1 × 105 and lower cross-reactivity with heterologous GPs (Fig. 3B). We next evaluated the coadministration of monovalent EBOV and SUDV VLPs, which is a potential strategy to enhance breadth. The coadministration of equal amounts of EBOV GP-Gag and SUDV GP-Gag VLPs induced strong antibody responses that were directed against both EBOV GP and SUDV GP. These antibodies showed moderate cross-reactivity with BDBV GP and lower cross-reactivity with MARV GP (Fig. 3C). Bivalent EBOV/SUDV GP-Gag VLPs represent another approach to generate breadth, with both glycoproteins expressed on a Gag core. Interestingly, immunization with bivalent EBOV/SUDV GP-Gag VLPs induced antibodies that reacted strongly not only with EBOV GP and SUDV GP but also with BDBV GP with endpoint antibody titers of 1 × 106, indicating an increase in both titer and breadth (Fig. 3D). These antibodies cross-reacted with MARV GP but at a much lower titer.
FIG 3.
Humoral immunogenicity of Ebola VLPs in rabbits. (A to D) Serum samples collected from rabbits immunized with monovalent or bivalent Ebola VLPs were tested for binding antibodies by ELISA using recombinant EBOV GP, SUDV GP, BDBV GP, and MARV GP as the coating antigens. Shown on the y axis are the average of optical density values from representative experiments repeated thrice. (E to H) Levels of anti-Ebola neutralizing antibodies in immune sera were measured by using an Ebola neutralization assay. HIV-1ΔEnv pseudovirions expressing EBOV GP, SUDV GP, BDBV GP, TAFV GP, or MARV GP were preincubated for 1 h with increasing dilutions of the sera before adding onto the TZM-bl cells expressing luciferase in an HIV-1 tat-dependent manner. Forty-eight hours later, luciferase activity was measured and the percent neutralization calculated. The broken gray line in each panel represents the IC50 value (50% neutralization). Results are shown as means ± standard deviations (SD) of triplicates from representative experiments repeated thrice. Symbols in panel E: *, P value between EBOV versus SUDV; ***, P value between EBOV versus MARV. Symbol in panel F: ***, P values between SUDV versus other pseudovirions. Symbols in panels G and H: ***, P values between MARV versus other pseudovirions. (I to L) ADCC-mediating antibodies in immune sera were measured against target cells expressing either EBOV GP or SUDV GP, with CD16 overexpressing NK-92 effector cells in a luciferase-based Ebola ADCC assay as described in Materials and Methods. Results are shown as means ± SD from three independent experiments. The broken gray line in each panel represents the cutoff of the Ebola ADCC assay used. *, **, and *** represent P values of <0.05, <0.01, and <0.001, respectively.
Sera from rabbits immunized with monovalent VLPs, mixed VLPs, or bivalent VLPs next were tested for their ability to neutralize Ebola viruses in a pseudovirus-based neutralization assay. Remarkably, antisera induced by EBOV GP-Gag VLPs neutralized not only EBOV GP pseudovirions but also those with BDBV GP and Tai Forest virus (TAFV) GP effectively (50% inhibitory concentration [IC50] of 1:960 for EBOV versus 1:480 for BDBV and TAFV). Neutralization of SUDV GP pseudovirions was significantly less effective (IC50 of 1:120, P < 0.05, EBOV versus SUDV, two-tailed paired t test), and little to no neutralization was observed with MARV GP pseudovirions (P < 0.001, EBOV versus MARV) (Fig. 3E). Sera from SUDV GP-Gag VLP-immunized rabbits neutralized only SUDV GP pseudovirions (IC50 of 1:1,920) with very little cross-neutralization of pseudovirions bearing GPs from other filoviruses (P < 0.001, SUDV versus other pseudovirions) (Fig. 3F). Antisera induced by the coadministered EBOV GP-Gag and SUDV GP-Gag VLPs neutralized pseudovirions with individual GPs from all four pathogenic Ebola viruses, with IC50 values of >1:960. No neutralization was observed against pseudoviruses bearing MARV GP (P < 0.001, MARV versus other pseudovirions) (Fig. 3G). Notably, sera from rabbits administered the bivalent EBOV/SUDV GP-Gag VLPs also strongly neutralized pseudovirions with GPs from all four Ebola viruses, with IC50 values of >1:1,920 for EBOV, BDBV, and TAFV and 1:480 for SUDV. The somewhat lower neutralization titers in anti-bivalent Ebola VLP sera observed against SUDV compared with monovalent SUDV VLP immunization may be attributable to the lower content of SUDV GP on the bivalent Ebola VLPs. Again, no neutralization was noted against pseudoviruses bearing the more distantly related MARV GP (P < 0.001, MARV versus other pseudovirions) (Fig. 3H).
ADCC responses have been demonstrated to confer protection against influenza and simian immunodeficiency virus (SIV) in animal models (62–64) and may contribute to vaccine-induced protection against Ebola (39, 65). We employed a recently described Ebola ADCC assay that utilizes target cells expressing EBOV GP or SUDV GP on the cell surface (66) to define ADCC activity of sera from VLP-immunized rabbits. Sera from animals immunized with EBOV GP-Gag VLPs mediated killing of EBOV GP-expressing targets, with significantly lower cross-reactivity against SUDV GP-expressing target cells (P < 0.01, EBOV GP versus SUDV GP, two-tailed paired t test) (Fig. 3I). Sera from SUDV GP-Gag VLP-immunized rabbits elicited ADCC-mediated killing of SUDV GP-expressing cells only, without cross-reactivity against EBOV GP-expressing targets (P < 0.01, SUDV GP versus EBOV GP) (Fig. 3J). Immunization with coadministered monovalent VLPs or that with bivalent EBOV/SUDV GP-Gag VLP produced antisera that effectively mediated killing of both EBOV GP- and SUDV GP-expressing target cells (Fig. 3K and L). Together, these results indicated that while immunization with monovalent EBOV GP-Gag or SUDV GP-Gag VLPs induce functional antibodies that are effective mainly against the specific Ebola proteins, the breadth of these responses can be enhanced by either mixing the two or by incorporation of both EBOV GP and SUDV GP on a single bivalent VLP vaccine. We selected the bivalent Ebola VLP approach as the preferred immunogen for further evaluation in rhesus macaques, reasoning that a single product generating broad responses may be advantageous in terms of production costs and further development.
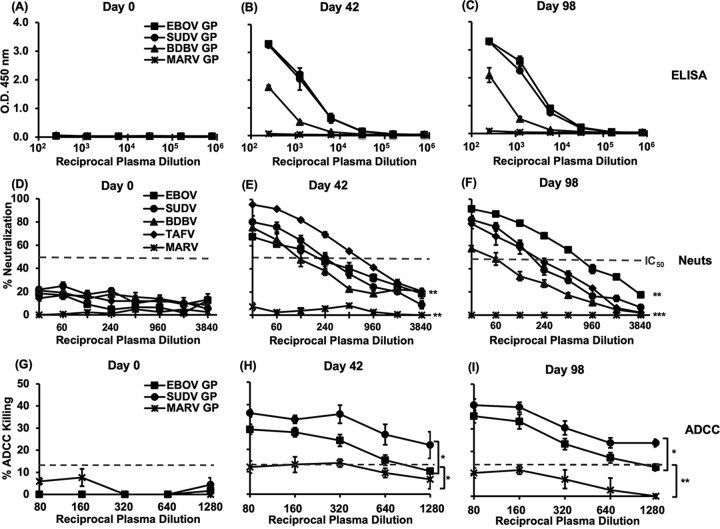
Immunogenicity of bivalent EBOV/SUDV GP-Gag VLPs and functionality of anti-Ebola GP antibodies generated in rhesus macaques.
To study the spectrum of immune responses induced by bivalent Ebola VLPs, rhesus macaques were immunized with VLPs (100 μg based on EBOV GP content) mixed with CpG and R848 adjuvants at 0, 4, and 12 weeks (days 0, 28, and 84). Although VLPs have some self-adjuvanting properties, VLP-based vaccines administered without adjuvants demonstrate limited immunogenicity and are generally coadministered with relevant adjuvants to augment the immunogenicity and durability of the induced immune responses (67–70). CpG and R848 were employed as adjuvants with Ebola VLP vaccines in our immunogenicity studies in rhesus macaques, as this combination has been shown to elicit high titers of binding, neutralizing, and ADCC-mediating antibodies against HIV-1 when using protein or VLP vaccines in this animal model (71–74). Binding anti-EBOV GP and anti-SUDV GP antibody responses were undetectable at day 0 and rose to endpoint titers of >1 × 104 2 weeks following the second immunization (Fig. 4B, day 42). These antibodies cross-reacted with BDBV GP at a low titer, and there was no cross-reactivity to MARV GP (Fig. 4A and B). As we had seen some low-level cross-reactivity versus MARV GP in rabbits, this complete lack of cross-reactivity was not expected but may represent species-specific differences in the dominant epitopes eliciting B cell responses. The additional booster dose administered on day 84 only marginally enhanced the titers of antibodies against different filo-GPs (Fig. 4C, day 98). We next assessed functional antibody responses in immunized macaques. Bivalent VLP immunization elicited neutralizing antibody responses in macaques against all four pathogenic Ebola viruses but not against MARV (P < 0.01, EBOV versus MARV and SUDV versus MARV, Wilcoxon matched-pairs signed rank test), with IC50 values that ranged between 1:120 and 1:480 (EBOV and SUDV, 1:240; BDBV, 1:120; and TAFV, 1:480). The higher responses against TAFV (P < 0.01, EBOV versus TAFV) in sera from this time point were unexpected (Fig. 4E, day 42). The second VLP booster enhanced the EBOV neutralizing titers (IC50, 1:480) with little change in titers for the other Ebola viruses (P < 0.01, EBOV versus TAFV) (Fig. 4F, day 98), suggesting enrichment and maturation of antibodies specific for critical epitopes of EBOV GP upon this booster immunization. In summary, of the neutralizing antibody responses, bivalent VLPs elicited neutralization against all four pathogenic Ebola species at reasonable titers.
FIG 4.
Humoral immunogenicity of bivalent EBOV/SUDV GP-Gag VLPs in rhesus macaques. (A to C) Rhesus macaques were immunized with bivalent EBOV/SUDV GP-Gag VLPs, and plasma samples collected on day 0 (A), day 42 (B), and day 98 (C) were tested for the presence of anti-EBOV GP, SUDV GP, BDBV GP, and MARV GP binding antibodies by ELISA. Results are expressed as means ± standard errors of the means (SEM) of data obtained from 4 animals run in duplicate. (D to F) Plasma samples collected on day 0, day 42, and day 98 were tested for the presence of anti-Ebola neutralizing antibodies using recombinant HIV-1△Env pseudovirions bearing different Ebola/MARV GPs. Results are expressed as means ± SEM of data obtained from 4 animals run in duplicate. Broken gray lines represent IC50 values (plasma dilution giving 50% virus neutralization). Symbols in panel E: **, lower, P values between EBOV versus MARV and SUDV versus MARV; **, upper, ** P value between EBOV versus TAFV. Symbols in panel F: ***, P values between MARV versus other pseudovirions; **, P values between EBOV versus TAFV. (G to I) Plasma samples collected on day 0, day 42, and day 98 were tested for the presence of ADCC killing anti-EBOV GP and anti-SUDV GP antibodies using EBOV GP- or SUDV GP-expressing target cells and natural killer cells overexpressing CD16 as effector cells. Target cells expressing MARV GP were used as controls. Results from a representative experiment are shown as means ± SEM of data obtained from 4 animals. The broken gray line in each panel represents the cutoff of the Ebola ADCC assay used. *, **, and *** represent P values of <0.05, <0.01, and <0.001, respectively.
ADCC responses were evaluated next against EBOV, SUDV, and control MARV GP-expressing target cells. Antisera from bivalent VLP-immunized macaques elicited ADCC-mediated killing of target cells expressing either EBOV GP or SUDV GP on their surfaces, with the slightly higher killing of SUDV GP over EBOV GP-expressing target cells (P < 0.05) (Fig. 4H, day 42). These values were only slightly enhanced following the additional VLP boost (Fig. 4I, day 98). No ADCC-mediated killing was observed when cells expressing MARV GP were used as the target cells in these assays (Fig. 4H and I). These results indicate that functional antibodies mediating both virus neutralization and ADCC against multiple Ebola species were elicited by immunization with bivalent VLPs.
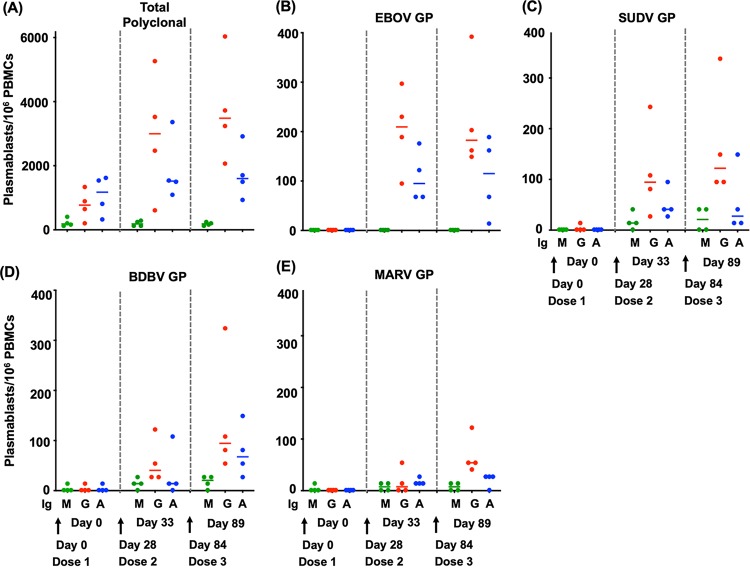
Anti-Ebola GP plasmablast responses elicited by bivalent Ebola GP-Gag VLPs in rhesus macaques.
Plasmablasts secreting total and Ebola GP-specific IgM, IgG, and IgA antibodies next were enumerated using an enzyme-linked immunosorbent spot (ELISpot) assay in which either polyclonal anti-monkey IgG-IgA-IgM antibodies or recombinant EBOV, SUDV, BDBV, or MARV GP were used as coating antigens. As shown in Fig. 5A, 5 days after the first boost there was an increase in the frequencies of total IgG-secreting plasmablasts relative to baseline (P = 0.059, baseline versus day 33, two-tailed paired t test), with values ranging between 608 and 5,265 per million peripheral blood mononuclear cells (PBMCs). These values were increased slightly following the second booster dose (P = 0.016, baseline versus day 89). The frequencies of total IgA-secreting plasmablasts increased slightly after the booster immunization but did not reach statistical significance compared with the baseline (Fig. 5A). EBOV GP- and SUDV GP-specific IgG plasmablast responses were present following each VLP boost, ranging between 95 and 297 cells and 27 and 243 cells per million PBMCs for EBOV GP- and SUDV GP-specific plasmablasts, respectively (P = 0.018, baseline versus day 33, and P = 0.028, baseline versus day 89, for EBOV GP; P = 0.082, baseline versus day 33, and P = 0.056, baseline versus day 89, for SUDV GP) (Fig. 5B and C). Boosting with VLPs also led to an increase in the frequencies of IgA-secreting EBOV GP- and SUDV GP-specific plasmablasts with numbers between 68 and 176 and 41 and 95 per million for EBOV GP- and SUDV GP-specific plasmablasts, respectively (P = 0.025, baseline versus day 33 for EBOV GP, and P = 0.045, baseline versus day 33 for SUDV GP) (Fig. 5B and C). Two out of the four animals also exhibited detectable numbers of IgG-secreting plasmablasts against BDBV GP in blood (range, 54 to 122) (P = 0.07, baseline versus day 33) (Fig. 5D). The number of anti-BDBV GP IgG-secreting plasmablasts showed an upward trend after the second booster dose. Plasmablasts specific for MARV GP were either undetectable or at very low levels (Fig. 5E). In summary, Ebola-GP-specific plasmablast responses were readily detected and were generally consistent with the binding and functional antibody responses shown in Fig. 4A to C.
FIG 5.
Frequencies of plasmablasts in PBMCs collected from rhesus macaques immunized with bivalent EBOV/SUDV GP-Gag VLPs. Rhesus macaques were immunized with bivalent EBOV/SUDV GP Gag VLPs, and frequencies of IgM-, IgG-, and IgA-secreting polyclonal (A), anti-EBOV GP (B), anti-SUDV GP (C), anti-BDBV GP (D), and anti-MARV GP (E) plasmablasts were measured on day 0, day 33 (5 days after the first VLP booster), and day 89 (5 days after the second VLP booster). Results are displayed as plasmablasts per million PBMCs. M, G, and A stand for IgM, IgG, and IgA, respectively.
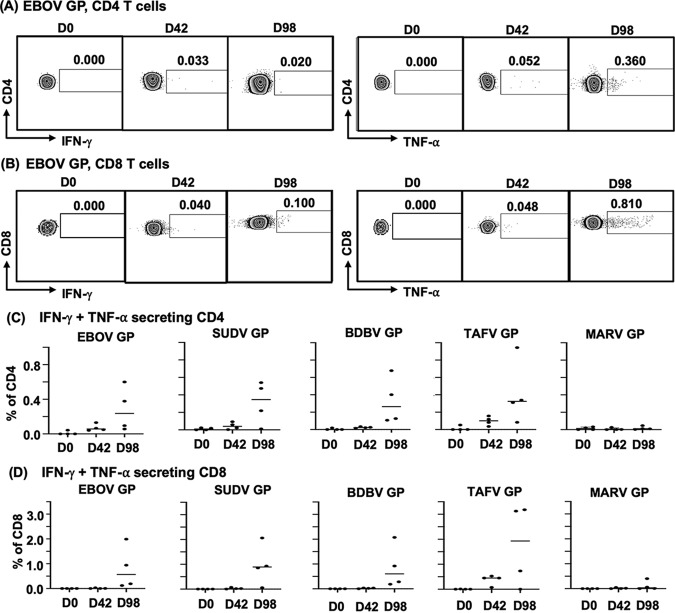
Ebola GP-specific T cell responses elicited by bivalent EBOV/SUDV GP-Gag VLPs in rhesus macaques.
We anticipated that an Ebola VLP approach would generate low but measurable cellular responses against Ebola GP antigens. Antigen-specific cellular responses were evaluated in an intracellular cytokine staining (ICS) assay for IFN-γ and tumor necrosis factor alpha (TNF-α). Representative dot blots for CD4 and CD8 T cells secreting IFN-γ or TNF-α in response to restimulation with EBOV GP are shown in Fig. 6A and B, respectively. Summary data from four animals showing frequencies of cytokine-secreting (IFN-γ and TNF-α) CD4 and CD8 T cells in response to restimulation with different Ebola GPs are shown in Fig. 6C and D. Note that the results shown in Fig. 6C and D represent the sum of all antigen-specific cytokine-secreting cells, whether single or double. IFN-γ and TNF-α CD4 T cell responses to Ebola GP were generally low after the first 2 immunizations (Fig. 6A and C). However, CD4 T cells collected after the second VLP boost showed detectable antigen-specific responses in all four animals against EBOV GP and in 3 out of 4 animals against SUDV GP. All four animals also had detectable cytokine-secreting CD4 T cells upon restimulation with heterologous BDBV GP or TAFV GP (Fig. 6C). There was no detectable CD4 T response to MARV GP (Fig. 6C). Ebola virus GP-specific CD8 T cell responses were also elicited at low but detectable levels and were slightly higher than those of CD4 responses (Fig. 6B and D). CD8 T cells from one animal also responded to MARV GP at a low level (Fig. 6D). There was an overall trend toward higher frequencies of peripheral CD4 and CD8 T cells responding to different Ebola GPs compared to the MARV GP control. These data indicate that the nonreplicating VLP vaccine approach generates a low level of Ebola virus GP-specific cellular immune responses.
FIG 6.
Frequencies of cytokine-secreting (IFN-γ and TNF-α) CD4 and CD8 T cells in PBMCs from rhesus macaques. Rhesus macaques were immunized with bivalent Ebola VLPs as described in the text, and PBMCs collected on day 0, day 42, and day 98 were frozen in liquid nitrogen. Cells were thawed, rested overnight, and then stimulated for 12 h with recombinant EBOV GP, SUDV GP, BDBV GP, MARV GP (all expressed in mammalian cells), or TAFV GP (expressed in bacterial cells) in the presence of secretion inhibitor. Following stimulation, cells were washed and stained for surface CD3, CD4, and CD8. Cells were fixed, permeabilized, and then stained for IFN-γ and TNF-α. Frequencies of CD4 and CD8 T cells positive for IFN-γ and TNF-α were determined by FlowJo analysis. (A and B) Representative dot blots of CD4 and CD8 T cells secreting IFN-γ or TNF-α upon restimulation with EBOV GP. (C and D) Summary of CD4 and CD8 T cells secreting IFN-γ and/or TNF-α upon restimulation with different filovirus GPs obtained from four animals.
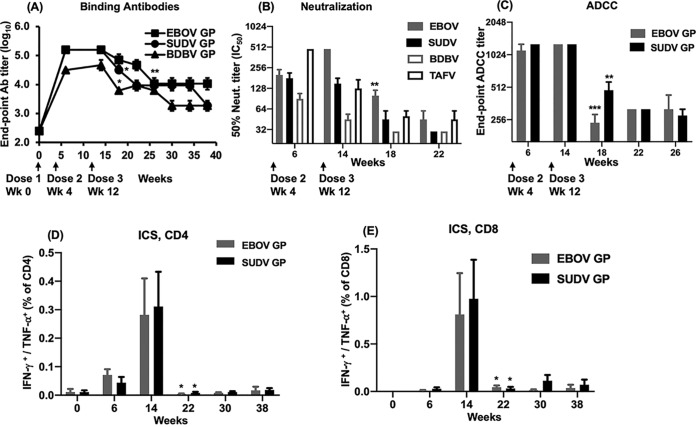
Durability of Ebola-specific immune responses following Ebola-VLP immunization.
The durability of humoral and cellular responses is an important consideration in evaluating candidate Ebola vaccines. Rhesus macaques immunized with bivalent Ebola VLPs were monitored for 26 weeks after the second booster dose to define the durability of Ebola-specific immune responses. Binding antibody titers against EBOV, SUDV, and BDBV demonstrated a decline from peak titers over this time period. While a significant decline in anti-EBOV GP antibody titers was observed starting at week 26 (P = 0.006, two-tailed paired t test), the decline was more rapid for anti-SUDV GP and anti-BDBV GP antibodies, with antibody titers declining significantly at week 18 (P = 0.029 for anti-SUDV GP and P = 0.015 for anti-BDBV GP). Anti-EBOV GP responses remained positive at endpoint titers of ∼1 × 104 6 months after the last VLP boost, with somewhat lower titers for SUDV GP and BDBV GP (Fig. 7A). Neutralizing antibody titers (IC50) peaked after the booster VLP doses with titers ranging from 1:40 to 1:480 and then declined significantly at week 18 (P < 0.01). At ten weeks after the second booster, IC50 titers against individual viruses ranged from 1:30 to 1:60 (Fig. 7B). Of note, 1:30 is the lowest plasma dilution that can be accurately determined by this assay, and lower plasma dilutions lead to nonspecific cell killing. ADCC killing activity against EBOV GP- or SUDV GP-expressing target cells was highest after the first immunization boost, with endpoint titers as high as 1:1,280. As observed for neutralizing activity, ADCC killing activity declined significantly by week 18 (P < 0.01, two-tailed paired t test) but remained detectable in plasma up to week 26 (14 weeks after the last booster dose) (Fig. 7C). IFN-γ- and TNF-α-secreting CD4 and CD8 T cell responses declined rapidly following the peak at week 14 (P < 0.05, week 14 versus week 22, two-tailed ratio paired t test), although very low numbers of both antigen-specific CD4 and CD8 T cells still could be detected as late as week 38 (Fig. 7D and E). These results indicate that immunization with bivalent EBOV/SUDV GP-Gag VLPs induced high levels of anti-Ebola GP antibody responses in rhesus macaques, and that binding antibodies were maintained with moderate durability of functional antibodies and rapid decline of cellular immune responses over ensuing weeks.
FIG 7.
Durability of Ebola-specific immune responses in rhesus macaques. Plasma and/or PBMC samples were collected from the rhesus macaques, every 4 weeks for 6 months, after the last VLP booster dose. Plasma samples were analyzed for the presence of binding (A), neutralizing (IC50 values) (B), and ADCC-mediating (C) anti-Ebola GPs antibodies and data plotted versus time. Results are expressed as means ± SEM of data obtained from 4 animals. Plasma samples from none of the animals neutralized >50% at 1:30 dilution (lowest dilution used in this assay) after week 22. Similarly, plasma samples from none of the animals showed ADCC killing higher than the background levels after week 26. PBMC samples were analyzed for the presence of CD4 and CD8 T cells secreting IFN-γ and TNF-α upon restimulation with EBOV GP or SUDV GP. Data were plotted as percent frequencies of cytokine-secreting (IFN-γ and/or TNF-α) CD4 (D) and CD8 (E) T cells versus time (weeks). Results are expressed as means ± SEM of data obtained from 4 animals. *, **, and *** represent P values of < 0.05, <0.01, and <0.001, respectively, and are placed at the first time point after the peak response at which the antibody titers or cell frequencies showed a statistically significant decline.
DISCUSSION
In this study, we evaluated a new type of Ebola VLP vaccine expressing EBOV GP, SUDV GP, or both, present on a spherical HIV-1 Gag core. The expression of Gag directed the formation of spherical particles that incorporated Ebola GPs in a dense array on the lipid bilayer of the VLP. The design included the incorporation of both EBOV GP and SUDV GP with the intent of broadening responses to all pathogenic Ebola virus species that infect humans. Initial immunogenicity studies with monovalent VLPs in rabbits were encouraging, indicating that VLP immunization elicits strong binding, neutralizing, and ADCC responses. However, we noted that monovalent EBOV GP-Gag VLP immunization elicited cross-reactive binding and functional antibodies against BDBV and TAFV but with much lower responses against SUDV. Immunization with a mixture of monovalent EBOV GP-Gag and SUDV GP-Gag VLPs or with bivalent VLPs incorporating both EBOV GP and SUDV GP on a single particle generated higher binding and neutralizing antibody titers against all pathogenic Ebola virus species. Given simpler production and development processes for a single bivalent VLP product compared with those of mixed monovalent VLPs, we pursued the further evaluation of the bivalent VLPs in rhesus macaques. Immunization of rhesus macaques with bivalent Ebola VLPs elicited strong anti-EBOV GP and anti-SUDV GP antibodies that also cross-reacted with GP from BDBV. Neutralizing antibody responses and ADCC responses were also cross-reactive, suggesting that the bivalent VLP approach can elicit immune responses directed against multiple pathogenic Ebola virus species.
Live vector-based vaccines against Ebola have advanced the farthest in human trials, including the VSV-ZEBOV vaccine, which has been shown to provide protection in the epidemic setting (2), and adenoviral vector-based regimens that are protective in the NHP model and safe and immunogenic in humans (3, 5, 8, 17). The VSV-based approach generates IgG-mediated protection against lethal filovirus challenge in rodents and nonhuman primates (29, 75) yet elicits relatively modest binding antibody titers against EBOV GP (endpoint titers in cynomolgus macaques of 102 to 103 prior to challenge [76]). Adenoviral vectors, in contrast, appear to protect in nonhuman primate models primarily via CD8+ T cell responses (15), although IgG-mediated responses can serve as a predictive correlate in macaques receiving recombinant adenovirus immunization. In this analysis, a potential 100% antibody protective titer in macaques receiving an adenovirus type 5 Ebola vaccine was predicted as 1:3,700 by IgG ELISA (77). The VLP approach described here was designed primarily to elicit protective antibodies. A direct comparison between VLPs described here and the vectors currently advancing in human trials was not performed, and we recognize that only a challenge study will establish the ability of Gag-based Ebola VLPs to generate protective immunity. Nevertheless, the titers of binding and neutralizing antibodies are comparable to or greater than those reported with other approaches. VLPs generated endpoint titers by ELISA of >1 × 104, which compare favorably with prechallenge levels reported in macaques for VSV-ZEBOV (76) and are in the same range of titers seen with VP40-based Ebola virus VLP vaccines that were also shown to be protective in nonhuman primates (22).
The current epidemic in the DRC illustrates the fact that Ebola remains a threat. The pursuit of an effective killed or non-live Ebola vaccine is worthwhile, even with more advanced live vector vaccines moving forward. Vaccines that are currently being deployed to contain spread in an epidemic setting may not be acceptable for all populations at risk, such as health care workers, travelers to epidemic regions who have not yet been exposed, or individuals with compromised immune systems. Protection against infection with species other than EBOV through vaccination has not yet been established. The waning of protective immunity in vaccinated individuals is likely to require boosting in the setting of reexposure in high-risk regions, and effective boosting may require either a heterologous vector or a recombinant protein or VLP approach. Furthermore, killed or inactivated vaccines may have advantages even when a protective live vector is available. For example, the inactivated (Salk) poliovirus vaccine is safe in immunocompromised individuals and lacks the potential of reversion to virulence, while the live oral (Sabin) vaccine is advantageous in terms of its ease of administration and ability to stimulate mucosal immunity. The fact that both live and killed vaccines now are being employed by the World Health Organization to achieve the eradication of polio illustrates the principle that it is best to have a choice of tools available in combating infectious diseases (78).
We note that Ebola vaccines deployed in the epidemic setting will need to rapidly elicit protective immune responses. While we do not yet have data proving protection from Ebola using Gag-GP Ebola VLPs, the immunogenicity data from rhesus macaques presented here indicate that one VLP prime followed by one VLP boost elicits substantial titers of functional antibodies. The plateau in antibody responses after 2 doses that we observed is similar to that reported for a VP40-based VLP vaccine candidate (51). We therefore propose that if used alone, a VLP approach will require two doses of vaccine, similar to the dosing required for the ChAd3 prime/MVA boost and Ad26 prime/MVA boost regimens moving forward in human trials currently (7, 9). The VLP approach also could be employed as a booster following a live vector prime and result in broadening of immune responses, a concept worthy of further study in animal models.
VLPs have potential advantages as vaccines. Human papillomavirus (HPV) vaccines are VLPs produced by the production of recombinant L1 protein that self-assembles to form empty capsid shells (79, 80). HPV vaccines have proven highly immunogenic and protective in human trials (79). VLPs can mimic the native presentation of antigens and present them effectively to antigen-presenting cells in a multivalent fashion (81–83), potentially making them attractive as a platform for generating responses to many pathogens. Filamentous VLPs for Ebola virus have been established as a means of protecting against Ebola viruses in mouse and NHP models (22, 50, 51, 84–86). They have been proposed as a means of developing a pan-filovirus vaccine due to the ability to incorporate multiple GPs and elicit cross-protective immunity (85). The work described here builds on this previously published work. The use of a heterologous shell from the HIV-1 Gag protein provides an alternative spherical VLP capable of incorporating multiple GPs, with potential advantages in production and purification that come from a uniform product. Small (<200 nm) spherical VLPs are easy to purify, and products are generally more stable than large and heterogeneous preparations (52). These particles also may be taken up much more efficiently than the bulky filamentous ones by antigen-presenting cells, such as macrophages and dendritic cells (53). In the present study, a Gag core efficiently incorporated Ebola GPs and elicited functional antibody responses in both the rabbit and NHP model, suggesting that this approach is a promising one.
The durability of protective immune responses is an important parameter to consider for Ebola vaccine development. While protective responses of relatively short duration may be effective in protecting individuals at risk for EVD during an outbreak, ideally protective immunity would extend beyond the outbreak to provide years of protection. Healthcare workers who may be repeatedly at risk of Ebola exposure will require prolonged protection. In the present study, EBOV GP, SUDV GP, and BDBV GP binding antibodies were maintained in plasma samples collected as late as 6 months after the last booster, although their endpoint titers decreased slowly over time. The initial high levels of anti-Ebola-neutralizing and ADCC killing-mediating antibodies also declined over time but showed reasonable durability for a nonreplicating VLP vaccine approach. The extent of protection of this approach has not yet been established and will need to be directly evaluated in an Ebola challenge model. However, we suggest that bivalent VLP boosting following a live vector vaccination is of particular interest in the future. This approach has the potential to expand both the breadth and durability of immune responses generated by live vector vaccination.
The induction of cellular immune responses against Ebola was not the primary goal of this VLP approach, yet the vaccine induced clearly detectable clonal expansions of EBOV GP- and SUDV GP-specific T cells, as evidenced by the detection of cytokine-producing T cells upon restimulation with Ebola GPs in vitro. The frequencies of Ebola GP-specific CD4 and CD8 T cells were roughly equivalent in magnitude to those observed after immunization of rhesus macaques with adenovirus-based Ebola vaccines that mediate protection through T cell-dependent mechanisms (13, 14). The induction of effector CD8 T cell responses was relatively slow in these animals, requiring three immunizations to generate detectable immune responses. However, similar to antibody responses, cell-mediated responses induced by bivalent VLPs were broadly specific for all four pathogenic Ebola viruses, underlining the breadth of the responses induced by this approach. The magnitude of EBOV GP- and SUDV GP-specific helper CD4 T cells secreting IFN-γ and/or TNF-α was also low but detectable after the first VLP booster and increased significantly following the second VLP booster. Therefore, VLPs elicited low levels of broadly cross-reactive CD4+ and CD8+ T cells against all Ebola GPs. It will be of interest in future studies to determine if potentially protective cellular responses generated by live vector approaches can be effectively boosted using Ebola VLPs.
In summary, a bivalent, spherical Ebola VLP approach elicits potent and functional antibody responses and detectable cellular responses against each of the four species of Ebola that cause disease in humans. Bivalent VLPs have the potential to provide protection against Ebola as a stand-alone regimen or to broaden and extend the durability of protection offered by live vector vaccine approaches. Future studies are needed to establish protection in relevant animal models and to directly examine VLP boosting following priming with live vector vaccines.
MATERIALS AND METHODS
Generation of Ebola GP-Gag VLP production cell lines.
Schematics of all the plasmids used in this study are shown in Fig. 1A. Plasmid pcDNA5/TO-puro EBOV GP (Mayinga) was created as described in Singh et al. (66). Briefly, a codon-optimized EBOV GP (Mayinga) gene was synthesized by GenScript (Piscataway, NJ) and placed under a tetracycline-controlled cytomegalovirus (CMV) promoter into plasmid pcDNA5/TO-puro using BamHI and EcoRI sites. Similarly, plasmid pcDNA5/TO-puro SUDV GP (Gulu) was created by cloning a codon-optimized SUDV GP (Gulu) gene obtained from Sino Biological (Beijing, PRC) between the BamHI and EcoRI sites of pcDNA5/TO-puro. Plasmid pcDNA5/TO-neo SUDV GP (Gulu) was created by cloning a codon-optimized SUDV GP (Gulu) gene between the BamHI and EcoRI sites of pcDNA5/TO-neo. Plasmid pcDNA4/TO-zeo HIV-1 Gag was created by introducing the PCR fragment of codon-optimized HIV-1 Gag into pcDNA4/TO (Invitrogen, Carlsbad, CA) plasmid containing a Zeocin-resistant gene sequence. For the examination of transient expression, 293T cells (ThermoFisher Scientific, Waltham, MA), cultured in Dulbecco’s modified Eagle’s medium (DMEM) (Gibco, Grand Island, NY) supplemented with 10% fetal bovine serum (FBS) (Sigma-Aldrich, St. Louis, MO), 1× GlutaMAX (Gibco), 100 IU/ml penicillin, and 100 μg/ml streptomycin (both Mediatech, Manassas, VA), were transfected with the indicated plasmids using Lipofectamine 2000 (Invitrogen, Carlsbad, CA). Cells were harvested 24 h later, and cell lysates were analyzed by Western blotting using specific antibodies against EBOV GP or SUDV GP (both from IBT Bioservices, Rockville, MD) and HIV-1 Gag (183-H12-5C; NIH AIDS Reagent Program).
To generate inducible stably transfected cells, 293F 6T/R cells (ThermoFisher Scientific) were cultured in FreeStyle 293 expression medium (ThermoFisher Scientific) supplemented with 5.0 μg/ml blasticidin (Invivogen, San Diego, CA). Cells were transfected with pcDNA4/TO-zeo HIV-1 Gag and either pcDNA5/TO-puro EBOV GP or pcDNA5/TO-puro SUDV GP plasmids using Lipofectamine 2000. Forty-eight hours later, cells were transferred into fresh medium supplemented with 5.0 μg/ml blasticidin, 10.0 μg/ml Zeocin (Invivogen), and 1.0 μg/ml puromycin (Invivogen), and antibiotic-resistant cells were selected over the next 3 to 4 weeks. Protein expression was elicited via the addition of 2.0 μg/ml doxycycline (Sigma-Aldrich) for 24 h, and lysates were prepared from induced and uninduced cells for Western blotting for EBOV GP or SUDV GP, HIV-1 Gag, and actin (Santa Cruz Biotechnology, Dallas, TX) using specific antibodies as listed above. Bivalent VLP producer cells were constructed by transfection of 293F 6T/R cells with pcDNA4/TO-zeo HIV-1 Gag, pcDNA5/TO-puro EBOV GP, and pcDNA5/TO-neo SUDV GP plasmids, followed by selection in appropriate antibiotic-supplemented media and protein analysis as before.
Production and characterization of Ebola VLPs.
293F 6T/R stable cells were grown in 40 ml of FreeStyle 293 expression medium, supplemented with relevant antibiotics, in 100-ml Erlenmeyer flasks. Cells were grown in suspension cultures, on a shaker set at 125 rpm, inside a 37°C, 8% CO2 incubator. When cell density reached ∼1.0 × 106/ml, cells were induced with 2.0 μg/ml of doxycycline (Sigma-Aldrich), and cultures continued for another 40 h. Culture supernatants were harvested and cleared by centrifugation at 5,000 × g at 4°C for 10 min, followed by filtration through a 0.45-μm filtration unit. Cleared supernatants were layered onto sterile 20% sucrose cushions in ultracentrifuge-compatible tubes and centrifuged at 30,000 rpm (110,500 × g) at 4°C for 1.5 h in an ultracentrifuge (SW32 Ti rotor; Beckman Coulter, Atlanta, GA), and VLP pellets were resuspended in cold sterile phosphate-buffered saline (PBS), pH 7.4. VLPs, along with the corresponding cell lysates, were probed by Western blotting for EBOV GP, SUDV GP, and HIV-1 Gag using specific antibodies. For determining buoyant density, VLPs were layered on the top of a 20 to 60% sucrose gradient and centrifuged at 35,000 rpm (151,200 × g) at 4°C for 16 h (SW41 rotor; Beckman Coulter). Equal fractions were collected and probed for EBOV GP, SUDV GP, and HIV-1 Gag using specific antibodies by Western blotting. The refractive index of the gradient fractions was measured on a refractometer, and buoyant density was calculated.
Electron microscopy.
For negative electron microscopic studies, VLPs isolated after ultracentrifugation on 20% sucrose cushions were resuspended in cold PBS. Nickel grids of 300 mesh with Formvar-supporting membrane (Electron Microscopy Sciences, Hatfield, PA) were glow discharged just before use and VLP specimens dropped on the grids. Grids were cleaned, air dried, and subjected to negative staining with 1% phosphotungstic acid (PTA) in distilled water, pH 7.4. Grids were cleaned, air dried, and examined using a Hitachi H7650 transmission electron microscope in the Pathology Research Core at Cincinnati Children’s Hospital Medical Center, Cincinnati, OH.
Immunization of rabbits for production of anti-Ebola VLP sera.
New Zealand White rabbits housed at CoCalico Biologicals, Inc. (Reamstown, PA), were utilized for initial studies of VLP immunogenicity under a protocol approved by the Institutional Animal Care and Use Committee (IACUC). Rabbits (n = 2 per vaccine group) were inoculated with VLP preparations equivalent to 10 μg of EBOV GP, SUDV GP, or both (for the monovalent VLPs) or 10 μg of EBOV GP and 2 μg of SUDV GP (for the bivalent VLPs) on day 0, with booster doses on day 21, day 42, and day 70. All doses included 200 μg of poly(I:C) (InvivoGen) and 500 μg of CpG oligodeoxynucleotides (ODNs) (IDT, Coralville, IA) as adjuvants. Sera were collected following a terminal bleed on day 84. Sera collected were heat inactivated at 56°C for 30 min, aliquoted, and either used immediately in various assays or frozen at –80°C for future use.
Immunization of rhesus macaques and immune analysis plan.
Adult Indian rhesus macaques (Macaca mulatta) were used in this study (body weight, 10 to 11 kg [average, 10.46 ± 0.06 kg]; age, 10 to 11 years [averages, 10.54 ± 0.07 years]). Animals were housed and maintained at the New Iberia Research Center (NIRC) of the University of Louisiana at Lafayette in accordance with the rules and regulations of the Committee on the Care and Use of Laboratory Animal Resources. The study was reviewed and approved by the University of Louisiana at Lafayette IACUC prior to its initiation. All animals were negative for SIV, simian T cell lymphotropic virus, and simian retrovirus. The immunization schema included priming of rhesus macaques with a VLP dose containing 100 μg of EBOV GP mixed with 500 μg of CpG ODNs (IDT) and 800 μg of R848 (InvivoGen), followed by a booster dose on day 28. Blood was collected on day 33 for antigen-specific and total plasmablast analysis and on day 42 for antibodies and cellular immune analysis. To investigate the recall responses, animals received a second VLP booster dose on day 84. Plasmablast responses were analyzed on day 89 and antibodies and cellular immune responses on day 98. For isolation of plasma and PBMCs, peripheral blood was collected in CPT tubes containing sodium citrate (BD Vacutainer) and processed according to the manufacturer’s instructions. PBMCs were either cryopreserved in RPMI plus 20% FBS plus 7.5% dimethyl sulfoxide (DMSO) and stored in liquid nitrogen or resuspended in complete RPMI medium for immediate use in plasmablast ELISpot assays. Preimmunization plasma and PBMC samples were collected from each animal to be included as controls in each assay.
Binding antibody measurement.
Binding antibody titers against different Ebola GPs were determined by ELISA using recombinant proteins as coating antigens. Briefly, duplicate wells of ELISA plates (Immuno plates; Thermo Scientific) were coated with 20 ng/well of each recombinant GP (recombinant EBOV GP, SUDV GP, BDBV GP, and MARV GP; all from IBT Bioservices, Rockville, MD), blocked with 5% skim milk for 1 h at 37°C, and incubated for 2 h at 37°C with different dilutions of serum/plasma. Following washing with PBS-Tween 20, plates were incubated with a 1:5,000 dilution of horseradish peroxidase (HRP)-conjugated secondary antibodies (Invitrogen) for 1 h at 37°C. Plates were washed and reactions developed by adding tetramethylbenzidine (TMB) substrate (Thermo Scientific) for up to 15 min. Reactions were stopped by the addition of 4N H2SO4, and optical density (OD) was read at 450 nm in an ELISA reader (Molecular Devices, San Jose, CA).
ELISpot assay.
Total and Ebola-specific plasmablast responses in blood were determined by ELISpot assay as previously described (87). Briefly, 96-well multiscreen HTS filter plates (Millipore, Burlington, MA) were coated overnight at 4°C with 100 μl/well of 10 μg/ml goat anti-monkey IgG-IgA-IgM (H&L) antibodies (Rockland, Limerick, PA) or 1.0 μg/ml recombinant EBOV GP, SUDV GP, BDBV GP, or MARV GP (all from IBT Bioservices). Plates were washed with PBS–0.05% Tween 20 (PBS-T) and blocked with complete RPMI medium at 37°C for 2 h. Freshly isolated PBMCs were resuspended in complete RPMI medium, plated in serial 3-fold dilutions in duplicates, and incubated overnight in a 5% CO2 incubator at 37°C. Plates were washed with PBS followed by PBS-T and then incubated with either anti-monkey IgM-, IgG-, or IgA-biotin-conjugated antibody (Rockland) diluted 1:1,000 for 1 h at 37°C. After washing, the plates were incubated with HRP-conjugated Avidin D (Vector Labs, Burlingame, CA) diluted 1:1,000 at room temperature for 1 h and finally developed using the AEC substrate kit (BD Biosciences, San Jose, CA). To stop the reaction, plates were washed extensively with water, followed by air drying. Spots were imaged and counted using the immunospot ELISpot analyzer (Cellular Technology Limited, Shaker Heights, OH). The number of spots specific for each Ig isotype was reported as the number of either total polyclonal or antigen-specific spots per million PBMCs.
Ebola neutralization assay.
The Ebola neutralization assay used in this study was a pseudotyping assay adapted from the TZM-bl HIV-1 neutralization assay (88, 89). Briefly, EBOV, SUDV, BDBV, TAFV, and MARV pseudovirions were generated by transient transfection of 293T cells with recombinant HIV-1ΔEnv containing plasmid and plasmid expressing one of the above-mentioned filovirus GPs. Forty-eight hours later culture supernatants were collected, cleared of debris, and frozen at –80°C. Fifty percent tissue culture infectious dose (TCID50) values for each of the pseudovirions were calculated as described previously (89). For the neutralization assay, TZM-bl cells (expressing luciferase in an HIV-1 tat-dependent manner) were plated on a 96-well tissue culture plate at a cell density of 1.5 × 104 cells per well and plates incubated overnight at 37°C and 5% CO2. The next day, pseudovirions were diluted to 50 TCID50, incubated for 1 h at 37°C with rhesus plasma (final plasma dilutions, 1:30 to 1:3,840), and then added to the corresponding wells of the plates containing TZM-bl cells. Wells with TZM-bl cells alone and those with TZM-bl cells plus the respective pseudovirions in the absence of plasma served as controls. Plates were incubated at 37°C and 5% CO2 for 48 h, and luciferase activity in each well was measured by adding Britelite Plus luciferase substrate (PerkinElmer, Waltham, MA) and reading the plates immediately on a plate luminometer (TopCount NXT luminescence counter; Perkin Elmer). Neutralization activity in each well was calculated by comparing luciferase activity with that of the corresponding control wells.
Ebola ADCC assay.
The Ebola ADCC assay was performed as previously described (66). Stable 293 Trex target cells with inducible expression of surface EBOV GP, SUDV GP, or MARV GP along with a luciferase reporter were cultured in 75-cm2 flasks in DMEM supplemented with 10% Tet-approved FBS (Clontech, Mountain View, CA), 1× GlutaMAX, 100 IU/ml penicillin, 100 μg/ml streptomycin, 5 μg/ml blasticidin, 200 μg/ml Zeocin, and 3.0 μg/ml puromycin (complete selection medium). Upon reaching 75% confluence, cells were induced with 2.0 μg/ml doxycycline and cultured for the next 24 h. Cells were harvested by trypsinization, washed twice, and resuspended in MyeloCult medium (StemCell Technologies, Vancouver, BC, Canada) containing 4.0 μg/ml doxycycline at a cell density of 5 × 105 cells/ml. CD16-176V-NK-92 effector cells (received from Kerry Campbell, Fox Chase Cancer Center, Philadelphia, PA) were cultured in 75-cm2 cell culture flasks in MyeloCult medium supplemented with 200 IU/ml of recombinant human interleukin-2 (IL-2; R&D Systems, Minneapolis, MN). On day 3, cells were washed twice and resuspended in MyeloCult medium at a cell density of 2 × 106 cells/ml. A total of 5 × 104 target cells/100 μl/well of a 96-well round-bottom culture plates (Corning, Corning, NY) were mixed with sequential 2-fold dilutions of anti-Ebola VLP serum/plasma samples diluted in 50 μl of MyeloCult medium, and plates were incubated at 37°C in 5% CO2 for 10 min. Effector cells then were added to each well at 1 × 105 cells/50 μl/well (target/effector ratio, 1:2) in a final volume of 200 μl/well. Plates were centrifuged at 300 × g for 2 min and incubated for 4 h at 37°C in a 6% CO2 incubator. Following incubation, plates were centrifuged at 300 × g for 5 min, and cells were washed twice with PBS and resuspended in 100 μl of MyeloCult medium. One hundred microliters of Britelite Plus luciferase substrate was added to each well, cells were lysed, and plates were read immediately on a luminometer. Percent ADCC killing was calculated using the following formula: % ADCC killing = [(luciferase unitsno antibody control – luciferase unitsantibody) × 100]/(luciferase unitsno antibody control).
ICS.
Frozen PBMCs were thawed and rested overnight in complete RPMI medium (RPMI supplemented with penicillin-streptomycin, GlutaMAX, NEM amino acids, sodium pyruvate, and 10% heat-inactivated human AB serum) in a 37°C, 5% CO2 incubator. The next day, cells were transferred to the wells of a 96-well tissue culture plate at a density of 2 × 105 cells/well. Cells were stimulated, in triplicate wells, with individual filovirus recombinant GP (final concentration, 1.0 μg/ml; recombinant EBOV GP, SUDV GP, BDBV GP, MARV GP [all from IBT Bioservices], and TAFV GP [Alpha Diagnostic International, San Antonio, TX]). Cells with medium alone and those stimulated with phorbol myristate acetate (50 ng/ml) plus ionomycin (1.0 μM) served as negative and positive controls, respectively. All wells received GolgiPlug (BD) as the secretion inhibitor. Plates were incubated for 12 h in a 37°C, 5% CO2 incubator. Cells from the triplicate wells were pooled, washed, and stained with anti-human CD3-BV605 (clone SP34-2), CD4-allophycocyanin (APC)-Cy7 (clone SK3), and CD8-V500 (clone RPA-T8; all from BD Biosciences). Cells were washed, fixed, and permeabilized using a fixation and permeabilization buffer set (BD). After washing, cells were stained with anti-human IFN-γ–fluorescein isothiocyanate (clone B27) and TNF-α–APC (clone Mab11) antibodies (both from BioLegend). Data were acquired on a BD Fortessa II and analyzed using FlowJo software (Tree Star, Inc. Ashland, OR).
Statistical analysis.
Statistical analysis was performed using GraphPad Prism software (version 8). Two-tailed t tests or nonparametric tests were used for all comparisons. P values of <0.05 were considered significant. Individual tests employed are included in Results.
ACKNOWLEDGMENTS
We thank Kerry Campbell, Fox Chase Cancer Center, Philadelphia, PA, and NantKwest, Inc., for supplying CD16-176V-NK-92 effector cells through a Material Transfer Agreement. We also thank the research and animal care staff at the New Iberia Research Center for their help with the primate studies.
The study was funded in part with a pilot grant awarded to Karnail Singh and Paul Spearman by Innovation Ventures, Cincinnati Children’s Hospital Medical Center, in part by funds provided to Karnail Singh by Cincinnati Children’s Research Foundation, Cincinnati, OH, and by support from the New Iberia Research Center, University of Louisiana at Lafayette. The funders had no role in study design, data collection and interpretation, or the decision to submit the work for publication.
The monovalent EBOV GP-Gag (EBOV) VLP and SUDV GP-Gag (SUDV) VLP vaccine products are the joint intellectual property of Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, and Emory University, Atlanta, GA. Paul Spearman, Karnail Singh, and Xuemin Chen are listed as inventors on this patent. Bivalent EBOV/SUDV GP-Gag (Ebola) VLP vaccine production and use are the intellectual property of Cincinnati Children’s Hospital Medical Center, Cincinnati, OH. Paul Spearman and Karnail Singh are listed as inventors on this patent. The Ebola ADCC assay procedure and the target cells described in this assay are the intellectual property of Emory University, Atlanta, GA. Paul Spearman, Karnail Singh, and Xuemin Chen are listed as inventors on this patent.
REFERENCES
- 1.WHO Ebola Response Team, Agua-Agum J, Allegranzi B, Ariyarajah A, Aylward R, Blake IM, Barboza P, Bausch D, Brennan RJ, Clement P, Coffey P, Cori A, Donnelly CA, Dorigatti I, Drury P, Durski K, Dye C, Eckmanns T, Ferguson NM, Fraser C, Garcia E, Garske T, Gasasira A, Gurry C, Hamblion E, Hinsley W, Holden R, Holmes D, Hugonnet S, Jaramillo Gutierrez G, Jombart T, Kelley E, Santhana R, Mahmoud N, Mills HL, Mohamed Y, Musa E, Naidoo D, Nedjati-Gilani G, Newton E, Norton I, Nouvellet P, Perkins D, Perkins M, Riley S, Schumacher D, Shah A, Tang M, Varsaneux O, Van Kerkhove MD. 2016. After Ebola in West Africa–unpredictable risks, preventable epidemics. N Engl J Med 375:587–596. doi: 10.1056/NEJMsr1513109. [DOI] [PubMed] [Google Scholar]
- 2.Henao-Restrepo AM, Camacho A, Longini IM, Watson CH, Edmunds WJ, Egger M, Carroll MW, Dean NE, Diatta I, Doumbia M, Draguez B, Duraffour S, Enwere G, Grais R, Gunther S, Gsell P-S, Hossmann S, Watle SV, Kondé MK, Kéïta S, Kone S, Kuisma E, Levine MM, Mandal S, Mauget T, Norheim G, Riveros X, Soumah A, Trelle S, Vicari AS, Røttingen J-A, Kieny M-P. 2017. Efficacy and effectiveness of an rVSV-vectored vaccine in preventing Ebola virus disease: final results from the Guinea ring vaccination, open-label, cluster-randomised trial (Ebola Ca Suffit!). Lancet 389:505–518. doi: 10.1016/S0140-6736(16)32621-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ledgerwood JE, VRC 207 Study Team, DeZure AD, Stanley DA, Coates EE, Novik L, Enama ME, Berkowitz NM, Hu Z, Joshi G, Ploquin A, Sitar S, Gordon IJ, Plummer SA, Holman LA, Hendel CS, Yamshchikov G, Roman F, Nicosia A, Colloca S, Cortese R, Bailer RT, Schwartz RM, Roederer M, Mascola JR, Koup RA, Sullivan NJ, Graham BS, Team V. 2017. Chimpanzee adenovirus vector ebola vaccine. N Engl J Med 376:928–938. doi: 10.1056/NEJMoa1410863. [DOI] [PubMed] [Google Scholar]
- 4.Li JX, Hou LH, Meng FY, Wu SP, Hu YM, Liang Q, Chu K, Zhang Z, Xu JJ, Tang R, Wang WJ, Liu P, Hu JL, Luo L, Jiang R, Zhu FC, Chen W. 2017. Immunity duration of a recombinant adenovirus type-5 vector-based Ebola vaccine and a homologous prime-boost immunisation in healthy adults in China: final report of a randomised, double-blind, placebo-controlled, phase 1 trial. Lancet Glob Health 5:e324–e334. doi: 10.1016/S2214-109X(16)30367-9. [DOI] [PubMed] [Google Scholar]
- 5.Milligan ID, Gibani MM, Sewell R, Clutterbuck EA, Campbell D, Plested E, Nuthall E, Voysey M, Silva-Reyes L, McElrath MJ, De Rosa SC, Frahm N, Cohen KW, Shukarev G, Orzabal N, van Duijnhoven W, Truyers C, Bachmayer N, Splinter D, Samy N, Pau MG, Schuitemaker H, Luhn K, Callendret B, Van Hoof J, Douoguih M, Ewer K, Angus B, Pollard AJ, Snape MD. 2016. Safety and immunogenicity of novel adenovirus type 26- and modified vaccinia Ankara-vectored Ebola vaccines: a randomized clinical trial. JAMA 315:1610–1623. doi: 10.1001/jama.2016.4218. [DOI] [PubMed] [Google Scholar]
- 6.Regules JA, Beigel JH, Paolino KM, Voell J, Castellano AR, Hu Z, Munoz P, Moon JE, Ruck RC, Bennett JW, Twomey PS, Gutierrez RL, Remich SA, Hack HR, Wisniewski ML, Josleyn MD, Kwilas SA, Van Deusen N, Mbaya OT, Zhou Y, Stanley DA, Jing W, Smith KS, Shi M, Ledgerwood JE, Graham BS, Sullivan NJ, Jagodzinski LL, Peel SA, Alimonti JB, Hooper JW, Silvera PM, Martin BK, Monath TP, Ramsey WJ, Link CJ, Lane HC, Michael NL, Davey RT Jr, Thomas SJ, rVSVΔG-ZEBOV-GP Study Group. 2017. A recombinant vesicular stomatitis virus Ebola vaccine. N Engl J Med 376:330–341. doi: 10.1056/NEJMoa1414216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tapia MD, Sow SO, Lyke KE, Haidara FC, Diallo F, Doumbia M, Traore A, Coulibaly F, Kodio M, Onwuchekwa U, Sztein MB, Wahid R, Campbell JD, Kieny MP, Moorthy V, Imoukhuede EB, Rampling T, Roman F, De Ryck I, Bellamy AR, Dally L, Mbaya OT, Ploquin A, Zhou Y, Stanley DA, Bailer R, Koup RA, Roederer M, Ledgerwood J, Hill AV, Ballou WR, Sullivan N, Graham B, Levine MM. 2016. Use of ChAd3-EBO-Z Ebola virus vaccine in Malian and US adults, and boosting of Malian adults with MVA-BN-Filo: a phase 1, single-blind, randomised trial, a phase 1b, open-label and double-blind, dose-escalation trial, and a nested, randomised, double-blind, placebo-controlled trial. Lancet Infect Dis 16:31–42. doi: 10.1016/S1473-3099(15)00362-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang Y, Li J, Hu Y, Liang Q, Wei M, Zhu F. 2017. Ebola vaccines in clinical trial: the promising candidates. Hum Vaccin Immunother 13:153–168. doi: 10.1080/21645515.2016.1225637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Winslow RL, Milligan ID, Voysey M, Luhn K, Shukarev G, Douoguih M, Snape MD. 2017. Immune responses to novel adenovirus type 26 and modified vaccinia virus Ankara-vectored Ebola vaccines at 1 year. JAMA 317:1075–1077. doi: 10.1001/jama.2016.20644. [DOI] [PubMed] [Google Scholar]
- 10.Zhu FC, Wurie AH, Hou LH, Liang Q, Li YH, Russell JB, Wu SP, Li JX, Hu YM, Guo Q, Xu WB, Wurie AR, Wang WJ, Zhang Z, Yin WJ, Ghazzawi M, Zhang X, Duan L, Wang JZ, Chen W. 2017. Safety and immunogenicity of a recombinant adenovirus type-5 vector-based Ebola vaccine in healthy adults in Sierra Leone: a single-centre, randomised, double-blind, placebo-controlled, phase 2 trial. Lancet 389:621–628. doi: 10.1016/S0140-6736(16)32617-4. [DOI] [PubMed] [Google Scholar]
- 11.Ewer K, Rampling T, Venkatraman N, Bowyer G, Wright D, Lambe T, Imoukhuede EB, Payne R, Fehling SK, Strecker T, Biedenkopf N, Krähling V, Tully CM, Edwards NJ, Bentley EM, Samuel D, Labbé G, Jin J, Gibani M, Minhinnick A, Wilkie M, Poulton I, Lella N, Roberts R, Hartnell F, Bliss C, Sierra-Davidson K, Powlson J, Berrie E, Tedder R, Roman F, De Ryck I, Nicosia A, Sullivan NJ, Stanley DA, Mbaya OT, Ledgerwood JE, Schwartz RM, Siani L, Colloca S, Folgori A, Di Marco S, Cortese R, Wright E, Becker S, Graham BS, Koup RA, Levine MM, Volkmann A, Chaplin P, Pollard AJ, Draper SJ, Ballou WR, Lawrie A, Gilbert SC, Hill AVS. 2016. A monovalent chimpanzee adenovirus ebola vaccine boosted with MVA. N Engl J Med 374:1635–1646. doi: 10.1056/NEJMoa1411627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ilunga Kalenga O, Moeti M, Sparrow A, Nguyen VK, Lucey D, Ghebreyesus TA. 2019. The ongoing ebola epidemic in the Democratic Republic of Congo, 2018-2019. N Engl J Med 381:373–383. doi: 10.1056/NEJMsr1904253. [DOI] [PubMed] [Google Scholar]
- 13.Geisbert TW, Bailey M, Hensley L, Asiedu C, Geisbert J, Stanley D, Honko A, Johnson J, Mulangu S, Pau MG, Custers J, Vellinga J, Hendriks J, Jahrling P, Roederer M, Goudsmit J, Koup R, Sullivan NJ. 2011. Recombinant adenovirus serotype 26 (Ad26) and Ad35 vaccine vectors bypass immunity to Ad5 and protect nonhuman primates against ebolavirus challenge. J Virol 85:4222–4233. doi: 10.1128/JVI.02407-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stanley DA, Honko AN, Asiedu C, Trefry JC, Lau-Kilby AW, Johnson JC, Hensley L, Ammendola V, Abbate A, Grazioli F, Foulds KE, Cheng C, Wang L, Donaldson MM, Colloca S, Folgori A, Roederer M, Nabel GJ, Mascola J, Nicosia A, Cortese R, Koup RA, Sullivan NJ. 2014. Chimpanzee adenovirus vaccine generates acute and durable protective immunity against ebolavirus challenge. Nat Med 20:1126–1129. doi: 10.1038/nm.3702. [DOI] [PubMed] [Google Scholar]
- 15.Sullivan NJ, Hensley L, Asiedu C, Geisbert TW, Stanley D, Johnson J, Honko A, Olinger G, Bailey M, Geisbert JB, Reimann KA, Bao S, Rao S, Roederer M, Jahrling PB, Koup RA, Nabel GJ. 2011. CD8+ cellular immunity mediates rAd5 vaccine protection against Ebola virus infection of nonhuman primates. Nat Med 17:1128–1131. doi: 10.1038/nm.2447. [DOI] [PubMed] [Google Scholar]
- 16.Keshwara R, Johnson RF, Schnell MJ. 2017. Toward an effective Ebola virus vaccine. Annu Rev Med 68:371–386. doi: 10.1146/annurev-med-051215-030919. [DOI] [PubMed] [Google Scholar]
- 17.Lévy Y, Lane C, Piot P, Beavogui AH, Kieh M, Leigh B, Doumbia S, D'Ortenzio E, Lévy-Marchal C, Pierson J, Watson-Jones D, Nguyen V-K, Larson H, Lysander J, Lacabaratz C, Thiebaut R, Augier A, Ishola D, Kennedy S, Chêne G, Greenwood B, Neaton J, Yazdanpanah Y. 2018. Prevention of Ebola virus disease through vaccination: where we are in 2018. Lancet 392:787–790. doi: 10.1016/S0140-6736(18)31710-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ledgerwood JE, Costner P, Desai N, Holman L, Enama ME, Yamshchikov G, Mulangu S, Hu Z, Andrews CA, Sheets RA, Koup RA, Roederer M, Bailer R, Mascola JR, Pau MG, Sullivan NJ, Goudsmit J, Nabel GJ, Graham BS, VRC 205 Study Team. 2010. A replication defective recombinant Ad5 vaccine expressing Ebola virus GP is safe and immunogenic in healthy adults. Vaccine 29:304–313. doi: 10.1016/j.vaccine.2010.10.037. [DOI] [PubMed] [Google Scholar]
- 19.Sumida SM, Truitt DM, Kishko MG, Arthur JC, Jackson SS, Gorgone DA, Lifton MA, Koudstaal W, Pau MG, Kostense S, Havenga MJ, Goudsmit J, Letvin NL, Barouch DH. 2004. Neutralizing antibodies and CD8+ T lymphocytes both contribute to immunity to adenovirus serotype 5 vaccine vectors. J Virol 78:2666–2673. doi: 10.1128/jvi.78.6.2666-2673.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhu FC, Hou LH, Li JX, Wu SP, Liu P, Zhang GR, Hu YM, Meng FY, Xu JJ, Tang R, Zhang JL, Wang WJ, Duan L, Chu K, Liang Q, Hu JL, Luo L, Zhu T, Wang JZ, Chen W. 2015. Safety and immunogenicity of a novel recombinant adenovirus type-5 vector-based Ebola vaccine in healthy adults in China: preliminary report of a randomised, double-blind, placebo-controlled, phase 1 trial. Lancet 385:2272–2279. doi: 10.1016/S0140-6736(15)60553-0. [DOI] [PubMed] [Google Scholar]
- 21.Agnandji ST, Huttner A, Zinser ME, Njuguna P, Dahlke C, Fernandes JF, Yerly S, Dayer J-A, Kraehling V, Kasonta R, Adegnika AA, Altfeld M, Auderset F, Bache EB, Biedenkopf N, Borregaard S, Brosnahan JS, Burrow R, Combescure C, Desmeules J, Eickmann M, Fehling SK, Finckh A, Goncalves AR, Grobusch MP, Hooper J, Jambrecina A, Kabwende AL, Kaya G, Kimani D, Lell B, Lemaître B, Lohse AW, Massinga-Loembe M, Matthey A, Mordmüller B, Nolting A, Ogwang C, Ramharter M, Schmidt-Chanasit J, Schmiedel S, Silvera P, Stahl FR, Staines HM, Strecker T, Stubbe HC, Tsofa B, Zaki S, Fast P, Moorthy V, Kaiser L, Krishna S, Becker S, Kieny M-P, Bejon P, Kremsner PG, Addo MM, Siegrist C-A. 2016. Phase 1 trials of rVSV Ebola vaccine in Africa and Europe. N Engl J Med 374:1647–1660. doi: 10.1056/NEJMoa1502924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Warfield KL, Swenson DL, Olinger GG, Kalina WV, Aman MJ, Bavari S. 2007. Ebola virus-like particle-based vaccine protects nonhuman primates against lethal Ebola virus challenge. J Infect Dis 196(Suppl 2):S430–437. doi: 10.1086/520583. [DOI] [PubMed] [Google Scholar]
- 23.McElroy AK, Akondy RS, Davis CW, Ellebedy AH, Mehta AK, Kraft CS, Lyon GM, Ribner BS, Varkey J, Sidney J, Sette A, Campbell S, Stroher U, Damon I, Nichol ST, Spiropoulou CF, Ahmed R. 2015. Human Ebola virus infection results in substantial immune activation. Proc Natl Acad Sci U S A 112:4719–4724. doi: 10.1073/pnas.1502619112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bradfute SB, Anthony SM, Stuthman KS, Ayithan N, Tailor P, Shaia CI, Bray M, Ozato K, Bavari S. 2015. Mechanisms of immunity in post-exposure vaccination against Ebola virus infection. PLoS One 10:e0118434. doi: 10.1371/journal.pone.0118434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bramble MS, Hoff N, Gilchuk P, Mukadi P, Lu K, Doshi RH, Steffen I, Nicholson BP, Lipson A, Vashist N, Sinai C, Spencer D, Olinger G, Wemakoy EO, Illunga BK, Pettitt J, Logue J, Marchand J, Varughese J, Bennett RS, Jahrling P, Cavet G, Serafini T, Ollmann Saphire E, Vilain E, Muyembe-Tamfum JJ, Hensely LE, Simmons G, Crowe JE Jr, Rimoin AW. 2018. Pan-filovirus serum neutralizing antibodies in a subset of Congolese ebolavirus infection survivors. J Infect Dis 218:1929–1936. doi: 10.1093/infdis/jiy453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cooper CL, Martins KA, Stronsky SM, Langan DP, Steffens J, Van Tongeren S, Bavari S. 2017. T-cell-dependent mechanisms promote Ebola VLP-induced antibody responses, but are dispensable for vaccine-mediated protection. Emerg Microbes Infect 6:e46. doi: 10.1038/emi.2017.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ebihara H, Rockx B, Marzi A, Feldmann F, Haddock E, Brining D, LaCasse RA, Gardner D, Feldmann H. 2011. Host response dynamics following lethal infection of rhesus macaques with Zaire ebolavirus. J Infect Dis 204(Suppl 3):S991–S999. doi: 10.1093/infdis/jir336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Khurana S, Fuentes S, Coyle EM, Ravichandran S, Davey RT Jr, Beigel JH. 2016. Human antibody repertoire after VSV-Ebola vaccination identifies novel targets and virus-neutralizing IgM antibodies. Nat Med 22:1439–1447. doi: 10.1038/nm.4201. [DOI] [PubMed] [Google Scholar]
- 29.Marzi A, Engelmann F, Feldmann F, Haberthur K, Shupert WL, Brining D, Scott DP, Geisbert TW, Kawaoka Y, Katze MG, Feldmann H, Messaoudi I. 2013. Antibodies are necessary for rVSV/ZEBOV-GP-mediated protection against lethal Ebola virus challenge in nonhuman primates. Proc Natl Acad Sci U S A 110:1893–1898. doi: 10.1073/pnas.1209591110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sakabe S, Sullivan BM, Hartnett JN, Robles-Sikisaka R, Gangavarapu K, Cubitt B, Ware BC, Kotliar D, Branco LM, Goba A, Momoh M, Sandi JD, Kanneh L, Grant DS, Garry RF, Andersen KG, de la Torre JC, Sabeti PC, Schieffelin JS, Oldstone M. 2018. Analysis of CD8(+) T cell response during the 2013–2016 Ebola epidemic in West Africa. Proc Natl Acad Sci U S A 115:E7578–E7586. doi: 10.1073/pnas.1806200115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ksiazek TG, Rollin PE, Williams AJ, Bressler DS, Martin ML, Swanepoel R, Burt FJ, Leman PA, Khan AS, Rowe AK, Mukunu R, Sanchez A, Peters CJ. 1999. Clinical virology of Ebola hemorrhagic fever (EHF): virus, virus antigen, and IgG and IgM antibody findings among EHF patients in Kikwit, Democratic Republic of the Congo, 1995. J Infect Dis 179(Suppl 1):S177–S187. doi: 10.1086/514321. [DOI] [PubMed] [Google Scholar]
- 32.Rowe AK, Bertolli J, Khan AS, Mukunu R, Muyembe-Tamfum JJ, Bressler D, Williams AJ, Peters CJ, Rodriguez L, Feldmann H, Nichol ST, Rollin PE, Ksiazek TG. 1999. Clinical, virologic, and immunologic follow-up of convalescent Ebola hemorrhagic fever patients and their household contacts, Kikwit, Democratic Republic of the Congo. Commission de Lutte contre les Epidemies a Kikwit. J Infect Dis 179(Suppl 1):S28–S35. doi: 10.1086/514318. [DOI] [PubMed] [Google Scholar]
- 33.Baize S, Leroy EM, Georges-Courbot MC, Capron M, Lansoud-Soukate J, Debré P, Fisher-Hoch SP, McCormick JB, Georges AJ. 1999. Defective humoral responses and extensive intravascular apoptosis are associated with fatal outcome in Ebola virus-infected patients. Nat Med 5:423–426. doi: 10.1038/7422. [DOI] [PubMed] [Google Scholar]
- 34.Qiu X, Wong G, Audet J, Bello A, Fernando L, Alimonti JB, Fausther-Bovendo H, Wei H, Aviles J, Hiatt E, Johnson A, Morton J, Swope K, Bohorov O, Bohorova N, Goodman C, Kim D, Pauly MH, Velasco J, Pettitt J, Olinger GG, Whaley K, Xu B, Strong JE, Zeitlin L, Kobinger GP. 2014. Reversion of advanced Ebola virus disease in nonhuman primates with ZMapp. Nature 514:47–53. doi: 10.1038/nature13777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Blaney JE, Marzi A, Willet M, Papaneri AB, Wirblich C, Feldmann F, Holbrook M, Jahrling P, Feldmann H, Schnell MJ. 2013. Antibody quality and protection from lethal Ebola virus challenge in nonhuman primates immunized with rabies virus based bivalent vaccine. PLoS Pathog 9:e1003389. doi: 10.1371/journal.ppat.1003389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lai L, Davey R, Beck A, Xu Y, Suffredini AF, Palmore T, Kabbani S, Rogers S, Kobinger G, Alimonti J, Link CJ Jr, Rubinson L, Stroher U, Wolcott M, Dorman W, Uyeki TM, Feldmann H, Lane HC, Mulligan MJ. 2015. Emergency postexposure vaccination with vesicular stomatitis virus-vectored Ebola vaccine after needlestick. JAMA 313:1249–1255. doi: 10.1001/jama.2015.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Marzi A, Robertson SJ, Haddock E, Feldmann F, Hanley PW, Scott DP, Strong JE, Kobinger G, Best SM, Feldmann H. 2015. EBOLA VACCINE. VSV-EBOV rapidly protects macaques against infection with the 2014/15 Ebola virus outbreak strain. Science 349:739–742. doi: 10.1126/science.aab3920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Marzi A, Hanley PW, Haddock E, Martellaro C, Kobinger G, Feldmann H. 2016. Efficacy of vesicular stomatitis virus-Ebola virus postexposure treatment in rhesus macaques infected with Ebola virus Makona. J Infect Dis 214:S360–S366. doi: 10.1093/infdis/jiw218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liu Q, Fan C, Li Q, Zhou S, Huang W, Wang L, Sun C, Wang M, Wu X, Ma J, Li B, Xie L, Wang Y. 2017. Antibody-dependent-cellular-cytotoxicity-inducing antibodies significantly affect the post-exposure treatment of Ebola virus infection. Sci Rep 7:45552. doi: 10.1038/srep45552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Marzi A, Yoshida R, Miyamoto H, Ishijima M, Suzuki Y, Higuchi M, Matsuyama Y, Igarashi M, Nakayama E, Kuroda M, Saijo M, Feldmann F, Brining D, Feldmann H, Takada A. 2012. Protective efficacy of neutralizing monoclonal antibodies in a nonhuman primate model of Ebola hemorrhagic fever. PLoS One 7:e36192. doi: 10.1371/journal.pone.0036192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Qiu X, Audet J, Lv M, He S, Wong G, Wei H, Luo L, Fernando L, Kroeker A, Fausther Bovendo H, Bello A, Li F, Ye P, Jacobs M, Ippolito G, Saphire EO, Bi S, Shen B, Gao GF, Zeitlin L, Feng J, Zhang B, Kobinger GP. 2016. Two-mAb cocktail protects macaques against the Makona variant of Ebola virus. Sci Transl Med 8:329ra33. doi: 10.1126/scitranslmed.aad9875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Qiu X, Audet J, Wong G, Pillet S, Bello A, Cabral T, Strong JE, Plummer F, Corbett CR, Alimonti JB, Kobinger GP. 2012. Successful treatment of Ebola virus-infected cynomolgus macaques with monoclonal antibodies. Sci Transl Med 4:138ra181. doi: 10.1126/scitranslmed.3003876. [DOI] [PubMed] [Google Scholar]
- 43.Takada A, Ebihara H, Jones S, Feldmann H, Kawaoka Y. 2007. Protective efficacy of neutralizing antibodies against Ebola virus infection. Vaccine 25:993–999. doi: 10.1016/j.vaccine.2006.09.076. [DOI] [PubMed] [Google Scholar]
- 44.Wec AZ, Nyakatura EK, Herbert AS, Howell KA, Holtsberg FW, Bakken RR, Mittler E, Christin JR, Shulenin S, Jangra RK, Bharrhan S, Kuehne AI, Bornholdt ZA, Flyak AI, Saphire EO, Crowe JE Jr, Aman MJ, Dye JM, Lai JR, Chandran K. 2016. A “Trojan horse” bispecific-antibody strategy for broad protection against ebolaviruses. Science 354:350–354. doi: 10.1126/science.aag3267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhang Q, Gui M, Niu X, He S, Wang R, Feng Y, Kroeker A, Zuo Y, Wang H, Wang Y, Li J, Li C, Shi Y, Shi X, Gao GF, Xiang Y, Qiu X, Chen L, Zhang L. 2016. Potent neutralizing monoclonal antibodies against Ebola virus infection. Sci Rep 6:25856. doi: 10.1038/srep25856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Willet M, Kurup D, Papaneri A, Wirblich C, Hooper JW, Kwilas SA, Keshwara R, Hudacek A, Beilfuss S, Rudolph G, Pommerening E, Vos A, Neubert A, Jahrling P, Blaney JE, Johnson RF, Schnell MJ. 2015. Preclinical development of inactivated rabies virus-based polyvalent vaccine against rabies and filoviruses. J Infect Dis 212(Suppl 2):S414–S424. doi: 10.1093/infdis/jiv251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Villinger F, Rollin PE, Brar SS, Chikkala NF, Winter J, Sundstrom JB, Zaki SR, Swanepoel R, Ansari AA, Peters CJ. 1999. Markedly elevated levels of interferon (IFN)-gamma, IFN-alpha, interleukin (IL)-2, IL-10, and tumor necrosis factor-alpha associated with fatal Ebola virus infection. J Infect Dis 179(Suppl 1):S188–S191. doi: 10.1086/514283. [DOI] [PubMed] [Google Scholar]
- 48.Wauquier N, Becquart P, Padilla C, Baize S, Leroy EM. 2010. Human fatal Zaire Ebola virus infection is associated with an aberrant innate immunity and with massive lymphocyte apoptosis. PLoS Negl Trop Dis 4:e837. doi: 10.1371/journal.pntd.0000837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Baize S, Leroy EM, Georges AJ, Georges-Courbot MC, Capron M, Bedjabaga I, Lansoud-Soukate J, Mavoungou E. 2002. Inflammatory responses in Ebola virus-infected patients. Clin Exp Immunol 128:163–168. doi: 10.1046/j.1365-2249.2002.01800.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Warfield KL, Bosio CM, Welcher BC, Deal EM, Mohamadzadeh M, Schmaljohn A, Aman MJ, Bavari S. 2003. Ebola virus-like particles protect from lethal Ebola virus infection. Proc Natl Acad Sci U S A 100:15889–15894. doi: 10.1073/pnas.2237038100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Warfield KL, Dye JM, Wells JB, Unfer RC, Holtsberg FW, Shulenin S, Vu H, Swenson DL, Bavari S, Aman MJ. 2015. Homologous and heterologous protection of nonhuman primates by Ebola and Sudan virus-like particles. PLoS One 10:e0118881. doi: 10.1371/journal.pone.0118881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Carra JH, Martins KA, Schokman RD, Robinson CG, Steffens JT, Bavari S. 2015. A thermostable, chromatographically purified Ebola nano-VLP vaccine. J Transl Med 13:228. doi: 10.1186/s12967-015-0593-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Champion JA, Mitragotri S. 2009. Shape induced inhibition of phagocytosis of polymer particles. Pharm Res 26:244–249. doi: 10.1007/s11095-008-9626-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Manolova V, Flace A, Bauer M, Schwarz K, Saudan P, Bachmann MF. 2008. Nanoparticles target distinct dendritic cell populations according to their size. Eur J Immunol 38:1404–1413. doi: 10.1002/eji.200737984. [DOI] [PubMed] [Google Scholar]
- 55.Zhu P, Chertova E, Bess J Jr, Lifson JD, Arthur LO, Liu J, Taylor KA, Roux KH. 2003. Electron tomography analysis of envelope glycoprotein trimers on HIV and simian immunodeficiency virus virions. Proc Natl Acad Sci U S A 100:15812–15817. doi: 10.1073/pnas.2634931100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hammonds J, Chen X, Ding L, Fouts T, De Vico A, Zur Megede J, Barnett S, Spearman P. 2003. Gp120 stability on HIV-1 virions and Gag-Env pseudovirions is enhanced by an uncleaved Gag core. Virology 314:636–649. doi: 10.1016/s0042-6822(03)00467-7. [DOI] [PubMed] [Google Scholar]
- 57.Bode C, Zhao G, Steinhagen F, Kinjo T, Klinman DM. 2011. CpG DNA as a vaccine adjuvant. Expert Rev Vaccines 10:499–511. doi: 10.1586/erv.10.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cimica V, Galarza JM. 2017. Adjuvant formulations for virus-like particle (VLP) based vaccines. Clin Immunol 183:99–108. doi: 10.1016/j.clim.2017.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Galarza JM, Latham T, Cupo A. 2005. Virus-like particle vaccine conferred complete protection against a lethal influenza virus challenge. Viral Immunol 18:365–372. doi: 10.1089/vim.2005.18.365. [DOI] [PubMed] [Google Scholar]
- 60.Martins KA, Steffens JT, van Tongeren SA, Wells JB, Bergeron AA, Dickson SP, Dye JM, Salazar AM, Bavari S. 2014. Toll-like receptor agonist augments virus-like particle-mediated protection from Ebola virus with transient immune activation. PLoS One 9:e89735. doi: 10.1371/journal.pone.0089735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Schneider-Ohrum K, Giles BM, Weirback HK, Williams BL, DeAlmeida DR, Ross TM. 2011. Adjuvants that stimulate TLR3 or NLPR3 pathways enhance the efficiency of influenza virus-like particle vaccines in aged mice. Vaccine 29:9081–9092. doi: 10.1016/j.vaccine.2011.09.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Jegaskanda S, Luke C, Hickman HD, Sangster MY, Wieland-Alter WF, McBride JM, Yewdell JW, Wright PF, Treanor J, Rosenberger CM, Subbarao K. 2016. Generation and protective ability of influenza virus-specific antibody-dependent cellular cytotoxicity in humans elicited by vaccination, natural infection, and experimental challenge. J Infect Dis 214:945–952. doi: 10.1093/infdis/jiw262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Jegaskanda S, Reading PC, Kent SJ. 2014. Influenza-specific antibody-dependent cellular cytotoxicity: toward a universal influenza vaccine. J Immunol 193:469–475. doi: 10.4049/jimmunol.1400432. [DOI] [PubMed] [Google Scholar]
- 64.Gomez-Roman VR, Patterson LJ, Venzon D, Liewehr D, Aldrich K, Florese R, Robert-Guroff M. 2005. Vaccine-elicited antibodies mediate antibody-dependent cellular cytotoxicity correlated with significantly reduced acute viremia in rhesus macaques challenged with SIVmac251. J Immunol 174:2185–2189. doi: 10.4049/jimmunol.174.4.2185. [DOI] [PubMed] [Google Scholar]
- 65.Schmaljohn A, Lewis GK. 2016. Cell-targeting antibodies in immunity to Ebola. Pathog Dis 74:ftw021. doi: 10.1093/femspd/ftw021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Singh K, Marasini B, Chen X, Spearman P. 2018. A novel Ebola virus antibody-dependent cell-mediated cytotoxicity (Ebola ADCC) assay. J Immunol Methods 460:10–16. doi: 10.1016/j.jim.2018.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Martins KA, Cooper CL, Stronsky SM, Norris SL, Kwilas SA, Steffens JT, Benko JG, van Tongeren SA, Bavari S. 2016. Adjuvant-enhanced CD4 T cell responses are critical to durable vaccine immunity. EBioMedicine 3:67–78. doi: 10.1016/j.ebiom.2015.11.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ruiz W, McClements WL, Jansen KU, Esser MT. 2005. Kinetics and isotype profile of antibody responses in rhesus macaques induced following vaccination with HPV 6, 11, 16 and 18 L1-virus-like particles formulated with or without Merck aluminum adjuvant. J Immune Based Ther Vaccines 3:2. doi: 10.1186/1476-8518-3-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wagner R, Teeuwsen VJ, Deml L, Notka F, Haaksma AG, Jhagjhoorsingh SS, Niphuis H, Wolf H, Heeney JL. 1998. Cytotoxic T cells and neutralizing antibodies induced in rhesus monkeys by virus-like particle HIV vaccines in the absence of protection from SHIV infection. Virology 245:65–74. doi: 10.1006/viro.1998.9104. [DOI] [PubMed] [Google Scholar]
- 70.Hammonds J, Chen X, Fouts T, DeVico A, Montefiori D, Spearman P. 2005. Induction of neutralizing antibodies against human immunodeficiency virus type 1 primary isolates by Gag-Env pseudovirion immunization. J Virol 79:14804–14814. doi: 10.1128/JVI.79.23.14804-14814.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gujer C, Sundling C, Seder RA, Karlsson Hedestam GB, Loré K. 2011. Human and rhesus plasmacytoid dendritic cell and B-cell responses to Toll-like receptor stimulation. Immunology 134:257–269. doi: 10.1111/j.1365-2567.2011.03484.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Iyer SS, Gangadhara S, Victor B, Shen X, Chen X, Nabi R, Kasturi SP, Sabula MJ, Labranche CC, Reddy PB, Tomaras GD, Montefiori DC, Moss B, Spearman P, Pulendran B, Kozlowski PA, Amara RR. 2016. Virus-like particles displaying trimeric simian immunodeficiency virus (SIV) envelope gp160 enhance the breadth of DNA/modified vaccinia virus Ankara SIV vaccine-induced antibody responses in rhesus macaques. J Virol 90:8842–8854. doi: 10.1128/JVI.01163-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Moody MA, Santra S, Vandergrift NA, Sutherland LL, Gurley TC, Drinker MS, Allen AA, Xia SM, Meyerhoff RR, Parks R, Lloyd KE, Easterhoff D, Alam SM, Liao HX, Ward BM, Ferrari G, Montefiori DC, Tomaras GD, Seder RA, Letvin NL, Haynes BF. 2014. Toll-like receptor 7/8 (TLR7/8) and TLR9 agonists cooperate to enhance HIV-1 envelope antibody responses in rhesus macaques. J Virol 88:3329–3339. doi: 10.1128/JVI.03309-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kasturi SP, Kozlowski PA, Nakaya HI, Burger MC, Russo P, Pham M, Kovalenkov Y, Silveira ELV, Havenar-Daughton C, Burton SL, Kilgore KM, Johnson MJ, Nabi R, Legere T, Sher ZJ, Chen X, Amara RR, Hunter E, Bosinger SE, Spearman P, Crotty S, Villinger F, Derdeyn CA, Wrammert J, Pulendran B. 2017. Adjuvanting a simian immunodeficiency virus vaccine with Toll-like receptor ligands encapsulated in nanoparticles induces persistent antibody responses and enhanced protection in TRIM5alpha restrictive macaques. J Virol 91:e01844-16. doi: 10.1128/JVI.01844-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wong G, Richardson JS, Pillet S, Patel A, Qiu X, Alimonti J, Hogan J, Zhang Y, Takada A, Feldmann H, Kobinger GP. 2012. Immune parameters correlate with protection against Ebola virus infection in rodents and nonhuman primates. Sci Transl Med 4:158ra146. doi: 10.1126/scitranslmed.3004582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Jones SM, Feldmann H, Stroher U, Geisbert JB, Fernando L, Grolla A, Klenk HD, Sullivan NJ, Volchkov VE, Fritz EA, Daddario KM, Hensley LE, Jahrling PB, Geisbert TW. 2005. Live attenuated recombinant vaccine protects nonhuman primates against Ebola and Marburg viruses. Nat Med 11:786–790. doi: 10.1038/nm1258. [DOI] [PubMed] [Google Scholar]
- 77.Sullivan NJ, Martin JE, Graham BS, Nabel GJ. 2009. Correlates of protective immunity for Ebola vaccines: implications for regulatory approval by the animal rule. Nat Rev Microbiol 7:393–400. doi: 10.1038/nrmicro2129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lien G, Heymann DL. 2013. The problems with polio: toward eradication. Infect Dis Ther 2:167–174. doi: 10.1007/s40121-013-0014-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.de Oliveira CM, Fregnani J, Villa LL. 2019. HPV vaccine: updates and highlights. Acta Cytol 63:159–168. doi: 10.1159/000497617. [DOI] [PubMed] [Google Scholar]
- 80.Schiller JT, Lowy DR. 1996. Papillomavirus-like particles and HPV vaccine development. Semin Cancer Biol 7:373–382. doi: 10.1006/scbi.1996.0046. [DOI] [PubMed] [Google Scholar]
- 81.Frietze KM, Peabody DS, Chackerian B. 2016. Engineering virus-like particles as vaccine platforms. Curr Opin Virol 18:44–49. doi: 10.1016/j.coviro.2016.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Naskalska A, Pyrc K. 2015. Virus like particles as immunogens and universal nanocarriers. Pol J Microbiol 64:3–13. doi: 10.33073/pjm-2015-001. [DOI] [PubMed] [Google Scholar]
- 83.Rynda-Apple A, Patterson DP, Douglas T. 2014. Virus-like particles as antigenic nanomaterials for inducing protective immune responses in the lung. Nanomedicine (Lond) 9:1857–1868. doi: 10.2217/nnm.14.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Sun Y, Carrion R Jr, Ye L, Wen Z, Ro YT, Brasky K, Ticer AE, Schwegler EE, Patterson JL, Compans RW, Yang C. 2009. Protection against lethal challenge by Ebola virus-like particles produced in insect cells. Virology 383:12–21. doi: 10.1016/j.virol.2008.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Swenson DL, Warfield KL, Negley DL, Schmaljohn A, Aman MJ, Bavari S. 2005. Virus-like particles exhibit potential as a pan-filovirus vaccine for both Ebola and Marburg viral infections. Vaccine 23:3033–3042. doi: 10.1016/j.vaccine.2004.11.070. [DOI] [PubMed] [Google Scholar]
- 86.Warfield KL, Olinger G, Deal EM, Swenson DL, Bailey M, Negley DL, Hart MK, Bavari S. 2005. Induction of humoral and CD8+ T cell responses are required for protection against lethal Ebola virus infection. J Immunol 175:1184–1191. doi: 10.4049/jimmunol.175.2.1184. [DOI] [PubMed] [Google Scholar]
- 87.Wrammert J, Smith K, Miller J, Langley WA, Kokko K, Larsen C, Zheng NY, Mays I, Garman L, Helms C, James J, Air GM, Capra JD, Ahmed R, Wilson PC. 2008. Rapid cloning of high-affinity human monoclonal antibodies against influenza virus. Nature 453:667–671. doi: 10.1038/nature06890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Sarzotti-Kelsoe M, Bailer RT, Turk E, Lin CL, Bilska M, Greene KM, Gao H, Todd CA, Ozaki DA, Seaman MS, Mascola JR, Montefiori DC. 2014. Optimization and validation of the TZM-bl assay for standardized assessments of neutralizing antibodies against HIV-1. J Immunol Methods 409:131–146. doi: 10.1016/j.jim.2013.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Montefiori DC. 2005. Evaluating neutralizing antibodies against HIV, SIV, and SHIV in luciferase reporter gene assays. Curr Protoc Immunol Chapter 12:Unit 12.11. doi: 10.1002/0471142735.im1211s64. [DOI] [PubMed] [Google Scholar]