Abstract
Background:
Through evaluations of training programs, systematic reviews, and meta-analyses, advances in identifying best practices for disseminating motivational interviewing (MI) have emerged. To advance this work further, inclusion of thorough descriptions of the following is needed in research publications: study (design, trainee characteristics, setting characteristics), training and coaching methods (if applicable), trainer qualifications, and evaluation of MI skills.
Methods:
The purpose of this study was to systematically evaluate the research on MI training of substance use treatment professionals for the inclusion of such descriptions. Twenty-five studies were reviewed using a scoring rubric developed by the authors.
Results:
Just over two thirds of the studies (68%) were randomized controlled trials of MI training. The majority of studies provided information about (a) trainee characteristics (professional background =76%, education =60%, experience =56%); (b) setting characteristics training (80%); (c) training methods (format =96%, length =92%); (d) coaching (76%); and (e) evaluation of MI skills (92%).
Conclusion:
Findings suggest advancements in MI training studies since previous reviews, especially in regards to the inclusion of feedback and coaching. However, this review also found that inconsistencies in methods and reporting of training characteristics, as well as limited follow-up assessment of trainees’ skill, continue to limit knowledge of effective training methods.
Keywords: Motivational interviewing, systematic review, training
Introduction
There has been a growing literature focused on motivational interviewing (MI) training, with an emphasis on the evaluation of different methods. The description of MI as a simple concept comprising a complex skill set1 underscores the importance of training guidelines for effective treatment delivery and quality implementation. Early research evaluating MI training methods showed significant changes in clinician behaviors from training,2 yet those changes were not reflected in client outcomes. In 2009, Madson et al. systematically reviewed the MI training literature, finding that although MI trainings were generally effective, they often relied on workshop/seminar formats, which incorporated limited experiential activities, and there were very little coaching or feedback to build MI competency.3 Based on their findings, Madson and colleagues recommended that best practices for reporting MI training and evaluation should include standardized training procedures, an outline of effective ingredients, incorporation of evidence-based measures of competency, and a method for linking training to client outcomes.3 Subsequently, 2 systematic reviews have supported these recommendations.4,5 Toward that end, the purpose of the current study was to systematically review published research on MI training with substance use (SU) treatment professionals.
Potential benchmarks for best practices related to the duration and frequency of MI training recently emerged from 2 meta-analytic studies. First, de Roten et al. identified 12–16 hours as an adequate dose of MI workshop training for providers to achieve gains in MI skill, noting that coaching and feedback further enhances skill.6 Schwalbe et al. showed that MI training effects were best maintained through at least 3–4 postworkshop contacts, totaling a minimum of 5 hours of coaching from an expert MI trainer over a 6-month period.7 Evidence for best practices are starting to emerge, most notably concerning the value of extended training, including feedback and coaching. However, each review further emphasized the need for methodological quality and consistency in MI training studies to further advance best practices.
In the current review, we focus on key elements that should be included in reports of MI training studies to strengthen future research.8–12 The review is organized around 3 broad categories: study methodology, training methods, and evaluation. With regard to study methodology, research design provides important information about the strength of conclusions that can be drawn from a particular study.13 Also of import with regard to MI training for SU are the characteristics of trainees and training settings, as these are often highly variable and significantly influence the generalizability of findings.9,14,15 With regard to training methods, evidence-based training protocols for MI or other interventions are often not readily available, with a few notable exceptions such as the MIA: STEP (Motivational. Interviewing Assessment: Supervisory Tools for Enhancing Proficiency) protocol.16 As such, thorough descriptions of the training methods will better inform training implementation outside the research context. Descriptions should include specific information about the training methods (e.g., workshop, experiential activities, etc.), how those methods were selected, and trainer qualifications.10 Given longstanding evidence for the importance of coaching and feedback,6,7 information on feedback/coaching methods (length, number of sessions, method of delivery) is also important. With regard to evaluation, it is important to note whether researchers evaluated competency/skill development with evidence-based assessment tools (e.g., observational, client-completed measures).17
Given the broad implementation of MI training world-wide and the continual evolution of the MI training literature, it is imperative to systematically evaluate the quality and limitations of the existing literature in an ongoing fashion. This ensures that future research continues to improve in quality and scope. The current study focuses on the quality of methods and descriptions in research on MI training. The current study differs from prior studies, which examined MI across several professional disciplines, health care settings, and target behaviors. There is established evidence for MI efficacy in treating SU disorders; therefore, SU providers are an important focal group for evaluating and refining guidelines for effective MI training, which can eventually be translated to other target behaviors. Thus, the purpose of this study was to advance the MI training research with SU providers by evaluating MI training through updated training quality recommendations. Specifically, the review examines the literature published since a review published by Madson et al.,3 with a focus on study methodology, training methods, and evaluation.
Review procedure
We conducted a systematic review following Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) standards18 by searching the PsycINFO, PsycARTICLES, MEDLINE, Academic Search Premier, ERIC, and SocIndex databases to identify articles from 2008 to January 2018. Key terms used include Motivational Interviewing, Motivational Enhancement Therapy, Brief Motivational Intervention, Training, Workshop, Implementation, Dissemination, Substance Abuse, SU, Addiction, Alcohol, and Drug. We also reviewed the bibliography page on the MI Web site (http://motivationalinter-view.org/library/biblio.html) to identify additional articles for the review. Our review resulted in 136 articles, all of which outlined use of MI training methods with providers who were treating patients with SU issues. Although the screening, brief intervention, and referral to treatment (SBIRT) protocols incorporate varying degrees and elements of MI, we decided to exclude such articles because MI is not the sole focus of SBIRT; rather, it is embedded within a broader training protocols that may vary substantially in adherence to practices and principles of MI. We also did not want to confuse MI for SBIRT. Additional articles were excluded if the methodology included survey research or if the treatment targets were not substance abuse. As a result, 25 articles were included in the current review. We chose to include articles that were secondary analyses of previous studies and methods/protocol papers because they help contribute to the training literature. These 3 papers are identified in Table 1. Figure 1 outlines the study inclusion procedures following PRISMA guidelines.18
Table 1.
Study methodology.
| Reference | Study design | Program type | N | Education | Professional background | Years of clinical experience |
|---|---|---|---|---|---|---|
| Ager19 | SA | — | 136 | M | — | — |
| Baer20 | SA, RCT | OP | — | — | — | — |
| Carpenter21 | SA, RCT | OP, RES | 58 | M, BD, NF | — | 7.2 |
| Secondary analysis of Smith22 | ||||||
| Clancy23 | SA | OTH | 64 | DD, M, GD, DG, CT, Dl | NRS, PSYCH, SW, OTH | 2.8/7.1 |
| Darnell24 | SA, RCT, LTS | OTH | 30 | DD, M, GD, DG, CT, Dl | NRS, SW, OTH | >1–31+ |
| Decker25 | SA, RCT, LTS | OP | 91 | DG | — | 9.1–11.5 |
| Secondary analysis of Martino26 | ||||||
| Doran27 | SA, LTS | — | 576 | DG | GM, NRS, PSYCH, OTH | 11.1 |
| Drapkin28 | SA | — | 264 | — | ADC, CN, NRS, PSY, PSYCH, SW, OTH | — |
| Dunn29 | SA, RCT | Med | 15 | M, BD | SW | 4.5–15.4 |
| Forrester30 | SA | OTH | 42 | — | SW | |
| Forsberg31 | SA, RCT, LTS | OTH | 18 | — | OTH | 8–10 |
| Forsberg32 | SA, RCT, LTS | OTH | 45 | — | CJ | — |
| Fu33 | SA, RTC | Med | 34 | — | GM, NRS | 11.1–14.1 |
| Isenhart34 | SA, RTC | Med | 2 | DD, MD | PSY, PSYCH | — |
| Jaffray35 | SA, RCT, LTS | OTH | 84 | — | PHAR | — |
| Malan36 | OTH | Med | 41 | MD, GD | GM, NRS | — |
| Martino37 | SA | OTH | 26 | DD, M, BD, AD, NF | ADC, NRS, PSYCH, SW, OTH | 12.5 |
| Martino26 | SA, RTC | OP | 90 | DD, M, BD, AD, NF | ADC, GM, NRS, PSYCH, SW, OTH | 8.9–10.7 |
| Martino16 | SA, RTC, LTS | Med | 30 | — | GM, NRS | — |
| Martino38 | SA, RTC | OP | 66 | DD, M, BD, AD, NF, CT | ADC, OTH | 8.9 |
| Methods paper | ||||||
| Mitcheson39 | SA, RTC | OTH | 30 | — | ADC | — |
| Moyers40 | SA, RTC | OTH | 190 | — | ADC, CN, NRS, PSYCH, SW, GM | 12.4 |
| Schumacher15 | SA | — | 16 | BD or higher, less than BD | ADC, OTH | 5.7 |
| Smith22 | SA, RTC | OP, RES | 97 | M, BD, NF | — | 7.8–8.5 |
| Stein41 | SA, RTC, LTS | — | 25 | M, BD | — | — |
Note. SA: stand-alone; RCT: randomized controlled trial; LTS: larger treatment study; OP: outpatient; Res: residential; Med: medical; OTH: other setting; DD: doctoral degree; MD: medical degree; M: master’s degree; GD: graduate degree; DG: degree; BD: bachelor’s degree; AD: associated degree; CT: certificate; DI: diploma; NF: no formal training; ADC: alcohol and drug counselor; CJ: criminal justice; GM: general medicine; CN: counseling; NRS: nursing; PSY: psychiatry; PSYCH: psychology; SW: social work; PHAR: pharmacy.
Figure 1.
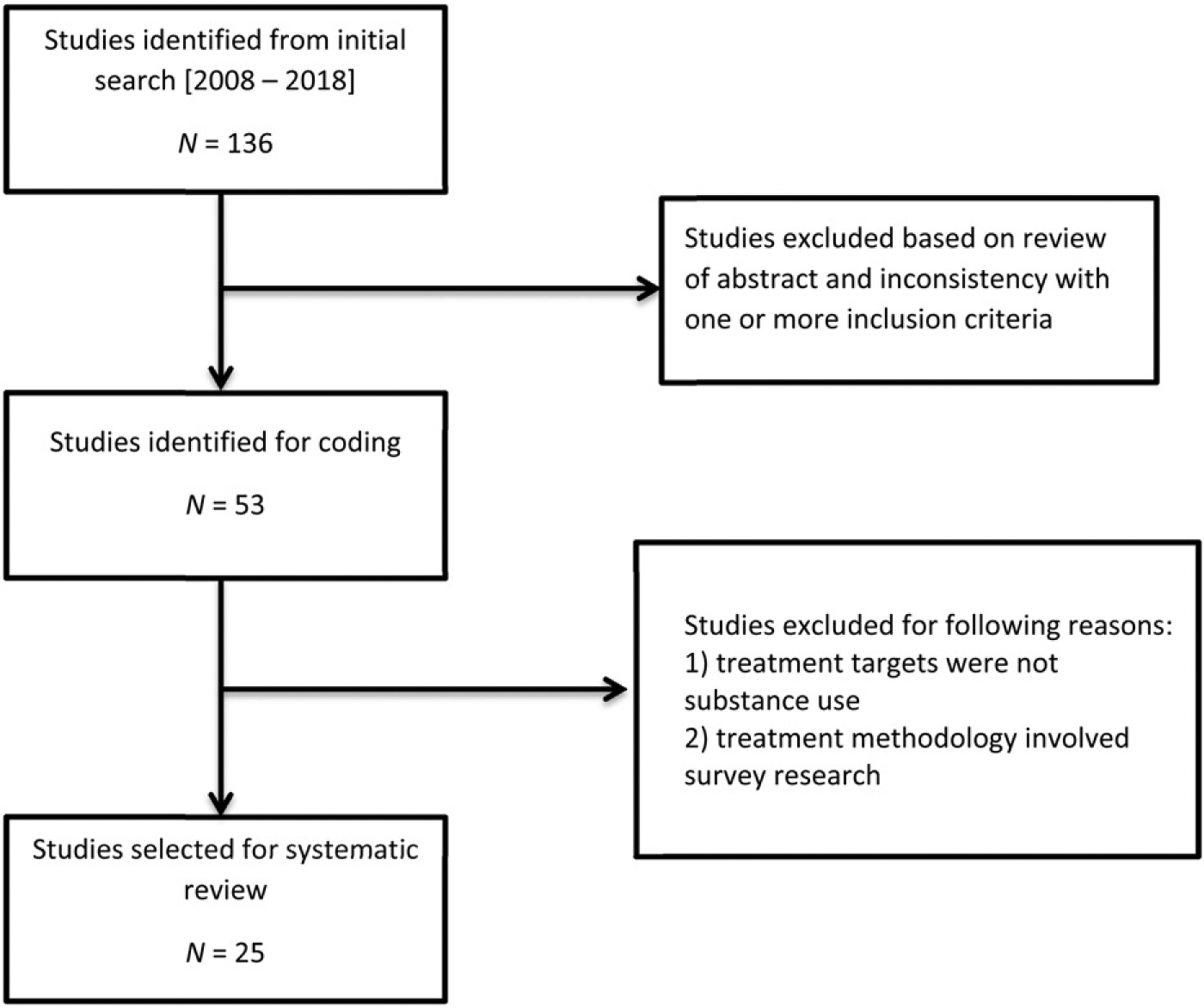
Flow chart of study inclusion.
The first 2 authors independently evaluated the included articles using a coding form developed by the second author. This form was based on recommendations for evaluating the methodological quality of MI training10 and was approved by the first 3 authors. Descriptors on the coding form were categorized under study methodology, training methods, and training evaluation. Study methodology descriptors included the study design, setting characteristics, and trainee characteristics. The training methods included descriptors of MI training method and trainer qualifications. Specific MI training method descriptors included MI workshop type, length and duration of training, feedback and coaching of MI using a valid fidelity measure, and amount and duration of feedback and coaching sessions. Descriptors of training evaluation included trainee outcomes and client outcomes.
Decision rules were also included to determine whether authors provided a thorough description of MI training methods and evaluation. If authors described the type of MI training and specified the number or length of training sessions, we determined that they provided a description of training methods. Further, if authors used a fidelity measure but did not provide feedback, then we determined that feedback and coaching methods were not adequately described. Regarding training evaluation, we determined that authors used a fidelity measure to evaluate trainees’ MI competency and proficiency if a combination of summary scores, global scores, and behavioral counts was reported. We also determined that the assessment of continued use of MI skills was appropriately described if authors reported trainee scores after 1, 3, 6, or 12 months of formal MI training.
A detailed account of the study findings is presented in Tables 1, 2, and 3. Specifically, study methodology findings are presented in Table 1. Details of training methods are presented in Table 2, and findings for training evaluation are presented in Table 3. Highlights of each evaluation component are described below.
Table 2.
Training methods.
| Reference | CPU | RE | WO | WEL | WFC | Comparison groups | No. Of sessions | Session length | Number of coaching sessions | Measure used | % completion |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Ager19 | — | — | — | — | — | — | — | — | 0 | No | 100 |
| Baer20 | X | X | WO vs. WFC | 2/5 | 15 hours | Not specified | No | 85 | |||
| Carpenter21 | X | X | X | WO vs. WEL vs. WFC | 2 | 8 hours | 5 | MITI | 51–75 | ||
| Clancy23 | X | X | WO vs. WFC | 2 | 2 days | 3 | No | 76–100 | |||
| Darnell24 | X | WFC vs. waitlist | 1 | 1day | 2–6 | MITI | 51–75 | ||||
| Decker | X | X | RE vs. WFC vs. TNT WFC | 1 | 15 hours | 3 | ITRS | ? | |||
| Doran27 | X | None | 2 | 3 days/2 days | 0 | No | No | ||||
| Drapkin28 | X | None | 1 | 3.5 days | 4 | MITI | 76–100 | ||||
| Dunn29 | X | RCP (high dose) vs. NRCP (low dose) | 1 | 5.9 (low dose) to 9.6 hours (high dose) | 5 | No | 76–100 | ||||
| Forrester30 | X | X | WEL vs. WFC | 2 | 1day | 5 | No | 76–100 | |||
| Forsberg31 | X | WFC vs. PAU | 1 | 12 hours | 28 (estimate) | MITI | 26–50 | ||||
| Forsberg32 | X | X | WEL vs. WFC vs. PAU | 1 | 5 days | 5 | MITI | 76–100 | |||
| Fu33 | X | X | WEL vs. WFC | 1 | ½ day | 6 | No | 76–100 | |||
| Isenhart34 | X | None | 1 | 1day | 10 | MICAFF | 76–100 | ||||
| Jaffray35 | X | WEL vs PAU | 4 | — | 0 | BECCI | 76 | ||||
| Malan36 | X | None | 4 | 2 hours | 0 | MITI, OTH | No | ||||
| Martino37 | X | X | X | None | 8 | 1–2 hours | 1–2 | ITRS | 51–75 | ||
| Martino26 | X | X | RE vs. WFC vs. TNT WFC | 1 | 15 hours | 3 | ITRS | 76–100 | |||
| Martino16 | X | X | WO vs. WFC | 1 | 1 day | 40 (estimate) | ITRS | 76–100 | |||
| Martino38 | X | WFC vs. WFC* | 1 | 8 hours | up to 7 | ITRS | 51–75 | ||||
| Mitcheson39 | X | X | WFC vs. RE | 1 | 2 days | 4 | No | 51–75 | |||
| Moyers40 | X | WFC vs. WFC* | 2 | 2 days | 4 (2 individual, 2 group) | MITI, MISC | 76–100 | ||||
| Schumacher15 | X | None | 1 | 2 day | 10 | MITI | 76–100 | ||||
| Smith22 | X | X | WEL vs. WFC vs. WFC-T | 1 | 13 hours | 5 | MITI | 76–100 | |||
| Stein41 | X | None | - | 2–5 days | Not specified | MITI | No |
Note. CPU: computer training; RE: reading; WO: workshop only; WEL: workshop plus experiential; WFC: workshop and feedback/coaching; PAU: practice as usual; CTT: context-tailored training; TNT: train the trainer; RCP: routine care providers; NRCP: nonroutine care providers; WFCT: workshop, feedback/coaching via teleconference; MITI: MI Treatment Integrity Code; MISC: MI Skill Code; BECCI: Behavior Change Counseling Index; ITRS: Independent Tape Rater Scale; MICAFF: VA MI Consultation and Feedback Form.
In these trials, enhanced forms of WFC were compared with general forms of WFC.
Table 3.
Training evaluation.
| Reference | Outcomes measured | Proficiency met | Competency met | Valid coding tool used | Sustained skill assessed | Client outcome measured | Type of client outcomes | Training connected to outcome |
|---|---|---|---|---|---|---|---|---|
| Ager19 | KN, SK | No | No | No | No | No | — | No |
| Baer20 | SK | Yes | Yes | MITI | Yes | No | — | No |
| Carpenter21 | SK | Yes | Yes | MITI | Yes | No | — | No |
| Clancy23 | KN, SC, OTH | — | — | — | No | No | — | No |
| Darnell24 | SK | Yes | Yes | MITI | Yes | No | — | No |
| Decker25 | SC, SK | — | — | IRTS | Yes | No | — | No |
| Doran27 | SK, OTH | Yes | No | VASE-R | No | No | — | No |
| Drapkin28 | KN, SK | — | Yes | Not reported | Yes | No | — | No |
| Dunn29 | SK | Yes | — | MITI | No | No | — | No |
| Forrester30 | KN, SK, OTH | No | Yes | Not reported | No | No | — | No |
| Forsberg31 | SK | Yes | No | MITI | Yes | No | — | No |
| Forsberg32 | SK | No | — | MITI | No | No | — | No |
| Fu33 | KN, SC, SK | No | No | MITI | No | No | — | No |
| Isenhart34 | SK | Yes | No | MICAFF | No | No | — | No |
| Jaffray35 | SK | No | No | BECCI | No | Yes | ABS, RET | No |
| Malan36 | SK | No | No | MITI, OTH | No | No | — | No |
| Martino37 | SK | Yes | Yes | ITRS | No | No | — | No |
| Martino26 | SK | Yes | Yes | ITRS | Yes | No | — | No |
| Martino16 | SAT, KN, SC, OTH | — | — | — | No | No | — | No |
| Martino38 | SK | — | Yes | ITRS | Yes | Yes | ABS, RET | No |
| Mitcheson39 | SK | No | No | MITI | Yes | No | — | No |
| Moyers40 | KN, SK, OTH | — | — | MITI, MISC | Yes | No | — | No |
| Schumacher15 | SK | No | No | MITI | Yes | No | — | No |
| Smith22 | SK | Yes | Yes | MITI | Yes | No | — | No |
| Stein41 | SK | No | No | OTH | No | No | — | No |
Note. SAT: satisfaction; KN: knowledge; SC: self-confidence; SK: skills; OTH: other; MITI: MI Treatment Integrity Code; BECCI: Behavior Change Counseling Index; ITRS: Independent Tape Rater Scale; VASE-R: video assessment of simulated encounters; ABS: abstinence; RET: treatment retention.
Results
Study design and sample size
All studies provided sufficient information to code study design. Just over two thirds of the studies (n = 17, 68%) were randomized controlled trials of MI training in which participants were randomly assigned either to receive various forms of MI training or to receive MI training or a comparison condition. The remaining studies utilized opentrial designs in which all participants received MI training. Almost all (n = 24, 96%) were studies of training in MI as a stand-alone intervention. The remaining study36 provided training in brief behavior change counseling. Eight studies (32%) provided training in MI as part of a larger treatment study in which MI was one of the interventions of interest. All studies with the exception of Baer et al.20 provided information about the number of individuals trained (n = 24, 96%). Sample size varied across studies, ranging from 2 to 576 with a mean of 86.25 (SD =120.44).25,34
Trainee professional backgrounds
Nineteen studies provided specific information about the professional backgrounds of training participants (76%). The most well-represented professions were nursing (n = 10, 40%), social work (n = 8, 36%), and psychology (n = 7, 28%). Alcohol and drug counselors (n =7, 28%) and general medical practitioners (n =6, 24%) were also included in several studies. Two studies (8%) included psychiatrists, and 2 included counselors (8%). Pharmacists and criminal justice employees were included in 1 study each (4%). Nine studies (36%) included trainees from other backgrounds, such as case managers,37 supervisory staff at community treatment facilities,15 and other professionals in patient care roles (e.g., nonspecified clinicians,23 physician’s assistants24).
Trainees’ and trainers’ educational backgrounds and years of experience
In addition to assessing professional background, we identified trainees’ education levels and years of clinical experience. Education level was reported in 60% of studies (n = 15), and years of clinical experience was reported in 56% (n = 14). Fifty-two percent of studies (n = 13) included trainees with advanced degrees (i.e., master’s or greater). Specifically, 40% of studies (n = 10) included trainees who had a master’s degree, 28% (n = 7) included trainees who had a nonmedical doctoral degree (e.g., PhD, PsyD, DSW), and 8% (n = 2) included trainees who had a medical doctoral degree (i.e., MD). In addition, 48% of studies (n = 12) included trainees with a bachelor’s degree or equivalent, and 32% (n = 8) included trainees with less than a bachelor’s degree (e.g., associate’s degree, certificate, high school diploma).1 In over a third of the studies (40%, n = 10), information regarding trainees’ educational background was not reported. Trainees’ years of clinical experience varied widely both within and across studies; whereas some trainees reported less than 1 year of clinical experience, others reported over 30. The majority of studies (n = 20, 80%) provided some information about trainer qualifications and/or years of experience, although the detail of information varied. Sixty percent of studies (n = 15) reported that trainers were members of the Motivational Interviewing Network of Trainers (i.e., MINT); in 12% of studies (n = 3), trainers were Department of Veterans Affairs (VA)-certified MI trainers.
Setting characteristics
Twenty studies (80%) provided sufficient information to code the type of program in which training participants provided substance abuse interventions. Just under a quarter of studies (24%, n = 6) were conducted with providers in outpatient clinics (e.g., community substance abuse clinics), and another fifth (20%, n = 5) were conducted with providers in medical settings (e.g., inpatient units). Two studies (8%) were conducted with providers in residential settings (e.g., community settings with a residential component).2 The most commonly coded category for program type was other (n = 9, 36%), indicating that frequently the training was offered to providers in program types that did not meet our a priori decision rules for coding setting. Examples of these types of programs included trauma centers,24 prison services,32 and pharmacies.35
Format and length of training
Most studies (96%, n = 24) provided information about the format of MI trainings.3 Consistent with recommendations,3,5,7 the majority of studies (84%, n = 21) used a workshop plus feedback/coaching training format as the primary method (i.e., experimental training condition) for at least 1 group of trainees (i.e., in some studies training method was the independent variable). The next most common training method comprised workshops and experiential exercises (e.g., role play, group exercises), used as the primary training method in 8% of studies (n = 2). In 1 study (4%), a didactic workshop was used as the primary training method. Although other methods (i.e., readings [n = 4, 16%], computer trainings [n = 1, 4%]) were used, these served as either the comparison group or steps in a trainee skill-based stepped process27 rather than the primary training format. Just over half of the reviewed studies (n = 13, 52%) compared trainings using workshops plus feedback/coaching with another training method. Additionally, in 2 studies (8%), workshops utilizing a general approach to feedback/coaching sessions were compared with trainings in which workshops and enhanced forms of feedback/coaching (i.e., MIA: STEP; MI-LEAF [Motivational Interviewing Language Enhanced Attention and Focus]) were utilized.16,40
The number of training sessions and length of each session varied across studies. Similar to Madson et al.,3 we found that just over half of the studies provided a single training session (n = 14, 56%), although the use of 2 training sessions was also common (n = 5, 20%). Four training sessions were used in 2 studies (8%). In the remaining 2 studies that reported number of training sessions, trainees underwent either 2 or 5 (n = 1, 4%) training sessions (i.e., depending on group assignment) or 8 (n = 1, 4%) training sessions. The reporting metric for session length (i.e., number of days vs. hours) varied across studies, limiting our ability to provide summary statistics about the length of sessions. However, as presented in Table 2, studies included in this review tended to provide more total hours of training than those reviewed previously;3 for example, 100% of the studies included in the current review provided more than 8 total hours of training, as compared with 71% of those in the previous review.
Coaching, feedback, and assessment of skills
Perhaps the most promising aspect of the studies included in the current review was a shift toward incorporating coaching and/or feedback into MI training. Despite previous authors stressing the importance of ongoing feedback for the development and maintenance of MI skills,7 in a prior review only 6 studies (22%) described the use of supervision and only 1 used ongoing coaching.3 In contrast, 84% of studies (n = 21) included in this review reported utilizing at least 1 coaching session, with the majority (n = 15, 60%) reporting the use of 4 or more sessions.
As an aspect of coaching, it was common for studies to utilize validated objective measures of performance. Such measures included the Motivational Interviewing Treatment Integrity (MITI; n = 10, 40%), the Independent Tape Rater Scale (ITRS; n = 5, 20%), the Motivational Interviewing Skill Code (MISC; n = 2, 8%), the MI Consultation and Feedback Form (MICAFF), and the Behavior Change Counseling Index (BECCI; n = 1 each, 4% each).4 In the majority of studies, such measures were used to assess trainees’ MI proficiency (n = 19, 76%; trainees achieved proficiency in 10 studies) and competency (n = 19, 76%; trainees achieved competency in 9 studies).
Training evaluation
With one exception, the validated measures of objective performance that were utilized to provide feedback-based coaching were also utilized to evaluate training outcomes. The only exception was Stein et al. who used the MITI for coaching41 but the Helpful Responses Questionnaire for outcomes.42 In addition to the studies that used validated coding measures based on work samples for both coaching and evaluation, an additional 5 studies (20%) used such measures for evaluation only. The most commonly assessed outcome was MI skills (n = 23, 92%), followed by knowledge (n = 7, 28%) and self-confidence (n = 4, 16%). Although also suggestive of a positive departure from earlier training methods in which few studies did so, just under half of the reviewed studies (n = 12, 48%) assessed whether trainees maintained skills after training concluded. In 1 study (4%), trainee satisfaction was assessed. Outcomes classified as other (e.g., trainee readiness to change; utilization of change talk) were assessed in 20% of studies (n = 5). Consistent with Madson et al.,3 it was uncommon for studies to assess client outcomes. In the 2 studies that did so,16,35 both treatment retention and substance use/abstinence use were assessed, and neither study found these outcomes to be associated with MI training.
Discussion
The goal of this paper was to systematically review the MI training literature for SU treatment, with a focus on the methods and reporting in recent MI training projects. Our review highlights that the literature has grown and improved significantly in quality since prior reviews. For example, the studies reviewed included enhanced descriptions of training methodology, populations, and settings. Moreover, many of the reviewed studies conducted some form of randomized trial that allowed comparison of training conditions. Studies such as these will uncover the optimal conditions to help clinicians acquire MI skills and provide evidence-based implementation methods to incorporate MI into standard practice. Further, a remarkable change over previous reviews was the number of studies that incorporated coaching and the use of valid observational tools. Nonetheless, we also uncovered areas for further development to strengthen the MI training literature.
In line with recommendations for a thorough description of trainee and setting characteristics involved in MI training programs,5,7,10 most of the reviewed studies provided adequate details of trainee and setting characteristics. However, the descriptions of trainer characteristics varied. In order to move the science forward, it will be imperative for future studies to include trainer qualifications; to ensure that MI skills are being transferred adequately, we must know that they are being transferred from those who have sufficient knowledge of the technology. Therefore, it is recommended that researchers continue to provide a basic description about trainees and the training setting as well as describe the trainer characteristics and qualifications. Further, information on who is being trained, their training, professional and theoretical (e.g., 12-step, cognitive behavioral) background, and prior experience with MI is important. This information will help clarify whether failures of technology transfer are related to the implementation process (e.g., methodology) or influential determinants of implementation outcome (e.g., trainer, trainee, or organizational issues).43 Training programs and clinical sites will also benefit from this information in determining the necessary qualifications of trainers in order to expect adequate outcomes from learners.
A promising change in studies of MI training has been the transition from primarily workshop/didactic-based trainings to trainings that incorporate coaching and feedback. In fact, many of the reviewed studies utilized workshop-only conditions as a comparison/control group, to better identify specific advantages of adding feedback/coaching training methods. Although an undeniable step toward progress, an important consideration for future studies is the need for additional description about the exact methods used (i.e., such that a training method could be directly replicated) for control/comparison and study conditions. Additionally, given that feedback is known to enhance training, future progress can be made by examining both the process and content of feedback. Of the reviewed studies, 2 provide excellent examples of how these aspects can be described (e.g., the systematic approach of MIA: STEP; the language focus of MI-LEAF) and compared with “feedback as usual.”16,40
There are various resources describing different MI training exercises and strategies,44 and it would benefit MI training research and practice to identify effective experiential MI training strategies. In this regard, researchers may consider modeling their training descriptions after Darnell et al.,24 who provided specifics about the training methods, including the content (e.g., 0–10 scaling questions to identify importance of and confidence in change) covered in training sessions. These detailed descriptions are vital for comparing effects across studies, as well as standardizing training to optimize efficiency and effectiveness of MI training programs and components. Moving forward, quality implementation of MI will entail identifying training components that are necessary for successful outcomes, as well as those components that can be modified based on organization, clinician, or client needs.45 Certainly, it is challenging to describe all the specifics of a MI training project given journal word limits. Some of the projects reviewed here24,40 or protocol papers26 provide examples for disseminating future MI training projects.
A major finding of the current review was that most studies included some form of coaching and feedback. Research by Forsberg et al. demonstrates one effort to meet these standards.31 Clinicians were provided with an initial MI training (workshop with experiential exercises) of 12 hours, followed by 84 hours of additional MI supervision across 11 assessment periods covering 2.5 years. During this time span, a total of 33 coded recordings per clinician were reviewed with a valid integrity measure (i.e., MITI 3.0). Moving forward, additional information about coaching methods can inform an effective, standardized approach to MI training.
We found great variability in the description of coaching methods. More consistent reporting of the processes and procedures would enhance conclusions on how to establish coaching best practices. Specifically, future studies should report the number of coaching sessions intended for each trainee, the number of sessions completed, and the average length of sessions. Some of the studies reviewed used individual coaching, whereas others used group coaching or a combination of approaches. However, we know little about the differential effectiveness of these coaching formats. Similarly, it appears that using valid observational measures enhance coaching, and it would be important to identify best practices for using these measures. For example, one could investigate the value of focusing on MITI global scores or behavioral counts or both when providing feedback. Similarly, there could be investigations for how this feedback is provided based on using a MI-consistent46 or inconsistent coaching style. The coaching and feedback literature may also benefit from incorporating other means of feedback on MI use. Recent developments in assessing client feedback using the Client Evaluation of MI (CEMI)47,48 may assist the coaching and feedback process and is worthy of investigation as an additional training element. Empirically identifying these best practices for coaching and feedback will further technology transfer and potentially lower costs associated with implementation, which is particularly important given the resource-intensive training process.
Despite the advancements in MI training, there continues to be a paucity of literature that links training outcomes with client outcomes. We found 2 studies that examined this relationship: Jaffray et al. and Martino et al. linked MI training to client substance use and treatment retention.16,35 Moving forward, it will be important to identify not only whether training processes develop clinician competency but ultimately also whether these processes facilitated MI consistent behaviors and positive behavior change in clients. Future MI training research should strive to link training outcomes, including global MI competency and behaviors, to client outcomes, including use behavior and treatment retention, as well as to therapeutic factors such as working alliance and treatment engagement.
This review provides an updated examination of the MI training literature, with a focus on the methods and quality in recent research. Although the findings are encouraging, they need to be considered within study limitations and necessary next steps. First, we limited the review to focus on SU professionals, and it may be valuable to replicate these results with other behaviors and nonprofessionals such as peer specialists/advocates.49 Our a priori criteria may have limited some of our findings, and future studies may want to consider broader evaluation criteria to reduce the large number of studies coded as “other.” We also decided to exclude SBIRT training studies from this review. Given the rapid developments in SBIRT,19 it may be valuable to systematically review those training studies to assess similarities and differences with these findings. Further, we chose to include 1 methods38 and 2 secondary analysis papers21,25 that have the potential to inflate MI training components or minimize outcomes. However, these papers were included in this review, as we believe they provide value not better captured elsewhere. Finally, this review addresses just one aspect of MI dissemination and implementation: training. Future investigations of MI training should include diverse methodologies such as qualitative designs and action research as well as mixed methods to better evaluate process and outcomes. Key questions about other factors (e.g., feasibility) that influence the integration of MI into practice settings must be addressed in future research.45,50
Funding
Villarosa-Hurlocker are supported by a training grant (T32-AA018108) from the National Institute on Alcohol Abuse and Alcoholism (NIAAA) in the United States.
Footnotes
Trainees from a variety of educational backgrounds tended to be included within a single study; as such percentages sum to over one-hundred.
These two studies conducted trainings in both outpatient and residential settings.
The one study that did not include information about training31 referenced an older paper (i.e., Ager et al., 200551) where this information was reported. To be consistent with our a priori decision rules regarding coding, we do not provide information that was not reported in the reviewed paper.31
Some studies utilized multiple measures; as such, percentages sum to over 100.
References
- [1].Miller W, Rollnick S. The effectiveness and ineffectiveness of complex behavioral interventions: impact of treatment fidelity. Contemp Clin Trials. 2014;37(2):234–241. [DOI] [PubMed] [Google Scholar]
- [2].Miller W, Mount K. A small study of training in motivational interviewing: does one workshop change clinician and client behavior? Behav Cognit Psychother. 2001;29(4):457–471. [Google Scholar]
- [3].Madson M, Loignon A, Lane C. Training in motivational interviewing: a systematic review. J Subst Abuse Treat. 2009;36(1): 101–109. [DOI] [PubMed] [Google Scholar]
- [4].Barwick M, Bennett L, Johnson S, McGowan J, Moore J. Training health and mental health professionals in motivational interviewing: a systematic review. Child Youth Serv Rev. 2012;34(9):1786–1795. [Google Scholar]
- [5].Söderlund L, Madson M, Rubak S, Nilsen P. A systematic review of motivational interviewing training for general health care practitioners. Patient Educ Couns. 2011;84(1):16–26. [DOI] [PubMed] [Google Scholar]
- [6].De Roten Y, Zimmermann G, Ortega D, Despland J. Meta-analysis of the effects of MI training on clinicians’ behavior. J Subst Abuse Treat. 2013;45(2):155–162. [DOI] [PubMed] [Google Scholar]
- [7].Schwalbe C, Oh H, Zweben A. Sustaining motivational interviewing: a meta-analysis of training studies. Addiction. 2014;109(8):1287–1294. [DOI] [PubMed] [Google Scholar]
- [8].Carroll K Training in vain? Addiction. 2016;111(7):1153–1154. [DOI] [PubMed] [Google Scholar]
- [9].Hall K, Staiger PK, Simpson A, Best D, Lubman DI. After 30 years of dissemination, have we achieved sustained practice change in motivational interviewing? Addiction 2016;111(7):1144–1150. [DOI] [PubMed] [Google Scholar]
- [10].Madson MB, Schumacher JA, Baer JS, Martino S. Motivational interviewing for substance use: Mapping out the next generation of research. J Subst Abuse Treat. 2016;65:1–5. [DOI] [PubMed] [Google Scholar]
- [11].Miller W, Moyers T. Asking better questions about clinical skills training. Addiction. 2016;111(7):1151–1152. [DOI] [PubMed] [Google Scholar]
- [12].Miller W, Moyers T. Motivational interviewing and the clinical science of Carl Rogers. J Consult Clin Psychol. 2017;85(8): 757–766. [DOI] [PubMed] [Google Scholar]
- [13].van Tulder MW, Furlan A, Bombardier C, Bouter L, Editorial B. Of The Cochrane Collaboration Back Review Group. Updated method guidelines for systematic reviews in the cochrane collaboration Back Review Group. Spine 2003;28(12): 1290–1299. [DOI] [PubMed] [Google Scholar]
- [14].Hallgren K, Dembe A, Pace B, et al. Variability in motivational interviewing adherence across sessions, providers, sites, and research contexts. J Subst Abuse Treat. 2018;84:30–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Schumacher J, Madson M, Norquist G. Using telehealth technology to enhance motivational interviewing training for rural substance abuse treatment providers: a services improvement project. Behav Ther 2011;34(4):64–70. [Google Scholar]
- [16].Martino S, Paris M, Añez L, et al. The effectiveness and cost of clinical supervision for Motivational Interviewing: A randomized controlled trial. J Subst Abuse Treat. 2016;68:11–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Bellg AJ, Borrelli B, Resnick B, et al. Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH behavior change consortium. Health Psychol. 2004;23(5):443–451. [DOI] [PubMed] [Google Scholar]
- [18].Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269. [DOI] [PubMed] [Google Scholar]
- [19].Ager R, Roahen-Harrison S, Rice J, et al. Predictors of adopting motivational enhancement therapy. Res Soc Work Pract. 2011;21(1):65–76. [Google Scholar]
- [20].Baer J, Wells E, Rosengren D, et al. Agency context and tailored training in technology transfer: a pilot evaluation of motivational interviewing training for community counselors. J Subst Abuse Treat. 2009;37(2):191–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Carpenter K, Cheng W, Nunes E, et al. "Old dogs" and new skills: how clinician characteristics relate to motivational interviewing skills before, during, and after training. J Consult Clin Psychol. 2012;80(4):560–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Smith J, Carpenter K, Nunes E, et al. Training substance abuse clinicians in motivational interviewing using live supervision via teleconferencing. J Consult Clin Psychol. 2012;80(3):450–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Clancy R, Taylor A. Engaging clinicians in motivational interviewing: Comparing online with face-to-face post-training consolidation. Int J Ment Health Nurs 2016;25:51–61. [DOI] [PubMed] [Google Scholar]
- [24].Darnell D, Dunn C, Atkins D, Ingraham L, Zatzick D. A randomized evaluation of motivational interviewing training for mandated implementation of alcohol screening and brief intervention in trauma centers. J Subst Abuse Treat. 2016;60:36–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Decker S, Martino S. Unintended effects of training on clinicians’ interest, confidence, and commitment in using motivational interviewing. Drug Alcohol Depend. 2013;132(3): 681–687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Martino S, Ball S, Nich C, et al. Teaching community program clinicians motivational interviewing using expert and train-the-trainer strategies. Addiction. 2011;106(2):428–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Doran N, Hohman M, Koutsenok I. Linking basic and advanced motivational interviewing training outcomes for juvenile correctional staff in California. J Psychoactive Drugs. 2011;43(Sup1):19–26. [DOI] [PubMed] [Google Scholar]
- [28].Drapkin M, Wilbourne P, Manuel J, et al. National dissemination of motivation enhancement therapy in the Veterans Health Administration: training program design and initial outcomes. J Subst Abuse Treat. 2016;65:83–87. [DOI] [PubMed] [Google Scholar]
- [29].Dunn C, Darnell D, Carmel A, et al. Comparing the motivational interviewing integrity in two prevalent models of brief intervention service delivery for primary care settings. J Subst Abuse Treat. 2015;51:47–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Forrester D, McCambridge J, Waissbein C, Emlyn-Jones R, Rollnick S. Child risk and parental resistance: can motivational interviewing improve the practice of child and family social workers in working with parental alcohol misuse? Br J Soc Work. 2008;38(7):1302–1319. [Google Scholar]
- [31].Forsberg L, Forsberg L, Lindqvist H, Helgason A. Clinician acquisition and retention of Motivational Interviewing skills: a two-and-a-half-year exploratory study. Subst Abuse Treat Prev Policy. 2010;5(1):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Forsberg L, Ernst D, Farbring C. Learning motivational interviewing in a real-life setting: a randomised controlled trial in the Swedish prison service. Crim Behav Ment Health. 2011;21(3):177–188. [DOI] [PubMed] [Google Scholar]
- [33].Fu S, Roth C, Zillich A, et al. Training primary care clinicians in motivational interviewing: a comparison of two models. Patient Educ Couns. 2015;98(1):61–68. [DOI] [PubMed] [Google Scholar]
- [34].Isenhart C, Dieperink E, Lenox R, et al. Training and maintaining motivational interviewing skills in a clinical trial. J Subst Use. 2014;19(1–2):164–170. [Google Scholar]
- [35].Jaffray M, Matheson C, Bond CM, et al. Does training in motivational interviewing for community pharmacists improve outcomes for methadone patients? A cluster randomised controlled trial. Int J Pharm Pract. 2014;22(1):4–12. [DOI] [PubMed] [Google Scholar]
- [36].Malan Z, Mash B, Everett-Murphy K. Evaluation of a training programme for primary care providers to offer brief behaviour change counselling on risk factors for non-communicable diseases in South Africa. Patient Educ Couns. 2016;99(1):125–131. [DOI] [PubMed] [Google Scholar]
- [37].Martino S, Canning-Ball M, Carroll K, Rounsaville B. A criterion-based stepwise approach for training counselors in motivational interviewing. J Subst Abuse Treat. 2011;40(4):357–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Martino S, Zimbrean P, Forray A, et al. See one, do one, order one: a study protocol for cluster randomized controlled trial testing three strategies for implementing motivational interviewing on medial inpatient units. Implementation Sci. 2015;10(1): 138–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Mitcheson L, Bhavsar K, McCambridge J. Randomized trial of training and supervision in motivational interviewing with adolescent drug treatment practitioners. J Subst Abuse Treat. 2009;37(1):73–78. [DOI] [PubMed] [Google Scholar]
- [40].Moyers T, Houck J, Glynn L, Hallgren K, Manuel J. A randomized controlled trial to influence client language in substance use disorder treatment. Drug Alcohol Depend. 2017;172:43–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Stein L, Clair M, Soenksen-Bassett S, Martin R, Clarke J. Studying process and proximal outcomes of supervision for motivational interviewing. Train Educ Prof Psychol. 2015;9(2):175–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Miller W, Hedrick K, Orlofsky D. The Helpful Responses Questionnaire: A procedure for measuring therapeutic empathy. J Clin Psychol. 1991;47(3):444–448. [DOI] [PubMed] [Google Scholar]
- [43].Schumacher J, Madson M, Nilsen P. Barriers to learning motivational interviewing: a survey of motivational interviewing trainers’ perceptions. J Addict Offender Couns. 2014;35(2):81–96. [Google Scholar]
- [44].Rosengren DB. Building Motivational Interviewing Skills: A Practitioner Workbook. 2nd Edition). New York: Guilford Press; 2017. [Google Scholar]
- [45].Damschroder L, Hagedorn H. A guiding framework and approach for implementation research in substance use disorders treatment. Psychol Addict Behav. 2011;25(2):194–205. [DOI] [PubMed] [Google Scholar]
- [46].Madson MB, Bullock EE, Speed AC, Hodges SA. Supervising substance abuse treatment: specific issues and a motivational interviewing model In Hess AK, Hess KD, Hess TH. eds. Psychotherapy Supervision: Theory Research and Practice. 2nd ed. Hoboken, NJ: John Wiley and Sons; 2008:340–358. [Google Scholar]
- [47].Madson M, Mohn R, Stein B, et al. Measuring client perceptions of motivational interviewing: factor analysis of the Client Evaluation of Motivational Interviewing Scale. J Subst Abuse Treat. 2013;44(3):330–335. [DOI] [PubMed] [Google Scholar]
- [48].Madson M, Villarosa M, Schumacher J, Mohn R. Evaluating the validity of the Client Evaluation of Motivational Interviewing Scale in a brief motivational intervention for college student drinkers. J Subst Abuse Treat. 2016;65:51–57. [DOI] [PubMed] [Google Scholar]
- [49].Tsai J, Klee A, Martino S, et al. Training peer specialists with mental illness in motivational interviewing: A pilot study. Psychiatr Rehabil J. 2017;40(4):354–360. [DOI] [PubMed] [Google Scholar]
- [50].Meyers D, Durlak J, Wandersman A. The quality implementation framework: A synthesis of critical steps in the implementation process. Am J Community Psychol. 2012;50(3–4):462–480. [DOI] [PubMed] [Google Scholar]
- [51].Ager RD, Roahen-Harrison S, Toriello PJ, et al. A study on the effectiveness of a brief motivational enhancement therapy training. J Addict Dis. 2005;24(Suppl 1):15–31. [Google Scholar]


