Abstract
Physician assistants (PAs) are expanding their role in academic emergency departments (EDs). There are no published models for how to integrate PAs into departmental educational activities, scholarship, and operations outside of a PA residency approach. We created a professional development program for PAs that would provide them with opportunities to integrate into all aspects of our department mission and provide them with a forum for personal growth and ongoing education. The program provides PAs with resources including protected time and mentorship to become a content expert in an academic area of interest. We review our 5‐year experience creating and implementing this program, which has grown from six PAs in 2013 to 24 PAs in 2018. These PAs now have formal roles in five of our eight divisions, participating in education, administrative, and research activities. The retention rate for PAs in this program is 90.2% versus 85.7% for PAs at our department who are not in the program. Our experience and results demonstrate the value of investing in the professional development and continued education of PAs at an academic ED versus the traditional model of service and the potential for integration into all aspects of an academic ED's mission.
Background
Physician assistants (PAs) have expanded their presence in emergency departments (EDs) at academic medical centers (AMCs) in parallel with increasing ED visits nationally.1 Most AMCs now employ PAs and almost two‐thirds utilize PAs in the ED.2 Evolving payment models, a decline in government funding for research and education, and a national physician shortage are some of the leading factors cited as contributing to this change.
Physician assistants as a group currently care for more than 50% of ED patients at our hospital and have become natural stakeholders in departmental scholarship, committees, and operations. Other AMCs report that PAs could play an important role in these activities.1 We suspected that integrating them into the departmental mission may improve ED efficiency, as well as job satisfaction and intention to leave practice, but to our knowledge, there are no published models for how to integrate PAs into these endeavors.3 To address our department need and gap in the literature, we created a professional development program named the PA‐II Program and describe its objectives, development, implementation, and outcomes.
Objectives of Innovation
The primary objectives of this innovation were threefold: 1) to develop a program for PAs to integrate into department operations, 2) to provide a forum for PAs to pursue professional development and personal growth, and 3) to enhance ongoing PA education. A secondary aim was to provide an incentive to help with PA retention.
Development Process
Job enrichment theory framed our design of a professional development program for PAs. This theory states that increasing the variety, autonomy, and complexity of one's work may improve job satisfaction and reduce burnout.4 Further, investing in professional growth on an individual level may improve the organization as a whole and its environment for PAs.4, 5 PA leadership defined the logistics of the program. Funding comes from our department in recognition of its commitment to PA professional development and investment in retention.
In brief, PAs who have worked for 3 years in the ED are eligible to become a PA II, which is considered a promotion and comes with a salary increase and 10 hours (0.0625 FTE) of protected and paid time each month to pursue an academic or scholarly activity. PAs submit a formal proposal (Data Supplement S1, available as supporting information in the online version of this paper, which is available at http://onlinelibrary.wiley.com/doi/10.1002/aet2.10382/full) outlining a potential role; its responsibilities; and how it may impact the group, department, or hospital. PA leadership supports them in this process by helping PAs explore their outside interests, identify a mentor, and identify existing or new opportunities within the department.
Implementation
A designated PA II director meets with individual PA IIs every 6 months to review progress and identify opportunities for expanding their project. The PA II director is a senior PA who has been with the department for more than 9 years and has approximately 0.1 FTE per month of protected and paid time to perform this role. PA leadership meets monthly for 1 hour with the PA II director to provide support, review PA II progress, and identify any barriers to a PA II's professional growth within the program.
In addition to PA leadership, designated faculty within our department are natural mentors for PA IIs and provide support through existing structures. For example, a PA II with interest in disaster medicine participates in monthly meetings with faculty from the MGH Center for Disaster Medicine and collaborates with them on biothreats and hazardous materials trainings. These faculty provide feedback to the PA II and PA leadership on the PA II's contributions to their group and progress in developing expertise.
Adoption of an innovation is most likely to succeed when there is a process for participants to create and share information.6 Therefore, we have imbedded forums for sharing this information so that the entire group may benefit from the individual's added expertise. For example, PA IIs with focus on ultrasound and simulation share their knowledge with rotating PA students, new hires, and PAs orienting to our critical care pod. Other PA II's have positions on department‐based interdisciplinary teams that develop strategies to improve the health care for our homeless population and disseminate information about these initiatives to providers in the department.
We document the number and proportion of PA II's in the PA group as part of surveillance of the program. We share PA and PA II retention rates before and after implementing the program as a potential measure of success of the PA II program and a surrogate for PA job satisfaction.
Outcomes
The program has expanded from six PA II's (25% of the group) in 2013, the first year of implementation, to 24 PA II's (68%) by 2018. There are now 14 unique PA II roles within six of eight departmental divisions. Example roles include simulation and ultrasound education, departmental quality and patient safety, and wilderness medicine. More recently PA IIs have explored interdepartmental roles in palliative care and pharmacology (see Data Supplement S2, available as supporting information in the online version of this paper, which is available at http://onlinelibrary.wiley.com/doi/10.1002/aet2.10382/full, for a full list.)
We have measured the annual retention rate for the PAs in our department since the PAs started in our department in 2010. Annual retention rate is presented as a percent and equal to one minus the ratio of PAs whose employment with our department ended during a given year relative to the total number of PAs on staff in the department at the end of that same year. The average retention rate for all PAs before the PA II program (2010–2012) was 87.3%, approximately the same as the average retention rate since starting the PA II program (2013–2018, 87.5%). However, the retention rate for PA IIs was higher than PAs not in the program (PA Is) in every year except 2017 (Figure 1). The average retention rate for PA IIs is 90.2% compared with 85.7% for PA Is.
Figure 1.
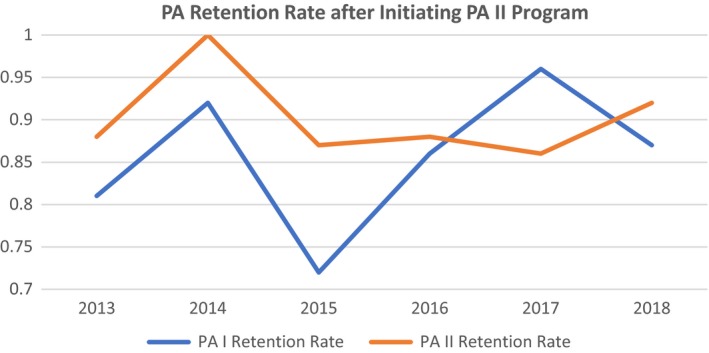
PA retention rate after initiating PA II program. PA = physician assistant.
Discussion
We have developed a formal program for PAs at an academic ED to pursue professional development in line with the AMC's mission of academic growth for the betterment of the individual and the organization. As PA groups expand and assume a larger presence within the health care system, it will be important to provide opportunities for professional growth and promotion. Although the participants in our program are PAs in an academic ED, we believe that this model could easily be applied to advanced practice providers (APPs) in other specialties.
Academic EDs are uniquely positioned to integrate PAs into the nonclinical activities of the department. We have found that existing resources, such as division faculty, ongoing research projects, and department committees, are eager to integrate PAs into their teams. This meets our first two objectives to integrate PAs into department operations and create forums for personal growth. Our third objective, to enhance PA education, is met by supporting PAs in developing roles dedicated to teaching, quality improvement, and clinical care, as well as dissemination of information. PAs in these roles not only teach their PA colleagues, but also collaborate as part of interprofessional teams in education initiatives within the department. These collaborations align with our hospital mission with regard to continued learning and have the potential to secure publication and grant funding.
As the PA II program expands, one of our primary challenges is maintaining surveillance of the program. Some projects and content areas are more amenable to a PA II position as they are already contained within an existing division or committee. However, some PAs have had interests in topics without a preexisting organized structure within our department. We view this as an opportunity to create interprofessional partnerships, and in these instances, we try to pair the PAs with faculty who have shared professional interests.
Finally, the annual retention rate for the MGH ED PA program is approximately the same since beginning the PA II program. However, the retention rate for PA IIs is greater than PA Is in every year except for one (2017). This suggests that the opportunities for professional development provided by our program may increase our ability to keep experienced PAs working in our academic ED for a longer period. Further, retention rate does not account for new hires (PA Is), which limits our ability to discern whether the PA II program motivates PA Is to continue employment. However, our turnover rate for PAIIs (9.8%) is less than the most recently reported national benchmark (14.2% in 2018).7 Together these data suggest efficacy of the PA II program.
In summary, the PA II program is a novel professional development program and promotional pathway for PAs at an AMC. It harnesses their individual academic and clinical interests in ways that improve personal accomplishment and we provide channels for PAs to share their growing expertise with their peers and the rest of the department. Our data suggest that this may improve job satisfaction and help reduce expensive workforce turnover. We believe that this ultimately contributes to group cohesion and a shared experience for the team outside of the traditional model of service for APPs.
Supporting information
Data Supplement S1. MGH Department of Emergency Medicine PAII Application.
Data Supplement S2. PA II Roles & Responsibilities.
AEM Education and Training 2020;4:154–157.
The authors have no relevant financial information or potential conflicts to disclose.
References
- 1. National Commission on Certification of Physician Assistants, Inc. 2016 Statistical Profile of Certified Physician Assistants: An Annual Report of the National Commission on Certification of Physician Assistants. Available at: http://www.nccpa.net/research. Accessed December 1, 2018.
- 2. Moote M, Krsek C, Kleinpell R, Todd B. Physician assistant and nurse practitioner utilization in academic medical centers. Am J Med Qual 2011;26:452–60. [DOI] [PubMed] [Google Scholar]
- 3. Linzer M, Sinsky CA, Poplau S, Brown R, Williams E; Healthy Workplace Investigators . Joy in medical practice: clinician satisfaction in the Healthy Work Place Trial. Health Aff (Millwood) 2017;36:1808–14. [DOI] [PubMed] [Google Scholar]
- 4. Hoff T, Carabetta S, Collinson GE. Satisfaction, burnout, and turnover among nurse practitioners and physician assistants: a review of the empirical literature. Med Care Res Rev 2019;76:3–31. [DOI] [PubMed] [Google Scholar]
- 5. Jolly B. Faculty development for organizational change In: Steinert Y. Faculty Development in the Health Professions. Innovation and Change in Professional Education. Vol 11 Dordrecht: Springer, 2014. p. 119–137. [Google Scholar]
- 6. Sahin I. Detailed review of Rogers’ diffusion of innovations theory and educational technology‐related studies based on Rogers’ theory. TOJET 2006;5:14–23. [Google Scholar]
- 7. 2018 National Health Care Retention and RN Staffing Report. Available at: https://business.dailypay.com/blog/employee-turnover-rates-in-the-healthcare-industry. Accessed March 15, 2019.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Supplement S1. MGH Department of Emergency Medicine PAII Application.
Data Supplement S2. PA II Roles & Responsibilities.


