Abstract
Background:
Atypical knee joint biomechanics after anterior cruciate ligament reconstruction (ACLR) are common. It is, however, unclear whether knee robustness (ability to tolerate perturbation and maintain joint configuration) and whole body movement strategies are compromised after ACLR.
Purpose:
To investigate landing control after ACLR with regard to dynamic knee robustness and whole body movement strategies during sports-mimicking side hops, and to evaluate functional performance of hop tests and knee strength.
Study Design:
Controlled laboratory study.
Methods:
An 8-camera motion capture system and 2 synchronized force plates were used to calculate joint angles and moments during standardized rebound side-hop landings performed by 32 individuals with an ACL-reconstructed knee (ACLR group; median, 16.0 months after reconstruction with hamstring tendon graft [interquartile range, 35.2 months]) and 32 matched asymptomatic controls (CTRL). Dynamic knee robustness was quantified using a finite helical axis approach, providing discrete values quantifying divergence of knee joint movements from flexion-extension (higher relative frontal and/or transverse plane motion equaled lower robustness) during momentary helical rotation intervals of 10°. Multivariate analyses of movement strategies included trunk, hip, and knee angles at initial contact and during landing and hip and knee peak moments during landing, comparing ACLR and CTRL, as well as legs within groups.
Results:
Knee robustness was lower for the first 10° motion interval after initial contact and then successively stabilized for both groups and legs. When landing with the injured leg, the ACLR group, as compared with the contralateral leg and/or CTRL, demonstrated significantly greater flexion of the trunk, hip, and knee; greater hip flexion moment; less knee flexion moment; and smaller angle but greater moment of knee internal rotation. The ACLR group also had lower but acceptable hop and strength performances (ratios to noninjured leg >90%) except for knee flexion strength (12% deficit).
Conclusion:
Knee robustness was not affected by ACLR during side-hop landings, but alterations in movement strategies were seen for the trunk, hip, and knee, as well as long-term deficits in knee flexion strength.
Clinical Relevance:
Knee robustness is lowest immediately after landing for both the ACLR group and the CTRL and should be targeted in training to reduce knee injury risk. Assessment of movement strategies during side-hop landings after ACLR should consider a whole body approach.
Keywords: biomechanics, kinematics, kinetics, helical axis
Rupture of the anterior cruciate ligament (ACL) is a potentially devastating knee injury, which often results in persistent decreased knee function despite rehabilitation programs up to a year or more.21,39 Treatment with ACL reconstruction (ACLR) is common for athletes,19 with ~80% of recreational athletes returning to sports and only ~50% of athletes returning to competitive-level sports after ACLR.1 The risk of a secondary ACL injury is unfortunately high, with ~23% of athletes <25 years old experiencing either a reinjury of the same ACL or an injury to the contralateral ACL after returning to sports.44 Primary ACL injuries and reinjuries occur in approximately 70% to 80% because of momentarily poor knee control in situations of noncontact or indirect contact,14,30 such as one-leg landing or side-cutting maneuvers with the knee relatively straight, abducted, and rotated.15,16,24,43 Consequently, for a safe return to activities that put considerable loading on the knee joint, individuals with an ACL-reconstructed knee should demonstrate sufficient lower limb control during tasks that involve high-impact side-to-side maneuvers.32,38
The few existing studies that have investigated landing mechanics in those with an ACL-reconstructed knee as compared with controls during such tasks have included small samples (n = 11-13 with an ACL-reconstructed knee), focused mainly on the knee, and found inconclusive results for knee joint angles, either with no differences between groups17,25 or with greater knee abduction for patients with an ACL-reconstructed knee.35 The results are more consistent for knee joint moments, with lower external knee moments in the sagittal plane and greater moments in the frontal and transverse planes for people with an ACL-reconstructed knee.17,25,35 While these findings provide evidence of atypical landing mechanics after ACLR, they do not indicate whether those with an ACL-reconstructed knee have different knee control strategies as compared with asymptomatic controls. This is important to evaluate since poor knee control most likely increases future risk of reinjury to the graft, as well as to the menisci, cartilage, and other knee ligaments.
One reason for the lack of knowledge regarding knee control for individuals with an ACL-reconstructed knee is the general absence of objective measures of knee control. One approach toward such a measure is to relate the inclination of the knee’s finite helical axis (FHA) to the flexion-extension axis of the knee over specific helical rotation intervals. This provides information of how much the knee motion diverges from pure flexion-extension movement for each motion interval, where more relative motion in the frontal and/or transverse planes is considered poor knee control. Thus, it is used to evaluate the knee-specific ability to tolerate perturbation and maintain joint configuration during landing, which defines how robust the knee is.27 Therefore, the FHA approach is used to evaluate dynamic knee robustness in real-life situations because knee frontal and transverse plane motion always occurs simultaneously to some degree and induces strain on the ACL when combined.2,12,23 This method has been applied to show reduced dynamic knee robustness among those with an ACL-reconstructed knee >20 years after injury.10 No study to date has used this approach to investigate if younger patients with an ACL-reconstructed knee display reduced dynamic knee robustness during sports-mimicking situations or if they alter whole body kinematics and/or kinetics to perform such tasks.
We compared landing control between individuals with an ACL-reconstructed knee and asymptomatic controls with regard to dynamic knee robustness and whole body movement strategies during sports-mimicking side hops. Functional performance was compared with outcome measures related to hop and knee strength parameters. Additionally, we compared between legs within groups to assess symmetry for the same outcome measures. We hypothesized that those with an ACL-reconstructed knee would show lower dynamic knee robustness and atypical movement strategies for the injured leg as compared with controls and the contralateral noninjured leg, whereas controls would not show asymmetry between legs.
Methods
Participants
A total of 32 participants with an ACL-reconstructed knee (ACLR group) and 32 age- and sex-matched asymptomatic controls (CTRL group) between 17 and 34 years of age participated. The ACLR group was prospectively and sequentially recruited over a period of ~2 years, mainly from the orthopaedic clinic of the regional hospital and in a few cases from advertisements around the university and hospital campus and from another local sports medicine clinic (Table 1). Inclusion criteria for the ACLR group were as follows: unilateral ACL injury and surgery with a hamstring tendon graft, a return to previous activity level/sports after clearance from physician and/or physiotherapist, and no other musculoskeletal or neurological pathology that might affect one’s ability to perform the hops (also applied to CTRL). CTRL group participants were recruited consecutively from advertisements at the university and hospital campus and by word of mouth. All participants were interviewed regarding inclusion criteria over the phone before participating and again before testing, when they also had a clinical knee examination for screening by an experienced physiotherapist. Minor surgery for the meniscus and minor injury to the medial collateral ligament were allowed, but any complete collateral ligament tear or any major surgical procedure resulted in exclusion. The study was approved by the regional ethical review board, Umeå, Sweden (Dnr 2015/67-31). Before partaking, all participants provided written informed consent in agreement with the Declaration of Helsinki.
Table 1.
Participant Characteristics by Group a
| ACLR | CTRL | |
|---|---|---|
| Age, y, mean (SD) | 24.1 (4.5) | 22.9 (3.1) |
| Male:female, n | 8:24 | 8:24 |
| Months after surgery, median (IQR) | 16.0 (35.2) | — |
| Anthropometric measurements, mean (SD) | ||
| Body height, m | 1.72 (0.08) | 1.71 (0.08) |
| Body mass, kg | 70.3 (10.3) | 66.9 (8.1) |
| Knee laxity I/ND-leg, mm | 9.6 (2.0) b | 6.3 (2.2) |
| Knee laxity NI/D-leg, mm | 7.0 (2.1) | 6.4 (2.2) |
| Patient-reported outcome scales, median (IQR) | ||
| IKDC 2000, % of maximum | 82.8 (15.0) b | 100 (1.1) |
| KOOS, % of maximum | ||
| Symptoms | 82.1 (25.0) b | 100 (7.1) |
| Pain | 91.7 (11.1) b | 100 (2.8) |
| Activities of Daily Living | 100 (1.5) b | 100 (0) |
| Sports/Recreation | 85.0 (20.0) b | 100 (0.0) |
| Quality of Life | 68.8 (25.0) b | 93.8 (12.5) |
| Lysholm score | 86.0 (13.0) b | 100 (4.0) |
| Tegner preinjury score | 9 (1) | — |
| Tegner current score | 7 (2) | 8 (4) |
| IPAQ total score | 3047 (2236) | 3506 (1848) |
ACLR, anterior cruciate ligament reconstruction group; CTRL, asymptomatic controls; IKDC 2000, International Knee Documentation Committee Subjective Knee Form; IQR, interquartile range; IPAQ, International Physical Activity Questionnaire; I/ND, injured (ACLR) / nondominant (CTRL); KOOS, Knee injury and Osteoarthritis Outcome Score; NI/D, noninjured (ACLR) / dominant (CTRL).
Significantly different from CTRL at .01 level.
Test Procedure
All participants were tested at U-motion laboratory, Umeå, Sweden. Participants first completed the following questionnaires and scales: 2000 International Knee Documentation Committee Subjective Knee Form, Knee injury and Osteoarthritis Outcome Score (KOOS) subscales, Lysholm scale, Tegner Activity Scale, and International Physical Activity Questionnaire. The knee was then clinically examined, and knee laxity was assessed with a KT-1000 arthrometer (Medmetric Corporation) with a 30-lb (13.5-kg) load of anterior pull force. To assess overall performance level, 3 hop tests were performed in the following order: one-leg hop for distance (OLHD), one-leg vertical hop (OLVH), and the standardized rebound side hop (SRSH),20 with the last evaluated for landing mechanics. The OLHD and OLVH were performed with participants initially standing upright on the testing leg before hopping forward or upward, respectively, as far as possible and landing on the same leg. The SRSH is a recently developed hop test particularly suited for kinematic and kinetic evaluation.20 In short, participants hopped on 1 leg to the side (laterally with respect to the hopping leg) over a distance of 25% of body height, followed by an immediate rebound back to the starting position for the same leg. All hop tests were performed barefoot on force plates (masked by modular walkway elements) while holding a 25-cm short rope (with knots) with both hands behind the back to emphasize lower limb control and to avoid obstructing the markers. One or 2 practice trials were allowed for familiarization of each test. Participants performed 3 to 5 trials per leg for the OLHD and OLVH to obtain maximal hop performances, while 10 trials were performed for the SRSH. Trials were deemed successful if the following criteria were fulfilled: a minimum 3-second single-leg stance after landing without releasing the rope, no contact of the contralateral foot with the floor, and no moving of the ipsilateral foot to maintain balance, all in analogy with those of previous studies.13,20,22,28,34,35 The ACLR group started on the noninjured leg, and the CTRL group started on the dominant leg (preferred leg for kicking a ball). They alternated between legs every trial to reduce fatigue. Participants had ~5 seconds of rest between trials and ~5 minutes of rest between tests. The biomechanical analyses focused on the landing phase after the lateral hop of the SRSH, defined from initial contact (IC; vertical force >20 N) until peak knee flexion.
Finally, maximal isometric knee extension and flexion strength were assessed with a dynamometer (Kinetic Communicator 125 Auto Positioning; Chattecx Corp). Participants were seated with a trunk angle of 78°, a seat angle of 10°, and the knee at ~65° (0° defined by the lever arm in a horizontal position), as recommended by the manufacturer. Straps were secured over the hips, both shoulders (crossed), and the thigh being tested. The axis of the dynamometer was aligned with the lateral femoral epicondyle, and the lowest part of the resistance pad was placed ~10 mm proximal to the medial malleolus. After 2 submaximal warm-up contractions of 2 seconds each, 3 maximal 5-second trials were performed, with a 5-second rest between repetitions. The noninjured leg for the ACLR group and the dominant leg for the CTRL group were tested first for knee extension strength, followed by knee flexion strength.
Missing Data
Data were lacking for 1 participant in each group (ACLR and CTRL) for KT-1000, questionnaires, and strength; 1 participant among the CTRL group lacked data for KT-1000 and strength; and 1 participant in each group (ACLR and CTRL) lacked data for KT-1000—all attributed to mixed technical and logistical circumstances not related to functional performance. Kinematic and kinetic data were obtained and used for all individuals.
Data Collection
Movements were registered at 240 Hz with an 8-camera motion capture system (Oqus 300; Qualisys AB). Ground-reaction forces were recorded at 1200 Hz with 2 force plates (model 9260AA; Kistler Instrument AG), which were time synchronized with the motion capture system. A 6 degrees of freedom model was constructed from 56 passive spherical markers attached with double-coated adhesive tape on the skin at anatomic landmarks, as previously described in detail.20 Participants wore rigid clusters on their thighs to improve construct validity by reducing effects of soft tissue artifacts.7 A functional joint method was used to define hip joint centers from hip circumduction movement with the pelvis as reference.31 Marker placements on femoral epicondyles and malleoli were used to define knee and ankle joint centers, respectively, during a stationary recording in standing. The same test leader (J.L.M.) applied markers and instructed all participants. The dynamometer data were recorded at 1500 Hz after application of a zero baseline correction for each participant’s leg weight.
Data Processing
The software Qualisys Track Manager (v 2.2; Qualisys AB) and Visual3D (v 5.02.19; C-Motion Inc) were used for data processing and calculation. Hip and knee joint moments, normalized to body mass, were calculated with inverse dynamics and presented as external moments (eg, an external abduction moment would tend to abduct the knee). Angle and moment data were filtered with a fourth-order bidirectional low-pass Butterworth digital filter with a cutoff frequency of 15 Hz. The Cardan rotation sequence XYZ was used (X, mediolateral axis; Y, anteroposterior axis; Z, longitudinal axis).6 Trunk angles were defined relative to the vertical axis of the laboratory coordinate system and hip and knee joint angles from movement of the distal segment relative to the proximal.
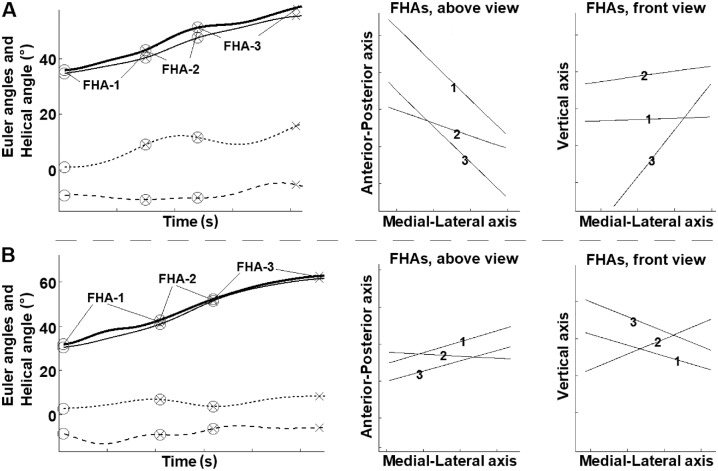
Dynamic knee robustness was evaluated by calculating discrete FHA inclination angles (0°-90°) of the knee helical axis relative to the knee flexion-extension axis for consecutive helical rotation intervals of 10° (from IC) over the landing phase. This computes how much the knee motion differed from a pure flexion-extension movement over each motion interval, regardless of whether this difference resulted from adduction/abduction and/or internal/external rotation.9,10 A greater inclination angle thus indicates lower dynamic knee robustness attributed to more motion in the frontal and/or transverse plane. The 10° interval was set to be small enough to capture motion changes over short time intervals but still to be within acceptable error levels based on error simulations. Figure 1 presents an example of 2 participants displaying high and low FHA inclination angles. Given that ACL injury mechanics mainly occur early after impact,15,16 the first FHA inclination angle was considered the most important to investigate and was evaluated for reliability (between trials within groups) with an intraclass correlation model(3,5). Excellent reliability was shown for both groups, with coefficients of 0.83 to 0.84.
Figure 1.
Example of a hop landing trial from 2 participants who demonstrated (A) high and (B) low finite helical axis (FHA) inclination angles. Displayed on the left are the knee motion curves during the landing (from initial contact to peak knee flexion), where the thick solid line is the helical axis rotation angle, the thin solid line is the flexion/extension angle, the dotted line is the adduction/abduction angle, and the dashed line is the internal/external rotation angle. The rings indicate the start of the knee helical motion for a new FHA, and crosses indicate when 10° of helical rotation has occurred, which generates the discrete FHA inclination angles. Greater motion in the knee frontal and/or transverse planes relative to the sagittal plane generates greater FHA inclination angles, which indicate poorer knee robustness. For visualization, in the middle are the FHAs as shown from above, where greater motion in the frontal relative to the sagittal plane results in FHAs directed more along the anterior-posterior axis. To the right are the FHAs as shown from the front, where greater motion in the transverse relative to the sagittal plane results in FHAs directed more along the vertical axis. The individual in panel A displayed FHA inclination angles of 57.8° for FHA-1, 20.7° for FHA-2, and 43.9° for FHA-3, while the individual in B displayed FHA inclination angles of 22.7° for FHA-1, 22.7° for FHA-2, and 26.0° for FHA-3.
Movement strategies were analyzed with the following discrete variables during the landing phase: angles at IC of the trunk in the sagittal and frontal planes; joint angles at IC of the hip and knee in the sagittal, frontal, and transverse planes; peak angles of trunk flexion and lateral bending; and peak angles and moments of hip flexion, hip adduction, hip internal rotation, knee flexion, knee abduction, and knee internal rotation. Excellent trial-to-trial and excellent to good test-retest reliability were recently reported for the variables of this test.20
Functional performances of all 3 hop tests were evaluated. Hop distance in OLHD was calculated from the displacement of a marker on the foot between starting position and landing, while hop height in OLVH was calculated from the displacement of the pelvis center of mass between standing and peak height. The highest peak values for distance and height from successful trials were used in the analyses. For the SRSH, the number of completed trials (out of 10), the contact time (defined from IC to next takeoff where vertical force <20 N), and the peak vertical force (normalized to weight) during landing were evaluated. Knee strength data from the dynamometer were filtered with a moving average of 60 ms, with the highest peak value from the trials normalized to body mass and used in analyses.
Statistical Analysis
The injured leg of the ACLR group was compared with the nondominant leg of the CTRL group for all between-group analyses. Mean values of FHA inclination angles and their time events from IC, as well as angles and moments, were calculated from the first 5 successful trials in SRSH. Consecutive FHAs were numbered FHA-1, FHA-2, FHA-3, and so on, with each representing a knee helical rotation interval of 10°. Given that knee motion may vary between trials for an individual, a different number of FHAs may be calculated. Therefore, at least 3 of the 5 trials had to generate a specific FHA (eg, FHA-3) to be considered representative of that individual’s knee motion and included in analyses. FHA inclination angles and their time of occurrence were compared between groups with independent t tests because data were normally distributed (Shapiro-Wilk test). Four separate multivariate analyses of variance (MANOVAs) were performed and compared between groups, including different sets of variables: angles at IC (trunk, hip, knee), peak angles during landing (trunk, hip, knee), peak moments during landing (hip, knee), and functional performance outcomes (hop and strength) (Table 2). Significant MANOVAs were further investigated with discriminant analysis, with values ≥0.32 interpreted as meaningful to group differences.37 Asymmetries within groups for the same blocks of variables were investigated with repeated-measures MANOVAs and, if significant, followed by Bonferroni post hoc tests. Partial eta-squared values as effect sizes (ESs; 0.01 = small, 0.1 = medium, 0.25 = large)41 were presented for main effects. Participant characteristics were analyzed with t tests, and questionnaires were analyzed with Mann-Whitney U tests. SPSS (v 23; IBM) was used with a 5% level for statistical significance set a priori.
Table 2.
Four Blocks of Variables Analyzed With MANOVAs Between Groups and Repeated-Measures MANOVAs Between Legs Within Groups a
| Angles at initial contact (8 variables) | Trunk in (1) sagittal and (2) frontal planes |
| Hip in (3) sagittal, (4) frontal, and (5) transverse planes | |
| Knee in (6) sagittal, (7) frontal, and (8) transverse planes | |
| Peak angles during landing (8 variables) | Trunk (1) flexion and (2) lateral bending |
| Hip (3) flexion, (4) adduction, and (5) internal rotation | |
| Knee (6) flexion, (7) abduction, and (8) internal rotation | |
| Peak moments during landing (6 variables) | Hip (1) flexion, (2) adduction, and (3) internal rotation |
| Knee (4) flexion, (5) abduction, and (6) internal rotation | |
| Functional performance outcomes (7 variables) | Maximal (1) OLHD and (2) OLVH performances |
| SRSH (3) successful hops, (4) contact time, and (5) peak vGRF | |
| Peak isometric knee (6) extensor and (7) flexor torque |
MANOVA, multivariate analysis of variance; OLHD, one-leg hop for distance; OLVH, one-leg vertical hop; SRSH, standardized rebound side hop; vGRF, vertical ground-reaction force.
Results
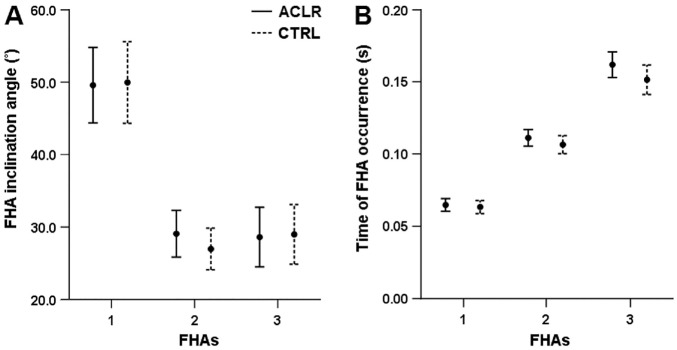
Participants in both groups had a similar range of knee motion, which provided an equal amount of FHAs (mean ± SD: 3.2 ± 0.9, ACLR; 3.5 ± 0.9, CTRL; P = .175). The number of participants who provided FHA-1, FHA-2, FHA-3, FHA-4, and FHA-5 occurrences were 31, 31, 24, 10, and 2, respectively, for the ACLR group (ie, 24 participants had 3 helical axis motion intervals to provide FHA-3) and 32, 32, 28, 14, and 5 for CTRL. One individual in the ACLR group had <10° of helical knee motion for 4 of the 5 trials (thus, no FHA for analysis). Further analyses of FHA inclination angles and their time of occurrence were therefore restricted to FHA-1 to FHA-3. These showed no differences between groups (P≥ .128) or between legs within groups (P≥ .060). The inclination angle was highest for FHA-1 and then successively stabilized (displayed with their times of occurrences in Figure 2).
Figure 2.
FHA (A) inclination angles and (B) times of occurrence presented in mean values (circles) and 95% CIs, with ACLR represented by solid lines and CTRL represented by dashed lines. Each FHA inclination angle represents a knee helical motion of ~10°. ACLR, anterior cruciate reconstruction group; CTRL, asymptomatic controls; FHA, finite helical axis.
Regarding movement strategies, a MANOVA revealed a significant main difference between groups for angles at IC (P = .005; ES = .32 [large]). Discriminant analysis showed that the ACLR group displayed greater hip and knee joint flexion angles at IC than the CTRL group (16% and 24% greater, respectively). A significant main difference between groups for peak angles during landing was also found (P = .002; ES = .35 [large]), where the ACLR group displayed greater peak knee flexion (6%) and less knee internal rotation (actually, 2.4° more external rotation). A significant main difference between groups for external peak moments during landing was also displayed (P = .015; ES = .23 [medium]), where the ACLR group demonstrated greater peak moments than the CTRL group for hip flexion (10% greater), knee flexion (7% greater), and knee internal rotation (30% greater) (Table 3).
Table 3.
Group Comparisons for Joint Angles and External Moments a
| ACLR | CTRL | ACLR-CTRL | |||||||
|---|---|---|---|---|---|---|---|---|---|
| I-Leg | NI-Leg | P Value: Main Effect | P Value: Post Hoc | ND-Leg | D-Leg | P Value: Main Effect | P Value: Main Effect | DISCRIM b | |
| Angles at IC, deg | .024 | .431 | .005 | ||||||
| Trunk flexion (+) | 18.4 (4.3) | 17.1 (4.8) | .029 | 16.4 (6.2) | 16.7 (5.5) | ||||
| Trunk lateral bending (–) | −7.6 (4.0) | −8.8 (3.0) | .202 | −7.1 (2.5) | −7.0 (3.1) | ||||
| Hip flexion (+) | 40.3 (7.8) | 37.8 (9.1) | .004 | 34.7 (7.6) | 34.2 (7.3) | −0.54 | |||
| Hip adduction (+) | −11.4 (4.8) | −12.4 (4.9) | .276 | −11.1 (5.1) | −11.0 (3.5) | ||||
| Hip internal rotation (+) | 4.2 (5.1) | 3.2 (5.4) | .351 | 3.8 (8.8) | 5.8 (6.9) | ||||
| Knee flexion (+) | 37.2 (6.2) | 36.5 (7.2) | .443 | 30.0 (6.6) | 30.1 (6.4) | −0.85 | |||
| Knee abduction (–) | −2.6 (5.0) | −2.6 (5.3) | .969 | −2.3 (5.7) | −1.6 (5.0) | ||||
| Knee internal rotation (+) | −10.7 (5.0) | −9.6 (5.0) | .330 | −9.8 (6.8) | −11.6 (5.8) | ||||
| Peak angles, deg | .015 | .281 | .002 | ||||||
| Trunk flexion (+) | 22.2 (5.3) | 20.8 (5.7) | .041 | 21.1 (8.9) | 21.7 (7.7) | ||||
| Trunk lateral bending (–) | −9.2 (4.4) | −9.7 (3.3) | .579 | −7.9 (2.5) | −7.8 (3.4) | ||||
| Hip flexion (+) | 49.1 (9.0) | 45.9 (9.1) | .006 | 45.4 (9.0) | 45.3 (9.0) | ||||
| Hip adduction (+) | −3.0 (7.0) | −5.0 (6.8) | .098 | −0.7 (6.8) | −0.2 (6.2) | ||||
| Hip internal rotation (+) | 10.7 (5.3) | 9.4 (5.7) | .203 | 10.8 (7.6) | 12.7 (5.5) | ||||
| Knee flexion (+) | 63.0 (6.8) | 62.9 (6.8) | .861 | 59.4 (7.2) | 59.9 (7.7) | −0.36 | |||
| Knee abduction (–) | −3.2 (5.0) | −2.9 (5.1) | .678 | −3.0 (5.6) | −1.9 (5.0) | ||||
| Knee internal rotation (+) | −3.2 (4.3) | −1.8 (5.3) | .102 | −0.8 (5.0) | −2.9 (4.1) | 0.35 | |||
| Peak moments, N·m/kg | .035 | .896 | .015 | ||||||
| Hip flexion (+) | 1.26 (0.31) | 1.19 (0.27) | .117 | 1.15 (0.30) | 1.12 (0.25) | 0.33 | |||
| Hip adduction (+) | 2.00 (0.34) | 2.09 (0.40) | .238 | 2.02 (0.49) | 2.01 (0.49) | ||||
| Hip internal rotation (+) | 0.83 (0.22) | 0.80 (0.26) | .240 | 0.78 (0.21) | 0.76 (0.23) | ||||
| Knee flexion (+) | 2.62 (0.50) | 2.82 (0.50) | .001 | 2.44 (0.55) | 2.40 (0.61) | 0.32 | |||
| Knee abduction (–) | −0.16 (0.08) | −0.16 (0.06) | .454 | −0.17 (0.07) | −0.18 (0.06) | ||||
| Knee internal rotation (+) | 0.13 (0.06) | 0.12 (0.05) | .338 | 0.10 (0.04) | 0.10 (0.03) | 0.54 | |||
Values are presented as mean (SD). Bold P values indicate a significant multivariate main effect or significant univariate effect (Bonferroni post hoc) at the .05 level. ACLR, anterior cruciate ligament reconstruction group; CTRL, asymptomatic control group; D-leg, dominant leg; I-leg, injured leg; IC, initial contact; ND-leg, nondominant leg; NI-leg, noninjured leg.
DISCRIM (discriminant analysis): post hoc analysis of a significant multivariate analysis of variance presents correlations between discriminating variables and standardized canonical discriminating functions. These vary between 1 and –1 and are presented only if ≥0.32 (absolute value).
Repeated-measures MANOVAs further displayed significant main differences between legs indicating asymmetry for the ACLR group for angles at IC (P = .024; ES = .48 [large]), peak angles during landing (P = .015; ES = .51 [large]), and peak moments during landing (P = .035; ES = .39 [large]). When landing with the injured leg, the ACLR group had, relative to the noninjured leg, a combination of larger angles of trunk and hip flexion at IC (8% and 7% greater, respectively) and during the landing phase (7% greater for both) and less knee flexion moment (7% less) during the landing phase (Table 3).
Concerning functional performances, a significant main difference between groups was found (P = .041; ES = .24 [medium]), although attributed only to shorter contact time in SRSH for ACLR (Table 4). A significant main difference between legs for the ACLR group was found (P = .001; ES = .60 [large]) but not for the CTRL group. The injured leg, relative to the noninjured leg, displayed significantly lower OLVH maximal height (8% less; P = .003), longer contact time in landing (5% longer; P = .020), lower peak vertical force (4% less; P = .002), and lower peak knee extensor strength (4% deficit; P = .040) and flexor strength (12% deficit; P < .001).
Table 4.
Functional Performance Outcomes of the Groups a
| ACLR | CTRL | |||
|---|---|---|---|---|
| I-Leg | NI-Leg | ND-Leg | D-Leg | |
| Maximal | ||||
| OLHD, m | 1.26 (0.18) | 1.28 (0.19) | 1.26 (0.23) | 1.29 (0.22) |
| OLVH, m | 0.22 (0.04) b | 0.24 (0.03) | 0.24 (0.04) | 0.25 (0.04) |
| SRSH | ||||
| Successful hops, out of 10 | 8.3 (1.2) | 8.1 (1.6) | 8.5 (1.7) | 8.9 (1.4) |
| Contact time, s | 0.45 (0.13) c , d | 0.43 (0.13) | 0.55 (0.26) | 0.54 (0.25) |
| Peak | ||||
| vGRF, ratio | 2.23 (0.21) b | 2.33 (0.24) | 2.30 (0.34) | 2.27 (0.28) |
| Knee extensor torque, N·m/kg | 2.57 (0.52) c | 2.67 (0.49) | 2.44 (0.48) | 2.54 (0.54) |
| Knee flexor torque, N·m/kg | 1.05 (0.23) b | 1.19 (0.24) | 1.10 (0.23) | 1.13 (0.22) |
Data are presented as mean (SD). ACLR, anterior cruciate ligament reconstruction group; CTRL, asymptomatic controls; D-leg, dominant leg; I-leg, injured leg; ND-leg, nondominant leg; NI-leg, noninjured leg; OLHD, one-leg hop for distance; OLVH, one-leg vertical hop; SRSH, standardized rebound side hop; vGRF, vertical ground reaction force.
Significant difference compared with the NI-leg with Bonferroni post hoc at the .01 level.
Significant difference compared with the NI-leg with Bonferroni post hoc at the .05 level.
Discriminated from CTRL with discriminant analysis.
Discussion
Our main findings were that the ACLR group had similar dynamic knee robustness but displayed atypical movement strategies for trunk, hip, and knee joints in preparation for and during landing after a side hop on the injured leg when compared with the CTRL group and the noninjured leg. This was observed at a median of 16.0 months (interquartile range, 35.2) after ACLR and despite the group displaying what is considered clinically acceptable functional performances (Table 4). The strategies included larger trunk, hip, and knee flexion angles, as well as an avoidance of knee internal rotation angle and less external knee flexion moment (Table 3). It also needs to be highlighted that neither of the groups maintained dynamic knee robustness early after landing, which is the most clinically important time point in relation to knee injury risk (Figure 2).
Individuals with ACL injuries who aim to return to sports, independent of ACLR, are commonly clinically evaluated on the basis of symmetry comparisons between their injured and noninjured legs in functional task performances.39 Such an approach is most likely not sensitive enough and further implies a risk of overestimating the function of the injured leg because of decreased neuromuscular function of the noninjured leg after injury.21 On a group level, the ACLR group had acceptable symmetry levels of knee extensor strength and hop performances according to existing criteria for return to pivoting, contact, and competitive sports (~100% strength, >90% hop performances).39 Only the knee flexor strength showed a deficit below these criteria (–12%), which is probably related to ACLR with hamstring grafts. The generally similar results in dynamic knee robustness and functional performances between groups and between legs within groups did not match the lower clinical scores of self-estimated knee joint function and health for the ACLR group (see Table 1). The lack of differences between groups in dynamic knee robustness was unexpected because such outcomes have discriminated patients with a history of ACL injury in the long term (>20 years) from asymptomatic controls,10 although there is a lack of data for younger patients. The FHA analyses did, however, demonstrate surprisingly low knee robustness for both groups early after landing, with higher mean values for FHA-1 (~50°) as compared with FHA-2 and FHA-3 (~27°-29°). This shows that greater knee motion occurred in the frontal and/or transverse planes relative to the sagittal plane during the first 10° of knee helical motion, which then stabilized (Figure 2). These findings are in accordance with evidence that ACL injuries usually occur early after impact,15,16,24,43 since knee frontal and transverse plane motion (specifically knee abduction and internal rotation) is considered a prerequisite for ACL strain and injury.2,12,23 As such, it seems that knee robustness is difficult to maintain when it is most important in relation to ACL injury risk. Efforts to maintain dynamic knee robustness immediately from initial contact by improving landing technique may therefore help to decrease the risk of knee injury among sports people with or without ACL injury.
Only a handful of studies have investigated kinematics and kinetics for patients with an ACL-reconstructed knee during mediolateral change-of-direction maneuvers, where ACL injuries often occur.15,16,24,43 Studies have analyzed either the side hop (10 consecutive hops across a distance of 30 cm with arms free)25 or side cutting with different cutting angles.13,17,29,35 Results showed that those with an ACL-reconstructed knee demonstrated lower peak knee flexion and abduction moments (but similar joint angles)25; greater knee abduction angles and moments35; greater knee adduction and external rotation moment17; fewer peak knee flexion angles, range of motion, and moment29; and greater asymmetry in hip abduction moment for a short period (0%-5% of landing) immediately after initial contact.13 Our results of ACLR displayed different angles at IC with regard to greater trunk and hip flexion (injured versus noninjured leg) and greater hip and knee flexion (versus the CTRL group) and indicated a different feed-forward motor scheme to manage the expected mechanical loading at landing. These movement adaptations result in a smaller patellar tendon insertion angle and greater hamstrings insertion angle, as well as less peak vertical force and anterior tibial shear force, as well as fewer tibiofemoral peak compression forces—all considered to decrease ACL strain.3,4,33,40 Greater trunk and hip flexion angles further positioned the ground-reaction force vector more anteriorly under the foot and to the knee, which resulted in greater hip joint moment22 and less knee flexion moment.22,34 The greater peak hip flexion moment (versus CTRL) and lower peak knee flexion moment (versus the noninjured leg) of our ACLR group further support the use of adapted movement strategies to decrease knee loading. The longer contact time and lower peak vertical force of the injured leg as compared with the noninjured leg also emphasize a knee-loading avoidance strategy. These strategies may explain the similar values in dynamic knee robustness that the ACLR group displayed for both legs, since less knee loading may keep the joint more robust. Furthermore, the higher avoidance of knee internal rotation angle despite greater moment for our ACLR group (versus CTRL), in relation to the aforementioned findings, provide support of a graft-protective strategy. Indeed, previous research has shown that a pivot-shift avoidance strategy with decreased or completely avoided knee abduction and internal rotation angles poses less strain on the ACL.2,12,23 The lack of differences in knee abduction angles and moments between our ACLR and CTRL groups, in contrast to what has previously been reported,25,29,35 needs further research for clarification.
Our findings of adapted movement strategies to unload the ACL-reconstructed knee corroborate previous research for hop testing, where ACLR transferred load onto nearby joints on the ipsilateral leg during the vertical hop8 or the hop for distance.22,28 Such adaptations indicate an inadequate rehabilitation of neuromuscular knee control for a successful return to sports, particularly in cases where the lower limb joints are exposed to high loads in relation to fast and unpredictable scenarios. These adaptations may in turn be related to the increased risk of reinjuries among patients with an ACL-reconstructed knee, as compared with their noninjured counterparts, that affects either the graft26,44 or the contralateral knee.26,30,44 Regaining movement symmetry and adequate neuromuscular knee control in sports-mimicking maneuvers therefore seems essential during rehabilitation after ACLR. However, it may be noted that the injured and reconstructed legs displayed mechanics similar to desired outcomes during hop landings after preventive neuromuscular training programs among healthy athletes. Common modifications include increased trunk, hip, and knee flexion angles and lower peak knee flexion moments.5,11,18 Neuromuscular training programs have also proved successful in decreasing ACL injury occurrences.36,42 As such, if the aim is to strive for symmetry in these outcomes for individuals with an ACL-reconstructed knee, it may be preferable to modify the landing mechanics of the noninjured leg to closer replicate those of the injured leg rather than vice versa. It should be emphasized that modifications to regain symmetry need to be incorporated with improved sports-specific performances to enable successful return to sports.
This study has methodological strengths and limitations. The knee FHA inclination angle calculation from helical motion intervals of 10° may be considered a strength because the motion planes are interrelated over short knee motion intervals, which is relevant for ACL injury mechanics.2,12,23 Using other criteria to determine intervals to evaluate relative knee motion, such as knee flexion angle or time, results in less control of the total knee motion as the main outcome of interest. We believe that such approaches do not adequately represent dynamic knee robustness. Moreover, the use of skin-attached markers needs consideration since this unavoidably results in soft tissue artifacts that affect angle and moment data. We tried to limit these artifacts by using rigid clusters to increase reliability and precision7 and by standardizing marker placements applied by the same test leader. Our protocol (barefoot performance, arms behind the back) also needs consideration when our results are being compared with findings of previous studies utilizing other protocols. Regarding the ACLR group, all patients had hamstring grafts, which may not allow extrapolation of our results to populations who had ACLR with other grafts. The acceptance of minor concomitant injuries may also have affected movement strategies. Furthermore, the time between ACLR and testing varied but displayed no significant correlations with any of the biomechanical outcomes. Finally, our study methodology is difficult to implement in clinical environments given the need for expert knowledge and equipment, time for data processing and analysis, and associated costs. Nevertheless, the SRSH is easy to administer and is time-efficient, requires minimal space, and allows easy video recording for simple biomechanical analysis.
In conclusion, individuals with ACL-reconstructed knees demonstrated different movement strategies but similar dynamic knee robustness in comparison with the contralateral noninjured leg and asymptomatic controls during landings in single-leg standardized rebound side hops. Atypical kinematics and kinetics of the trunk, hip, and knee joints were seen in preparation for and during landing, despite acceptable functional performances according to current clinical standards. Interestingly, knee robustness was not maintained by individuals with ACL-reconstructed knees or controls immediately after landing, which is the most crucial time point in relation to knee injury risk. Further attention to dynamic knee robustness and to the combined movements of the upper and lower body is necessary to properly evaluate adopted movement strategies in the ambition to decrease the risk of future injuries.
Acknowledgments
The authors are grateful to the participants of this study. They also acknowledge Jonas Selling, MEng, for technical assistance; Eva Tengman, PT, PhD, and Ashokan Arumugam, PT, PhD, for clinical examination of the participants; and Andrew Strong, PhD student, for help with the data collection.
Footnotes
Submitted September 10, 2019; accepted January 27, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: Swedish Scientific Council (Dnr K2014 and Dnr 2016-02763), Young Researcher Awardee to C.K.H. (Dnr 223-514-09), Västerbotten County Council (ALFVLL7002689), Swedish National Centre for Research in Sports (Dnr CIF 2015/11 P2016-0042), and Umeå University School of Sport Science (Dnr IH 5.3-13 2015). AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Ardern CL, Taylor NF, Feller JA, Webster KE. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48(21):1543-1552. [DOI] [PubMed] [Google Scholar]
- 2. Bates NA, Nesbitt RJ, Shearn JT, Myer GD, Hewett TE. Knee abduction affects greater magnitude of change in ACL and MCL strains than matched internal tibial rotation in vitro. Clin Orthop Relat Res. 2017;475(10):2385-2396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Blackburn JT, Padua DA. Influence of trunk flexion on hip and knee joint kinematics during a controlled drop landing. Clin Biomech. 2008;23(3):313-319. [DOI] [PubMed] [Google Scholar]
- 4. Blackburn JT, Padua DA. Sagittal-plane trunk position, landing forces, and quadriceps electromyographic activity. J Athl Train. 2009;44(2):174-179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chappell JD, Limpisvasti O. Effect of a neuromuscular training program on the kinetics and kinematics of jumping tasks. Am J Sports Med. 2008;36(6):1081-1086. [DOI] [PubMed] [Google Scholar]
- 6. Cole GK, Nigg BM, Ronsky JL, Yeadon MR. Application of the joint coordinate system to three-dimensional joint attitude and movement representation: a standardization proposal. J Biomech Eng. 1993;115(4A):344-349. [DOI] [PubMed] [Google Scholar]
- 7. Collins TD, Ghoussayni SN, Ewins DJ, Kent JA. A six degrees-of-freedom marker set for gait analysis: repeatability and comparison with a modified Helen Hayes set. Gait Posture. 2009;30(2):173-180. [DOI] [PubMed] [Google Scholar]
- 8. Ernst GP, Saliba E, Diduch DR, Hurwitz SR, Ball DW. Lower extremity compensations following anterior cruciate ligament reconstruction. Phys Ther. 2000;80(3):251-260. [PubMed] [Google Scholar]
- 9. Grip H, Häger C. A new approach to measure functional stability of the knee based on changes in knee axis orientation. J Biomech. 2013;46(5):855-862. [DOI] [PubMed] [Google Scholar]
- 10. Grip H, Tengman E, Häger CK. Dynamic knee stability estimated by finite helical axis methods during functional performance approximately twenty years after anterior cruciate ligament injury. J Biomech. 2015;48(10):1906-1914. [DOI] [PubMed] [Google Scholar]
- 11. Hewett TE, Ford KR, Xu YY, Khoury J, Myer GD. Effectiveness of neuromuscular training based on the neuromuscular risk profile. Am J Sports Med. 2017;45(9):2142-2147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kiapour AM, Demetropoulos CK, Kiapour A, et al. Strain response of the anterior cruciate ligament to uniplanar and multiplanar loads during simulated landings: implications for injury mechanism. Am J Sports Med. 2016;44(8):2087-2096. [DOI] [PubMed] [Google Scholar]
- 13. King E, Richter C, Franklyn-Miller A, Wadey R, Moran R, Strike S. Back to normal symmetry? Biomechanical variables remain more asymmetrical than normal during jump and change-of-direction testing 9 months after anterior cruciate ligament reconstruction. Am J Sports Med. 2019;47(5):1175-1185. [DOI] [PubMed] [Google Scholar]
- 14. Kobayashi H, Kanamura T, Koshida S, et al. Mechanisms of the anterior cruciate ligament injury in sports: a twenty-year clinical research of 1700 athletes. J Sports Sci Med. 2010;9:669-675. [PMC free article] [PubMed] [Google Scholar]
- 15. Koga H, Nakamae A, Shima Y, et al. Mechanisms for noncontact anterior cruciate ligament injuries: knee joint kinematics in 10 injury situations from female team handball and basketball. Am J Sports Med. 2010;38(11):2218-2225. [DOI] [PubMed] [Google Scholar]
- 16. Krosshaug T, Nakamae A, Boden BP, et al. Mechanisms of anterior cruciate ligament injury in basketball: video analysis of 39 cases. Am J Sports Med. 2007;35(3):359-367. [DOI] [PubMed] [Google Scholar]
- 17. Lee SP, Chow JW, Tillman MD. Persons with reconstructed ACL exhibit altered knee mechanics during high-speed maneuvers. Int J Sports Med. 2014;35(6):528-533. [DOI] [PubMed] [Google Scholar]
- 18. Lopes TJA, Simic M, Myer GD, Ford KR, Hewett TE, Pappas E. The effects of injury prevention programs on the biomechanics of landing tasks: a systematic review with meta-analysis. Am J Sports Med. 2018;46(6):1492-1499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lyman S, Koulouvaris P, Sherman S, Do H, Mandl LA, Marx RG. Epidemiology of anterior cruciate ligament reconstruction: trends, readmissions, and subsequent knee surgery. J Bone Joint Surg Am. 2009;91(10):2321-2328. [DOI] [PubMed] [Google Scholar]
- 20. Markström JL, Schelin L, Häger CK. A novel standardised side hop test reliably evaluates landing mechanics for anterior cruciate ligament reconstructed persons and controls [published online December 10, 2018]. Sports Biomech. doi: 10.1080/14763141.2018.1538385 [DOI] [PubMed] [Google Scholar]
- 21. Nawasreh Z, Logerstedt D, Cummer K, Axe MJ, Risberg MA, Snyder-Mackler L. Do patients failing return-to-activity criteria at 6 months after anterior cruciate ligament reconstruction continue demonstrating deficits at 2 years? Am J Sports Med. 2017;45(5):1037-1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Oberländer KD, Brüggemann GP, Höher J, Karamanidis K. Altered landing mechanics in ACL-reconstructed patients. Med Sci Sports Exerc. 2013;45(3):506-513. [DOI] [PubMed] [Google Scholar]
- 23. Oh YK, Lipps DB, Ashton-Miller JA, Wojtys EM. What strains the anterior cruciate ligament during a pivot landing? Am J Sports Med. 2012;40(3):574-583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Olsen O-E, Myklebust G, Engebretsen L, Bahr R. Injury mechanisms for anterior cruciate ligament injuries in team handball: a systematic video analysis. Am J Sports Med. 2004;32(4):1002-1012. [DOI] [PubMed] [Google Scholar]
- 25. Ortiz A, Olson S, Trudelle-Jackson E, Rosario M, Venegas HL. Landing mechanics during side hopping and crossover hopping maneuvers in noninjured women and women with anterior cruciate ligament reconstruction. PM R. 2011;3(1):13-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. Am J Sports Med. 2014;42(7):1567-1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Reeves NP, Narendra KS, Cholewicki J. Spine stability: the six blind men and the elephant. Clin Biomech. 2007;22(3):266-274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Roos PE, Button K, Sparkes V, van Deursen RW. Altered biomechanical strategies and medio-lateral control of the knee represent incomplete recovery of individuals with injury during single leg hop. J Biomech. 2014;47(3):675-680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Saxby DJ, Bryant AL, Modenese L, et al. Tibiofemoral contact forces in the anterior cruciate ligament–reconstructed knee. Med Sci Sports Exerc. 2016;48(11):2195-2206. [DOI] [PubMed] [Google Scholar]
- 30. Schilaty ND, Nagelli C, Bates NA, et al. Incidence of second anterior cruciate ligament tears and identification of associated risk factors from 2001 to 2010 using a geographic database. Orthop J Sports Med. 2017;5(8):2325967117724196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Schwartz MH, Rozumalski A. A new method for estimating joint parameters from motion data. J Biomech. 2005;38(1):107-116. [DOI] [PubMed] [Google Scholar]
- 32. Sell TC, Ferris CM, Abt JP, et al. The effect of direction and reaction on the neuromuscular and biomechanical characteristics of the knee during tasks that simulate the noncontact anterior cruciate ligament injury mechanism. Am J Sports Med. 2006;34(1):43-54. [DOI] [PubMed] [Google Scholar]
- 33. Shimokochi Y, Ambegaonkar JP, Meyer EG, Lee SY, Shultz SJ. Changing sagittal plane body position during single-leg landings influences the risk of non-contact anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc. 2013;21(4):888-897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Shimokochi Y, Yong Lee S, Shultz SJ, Schmitz RJ. The relationships among sagittal-plane lower extremity moments: implications for landing strategy in anterior cruciate ligament injury prevention. J Athl Train. 2009;44(1):33-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Stearns KM, Pollard CD. Abnormal frontal plane knee mechanics during sidestep cutting in female soccer athletes after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2013;41(4):918-923. [DOI] [PubMed] [Google Scholar]
- 36. Sugimoto D, Myer GD, Barber Foss KD, Pepin MJ, Micheli LJ, Hewett TE. Critical components of neuromuscular training to reduce ACL injury risk in female athletes: meta-regression analysis. Br J Sports Med. 2016;50(20):1259-1266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Tabachnick BG, Fidell LS. Using Multivariate Statistics. 6th ed. Harlow, England: Pearson; 2014. [Google Scholar]
- 38. Taylor JB, Ford KR, Nguyen AD, Shultz SJ. Biomechanical comparison of single- and double-leg jump landings in the sagittal and frontal plane. Orthop J Sports Med. 2016;4(6):2325967116655158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Thomeé R, Kaplan Y, Kvist J, et al. Muscle strength and hop performance criteria prior to return to sports after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19(11):1798-1805. [DOI] [PubMed] [Google Scholar]
- 40. Tsai LC, Powers CM. Increased hip and knee flexion during landing decreases tibiofemoral compressive forces in women who have undergone anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41(2):423-429. [DOI] [PubMed] [Google Scholar]
- 41. Vacha-Haase T, Thompson B. How to estimate and interpret various effect sizes. J Couns Psychol. 2004;51(4):473-481. [Google Scholar]
- 42. Walden M, Atroshi I, Magnusson H, Wagner P, Hagglund M. Prevention of acute knee injuries in adolescent female football players: cluster randomised controlled trial. BMJ. 2012;344:e3042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Walden M, Krosshaug T, Bjorneboe J, Andersen TE, Faul O, Hagglund M. Three distinct mechanisms predominate in non-contact anterior cruciate ligament injuries in male professional football players: a systematic video analysis of 39 cases. Br J Sports Med. 2015;49(22):1452-1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med. 2016;44(7):1861-1876. [DOI] [PMC free article] [PubMed] [Google Scholar]