Abstract
This case report documents the rare occurrence of axillary metastasis in a patient with a history of typical urothelial bladder cancer. Bladder cancer rarely metastasizes to supradiaphragmatic cutaneous tissues, and this presentation confers a poorer prognosis as well as an association with atypical variants of bladder cancer. However, this paper suggests that typical pure urothelial bladder cancer may be just as aggressive as its atypical counterpart. In addition, the work-up of axillary masses in a patient with a history of bladder cancer, whether typical or variant, should include metastatic disease as part of the differential diagnosis and guide treatment strategies.
Keywords: Bladder cancer, Axillary mass, Metastasis
Introduction
Bladder cancer is the most common malignant disease of urinary tract. It is a disease of older age, and is more prevalent in men than women.1 Bladder cancer can be classified as urothelial and non-urothelial carcinoma.2 Urothelial carcinoma accounts for 90% of bladder cancer in western countries, and squamous cell carcinoma is the most common bladder cancer in Eastern Africa and the Middle East where schistomiasis is prevalent.1 The World Health Organization classification of urothelial cancers lists 13 different histologic variants of urothelial cancer, where non-urothelial bladder cancer and variants of urothelial carcinoma account for 25% of all bladder cancers.2
In regards to the metastatic potential of bladder cancer, it is variable and almost any organ can be involved.1 Of note, 75% of newly diagnosed bladder cancers are non-invasive while the rest are invasive and require radical treatment.2 The most common local regional metastasis involves lymph nodes and the most common site of distant metastasis involves the bone. Other sites of spread include the lung, liver, peritoneum, pleura, kidney, adrenal gland, intestine, and rarely the skin.1,3 Interestingly, the skin metastasis confers a very poor prognostic sign to the patient, as they are usually resistant to available treatment modalities.4
One case report documents a patient with muscle invasive transitional cell carcinoma with left supradiaphragmatic metastasis without evidence of visceral or bony metastasis; this patient was treated with palliative radiotherapy and chemotherapy, and subsequently died 6 months later.3 This study demonstrates the rare presentation and poor prognosis of supradiaphgramatic metastatic bladder cancer.
Furthermore, the rarity of skin metastasis is reinforced in one study of 150 patients with muscle invasive bladder cancer; here it was found that metastasis to soft tissue including muscle and subcutaneous tissue only occurred in a very small subset of patients.1
Case
A 71-year-old male with past medical history of CVA in 2010, BPH s/p laser prostatectomy 2015, who presented February 2019 with hematuria and urinary retention. Cystoscopy showing large posterior bladder lesion. Biopsy showed high grade urothelial carcinoma with muscular propia invasion. CT chest, abdomen and pelvis showed 6.8 × 4.5 × 4.3 cm posterior bladder mass with no obvious metastatic disease. Muscle invasive bladder cancer, stage 2, T2N0. Was planned to have 4 cycles of chemotherapy. He was then admitted with a CHF exacerbation March 2019 and found to have aortic insufficiency status post aortic valve replacement 3/19/19. He then developed bilateral ureteral obstruction and therefore underwent radical cystoprostatectomy, bilateral pelvic lymph node dissection, and creation of ileal conduit on 5/16/19 with plans for adjuvant chemotherapy. Pathology revealed urothelial carcinoma, with invasion extending into the perivesicular soft tissue 0/13 lymph nodes but with lymphovascular invasion, margins negative, pT3aN0. Post operatively he had an acute stroke that resulted in right upper extremity weakness requiring prolonged rehab and delay in adjuvant chemotherapy.
In early July 2019, he developed a left axillary mass (Fig. 1). Per report, he noticed it a few weeks prior and it was not painful. The mass was about 5 cm in diameter pedunculated, vascular appearing, painless, and tethered on a stalk to the axillary fossa. A CT scan was done showing solid, soft tissue mass within the subcutaneous tissue with no large vascular arterial involvement (Fig. 2). Given the vascularity of the mass a bedside core biopsy was aborted and the patient was taken to the operating room for excision of the left axillary mass. The patient tolerated the procedure without issue. Pathology of the specimen resulted as metastatic carcinoma consistent with bladder primary (Fig. 3).
Fig. 1.
Left axillary mass.
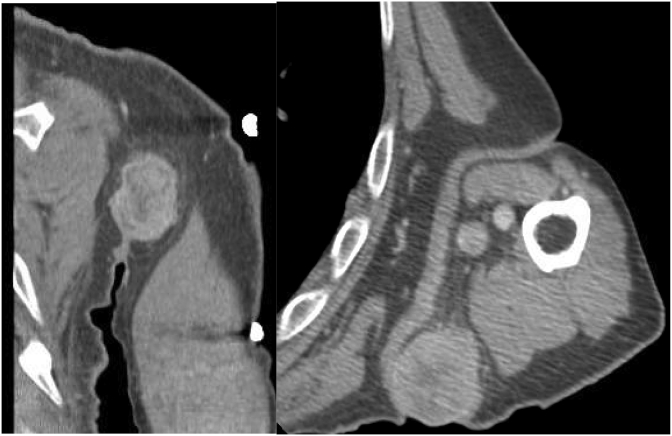
Fig. 2.
CT Impression: Spherical, solid soft tissue mass with minimal surrounding edema of the posterior, subcutaneous portion of the left axilla and inhomogeneous internal enhancement.
Fig. 3.
Axillary mass gross specimen.
Discussion
Bladder cancer metastasis in muscle invasive disease can rarely present as cutaneous lesions above the diaphragm.5 It is theorized that these distant metastases spread to the head and neck region hematogenously via the vertebral veins and lymphatics.3 Reasonably, bladder cancer that presents with such metastasis to the head and neck region confers a lower survival rate.3 Historically, variant histology bladder cancer is associated with these supradiaphragmatic cutaneous metastasis and therefore, confers a worse prognosis.2 This case report of typical bladder cancer with an axillary cutaneous metastasis, suggest that typical bladder cancer can also be similarly aggressive.
Non-urothelial carcinoma typically exhibits aggressive behavior and often advanced stages at primary resection are observed.2 One study of 150 cases of muscle invasive bladder cancer (pT2-4) compared the metastatic patterns of transitional cell carcinoma and those with atypical histologic features.1 The study found no significant difference in the metastatic pattern of tumors in the different T categories, however that patient with atypical histologic features had significantly higher incidence of peritoneal metastasis and therefore a worse prognosis,1 thereby guiding a more aggressive and radical treatment of atypical bladder cancer in comparison to pure urothelial carcinoma. However, this case report highlights the reality that typical pure urothelial metastatic bladder cancer may require equivalent radical treatment as these two entities behave similarly in regard to cutaneous metastases.
In conclusion, this rare presentation of axillary metastatic bladder cancer suggests that the work up of new head and neck and axillary masses in a patient with a history of bladder cancer should include metastasis on the differential.3 Furthermore, literature suggests that such aggressive disease is associated with atypical variants of bladder cancer, and should be treated with palliative radiotherapy and chemotherapy (with systemic cisplatin-based chemotherapy as the standard approach for patients with inoperable or locally advanced or metastatic disease, with average response rates of 50–60%5) when encountered. This case highlights a typical variant of bladder cancer with supradiaphragmatic cutaneous metastasis showing a similar aggressive pattern.
References
- 1.Shinagare A.B., Ramaiya N.H., Jagannathan J.P., Fennessy F.M., Taplin M.E., Van den Abbeele A.D. Metastatic pattern of bladder cancer: correlation with the characteristics of the primary tumor. AJR Am J Roentgenol. 2011;196(1):117–122. doi: 10.2214/AJR.10.5036. [DOI] [PubMed] [Google Scholar]
- 2.Klaile Y., Schlack K., Boegemann M., Steinestel J., Schrader A.J., Krabbe L.M. Variant histology in bladder cancer: how it should change the management in non-muscle invasive and muscle invasive disease? Transl Androl Urol. 2016;5(5):692–701. doi: 10.21037/tau.2016.06.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tunio M., Asirir M., Bayoumi Y., Fareed M., Shmad S. Cervical lymph node metastasis from transitional cell carcinoma of urinary bladder: case report and review of literature. J Solid Tumors. 2012;2(3):59–62. [Google Scholar]
- 4.Garg G., Sharma A., Sankhwar S. Metastatic adenocarcinoma of bladder presenting with skin and visceral metastasis. BMJ Case Rep. 2018;11(1) doi: 10.1136/bcr-2018-227042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kancharla V.P., Gulmi F.A., Agheli A. Transitional cell carcinoma of the bladder manifestating as malignant lymphoma with generalized lymphadenopathy. Case Rep Oncol. 2010;3(2):125–130. doi: 10.1159/000312424. [DOI] [PMC free article] [PubMed] [Google Scholar]