Abstract
Objectives
This study aimed to determine the impact on practice of applying the Extracorporeal Treatments in Poisoning (EXTRIP) Workgroup criteria to lithium toxicity.
Method
We retrospectively examined the medical records of patients from three hospitals who presented with chronic or acute on chronic lithium poisoning with a lithium concentration ≥1.3 mmol/L (2008‐2018). We determined which criteria were met by patients and their subsequent course. We developed and validated a method to predict if lithium concentration would be >1mmol/L at 36 hours.
Results
There were 111 acute on chronic and 250 chronic lithium toxic patients. Nine patients (2.5%) were treated with haemodialysis. Six chronic patients had neurological sequelae. The “estimated lithium concentration at 36 hours > 1 mmol/L” criterion required pharmacokinetic calculations. A simple nomogram was developed using Estimated Glomerular Filtration Rate (eGFR) and lithium concentration. For chronic toxicity, the nomogram would have correctly predicted lithium concentration >1.4 mmol/L at 36 hours in all except two patients. If EXTRIP criteria were followed, dialysis would have been instituted for 211 patients (58%). However, only 51 patients with chronic toxicity fulfilled both a concentration and a clinical criterion. Late neurological sequelae were observed in five out of six patients who fulfilled a concentration and a clinical criterion on admission, with the sixth meeting these criteria shortly after admission.
Conclusions
The EXTRIP criteria are too broad, but minor modifications allow haemodialysis to be targeted to those most at risk of sequelae. Most acute on chronic poisonings do not need haemodialysis, but it might shorten hospital stay in those with very high concentrations. The nomogram accurately predicts the fall in lithium concentration for chronic poisoning.
Keywords: acute on chronic lithium poisoning, chronic lithium toxicity, EXTRIP, haemodialysis, nomogram

What is already known about this subject
Lithium toxicity can cause permanent neurological sequelae and haemodialysis increases lithium elimination.
The EXTRIP group provide suggested indications for haemodialysis in lithium toxicity, but these have not been validated.
The same recommendations appeared to apply to acute, acute on chronic or chronic lithium poisonings, and many were only loosely defined.
What this study adds
This study refines the EXTRIP recommendations, reducing by two‐thirds the number of patients indicated for haemodialysis but still selecting all those at risk of sequelae.
A nomogram was developed to aid prediction of the EXTRIP criteria based on the expected fall in lithium concentrations over 36 hours in chronic lithium poisoning.
Acute vs chronic setting and selected EXTRIP criteria for lithium concentration, renal function and neurological symptoms work well in combination to determine which patients should receive haemodialysis.
1. INTRODUCTION
Lithium toxicity has low mortality but very significant morbidity. Prolonged admissions and recovery are common, and there is a significant risk of permanent neurological sequelae.1 Lithium elimination is greatly enhanced by haemodialysis.2 Endogenous lithium clearance is about 15‐20 mL/min with normal renal function. High efficiency intermittent haemodialysis can increase lithium clearance 10‐fold,2 and even low intensity methods (eg continuous renal replacement therapy [CRRT]) will triple clearance.2 An even greater proportion of lithium will be removed by extracorporeal treatment for patients with renal impairment, as the endogenous lithium clearance will be lower. Morbidity might be reduced by haemodialysis, but the indications are not well established.3
Recently, the Extracorporeal Treatments in Poisoning (EXTRIP) Workgroup systematically reviewed the evidence in the literature and provided their evidence‐based criteria of the indications for haemodialysis in lithium poisoning (Table 1).2 However, the criteria indicating need for dialysis were an unrelated set that lacked context with respect to the type of lithium poisoning. This may reflect the various sources from which the data were collected. The source references for each criterion are not explicitly referenced. They did not differentiate acute, acute on chronic or chronic lithium poisonings.2 Several criteria were vague, and it was unclear how some would work in multi‐agent exposures in acute poisoning. For example, decreased level of consciousness is a recommended criterion for haemodialysis but it is not quantified in order for it to apply in clinical settings. We have used a GCS < 15 as the definition for a decreased level of consciousness. EXTRIP suggested an estimated lithium concentration >1 mmol/L at 36 hours should be considered for haemodialysis. However, no method was provided to assist clinicians to make such an estimation. We aimed to apply these criteria to a cohort of patients with lithium toxicity/poisoning (most of whom did not receive dialysis) to provide insight into when and how the EXTRIP criteria should be adopted. In addition, we developed and validated a nomogram to predict lithium concentrations at 36 hours and determined how this might affect risk assessment for chronic and acute on chronic poisonings.
Table 1.
EXTRIP recommendations for lithium poisoning
| Extracorporeal treatment is recommended (1D) |
| Severe lithium poisoning |
| If kidney function is impaired and [Li + ] > 4.0 mEq/L a |
| A decreased level of consciousness b |
| Seizure |
| Life‐threatening dysrhythmias |
| Extracorporeal treatment is suggested (2D) |
| [Li + ] > 5 mEq/L |
| If confusion is present |
| If the expected time to obtain [Li + ] < 1.0 mEq/L with optimal management is >36 hours c |
We defined severe lithium poisoning as
‐ stupor, rigidity, hypertonia, hypotension
‐ coma, convulsion, myoclonus, cardiopulmonary collapse.
We defined impaired kidney function as eGFR < 45 mL/min/1.73 m2.
We defined decreased level of consciousness as GCS < 15.
We developed a method to predict lithium concentration at 36 hours using estimated parameters.
2. METHODS
This is a retrospective review of patients who had either acute on chronic or chronic lithium toxicity with a recorded plasma lithium level of at least 1.3 mmol/L (therapeutic range 0.8‐1.2 mmol/L in the acute phase, 0.5‐0.8 mmol/L in the maintenance phase) from the New South Wales (NSW) Health Pathology and South Eastern Area Toxicology Service (SEATS) database (1/2008 to 12/2018) in Sydney and the Princess Alexandra Toxicology Service (PATS) database in Queensland (7/2014 to 4/2019). The NSW Health Pathology and SEATS data were from the Prince of Wales and Sutherland Hospitals in Sydney. The PATS data included patients from the Princess Alexandra, Logan, Royal Brisbane and Redlands Hospitals in Queensland. We systematically extracted the following from records: patient demographics, signs and symptoms of toxicity, concurrent medications, treatments and outcomes. Acute on chronic poisonings were defined as patients who had taken an acute overdose while on lithium therapy. Chronic poisonings were defined as patients who developed toxicity while taking regular doses of lithium. We excluded patients whose medical records did not contain the data needed to determine if EXTRIP criteria were met and key outcomes occurred. We excluded repeat presentations if there was a gap of less than 2 months from a prior presentation with lithium toxicity.
One EXTRIP criterion is an expected lithium concentration >1 mmol/L in 36 hours.2 The source paper for this was not referenced, and there were no instructions for calculation. Therefore, we calculated this using an estimate of renal function to estimate lithium clearance. We estimated creatinine clearance (CrCL) using the Cockcroft Gault equation. As weight was rarely recorded we used a standard weight of 85 kg for men and 68 kg for women (derived from Australian population medians). Lithium clearance (mL/min) was set as 0.161 × CrCL + 6.47.6 (We explored an alternative calculation of lithium clearance using 0.235 × CrCL but the former method led to slightly better agreement, data not shown). From the estimated clearance and the initial concentration (C 0) an estimate can be made of future concentrations (C t) using the simple method of C t = C 0 × e–kt, where k = Cl/V d. Volume of distribution V d was set at 48 L for women and 60 L for men (based on 0.8 L/ideal body weight kg). We used a simpler method using k = (0.161 × eGFR + 6.47)/55 to produce a nomogram that applied to all patients irrespective of variables other than the eGFR. eGFR values were calculated using serum creatinine levels in accordance to the Chronic Kidney Disease Epidemiology Collaboration (CKD‐EPI) formula.7 The predicted lithium concentrations at 36 hours were compared with actual concentrations from patients who were not dialysed and had serial lithium levels taken.
Patient medical records were carefully examined to determine if patients fulfilled the EXTRIP criteria. We derived the EXTRIP criteria met by each patient on initial assessment. We compared the acute on chronic with chronic groups using the Mann‐Whitney or Chi‐square test as appropriate. We also graphically compared criteria and estimates; all analysis was done using GraphPad Prism ® (V8). The study was approved by the South Eastern Area Health Human Research Ethics Committee (Ref Number: 17/201) and the Metro South Human Education & Research Centre (HREC) (14/QPAH/308).
3. RESULTS
We extracted data on 111 acute on chronic and 250 chronic lithium intoxications; 167 other admissions were excluded due to insufficient medical records or repeat presentation within 2 months (Figure S1). The acute on chronic group was younger and had a higher lithium concentration, better renal function and higher estimated lithium clearance compared with the chronic group (Table 2). Nine patients (2.5%) were treated with dialysis (continuous veno venous haemodiafiltration (n = 5), intermittent haemodialysis (n = 3), sustained low efficiency dialysis (n = 1)) (Table S1). Six patients who were not dialysed from the chronic group were diagnosed with severe neurological sequelae (Table S1). They had lithium concentrations between 1.8 and 3.2 mmol/L and moderate to severe renal impairment (eGFR: 21‐54). One patient died with acute renal failure, pneumonia, and right heart failure; the death was deemed not related to lithium toxicity (Li concentration was 1.3 mmol/L on admission).
Table 2.
Demographic and clinical characteristics of acute on chronic and chronic lithium toxicity
| Acute on chronic (n = 111) | Chronic (n = 250) | P valuea | |
|---|---|---|---|
| Female | 84 (76%) | 160 (64%) | 0.028 |
| Age (years) | 40 (16‐93) | 56 (15‐96) | <0.0001 |
| Initial serum Li (mmol/L) | 2.4 (1.3‐8.6) | 1.6 (1.3‐7.1) | <0.0001 |
| Lithium dose (mg) | 900 (250‐1750) | 900 (125‐2500) | 0.4 |
| eGFR (mL/min/1.73 m2) | 96 (16‐155) | 66 (5‐148) | <0.0001 |
| Lithium clearance (ml/min) | 23 (10‐42) | 18 (8‐38) | <0.0001 |
| Nephrotoxic drugs | 0 (0.0%) | 6 (2.4%) | 0.1 |
| Lithium drug interactions | 12 (11%) | 62 (25%) | 0.0024 |
| Suspected to have infection | 1 (0.9%) | 62 (25%) | <0.0001 |
| Median length of stay (d) | 1.4 (0.1‐33) | 4 (0.1‐94) | 0.0014 |
Note. Data are shown as medians (range) or counts (%). Nephrotoxic drugs were cyclosporin, cisplatin, β‐lactam antibiotics, amphotericin B. Lithium drug interactions were diuretics, angiotensin converting enzyme inhibitors, angiotensin receptor blockers, nonsteroidal anti‐inflammatory drugs.
Mann‐Whitney U test or Chi‐square for categorical variables.
Serial lithium samples were taken from most patients (Figure 1). The chronic toxicity patients’ serum lithium concentrations generally fell steadily from the time of admission. Acute on chronic overdoses had very unpredictable serum concentrations, although all patients had concentrations <1 mmol/L by 72 hours. Some acute on chronic poisoned patients had rising concentrations for up to 24 hours. Conversely, many had rapidly falling concentrations (apparent half‐life <12 hours), suggesting a predominant effect of distribution rather than elimination. Consequently, the predictions of concentrations 36 hours later were excellent for chronic toxicity (mean bias 0 mmol/L, SD 0.3, 95% limits of agreement –0.7 to +0.6). In contrast, in acute on chronic toxicity, prediction was very poor (mean bias +0.4 mmol/L, SD 0.4, 95% limits of agreement –0.5 to +1.2). The simpler eGFR method had equivalent bias and limits of agreement to the above for both acute on chronic and chronic toxicity groups (Figure S2).
Figure 1.

Serial lithium concentrations in patients with chronic toxicity and acute on chronic poisoning. Red lines indicate patients who were dialysed, purple lines indicate patients with rising levels and blue lines indicate patients with initially rapidly falling levels (apparent half‐life <12 hours), indicating the rapid change was caused predominantly by distribution. Black lines represent patients who have an expected drop in serial lithium concentration. Green areas represent lithium concentrations up to 1.0 mmol/L
A nomogram was developed from the simple eGFR method to indicate which patients would have a lithium concentration above 1 mmol/L at 36 hours (Figure 2). The results of patients plotted on this nomogram are shown in Figure 3. For chronic toxicity the nomogram would have suggested dialysis for all patients who developed neurological sequelae, all patients who were dialysed and all but two patients who still had lithium >1.4 mmol/L at 36 hours.
Figure 2.

Lithium nomogram to indicate if lithium concentration is predicted to be >1 mmol/L at 36 hours. This nomogram used lithium concentration and eGFR on presentation to predict if lithium concentration will be above 1 mmol/L at 36 hours
Figure 3.

Outcomes for patients compared to predicted lithium concentrations. Patients above the nomogram line were predicted to have lithium concentration >1 mmol/L at 36 hours. Only the 128 chronic and 78 acute on chronic patients with sufficient serial samples to reasonably estimate actual concentrations at 36 hours are shown
There were 81/111(73%) acute on chronic and 130/250 (52%) chronic lithium toxicity patients who fulfilled at least one of the EXTRIP criteria for dialysis (Figure 3). Each individual criterion was met by between 0 and 80 patients (Figure 4). Only 51 chronic toxicity patients fulfilled both a concentration (eg Li > 1 at 36 hours) and a clinical (eg neurological toxicity, GCS < 15 or confusion) criterion. This included 5/5 (100%) patients who had haemodialysis and 5/6 (83%) patients who had neurological sequelae. One patient who developed neurological sequelae fulfilled the concentration criteria, but was recorded as having no neurological deficit on initial examination. The patient subsequently was recorded as confused within a few hours.
Figure 4.
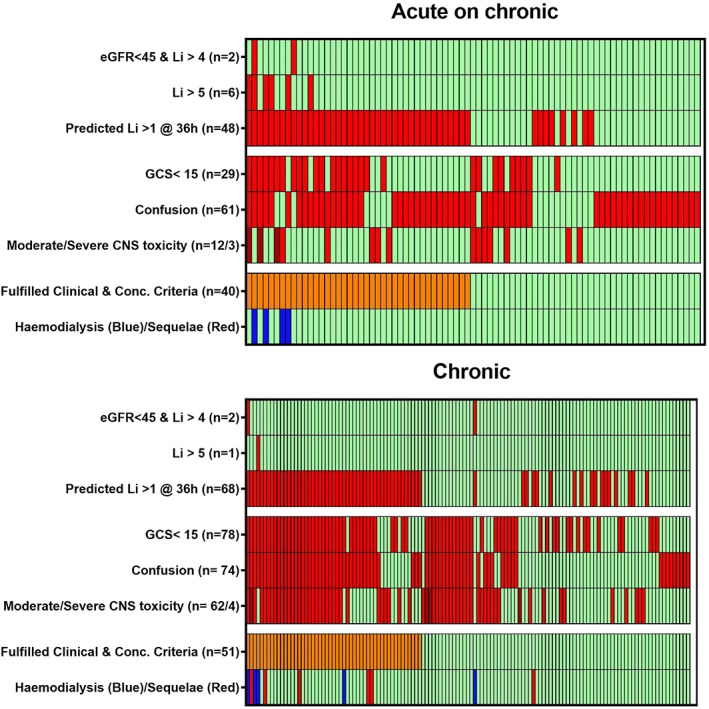
Heatmap representation of overlap of criteria in patients who fulfilled one or more EXTRIP criteria. Notes: Each column represents one patient. A red or dark red bar indicates they fulfilled the EXTRIP criteria. Moderate/severe central nervous system toxicity: stupor, rigidity, hypertonia, hypotension, coma, convulsion, myoclonus, cardiopulmonary collapse. Not shown are the 150 patients who did not fulfil any criteria: acute on chronic (30/111) and chronic (120/250) group
There were 40 acute on chronic patients who fulfilled both a concentration and a clinical criterion. However, only 7 met the “>4 mmol/L and eGFR < 45” or “>5 mmol/L” concentration criteria on initial assessment (8 patients at any time during admission). The clinical criteria in the acute on chronic ingestions were generally short‐lived and in patients who had co‐ingested other agents, causing sedation and/or confusion.
4. DISCUSSION
Lithium intoxication can cause severe morbidity and occasionally irreversible neurological damage, generally with chronic toxicity.4, 10 Patients who have both clinical features and lithium concentrations that are expected to be elevated for some time are those most likely to derive benefit from haemodialysis.1, 4, 5 These criteria would result in dialysis for roughly 20% of chronic toxicity patients; in our series this included all those who developed neurological sequelae. However, acute on chronic toxicity has much lower risk. We found that lithium concentrations in acute on chronic toxicity had no predictable pattern, generally resolved within a few days and most CNS effects were probably due to other agents. Thus, the two absolute concentration criteria were the only potentially useful criteria for dialysis after acute on chronic toxicity. These criteria would result in dialysis for around 7% of acute on chronic toxicity patients. Using both recommended and suggested EXTRIP criteria would lead to dialysis for 58% of all patients (Table 1) and 38% if restricting to just EXTRIP ‘recommendations’ (Table 1). Only 16% of patients would be dialysed according to our suggested modification of these guidelines (Figure 5), and yet this would still capture all those most likely to benefit and those who had long‐term neurological sequelae.
Figure 5.

Simplified flowchart of proposed indications for haemodialysis in lithium poisoning. This flowchart outlines the approach to whether haemodialysis should be used in patients with acute on chronic and chronic lithium poisoning by looking at the lithium concentration and symptoms of neurotoxicity
Haemodialysis may reduce the duration of brain exposure to toxic lithium concentrations, although this is hard to demonstrate. Lithium redistributes very slowly in and out of the brain, and recovery from chronic toxicity after concentrations fall frequently takes many days or weeks.4, 10 Renal lithium clearance was estimated to be 10‐25 mL/min in most of our patients. Intermittent haemodialysis can achieve lithium clearance as high as 170 mL/min while CRRT has an average clearance of 43 mL/min.2 It follows that any mode of dialysis will increase the elimination of lithium several fold.
The nomogram we developed allows a simple and quick determination of whether lithium concentrations will remain elevated (Figure 2). More complex nomograms that estimate actual lithium concentration at 36 hours have been described.8 The origin of the EXTRIP's suggested criteria regarding lithium concentration >1.0 mmol/L at 36 hours is unclear, but Hansen and Amdisen suggested dialysis should be instituted in patients whose plasma lithium concentration cannot be reduced to 1 mmol/L within 30 hours.4 In any case, longer or shorter time frame prediction is equally possible. We suspect even more accurate predictions would be possible using actual body weight to derive estimates of CrCl and Li V d. However, the nomogram worked surprisingly well and has the advantage of avoiding the risk of calculation and data entry errors. Notably, our determination of the 36 hour lithium concentration using the nomogram was based on initial (or presentation) blood tests. However, the steady decline in serial concentrations in chronic toxicity suggest that the nomogram could utilise lithium measurements at any time point.
The EXTRIP recommendations did not differentiate between chronic and acute poisoning. However, most previous studies have highlighted that acute on chronic poisonings commonly have better kidney function and much lower risk of neurotoxicity,1, 4, 5, 10 and it is not logical to have exactly the same criteria for all patients. Even using the two higher concentration criteria may be unnecessarily interventional, as good outcomes are usual with conservative management. Chronic toxicity has a much poorer prognosis.4, 10 Plasma concentrations then reflect intracellular brain concentrations.9 Haemodialysis is commonly recommended for patients with high serum concentrations (typically >2.5 mmol/L) of lithium as these are associated with severe neurological toxicity.4 It might be assumed these are also the patients most at risk of neurological sequelae. However, in our study, the patients with neurological sequelae had concentrations as low as 1.8 mmol/L, but they were also elderly with poor renal function (Table S1). The advantage of the criterion of expected lithium concentration >1 mmol/L at 36 hours is that it captured these patients. The mechanism of lithium‐induced neurological sequelae is not clear, and it may not be simply lithium‐induced neurotoxicity. For example, it might result from wide osmotic fluctuations due to volume depletion and dehydration from nephrogenic diabetes insipidus, which might be more common amongst the elderly, chronic lithium users and those with poorer kidney function.10
The key limitations of our study were that it was retrospective and relied on the accuracy of data from medical records. A moderate number of patients were excluded due to a lack of data recorded in their medical records. There may be inaccurately recorded outcomes and we had to use estimated body weights based on population means. For patients who are well outside the normal range of body weight, it would be better to use direct calculations for prediction. Prospective studies utilising these modified EXTRIP criteria would be useful to determine if they have an impact on short‐ and long‐term morbidity. In addition, the formulation of the lithium carbonate tablets was not well documented to indicate whether they were immediate or sustained‐release products. The two products have different pharmacokinetics. However, based on the lithium dosages, we worked out about 37% patients were on sustained‐release formulation.
5. CONCLUSION
The current EXTRIP criteria require refinement to provide more precise guidance on which lithium intoxicated patients are likely to benefit from haemodialysis. Our study clearly highlights the benefits of determining the need for dialysis based on an integrated assessment of the type of poisoning, lithium concentration, renal function and clinical toxic effects (Figure 5). This reduces the numbers by two‐thirds, but still accurately identifies those most likely to benefit.
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare.
Supporting information
Figure S1. A flowchart of the number of patients who were included in the study and their outcome.
Supporting Information Figure 2. Residual plots of predicted‐actual on chronic eGFR vs actual lithium concentrations at 36 hours.
Supporting Information Table 1. EXTRIP criteria met by patients treated with haemodialysis and those with neurological sequelae and outcome at discharge.
ACKNOWLEDGEMENTS
N.B. was responsible for designing the study and developing the nomogram. S.C. was responsible for collecting and entering data into the database from SEATS and NSW Health Pathology. K.I. was responsible for collecting and entering the data from PAT. A.C. and W.S. were responsible for providing data from SEATS. E.V. was responsible for providing data from NSW Health Pathology. B.C. was responsible for analysing the data. N.B. and B.C. were primarily responsible for writing the paper. All authors have contributed in reviewing and writing the paper.
Buckley NA, Cheng S, Isoardi K, et al. Haemodialysis for lithium poisoning: Translating EXTRIP recommendations into practical guidelines. Br J Clin Pharmacol. 2020;86:999–1006. 10.1111/bcp.14212
N.B. is the primary individual responsible for the design of the study, data review and analysis as well as writing up the article.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author, subject to ethical approval. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- 1. Vodovar D, El BS, Curis E, Deye N, Megarbane B. Lithium poisoning in the intensive care unit: predictive factors of severity and indications for extracorporeal toxin removal to improve outcome. Clin Toxicol (Phila). 2016. September;54(8):615‐623. [DOI] [PubMed] [Google Scholar]
- 2. Decker BS, Goldfarb DS, Dargan PI, et al. Extracorporeal treatment for lithium poisoning: systematic review and recommendations from the EXTRIP workgroup. Clin J Am Soc Nephrol. 2015. May 7;10(5):875‐887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bailey B, McGuigan M. Comparison of patients hemodialyzed for lithium poisoning and those for whom dialysis was recommended by PCC but not done: what lesson can we learn? Clin Nephrol. 2000. November;54(5):388‐392. [PubMed] [Google Scholar]
- 4. Hansen HE, Amdisen A. Lithium intoxication. (report of 23 cases and review of 100 cases from the literature). Q J Med. 1978. April;47(186):123‐144. [PubMed] [Google Scholar]
- 5. Waring WS, Laing WJ, Good AM, Bateman DN. Pattern of lithium exposure predicts poisoning severity: evaluation of referrals to a regional poisons unit. QJM. 2007. May;100(5):271‐276. [DOI] [PubMed] [Google Scholar]
- 6. Motoki T, Fukuoka N, Yamaguchi K, et al. Calculation of lithium clearance for clinical use based on renal excretion in Japanese patients. Int J Clin Pharmacol Pharmacother. 2016;1(107):1–5. [Google Scholar]
- 7. Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009. May 5;150(9):604‐612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Buckley NA, Dawson AH, Whyte IM. Hypertox. Assessment and Treatment of Poisoning. http://www.hypertox.com http://www.wikitox.com 2017;
- 9. Riedl U, Barocka A, Kolem H, et al. Duration of lithium treatment and brain lithium concentration in patients with unipolar and schizoaffective disorder‐‐a study with magnetic resonance spectroscopy. Biol Psychiatry. 1997. April 15;41(8):844‐850. [DOI] [PubMed] [Google Scholar]
- 10. Oakley PW, Whyte IM, Carter GL. Lithium toxicity: an iatrogenic problem in susceptible individuals. Aust N Z J Psychiatry. 2001. December;35(6):833‐840. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. A flowchart of the number of patients who were included in the study and their outcome.
Supporting Information Figure 2. Residual plots of predicted‐actual on chronic eGFR vs actual lithium concentrations at 36 hours.
Supporting Information Table 1. EXTRIP criteria met by patients treated with haemodialysis and those with neurological sequelae and outcome at discharge.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author, subject to ethical approval. The data are not publicly available due to privacy or ethical restrictions.


