Abstract
Extensive research supports a strong and cumulative relationship between adverse childhood experiences (ACEs) and risky adult behaviors, mental health disorders, diseases, and health status. Additional factors, such as poor maternal wellbeing and economic hardship, compound the detrimental health and wellbeing implications associated with childhood exposure to ACEs. However, limited research has explored the differentiating effects of economic hardship and maternal wellbeing on a child’s cumulative ACE exposure. This study examined the differing effects of poor maternal wellbeing and economic hardship on a child’s exposure to ACEs. This study used a random sub-sample (n = 4000) from the 2011 to 2012 National Survey on Children’s Health (NSCH), a nationally representative cross-sectional study of children (N = 95,677) between birth and 17 years old. Confirmatory factor analysis results revealed greater economic hardship had a significant direct effect on a child’s ACE exposure and poorer maternal wellbeing. Poor maternal wellbeing had a significant mediation-like effect on the relationship between economic hardship and a child’s cumulative ACE exposure. Practice and policy implications include early ACE assessments tailored to identify children and families experiencing adversity across multiple domains.
Keywords: Economic hardship, Maternal wellbeing, Adverse childhood experiences (ACEs)
Adverse childhood experiences (ACEs) include any childhood exposure to a traumatic incident, adverse family experience, or circumstance that may have long-term negative consequences across an individual’s lifespan (Bramlett and Radel 2014; Kalmakis and Chandler 2014). Nearly 60% of adults report exposure to one ACE with approximately 9% reporting five or more adversities (Bynum et al. 2010; Dong et al. 2004; Folger et al. 2018). Extensive research documents the prevalence and life-course consequences of childhood exposure to specific ACEs, such as child physical abuse, neglect, and exposure to parental substance misuse, however, limited research exists on the determinants and outcomes of childhood exposure to multiple ACEs (Edwards et al. 2003; Sabri et al. 2013; Turner et al. 2006; Turner et al. 2010).
Exposure to ACEs is not only a salient public health issue but a significant economic burden with confirmed cases of child maltreatment, including ACEs such as child physical, sexual and emotional abuse, and physical and emotional neglect, estimated to have an aggregated lifetime economic cost of $124 billion, totaling to a lifetime cost of $210,000 per child (Fang et al. 2012). Furthermore, additional adversities such as poor maternal wellbeing and familial economic hardship compound the detrimental health and wellbeing implications associated with childhood ACE exposure. Despite the empirical evidence revealing the interrelatedness of ACEs and the cumulative risks associated with ACE exposure, minimal literature exists exploring the differentiating impact of economic hardship and maternal wellbeing on a child’s risk of exposure to ACEs. In an attempt to deepen the discussion and to bridge the gaps in literature, this study sought to examine the separate effects of economic hardship and poor maternal wellbeing on a child’s ACE exposure to enhance the knowledge base and understanding of mitigating familial risk factors.
Adverse Childhood Experiences (ACEs)
The seminal ACE Study, conducted during the 1990s, was the first large-scale, cross-sectional study to reveal a significantly strong and cumulative relationship between ACEs and leading causes of death in adulthood (Felitti et al. 1998). Results demonstrated a strong interrelationship between the surveyed adversities finding that individuals who identified childhood exposure to multiple ACEs were more likely to have several health risk factors in adulthood including: smoking, alcoholism, suicidality, depression, have numerous sexual partners, and drug abuse (Felitti et al. 1998). Since the formative ACE Study, researchers have linked ACE exposure to neurological impairments (Anda et al. 2006), unintended pregnancy (Hillis et al. 2004), fetal death (Hillis et al. 2004), suicidality (Dube et al. 2001), hospitalizations related to autoimmune diseases (Dube et al. 2009), illicit drug use (Dube et al. 2003), learning and behavior disorders (Burke et al. 2011), unemployment (Liu et al. 2013), and adult homelessness (Herman et al. 1997). Although informative, current empirical research is fragmented by examining certain, and often specific combinations of ACEs (i.e. exposure to child abuse and parental violence), this restriction may overlook the interrelationships of ACEs and presume the absence of other adversities, therefore, overestimating the influence of certain ACEs on wellbeing and developmental outcomes (Edwards et al. 2003; Finkelhor et al. 2005; Liming and Grube 2018). Further, this burgeoning and robust empirical literature base is overwhelmingly represented by retrospective adult-reports of ACEs, often examining health and wellbeing outcomes associated with increased ACE exposure. A limited amount of research exists exploring potential contextual determinants of increased ACE exposure among children—specifically caregiver and environmental characteristics that could be potentiating risk factors for increased exposure to adversity.
Cumulative ACE Exposure
Finkelhor et al. (2005) found, in a nationally representative study of children between 2 and 17 years old, that youth who experienced any victimization were 69% more likely to experience another form of adversity within a given year. The same researchers found that eight-percent of a nationally representative sample had experienced seven or more adversities within the past year (Finkelhor et al. 2011). Their results revealed children who experienced multiple direct and indirect adversities were disproportionately exposed to the most serious forms of adversities, including child sexual abuse and maltreatment, and were significantly more likely to exhibit psychological distress symptomology (Finkelhor et al. 2011). These findings are critical, providing strong evidence that exposure to one form of adversity is a predictor of future adversity (Finkelhor et al. 2011).
Looking specifically at child welfare-involved children in early childhood, birth through 71 months, Kerker and colleagues (2015) found that more than 98% of their high-risk sample had been exposed to at least one ACE with over half of the sample reporting four or more. For each additional ACE reported, the child was 21% more likely to have a chronic medical condition, 32% more likely to have a clinical-range Child Behavioral Checklist (CBCL) score, and, for children 36–71 months old, 77% more likely to report social development issues (Kerker et al. 2015). High ACE exposure rates were also found in a systematic review examining wellbeing outcomes of young children exposed to cumulative ACEs; among high-risk samples of children 0 to 83 months old, results showed between 12.3 and 70% were exposed to three or more adversities (Liming and Grube 2018). Taken together, these findings provide evidence that high-risk, vulnerable young children are at increased risk of cumulative ACE exposure, that exposure to multiple adversities may have almost immediate negative implications for children in early childhood (Kerker et al. 2015), and that high-risk environments may compound a child’s exposure to adversity (Finkelhor et al. 2011).
Turner et al. (2010) found that youth who experienced compounding adversities were more likely to have increased trauma symptomology (e.g. anger, anxiety, depression, and dissociation), compared to youth who reported repeated exposure to a single victimization/adversity. This key finding provides evidence that previous research focusing on sole adversities, although important, may overestimate the relationship between the respective ACE and subsequent negative outcomes. Similarly, Dong and colleagues (2004) found that participants who reported exposure to one ACE were between 2 and 17.7% times more likely to report exposure to a second adversity, supporting the comorbidity among ACEs and reinforcing the importance of assessing for, identifying, and treating youth who have been exposed to multiple adversities.
Aligning closely with the theoretical framework guiding this study, the ecological transactional model of child maltreatment, Turner et al. (2010) posit that for children exposed to multiple adversities, such exposure is experienced across systems levels (i.e. by school peers, family members, neighbors, etc.), and that for these vulnerable children, victimization resembles a life condition. Widespread adversity experienced across systems levels decreases the potential of resiliency and, therefore, cumulative adversities are likely to produce significant deleterious effects on the child’s social, behavioral, emotional, and academic development (Turner et al. 2010). The findings from this study further support the notion that researchers should consider potential contextual and environmental variables that influence cumulative ACE exposure, because often, children who experience one ACE also experience compounding adversities across multiple domains. Adding to the literature base, the present study considers pathways through which two specific contextual variables—maternal wellbeing and economic hardship—relate, directly and indirectly, to a child’s cumulative ACE exposure.
Caregiver Wellbeing
Characteristics within the child’s most proximal environments, including their family system and attachment with their primary caregivers, have the greatest influence on the child’s development and wellbeing, both positively and negatively (Cicchetti and Lynch 1993). Exploring the influence of caregiver wellbeing and child outcomes will help lay the foundation for examining the differing effects of caregiver mental and physical health status and their children’s exposure to potential adversities.
Caregiver Mental Health
Common to the ACE literature is childhood exposure to caregiver mental health issues. A vast amount of research has shown mothers who have depression are more likely to have children with: depression, asthma morbidity, behavioral problems, and greater risk for developmental delays (Kahn et al. 2004; Spieker et al. 1999). Goodman et al. (2011) conducted a meta-analysis on the effects of maternal depression and child psychopathology and found that maternal depression was significantly associated with higher levels of general psychopathology, internalizing, externalizing, and negative behavior/affect in their children. Goodman and researchers (2011) also found that when family income was used as a moderator in the association between maternal depression and child outcomes, children from low-income families were significantly more likely to exhibit internalizing behaviors, externalizing behaviors, negative affect and behavior, and general psychopathology, compared to children with mothers who have depression living in middle-income or mixed-income households.
Examining the relationship between paternal and maternal mental health and children’s emotional and behavioral health in two-parent households, Kahn et al. (2004) found that children who had mothers with poor mental health were more likely than other children to also have fathers with poor mental health (Kahn et al. 2004). Behavioral issues among the sampled children were also more likely if their mother had less education, if either parent reported smoking, and if they lived in a low-income household, compared to other children in the study (Kahn et al. 2004). These findings emphasize the weighted effects of poor maternal mental health on child’s developmental and behavioral outcomes of children living in households with poor caregiver mental health.
In one longitudinal study examining the association of early childhood exposure to maternal depression and anxiety, poverty, and marital status and adolescent anxiety and depression symptomology at age 14, Spence and colleagues (2002) found that maternal depression, experienced within the first 5 years of life, had a significant direct effect on anxiety-depression symptoms in the adolescent participant. These results remained statistically significant even after controlling for poverty and relationship status. Moreover, chronic and prolonged exposure to maternal depression throughout the child’s life (as oppose to one time point) had significant cumulative effects on the youth’s anxiety-depression symptomology at 14 years old, above and beyond the effects of poverty and marital status (Spence et al. 2002).
Caregiver Physical Health
Prince et al. (2007) posit that an individual’s mental health status must be considered in all faucets of health policy, planning, delivery, and care systems, because decent physical health cannot be achieved without decent mental health. The results from a qualitative study of 40 caregivers of disabled children strongly support the complex and intimate relationship between physical and mental health status (Murphy et al. 2007). Qualitative results showed that, within the past year, 41% of the participants self-reported that their overall physical and mental health had worsened, and, for this sample, caregivers overlooked their health conditions, instead prioritizing the needs of their children (Murphy et al. 2007). Although these findings cannot be generalized, it is noteworthy that the five emergent qualitative themes (e.g. 1) stress of caregiving; 2) negative impact on caregiver health; 3) sharing the burden; 4) worry about the future; and 5) caregiver coping strategies) can also be applied to caregivers experiencing other adversities, such as low-income, substance abuse, or even single-parenthood (Murphy et al. 2007, p. 182–184). These findings may highlight that caregivers experiencing chronic stress, such as caring for a child with a disability or living in poverty, threatens both their physical and mental health, which in turn may also impact their caregiving and parenting abilities.
Exploring the association between household income, state income inequality, and the mental and physical health of mothers with young children, Kahn and colleagues (2000) found that mothers who were unmarried, young, non-white, and had fewer years of education were significantly more likely to report their physical health status as fair or poor and to report symptoms of depression (Kahn et al. 2000). Kahn et al. (2000) compared the wealthiest 20% of participant mothers to the poorest 20% and found that low-income mothers were more likely to self-report fair or poor health (15% v. 2%, p < .001) and more likely to report symptoms of depression (33% v. 9%, p < .001). Poverty and greater state income inequality had compounding effects on a maternal caregiver’s mental and physical health (Kahn et al. 2000). Compared to low-income mothers living in states with low income inequality, researchers found that mothers of young children living in states with greater income inequality were 60% more like to report depressive symptoms and 80% more likely to rate their health as fair or poor (Kahn et al. 2000). Hence, the effects of poverty are compounded when state income inequality is greater, in turn increasing the likelihood of worse maternal wellbeing. The findings from Kahn and researchers (2000) provide insight into the transactional effects and compounding-nature of contextual adversities (i.e. low-income and high state inequality) on an individual’s wellbeing.
Although outcome variables and variables of interest vary in the current literature addressing the implications of poor mental and physical health, it seems clear that the overall health and wellbeing of a child’s caregiver is intimately intertwined with environmental variables and the health and wellbeing of their children. The same caregiver variables often used as risk factors can be protective factors for children as well, given nurturing and supportive conditions. Research exploring the relationship between a child-rearing environment, maternal wellbeing, and exposure to adversities is critical to advancing the current knowledge base in helping to identify extremely vulnerable children.
Economic Hardship
Extensive research has been conducted on the effects of familial poverty and a variety of child outcomes (Brooks-Gunn and Duncan 1997; Duncan et al. 1994; Petterson and Albers 2001), and the association between an individual’s health and socioeconomic status (Kahn et al. 2000). Although poverty is a strong predictor of negative physical health, socio-emotional, and cognitive outcomes (Duncan et al. 1994; Evans 2004; Evans and Kim 2013), a limited amount of empirical literature exists exploring the direct and indirect relationships between economic hardship and increased exposure to ACEs. Given the extreme overlap that exists between the risk factors and outcomes associated with childhood exposure to poverty and ACEs, there is a need for research to advance the current literature base examining the differentiating effects of economic instability and the association with ACE exposure.
Supporting the interrelatedness of these two areas of literature, Evans and Kim (2013) state that lower-income caregivers have lower levels of engagement with their children, and subsequently are less responsive and less attentive to their child’s needs. Children living in low-income households are also exposed to higher levels of hostility, familial conflict, marital dissolution, maternal depression, and are more likely to be physically disciplined (Evans 2004; Evans and Kim 2013; Petterson and Albers 2001). Evans and Kim (2013) highlight the potentiating risk factors across systems levels experienced by children living in households affected by economic instability: “One implication of the ecological context of childhood poverty is that disadvantaged children not only face a greater confluence of cumulative risk factors but do so across multiple domains of risk” (p.44).
This finding is supported by Pelton (2015) who argued that impoverishment underpins high-risk environments, leading to circumstances that may endanger children by increasing opportunities for adversity. Specifically, Pelton (2015) states that:
…poverty produces material hardships that can lead to parental stress. This stress…can cause anger in parents that might eventuate child abuse, or depression that might eventuate in neglect…the material deficits of poverty, such as the health and safety hazards of inadequate housing, can directly lead to child harm and endangerment, with the parents being implicated for child neglect for not sufficiently protecting the child from these hazards (p. 34).
Pelton (2015) illustrates that economic hardship can indirectly influence a child’s exposure to ACEs through caregiver stress and decreased wellbeing, and directly influence exposure to adversities by underpinning high-risk environments. It is important to note that although Pelton (2015) postulates the direct and indirect effects of poverty on a child’s exposure to maltreatment and neglect, these findings have only been supported independently, and to this author’s knowledge, no study has examined how caregiver wellbeing influences the relationship of economic hardship and a child’s exposure to broader adversity. Additionally, Evans (2004) posits that chronic and persistent economic hardship has more adverse effects on children and that such effects are cumulative across environmental contexts.
Further, several studies have examined the effects of poverty and maternal depression on a child’s development (Brooks-Gunn and Duncan 1997; Duncan et al. 1994; Evans 2004; Petterson and Albers 2001; Spence et al. 2002). Petterson and Albers (2001) examined the mediating effect of maternal depression between poverty and early childhood development and found that both poverty and maternal depression jeopardize development in young children with affluence slightly buffering the consequences of maternal depression.
Research has independently demonstrated the detrimental consequences of childhood exposure to economic hardship, poor caregiver wellbeing, and cumulative exposure to ACEs; however, a scarce amount of literature has examined, together, the differentiating effects of such contextual variables on a child’s exposure to adversity. In an attempt to deepen the understanding and comprehension, and advance theory development, the objective of this manuscript was to provide further insight into the association between potential contextual determinants of increased exposure to childhood adversity. Knowledge building is the first step to inform prevention and intervention efforts and advance practice and policy.
Theory & Hypotheses
Extant research reveals children who experience any adversity are highly likely to experience several types of adversity across domains and such adversities tend to cluster due to exposure to high-risk environments (Finkelhor et al. 2005). The interrelatedness of ACEs across institutions aligns well with the ecological systems framework. Stemming from Urie Bronfenbrenner’s ecological system theory (Bronfenbrenner 1977), this study was guided by the ecological-transactional model of child maltreatment (Cicchetti et al. 2000) to shed light on the transactional effects of economic hardship, poor maternal wellbeing, and a child’s risk for cumulative ACE exposure. The ecological-transactional model of child maltreatment proposes that there is a reciprocal relationship between the environment, the child’s caregivers, and the child/individual, all manipulating and influencing the child’s exposure to adversity and subsequent development (Cicchetti and Lynch 1993; Cicchetti et al. 2000).
Broadly applying the ecological transactional model to ACEs, it is proposed that exposure to any ACE at the microsystem level (e.g. child physical abuse, caregiver substance abuse, intimate partner violence, etc.) has reciprocal and potentiating risk factors on the child’s cognitive, social and mental health development, peer-to-peer relationships, family interactions, and factors at the mesosystem (e.g. community violence) and exosystem levels (e.g. sexual violence). For the present study, the ecological-transactional model provided a contextualized approach to understand potentiating and differentiating effects of familial economic hardships and poor maternal wellbeing on a child’s exposure to ACEs. The expansive and dynamic theoretical approach offered by the ecological-transactional model of child maltreatment pairs well with structural equation modeling (SEM). SEM is a theory-driven statistical analysis approach that allows researchers to assess, modify, and further develop theoretical frameworks (Anderson and Gerbing 1988; Little 2013). Together, this study’s theoretical and statistical approach allows for a fruitful examination of the differentiating effects of economic hardship and poor maternal wellbeing on a child’s exposure to ACEs.
Despite the wealth of empirical research revealing the potential detrimental outcomes and comorbidity of ACEs and the compounding effects of poverty and poor caregiver mental and physical health, little is known regarding how poor maternal wellbeing influences the association between economic hardship and child’s exposure to adversity. To address this gap in literature, and to the knowledge of this author, no prior study has examined the differentiating effects of familial economic hardship and caregiver wellbeing on a child’s risk for ACE exposure. This study sought to explore the direct and indirect effects of familial economic hardship and caregiver wellbeing on a child’s cumulative ACE exposure to provide insight into potential mechanisms that increase a child’s likelihood of exposure to adversities and to better inform prevention and intervention efforts and mitigation strategies. Specifically, it was hypothesized that poorer maternal wellbeing, as measured by self-reported maternal mental health status and overall physical health condition, would be associated with greater child ACE exposure. Further, this study hypothesized familial economic hardship would have a direct and indirect effect, through poor maternal wellbeing, on the focal child’s cumulative ACE exposures: the more economic hardships experienced within the familial institution would directly increase ACE exposures; and, increased frequency of economic hardships would decrease maternal wellbeing, thus indirectly increasing the child’s total ACE exposure.
Methods
Data
This study conducted a secondary data analysis on the 2011–2012 National Survey of Children’s Health (NSCH). The 2011–2012 NSCH is a nationally representative, cross-sectional, random-digit-dial telephone survey of United States households with children between the ages of birth and 17 years old. Phone surveys were conducted between February 2011 and June 2012, yielding a total of 95,677 caregiver-completed interviews. The 2011–2012 NSCH collected data from the child’s parent or guardian on the focal child’s emotional and physical health and potential risk factors for child wellbeing. Survey questions included topic areas such as physical health and development, academic performance, household conditions, and wellbeing-related topics such as school experiences, after-school activities, medical issues, medical coverage, familial interactions, parental mental and physical health, and characteristics of their neighborhood. More information regarding sampling technique, study design, and survey questions is available elsewhere (Child and Adolescent Health Measurement Initiative [CAHMI] 2012; CAHMI 2013).
Sample
The 2011–2012 NSCH had a total sample of 95,677 completed caregiver interviews. Due to previous research indicating the nexus between maternal wellbeing and the negative consequences on child health and wellbeing (Kahn et al. 2004), the study’s sample was restricted to mother-respondents only (n = 65,342). Further, in order to account for statistical power, a power analysis was conducted using Sample Power 3 to determine an appropriate sample size for .85 power, alpha value of .05, and beta value of .15. Given the results, a random sample of 4000 participants was pulled from the restricted maternal-caregiver data set to ensure that the findings of the analysis are statistically accurate. The final sample size for this study was 4000 cases.
Measures
In an attempt to differentiate the effects of familial economic hardship and maternal wellbeing on a child’s ACE exposure, this study hypothesized a mediation-like effect would occur between economic hardship and poor maternal wellbeing. It was predicted that poor maternal wellbeing would “transmit” some of the effects of familial economic hardship onto the outcome variable, cumulative ACE exposure (Kline 2011, p.105). As previously mentioned, poor maternal wellbeing was hypothesized to directly affect a child’s cumulative ACE exposure, and that both a direct and indirect effect, via poor maternal wellbeing, would be experienced between economic hardship and cumulative ACE exposure. The outcome variable for this study was cumulative ACE exposure, which was composed of eight separate ACE indicators.
Variables
Poor Maternal Wellbeing
The latent variable poor maternal wellbeing was measured with two items from the 2011–2012 NSCH: overall maternal physical health and maternal mental health status. The NSCH interviewers asked all maternal caregiver-respondents two separate questions concerning their mental/emotional health and their overall physical health, respectively. The questions pertaining to maternal mental/emotional and physical health were used in previous NSCH waves (i.e. 2003 and 2007) (CAHMI 2012; CAHMI 2013), but were not derived from standardized measures. Both questions were scored on a five-point Likert scale: excellent (1), very good (2), good (3), fair (4), and poor (5). Higher scores indicated poorer maternal mental and physical health status. The latent variable poor maternal wellbeing was comprised of two indicators, maternal mental health and maternal physical health. For the purposes of this study, only maternal respondents were included in this study.
Economic Hardship
The 2011–2012 NSCH asked all caregiver-respondents to rate, on a five-point scale, how often they found it difficult to get by on their family income: very often (1), somewhat often (2), rarely (3), never (4). For consistency and interpretability, this variable was reverse coded so that higher scores pertained to children living in families with more economic instability. This study hypothesized perceived familial economic hardship has a direct and indirect effect, through poor maternal wellbeing, on the child’s cumulative ACE exposure.
Exposure to Adverse Childhood Experiences
The outcome variable for this study was cumulative ACE exposure, which was composed of eight separate ACE indicators. The NSCH interviewers asked all caregiver survey respondents to report whether or not the selected child had been exposed to ten adverse childhood experiences (ACEs) at any time throughout the child’s life. The NSCH 2011–2012 assessed for the following ACEs: (1) parental separation or divorce (divorce); (2) loss of a parent (death); (3) parent/guardian served time in jail or prison (incarceration); (4) parental intimate partner violence (IPV); (5) being the victim of, or witness to, neighborhood violence (neighborhood violence); (6) household member with mental illness, was suicidal, or severely depressed (caregiver mental health issues); (7) household member who was an alcoholic or abused substances (caregiver substance abuse issues); (8) judged unfairly due to their race or ethnicity (discrimination); (9) how often the child was treated or judged unfairly; and (10) how often the family had found it difficult to get by on the household income. Table 1 presents the frequencies of ACE exposures and Table 2 presents the sample characteristics and cumulative ACE scores reported by this study’s random sample.
Table 1.
Frequencies of ACE exposure (n = 4000)
| Categorical variables | |
|---|---|
| Adverse childhood experience | Number (valid percent) |
| Parental divorce or separation | |
| Exposure | 693 (18) |
| No exposure | 3275 (82) |
| Death of parent | |
| Exposure | 101 (3) |
| No exposure | 3874 (97) |
| Parental incarceration | |
| Exposure | 193 (5) |
| No exposure | 3777 (95) |
| Parental intimate partner violence | |
| Exposure | 222 (6) |
| No exposure | 3723 (94) |
| Victim/witness of neighborhood violence | |
| Exposure | 273 (7) |
| No exposure | 3687 (93) |
| Parental mental illness or suicide | |
| Exposure | 357 (9) |
| No exposure | 3603 (91) |
| Parental substance abuse | |
| Exposure | 424 (11) |
| No exposure | 3547 (89) |
| Victim of racial/ethnic discrimination | |
| Exposure | 144 (4) |
| No exposure | 3814 (96) |
Table 2.
Characteristics of Study Random Sample (n=4,000)
| Variable Name | ||
| Categorical Variables | Number (Percent) | |
| Child’s Gender | ||
| Male | 2,028 (51) | |
| Female | 1,965 (49) | |
| Child’s Race | ||
| White | 2,603 (65) | |
| Black | 391(10) | |
| Hispanic | 3548 (14) | |
| Multi-Racial/ Other Non-Hispanic | 399 (10) | |
| Variables of Interest | ||
| Mothers Physical Health | ||
| Excellent | ||
| Very Good | 1511 (38) | |
| Good | 943 (23) | |
| Fair | 360 (9) | |
| Poor | 73 (2) | |
| Mothers Mental Health Status | ||
| Excellent | 1308 (33) | |
| Very Good | 1639 (41) | |
| Good | 794 (20) | |
| Fair | 214 (5) | |
| Poor | 32 (1) | |
| Frequency of Economic Hardship | ||
| Very Often | 233 (6) | |
| Somewhat Often | 675 (17) | |
| Not Very Often | 1200 (30) | |
| Never | 1845 (47) | |
| Outcome Variables | ||
| Total Adverse Childhood Experience | ||
| No Exposures | 2,635 (68) | |
| 1 Exposure | 711 (18) | |
| 2 Exposures | 259 (7) | |
| 3 Exposures | 151 (4) | |
| 4 Exposures | 76 (2) | |
| 5 Exposures | 37 (1) | |
| 6 Exposures | 13 (.3) | |
| 7 Exposures | 4 (.1) | |
| Continuous Variables | S.D. | |
| Child’s Age | 8.96 | 5.25 |
| ACE Score | .59 | 1.09 |
For the purposes of this study, only eight of the ten ACEs were included as indicators for the cumulative ACE exposure latent variable. All eight ACE indicators included in the analysis were dichotomous variables measuring exposure (1) or no exposure (0). This study eliminated one ACE item: “how often was your child treated or judged unfairly?” and used the economic hardship ACE as the predictor variable. This study excluded the one ACE variable for two reasons. Unlike the eight ACEs included, the ACE item measuring the frequency of unfair treatment was measured on a four-point Likert scale. Second, this ACE variable was removed due to redundancy with the discrimination ACE indicator. It is important to note that the 2011–2012 NSCH did not survey for several of the most commonly identified ACEs, including child physical abuse, emotional/psychological abuse, sexual abuse, and child physical and/or emotional neglect.
Additionally, no control variables were included in this initial study for three main reasons. First, given the nature of this study and the study objective of providing insight into contextual mechanisms that influence a child’s ACE exposure, the most parsimonious model was selected to examine the fit of the hypothesized model. Researchers argue that structural equation modeling (SEM) is more stringent in parsimonious models since the number of estimated parameters is reduced (Brown 2014; Cheng 2001; Kline 2011). Second, there are several variables that interact with childhood exposure to adversity, caregiver health status, and economic hardships, specifically race/ethnicity. In addition to the goal of parsimony, it was determined by this researcher to not include a dummy coded control variable for the child’s race on the premise that the dichotomized variable would not paint the full picture, rather a subsequent study is underway exploring how a child’s race influences exposure to ACEs. However, it is important to note, this researcher did include a dichotomized child’s race control variable (white [0]; non-white [1]) in previous variations of the hypothesized model; model fit indices indicated a worse fitting model and that child’s race was not statistically significantly associated with a child’s exposure to ACEs. Third, from the ecological transactional model of child maltreatment perspective, this study sought to examine how two contextual variables influenced childhood exposure to adversity, to build the knowledge base and aid theory development; inclusion of an ontogenic control variable would modify the hypothesized model and is outside the scope of this study.
Analysis Plan
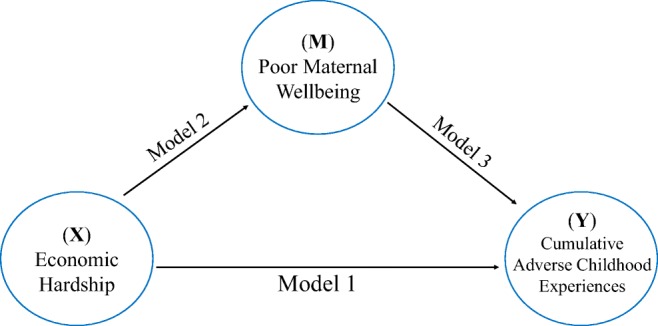
In an attempt to differentiate the effects of familial economic hardship and maternal wellbeing on a child’s ACE exposure, this study hypothesized a mediation-like effect would occur between economic hardship and poor maternal wellbeing. It was proposed that maternal wellbeing would “transmit” some of the effects of familial economic hardship onto the outcome variable, cumulative ACE exposure (Kline 2011, p.105). As previously mentioned, both poor maternal wellbeing was hypothesized to directly effect a child’s cumulative ACE exposure, and that both a direct and indirect effect, via poor maternal wellbeing, would be experienced between economic hardship and cumulative ACE exposure.
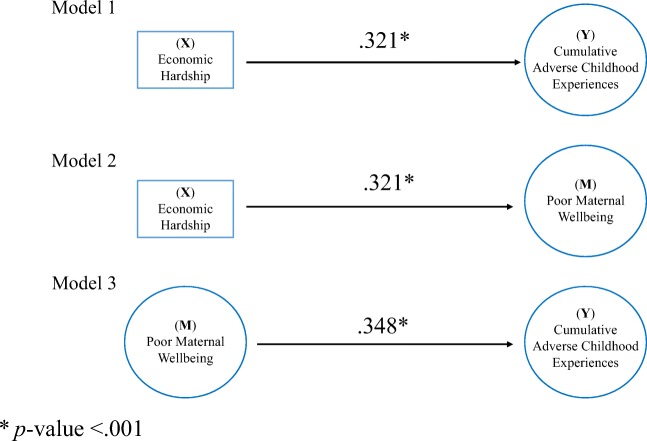
Baron and Kenny’s (1986) seminal article on mediation analyses outlined three empirical conditions required to claim the presence of a mediating effect (Hayes 2017). First, the exogenous (or independent) variable, X, must significantly affect the dependent variable, Y; second, the independent variable, X, must significantly affect the hypothesized mediating variable, M; third, the mediating variable, M, must be significantly related to the outcome (or dependent) variable, Y. If these conditions hold, then the effect of the independent variable, X, on the dependent variable, Y, must diminish when the hypothesized mediator, M, is added to the predicted model (Baron and Kenny 1986; Little et al. 2007). Though, Baron and Kenny’s (1986) clarion guidelines for testing mediation have been valuable to scholars, recent research has revealed these conditions are limited (Cole and Maxwell 2003; Hayes 2009; MacKinnon and Fairchild 2009). Among the critiques, Cole and Maxwell (2003) posit that longitudinal designs enable scholars to examine temporal-precedence and conclude more rigorous inferences about causal-ordering of the respective mediating variables. It is important to note, the overarching goal of this study is to provide a more detailed understanding of the direct and indirect effects of how economic hardship, through maternal wellbeing, is related to a child’s ACE exposure. Given the use of cross-sectional data, full mediation and inferences about temporal-precedence cannot be inferred, rather, this study aims to advance current literature and theoretical development by answering the following research question: How does poor maternal wellbeing effect the association between economic hardship and a child’s exposure to ACEs?
In an attempt to shed light on the direct and indirect effects of the study’s variables, this study was guided by Baron and Kenny’s (1986) conditions for mediation analysis and Little and colleagues (Little et al. 2007). Each of these conditions were tested and confirmed prior to testing the hypothesized model. See Fig. 1 for an illustration of the mediation model conditions and Table 3 for an outline and description of all study models. It is essential to note that this study is not one of moderation where the research question would instead be interested in examining the change in relationship between economic hardship and a child’s cumulative ACE exposure through the interaction of maternal wellbeing and economic hardship (Little et al. 2007).
Fig. 1.
Theory tested through mediation model conditions
Table 3.
Description of study models
| Model # | Model testing conditions |
|---|---|
| Model 1 | Economic Hardship (X) is significantly related to focal child’s Cumulative Adverse Childhood Experiences (Y) |
| Model 2 | Economic Hardship (X) is significantly related to Poor Maternal Wellbeing (M) |
| Model 3 | Poor Maternal Wellbeing (M) is significantly related to focal child’s Cumulative Adverse Childhood Experiences (Y) |
| Model 4 | The relationship between Economic Hardship (X) and Cumulative Adverse Childhood Experiences (Y) significantly diminishes when Poor Maternal Wellbeing (M) is added to model |
| Model 5 | Model 4 with 10,000 Bootstraps |
Using a confirmatory factor analysis (CFA), this study proposed that poor maternal wellbeing would have a mediating-like effect on the association between economic hardship and the focal child’s cumulative ACE exposure. This study used 11 variables and two latent factors to test a CFA measurement model in R Studio version 3.4.2 software. For this study, the variables of interest included the predictor variable, economic hardship, and the intervening variable, poor maternal wellbeing, which was comprised of two indicators: (1) self-reported mental/emotional health status; (2) self-reported overall physical health. The outcome latent variable was cumulative ACE exposure, consisting of eight ACE indicators.
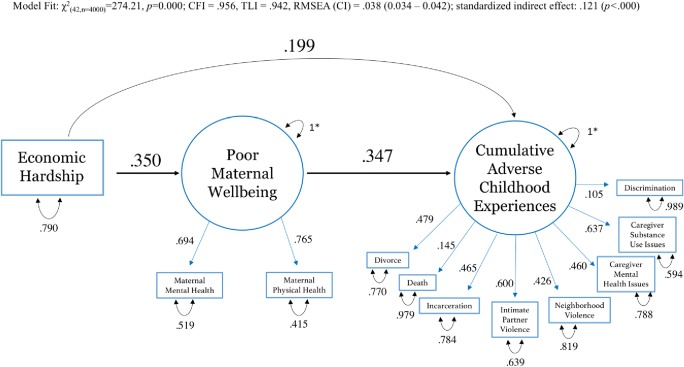
After the initial conditions testing for a mediation-like effect were confirmed, a CFA measurement model was tested to determine the overall fit of the hypothesized model. For identification of the measurement model, fixed factor scaling method was utilized for both latent variables. Goodness of fit statistics including, root mean square error of approximation (RMSEA) (criterion <0.08), Bentler comparative fit index (CFI) (criterion >0.90), and chi-square value and significance, were examined. All indicator loading values were significant at p < .001. The hypothesized measurement model (available upon request) indicated a well-fitting model: χ2(42,n = 4000) = 274.21, p < 0.000; CFI = .956, TLI = .942, RMSEA [90%CI] = .038 [0.034–0.042]. Second, a full and partial structural model were fit to test the direct and indirect relationships. Lastly, the direct and indirect effects were tested using a bootstrapping approach with 10,000 bootstrap samples.
Prior to running the CFA, frequencies and means were run for descriptive purposes on the study’s sample (see Table 1 and Table 2, above). Descriptive statistics and frequencies are also available upon request for the entire 2011–2012 NSCH data set.
Results
Baron and Kenny’s (1986) three empirical conditions were confirmed prior to running the CFA model. All three conditions, detailed above in Table 3 (Models 1–3) were satisfied. Figure 2 presents the standardized regression parameters and Table 4 presents the standardized parameter estimates for the mediation testing conditions. The results indicate that the separate direct relationships between all study variables were significant at a p value of <.001.
Fig. 2.
Standardized regression parameters for mediation testing conditions
Table 4.
Results from testing for meditation conditions
| Model # | χ 2 | df | p | CFI | TLI | RMSEA (90%CI) | R | p |
|---|---|---|---|---|---|---|---|---|
| Model 1: X ➞ Y | 170.12 | 27 | .000 | .957 | .942 | 0.037 (.032–.042) | .321 | .000 |
| Model 2: X ➞ M | 205.49 | 1 | .000 | .888 | .664 | 0.228 (.202–.254) | .321 | .000 |
| Model 3: M➞ Y | 239.52 | 34 | .000 | .955 | .940 | 0.039 (.035–.044) | .348 | .000 |
The CFA measurement model global fit indices indicate the hypothesized model fits the data well [χ2(42,n = 4000) = 274.21, p < .000; CFI = .956, TLI = .942, RMSEA (90%CI) = .038 (0.034–0.042)]. Figure 3, Final Model: 10,000 Bootstraps Results, presents the statistically significant values for all psi, lambda, and theta values. All values for the CFA measurement model were significant at p < .001, further confirming the hypothesized structure.
Fig. 3.
Final model: 10,000 bootstraps results
The second step in the analysis was testing the full and partial structural models resembling the hypothesized relationships between constructs and indicators, determined a priori. Using the fixed factor method, results revealed a well-fitting model. No parameters for the single indicator (economic hardship) were fixed. Both maternal mental health status and maternal physical health status have relatively large loadings on the latent variable poor maternal wellbeing. Of the eight ACE indicators, caregiver substance use issues and exposure to intimate partner violence (IPV) have the largest standardized loadings on the latent variable (respectively, λ = .637, λ = .600, p < .001). Exposure to parental divorce, incarceration, mental health issues, and neighborhood violence have similar loadings on the respective latent variable. Parental death and child exposure to racial or ethnic discrimination had relatively weak loadings of .145 and .105, respectively. All eight ACE indicator loadings were significant at a p value of <.001.
The results of the proposed model testing the differentiating effects of economic hardship and poor maternal wellbeing on the focal child’s cumulative ACE exposure supports the study’s hypotheses. The 10,000 bootstrap model results show that poor maternal wellbeing, as measured by maternal mental and physical health status, has a direct effect (R = .347, p < .001) on the focal child’s ACE exposures (see Table 5). Indicating that children living in households with maternal caregivers who self-report poorer mental and physical health are significantly more likely to have higher cumulative ACE scores. As hypothesized, economic hardship has both a direct (R = .199, p < .001) and indirect effect (R = .118, p < .001) on cumulative ACE exposure. Regression estimates also revealed a significant direct effect between economic hardship and poor maternal wellbeing (R = .350, p < .001). Children living in households with more economic instability are significantly more likely to be exposed to greater adversity. Further, economic hardship has an indirect effect on cumulative ACE exposures via poor maternal wellbeing. The indirect effect reveals that children living in households with greater economic instability are significantly more likely to have a maternal caregiver report poorer maternal wellbeing and to have higher cumulative ACE exposures. Examining the direct effects, poorer maternal wellbeing was a stronger predictor of a child’s cumulative ACE exposure than economic hardships, although both direct effects were statistically significant.
Table 5.
Final 10,000 bootstrap model 5 standardized parameter estimates
| Value | SE | z | p | Std value | |
|---|---|---|---|---|---|
| Direct effect | |||||
| Economic Hardship (EH) ➔ Cumulative ACEs (ACEs) | 0.171 | 0.019 | 8.95 | 0.000 | 0.199 |
| Economic Hardship ➔ Poor Maternal Wellbeing (PMW) | 0.320 | 0.020 | 15.82 | 0.000 | 0.350 |
| Poor Maternal Wellbeing ➔ Cumulative ACEs | 0.370 | 0.031 | 12.08 | 0.000 | 0.347 |
| Indirect effect | |||||
| EH ➔PMW ➔ACEs | 0.118 | 0.012 | 9.76 | 0.000 | 0.121 |
| Total indirect effect (Indirect + Direct) | |||||
| (EH ➔PMW ➔ACEs) + (EH➔ACEs) + (PMW ➔ACEs) | 0.289 | 0.018 | 15.94 | 0.000 | 0.320 |
Lastly, the parameter estimates and confidence intervals from testing the model with 10,000 bootstraps are presented in Table 6. All bootstrapping confidence intervals were significant (i.e. did not include zero). The bootstrapping results support the pattern of a partial mediation-like effect and confirm all direct and indirect effects are statistically significant.
Table 6.
Parameter estimates & bootstrapping confidence intervals
| Value | Lower bound | Upper bound | |
|---|---|---|---|
| Direct effect | |||
| Economic Hardship (EH) ➔ Cumulative ACEs (ACEs) | 0.171 | 0.208 | 0.134 |
| Economic Hardship ➔ Poor Maternal Wellbeing (PMW) | 0.320 | 0.359 | 0.281 |
| Poor Maternal Wellbeing ➔ Cumulative ACEs | 0.370 | 0.431 | 0.309 |
| Indirect effect | |||
| EH ➔PMW ➔ACEs | 0.118 | 0.142 | 0.095 |
| Total indirect effect (Indirect + Direct) | |||
| (EH ➔PMW ➔ACEs) + (EH➔ACEs) + (PMW ➔ACEs) | 0.289 | 0.324 | 0.254 |
Discussion
Despite the ample amount of research focusing on the separate relationships between maternal mental health, economic deprivation, a child’s exposure to adversities, and the negative health and wellbeing outcomes, these fields continue to remain siloed and fragmented. The results of this study help bridge these islands of research by exploring the differentiating effects of familial economic hardship and poor maternal wellbeing on a child’s cumulative ACE exposure. Both economic hardship and poor maternal wellbeing had significant direct effects on a child’s increased ACE exposure. Frequent familial economic hardships significantly predicted poor maternal wellbeing and had a significant indirect effect on cumulative ACE exposure via poor maternal mental health. In other words, children living in households with more economic instability are also more likely to have maternal caregivers with worse mental and physical health status and are significantly more likely to have higher ACE exposures. The results from this study help advance the current understanding of potential contextual determinants that increase a child’s risk for multiple ACE exposures.
A key finding of this study was that poor maternal wellbeing had a stronger direct effect on a child’s cumulative ACE exposure than exposure to economic hardship. This finding suggests maternal caregivers may have a greater influence on a child’s exposure to adversities than potential environmental conditions, such as economic hardship. The direct effect of economic hardship on poor maternal wellbeing was greater than the direct effect on a child’s cumulative ACE exposure. Indicating maternal wellbeing had a mediation-like effect on the relationship between economic hardship and a child’s exposure to adversity. Poor maternal wellbeing was found to transmit some of the effect of economic hardship on a child’s exposure to adversity, as hypothesized. The direct and indirect effects found in this study are supported by Pelton (2015) and advance theory development by providing evidence of the transactional effects of adversities experienced across contexts. Further, this study helps provide insight into the mechanisms that increase a child’s risk for adversity and to where family intervention and prevention efforts should be targeted: towards enhancing and promoting the physical and mental health of caregivers acknowledging the direct relationship between poor caregiver wellbeing and greater ACE exposure for their offspring.
Further, the finding that economic hardship had a greater direct effect on poor maternal wellbeing than a child’s exposure to adversity demonstrates that maternal caregivers and children are not equally impacted by frequent economic hardship. The results from this study illustrate caregivers may buffer their children from—along with transmit—some of the toxic effects associated with increased economic hardship. This finding is congruent with current literature and the ecological transactional perspective that caregiver characteristics and family contexts can serve as both risk and protective factors for the child. Future research should conduct a similar study exploring both research-identified caregiver risk and protective factors (loading on separate latent variables) to identified associations with a child’s ACE exposure. Such a study would advance current empirical and theoretical literature.
Another key finding from this study was the lambda loadings associated with caregiver substance abuse and intimate partner violence (IPV) on the latent outcome variable, cumulative ACE exposure. The combination of these two exposures has robust empirical support. Of the ACEs surveyed, these two adversities may be the most recurrent and outwardly visible to the child compared to other ACE indicators included in this study. Exposures to these two adversities may also create the greatest sense of fear, or perceived fear by the maternal-caregiver respondent, and may also impair caregiving abilities the greatest. Thus, explaining the largest loadings on the cumulative ACE latent variable.
Limitations & Implications
Although the results of this study add to the current empirical research base, there are several noteworthy limitations. First, the ACE variables available in the 2011–2012 NSCH data set excluded important direct exposures commonly identified in the ACE literature (e.g. child physical, emotional, and sexual abuse, and emotional and physical neglect). Eliminating direct victimizations from the list of ACEs surveyed may substantially impact this study’s findings which included eight primarily indirect ACEs (i.e. the child was not the direct victim). Extensive research has documented that direct victimizations, specifically child physical, emotional, and sexual abuse are among the most commonly reported ACEs (Edwards et al. 2003; Felitti et al. 1998; Finkelhor et al. 2007; Finkelhor et al. 2005; Finkelhor et al. 2009).
In the same vein, given the restricted number of ACE variables available in the data set, a limited number of ACE indicators were used for this analysis. In the seminal ACE Study, Felitti and colleagues (1998) identified seven ACEs. However, given the ambiguity of what classifies an ACE (Kalmakis and Chandler 2014), several researchers have identified other traumatic and distressing events that should be recognized as an ACE. Such ACEs include: poverty, episodes of homelessness, parental unemployment, dating violence, witnessing a drug deal, witnessing a parent being arrested, peer violence, victim of bullying, cyber bullying, and living in foster care and/or kinship care (Bramlett and Radel 2014; Sabri et al. 2013; Turner et al. 2006). Future research should examine the direct and indirect effects of economic hardship and maternal wellbeing on a broader variety of adversities, including direct and indirect exposures. Considering a wide array of ACEs is vital to accurately assess and understand not only the developmental implications of childhood exposure levels and the differential effects of certain exposures, but the common combinations of ACEs which may be more likely to cluster (i.e. poverty and caregiver substance use) (Evans 2004).
Limitations pertaining to the utilized data set include the self-report nature of all the study variables and the use of non-standardized measures in the 2011–2012 NSCH. Due to the sensitive nature of the study variables, it is probable that caregiver-respondents answered in a socially desirable manner. Moreover, given the cross-sectional design of the present study, a true full-mediating effect cannot be tested for and causal-ordering of the study variables cannot be inferred since temporal precedence is required to claim mediation. Despite this, the current study adds to the existing literature base by exploring the direct and indirect effects of economic hardship, through poor maternal wellbeing, on a child’s exposure to adversities, providing evidence for future prospective longitudinal studies to explore these differentiating effects, over time, and to assess for a variety of ACEs along with severity and chronicity to better understand the how maternal wellbeing serves as a potential risk and protective intervening variable.
Recognizing the complex interrelatedness of poverty and exposure to other adversities and the negative effects on wellbeing outcomes (Evans 2004), this study sought to examine the differing effects of economic hardship on maternal wellbeing and cumulative ACE exposures. However, the use of the single-indicator variable was limiting in that it only offered self-reported answers on how often the maternal caregiver-respondent perceived economic hardships. Although maternal perception of economic hardships provides insight into environments that may expose children to adversities, future research should look at the association between exposure to ACEs and the family’s economic hardship based on the Federal Poverty Line (FPL) thresholds. Providing some evidence that perceptions of economic hardship may be a better variable to assess poverty, Duncan et al. (1994) have acknowledged that even if a family moves slightly above the FPL, the family may still struggle, without the additional governmental supports, to make any substantial changes that would benefit the child’s development. Accordingly, perceptions of economic hardships may more accurately reflect living conditions for the child because it considers the feasibility of sustainability with the given household income to provide for the household dependents (Waltermaurer et al. 2006). Prospective research should explore the duration and chronicity of poverty experienced by the child and the timing of such economic hardships since research has demonstrated the timing of poverty has varying affects for children across developmental stages (Brooks-Gunn and Duncan 1997; Evans 2004).
Despite the strengths of this study, important variables were missing, such as age of exposure, frequency/chronicity of exposure, education level of the mother, relationship status of the mother, race and ethnic demographics of the child and caregiver, and the time-order of the variables. Coinciding with the ecological-transactional framework, it is possible children with higher ACE exposures may also influence their mother’s overall wellbeing, and that a caregiver’s mental and physical state may directly influence their employment status and parenting practices, thus having a direct and transactional effect on their household income and child’s ACE exposure. Future research should look at additional child, caregiver, and family characteristics may more accurately identify certain populations that might be at highest risk for exposure to multiple ACEs. Additionally, forthcoming research should control for the aforementioned caregiver variables to see if the direct and indirect effects of economic hardship and maternal wellbeing remain.
With regard to the guiding theoretical framework, ecological transactional model of child maltreatment, this study utilized variables at a varying system levels and provides evidence supporting the comorbidity of ACEs and transactional effects of contextual circumstances on a child’s ACE exposure. Aligning with social and direct service professions, and adding significantly to the field of social work, a profession that is centered on the notion of person within their environment, the results support the complex transactional and potentiating relationships between an individual and their environment. Similarly, this study’s findings provide support for broadening the application of the ecological transactional model of child maltreatment to a host of childhood adversities (instead of common forms of child maltreatment) experienced at varying ecological system-levels. Recognizing the complexities of these relationships, researchers and scholars alike should tailor prevention work towards incorporating protective factors across systems levels, through program practice, implementation and policy revision, specifically for families facing several adversities in multiple domains.
Nonetheless, further insights into the direct effects of maternal wellbeing and a child’s cumulative ACE exposure may be more precisely examined through an attachment theory framework or cumulative risk theory. Prospective research should also explore the differentiating effects of poverty and caregiver wellbeing on a child’s exposure across groups of specific system-level exposures (e.g. individual/direct exposures; microsystem/family system exposures; communal/neighborhood exposures). For instance, it is probable that families living in poverty are more likely to live in violent neighborhoods (mesosystem) exposing children to higher rates of crime (Evans 2004), whereas children living in households with poor maternal mental health may be more likely to have exposure to caregiver substance abuse (microsystem). Answering these questions are essential to promoting a comprehensive understanding of the influences and potential contextual determinants of adversities across systems-levels and testing and further developing theoretical frameworks. Greater articulation and integration of ecological risk and protective factors will enhance the comprehension of the mechanisms and social determinants that influence childhood exposure to multiple ACEs.
Further, widespread adversity experienced in several domains decreases the potential of resiliency and, therefore, exposure to multiple ACEs may yield significant toxic effects on the child’s social, behavioral, emotional, and academic development (Turner et al. 2010). Aligning with the ecological transactional framework, fortunately, the inverse is also true: that exposure to multiple positive or protective experiences can have constructive effects and enhance the child’s development and wellbeing (Sege and Browne 2017). However, in order to effectively build upon the strengths within a child’s environment, direct service workers must be aware of the myriad of contextual risk factors and traumatic experiences because such protective effects must be understood within context of the family’s circumstances. The findings from this study support multiple intervention points to help mitigate the negative consequences that research has shown to be related to ACEs. Tailored prevention and intervention efforts should be targeted towards enhancing the mental and physical health of caregivers and assessing for ACE exposure among children, recognizing that improvements in a caregiver’s wellbeing will have compensatory effects on the child’s development, mitigate exposure to ACEs and enrich the caregiver-child relationship.
From a child welfare professional perspective, exposure to multiple ACEs could serve as an additional challenge during the child welfare investigation, family reunification, and/or foster care placements. The more intricately interwoven the ACEs, the more pertinent the need for the social workers and social service professionals to identify compensatory factors. It is critical that practitioners and policymakers alike consider caregiver attributes and the entire family unit within their respective contexts. Practice implications include continued training for direct service providers who work with families receiving social services. Moreover, multidisciplinary teams comprised of nurses, psychologists, social workers, and mental health specialists, and school counselors should work collaboratively to identify the most vulnerable children and families within their communities and advocate for an integrated service delivery system that works to identify contextual and individual adversities and empower families to seek available community resources (Liming and Grube 2018).
Compliance with Ethical Standards
Conflict of Interest
The corresponding author declares no conflict of interest.
Ethical Standards and Informed Consent
For this type of study, secondary data analysis, formal consent is not required. In the original study, the National Survey on Children’s Health (NSCH) 2011–2012, informed consent was obtained from all individual participants included in the study.
References
- Anda, R. F., Felitti, V. J., Bremner, J. D., Walker, J. D., Whitfield, C. H., Perry, B. D., … Giles, W. H. (2006). The enduring effects of abuse and related adverse experiences in childhood. European Archives of Psychiatry and Clinical Neuroscience, 256, 174–186. [DOI] [PMC free article] [PubMed]
- Anderson JC, Gerbing DW. Structural equation modeling in practice: A review and recommended two-step approach. Psychological Bulletin. 1988;103(3):411–423. doi: 10.1037/0033-2909.103.3.411. [DOI] [Google Scholar]
- Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51(6):1173–1182. doi: 10.1037/0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bramlett, M. D., & Radel, L. F. (2014). Adverse family experiences among children in nonparental care, 2011–2012. (Report No. 74). Hyattsville, MD: National Center for Health Statistics. [PubMed]
- Bronfenbrenner U. Toward an experimental ecology of human development. American Psychologist. 1977;32(7):513–531. doi: 10.1037/0003-066X.32.7.513. [DOI] [Google Scholar]
- Brooks-Gunn J, Duncan GJ. The effects of poverty on children. The Future of Children. 1997;7:55–71. doi: 10.2307/1602387. [DOI] [PubMed] [Google Scholar]
- Brown, T. A. (2014). Confirmatory factor analysis for applied research. New York, NY: The Guilford Publications.
- Burke NJ, Hellman JL, Scott BG, Weems CF, Carrion VG. The impact of adverse childhood experiences on an urban pediatric population. Child Abuse & Neglect. 2011;35:408–413. doi: 10.1016/j.chiabu.2011.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bynum, L., Griffin, T., Riding, D. L., Wynkoop, K. S., Anda, R. F., Edwards, V. J., … Croft, J. B. (2010). Adverse childhood experiences reported by adults-five states, 2009. Morbidity and Mortality Weekly Report, 59(49), 1609–1613. [PubMed]
- Cheng EW. SEM being more effective than multiple regression in parsimonious model testing for management development research. Journal of Management Development. 2001;20(7):650–667. doi: 10.1108/02621710110400564. [DOI] [Google Scholar]
- Child and Adolescent Health Measurement Initiative (CAHMI). (2012). 2011/12 National Survey of Children’s health (2012), sampling and survey administration. Data resource center, supported by cooperative agreement 1-U59-MC06980–01 from the U.S. Department of Health and Human Services, Health Resources and Services Administration (HRSA), Maternal and Child Health Bureau (MCHB). Retrieved from www.childhealthdata.org.
- Child and Adolescent Health Measurement Initiative (CAHMI). (2013). 2011-2012 NSCH: Child Health Indicator and Subgroups SAS Codebook, Version 1.0 [data file and code book]. Data resource Center for Child and Adolescent Health. Retrieved from http://www.childhealthdata.org.
- Cicchetti D, Lynch M. Toward an ecological/transactional model of community violence and child maltreatment: Consequences for children’s development. Psychiatry. 1993;56(1):96–118. doi: 10.1080/00332747.1993.11024624. [DOI] [PubMed] [Google Scholar]
- Cicchetti, D., Toth, S. L., & Maughan, A. (2000). An ecological-transactional model of child maltreatment. In A. J. Sameroff, M. Lewis, & S. M. Miller (Eds.), Handbook of Developmental Psychopathology (pp. 689–722). New York, NY: Springer US.
- Cole DA, Maxwell SE. Testing mediational models with longitudinal data: Questions and tips in the use of structural equation modeling. Journal of Abnormal Psychology. 2003;112(4):558–577. doi: 10.1037/0021-843X.112.4.558. [DOI] [PubMed] [Google Scholar]
- Dong, M., Anda, R. F., Felitti, V. J., Dube, S. R., Williamson, D. F., Thompson, T. J., … Giles, W. H. (2004). The interrelatedness of multiple forms of childhood abuse, neglect, and household dysfunction. Child Abuse & Neglect, 28(7), 771–784. 10.1016/j.chiabu.2004.01.008 [DOI] [PubMed]
- Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, Giles WH. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: Findings from the adverse childhood experiences study. JAMA. 2001;286:3089–3096. doi: 10.1001/jama.286.24.3089. [DOI] [PubMed] [Google Scholar]
- Dube SR, Felitti VJ, Dong M, Chapman DP, Giles WH, Anda RF. Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: The adverse childhood experiences study. Pediatrics. 2003;111(3):564–572. doi: 10.1542/peds.111.3.564. [DOI] [PubMed] [Google Scholar]
- Dube SR, Fairweather D, Pearson WS, Felitti VJ, Anda RF, Croft JB. Cumulative childhood stress and autoimmune diseases in adults. Psychosomatic Medicine; Baltimore. 2009;71:243–250. doi: 10.1097/PSY.0b013e3181907888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan GJ, Brooks-Gunn J, Klebanov PK. Economic deprivation and early childhood development. Child Development. 1994;65(2):296–318. doi: 10.2307/1131385. [DOI] [PubMed] [Google Scholar]
- Edwards VJ, Holden GW, Felitti VJ, Anda RF. Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: Results from the adverse childhood experiences study. American Journal of Psychiatry. 2003;160(8):1453–1460. doi: 10.1176/appi.ajp.160.8.1453. [DOI] [PubMed] [Google Scholar]
- Evans GW. The environment of childhood poverty. American Psychologist. 2004;59(2):77–92. doi: 10.1037/0003-066X.59.2.77. [DOI] [PubMed] [Google Scholar]
- Evans GW, Kim P. Childhood poverty, chronic stress, self-regulation, and coping. Child Development Perspectives. 2013;7:43–48. doi: 10.1111/cdep.12013. [DOI] [Google Scholar]
- Fang X, Brown DS, Florence CS, Mercy JA. The economic burden of child maltreatment in the United States and implications for prevention. Child Abuse & Neglect. 2012;36:156–165. doi: 10.1016/j.chiabu.2011.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., … Marks, J. S. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences (ACE) study. American Journal of Preventive Medicine, 14, 245–258. [DOI] [PubMed]
- Finkelhor D, Ormrod R, Turner H, Hamby SL. The victimization of children and youth: A comprehensive, national survey. Child Maltreatment. 2005;10:5–25. doi: 10.1177/1077559504271287. [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Ormrod RK, Turner HA. Poly-victimization: A neglected component in child victimization. Child Abuse & Neglect. 2007;31:7–26. doi: 10.1016/j.chiabu.2006.06.008. [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Ormrod R, Turner H, Holt M. Pathways to poly-victimization. Child Maltreatment. 2009;14:316–329. doi: 10.1177/1077559509347012. [DOI] [PubMed] [Google Scholar]
- Finkelhor, D., Turner, H., Hamby, S. L., & Ormrod, R. (2011). Polyvictimization: children’s exposure to multiple types of violence, crime, and abuse. OJJDP Juvenile Justice Bulletin - NCJ235504 (pgs. 1-12). Washington, DC: US Government Printing Office.
- Folger AT, Eismann EA, Stephenson NB, Shapiro RA, Macaluso M, Brownrigg ME, Gillespie RJ. Parental adverse childhood experiences and offspring development at 2 years of age. Pediatrics. 2018;141:e20172826. doi: 10.1542/peds.2017-2826. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, Heyward D. Maternal depression and child psychopathology: A meta-analytic review. Clinical Child and Family Psychology Review. 2011;14:1–27. doi: 10.1007/s10567-010-0080-1. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Beyond baron and Kenny: Statistical mediation analysis in the new millennium. Communication Monographs. 2009;76(4):408–420. doi: 10.1080/03637750903310360. [DOI] [Google Scholar]
- Hayes, A. F. (2017). Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. New York, NY: Guilford Publications.
- Herman DB, Susser ES, Struening EL, Link BL. Adverse childhood experiences: Are they risk factors for adult homelessness? American Journal of Public Health. 1997;87:249–255. doi: 10.2105/AJPH.87.2.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hillis SD, Anda RF, Dube SR, Felitti VJ, Marchbanks PA, Marks JS. The association between adverse childhood experiences and adolescent pregnancy, long-term psychosocial consequences, and fetal death. Pediatrics. 2004;113:320–327. doi: 10.1542/peds.113.2.320. [DOI] [PubMed] [Google Scholar]
- Kahn RS, Wise PH, Kennedy BP, Kawachi I. State income inequality, household income, and maternal mental and physical health: Cross sectional national survey. BMJ [British Medical Journal] 2000;321:1311–1315. doi: 10.1136/bmj.321.7272.1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahn RS, Brandt D, Whitaker RC. Combined effect of mothers’ and fathers’ mental health symptoms on children’s behavioral and emotional well-being. Archives of Pediatrics & Adolescent Medicine. 2004;158:721–729. doi: 10.1001/archpedi.158.8.721. [DOI] [PubMed] [Google Scholar]
- Kalmakis KA, Chandler GE. Adverse childhood experiences: Towards a clear conceptual meaning. Journal of Advanced Nursing. 2014;70(7):1489–1501. doi: 10.1111/jan.12329. [DOI] [PubMed] [Google Scholar]
- Kerker, B. D., Zhang, J., Nadeem, E., Stein, R. E. K., Hurlburt, M. S., Heneghan, A., … Horwitz, S. M. (2015). Adverse childhood experiences and mental health, chronic medical conditions, and development in young children. Academic Pediatrics, 15, 510–517. [DOI] [PMC free article] [PubMed]
- Kline RB. Principles and practice of structural equation modeling. 3. New York: Guilford Press; 2011. [Google Scholar]
- Liming, K. W., & Grube, W. A. (2018). Wellbeing outcomes for children exposed to multiple adverse experiences in early childhood: a systematic review. Child and Adolescent Social Work Journal, 32, 1–19. 10.1007/s10560-018-0532-x.
- Little, T. D. (2013). Longitudinal structural equation modeling. New York, NY: Guilford Press.
- Little, T. D., Card, N. A., Bovaird, J. A., Preacher, K. J., & Crandall, C. S. (2007). Structural equation modeling of mediation and moderation with contextual factors. In T. D. Little, J. A. Bovaird, & N. A. Card (Eds.), Modeling contextual effects in longitudinal studies (pp. 207–230). Mahwah, NJ, US: Lawrence Erlbaum Associates Publishers.
- Liu Y, Croft JB, Chapman DP, Perry GS, Greenlund KJ, Zhao G, Edwards VJ. Relationship between adverse childhood experiences and unemployment among adults from five US states. Social Psychiatry and Psychiatric Epidemiology. 2013;48(3):357–369. doi: 10.1007/s00127-012-0554-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Fairchild AJ. Current directions in mediation analysis. Current Directions in Psychological Science. 2009;18(1):16–20. doi: 10.1111/j.1467-8721.2009.01598.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy NA, Christian B, Caplin DA, Young PC. The health of caregivers for children with disabilities: Caregiver perspectives. Child: Care, Health and Development. 2007;33:180–187. doi: 10.1111/j.1365-2214.2006.00644.x. [DOI] [PubMed] [Google Scholar]
- Pelton LH. The continuing role of material factors in child maltreatment and placement. Child Abuse & Neglect. 2015;41:30–39. doi: 10.1016/j.chiabu.2014.08.001. [DOI] [PubMed] [Google Scholar]
- Petterson SM, Albers AB. Effects of poverty and maternal depression on early child development. Child Development. 2001;72:1794–1813. doi: 10.1111/1467-8624.00379. [DOI] [PubMed] [Google Scholar]
- Prince M, Patel V, Saxena S, Maj M, Maselko J, Phillips MR, Rahman A. No health without mental health. The Lancet. 2007;370:859–877. doi: 10.1016/S0140-6736(07)61238-0. [DOI] [PubMed] [Google Scholar]
- Sabri B, Hong JS, Campbell JC, Cho H. Understanding children and adolescents’ victimizations at multiple levels: An ecological review of the literature. Journal of Social Service Research. 2013;39:322–334. doi: 10.1080/01488376.2013.769835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sege RD, Browne CH. Responding to ACEs with HOPE: Health outcomes from positive experiences. Academic Pediatrics. 2017;17(7):S79–S85. doi: 10.1016/j.acap.2017.03.007. [DOI] [PubMed] [Google Scholar]
- Spence SH, Najman JM, Bor W, O’callaghan MJ, Williams GM. Maternal anxiety and depression, poverty and marital relationship factors during early childhood as predictors of anxiety and depressive symptoms in adolescence. Journal of Child Psychology and Psychiatry. 2002;43:457–469. doi: 10.1111/1469-7610.00037. [DOI] [PubMed] [Google Scholar]
- Spieker SJ, Larson NC, Lewis SM, Keller TE, Gilchrist L. Developmental trajectories of disruptive behavior problems in preschool children of adolescent mothers. Child Development. 1999;70:443–458. doi: 10.1111/1467-8624.00032. [DOI] [PubMed] [Google Scholar]
- Turner HA, Finkelhor D, Ormrod R. The effect of lifetime victimization on the mental health of children and adolescents. Social Science & Medicine. 2006;62:13–27. doi: 10.1016/j.socscimed.2005.05.030. [DOI] [PubMed] [Google Scholar]
- Turner HA, Finkelhor D, Ormrod R. Poly-victimization in a national sample of children and youth. American Journal of Preventive Medicine. 2010;38:323–330. doi: 10.1016/j.amepre.2009.11.012. [DOI] [PubMed] [Google Scholar]
- Waltermaurer E, Watson CA, McNutt LA. Black women's health: The effect of perceived racism and intimate partner violence. Violence Against Women. 2006;12:1214–1222. doi: 10.1177/1077801206293545. [DOI] [PubMed] [Google Scholar]