Abstract
Preliminary evidence supports a possible association between post-traumatic stress disorder (PTSD) and sensory modulation disorder (SMD). Nevertheless, the research focusing on this relationship in children is notably limited. This study examined children with and without PTS symptoms, by comparing their mothers’ perceptions of their responses to sensory events in daily life. Mothers of 134 non-referred children aged 5–11, exposed to continuous traumatic stress due to political violence, completed the UCLA-RI and the Short Sensory Profile questionnaires. Significant differences emerged between children with different levels of PTS symptoms in various sensory modalities. Furthermore, half of the symptomatic children had suspected clinically significant deficits in sensory processing. In addition, PTSD symptoms were significantly associated with most of the sensory processing scores. Logistic regression indicated that the overall sensory processing score was a significant predictor of group classification. The results indicate that children with PTS symptoms may be at increased risk for sensory processing deficits. Evaluation of sensory processing should be incorporated into the routine evaluation of this population in order to determine whether this is an additional factor contributing to a child’s difficulties in participating in daily activities. Subsequent intervention programs should then address the multiple needs of these children.
Keywords: Post-traumatic stress disorder, Sensory processing, Sensory profile, Regulation, Hyperarousal
Individuals differ in their responses to sensations with respect to the type, intensity, and affective tone displayed (Ben-Sasson et al. 2009). These typical individual differences influence peoples’ interest in, tolerance for, and pleasure derived from sensations, which in turn affect their behavior and life choices (Dunn 2001). However, persons with sensory modulation disorder (SMD) experience more pervasive and clinically aberrant responses to sensory input, to an extent that profoundly interferes with their participation in daily activities (Bar-Shalita et al. 2008) and quality of life (Kinnealey et al. 2011).
Sensory modulation disorder, a subtype of sensory processing disorder (SPD), is a disorder of the regulatory component of sensory processing; it is expressed as sensory over-responsivity (SOR) and/or under-responsivity (SUR) to one or more types of sensory stimuli (Miller et al. 2007). Individuals with SOR experience sensations more intensely and for longer durations, resulting in increased arousal levels. These individuals experience otherwise benign sensations as unpleasant, distracting, or even painful. They react with a fight/flight response, manifested as exaggerated avoidant and defensive behaviors that are out of sync with the environmental demands (Miller et al. 2007; Schaaf et al. 2003). In contrast, individuals with SUR have a delayed or decreased response to various sensations, resulting in reduced arousal levels, and leading to characteristics such as passive behavior and a seeming lack of interest or motivation to initiate socialization and exploration (Miller et al. 2007).
Sensory modulation disorder is prevalent in 5–16% of typically developing children (Ahn et al. 2004; Ben-Sasson et al. 2009; Gouze et al. 2009). Although SMD can be evident without the presence of other deficits (Miller et al. 2012; Yochman et al. 2013), research increasingly indicates extremely elevated rates of SMD in an array of psychiatric disorders (Ben-Sasson and Podoly 2017; Dar et al. 2012; Lewin et al. 2015; Lipskaya-Velikovsky et al. 2015; Reynolds and Lane 2009), including post-traumatic stress disorder (PTSD) (Engel-Yeger et al. 2013).
The Diagnostic and Statistical Manual of Mental Disorders (DSM-5; American Psychiatric Association 2013) classifies PTSD under trauma and stressor-related disorders. A diagnosis of PTSD requires the person to have experienced, witnessed, or learned of a traumatic event. Thus for example, studies indicate that children exposed to continuous political violence are at high risk of suffering from full or partial post-traumatic stress symptoms (Karr 2009; Wolmer et al. 2015).
It is noteworthy that in most cases, resilience to trauma is more common than PTSD in children and adolescents as well as in adults (Bonanno 2004; Lacoviello and Charney 2014; Masten 2001). The risk of developing PTSD after exposure to a traumatic event depends on a complex interaction between risk and protective factors (Pat-Horenczyk et al. 2009a). These factors operate at many levels and include the individual’s determinants, attributes of the child’s family, as well as characteristics of the individual’s larger social and cultural environment (Betancourt and Khan 2008; Nugent et al. 2014; Pat-Horenczyk et al. 2017).
Thus, PTSD is defined not only by its presumed cause, but also by meeting the requirements of all four symptom clusters that characterize the disorder: re-experiencing of the traumatic event, avoidance of trauma-related stimuli, negative thoughts and/or emotions, and increased arousal and reactivity (American Psychiatric Association 2013). Although not having been fully subsumed under the DSM-5’s hyperarousal symptom cluster, a disruption of sensory processing frequently accompanies the described dysregulatory state in PTSD, causing common behavioral characteristics like those found in individuals with SMD. Similar to SMD-SOR, people with PTSD frequently complain of increased hypervigilance and hypersensitivity to a broad range of everyday stimuli, over and beyond trauma-related or threatening cues (Ehlers and Clark 2000; Hayes et al. 2012; Stewart and White 2008).
Several hypotheses can be advanced to explain the possible mechanisms that may contribute to the co-occurrence of PTSD and SMD. Firstly, trauma-originated excessive stimulation of the central nervous system (CNS) has been shown to cause permanent neural changes that impede habituation to sensory stimuli, both related and unrelated to the original trauma. CNS hypo-habituation may essentially express itself as secondary SMD-SOR symptoms (Van der Kolk 2006; Warner et al. 2013).
A second possibility suggests that premorbid SMD may be a risk factor for developing psychopathology, and inter alia, PTSD (Levit-Binnun and Golland 2012). Thus, hypersensitivity and exaggerated pain perception (Bar-Shalita et al. 2014; Meredith et al. 2015), anxiety (Green and Ben-Sasson 2010; Lane et al. 2012; Levit-Binnun et al. 2014; Reynolds and Lane 2009), and reduced resilience (Dean et al. 2018) are all found to be characteristic of individuals with SMD. These may significantly lead to amplification of the traumatic experience, as well as reduce the probability of resolving the trauma experience, thus increasing the risk of developing PTSD (Trickey et al. 2012).
In addition, it could be argued that these coexisting disorders may share a common cause. Thus, for example, inadequate executive resources are likely to further contribute to a mutually driven perpetuation of CNS dysfunction. Studies of both intrinsic visual cortical activity and bottom-up sensory-driven causal connectivity in PTSD (Clancy et al. 2017) and multisensory integration (MSI) in SMD (Brett-Green et al. 2008, 2010) cite excessive frontal activation, likely to be recruited in an effort to manage the core lower-level dysregulatory symptoms of the two disorders. The added strain placed on the executive resources in the case of co-occurring SMD and PTSD is likely to cause a further drop in the higher-level self-regulatory capacity of the lower-level hyperstimulation.
Since a number of factors may contribute to the interplay between SMD and PTSD, it is likely that these relationships cannot adequately be explained by any single cause; nor does it follow that these hypotheses are mutually exclusive. Despite the evidence lending support to the possible coexistence of these disorders, limited research has focused on this issue. Most research regarding the sensory processing abilities of individuals with PTSD has focused on understanding basic fundamental physiological processes of abnormal sensory function, usually isolated to one sensory modality (mainly auditory and visual) (Ghisolfi et al. 2004; Holstein et al. 2010; Karl et al. 2006; McFarlane et al. 1993; Shalev et al. 2000; Stewart and White 2008). Extremely limited research has focused on assessing behavioral responses to sensory stimuli from multiple sensory modalities in everyday life situations (Bailliard and Whigham 2017). One such study was conducted by Engel-Yeger et al. (2013), who focused on the sensory profile of adults with PTS symptoms using the Adolescent/Adult Sensory Profile questionnaire (Brown and Dunn 2002). They found significantly greater tendencies for sensory sensitivity, sensation avoidance, low registration, and a lower tendency for sensory seeking in individuals with PTS compared to typical adults. Furthermore, discriminant analysis predicted group classification of 73% of the study group and 80% of the controls, thus further confirming the unique sensory profile of this population.
In an additional study, sensory processing difficulties were found to possibly impede adults with PTS in forming intimate relationships (Engel-Yeger et al. 2015). Muffly and Gerney (2015) focused on a specific trauma among woman who had been sexually assaulted, finding unique patterns of sensory processing, specifically with regard to touch while engaging in everyday occupations.
With regard to the pediatric population, Atchison (2007) reported that based on data obtained from the Sensory Profile questionnaire administered to 900 children referred to a trauma assessment center, more than half of the children demonstrated symptoms of SMD, with 35% of them scoring two standard deviations (SDs) below the mean. Thus, despite the limited empirical literature indicating the possibility of sensory modulation dysfunction among individuals with PTS symptoms, to our knowledge no research has examined this relationship in children.
The objectives of the present study were to (1) compare the sensory profiles of non-referred children, aged 5–11, with and without PTS symptoms; (2) examine the correlation between the severity of PTS symptoms and sensory processing abilities; and (3) identify whether the sensory profile measure can predict group classification of children with and without PTS symptoms.
Methods
Participants
The sample consisted of 134 Israeli mothers of children aged 7–11 years (mean age = 9.1 years; SD = 1.0) who were exposed to continuous traumatic stress. Inclusion criteria were: (a) a caregiver fluent in Hebrew; (b) residents of Sderot, an Israeli city adjacent to the Gaza Strip, which at the time of the study had been exposed to repeated missile attacks for over a decade; (c) children with no history of any clearly defined developmental disorder, physical, sensory, or neurological deficit. Three subgroups were created based on the scores of the University of California-Los Angeles Reaction Index questionnaire (UCLA-RI): 16 children defined with full PTS symptoms, 54 children with partial PTS symptoms, and 64 children without symptoms of PTS (See Table 1).
Table 1.
Demographics and levels of post-traumatic symptoms (N = 134)
| N = 134 | Mean (SD) | % (N) | |
|---|---|---|---|
| Gender | Boy | 44.8% (60) | |
| Girl | 55.2% (74) | ||
| Age | 9.1 (1.0) | ||
| Mother’s Education | Elementary school | 7.5% (10) | |
| High School | 34.3% (46) | ||
| Professional | 13.4% (18) | ||
| Academic | 44.8% (60) | ||
| Post-traumatic Symptoms | 17.0 (12.3) | ||
| No PTSD | 47.8% (64) | ||
| Partial PTSD | 40.3% (54) | ||
| Full PTSD | 11.9% (16) |
Setting and Procedure
This study is part of a larger longitudinal study aimed at studying the impact of continuous traumatic stress and exposure to prolonged political violence on children living in Sderot, an Israeli city exposed to numerous recurrent missile attacks. In addition to the physical injuries and loss of lives, the psychological, social, and economic impact on the population has been vast. Previous studies have documented a high rate of psychological distress – especially PTSD – among those exposed to political violence on both sides of the Israeli-Palestinian conflict (Barron and Abdallah 2015; Pat-Horenczyk et al. 2009b, 2013).
In the first phase of the study, 255 children aged 2–5 years were assessed, after their parents signed a consent form agreeing to future contact for further assessment. In the current follow-up study, 64% of the initial sample were reassessed when the children were 7–11 years old. The remaining parents of the original sample did not participate, mainly because the families no longer lived in the area or were not located. Four families explicitly refused to participate.
Families were contacted by phone in order to explain the aim of the study. Interested families who met the inclusion criteria were scheduled for an in-home visit. By means of a structured face-to-face interview, trained research assistants administered a variety of questionnaires to the mothers, including the UCLA and Sensory Profile questionnaires. Except for unclear words that were clarified, no mediation was provided. Before the interview, informed consent was obtained by both mother and child. Each family received a gift voucher in appreciation for their participation in the study.
Measures
Demographics
A short questionnaire was designed for this study, including items regarding demographic status, as well as medical and developmental information about the child.
Exposure to Traumatic Events
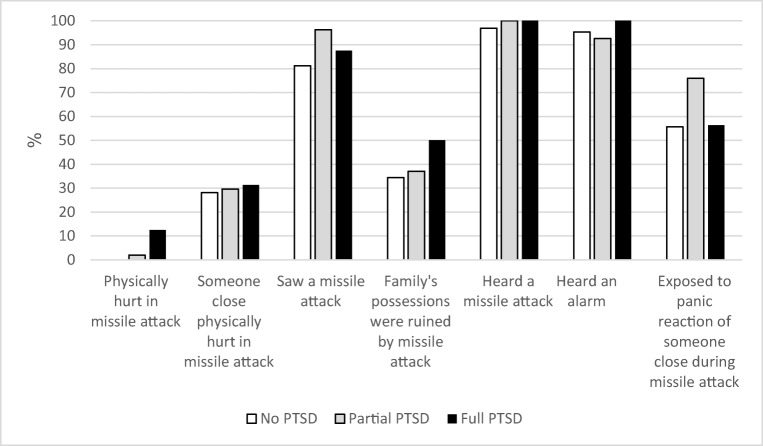
The type and intensity of exposure to political violence was measured by a questionnaire developed for this specific psycho-political context, which has been used in prior studies (Pat-Horenczyk 2004; Pat-Horenczyk et al. 2013). The eight items on the questionnaire represent various forms of exposure to missile attacks, and how many times these exposures occurred (never, once, twice, three times, more than three times). For each item respondents answer “yes” or “no” to whether their child experienced this type of traumatic event. Because it was impossible to obtain reliable reports on the exact number of events, we calculated only the number of separate types of events the child experienced, and this measure was used as the total score for exposure (See Fig. 1).
Fig. 1.
Percent of Children Exposed to Different Aspects of Missile Attacks According to Child’s PTS Symptom Levels
UCLA Reaction Index
The UCLA-RI (Steinberg et al. 2004) is among the most widely used research tools for measuring child PTSD symptoms. The measure consists of two components: a trauma exposure section and a PTSD symptom scale. This study used the PTSD symptom scale only, since trauma exposure was assessed by the more specific above-mentioned questionnaire. The PTSD symptom scale is comprised of 22 items, based on the DSM-4 (American Psychiatric Association 1994), and rated on a 5-point Likert-type scale (0 = none to 4 = very often). The total PTSD severity score is a sum total of all items. In addition, score sums were calculated for three categories of symptom clusters derived from the DSM-4: intrusive symptoms (criterion B), avoidance symptoms (criterion C), and hyperarousal symptoms (criterion D). For each category the score obtained can indicate whether the child’s functioning is within the norm. Symptoms were classified as full PTSS when deficit scores were obtained in all three categories. Partial PTSS was assigned when deficit scores emerged in two out of the three, and no PTSS when no deficit scores were obtained. In addition, the criteria of exposure to the traumatic event had to be met.
In published studies, alpha coefficients of the UCLA-RI have demonstrated high internal consistency (0.90–0.85) and good test-retest reliability at 0.84 (Roussos et al. 2005). The questionnaire demonstrates acceptable convergent validity when compared to similar measures (Steinberg et al. 2004). The present study found Cronbach’s alpha to be well within acceptable limits (0.83).
Short Sensory Profile
The SSP (McIntosh et al. 1999a) is a 38-item caregiver questionnaire that provides a standard measure of a child’s sensory processing patterns in the context of everyday life. The SSP includes those items that demonstrate the highest discriminative power of atypical sensory processing among all the items from the long version of the Sensory Profile. Research indicates that due to its value in screening for atypical sensory processing, the SSP is recommended for research protocols (McIntosh et al. 1999b). The seven sections of the SSP are: tactile sensitivity (7 items), movement sensitivity (3 items), taste / smell sensitivity (4 items), under-responsive / seeks sensation (7 items), auditory filtering (6 items), visual / auditory sensitivity (5 items), and low energy / weak (6 items). Items are scored on a 5-point Likert scale measuring frequency of behaviors. Section scores and a total score are recorded, with higher scores (155–190) reflecting typical performance, a score of 142–154 reflecting a probable difference in sensory processing (1.5 SD below the mean of typically developing children, according to manual norms), and a score of 38–141 reflecting a definite difference (2 SDs below the mean). Internal consistency of the sections ranged from 0.70 to 0.90, and construct validity has been demonstrated through the known-group procedure as well as factor analysis, used to examine the intercorrelations of the SSP total and section scores (range r = 0.25–0.76) (McIntosh et al. 1999a).
In addition, construct validity has been further analyzed using electrodermal response testing, which has shown that low scorers on electrodermal response have significantly lower scores on the SSP (McIntosh et al. 1999b). The Hebrew version of the SSP was found to have good psychometric properties (Engel-Yeger 2010). The analysis of internal reliability coefficients for the present study revealed that the total score and all section scores were above 0.8, apart from “tactile sensitivity”, which was 0.634.
Results
Descriptive Statistics
Table 1 contains the demographics and levels of post-traumatic symptoms of 134 children, ranging from 7 to 11 years old. Forty-five percent of the children’s mothers have an academic education, and 34% of the mothers have a high school diploma. Fifty-two percent of the children suffered from partial or full PTS symptoms. All of the children were exposed to some aspect of missile attacks (see Fig. 1).
Comparison of Group Scores on SSP Sections
Statistical analysis was performed using SPSS 25.0. The results of the multivariate analysis of variance (MANOVA) revealed a significant group effect on the combined dependent variables (F(14, 250) = 3.88, p < .001, η2 = 0.179). Follow-up univariate ANOVAs showed that all sections, excluding Taste/Smell Sensitivity, were significantly different in children with various levels of PTS symptoms (See Table 2). Follow-up with a post-hoc Tukey’s test indicated that the scores for children with full PTS symptoms were significantly lower than for the children with no PTS symptoms; this applied to total scores and all sections scores, excluding Taste/Smell Sensitivity. The effect sizes found for these results were moderate to high, with the highest for the tactile system (η2 = 0.164). There were also significant differences between children with partial vs. full PTSD in the total scores, tactile scores, and under-responsive scores, where sensory modulation scores were lower for children with full PTSD.
Table 2.
Comparison of the SSP total and section scores among children with no, partial and full PTS symptoms
| No PTSD (n = 64) | Partial PTSD (n = 53) | Full PTSD (n = 17) | Test of Differences | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensory Regulation | M | SD | M | SD | M | SD | df1 | df2 | F | η2 | Post Hoc Tests |
| Total | 168.14 | 18.88 | 158.68 | 17.01 | 142.82 | 18.99 | 14 | 250 | 3.88*** | 0.179 | N > P > F |
| Tactile | 32.39 | 3.25 | 31.66 | 3.33 | 27.41 | 4.09 | 2 | 131 | 12.82*** | 0.164 | N = P > F |
| Taste/Smell Sensitivity | 17.16 | 3.52 | 16.42 | 3.93 | 16.59 | 3.22 | 2 | 131 | 0.72 | 0.011 | |
| Movement | 13.36 | 2.60 | 12.45 | 2.95 | 10.71 | 3.57 | 2 | 131 | 6.15** | 0.086 | N > F |
| Under-responsive | 30.09 | 5.14 | 29.64 | 4.90 | 25.00 | 6.27 | 2 | 131 | 4.56** | 0.065 | N = P > F |
| Auditory Filtering | 24.16 | 4.94 | 20.96 | 6.31 | 18.82 | 4.54 | 2 | 131 | 9.38*** | 0.125 | N > P = F |
| Low Energy/Weak | 28.17 | 4.03 | 26.53 | 4.65 | 25.94 | 5.84 | 2 | 131 | 4.61* | 0.066 | N > P = F |
| Visual Auditory Sensitivity | 22.81 | 3.01 | 21.02 | 3.92 | 18.35 | 5.07 | 2 | 131 | 10.19*** | 0.135 | N > P = F |
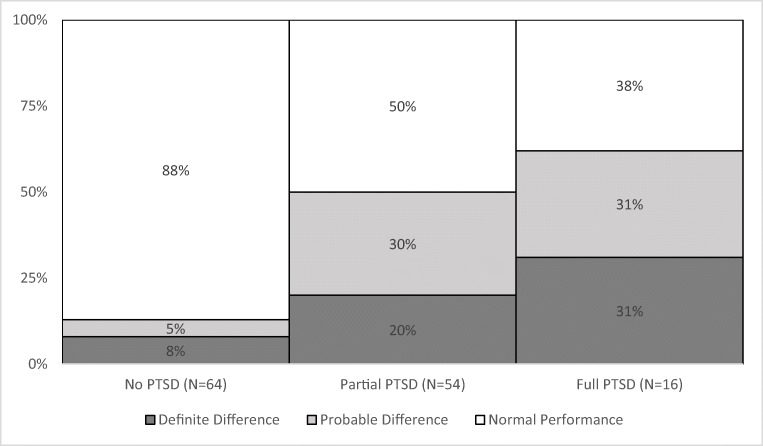
In addition, the percentage of children classified with suspected clinically significant deficits according to SSP manual norms was calculated, and Fisher’s exact test was used to examine the dependency between PTSS and sensory processing. More than half of the children (51%) with full or partial PTS symptoms exhibited definite differences in sensory processing, as opposed to 8% of the children with no PTS symptoms (see Fig. 2). There was a statistically significant association between sensory processing deficits and PTS levels as assessed by Fisher’s exact test: p < .001.
Fig. 2.
Percent of Children with and without PTS Symptoms with SSP Total Score below the Cutoff Point
Correlation Analysis
Pearson correlation analysis between the level of PTS symptoms and scores of sensory processing yielded significant negative low to moderate correlations on all sections, excluding Taste/Smell Sensitivity (see Table 3). The highest correlations were between the total and auditory filtering sensory scores and the post-traumatic symptoms. These results suggest that children who suffer from high PTS symptoms are more likely to have more impaired sensory processing.
Table 3.
Correlations between SSP total and section scores and UCLA-RI scores of post-traumatic symptoms (n = 127)
| Sensory regulation | Posttraumatic symptoms |
|---|---|
| Total | −.477*** |
| Tactile | −.305*** |
| Taste\Smell Sensitivity | −.004 |
| Movement | −.340*** |
| Under-responsive | −.261** |
| Auditory Filtering | −.459*** |
| Low Energy/Weak | −.274** |
| Visual Auditory Sensitivity | −.442*** |
*** p < 0.001, ** p < 0.01
PTS symptoms - higher scores represent greater dysfunction. Sensory processing symptoms - lower scores represent greater dysfunction
Logistic Regression Analysis
Finally, a binomial logistic regression analysis was performed to ascertain the effects of sensory processing abilities on post-traumatic symptoms. The results indicated that decreased sensory processing abilities were associated with an increased likelihood of exhibiting post-traumatic symptoms among children (Odds Ratio = 0.953, R2 = .199, Χ2(1) = 21.640, p < .001).
Discussion
In view of the importance of sensory processing to functioning, this study compared mothers’ perceptions of the responses of their children, with and without PTS symptoms, to sensory events in daily life. To our best knowledge, this association has scarcely been addressed in children. Our findings further reinforce the association between PTS symptoms and sensory modulation dysfunction, specifically in children exposed to continuous traumatic stress. The results show that children with PTS symptoms performed significantly worse in the majority of the SSP section scores compared to children without PTS symptoms. Moreover, the moderate to large effect sizes found for these results suggest that the differences between the groups can be meaningful for application to clinical practice. Since we examined PTS symptoms dimensionally rather than categorically, our findings also indicate that the level of PTS symptoms may predict the degree of sensory modulation difficulties in children. Furthermore, given that over half of the symptomatic children had suspected clinically significant deficits, it appears that co-occurring sensory modulation deficits are not a marginal phenomenon; therefore, they need to be at the center of our clinical attention.
Our results also show that a substantial number of children with PTS symptoms scored within normal ranges of sensory processing. This variability emphasizes the importance of relating to the individual child and not only to the characteristics of a group. With regard to these prevalence rates, our sample was unique in that it compared children with and without PTS symptoms who were all exposed to the same trauma of missile attacks. In the group of children without post-traumatic symptoms, we found a significantly lower rate of suspected sensory deficits (8%), a result similar to those of previous studies among typically developing children (Ahn et al. 2004; Ben-Sasson et al. 2009).
Specifically, significant group differences were found in the tactile, movement (vestibular), auditory, and visual sensory systems. Although the diagnoses of SMD and PTSD share some common behavioral characteristics, it is important to note that children with PTS symptoms in this study were found to have difficulties responding to various types of stimulation in daily-life activities (e.g., “expresses distress during grooming,” “is bothered by bright lights”), beyond what might be considered trauma-related stimuli or core symptoms of PTSD.
In addition to findings of low performance in several modalities, the subsection scores reflected behaviors characteristic of both over-responsivity (e.g., “avoids going barefoot in sand or grass”) and under-responsivity (e.g., “does not seem to notice when face or hands are messy”). The literature regarding the association between PTSD and sensory modulation has focused mainly on over-responsivity to sensory stimuli. Nevertheless, the psychophysiological characteristics of trauma are experienced on a spectrum ranging from under-responsivity to over-responsivity (Engel-Yeger et al. 2013), and it is common for a person to fluctuate between diminished awareness to environmental stimuli and hypersensitivity or avoidance (Atchison 2007; Atchison and Morkut 2012). Furthermore, in some cases under-responsivity may also be a result of an extremely over- aroused system that compensates by shutting down (Lane 2002).
Most research on individuals with PTSD regarding atypical sensory processing functioning has focused on basic fundamental physiological processes (Bailliard and Whigham 2017). Our findings are comparable to those of the limited research employing the use of sensory profile questionnaires, which measure behavioral responses to sensory stimuli in daily-life situations. For example, Engel-Yeger et al. (2013) in a study on adults with and without PTS symptoms also found significant differences in individual sensory processing patterns in the vestibular, tactile, and auditory modalities. Atchison (2007) also reported finding relatively high rates of SMD among children referred to a trauma assessment center. Since the participants of our present research were selected from the community, the rates in clinical samples may be presumed even higher.
The findings of this study have implications for the assessment and treatment of children showing symptoms of PTS. Evaluation of sensory processing should be incorporated into the routine evaluation of this population, in order to determine if this is an additional factor contributing to a child’s difficulties in participating in daily activities. Subsequent intervention programs should then address the multiple needs of these children. While the relationship between PTS symptoms and SMD is under studied, the value of a focus on sensory modulation in treating individuals with PTS symptoms has become increasingly evident, regardless of whether SMD is a result or a contributing cause of PTSD (Champagne and Tewfick 2010; Koomar 2009).
Difficulties in self-regulation and hyperarousal are common behavioral characteristics of individuals with both SMD and PTS symptoms. The state of arousal of a person influences all aspects of human functioning, and therefore guides therapeutic interventions in multiple directions (Perry 2006; Ryan and Lane 2017). Improved regulation of core physiological states can have a broad positive impact on post-traumatic sequelae and offer an additional therapeutic perspective which has been found to be notably helpful (Kinniburgh et al. 2005; Perry 2006, 2009; Ryan and Lane 2017; Van der Kolk 2006).
Thus, several intervention programs for individuals with PTS symptoms as well as complex trauma have been developed, which emphasize the sensory component of regulation. Examples include interventions such as the Sensory Motor Arousal Regulation Treatment (SMART) (Koomar 2009; Warner et al. 2013), the Safe Place (May-Benson and Sawyer 2016), the Neurosequential Model of Therapeutics (NMT) (Perry 2006, 2009), and the Sensorimotor Approach to the treatment of trauma and dissociation (Ogden et al. 2006). These interventions emphasize building regulation abilities by providing carefully chosen sensory experiences, adapted to both the individual and the situation. All interventions are trauma-informed, fostering therapeutic relationships and the development of secure attachment systems (Champagne 2010; Champagne and Tewfick 2010; LeBel et al. 2010; Torchalla et al. 2018; Ryan and Lane 2017). For treatment to be optimal, clinicians need to consider the range of possible causes that might underlie the co-occurrence of PTS symptoms and SMD.
Limitations and Future Directions
Certain limitations of this study need to be taken into account when relating to the findings. First, the community-based convenience sample, restricted to one geographic region, limits the study’s generalizability. The study also related specifically to terrorism-induced trauma, again limiting generalizability. Future research should pursue similar questions with larger, heterogeneous samples, as well as relating to different types and complexities of trauma.
In addition, due to the fact that this study was part of a larger study that included the administration of a variety of questionnaires, the Short Sensory Profile was used here. Although this screening questionnaire is recommended for research protocols (McIntosh et al. 1999a) and is frequently used in research, the longer diagnostic version would have provided a more in-depth evaluation. Further, the results are based solely on parents’ reports, which by their very nature are subjective. On the other hand, in the intimate forum of daily life, parents are the most likely source for obtaining an accurate picture of a child’s behavior. Due to the paucity of research and the study limitations, additional studies are necessary before we can arrive at more definitive conclusions. Beyond describing the sensory profile of children with PTSD, future research should be aimed at understanding the etiology and mutual interdependence of these co-occurring deficits.
Conclusion
Our results are consistent with the accumulating literature documenting the pervasive negative impact of continuous traumatic stress resulting from political terrorism, manifested in a wide range of developmental domains (Feldman and Vengrober 2011; Halevi et al. 2016; Sagi-Schwartz 2008; Slone and Mann 2016; Thabet et al. 2006). Our study adds to the literature by providing initial evidence that broadens this understanding, showing that children with higher levels of PTS symptoms are at greater risk for additional impairment in their sensory processing.
Funding
This study was supported by a grant from the Israel Science Foundation (ISF) to Ruth. Pat-Horenczyk, Principal investigator. We are grateful to the Bernard van Leer Foundation and Herbert Bearman Foundation for their generous support of the study and the treatment of the traumatized families.
Compliance with Ethical Standards
Conflict of Interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical Standards and Informed Consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation [institutional and national] and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Ahn RR, Miller LJ, Milberger S, McIntosh DN. Prevalence of parents perceptions of sensory processing disorders among kindergarten children. American Journal of Occupational Therapy. 2004;58:287–302. doi: 10.5014/ajot.58.3.287. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 5. Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- Atchison BJ. Sensory modulation disorders among children with a history of trauma: A frame of reference for speech pathologists. Language, Speech, and Hearing Services in Schools. 2007;38:109–116. doi: 10.1044/0161-1461(2007/011). [DOI] [PubMed] [Google Scholar]
- Atchison B, Morkut B. Developmental trauma disorder. In: Atchison B, Dirette DK, editors. Conditions in occupational therapy: Effect on occupational performance. Philadelphia, PA: Lippincott Williams & Wilkins; 2012. pp. 323–334. [Google Scholar]
- Bailliard AL, Whigham SC. Centennial topics—Linking neuroscience, function, and intervention: A scoping review of sensory processing and mental illness. American Journal of Occupational Therapy. 2017;71:1–18. doi: 10.5014/ajot.2017.024497. [DOI] [PubMed] [Google Scholar]
- Barron IG, Abdallah G. Intergenerational trauma in the occupied Palestinian territories: Effect on children and promotion of healing. Journal of Child & Adolescent Trauma. 2015;8(2):103–110. doi: 10.1007/s40653-015-0046-z. [DOI] [Google Scholar]
- Bar-Shalita T, Vatine J, Parush S. Sensory modulation disorder: A risk factor for participation in daily life activities. Developmental Medicine and Child Neurology. 2008;50(12):932–937. doi: 10.1111/j.1469-8749.2008.03095.x. [DOI] [PubMed] [Google Scholar]
- Bar-Shalita T, Vatine J, Yarnitsky D, Parush S, Weissman-Fogel I. Atypical central pain processing in sensory modulation disorder: Absence of temporal summation and higher after-sensation. Experimental Brain Research. 2014;232(2):587–595. doi: 10.1007/s00221-013-3767-y. [DOI] [PubMed] [Google Scholar]
- Ben-Sasson A, Podoly TY. Sensory over-responsivity and obsessive-compulsive symptoms: A cluster analysis. Comprehensive Psychiatry. 2017;73:151–159. doi: 10.1016/j.comppsych.2016.10.013. [DOI] [PubMed] [Google Scholar]
- Ben-Sasson A, Carter AS, Briggs-Gowan MJ. Sensory over-responsivity in elementary school: Prevalence and social-emotional correlates. Journal of Abnormal Child Psychology. 2009;37(5):705–716. doi: 10.1007/s10802-008-9295-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betancourt TS, Khan KT. The mental health of children affected by armed conflict: Protective processes and pathways to resilience. International Review of Psychiatry. 2008;20(3):317–328. doi: 10.1080/09540260802090363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonanno GA. Loss, trauma, and human resilience: Have we underestimated the human capacity to thrive after extremely aversive events? American Psychologist. 2004;59(1):20–28. doi: 10.1037/0003-066X.59.1.20. [DOI] [PubMed] [Google Scholar]
- Brett-Green BA, Miller LJ, Gavin WJ, Davies PL. Multisensory integration in children: A preliminary ERP study. Brain Research. 2008;1242:283–290. doi: 10.1016/j.brainres.2008.03.090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brett-Green BA, Miller LJ, Schoen SA, Nielsen DM. An exploratory event-related potential study of multisensory integration in sensory over-responsive children. Brain Research. 2010;1321:67–77. doi: 10.1016/j.brainres.2010.01.043. [DOI] [PubMed] [Google Scholar]
- Brown C, Dunn W. Adolescent-adult sensory profile: User’s manual. San Antonio, TX: Therapy Skill Builders; 2002. [Google Scholar]
- Champagne T. Occupational therapy in special and high-risk situations. In: Scheinholtz MA, editor. Occupational therapy in mental health: Considerations for advanced practice. Bethesda, MD: American Occupational Therapy Association; 2010. pp. 179–197. [Google Scholar]
- Champagne T, Tewfick D. Trauma, mental health care & occupational therapy practice. In: Scheinholtz MA, editor. Occupational therapy in mental health: Considerations for advanced practice. Bethesda, MD: American Occupational Therapy Association; 2010. pp. 215–230. [Google Scholar]
- Clancy K, Ding M, Bernat E, Schmidt NB, Li W. Restless ‘rest’: Intrinsic sensory hyperactivity and disinhibition in post-traumatic stress disorder. Brain. 2017;140(7):2041–2050. doi: 10.1093/brain/awx116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dar R, Kahn DT, Carmeli R. The relationship between sensory processing, childhood rituals and obsessive-compulsive symptoms. Journal of Behavior Therapy and Experimental Psychiatry. 2012;43(1):679–684. doi: 10.1016/j.jbtep.2011.09.008. [DOI] [PubMed] [Google Scholar]
- Dean EE, Little L, Tomchek S, Dunn W. Sensory processing in the general population: Adaptability, resiliency, and challenging behavior. American Journal of Occupational Therapy. 2018;72:1–8. doi: 10.5014/ajot.2018.019919. [DOI] [PubMed] [Google Scholar]
- Dunn W. The sensations of everyday life: Empirical, theoretical, and pragmatic considerations. American Journal of Occupational Therapy. 2001;55:608–620. doi: 10.5014/ajot.55.6.608. [DOI] [PubMed] [Google Scholar]
- Ehlers A, Clark DM. A cognitive model of post-traumatic stress disorder. Behaviour Research and Therapy. 2000;38(4):319–345. doi: 10.1016/S0005-7967(99)00123-0. [DOI] [PubMed] [Google Scholar]
- Engel-Yeger B. The applicability of the short sensory profile for screening sensory processing disorders among Israeli children. International Journal of Rehabilitation Research. 2010;33:311–318. doi: 10.1097/MRR.0b013e32833abe59. [DOI] [PubMed] [Google Scholar]
- Engel-Yeger B, Palgy-Levin D, Lev-Wiesel R. The sensory profile of people with post-traumatic stress symptoms. Occupational Therapy in Mental Health. 2013;29:266–278. doi: 10.1080/0164212x.2013.819466. [DOI] [Google Scholar]
- Engel-Yeger B, Palgy-Levin D, Lev-Wiesel R. Predicting fears of intimacy among individuals with post-traumatic stress symptoms by their sensory profile. British Journal of Occupational Therapy. 2015;78(1):51–57. doi: 10.1177/0308022614557628. [DOI] [Google Scholar]
- Feldman R, Vengrober A. Post-traumatic stress disorder in infants and young children exposed to war-related trauma. Journal of the American Academy of Child & Adolescent Psychiatry. 2011;50(7):645–658. doi: 10.1016/j.jaac.2011.03.001. [DOI] [PubMed] [Google Scholar]
- Ghisolfi ES, Margis R, Becker J, Zanardo AP, Strimitzer IM, Lara DR. Impaired P50 sensory gating in post-traumatic stress disorder secondary to urban violence. International Journal of Psychophysiology. 2004;51(3):209–214. doi: 10.1016/j.ijpsycho.2003.09.002. [DOI] [PubMed] [Google Scholar]
- Gouze KR, Hopkins J, Lebailly SA, Lavigne JV. Re-examining the epidemiology of sensory regulation dysfunction and comorbid psychopathology. Journal of Abnormal Child Psychology. 2009;37(8):1077–1087. doi: 10.1007/s10802-009-9333-1. [DOI] [PubMed] [Google Scholar]
- Green SA, Ben-Sasson A. Anxiety disorders and sensory over-responsivity in children with autism spectrum disorders: Is there a causal relationship? Journal of Autism and Developmental Disorders. 2010;40:1495–1504. doi: 10.1007/s10803-010-1007-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halevi G, Djalovski A, Vengrober A, Feldman R. Risk and resilience trajectories in war-exposed children across the first decade of life. Journal of Child Psychology and Psychiatry. 2016;57(10):1183–1193. doi: 10.1111/jcpp.12622. [DOI] [PubMed] [Google Scholar]
- Hayes JP, Van Elzakker MB, Shin LM. Emotion and cognition interactions in PTSD: A review of neurocognitive and neuroimaging studies. Frontiers in Integrative Neuroscience. 2012;6:89. doi: 10.3389/fnint.2012.00089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holstein DH, Vollenweider FX, Jäncke L, Schopper C, Csomor PA. P50 suppression, pre-pulse inhibition, and startle reactivity in the same patient cohort suffering from post-traumatic stress disorder. Journal of Affective Disorders. 2010;126:188–197. doi: 10.1016/j.jad.2010.02.122. [DOI] [PubMed] [Google Scholar]
- Karl A, Malta LS, Maercker A. Meta-analytic review of event related potential studies in post-traumatic stress disorder. Biological Psychology. 2006;71(2):123–147. doi: 10.1016/j.biopsycho.2005.03.004. [DOI] [PubMed] [Google Scholar]
- Karr N. Psychological impact of disasters on children: Review of assessment and intervention. World Journal of Pediatrics. 2009;5:5–11. doi: 10.1007/s12519-009-0001-x. [DOI] [PubMed] [Google Scholar]
- Kinnealey M, Koenig KP, Smith S. Relationships between sensory modulation and social supports and health-related quality of life. American Journal of Occupational Therapy. 2011;65(3):320–327. doi: 10.5014/ajot.2011.001370. [DOI] [PubMed] [Google Scholar]
- Kinniburgh KJ, Blaustein M, Spinazzola J, Van der Kolk BA. Attachment, Self- Regulation, and Competency: A comprehensive intervention framework for children with complex trauma. Psychiatric Annals. 2005;35:424–430. doi: 10.3928/00485713-20050501-08. [DOI] [Google Scholar]
- Koomar JA. Trauma and attachment-informed sensory integration assessment and intervention. Sensory Integration Special Interest Section Quarterly. 2009;32(4):1–4. [Google Scholar]
- Lacoviello BM, Charney DS. Psychosocial facets of resilience: Implications for preventing posttrauma psychopathology, treating trauma survivors, and enhancing community resilience. European Journal of Psychotraumatology. 2014;5:1. doi: 10.3402/ejpt.v5.23970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lane, S. J. (2002). Sensory modulation. In Bundy. A.C., Lane, S.J., & Murray, E.A. (Eds.). Sensory integration: Theory and practice (pp. 101–122). Philadelphia, PA: F. A. Davis Company.
- Lane SJ, Reynolds S, Dumenci L. Sensory over-responsivity and anxiety in typically developing children and children with autism and attention deficit hyperactivity disorder: Cause or coexistence? American Journal of Occupational Therapy. 2012;66:595–603. doi: 10.5014/ajot.2012.004523. [DOI] [PubMed] [Google Scholar]
- LeBel J, Champagne T, Stromberg N, Coyle R. Integrating sensory and trauma-informed interventions: A Massachusetts state initiative, part 1. Mental Health Special Interest Section Quarterly. 2010;33(1):1–4. [Google Scholar]
- Levit-Binnun N, Golland Y. Finding behavioral and network indicators of brain vulnerability. Frontiers in Human Neuroscience. 2012;6:10. doi: 10.3389/fnhum.2012.00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levit-Binnun N, Szepsenwol O, Stern-Ellran K, Engel-Yeger B. The relationship between sensory responsiveness profiles, attachment orientations, and anxiety symptoms. Australian Journal of Psychology. 2014;66(4):233–240. doi: 10.1111/ajpy.12064. [DOI] [Google Scholar]
- Lewin AB, Wu MS, Murphy TK, Storch EA. Sensory over-responsivity in pediatric obsessive-compulsive disorder. Journal of Psychopathology and Behavioral Assessment. 2015;37(1):13–143. doi: 10.1007/s10862-014-9442-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipskaya-Velikovsky L, Bar-Shalita T, Bart O. Sensory modulation and daily-life participation in people with schizophrenia. Comprehensive Psychiatry. 2015;58:130–137. doi: 10.1016/j.comppsych.2014.12.009. [DOI] [PubMed] [Google Scholar]
- Masten AS. Ordinary magic: Resilience processes in development. American Psychologist. 2001;56(3):227–238. doi: 10.1037/0003-066X.56.3.227. [DOI] [PubMed] [Google Scholar]
- May-Benson T, Sawyer S. An intervention manual for SAFE PLACE. Newton, MA: OTA The Koomar Center; 2016. [Google Scholar]
- McFarlane AC, Weber DL, Clark CR. Abnormal stimulus processing in post-traumatic stress disorder. Biological Psychiatry. 1993;34(5):311–320. doi: 10.1016/0006-3223(93)90088-U. [DOI] [PubMed] [Google Scholar]
- McIntosh, D. N., Miller, L. J., & Dunn, W. (1999a). Overview of the short sensory profile (SSP). In W. Dunn (Ed.), The sensory profile: Examiner’s manual (pp. 59–73). San Antonio, TX: The Psychological Corporation.
- McIntosh DN, Miller LJ, Shyu V, Hagerman RJ. Sensory modulation disruption, electrodermal response, and functional behaviors. Developmental Medicine and Child Neurology. 1999;41(9):608–615. doi: 10.1111/j.1469-8749.1999.tb00664.x. [DOI] [PubMed] [Google Scholar]
- Meredith PJ, Rappel G, Strong J, Bailey KJ. Sensory sensitivity and strategies for coping with pain. American Journal of Occupational Therapy. 2015;69:1–10. doi: 10.5014/ajot.2015.014621. [DOI] [PubMed] [Google Scholar]
- Miller LJ, Anzalone ME, Lane SJ, Cermak SA, Osten ET. Concept evolution in sensory integration: A proposed nosology for diagnosis. The American Journal of Occupational Therapy. 2007;21:135–140. doi: 10.5014/ajot.61.2.135. [DOI] [PubMed] [Google Scholar]
- Miller LJ, Nielsen DM, Schoen SA. Attention deficit hyperactivity disorder and sensory modulation disorder: A comparison of behavior and physiology. Research in Developmental Disabilities. 2012;33:804–818. doi: 10.1016/j.Ridd.2011.12.005. [DOI] [PubMed] [Google Scholar]
- Muffly A, Gerney A. Occupational preferences of people who have experienced sexual assault. Occupational Therapy in Mental Health. 2015;31(2):101–112. doi: 10.1080/0164212X.2015.1027842. [DOI] [Google Scholar]
- Nugent NR, Sumner JA, Amstadter AB. Resilience after trauma: From surviving to thriving. European Journal of Psychotraumatology. 2014;5(1):25339. doi: 10.3402/ejpt.v5.25339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden P, Pain C, Fisher J. A sensorimotor approach to the treatment of trauma and dissociation. Psychiatric Clinics of North America. 2006;29:263–279. doi: 10.1016/j.psc.2005.10.012. [DOI] [PubMed] [Google Scholar]
- Pat-Horenczyk Ruth. Post-Traumatic Distress in Israeli Adolescents Exposed to Ongoing Terrorism. Journal of Aggression, Maltreatment & Trauma. 2005;9(3-4):335–347. doi: 10.1300/J146v09n03_04. [DOI] [Google Scholar]
- Pat-Horenczyk R, Rabinowitz R, Rice A, Tucker-Levin A. The search for risk and protective factors in childhood PTSD: From variables to processes. In: Brom D, Pat-Horenczyk R, Ford J, editors. Treating traumatized children: Risk, resilience and recovery. London: Routledge; 2009. pp. 51–71. [Google Scholar]
- Pat-Horenczyk R, Qasrawi R, Lesack R, Haj-Yahia M, Peled O, Shaheen M, Berger R, Brom D, Garber R, Abdeen Z. Post-traumatic symptoms, functional impairment, and coping among adolescents on both sides of the Israeli–Palestinian conflict: A cross-cultural approach. Applied Psychology. 2009;58(4):688–708. doi: 10.1111/j.1464-0597.2008.00372.x. [DOI] [Google Scholar]
- Pat-Horenczyk R, Ziv Y, Asulin-Peretz L, Achituv M, Cohen S, Brom D. Relational trauma in times of political violence: Continuous versus past traumatic stress. Peace and Conflict: Journal of Peace Psychology. 2013;19(2):125–137. doi: 10.1037/a0032488. [DOI] [Google Scholar]
- Pat-Horenczyk Ruth, Cohen Sarale, Ziv Yuval, Achituv M., Brickman Sophie, Blanchard Tamar, Brom Danny. Stability and Change in Posttraumatic Distress: A 7-Year Follow-Up Study of Mothers and Young Children Exposed to Cumulative Trauma. Journal of Traumatic Stress. 2017;30(2):115–124. doi: 10.1002/jts.22177. [DOI] [PubMed] [Google Scholar]
- Perry BD. Applying principles of neurodevelopment to clinical work with maltreated and traumatized children. In: Webb NB, editor. Working with traumatized youth in child welfare. New York, NY: Guilford Press; 2006. pp. 27–52. [Google Scholar]
- Perry BD. Examining child maltreatment through a neurodevelopmental lens: Clinical applications of the neurosequential model of therapeutics (NMT) Journal of Trauma and Loss. 2009;14:1–16. doi: 10.1080/15325020903004350. [DOI] [Google Scholar]
- Reynolds S, Lane SJ. Sensory over-responsivity and anxiety in children with ADHD. American Journal of Occupational Therapy. 2009;63:433–440. doi: 10.5014/ajot.63.4.433. [DOI] [PubMed] [Google Scholar]
- Roussos A, Goenjian AK, Steinberg AM, Sotiropoulou C, Kakaki M, Kabakos C, Manouras V. Post-traumatic stress and depressive reactions among children and adolescents after the 1999 earthquake in Ano Liosia, Greece. American Journal of Psychiatry. 2005;162(3):530–537. doi: 10.1176/appi.ajp.162.3.530. [DOI] [PubMed] [Google Scholar]
- Ryan Katherine, Lane Shelly J., Powers Denise. A multidisciplinary model for treating complex trauma in early childhood. International Journal of Play Therapy. 2017;26(2):111–123. doi: 10.1037/pla0000044. [DOI] [Google Scholar]
- Sagi-Schwartz A. The wellbeing of children living in chronic war zones: The Palestinian- Israeli case. International Journal of Behavioral Development. 2008;32(4):322–336. doi: 10.1177/0165025408090974. [DOI] [Google Scholar]
- Schaaf RC, Miller LJ, Seawell D, O’Keefe S. Children with disturbances in sensory processing: A pilot study examining the role of the parasympathetic nervous system. American Journal of Occupational Therapy. 2003;57:442–449. doi: 10.5014/ajot.57.4.442. [DOI] [PubMed] [Google Scholar]
- Shalev AY, Peri T, Brandes D, Freedman S, Orr S, Pitman R. Auditory startle response in trauma survivors with post-traumatic stress disorder: A prospective study. American Journal of Psychiatry. 2000;157(2):255–261. doi: 10.1176/appi.ajp.157.2.255. [DOI] [PubMed] [Google Scholar]
- Slone M, Mann S. Effects of war, terrorism, and armed conflict on young children: A systematic review. Child Psychiatry & Human Development. 2016;47(6):950–965. doi: 10.1007/s10578-016-0626-7. [DOI] [PubMed] [Google Scholar]
- Steinberg AM, Brymer MJ, Decker KB, Pynoos RS. The University of California at Los Angeles post-traumatic stress disorder reaction index. Current Psychiatry Reports. 2004;6(2):96–100. doi: 10.1007/s11920-004-0048-2. [DOI] [PubMed] [Google Scholar]
- Stewart LP, White PM. Sensory filtering phenomenology in PTSD. Depression and Anxiety. 2008;25(1):38–45. doi: 10.1002/da.20255. [DOI] [PubMed] [Google Scholar]
- Thabet AA, Karim K, Vostanis P. Trauma exposure in preschool children in a war zone. The British Journal of Psychiatry. 2006;188(2):154–158. doi: 10.1192/bjp.188.2.154. [DOI] [PubMed] [Google Scholar]
- Torchalla Iris, Killoran John, Fisher Daniela, Bahen Montana. Trauma-Focused Treatment for Individuals with Posttraumatic Stress Disorder: The Role of Occupational Therapy. Occupational Therapy in Mental Health. 2018;35(4):386–406. doi: 10.1080/0164212X.2018.1510800. [DOI] [Google Scholar]
- Trickey D, Siddaway AP, Meiser-Stedman R, Serpell L, Field AP. A meta-analysis of risk factors for post-traumatic stress disorder in children and adolescents. Clinical Psychological Review. 2012;32:122–138. doi: 10.1016/j.cpr.2011.12.001. [DOI] [PubMed] [Google Scholar]
- Van der Kolk BA. Clinical implications of neuroscience research in PTSD. Annals of the New York Academy of Sciences. 2006;1071(1):277–293. doi: 10.1196/annals.1364.022. [DOI] [PubMed] [Google Scholar]
- Warner E, Koomar J, Lary B, Cook A. Can the body change the score? Application of sensory modulation principles in the treatment of traumatized adolescents in residential settings. Journal of Family Violence. 2013;28:729–738. doi: 10.1007/s10896-013-9535-8. [DOI] [Google Scholar]
- Wolmer L, Hamiel D, Versano-Eisman T, Slone M, Margalit N, Laor N. Preschool Israeli children exposed to rocket attacks: Assessment, risk, and resilience. Journal of Traumatic Stress. 2015;28(5):441–447. doi: 10.1002/jts.22040. [DOI] [PubMed] [Google Scholar]
- Yochman A, Alon-Beery O, Sribman A, Parush S. Differential diagnosis of sensory modulation dysfunction (SMD) and attention deficit hyperactivity disorder (ADHD): Participation, sensation, and attention. Frontiers in Human Neuroscience. 2013;7:1–10. doi: 10.3389/fnhum.2013.00862. [DOI] [PMC free article] [PubMed] [Google Scholar]