Abstract
We report two studies examining psychometric properties of an expanded measure of adverse childhood experiences (ACEs) that combined the original ACEs items with items from the Juvenile Victimization Questionnaire. In Study 1, we examined its factorial structure, internal consistency, and concurrent validity in undergraduates (N = 1479). In Study 2, we also examined replicability of frequencies of ACEs, test-retest reliability, and convergent and predictive validity. Results suggested a model with four inter-related factors: maltreatment, household dysfunction, community dysfunction, and peer dysfunction/property victimization. Internal consistency, test-retest reliability, concurrent and convergent validity were acceptable, and findings were replicated across samples. We suggest that this expanded measure is assessing early experiences of victimization and helplessness in the face of perceived intentional emotional and physical threats or actual harm by others, and that although they may not all be “traumatic,” their cumulative impact is associated with poor mental health in young adults.
Keywords: Adverse childhood experiences, Trauma, Reliability, Validity, Factorial structure, Mental health, Stress
In their seminal paper arguing for a causal relationship between adverse childhood experiences (ACEs) and long-term health consequences, Felitti and colleagues (Felitti et al. 1998) defined ACEs as “childhood abuse and household dysfunction.” Their concern with ACEs began with an attempt to identify risk factors for dropping out of a weight-loss program in a predominantly White, middle-class sample of adults (Felitti 1993). The factors they identified included sexual and other forms of abuse, and a “dysfunctional family life” (e.g., drug use and criminal activity by parents, domestic violence), as it frequently co-occurs with abuse (Felitti et al. 1998). The combination of these risk factors turned out to be extremely good at predicting poor outcomes far beyond dropping out of a weight-loss program, and a large body of research has accumulated that provides incontrovertible evidence for the cumulative influence of these early adversities on health (Anda et al. 2010, 2006).
Nevertheless, given that children, especially those who live in poverty or who are ethnic/racial minorities, face adversities outside the home as well, it is time to reconsider whether the definition of ACEs should be limited to maltreatment and household dysfunction. The items on the original ACEs scale were selected because they had predicted negative outcomes in previous research (Felitti et al. 1998). No justification was made for why only certain risk factors were chosen to predict such a wide variety of illnesses and health-risk behaviors. However, limiting the definition to maltreatment and household dysfunction risks misdirecting the focus of intervention efforts for ACEs to only family dysfunction and parenting practices.
Thus, the purpose of the current study was to examine the psychometric properties of an expanded scale of ACEs that included not only maltreatment and household dysfunction but also victimization experiences outside the home. In the article, we will elaborate on the implications of the data for a more cogent definition of ACEs.
Psychometric Properties of the Original ACEs Scale
Although there are several measures of childhood adversities that assess maltreatment and other stressful life events, we focused on the original ACEs scale because a large body of research has accumulated in the last 20 years linking this measure to many health outcomes in a wide variety of populations across the world. Thus, the original ACEs scale has caught the imagination of the researchers and the public and might be said to exert a disproportionate influence in discussions of early adversity.
A number of studies have examined the psychometric properties of the original ACEs scale. The items on this scale are interrelated, and the presence of each ACE is associated with an elevated probability of other ACEs in adults (Bellis et al. 2014a, b; Dong et al. 2004; Felitti et al. 1998; Mersky et al. 2017) and children (Scott et al. 2013). The scale has acceptable internal consistency in a variety of samples (Bruskas 2013; Ford et al. 2014; Mersky et al. 2017; Wingenfeld et al. 2011; Zanotti et al. 2017). Satisfactory convergent validity with the Childhood Trauma Questionnaire (CTQ) was found in clinical and non-clinical samples in Germany (Wingenfeld et al. 2011). Higher levels of ACEs are associated with higher levels of perceived stress and mental health problems measured concurrently (Anda et al. 2006) and prospectively (Schilling et al., 2007).
Do these findings mean that the original ACEs scale measures a unitary construct? Several studies have examined the factor structure of items on the original ACEs scale using both exploratory and confirmatory factor analyses (EFAs and CFAs). A large epidemiological sample yielded three factors after EFA and CFA: household dysfunction, physical/emotional abuse, and sexual abuse (Ford et al. 2014), with moderate to high correlations among factors. Three of the 11 questions on this scale pertained to sexual abuse, which may have led to a differentiation between sexual and other forms of abuse. A chart review of parental reports of a low-income sample of children (B. G. Scott et al. 2013) found a three-factor solution with EFA, consisting of an abuse factor (physical, emotional, and sexual), a household dysfunction factor, and a mixed factor (sexual abuse, parental drug use and absence, and emotional neglect). Inter-factor correlations were not reported. A study of young, low-income women receiving home-visiting services produced a two-factor solution after EFA, consisting of maltreatment and household dysfunction, with a correlation of .48 between factors (Mersky et al. 2017). Another analysis of a short form of the ACEs that only included maltreatment items in Romanian adolescents also produced a two-factor solution after both EFA and CFA, consisting of physical/emotional abuse and sexual abuse, with a moderate (.48) correlation between them (Meinck et al. 2017). In summary, findings demonstrate that the factorial structure of an ACEs scale is a function of the items included, and that regardless of variations in items, the emerging factors are moderately correlated with each other.
Concerns have been raised about the validity of retrospective recall of early adversities. Some evidence suggests ACEs may be subject to recall bias, especially for those who are currently depressed (Scott et al. 2010). Other studies, however, indicate that current symptoms do not affect reliability of reports of child maltreatment in young adults (Pinto et al. 2014). Evidence further suggests that the relation between number of ACEs and negative outcomes holds for both prospective (Clark et al. 2010; K. M. Scott et al. 2010) and retrospective studies (Afifi et al. 2011; Anda et al. 2008). Comparisons of prospective and retrospective data show no bias in assessment and no differences among associations between number of ACEs and outcomes as a function of time of reporting (Hardt et al. 2010; K. M. Scott et al. 2010). Furthermore, test-retest reliability for the sum of the items is acceptable over intervals ranging from 6 to 20 months, though with variable results for individual items (Dube et al. 2004; Mersky et al. 2017; Pinto et al. 2014; Zanotti et al. 2017).
The Juvenile Victimization Questionnaire (JVQ)
We chose to expand the original ACEs scale with items from the JVQ (Finkelhor et al. 2005; Hamby and Finkelhor 2000) for several reasons. First, it is based on a perspective that acknowledges that victimization outside the home is just as noteworthy as victimization in the home, grounding it in a thoughtful consideration of a wide range of risk factors that need to be included in a measure of childhood adversity (Finkelhor et al. 2011; Hamby and Finkelhor 2000). It also covers a wide age range in childhood and has versions for both children and adults. In a large, nationally representative sample of 2- to 17-year-olds, it was shown to have good test-retest reliability and internal consistency as well as concurrent validity, assessed through a measure of trauma symptoms (Finkelhor et al. 2005). There is not as much research on the relationship between JVQ scores and health outcomes as there is for the original ACEs scale. Nevertheless, items from the JVQ, such as items related to peer and property victimization and exposure to community violence, are associated with trauma symptoms in 10- to 17-year-olds at least as strongly as items based on the original ACEs questionnaire (Finkelhor et al. 2013, 2015).
Purpose of the Current Studies
In the current paper, we report on two studies examining the psychometric properties of a measure that combined the original ACEs questionnaire with the JVQ. In the first study, we examined the factorial structure, internal consistency, and concurrent validity of the measure in a large sample of college students. We expected high internal consistency and substantial, positive associations with concurrent measures of mental well-being and stress.
Study 1: Method
Participants
Participants were drawn from four studies conducted between 2015 and 2018 that examined the relationship of ACEs to health, response to health-related interventions, and academic performance in undergraduates in a large, Midwestern public university. Participants for three studies (N = 1417) were recruited from psychology classes that offered course credit for research participation. According to the administrators of this pool, it is comprised of approximately 15% psychology majors, 25% business majors, and 25% pre-med students. In the one study in which we inquired about majors (N = 341), only 11.9% indicated that they were majoring in psychology. Participants for the fourth study (N = 62) were recruited from flyers posted around campus. Average age across all participants was 19.9 (Mdn = 19, SD = 2.5, range = 18–49), with 97% of the participants under the age of 26. Three quarters (75.1%) identified as female. Most (71.1%) students identified as White, 20.0% identified as Asian, and smaller numbers identified as Black (3.2%), multiracial (3.2%), other (1.8%), and Native American (0.5%). Participants who did not respond to at least one ACE question were excluded (N = 25).
Measures
ACEs
The expanded ACEs questionnaire was created by combining the original ACEs questionnaire (Felitti et al. 1998) and the JVQ (Finkelhor et al. 2013) and consisted of 33 items assessing moderate to severe adversity between ages 0 and 18. The instructions were based on the adult retrospective version of the JVQ (http://www.unh.edu/ccrc/jvq/index_new.html): “These are questions about some things that might have happened during your childhood. Your ‘childhood’ begins when you are born and continues through age 17. It might help to take a minute and think about the different schools you attended, different places you might have lived, or different people who took care of you during your childhood. Try your best to think about your entire childhood as you answer these questions.” Participants responded to each question with a “yes” or “no”; “yes” responses were summed to yield an ACEs score that could range from 0 to 33. Participants in all studies completed the same items on this measure in the same order, close to the beginning of the full survey. All questions are listed in the Appendix in the order in which they were administered.
Mental and Physical Health
The 36-item short-form survey (SF-36) was used to assess current health (Ware et al. 1993) in three of the studies (N = 995). Individual scales (Physical Functioning, Role Limitations Due to Physical Health, Role Limitations Due to Emotional Problems, Energy/Fatigue, Emotional Well-Being, Social Functioning, Pain, and General Health) are scored from 0 to 100, with higher scores indicating better health. Scores were transformed into normed Physical and Mental Summary scores based on instructions provided by survey developers (Ware and Kosinski 2001; Ware et al. 1993).
Anxiety and Depression
The Hopkins Symptom Checklist-10 (HSCL; Syed et al. 2008), is a 10-item measure of anxiety and depression and was administered in one of the studies (N = 341). Participants rated their experiences in the past week, such as “feeling fearful” and “feeling blue” (1 = not at all and 4 = extremely), and their ratings were averaged to yield a total score from 1 to 4. The measure shows good internal consistency and convergent validity (Syed et al. 2008). Internal consistency (Cronbach’s α) in the current sample was .92.
Perceived Stress
In all four studies, we assessed stress with the 10-item Perceived Stress Scale (PSS; Cohen and Williamson 1988), which has good psychometric properties in undergraduates (Roberti 2006). Participants rated how often they experienced feelings of uncontrollability, unpredictability, and being overwhelmed in the past month (e.g., “In the last month, how often have you been upset because of something that happened unexpectedly?”) on a 4-point scale (0 = never and 4 = very often). Scores were summed to yield a total stress score, which could range from 0 to 40. Internal consistency in the current sample was 0.88.
Parental Education
In all studies, we assessed parental education as a proxy for childhood socioeconomic status (SES). Participants rated the highest grade completed by their parents or primary caretakers (1 = no formal education and 7 = completed post-college work), with options for Don’t know and No primary male/female caretaker. If information was provided for only one parent, that parent’s level of education was used; if data were provided for both parents, their average was calculated. Scores could range from 1 to 7.
Procedure
In all studies, participants completed surveys online through the university’s secure survey service (Qualtrics). In three studies, they filled out the surveys once during the semester. In the fourth study (N = 62), they filled out surveys at the beginning and end of the semester; only Time 1 responses were included in current analyses. The questionnaires took 1–1 ½ hours to complete. Participants in three studies were compensated with course credit, and participants in the fourth study were compensated with $20 after completing surveys at both times. All studies were approved by the Institutional Review Board (IRB).
Data Analyses
Data were examined for missing values, and continuous data were checked for outliers and deviations from normality. No outliers were found. For analyses of concurrent validity, we log-transformed scores on the expanded ACEs measure to normalize the distribution of the scores. Scores on the original ACEs measure could not be normalized through a transformation.
Internal consistency was assessed with Cronbach’s ⍺. An ⍺ of over .70 was considered acceptable (Cortina 1993). To explore factor structure, we first conducted an EFA in a random half of the sample and then used the extracted factors to conduct a CFA in the other half. Both analyses were based on the data of students who had no missing data on any of the items.
For the EFA (T. A. Brown 2014; Costello and Osborne 2005), we first checked data factorability through the Kaiser–Meyer–Olkin (KMO) statistic and Bartlett’s test of sphericity. The tetrachoric correlation matrix was entered into analyses for a weighted-least-squares extraction EFA. We used oblique rotation (“oblimin”), as we assumed that the factors would covary. We used the scree test to decide on the maximum number of factors. We then adjusted the number of factors until they had at least three items with factor loadings of at least .30. In choosing among different solutions, we tried to make sure that factors were conceptually coherent and to minimize the number of items with low communality values (< .70) and high loadings on more than one factor.
Next, we used the extracted factors to conduct a confirmatory factor analysis (CFA) on raw ACEs data using the lavaan package (Rosseel 2012). The weighted least square means and variance (WLSMV) estimator was used to conduct the analysis of binary endogenous measures. All items were constrained to load onto only one factor, and factors were assumed to covary. Model fit was assessed on three goodness-of-fit indicators appropriate for binary indicators: the comparative fit index (CFI), the robust value of the root mean square error of approximation (RMSEA), and the robust value of the chi-square. A CFI of over .90 and an RMSEA of less than .08 were considered acceptable for model fit (T. A. Brown 2014). We reported Χ2 values, although in such a large sample, significant Χ2 values do not indicate poor fit (T. A. Brown 2014). Model fit was further examined through factor loadings of the indicators onto the latent variables and R2 values for individual items.
We used Pearson product-moment correlations to assess associations between ACEs and potential covariates for concurrent validity. Log-transformed ACEs scores were related to parental education, r (1476) = −.19, p < .001. In addition, women reported slightly more ACEs than men, t (608.6) = 2.06, p = .04, d = −.15. Thus, to examine concurrent validity, we conducted linear regressions and controlled for gender and average parent education. All analyses were conducted in R Version 3.4.5 (R Core Team 2017). Significance level was set at .05.
Results
Factorial Structure
Factor Analyses of the Expanded ACEs Scale
An EFA was conducted on ACEs data from a random half of the sample (N = 740). The KMO measure was satisfactory at .85, and Bartlett’s test of sphericity was significant, χ2 (528) = 5287.43, p < .001, both of which indicate that the data were amenable to an EFA. The scree plot suggested five factors. Analyses with four, five, and six factors indicated that a four-factor solution would yield the most parsimonious fit (Table 1). We labeled the factors as “child maltreatment,” “household dysfunction,” “community dysfunction,” and “peer dysfunction/property victimization.” The two items related to accidents and illnesses of loved ones were dropped because they yielded negative loadings on “child maltreatment,” and they were the only items with negative loadings on any factor. The four factors collectively accounted for 60% of the variance in the remaining data.
Table 1.
Oblimin-Rotated Factor Loadings from the Exploratory Factor Analysis (EFA) on the 33-Item Expanded ACEs Scale in Study 1
| Items and Proposed factors | Child maltreatment | Household dysfunction | Peer dysfunction/property victimization | Community dysfunction | Communality (h2) |
|---|---|---|---|---|---|
| Community dysfunction (19%) | |||||
| Witnessing murder (25) | .79 | .77 | |||
| Witnessing war (27) | .34 | .75 | .87 | ||
| Murder of someone close (24) | .74 | .61 | |||
| Witnessing riots, etc. (26) | .67 | .52 | |||
| Imprisonment of parental fig. (11) | .38 | .63 | .76 | ||
| Witnessing physical violence (22) | .31 | .63 | .58 | ||
| Sexual abuse by grown-ups (4) | .42 | .55 | .53 | ||
| Burglary (23) | .33 | .51 | .42 | ||
| Parental figure going to war (14) | .46 | .40 | |||
| Death of parental fig. (12) | .46 | .43 | |||
| Forced sex by peers/sibs (19) | .45 | .49 | |||
| Peer dysfunction/property victimization (17%) | |||||
| Break/ruin things on purpose (30) | .81 | .67 | |||
| Stealing (28) | .70 | .53 | |||
| Stealing by force (29) | .67 | .64 | |||
| Name-calling, etc. (18) | .66 | .63 | |||
| Physical bullying (16) | .66 | .73 | |||
| Threat of physical bullying (17) | .64 | .67 | |||
| Social isolation (33) | .32 | .53 | .32 | ||
| Physical attacks due to discrimination (20) | .51 | .35 | .60 | ||
| Child maltreatment (15%) | |||||
| Physical abuse (3) | .85 | .74 | |||
| Verbal abuse (1) | .74 | .73 | |||
| Domestic violence at sibs (10) | .64 | .67 | |||
| Physical neglect (5) | .62 | .60 | |||
| Psychological neglect (2) | .54 | .35 | .63 | ||
| Physical domestic violence (9) | .50 | .43 | .68 | ||
| Forced separation from family (15) | .38 | .35 | .46 | ||
| Perceived discrimination (21) | .37 | .32 | .35 | ||
| Household dysfunction (10%) | |||||
| Family substance abuse (7) | .72 | .67 | |||
| Divorce/separation of parents (13) | .68 | .58 | |||
| Family psychopathology (6) | .64 | .56 | |||
| Verbal domestic violence (8) | .40 | .49 | .38 | .66 | |
The numbers in parentheses after the factor description refer to the proportion of variance accounted for. The numbers in parentheses after the item description refer to the item’s number in the Appendix. Only factor loadings > .30 are displayed. Bold = highest factor loading for the item
Next, we conducted a CFA on the second half of the sample (N = 739), using the 31 items and the four factors extracted from the EFA. As shown in Table 2, the items had high factor loadings, and the fit indices were acceptable, CFI = .94, RMSEA = .028, 95% confidence interval = .024–.032, χ2 (428) = 746.97, p < .09. The factors were strongly correlated with each other. All subsequent analyses on the expanded ACEs scale were conducted on these 31 items.
Table 2.
Results of the Confirmatory Factor Analysis (CFA) on the 31-Item Expanded ACEs Scale in Study 1 (N = 740) and Study 2 (N = 75)
| Factor loading | R2 | ||
|---|---|---|---|
| Community dysfunction | |||
| Sexual abuse by grown-ups (4) | .74 | (.55) | |
| Witnessing physical violence (22) | .64 | (.40) | |
| Burglary (23) | .62 | (.39) | |
| Forced sex by peers/sibs (19) | .61 | (.37) | |
| Imprisonment of parental fig. (11) | .60 | (.36) | |
| Witnessing riots, etc. (26) | .57 | (.32) | |
| Witnessing war (27) | .48 | (.23) | |
| Murder of someone close (24) | .48 | (.23) | |
| Parental figure going to war (14) | .46 | (.21) | |
| Death of parental fig. (12) | .42 | (.18) | |
| Witnessing murder (25) | .38 | (.14) | |
| Difficulties with peers/siblings and property victimization | |||
| Physical bullying (16) | .79 | (.63) | |
| Threat of physical bullying (17) | .78 | (.60) | |
| Name-calling, etc. (18) | .74 | (.55) | |
| Physical attacks due to discrimination (20) | .65 | (.43) | |
| Break/ruin things on purpose (30) | .64 | (.41) | |
| Social isolation (33) | .62 | (.39) | |
| Stealing (28) | .51 | (.26) | |
| Stealing by force (29) | .49 | (.24) | |
| Child maltreatment | |||
| Domestic violence at sibs (10) | .84 | (.70) | |
| Physical abuse (3) | .83 | (.68) | |
| Physical neglect (5) | .79 | (.62) | |
| Verbal abuse (1) | .78 | (.60) | |
| Physical domestic violence (9) | .78 | (.61) | |
| Psychological neglect (2) | .75 | (.57) | |
| Forced separation from family (15) | .64 | (.41) | |
| Perceived discrimination (21) | .63 | (.39) | |
| Household dysfunction | |||
| Verbal domestic violence (8) | .92 | (.85) | |
| Family substance abuse (7) | .66 | (.44) | |
| Divorce/separation of parents (13) | .53 | (.28) | |
| Family psychopathology (6) | .49 | (.24) | |
| Correlations Among Factors | |||
| Community dysfunction | Peer/sibling dysfunction | Child maltreatment | |
| Community dysfunction | |||
| Peer/sibling dysfunction | .76 | ||
| Child maltreatment | .77 | .72 | |
| Household dysfunction | .61 | .59 | .68 |
The numbers in parentheses after the item description refer to the item’s number in the Appendix. Factor loadings refer to standardized factor loadings of the indicator with the latent factor
Factor Analyses of the Original ACEs Scale
The EFA conducted on the first half of the sample yielded satisfactory values for the KMO statistic (.80), and Bartlett’s test of sphericity, χ2 (45) = 1088.76, p < .001. The scree plot suggested two factors, and a two-factor solution (Table 3), consisting of child maltreatment and household dysfunction, provided the best fit for the data, collectively accounting for 54% of the variance. A CFA on these two factors yielded a good fit, CFI = .96, RMSEA = .047, 95% confidence interval = .035–.059; χ2 (34) = 88.80, p < .001, with generally high loadings on the factors (Table 4). The correlation between the two factors was .61.
Table 3.
Oblimin-Rotated Factor Loadings from the Exploratory Factor Analysis (EFA) on the Original ACEs Scale in Study 1
| Items and Proposed factors | Child maltreatment | Household dysfunction | Communality (h2) |
|---|---|---|---|
| Child maltreatment (32% | |||
| Physical abuse (3) | .87 | .75 | |
| Verbal abuse (1) | .87 | .66 | |
| Physical neglect (5) | .66 | .56 | |
| Psychological neglect (2) | .58 | .52 | |
| Sexual abuse by grown-ups (4) | .54 | .25 | |
| Physical domestic violence (9) | .50 | .40 | .62 |
| Household dysfunction (23%) | |||
| Family substance abuse (7) | .87 | .69 | |
| Family psychopathology (6) | .63 | .38 | |
| Imprisonment of parental fig. (11) | .58 | .61 | |
| Divorce/separation of parents (13) | .50 | .40 | |
The numbers in parentheses after the factor description refer to the proportion of variance accounted for. The numbers in parentheses after the item description refer to the item’s number in the Appendix. Only factor loadings > .30 are displayed. Bold = highest factor loading for the item
Table 4.
Results of the Confirmatory Factor Analysis (CFA) on the Original ACEs Scale in Study 1
| Factor loading | R2 | |
|---|---|---|
| Child maltreatment | ||
| Physical abuse (3) | .82 | .68 |
| Verbal abuse (1) | .82 | .67 |
| Physical neglect (5) | .81 | .66 |
| Sexual abuse by grown-ups (4) | .74 | .55 |
| Psychological neglect (2) | .73 | .54 |
| Physical domestic violence (9) | .72 | .52 |
| Household dysfunction | ||
| Imprisonment of parental fig. (11) | .83 | .69 |
| Family substance abuse (7) | .77 | .60 |
| Divorce/separation of parents (13) | .57 | .32 |
| Family psychopathology (6) | .49 | .24 |
The numbers in parentheses after the item description refer to the item’s number in the AppendixFactor loadings refer to standardized factor loadings of the indicator with the latent factor. The correlation between the two factors was .61
Frequencies of ACEs
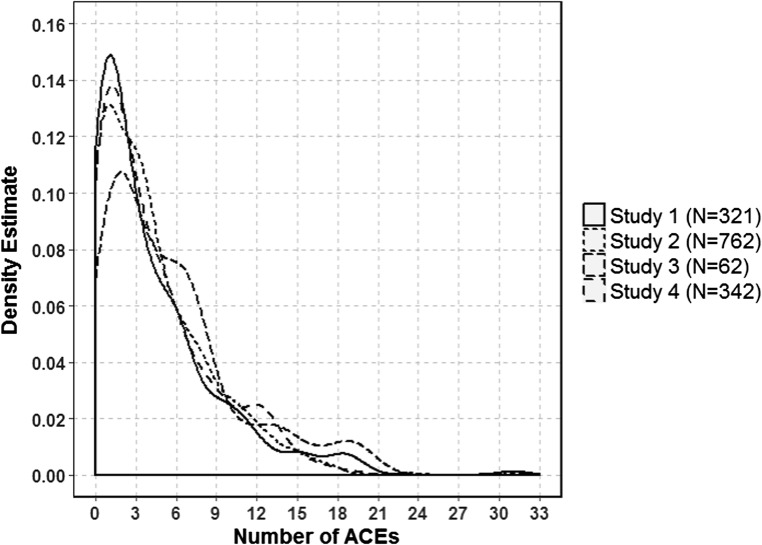
Descriptive statistics of the measures used in both studies are listed in Table 5. We included the number of ACEs from the original ACEs scale for the purpose of direct comparisons of the frequencies to other studies. The Appendix displays proportions of students who endorsed each ACE. Over a third (43%) had 0 to 2 ACEs, 27% had 3 to 5 ACEs, and 30% had 6 or more ACEs. As shown in Fig. 1, frequency distributions of ACEs did not seem to differ substantially across studies. An ANOVA, with study as the predictor and log-transformed ACEs scores as the outcome, confirmed that the effect of study was not significant.
Table 5.
Descriptive Statistics for the Measures Used in Study 1 and 2
| M (SD) | Median | Range | 95% CI | |||||
|---|---|---|---|---|---|---|---|---|
| Study 1 | Study 2 | Study 1 | Study 2 | Study 1 | Study 2 | Study 1 | Study 2 | |
| Expanded ACEs (31 items) a | 4.3 (4.2) | 4.3 (4.2) | 3.0 | 3.0 | 0–31 | 0–24 | 4.1–4.5 | 3.3–5.3 |
| Original ACEs | 1.4 (1.8) | 1.3 (1.7) | 1.0 | 1.0 | 0–10 | 0–8 | 1.4–1.5 | 0.9–1.7 |
| SF-36 Mental Summary | 40.1 (12.7) | 39.6 (14.2) | 42.6 | 44.0 | −1.7 – 61.4 | 2.8–60.3 | 39.2–41.1 | 36.3–42.9 |
| SF-36 Physical Summary | 56.9 (6.3) | 56.7 (7.5) | 57.5 | 58.2 | 26.3–72.2 | 32.4–69.0 | 56.4–57.3 | 55.0–58.4 |
| HSCL | 1.9 (0.7) | 1.9 (0.7) | 1.8 | 1.6 | 1–4 | 1–3.9 | 1.8–2.0 | 1.7–2.1 |
| Perceived Stress Scale | 18.5 (6.4) | 18.3 (7.2) | 19.0 | 18.0 | 1–39 | 4–36 | 18.1–18.8 | 16.6–20.0 |
| SLESQ | n/a | 1.3 (1.9) | n/a | 1.0 | n/a | 0–8 | n/a | 0.9–1.7 |
| CTQ | n/a | 1.4 (0.5) | n/a | 1.2 | n/a | 1–4.2 | n/a | 1.3–1.5 |
For Study 2, only the scores at Time 1 are listed in the table. ACEs = Adverse childhood experiences. CI = Confidence interval. CTQ = Childhood Trauma Questionnaire. HSCL = HSCL = Hopkins Symptom Checklist-10. SF-36 = Short Form-36. SLESQ = Stressful Life Experiences Questionnaire
aDoes not include the three items dropped from analyses after the EFA in Study 1 (accidents and illnesses of loved ones and burglaries)
Fig. 1.
Frequency distribution of the 31 ACEs across the four studies included in Study 1. ACE = adverse childhood experiences
Internal Consistency
Cronbach’s ⍺ of the 31-item scale was good (.84). Inspection of item statistics showed that reliability would not improve if any of the items were dropped. The Appendix lists the correlation of each item with the scale composed of the remaining items. The internal consistency of the original scale was lower (⍺ = .72), as it had fewer items.
Concurrent Validity
Table 6 displays the results of regression analyses assessing concurrent validity of the expanded and original ACEs scales. As can be seen in this table, there were robust associations between both ACEs measures versus measures of mental wellbeing, anxiety and depression, and perceived stress. The associations with physical wellbeing were much smaller.
Table 6.
Concurrent Validity of the ACEs Scale in Study 1 and 2
| Expanded ACEs scale | Original ACEs scale | |||||
|---|---|---|---|---|---|---|
| B (SE) |
β
(95% CI) |
t
(p) |
B (SE) |
β
(95% CI) |
t
(p) |
|
| Study 1 | ||||||
| SF-36 Physical Summary |
−0.57 (0.29) |
−.08 (−.15- -.0003) |
−1.97 (.05) |
−0.51 (0.37) |
−.05 (−.13- -.02) |
−1.40 ns |
| SF-36 Mental Summary |
−6.22 (0.52) |
−.41 (−.47 - -.34) |
−11.90 (< .001) |
−6.36 (0.67) |
−.33 (−.40 - -.26) |
−9.44 (< .001) |
| HSCL |
0.37 (0.05) |
.41 (.31–.51) |
8.32 (< .001) |
0.33 (0.06) |
.29 (.18–.39) |
5.54 (< .001) |
| Perceived Stress Scale (PSS) |
2.43 (0.20) |
.31 (.26–.36) |
12.35 (<.001) |
2.57 (0.25) |
.26 (.21–.31) |
10.18 (<.001) |
| Study 2 | ||||||
| SF-36 Physical Summary |
0.13 (1.15) |
.01 (−.22–.25) |
0.11 ns |
−0. 25 (0.50) |
−.06 (−.30–.17) |
−0.51 ns |
| SF-36 Mental Summary |
−9.30 (1.88) |
−.51 (−.71 - -.31) |
4.96 (<.001) |
−2.80 (0.88) |
−.36 (−.57 - -.14) |
−3.18 (< .001) |
| HSCL |
0.55 (0.09) |
.58 (.39–.77) |
5.93 (< .001) |
0.17 (0.04) |
.41 (.20–.63) |
3.79 (< .001) |
| Perceived Stress Scale (PSS) |
3.56 (1.05) |
.38 (.16–.61) |
3.39 (.001) |
1.08 (0.50) |
.27 (.04–.50) |
2.29 (.03) |
ACE = adverse childhood experiences. B = unstandardized beta. Β = standardized beta. HSCL = Hopkins Symptom Checklist-10. ns = not significant. SF-36 = Short Form-36. The linear regression analyses controlled for gender and average parent education; however, only the results pertaining to the ACEs variable are reported in this table
Preliminary Conclusions
Results show that substantial numbers of undergraduates at a large university report a disturbing number of ACEs. An EFA on a random half of the sample indicated that the two JVQ items inquiring about severe accidents and illnesses of loved ones did not fit with the rest. After these items were dropped, results yielded a four-factor model, with the factors consisting of child maltreatment, household dysfunction, community dysfunction, and peer dysfunction/property victimization. A CFA with these four factors on the second half of the sample yielded a satisfactory fit, and the four factors were strongly inter-correlated. The expanded ACEs measure was internally consistent. It was also correlated with measures of mental health and perceived stress, and to a lesser degree, with physical well-being. Results support its concurrent validity.
Study 2
In Study 2, in addition to examining internal consistency and concurrent validity, we examined replicability of the frequencies of ACEs in a smaller, independent sample. We further determined test-retest reliability, and convergent and predictive validity of the expanded ACEs measure. We expected to replicate the results of the first study. We further expected that the expanded measure would have acceptable levels of test-retest reliability and convergent validity with established measures of stressful and traumatic events, and we expected that ACEs scores would predict deterioration in mental health over the course of a semester.
Method
Participants
Participants were recruited from psychology classes, as in in Study 1. Out of 75 participants who completed the full survey at Time 1, 69 completed it at Time 2, resulting in a completion rate of 92% for calculations of test-retest reliability and predictive validity. Average age was 20.0 (SD = 1.5, range = 18–26). Participants predominantly self-identified as female (84%). As in Study 1, most participants were White (79%) or Asian (16%), with a smaller number of multiracial (3%), Native American (1%), or of another race (1%).
Measures
ACEs
Based on the results of the EFA in Study 1, we excluded the two items on accidents and illnesses from analyses in Study 2. The other items were the same as in Study 1.
Mental and Physical Health
SF-36 was used to assess health, as in Study 1.
Anxiety and Depression
Anxiety and depression were assessed on the HSCL, as in Study 1. Internal consistency was .92 at both Time 1 and 2.
Perceived Stress
The PSS was used, as in Study 1. Internal consistency was .91 at both Time 1 and 2.
Parental Education
This measure was the same as in Study 1.
Childhood Trauma
Convergent validity was assessed with the 25-item CTQ—Short Form (Bernstein et al. 2003). This scale assesses different forms of trauma experienced “growing up as a child and teenager” and covers emotional and physical neglect and abuse, and sexual abuse. Participants rated their responses on a 5-point scale (1 = never true and 5 = very often true). Some items were worded in the opposite direction to reduce response bias. Scores were averaged to yield a total score that could range from 1 to 5, with higher numbers indicating greater trauma. Internal consistency was 0.93 at Time 1 and 0.95 at Time 2.
Stressful Life Events
Convergent validity was also assessed with the Stressful Life Events Screening Questionnaire—Revised (SLESQ; Green and Green 2006). This 13-item measure assesses significantly stressful events experienced during one’s entire life (e.g., a life-threatening illness, physical or sexual abuse). As our goal was simply to establish convergent validity, we only asked about the presence of the 13 events and did not probe further details. Internal consistency in the current sample was 0.75 at Time 1 and 0.68 at Time 2.
Procedure
Participants were administered two surveys, once at the beginning and once at the end of the semester. The average interval between administrations was 48.8 days (SD = 15.3). The rest of the procedure was the same as in Study 1. The study was approved by the IRB.
Data Analyses
Initial data checks were conducted as in Study 1. ACEs scores on the expanded scale were again log-transformed. HSCL, CTQ and SLESQ scores and ACEs scores on the original scale were too skewed to be normalized through transformations. We used Pearson product-moment correlations for normally distributed variables and Kendall’s τ to assess correlations for non-normally distributed variables. A Wilcoxon signed-rank test was used to examine changes in HSCL from Time 1 to 2. Predictive validity was assessed with linear regressions that controlled for gender and average parent education. In addition, we report Cohen’s kappa and percent agreement statistics for test-retest reliability of individual items.
Results
Replicability
As can be seen in the Appendix, the proportions of students endorsing each item in Study 1 were similar to those at Time 1 in Study 2.
Internal Consistency
Internal consistency was .84 for the expanded scale at both Time 1 and 2, replicating the results of Study 1. Internal consistency for the original scale was .74 at Time 1 and .71 at Time 2.
Test-Retest Reliability
Test-retest reliability was good for both the expanded ACEs scale, r (67) = .77 and the original ACEs scale, τ = .79. Test-retest reliability was also acceptable for SF-36 Mental Summary (r = .81), HSCL (τ = .62), Perceived Stress Scale (r = .76), CTQ (τ = .60), and SLESQ (τ = .66). All correlations were significant at p < .001.
The median number of ACEs on the expanded scale was at 3 at both times. Although the average number of ACEs dropped slightly from 4.0 (SD = 4.0) at Time 1 to 3.8 (SD = 3.9) at Time 2 among students who completed the survey at both times, a dependent-samples t test showed that the difference was not significant. As can be seen in the Appendix, which shows the percentage agreement between Time 1 and Time 2, participants responded somewhat less reliably to certain items assessing several kinds of peer and property victimization. However, percent agreement between Time 1 and 2 was over 90% for the large majority of the items.
Concurrent Validity
As shown in Table 6, correlations between the ACEs measures and measures of concurrent validity replicated the results of Study 1.
Convergent Validity
Correlations between the 31-item ACEs measure and the other measures of stressful events and trauma at Time 1 were significant (SLEQ: τ = .43, p < .001; CTQ: τ = .54, p < .001). The original ACEs scale was also significantly correlated with these measures (SLEQ: τ = .29, p = .003, CTQ: τ = .47, p < .001).
Predictive Validity
To assess deterioration in functioning, we subtracted scores at Time 2 from scores at Time 1 for Mental Summary, HSCL, and Perceived Stress. Thus, positive scores indicate deterioration. Students showed little change in Mental Summary (M = 0.3, SD = 9.2) and Perceived Stress (M = −0.4, SD = 4.8) over the 7 weeks of the study. Neither difference was significant. Although the change in HSCL scores was also small (M = 0.2, SD = 0.6), a Wilcoxon signed-rank test showed that the difference was significant, V = 565.5, p = .006.
To examine the predictive validity of the expanded ACEs measure, we conducted separate regressions on deterioration in Mental Summary, HSCL, and Perceived Stress scores, each with the log-transformed ACEs scores at Time 1 as the predictor and average parental education and gender as covariates. None of the results for ACEs, gender or parental education was significant, with standardized betas (βs) for ACEs ranging from −.12 to .14. The same was true for the original scale as well, with βs for ACEs ranging from −.07 to .20.
Discussion
Frequencies of ACEs
A key finding of this study is that undergraduates at a large Midwestern university, most of whom are White and middle class, report being exposed to disturbingly high levels of ACEs. Across five studies with independent samples, 43–45% of the participants reported feeling socially isolated as they were growing up, 39–41% reported witnessing domestic verbal abuse, 28–32% reported having been verbally bullied by peers or siblings, 35–39% reported that someone stole their property, 30–32% reported growing up with a family member who was diagnosed with a psychiatric disorder or attempted suicide, and 12–13% reported having been physically abused by their caregivers (please see the Appendix for more information on other items). These findings highlight the importance of paying attention to ACEs in interventions aimed at improving the mental health of college students. At a minimum, greater efforts should be made to increase awareness of faculty and staff about ACEs in general and about the frequencies of ACEs in students they work with so that they can be vigilant about these risk factors and make appropriate referrals as needed. The focus of the current study is on the psychometric properties of the ACEs scale, but we discuss the issue of high frequencies of ACEs in college students in other manuscripts (Karatekin 2018a, b; Karatekin and Ahluwalia 2016).
Factorial Structure and Internal Consistency of the ACEs Measures
An EFA and a CFA of the original ACEs scale confirmed the conceptualization of the items in terms of child maltreatment and household dysfunction, which are correlated with each other. However, when we included additional items, a different factorial structure emerged. An EFA of the expanded scale revealed that early adversity related to serious illnesses and accidents of loved ones clearly did not fit with the 31 other types of adversity assessed on this scale. In their study of a revised inventory of ACEs, Finkelhor and colleagues (Finkelhor et al. 2015) also argued for the omission of items related to serious accidents and illnesses of loved ones. We concur with this suggestion. After these items were dropped, an EFA yielded four factors: (1) child maltreatment, (2) family dysfunction, (3) community dysfunction, and (4) peer dysfunction/property victimization. A CFA confirmed that this four-factor model was a good fit to the data. Furthermore, the factors were strongly correlated.
The 31-item ACEs measure also showed good internal consistency in both Study 1 and 2 (.84–.85), which was similar to the consistency of .74 to .81 for the original ACEs scale (Bruskas 2013; Ford et al. 2014; Mersky et al. 2017) and .80 for the JVQ (Finkelhor et al. 2005).
Results replicate and extend the moderate to high correlations found among latent factors in previous factorial analyses of the original ACEs scale (Ford et al. 2014; Meinck et al. 2017; Mersky et al. 2017), and the inter-relatedness of the items (Felitti et al. 1998).
Replicability and Test-Retest Reliability of the Expanded ACEs Measure
Results were replicable across independent samples. Distributions of ACEs were similar across the four samples in Study 1 (Fig. 1), and percentages of students endorsing each ACE were consistent between Study 1 and Study 2 (Appendix).
Test-retest reliability of the sum of ACEs on the expanded ACEs scale (r = .77) was acceptable. Percentage agreement for individual items between the two administrations ranged from 75 to 100%. Kappas were low for several questions related to attacks by peers and property victimization, consistent with lower test-retest reliabilities of these items on the JVQ in 10- to 17-year-olds (Finkelhor et al. 2005).
Previous studies of the total score for the original ACEs scale found test-retest reliability of .60 across 9 months in maltreated Portuguese youth (Pinto et al. 2014), .64 across 20 months in adult patients at a primary care clinic (Dube et al. 2004), .71 across a year in college athletes (Zanotti et al. 2017), and .90 across 9 months in low-income women (Mersky et al. 2017). The current reliability (τ = .79) over 7 weeks for the original ACEs questions was in this range.
Convergent and Concurrent Validity of the Expanded ACEs Measure
Convergent validity with measures of traumatic and stressful events was acceptable, and the expanded 31-item measure was moderately to strongly associated with concurrent measures of mental health and perceived stress. Findings replicate and extend previous studies of the original ACEs measure (Anda et al. 2006; Wingenfeld et al. 2011) and the JVQ (Finkelhor et al. 2005). Indeed, the associations between the original ACEs items and the PSS (β = .26 in both Study 1 and 2) were essentially identical to the correlation of .27 found by in a study using the same measures in a similarly large sample of low-income women (Mersky et al. 2017). The lack of association of ACEs with physical health in the current sample may be due to the fact that participants were young and that our self-report measure of physical health was not sensitive to fine-grained indicators of physical problems.
Predictive Validity of the Expanded ACEs Measure
The expanded ACEs scale did not predict deterioration in mental health or stress over 7 weeks. This could be attributable to the lack of clinically significant change on the outcome measures during the relatively short test-retest interval.
What Are ACEs and why Does their Definition Matter?
Why does it matter how one defines ACEs? First, it matters if one wishes to develop a theory that includes ACEs. A good theory requires well-defined explanatory constructs as building blocks that can then be related in a systematic manner to other well-defined constructs and observable measures in a “nomological network” (Cronbach and Meehl 1955). In turn, a good theory can lead to a better understanding of the phenomena under study, the mechanisms of action underlying the relationship between predictors and outcomes, and how these unfold over time. A better theoretical understanding can then lead to more effective and targeted interventions. The definition also matters because the definition of the problem, which is a matter of choice, shapes the solutions that can be imagined. As noted before, ACEs research has been used as an “advocacy tool” (Finkelhor et al. 2015). If researchers choose to conceptualize ACEs as only including child maltreatment and household dysfunction, then the solutions they will advocate for will focus on the individual and the family (e.g., individual or family therapy, parenting skills training). If ACEs are defined more broadly and their interconnectedness is highlighted, then proposed solutions will be broader, such as addressing the structural roots of unemployment, community violence, and limited educational opportunities (Metzler et al. 2017).
Currently, there is no consensus among researchers on the definition of ACEs. For example, some researchers include indicators of general poverty, changes in residency, and death of a parent or sibling in their list (Björkenstam et al. 2013; Dunn et al. 2011; Finkelhor et al. 2015; Giovanelli et al. 2016; Harkonmäki et al. 2007; Korkeila et al. 2010). After reviewing the literature on the definition of ACEs, Kalmakis and Chandler (2014) proposed that ACEs should be defined as “childhood events, varying in severity and often chronic, occurring within a child’s family or social environment that cause harm or distress, thereby disrupting the child’s physical or psychological health or development” (p. 1495). This broad definition would characterize any event with any negative consequences as an ACE and risks being circular. Some define ACEs as either stressful or traumatic events (Austin and Herrick 2014; S. M. Brown and Heneghan 2017), whereas others define them as traumatic experiences (Layne et al. 2014) or “traumatic stressors” (Anda et al. 2010) or simply enumerate the original ACEs (Bellis et al. 2014a, b; Burke et al. 2011). However, given that there is a multitude of risk factors that could be viewed as childhood adversities, the lack of a clear definition makes any subset of specific adversities somewhat arbitrary.
Of even greater concern, it is not always clear in published research whether ACEs refer to a construct (e.g., “early adversity,” an explanatory variable that is not observable), or a particular operationalization of that construct, or whether they simply represent the sum of a number of somewhat arbitrarily determined risk factors, with no assumption regarding an underlying construct. Each individual item on the original ACEs scale can be treated as a specific risk factor and not as a hypothetical construct. However, when these are added together and given the label “adverse childhood experiences,” there may develop an implicit tendency toward an acknowledgment that these particular experiences represent something greater than the sum of their parts. As a result, ACEs as the items on the original scale and ACEs as an explanatory construct sometimes tend to be conflated, as the same phrase (“ACEs”) is used to describe both.
Also unclear is whether ACEs should refer to a list of objectively verifiable events or subjective experiences of those events. The term refers to adverse “experiences,” which implies that it is not the event itself but the internal processing of the event that matters. However, the items on the original ACEs scale are a mix of objective events (e.g., parental incarceration), which are presumably adverse experiences for everyone, and purely subjective experiences (e.g., feeling psychologically neglected).
Casting a broad, atheoretical net for any kind of adversity associated with any negative outcome might help identify individuals at risk but hinders a clear understanding of the phenomena and the development of effective interventions. The goal of the current study was not to provide a definitive definition of ACEs but to highlight the limitations in the original definition and to demonstrate that a scale that covers a broader range of ACEs is psychometrically sound. Nevertheless, the results have some implications for researchers who wish to develop a more cogent definition of ACEs.
First, results suggest that not every experience of adversity in childhood should be included in the definition of “adverse childhood experiences.” The fact that items related to serious illness and accidents of loved ones clearly stood apart from the rest of the adversities in the current study, as well as in a previous study (Finkelhor et al. 2015), contradicts the notion of undifferentiated adversity.
Second, the factorial structure of the expanded ACEs scale also contradicts the notion of undifferentiated adversity. We showed that the 31 items can be grouped into coherent clusters, but that the clusters are inter-related. The current results, along with previous research summarized earlier on the inter-relatedness of specific items and factors, are consistent with a multi-faceted but unitary view of ACEs.
Third, the definition of ACEs as a construct depends on the items included in measures assessing ACEs. The original ACEs scale included only items related to child maltreatment and household dysfunction, and the construct has come to be equated with these two factors. When we expanded the ACEs scale with another well-established measure of childhood adversities, we found two additional factors, related to community dysfunction and peer dysfunction/property victimization.
Fourth, the meaning of individual items may change depending on the other items included in the measure. On the original ACEs scale, sexual abuse by grown-ups loads onto a “child maltreatment” factor, and parental incarceration loads onto a “household dysfunction” factor. On the expanded ACEs scale, both of these items loaded more highly onto the “community dysfunction” factor than onto either the “household dysfunction” and “child maltreatment” factors. In other words, in the context of one ACE scale, these items would be conceptualized as problems with the caregivers, whereas in the context of an expanded scale, they are better conceptualized as reflecting a wider dysfunction in the community.
So far, we discussed several empirical findings that should be considered in the definition of ACEs as a risk factor. However, it is important to acknowledge that this definition also involves choices about what ACEs should predict. So far, the vast majority of research on ACEs has focused on long-term health consequences. However, studies have also shown associations between ACEs and other outcomes, such as failure to graduate from high school, unemployment and underemployment, arrest, and incarceration (Bellis, Lowey, et al., 2014; Giovanelli et al. 2016; Liu et al. 2013; Metzler et al. 2017). The optimal set of ACEs that constitute risk for poor health may be different from the set of ACEs that constitute risk for other consequences. It may also be that the ACEs lead to negative outcomes such as unemployment and incarceration through their effects on health or health risk behaviors. Lack of clarity about the construct and what it is a risk for result in a lack of clarity about mechanisms of risk versus outcomes.
We propose that, to advance the field, researchers work toward a more cogent and developmentally informed definition of early adversity as a hypothetical, explanatory construct and refer to specific ACEs scales as particular operationalizations of this construct. We suggest that the 31 items used in the current study might be reflecting early experiences of victimization and helplessness in the face of perceived intentional emotional and physical threats or actual harm by others. Although they may not all be “traumatic” by themselves, the current results demonstrate that their cumulative impact is associated with poor mental health in young adults. This definition might be a starting point for examining whether these 31 items have good content validity and whether this definition holds up better than other possible definitions of early adversity.
We also strongly encourage researchers not to limit their definition to adversities that occur solely or mostly within the child’s immediate family. Otherwise, consequential adversities that occur outside the household (e.g., bullying by peers), as well as the societal context of the adversities within the household, are in danger of being ignored, and potentially effective interventions might be missed. Felitti and colleagues (Felitti et al. 1998) initiated the current wave of ACEs research by warning researchers focusing only on specific types of maltreatment that “without measuring these household factors as well, long-term influence might be wrongly attributed solely to single types of abuse and the cumulative influence of multiple categories of adverse childhood experiences would not be assessed” (p. 246). Given the strong associations between adversities inside and outside the home found in the current study, we would like to extend this notion by suggesting that without a broader understanding of early adversity, long-term influences might be wrongly attributed solely to individual and familial causes at the risk of overlooking societal determinants of health.
Finally, a robust definition of early adversity needs to be grounded in research with more diverse populations than the one included in the current study. We tested a convenience sample of undergraduates at a large Midwestern university, which consisted predominantly of Whites and females. Rates of specific adversities included in the expanded scale are likely to differ across populations, which may affect the psychometric properties of the scale. Other researchers highlight the importance of other adversities (e.g., those related to historical trauma, forced marriages, refugee status, being conscripted into armies, growing up in urban poverty) in other populations (Anda et al. 2010; Wade et al. 2014). More research is needed to determine whether additional factors should be considered in different populations and whether different items may be necessary to tap into the factors that emerged in the current study. It is also an open question whether mechanisms of action might be similar across different populations despite differences in particular adversities (e.g., experiences of perceived victimization may lead to poor health through the same psychobiological mechanisms in different populations, even though the specific types of victimization may differ).
Conclusions
We conclude that the psychometric properties of the expanded, 31-item ACEs scale are acceptable enough to be used with the types of college students investigated in this study. However, two important types of validity we did not assess in the current study are content and construct validity, as there is no consensus in the research literature on the definition of ACEs. More research is needed to clarify the definition of ACEs as a construct and to establish the construct validity of measures of ACEs across different populations, while being cognizant of the consequences of the choices one makes regarding the types of adversities included in this definition.
Appendix
Table 7.
The Expanded ACEs Questionnaire
| Proportion who endorsed the question (Study 1; N = 1480) | Proportion who endorsed the question at Time 1 (Study 2) | Cohen’s κ (Study 2) | % agreement (Study 2) | Correlation with scale composed of remaining items (Study 1) | |
|---|---|---|---|---|---|
| 1. Did you get scared or feel really bad because grown-ups who took care of you (for example, parents, adult relatives, other adults who lived with you) called you names, said mean things to you, or said they didn’t want you? | 19% | 16% |
.66 (p < .001) |
90% | .49 |
| 2. Did you often feel that no one in your family loved you or thought you were important or special? Or did you feel that your family members didn’t look out for each other, feel close to each other, or support each other? | 18% | 12% |
.72 (p < .001) |
94% | .48 |
| 3. Not including spanking on your bottom, did grown-ups who took care of you (for example, parents, adult relatives, other adults who lived with you) ever hit, beat, kick, or physically hurt you in any way? | 13% | 12% |
.67 (p < .001) |
93% | .44 |
| 4. Did any grown-up in your life (whether you knew him/her or not) touch your private parts when they shouldn’t have or make you touch their private parts? Or did a grown-up force you to have sex, that is sexual intercourse of any kind? | 5% | 4% |
1.0 (p < .001) |
100% | .27 |
| 5. When someone is neglected, it means that the grown-ups in their life didn’t take care of them the way they should. They might not get them enough food, take them to the doctor when they are sick, or make sure they have a safe place to stay. Were you neglected? | 4% | 5% |
.85 (p < .001) |
99% | .35 |
| 6. Was a member of your household diagnosed with depression, bipolar disorder, anxiety, or other psychiatric disorder? Or did a household member attempt suicide? | 30% | 32% |
.78 (p < .001) |
91% | .31 |
| 7. Was there a time that a member of your household drank or used drugs so often that it caused problems? | 19% | 12% |
.93 (p < .001) |
99% | .38 |
| 8. Was there a time when a grown-up member of your household (for example, a parent, step-parent, an adult relative, your parent’s boyfriend or girlfriend) was arguing with, yelling at, and angry at another grown-up family member a lot of the time? | 39% | 41% |
.75 (p < .001) |
88% | .50 |
| 9. Did you SEE a grown-up in your household get pushed, slapped, hit, punched, beat up, or hurt with or threatened with a weapon by another grown-up in the house? | 11% | 16% |
.62 (p < .001) |
91% | .46 |
| 10. Did you SEE a grown-up member of your household hit, beat, kick or physically hurt your brothers or sisters, not including a spanking on the bottom? | 9% | 11% |
.68 (p < .001) |
94% | .46 |
| 11. Did a parent, or someone who was like a parent to you (for example, a step-parent, guardian, close adult relative), have to go to prison? | 4% | 3% |
.79 (p < .001) |
99% | .31 |
| 12. Did a parent, or someone who was like a parent to you, die for reasons other than being murdered? | 7% | 11% |
.75 (p < .001) |
96% | .24 |
| 13. Were your parents separated or divorced? | 22% | 27% |
1.0 (p < .001) |
100% | .30 |
| 14. Did a parent, or someone who was like a parent to you, have to leave the country to fight in a war and was gone for several months or longer? | 3% | 1% |
n/a (too few positives) |
99% | .23 |
| 15. Were you sent away or taken away from a parent or your family for any reason (not including voluntary separations, such as going to summer camp)? | 4% | 4% |
.65 (p < .001) |
97% | .30 |
| 16. Sometimes people are attacked with sticks, rocks, guns, knives, or other things that would hurt. Did other kids, your siblings, or a girlfriend or boyfriend hit or attack you on purpose WITH an object or weapon? Somewhere like: at school, at a store, in a car, on the street, or anywhere else? | 6% | 4% |
.38 (p = .001) |
96% | .41 |
| 17. Did other kids, your siblings, or a girlfriend or boyfriend threaten to physically hurt you when you thought they might really do it? | 13% | 9% |
.27 (p = .025) |
88% | .46 |
| 18. Did you get scared or feel really bad because other kids, your siblings, your girlfriend or boyfriend were calling you names, saying mean things to you, or saying they didn’t want you around? | 28% | 32% |
.79 (p < .001) |
91% | .47 |
| 19. Did other kids, your siblings, a boyfriend, or a girlfriend force you to do sexual things? | 8% | 11% |
.58 (p < .001) |
93% | .33 |
| 20. Were you hit or attacked because of your skin color, religion, or where your family comes from? Because of a physical problem you have? Or because someone said you were gay? | 3% | 3% |
.49 (p < .001) |
97% | .31 |
| 21. Excluding instances where you were hit or attacked because of your skin color, religion, physical disability, sexual orientation, or where your family comes from, did you FEEL discriminated against because of these characteristics? | 16% | 12% |
.40 (p = .001) |
87% | .35 |
| 22. Did you SEE anyone in real life get attacked on purpose WITH a stick, rock, gun, knife, or other thing that would hurt? Somewhere like: at school, at a store, in a car, on the street, or anywhere else outside of home? | 13% | 11% |
.45 (p < .001) |
91% | .37 |
| 23. Did anyone steal something from your house that belongs to your family or someone you lived with? Things like a TV, stereo, car, or anything else? | 18% | 13% |
.31 (p = .007) |
90% | .33 |
| 24. Was anyone close to you (for example, a family member, a friend, or neighbor) murdered? | 3% | 3% |
1.0 (p < .001) |
100% | .23 |
| 25. Did you see someone murdered in real life (not on TV, video games, or in the movies)? | 2% | 1% | n/a | 100% | .21 |
| 26. Were you in any place in real life where you could see or hear people being shot, bombs going off, or street riots? | 6% | 7% |
.55 (p < .001) |
96% | .27 |
| 27. Were you in the middle of a war where you could hear real fighting with guns or bombs? | 1% | 0% | n/a | 100% | .20 |
| 28. Did anyone steal something from you and never give it back? Things like a backpack, money, watch, clothing, bike, stereo, or anything else? | 35% | 39% |
.45 (p < .001) |
75% | .33 |
| 29. Did anyone use force to take something away from you that you were carrying or wearing? | 6% | 9% |
−.07 (ns) |
87% | .31 |
| 30. Did anyone break or ruin any of your things on purpose? | 24% | 24% |
.32 (p = .007) |
75% | .41 |
| 33. Was there a period of time when you had no really good friends and there was no one else you felt close to? | 43% | 45% |
.62 (p < .001) |
81% | .39 |
Items 1–7, 9, 11, and 13 are based on the original ACEs scale. ACE = adverse childhood experiences. The two questions that were omitted from the analyses after the EFA were (31) “Did someone you were really close to have a VERY BAD illness (e.g., heart attack, stroke, cancer) where he or she had to be in the hospital a lot? This would be someone important to you, like a family member or best friend” and (32) “Did someone you were really close to have a VERY BAD accident (e.g., a traffic accident) where he or she had to be in the hospital for many days? Again, this would be someone important to you, like a family member or best friend.” In Study 1, 39% and 18% of the sample, respectively, endorsed these items
Compliance with Ethical Standards
Conflict of Interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Afifi TO, Mather A, Boman J, Fleisher W, Enns MW, MacMillan H, Sareen J. Childhood adversity and personality disorders: Results from a nationally representative population-based study. Journal of Psychiatric Research. 2011;45:814–822. doi: 10.1016/j.jpsychires.2010.11.008. [DOI] [PubMed] [Google Scholar]
- Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield CH, Perry BD, et al. The enduring effects of abuse and related adverse experiences in childhood. European Archives of Psychiatry and Clinical Neuroscience. 2006;256(3):174–186. doi: 10.1007/s00406-005-0624-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anda RF, Brown DW, Dube SR, Bremner JD, Felitti VJ, Giles WH. Adverse childhood experiences and chronic obstructive pulmonary disease in adults. American Journal of Preventive Medicine. 2008;34:396–403. doi: 10.1016/j.amepre.2008.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anda RF, Butchart A, Felitti VJ, Brown DW. Building a framework for global surveillance of the public health implications of adverse childhood experiences. American Journal of Preventive Medicine. 2010;39(1):93–98. doi: 10.1016/j.amepre.2010.03.015. [DOI] [PubMed] [Google Scholar]
- Austin AE, Herrick HW. The effect of adverse childhood experiences on adult health: 2012 North Carolina Behavioral Risk Factor Surveillance System Survey. Raleigh: North Carolina Department of Health and Human Services, Division of Public Health; 2014. [Google Scholar]
- Bellis MA, Hughes K, Leckenby N, Jones L, Baban A, Kachaeva M, Povilaitis R, Pudule I, Qirjako G, Ulukol B, Raleva M, Terzic N. Adverse childhood experiences and associations with health-harming behaviours in young adults: Surveys in eight eastern European countries. Bulletin of the World Health Organization. 2014;92(9):641–655. doi: 10.2471/BLT.13.129247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellis MA, Lowey H, Leckenby N, Hughes K, Harrison D. Adverse childhood experiences: Retrospective study to determine their impact on adult health behaviours and health outcomes in a UK population. Journal of Public Health. 2014;36(1):81–91. doi: 10.1093/pubmed/fdt038. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, Stokes J, Handelsman L, Medrano M, Desmond D, Zule W. Development and validation of a brief screening version of the childhood trauma questionnaire. Child Abuse & Neglect. 2003;27(2):169–190. doi: 10.1016/S0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- Björkenstam E, Hjern A, Mittendorfer-Rutz E, Vinnerljung B, Hallqvist J, Ljung R. Multi-exposure and clustering of adverse childhood experiences, socioeconomic differences and psychotropic medication in young adults. PLoS One. 2013;8:e53551. doi: 10.1371/journal.pone.0053551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown, T. A. (2014). Confirmatory factor analysis for applied research. Guilford Publications.
- Brown SM, Heneghan AM. Childhood adversity and the risk of substance use and delinquency: The role of protective adult relationships. Child Abuse & Neglect. 2017;63:211–221. doi: 10.1016/j.chiabu.2016.11.006. [DOI] [PubMed] [Google Scholar]
- Bruskas D. Adverse childhood experiences and psychosocial well-being of women who were in foster care as children. The Permanente Journal. 2013;17(3):e131–e141. doi: 10.7812/TPP/12-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke NJ, Hellman JL, Scott BG, Weems CF, Carrion VG. The impact of adverse childhood experiences on an urban pediatric population. Child Abuse & Neglect. 2011;35(6):408–413. doi: 10.1016/j.chiabu.2011.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark C, Caldwell T, Power C, Stansfeld SA. Does the influence of childhood adversity on psychopathology persist across the lifecourse? A 45-year prospective epidemiologic study. Annals of Epidemiology. 2010;20:385–394. doi: 10.1016/j.annepidem.2010.02.008. [DOI] [PubMed] [Google Scholar]
- Cohen S, Williamson G. Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S, editors. The Social Psychology of Health: The Claremont Symposium on Applied Social Psychology. Sage: Newbury Park; 1988. pp. 31–67. [Google Scholar]
- Cortina JM. What is coefficient alpha? An examination of theory and applications. Journal of Applied Psychology. 1993;78(1):98–104. doi: 10.1037/0021-9010.78.1.98. [DOI] [Google Scholar]
- Costello AB, Osborne JW. Best practices in exploratory factor analysis: Four recommendations for getting the most from your analysis. Exploratory Factor Analysis. 2005;10(7):9. [Google Scholar]
- Cronbach LJ, Meehl PE. Construct validity in psychological tests. Psychological Bulletin. 1955;52(4):281–302. doi: 10.1037/h0040957. [DOI] [PubMed] [Google Scholar]
- Dong M, Anda RF, Felitti VJ, Dube SR, Williamson DF, Thompson TJ, Loo CM, Giles WH. The interrelatedness of multiple forms of childhood abuse, neglect, and household dysfunction. Child Abuse & Neglect. 2004;28(7):771–784. doi: 10.1016/j.chiabu.2004.01.008. [DOI] [PubMed] [Google Scholar]
- Dube SR, Williamson DF, Thompson T, Felitti VJ, Anda RF. Assessing the reliability of retrospective reports of adverse childhood experiences among adult HMO members attending a primary care clinic. Child Abuse & Neglect. 2004;28(7):729–737. doi: 10.1016/j.chiabu.2003.08.009. [DOI] [PubMed] [Google Scholar]
- Dunn VJ, Abbott RA, Croudace TJ, Wilkinson P, Jones PB, Herbert J, Goodyer IM. Profiles of family-focused adverse experiences through childhood and early adolescence: The ROOTS project a community investigation of adolescent mental health. BMC Psychiatry. 2011;11(1):109. doi: 10.1186/1471-244X-11-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felitti VJ. Childhood sexual abuse, depression, and family dysfunction in adult obese patients: A case control study. Southern Medical Journal. 1993;86(7):732–736. doi: 10.1097/00007611-199307000-00002. [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences (ACE) study. American Journal of Preventive Medicine. 1998;14(4):245–258. doi: 10.1016/S0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Hamby SL, Ormrod R, Turner H. The juvenile victimization questionnaire: Reliability, validity, and national norms. Child Abuse & Neglect. 2005;29(4):383–412. doi: 10.1016/j.chiabu.2004.11.001. [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Shattuck A, Turner HA, Ormrod R, Hamby SL. Polyvictimization in developmental context. Journal of Child & Adolescent Trauma. 2011;4(4):291–300. doi: 10.1080/19361521.2011.610432. [DOI] [Google Scholar]
- Finkelhor D, Shattuck A, Turner H, Hamby S. Improving the adverse childhood experiences study scale. JAMA Pediatrics. 2013;167:70–75. doi: 10.1001/jamapediatrics.2013.420. [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Shattuck A, Turner H, Hamby S. A revised inventory of adverse childhood experiences. Child Abuse & Neglect. 2015;48:13–21. doi: 10.1016/j.chiabu.2015.07.011. [DOI] [PubMed] [Google Scholar]
- Ford DC, Merrick MT, Parks SE, Breiding MJ, Gilbert LK, Edwards VJ, Dhingra SS, Barile JP, Thompson WW. Examination of the factorial structure of adverse childhood experiences and recommendations for three subscale scores. Psychology of Violence. 2014;4(4):432–444. doi: 10.1037/a0037723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giovanelli, A., Reynolds, A. J., Mondi, C. F., & Ou, S.-R. (2016). Adverse childhood experiences and adult well-being in a low-income, urban cohort. Pediatrics, 137(4). 10.1542/peds.2015-4016. [DOI] [PMC free article] [PubMed]
- Green G, Green BL. Evaluating the cultural validity of the stressful life events screening questionnaire. Violence Against Women. 2006;12(12):1191–1213. doi: 10.1177/1077801206294534. [DOI] [PubMed] [Google Scholar]
- Hamby SL, Finkelhor D. The victimization of children: Recommendations for assessment and instrument development. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39(7):829–840. doi: 10.1097/00004583-200007000-00011. [DOI] [PubMed] [Google Scholar]
- Hardt J, Vellaisamy P, Schoon I. Sequelae of prospective versus retrospective reports of adverse childhood experiences. Psychological Reports. 2010;107(2):425–440. doi: 10.2466/02.04.09.10.16.21.PR0.107.5.425-440. [DOI] [PubMed] [Google Scholar]
- Harkonmäki K, Korkeila K, Vahtera J, Kivimäki M, Suominen S, Sillanmäki L, Koskenvuo M. Childhood adversities as a predictor of disability retirement. Journal of Epidemiology and Community Health. 2007;61(6):479–484. doi: 10.1136/jech.2006.052670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalmakis KA, Chandler GE. Adverse childhood experiences: Towards a clear conceptual meaning. Journal of Advanced Nursing. 2014;70(7):1489–1501. doi: 10.1111/jan.12329. [DOI] [PubMed] [Google Scholar]
- Karatekin, C. (2018a). Adverse childhood experiences (ACEs) and help-seeking for health-related interventions in young adults. Journal of Psychology: Interdisciplinary and Applied. 10.1080/00223980.2018.1476316 [DOI] [PubMed]
- Karatekin C. Adverse childhood experiences (ACEs), stress and mental health in college students. Stress and Health. 2018;34:36–45. doi: 10.1002/smi.2761. [DOI] [PubMed] [Google Scholar]
- Karatekin, C., & Ahluwalia, R. (2016). Effects of adverse childhood experiences, stress, and social support on the health of college students. Journal of Interpersonal Violence. 10.1177/0886260516681880. [DOI] [PubMed]
- Korkeila J, Vahtera J, Nabi H, Kivimäki M, Korkeila K, Sumanen M, Koskenvuo K, Koskenvuo M. Childhood adversities, adulthood life events and depression. Journal of Affective Disorders. 2010;127:130–138. doi: 10.1016/j.jad.2010.04.031. [DOI] [PubMed] [Google Scholar]
- Layne CM, Greeson JKP, Ostrowski SA, Kim S, Reading S, Vivrette RL, et al. Cumulative trauma exposure and high risk behavior in adolescence: Findings from the National Child Traumatic Stress Network Core Data set. Psychological Trauma: Theory, Research, Practice, and Policy. 2014;6(Suppl 1):S40–S49. doi: 10.1037/a0037799. [DOI] [Google Scholar]
- Liu Y, Croft JB, Chapman DP, Perry GS, Greenlund KJ, Zhao G, Edwards VJ. Relationship between adverse childhood experiences and unemployment among adults from five US states. Social Psychiatry and Psychiatric Epidemiology. 2013;48(3):357–369. doi: 10.1007/s00127-012-0554-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meinck F, Cosma AP, Mikton C, Baban A. Psychometric properties of the adverse childhood experiences abuse short form (ACE-ASF) among Romanian high school students. Child Abuse & Neglect. 2017;72:326–337. doi: 10.1016/j.chiabu.2017.08.016. [DOI] [PubMed] [Google Scholar]
- Mersky JP, Janczewski CE, Topitzes J. Rethinking the measurement of adversity: Moving toward second-generation research on adverse childhood experiences. Child Maltreatment. 2017;22(1):58–68. doi: 10.1177/1077559516679513. [DOI] [PubMed] [Google Scholar]
- Metzler M, Merrick MT, Klevens J, Ports KA, Ford DC. Adverse childhood experiences and life opportunities: Shifting the narrative. Children and Youth Services Review. 2017;72:141–149. doi: 10.1016/j.childyouth.2016.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinto R, Correia L, Maia Â. Assessing the reliability of retrospective reports of adverse childhood experiences among adolescents with documented childhood maltreatment. Journal of Family Violence. 2014;29:431–438. doi: 10.1007/s10896-014-9602-9. [DOI] [Google Scholar]
- R Core Team. (2017). R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing Retrieved from https://www.R-project.org/. Accessed 11/8/18.
- Roberti J. Further psychometric support for the 10-item version of the perceived stress scale. Journal of College Counseling. 2006;9:135–147. doi: 10.1002/j.2161-1882.2006.tb00100.x. [DOI] [Google Scholar]
- Rosseel Y. Lavaan: An R package for structural equation modeling. Journal of Statistical Software. 2012;48(2):1–36. doi: 10.18637/jss.v048.i02. [DOI] [Google Scholar]
- Schilling EA, Aseltine RH, Gore S. Adverse childhood experiences and mental health in young adults: A longitudinal survey. BMC Public Health. 2007;7(1):1140–1151. doi: 10.1186/1471-2458-7-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott KM, Smith DR, Ellis PM. Prospectively ascertained child maltreatment and its association with DSM-IV mental disorders in young adults. Archives of General Psychiatry. 2010;67:712–719. doi: 10.1001/archgenpsychiatry.2010.71. [DOI] [PubMed] [Google Scholar]
- Scott BG, Burke NJ, Weems CF, Hellman JL, Carrión VG. The interrelation of adverse childhood experiences within an at-risk pediatric sample. Journal of Child and Adolescent Trauma. 2013;6(3):217–229. doi: 10.1080/19361521.2013.811459. [DOI] [Google Scholar]
- Syed HR, Zachrisson HD, Dalgard OS, Dalen I, Ahlberg N. Concordance between Hopkins symptom checklist (HSCL-10) and Pakistan anxiety and depression questionnaire (PADQ), in a rural self-motivated population in Pakistan. BMC Psychiatry. 2008;8(1):1. doi: 10.1186/1471-244X-8-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wade R, Shea JA, Rubin D, Wood J. Adverse childhood experiences of low-income urban youth. Pediatrics. 2014;134(1):e13–e20. doi: 10.1542/peds.2013-2475. [DOI] [PubMed] [Google Scholar]
- Ware JE, Jr, Snow KK, Kosinski M, Gandek B. SF-36 health survey manual and interpretation guide. Boston: The Health Institute, New England Medical Center Hospitals; 1993. [Google Scholar]
- Ware JE, Kosinski M. SF-36 physical & mental health summary scales: a manual for users of version 1. Lincoln: Quality Metric; 2001. [Google Scholar]
- Wingenfeld K, Schäfer I, Terfehr K, Grabski H, Driessen M, Grabe H, Löwe B, Spitzer C. The reliable, valid and economic assessment of early traumatization: First psychometric characteristics of the German version of the adverse childhood experiences questionnaire (ACE) Psychotherapie, Psychosomatik, Medizinische Psychologie. 2011;61(1):e10–e14. doi: 10.1055/s-0030-1263161. [DOI] [PubMed] [Google Scholar]
- Zanotti, D. C., Kaier, E., Vanasse, R., Davis, J. L., Strunk, K. C., & Cromer, L. D. (2017). An examination of the test–retest reliability of the ACE-SQ in a sample of college athletes. Psychological Trauma: Theory, Research, Practice, and Policy. 10.1037/tra0000299. [DOI] [PubMed]