Abstract
STUDY QUESTION
What variations underlie the menstrual cycle length and ovulation day of women trying to conceive?
SUMMARY ANSWER
Big data from a connected ovulation test revealed the extent of variation in menstrual cycle length and ovulation day in women trying to conceive.
WHAT IS KNOWN ALREADY
Timing intercourse to coincide with the fertile period of a woman maximises the chances of conception. The day of ovulation varies on an inter- and intra-individual level.
STUDY DESIGN, SIZE, DURATION
A total of 32 595 women who had purchased a connected ovulation test system contributed 75 981 cycles for analysis. Day of ovulation was determined from the fertility test results. The connected home ovulation test system enables users to identify their fertile phase. The app benefits users by enabling them to understand their personal fertility information. During each menstrual cycle, users input their perceived cycle length into an accessory application, and data on hormone levels from the tests are uploaded to the application and stored in an anonymised cloud database. This study compared users’ perceived cycle characteristics with actual cycle characteristics. The perceived and actual cycle length information was analysed to provide population ranges.
PARTICIPANTS/MATERIALS, SETTING, METHODS
This study analysed data from the at-home use of a commercially available connected home ovulation test by women across the USA and UK.
MAIN RESULTS AND THE ROLE OF CHANCE
Overall, 25.3% of users selected a 28-day cycle as their perceived cycle length; however, only 12.4% of users actually had a 28-day cycle. Most women (87%) had actual menstrual cycle lengths between 23 and 35 days, with a normal distribution centred on day 28, and over half of the users (52%) had cycles that varied by 5 days or more. There was a 10-day spread of observed ovulation days for a 28-day cycle, with the most common day of ovulation being Day 15. Similar variation was observed for all cycle lengths examined. For users who conducted a test on every day requested by the app, a luteinising hormone (LH) surge was detected in 97.9% of cycles.
LIMITATIONS, REASONS FOR CAUTION
Data were from a self-selected population of women who were prepared to purchase a commercially available product to aid conception and so may not fully represent the wider population. No corresponding demographic data were collected with the cycle information.
WIDER IMPLICATIONS OF THE FINDINGS
Using big data has provided more personalised insights into women’s fertility; this could enable women trying to conceive to better time intercourse, increasing the likelihood of conception.
STUDY FUNDING/COMPETING INTERESTS
The study was funded by SPD Development Company Ltd (Bedford, UK), a fully owned subsidiary of SPD Swiss Precision Diagnostics GmbH (Geneva, Switzerland). I.S., B.G. and S.J. are employees of the SPD Development Company Ltd.
Keywords: connected ovulation test systems, menstrual cycle length, ovulation, menstrual cycle, menstrual cycle variability
WHAT DOES THIS MEAN FOR PATIENTS?
Collection of big data from women seeking to conceive using a connected ovulation test system found that menstrual cycles are much more variable than the textbook definition of ‘28 days’. Yet, many women seeking to conceive incorrectly believe this definition applies to them. By recording cycles in the connected app, women become more knowledgeable about their own cycles. Being better informed can aid discussions about reproductive health with healthcare professionals, but can also help on a day-to-day basis (e.g. knowing when to carry sanitary protection or being able to better predict premenstrual syndrome).
To become pregnant, intercourse in the days leading up to and including day of ovulation is needed. This study has found that even if cycle length can be predicted, the day of ovulation can be very variable, meaning that you cannot accurately predict the fertile phase using cycle length alone. If a woman is wishing to time intercourse to the fertile period to maximise her chances of pregnancy, she should use an accurate method for identification, such as a urinary hormone tests.
Introduction
Couples are increasingly delaying childbearing, often until their late 30s or early 40s, for reasons such as furthering education, career, financial security or fulfilment of personal goals, thereby risking involuntary childlessness, infertility or a smaller family size than desired (Mills et al. 2011; Bellieni 2016; Sobotka 2017). In the UK, one in six couples and an estimated 48.5 million couples worldwide experience infertility (Mascarenhas et al. 2012; Fertility Fairness, 2019), and failure to become pregnant when trying to conceive can cause considerable stress (Severy et al. 2006).
There is a lack of understanding regarding fertility, even in women seeking to conceive (Kudesia et al. 2017). Successful natural conception may occur following intercourse during the 5 days prior to ovulation and the day of ovulation itself (Wilcox and Baird 2000; Stanford et al. 2002). Incorrect timing of intercourse appears to be an important reason for couples failing to conceive, due to a combination of lack of fertility knowledge and inaccurate perception of their own menstrual cycles (Zinaman et al. 2012). An accurate prediction of the woman’s unique fertile window is therefore needed to enable appropriate timing of intercourse (Robinson et al. 2007).
Tools for identification of the fertile window are popular among women; these include smartphone calendar applications (apps), temperature readings, cervical secretion monitoring and the use of ovulation tests (Brezina et al. 2011). However, the accuracy of tests that predict ovulation varies from 19% (based on 32 apps tested in 2017) to 99% (for market-leading home ovulation tests) (Johnson et al. 2018).
Ovulation tests typically measure luteinising hormone (LH) that surges ~1 day before ovulation (Johnson et al. 2015; Roos et al. 2015). Some ovulation tests also measure the oestrogen metabolite, estrone-3-glucuronide (E3G), which rises prior to the LH surge and marks the onset of the fertile window (Johnson et al. 2015; Roos et al. 2015).
Although the average length of a woman’s menstrual cycle is 28 days, there is considerable intra- and inter-individual variation in cycle lengths as well as changes in a woman’s own personal cycle with time (Treloar et al. 1967; Chiazze et al. 1968; Vollman 1977; Münster et al. 1992; Park et al. 2007; Johnson et al. 2009). The same degree of variation applies to the length of the follicular phase (from the beginning of the cycle to the time of ovulation) (Vollman 1977; Johnson et al. 2009). This means that timing of the fertile window is also likely to be highly variable.
Apps to track fertility are increasingly being used among women who are seeking to conceive, and many purport to predict ovulation based on cycle length characteristics alone, which can have extremely low predictive accuracy (Moglia et al. 2016; Setton et al. 2016; Johnson et al. 2018). These apps also assume each woman’s fertile window is the same length, disregarding evidence that the length of the fertile window differs among women (Keulers et al. 2007).
A connected home ovulation test system combines the use of urinary ovulation tests and an accessory app. The user inputs cycle length information into the app to determine which days to conduct tests on. The urine tests track E3G and LH, with a surge in E3G marking the onset of the fertile phase (high fertility) and an LH surge indicating impending ovulation (peak fertility). These data on users’ cycles and ovulation test results are stored anonymously in a cloud database in order to enable big data-based insights on menstrual cycles under a framework of continuous improvement of the test system. This study aims to explore real-time big data to better understand the variations of menstrual cycle length and ovulation day in women seeking to conceive.
Materials and Methods
Participants
The present study was performed using data from the anonymous information stored in the cloud database from users of the Clearblue® Connected Ovulation Test System (SPD Swiss Precision Diagnostics, GmbH, Geneva, Switzerland). These data included information on menstrual cycle lengths and urinary hormone test results from women in the USA and UK. The data snapshot made available for this study consisted of 354 687 ovulation test results and 75 982 cycles inputted by 32 595 users. The product is intended to aid conception for women ≥18 years old and is not intended for women who are pregnant (or recently pregnant), menopausal, diagnosed with polycystic ovarian syndrome or taking fertility medications.
Institutional Review Board approval was not required because this study consisted of the examination of anonymised data from a legally marketed medical device. The product is an in vitro diagnostic device and meets the requirements of relevant legislation for the countries in which it is sold. Users were subject to terms and conditions that explicitly stated that scientific data may be investigated and published in an anonymised fashion and that the product is for use by those over the age of 18.
System information
The information stored in the cloud database was from users who, when using the app, were asked to input their perceived average menstrual cycle length into the system. Based on this information, the app generated a testing plan for the users, who were then prompted to conduct fertility urine tests at specific periods of their cycle; for example, a user with an average cycle length of 23 days would start testing on Day 6, whereas testing would begin on Day 8 for a 28-day cycle and Day 15 for a 35-day cycle. At the start of each new cycle, the user is prompted to re-enter their average cycle length, but has previous data available to aid selection.
When the user performed a test, the device determines whether hormone levels are baseline (determined via a rolling average of assay signal levels) or represent a surge in hormone levels (reaching a signal threshold relative to the individual’s hormone baseline). The result is displayed as either low, high or peak fertility. Low fertility indicates that E3G and LH concentrations are at baseline levels, while high fertility indicates that a rise in E3G had been detected, marking the onset of the fertility window. The peak fertility result refers to the LH surge and can be mapped chronologically as 1 day before ovulation (Johnson et al. 2015; Roos et al. 2015). The app instructs users to test each day until peak fertility is detected.
Users were able to add additional information, such as days of menstruation and intercourse, which, along with the test results, was presented to the user as a summary of their current cycle on the app. The inputted menstrual bleeding data were used to calculate the actual cycle length (cycle start day to the day before the next cycle start day). Cycle start day (first day of menses) was classed as the day of first menstrual bleeding inputted by the user.
The self-reported estimation of cycle length (user cycle length) that was inputted at the beginning of the cycle was compared with the actual cycle length (cycle start day to the day before the next cycle start day) (Supplementary Fig. S1). Data on all current/unfinished cycles were excluded as there were no end events that would allow for the calculation of actual cycle length.
Statistical analysis
The total 5th–95th centile uncensored range for cycle length was 23–67 days, but it is possible that some of the very long cycles were due to failure to input menses information between consecutive cycles; this would introduce error in comparative analyses. Therefore, cycles where the calculated (actual) cycle length was longer or shorter than 1.5 times the user cycle length were excluded from the comparative analyses as extreme differences were most likely attributable to user inputting errors. Examples of inputting errors had been gathered from usability testing during development of the product and were found to produce data mimicking very short or long cycles, e.g. only inputting day of first and last menstrual bleeding would appear as a very short cycle, whereas having a break from testing and not logging menses during that time results in very long cycles.
Users who had completed 4 cycles formed a subgroup to investigate the level of variability from cycle to cycle. Fewer cycles may not show the scale of the variation among women, while the sample size was not substantive enough for higher numbers of cycles. Cycle length variation was described as the difference between the shortest and longest cycles and was calculated for users who had exactly 4 cycles worth of data (n = 1143).
The cycles where an LH surge had occurred were analysed, and data were grouped by the actual cycle length in order to calculate the probability of ovulation per cycle day for each cycle length.
Examination of the menstrual cycle phases was possible because the ovulation day could be calculated, providing useful information on the positioning of the fertile window. The Pearson correlation coefficient was used to explore the correlation between cycle length and cycle phase. To further explore the relationship between the follicular phase and the cycle length, a robust regression analysis using Huber’s M-estimator was performed, as data showed signs of heteroscedasticity (Huber 1964; Huber 1981). Python 3™ (an interpreted, interactive, object-oriented programming language) and the relevant numerical, statistical and data science libraries, including ‘Pandas’, were used to develop the Jupyter notebooks for this study.
Data availability
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request.
Results
The perception and variation of cycle length
A total of 75 981 cycles from 32 595 users were available for analysis, of which 46 704 were completed, in that they had a subsequent cycle, and 29 277 were unfinished, in that there was no cycle end defined. The number of users and the cycles they have contributed are grouped and presented in Table I.
Table I.
Intra-individual variation in cycle length (min to max) for different numbers of contributory cycles.
| Number of days difference (min–max) | Percentage of cycles with each level of variation, by number of completed cycles | ||||
|---|---|---|---|---|---|
| 2 (n = 3682) | 3 (n = 2152) | 4 (n = 1143) | 5 (n = 697) | 6 (n = 465) | |
| 0 | 11.5 | 2.3 | 0.6 | 0.0 | 0.0 |
| 1 | 21.7 | 10.7 | 7.0 | 2.7 | 1.1 |
| 2 | 18.1 | 14.5 | 12.5 | 6.5 | 6.9 |
| 3 | 12.0 | 15.7 | 13.9 | 13.4 | 10.7 |
| 4 | 8.6 | 13.8 | 13.1 | 13.4 | 13.8 |
| 5 | 6.6 | 9.2 | 12.0 | 13.6 | 15.7 |
| 6 | 5.0 | 6.5 | 7.9 | 10.2 | 9.6 |
| 7 | 3.9 | 6.0 | 6.9 | 8.0 | 6.9 |
| 8 | 2.8 | 4.6 | 5.5 | 6.6 | 7.5 |
| 9 | 2.3 | 3.3 | 4.7 | 4.7 | 6.3 |
| 10 | 1.8 | 2.7 | 3.8 | 6.0 | 5.2 |
| 11 | 1.3 | 2.5 | 2.1 | 3.7 | 4.4 |
| 12 | 1.0 | 2.1 | 2.0 | 2.2 | 2.7 |
| >12 | 2.7 | 5.3 | 6.9 | 7.7 | 8.0 |
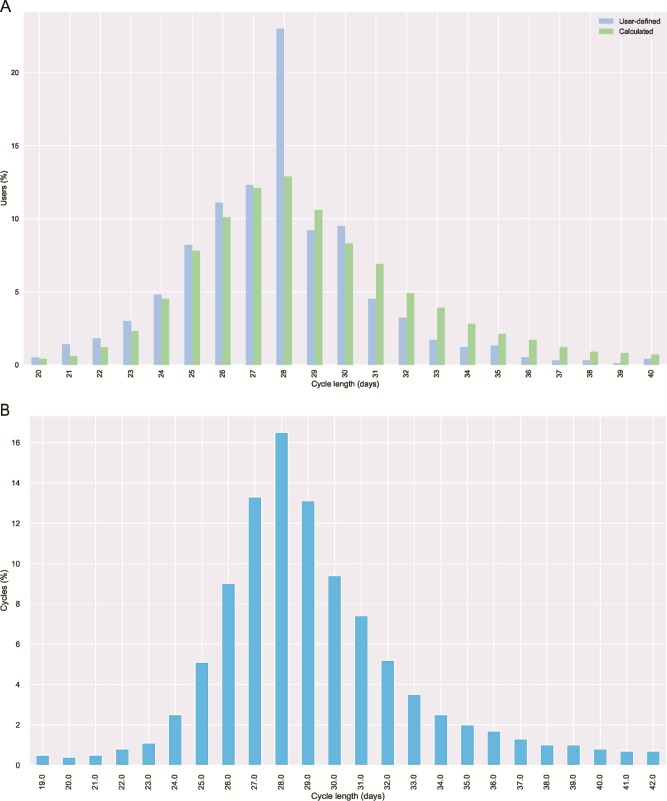
When users recorded their cycle length for the first time, the two most popular choices were 28 (31.1%) and 30 days (11.9%). However, this changed over time when users inputted information regarding their subsequent cycles. Overall, users selected a 28-day cycle 23.3% of the time, with the next most common choices being 27 (11.8%), 26 (10.5%) and 30 (9.7%) days (Fig. 1A). The actual cycle length was normally distributed, with the most common length also being 28 days, but at a lower frequency of 12.4% (Fig. 1A).
Figure 1.
Actual menstrual cycle length. (A) User-defined versus actual menstrual cycle length. (B) Distribution of actual cycle length for users with a 28-day estimated cycle.
The actual next cycle lengths of the women after they inputted a 28-day cycle at any point during product use (23.3% of cycles) also appeared to be normally distributed (Fig. 1B), and 61.8% had their next cycle within 2 days of their 28-day estimate; however, 26.2% were 4 or more days out in their prediction and 18.5% were 5 or more days out (total range 9 days too short to 14 days too long). Selecting a different cycle length for subsequent cycles was common (68.5%), and predictions more closely matched actual cycle distribution with each successive cycle, until reaching a plateau at cycle 4.
Intra-individual variability of cycles
Intra-individual cycle variation was observed in this study (Table I), with less than 1% of users having the same cycle length across four consecutive cycles. Over half of the users (52.3%) had cycle lengths that varied by 5 or more days. The variation had a skewed distribution and seemed to demonstrate some exponential characteristics. Indeed, an exponentially modified Gaussian distribution was fitted (ex-Gaussian), which is the sum of two independent distributions, a normal and an exponential. The parameters for the normal distribution are μ = 1.635 and σ = 0.9138 while the rate for the exponential part of the distribution is λ = 0.234.
The absolute difference in min–max cycle length increases with the number of cycles a user has completed, which is a function of having more data available but may also indicate population differences based on how quickly the woman conceives.
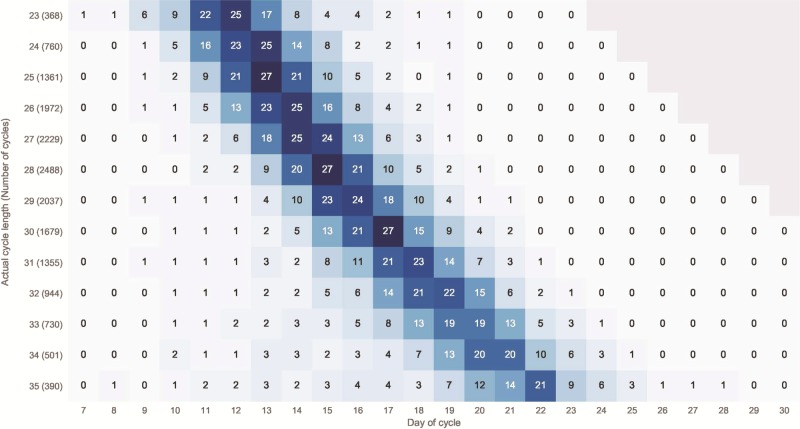
Probability of ovulation
All ovulation events (n = 27 210) were grouped by cycle length in order to estimate the frequency of occurrence as a percentage of the total ovulations per cycle length. Fig. 2 shows the results for the cycles between 23 and 35 days. These were the most common cycle lengths, representing 87.7% of the cycle data; sample sizes for shorter and longer cycles were too small to make accurate frequency assessments. For the 28-day cycles, ovulation occurred most commonly on Day 15 (27%), followed by Day 16 (21%) and Day 14 (20%). There was a 10-day spread of observed ovulation days for a 28-day cycle, and a similar variation was observed for all cycle lengths examined. For users who conducted a test on every day requested by the app, a surge was detected in 97.9% of cycles.
Figure 2.
Probability of ovulation (%) per cycle day for cycles with length between 23 and 35 days. Probability per cycle day is shown as a percentage. Sample size for each cycle length is shown in brackets (n). Shading represents probability level (darkest = highest probability).
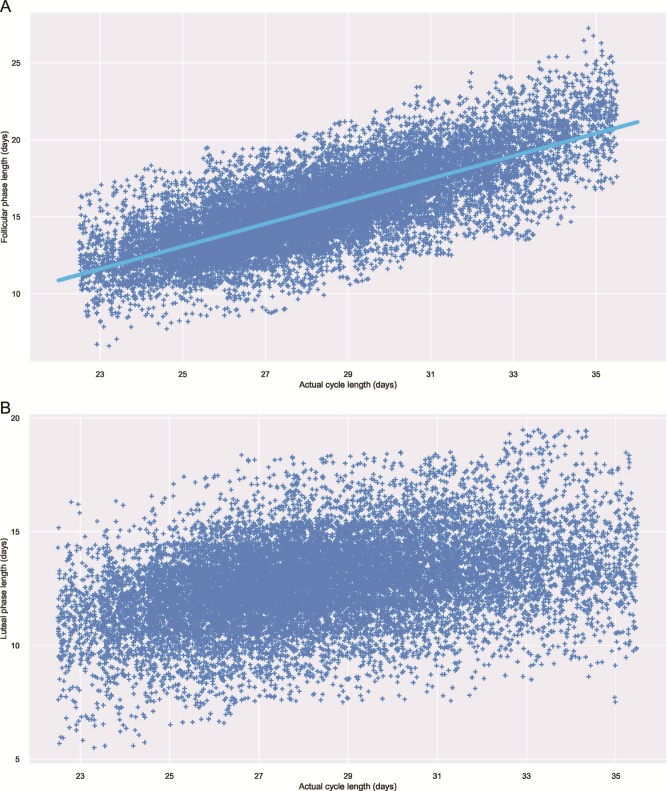
Ovulation day and cycle length
Strong correlation was seen between the follicular phase and the actual cycle length for cycle lengths of 23 to 35 days (Pearson’s r = 0.77, P < 0.001), while the correlation between the actual cycle length and the luteal phase length was weaker (Pearson’s r = 0.37, P < 0.001), as shown in the scatter plots of the follicular and luteal phase versus the cycle length (Fig. 3A and B). A normal distribution was fitted to the luteal phase, and it was estimated that the mean length was 12.77 ± 1.86 days. A robust regression model for the follicular phase length was fitted using Huber’s M-estimator, as the data show characteristics of heteroscedasticity (Huber 1964). The robust regression model for the follicular phase length is described as
 |
Figure 3.
Scatter plots showing menstrual cycle data. (A) Scatter plot showing the actual cycle length (days) and the follicular phase length, fitted with a robust regression. (B) Scatter plot showing the actual cycle length (days) and the luteal phase length. Jitter (off-setting overlapping data points on the x-axis) was applied to aid visualisation of the data in the graphs. The jitter added to the scatter plots was not taken into account when the model was fitted. Data are shown for cycle lengths 23–35 days.
This model can be applied to predict the most likely day for ovulation, with the full spread of possible days described in Fig. 2.
Discussion
The current study investigated a large dataset on the menstrual cycles of women seeking to conceive. In contrast to previous studies, this investigation used real-life data anonymously collected by users inputting their menstrual cycle information into an app, which was then stored in the cloud database. Most of the women (87.7%) who were using the app had cycle lengths between 23 and 35 days, which is in agreement with the ranges of menstrual cycle length reported in observational cohort studies (Chiazze et al. 1968; Vollman 1977; Johnson et al. 2009). This equivalence in characteristics is very reassuring as it provides cross-validation of real-life data with clinical study data.
It is evident that there exists a lack of knowledge among women regarding their own personal menstrual cycles, and this could be an important reason why couples fail to conceive. In this study, there were discrepancies between women’s perceived cycle length compared with the actual cycle length; this was highlighted by 23.3% (31.1% on first use) of users recording their cycle as 28 days, whereas only 12.4% of the individuals had an actual cycle length of 28 days. This finding was similarly shown by Johnson et al. (2018), where 34% of women perceived their cycle to be 28 days, while only 15% of users had a cycle of that length (Johnson et al. 2018). Some discrepancy would be expected (as this study highlights, future cycle lengths are very difficult to predict); but nearly a fifth of women got their prediction wrong by five or more days, which suggests lack of personal knowledge combined with intra-individual cycle variability. However, predictions improved with usage of the app, suggesting increased awareness.
A 10-day spread of observed ovulation days was observed for all cycle lengths examined; this also agrees with the findings of Johnson et al. (2018). In this study, ovulation day was assigned as the day following the LH surge, as comparisons between the assays used by the connected ovulation tests and transvaginal ultrasonography have indicated that this is the average relationship between the measures. However, imprecision of ±1 day has been reported for this assay (Behre et al. 2000).
The day of ovulation seems to be linearly related to the cycle length, while the luteal phase length seems to have only small effect on the cycle length, as shown by the predictive equation. The cycle characteristics described in this study are consistent with previous findings on research cohorts (Chiazze et al. 1968; Vollman 1977; Münster et al. 1992; Johnson et al. 2009; 2018), indicating that previous clinical findings are still reflective of cycle characteristics of today’s population of women who are seeking to conceive. It is clearly not possible to predict cycle length in advance of its commencement, but even if it were, the variation in ovulation day for any given cycle length provides additional unpredictability of the fertile phase if the only information available is cycle length. The predictive equation generated from these data has utility in only providing the most likely day of ovulation. These findings emphasise the need for women wishing to time intercourse to the fertile period to use true prospective methods, such as hormone monitoring. However, women having frequent intercourse (two to three times per week) are likely to coincide intercourse with the fertile period, so they would have no need to use methods for fertile phase detection. The findings also show it is not possible to adapt the app component of the system examined here to provide accurate predictions based on the calendar input alone.
Although variability in cycle length is normal, considerable irregularity along with unsuccessful attempts to conceive may indicate peri-menopause or another endocrine abnormality that would require a specialist’s attention. Having an app that stores cycle information and intercourse data may help in these cases because it can be presented to a specialist. The availability of historical data on menstrual cycles enables users to compare and understand their own personal cycles; this provides couples with better information to time intercourse for conception and also helps women gain a general understanding of their menstrual cycles.
Use of anonymised big data comes with some limitations; importantly, in this study corresponding demographics are not available so it is not possible to determine whether certain cycle characteristics are associated with specific demographics such as age, BMI or parity. Unlike controlled clinical studies, it is also not possible to determine the causes of extreme observations; for example, whether a very long cycle is genuine, due to early pregnancy loss or due to the user choosing not to, or forgetting to test or add information. Therefore, the cycle characterisation presented here focuses on the robust data for cycle lengths of 23 to 35 days, where big data offers the advantage of providing thousands of observations for analysis.
The insights gained from these findings highlight the uniqueness of women’s menstrual cycles as well as indicate why accurate, personalised information is of great importance. Future work could involve creation of individualised probabilistic models to predict the likely time of ovulation based on previous ovulation information and could make use of the regression equation described from these data; however, given the variability highlighted here, success may be limited. The use of the app to store information will allow women to better understand their own cycles, which in turn will enable them to accurately time intercourse to increase the likelihood of successful conception (Stanford et al. 2002; Robinson et al. 2007; Yeh et al. 2019). Identification of the fertile phase can also be applied for the avoidance of pregnancy, but different algorithms are needed as it is important to identify every day in which unprotected intercourse could lead to pregnancy, whereas for conception purposes, it is more helpful to the user to identify only the best days for timing of intercourse.
Analysis of big data from women trying to conceive using a connected ovulation test system has provided important insights into how variable and personal menstrual cycles and the fertile window are both within and between women. The observation that the data are consistent with published clinical cohort studies is extremely important as it suggests that such data give an accurate picture of women’s cycles. The variability in the fertile window seen in this study demonstrates that timing intercourse based on women’s own predictions is often unlikely to be accurate; a true, prospective method, such as one that measures hormone levels, is therefore needed.
Supplementary Material
Acknowledgements
The authors would like to thank Abisola Akinbowale from integrated medhealth communication (funded by SPD Development Company Ltd) for providing medical writing assistance.
Authors’ roles
Conception and design of study were by all authors. Data acquisition and analysis were conducted by I.S. I.S. and S.J. wrote the main manuscript text. All authors reviewed the manuscript and provided final approval of the manuscript.
Funding
This study was funded by SPD Development Company Ltd (Bedford, UK), a fully owned subsidiary of SPD Swiss Precision Diagnostics GmbH (Geneva, Switzerland).
Conflict of interest
I.S., B.G. and S.J. are employees of the SPD Development Company Ltd.
References
- Behre HM, Kuhlage J, Gassner C, Sonntag B, Schem C, Schneider HP, Nieschlag E. Prediction of ovulation by urinary hormone measurements with the home use ClearPlan fertility monitor: comparison with transvaginal ultrasound scans and serum hormone measurements. Hum Reprod 2000;15:2478–2482. [DOI] [PubMed] [Google Scholar]
- Bellieni C. The best age for pregnancy and undue pressures. J Family Reprod Health 2016;10:104–107. [PMC free article] [PubMed] [Google Scholar]
- Brezina PR, Haberl E, Wallach E. At home testing: optimizing management for the infertility physician. Fertil Steril 2011;95:1867–1878. [DOI] [PubMed] [Google Scholar]
- Chiazze LBFJ, Macisco JJ Jr, Parker MP, Duffy BJ. The length and variability of the human menstrual cycle. JAMA 1968;377–380. [PubMed] [Google Scholar]
- Fertility Fairness What is ‘Infertility’? Available at: https://www.fertilityfairness.co.uk/nhs-fertility-services/what-is-infertility/ (10 January 2020, date last accessed).
- Huber P. Robust estimation of a location parameter. Ann Math Statist 1964;73–101. [Google Scholar]
- Huber P. Robust Statistics. Canada: John Wiley & Sons, 1981. [Google Scholar]
- Johnson S, Marriott L, Zinaman M. Can apps and calendar methods predict ovulation with accuracy? Curr Med Res Opin 2018;34:1587–1594. [DOI] [PubMed] [Google Scholar]
- Johnson S, Weddell S, Godbert S, Freundl G, Roos J, Gnoth C. Development of the first urinary reproductive hormone ranges referenced to independently determined ovulation day. Clin Chem Lab Med 2015;53:1099–1108. [DOI] [PubMed] [Google Scholar]
- Johnson SR, Miro F, Barrett S, Ellis JE. Levels of urinary human chorionic gonadotrophin (hCG) following conception and variability of menstrual cycle length in a cohort of women attempting to conceive. Curr Med Res Opin 2009;25:741–748. [DOI] [PubMed] [Google Scholar]
- Keulers MJ, Hamilton CJ, Franx A, Evers JL, Bots RS. The length of the fertile window is associated with the chance of spontaneously conceiving an ongoing pregnancy in subfertile couples. Hum Reprod 2007;22:1652–1656. [DOI] [PubMed] [Google Scholar]
- Kudesia R, Chernyak E, McAvey B. Low fertility awareness in United States reproductive-aged women and medical trainees: creation and validation of the Fertility & Infertility Treatment Knowledge Score (FIT-KS). Fertil Steril 2017;108:711–717. [DOI] [PubMed] [Google Scholar]
- Mascarenhas MN, Flaxman SR, Boerma T, Vanderpoel S, Stevens GA. National, regional, and global trends in infertility prevalence since 1990: a systematic analysis of 277 health surveys. PLoS Med 2012;9:e1001356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills M, Rindfuss RR, McDonald P, Velde E, Reproduction E, Society Task F. Why do people postpone parenthood? Reasons and social policy incentives. Hum Reprod Update 2011;17:848–860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moglia ML, Nguyen HV, Chyjek K, Chen KT, Castano PM. Evaluation of smartphone menstrual cycle tracking applications using an adapted APPLICATIONS scoring system. Obstet Gynecol 2016;127:1153–1160. [DOI] [PubMed] [Google Scholar]
- Münster K, Schmidt L, Helm P. Length and variation in the menstrual cycle--a cross-sectional study from a Danish county. Br J Obstet Gynaecol 1992;99:422–429. [DOI] [PubMed] [Google Scholar]
- Park SJ, Goldsmith LT, Skurnick JH, Wojtczuk A, Weiss G. Characteristics of the urinary luteinizing hormone surge in young ovulatory women. Fertil Steril 2007;88:684–690. [DOI] [PubMed] [Google Scholar]
- Vollman RF. The menstrual cycle. Major Probl Obstet Gynecol 1977;1–193. [PubMed] [Google Scholar]
- Robinson JE, Wakelin M, Ellis JE. Increased pregnancy rate with use of the Clearblue easy fertility monitor. Fertil Steril 2007;87:329–334. [DOI] [PubMed] [Google Scholar]
- Roos J, Johnson S, Weddell S, Godehardt E, Schiffner J, Freundl G, Gnoth C. Monitoring the menstrual cycle: Comparison of urinary and serum reproductive hormones referenced to true ovulation. Eur J Contracept Reprod Health Care 2015;20:438–450. [DOI] [PubMed] [Google Scholar]
- Setton R, Tierney C, Tsai T. The accuracy of web sites and cellular phone applications in predicting the fertile window. Obstet Gynecol 2016;128:58–63. [DOI] [PubMed] [Google Scholar]
- Severy LJ, Robinson J, Findley-Klein C, McNulty J. Acceptability of a home monitor used to aid in conception: psychosocial factors and couple dynamics. Contraception 2006;73:65–71. [DOI] [PubMed] [Google Scholar]
- Sobotka T. Vienna Institute of Demography Working Papers: post-transitional fertility: childbearing postponement and the shift to low and unstable fertility levels. J Biosoc Sci 2017;49:S20–S45. [DOI] [PubMed] [Google Scholar]
- Stanford JB, White GL, Hatasaka H. Timing intercourse to achieve pregnancy: current evidence. Obstet Gynecol 2002;100:1333–1341. [DOI] [PubMed] [Google Scholar]
- Treloar AEBR, Behn BG, Brown BW. Variation of the human menstrual cycle through reproductive life. Int J Fertil 1967;77–126. [PubMed] [Google Scholar]
- Wilcox AJDD, Baird DD. The timing of the “fertile window” in the menstrual cycle: day specific estimates from a prospective study. BMJ 2000;321:1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeh PT, Kennedy CE, Van der Poel S, Matsaseng T, Bernard L, Narasimhan M. Should home-based ovulation predictor kits be offered as an additional approach for fertility management for women and couples desiring pregnancy? A systematic review and meta-analysis. BMJ Glob Health 2019;4:e001403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zinaman M, Johnson S, Ellis J, Ledger W. Accuracy of perception of ovulation day in women trying to conceive. Curr Med Res Opin 2012;28:749–754. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request.