Abstract
Objective
Our objective was to characterize Canadian workforce attributes of extended role practitioners (ERPs) in arthritis care.
Methods
We used an exploratory, mixed‐methods study that was based on the Canadian Rheumatology Association's Stand Up and Be Counted Rheumatologist Workforce Survey (2015). An anonymous online survey was deployed to groups of non‐physician health care professionals across Canada who potentially had post‐licensure training in arthritis care. Demographic and practice information were elicited. Qualitative responses were analyzed using grounded theory techniques.
Results
Of 141 respondents, 91 identified as practicing in extended role capacities. The mean age of ERP respondents was 48.7; 87% were female, and 41% of ERPs planned to retire within 5 to 10 years. Respondents were largely physical or occupational therapists by profession and practiced in urban/academic (46%), community (39%), and rural settings (13%). Differences in practice patterns were noted between ERPs (64.5%) and non‐ERPs (34.5%), with more ERPs working in extended role capacities while retaining activities reflective of their professional backgrounds. Most respondents (95%) agreed that formal training is necessary to work as an ERP, but only half perceived they had sufficient training opportunities. Barriers to pursuing training were varied, including personal barriers, geographic barriers, patient‐care needs, and financial/remuneration concerns.
Conclusion
To our knowledge, no previous studies have assessed the workforce capacity or the perceived need for the training of ERPs working in arthritis and musculoskeletal care. Measurement is important because in these health disciplines, practitioners’ scopes of practice evolve, and ERPs integrate into the Canadian health care system. ERPs have emerged to augment provision of arthritis care, but funding for continuing professional development opportunities and for role implementation remains tenuous.
INTRODUCTION
In Canada, it has been proposed that the number of rheumatologists per capita is a system‐level performance measure for arthritis care (1). Their dearth and unequal distribution are well documented (1, 2, 3). Although arthritis and musculoskeletal (MSK) disorders are the most common chronic health conditions in Canada (4), the growing health care needs of an aging population are threatened because of a known critical and growing shortage of rheumatologists, which is attributed to their retirement plans and practice patterns (2).
Given the service‐demand issues (5), new and more efficient models of care involving advanced practice practitioners (APPs)/extended role practitioners (ERPs) invested in arthritis care are considered viable solutions (6) to better triage and co‐manage the growing number of patients with arthritis and MSK disorders (7, 8, 9, 10, 11, 12, 13, 14, 15). At the core of these new models of arthritis care is the reliance on strong interprofessional collaborative relationships between MSK specialists, including rheumatologists and orthopedic surgeons, and ERPs. ERPs often practice to the full scope of their profession, including activities achieved through delegation or medical directives. In these delivery models, with medical directives or authorized activities in place (16), the skill sets of ERPs are leveraged to magnify the workforce capacity and improve access to care (7, 15, 17, 18, 19, 20).
Many ERPs have been trained through various developed programs with the aim of expanding the pool of human resources capable of providing specialized arthritis care (21, 22, 23, 24), giving rise to concomitant challenges of devising standardized competency‐based education (25). Although the development of accredited programs to train ERPs in arthritis care is considered central to preparing practitioners for advanced interprofessional practice (8, 26, 27), many positions are undertaken without requisite formal training (28). Currently, health regulatory colleges and professional associations neither endorse nor demand evidence of standardized training to support advanced/extended roles in practice.
Although there is considerable evidence to support the use of APPs/ERPs (7, 15, 20, 29, 30), there are no studies to date documenting workforce attributes, capacity, or learning needs of these health professionals in Canada. This information would complement the results of the extensive national Canadian workforce survey of rheumatologists (the Stand Up and Be Counted Workforce Survey of 2015) (2) and permit a broader grasp of the Canadian arthritis care provider landscape.
The purpose of this exploratory mixed‐methods study was to better understand the current workforce attributes and the capacity of those working in extended practice roles in arthritis care in Canada. In addition, we sought to determine the perceived enablers of, and barriers to, pursuing formal clinical/academic training to support these roles.
PARTICIPANTS AND METHODS
This pan‐Canadian exploratory, mixed‐methods, cross‐sectional, self‐report study was developed and based on the original Stand Up and Be Counted Rheumatologist Workforce Survey (2). Data were collected by deploying an anonymous online survey in 2018 to groups of non‐physician health care professionals in Canada who had potentially undertaken formal and/or informal post‐licensure training in arthritis care. (Table 1)
Table 1.
Canadian arthritis care networks and associations/non‐physician health care professionals approached for recruitment
| Association | Approximate No. of Graduates/Members as of 2018 |
|---|---|
| AHPA | 140 |
| AAC | N/A |
| CRA | N/A |
| ACPAC | 79 |
| Mary Pack ACE | ~300 |
| Arthritis Society clinician employees | 40 |
| TAS‐CPSIA | ~176 |
| ISAEC | 14 |
| Institutional training (Sunnybrook‐Holland Network) | ~20 |
Abbreviation: AAC, Arthritis Alliance of Canada; ACPAC, Advanced Clinician Practitioner in Arthritis Care; AHPA, Arthritis Health Professionals Association; CRA, Canadian Rheumatology Association; ISAEC, Interprofessional Spine Assessment and Education Clinics; Mary Pack Arthritis Continuing Education; N/A, not applicable; TAS‐CPSIA, The Arthritis Society Clinical Practice Skills for Inflammatory Arthritis.
Study population
For the purpose of the survey, an ERP is defined as a non‐physician health care professional working, or having the capacity to work, in arthritis/MSK care. Their practice is defined by the affirmation of at least two of the following three statements:
Works in a shared‐care model (ie, co‐manages patients with physician specialists or has the potential to do so) for triage and ongoing management of patients.
Has advanced knowledge and clinical skills related to arthritis care obtained through an additional formal training program.
Performs additional activities beyond the traditional scope of practice under medical directives or authorized activities.
Participants who did not affirm any of these statements, or who only affirmed one, were classified as non‐ERPs. For the purpose of analysis, those working in administrative/research roles with no direct clinical time were separated from the other non‐ERP respondents in recognition of the unique role arthritis care program administrators have in supporting arthritis care providers and/or ERP roles.
Inclusion/exclusion criteria
This study included those currently working as health care professionals in arthritis/MSK care in advanced/extended practice roles (as per the criteria outlined previously) or supporting others who work in these roles. Those who were unable to complete the survey in English were excluded.
Recruitment
The principal investigator (PI) identified potential participants through contact with champions from programs known to provide post‐licensure training in arthritis/MSK care in Canada (Table 1). Champions were sent a template of an introductory e‐mail, which included a link to the survey, to use to approach their graduates/members. We used snowball sampling, whereby health care professionals receiving the survey were encouraged to send the survey to other health professionals perceived as working in advanced/extended practice roles in arthritis/MSK care in Canada. Networks and specialty interest groups, including the Arthritis Health Professionals Association (AHPA), the Canadian Rheumatology Association (CRA), and the Arthritis Alliance of Canada (AAC), were approached to electronically post a study description and survey link in two sequential issues of their newsletters. The AHPA has a membership of approximately 140 members of multidisciplinary arthritis health care professionals across Canada, which acted as our benchmark for sample size.
Because there was multiplicity in membership within the key contact groups, an initial request and one reminder per group was issued in a staggered manner to optimize contact between February 2018 and September 2018. Consent was implied if the participant chose to complete and submit the anonymous online survey.
Survey design
The survey was based on another survey developed by this study's collaborator (CB) in 2015 (2). The wording of questions was modified from “rheumatology practice” to “advanced/extended practice.” Some questions were not relevant and were removed. Additional questions were included to identify activities performed in ERP roles, including those performed under medical directives. A draft of the modified survey was circulated to a working group of stakeholders, including two rheumatologists, four MSK clinician‐researchers, and one Advanced Clinical Practitioner in Arthritis Care (ACPAC) ERP graduate, for feedback on the content and wording of questions. The final online survey consisted of 49 questions that generated both quantitative and qualitative data.
Quantitative questions were included to estimate the number and characteristics of ERPs working in arthritis care in Canada and to determine their demographic makeup, clinical practice setting, and type of practice. The final five questions were qualitative, aiming to identify perceived enablers of, and barriers to, the pursuit of formal academic/clinical training programs that support the development of advanced or extended practice roles in arthritis care (see Appendix 1).
Data management
The survey was deployed using Survey Monkey® software (http://www.surveymonkey.com). Any identifying information (eg, IP address) was not included in the export of the data from Survey Monkey® to ensure anonymity. Each respondent was assigned a unique identifier. Quantitative data from the electronic survey was exported into SAS version 9.4 (SAS Institute) (31), and qualitative responses of the survey were imported into NVivo version 12 (QSR International) (32) for analysis.
Analysis
Descriptive and univariate statistics were generated to describe the respondents (demographics, professional background, and advanced training pursued in arthritis care) and the context of their clinical practice (clinical setting, patient populations, and tasks performed in extended practice roles). Results were grouped by respondent: ERPs and non‐ERPs and/or administrators. Shapiro‐Wilk tests of normality were employed; the sample was considered to be normally distributed if the P value was more than 0.05 and was considered nonparametric if the P value was less than 0.05. Because the variables related to clinical tasks all proved to be nonparametric, Wilcoxon rank‐sum tests were used to assess the clinical tasks performed by ERPs and non‐ERPs.
Three of the five open‐ended questions asked respondents to indicate agreement or disagreement with statements. These results were calculated, expressed in percentages, and analyzed by group. Qualitative analysis of the open‐ended responses related to barriers and enablers to the pursuit of training was done by interpreting the reflective responses via grounded theory and descriptive analysis techniques (33, 34, 35). The qualitative research analyst (MP) initially read each of the responses, attributing codes to sentences, paragraphs, or sections. Codes were grouped into possible themes. The study PI (KL) reviewed these codes and themes. Once the PI and analyst reached a satisfactory level of agreement over the coding scheme, the analyst recoded responses, adding new codes as necessary. Themes were then brought to the full research team for discussion. Themes were used to describe the participants’ experiences and form conclusions.
Ethics
Permission to perform this study was approved by the Research Ethics Board (REB) of St. Michael's Hospital (REB No. 17‐185) prior to study commencement. Individual‐signed informed consent forms were not required by the REB because submission of the anonymous online survey implied consent. All data were maintained with confidentiality in accordance with the Declaration of Helsinki.
RESULTS
A total of 141 respondents completed the online survey, 64.5% (n = 91) of whom were classified as ERPs, whereas 35.5% of respondents (n = 50) were classified as non‐ERPs. Of the latter, eight were identified as being in exclusively administrative/research roles related to arthritis care with no direct clinical time. Health disciplines represented among the ERPs included physical therapists (PTs) (65.9%), occupational therapists (OTs) (18.7%), registered nurses (RNs) (8.8%), and chiropractors/pharmacists (6.6% collectively). Most of the respondents were female (ERP = 86.8%; non‐ERP = 85.7%) with a mean age of 48.7 and 47.2 years respectively. Of ERPs, 40.7% plan to retire in the next 5 to 10 years. Most geographic practice sites were in Ontario, followed by Alberta, British Columbia, and Newfoundland. Almost half of the ERPs (49.5%) reported managing patients specifically with inflammatory arthritis (IA). Non‐ERPs included PTs (57.1%), OTs (28.6%), and RNs, social workers and pharmacists (14.3% collectively). ERP respondents had practiced for an average of 17.8 years in arthritis/MSK care and 7.3 years in an ERP capacity. Non‐ERPs were similarly experienced, averaging 15.4 years in arthritis/MSK care (Table 2).
Table 2.
Descriptive characteristics of ERPs and non‐ERPs
| ERP (n = 91) | Non‐ERPa (n = 42) | |
|---|---|---|
| Age, mean (SD), y | 48.7 (9.0) | 47.2 (11.8) |
| Female sex, % | 86.8 | 85.7 |
| Practicing in MSK care, mean (SD), y | 17.8 (8.9) | 15.4 (11.3) |
| Practicing as an ERP, mean (SD), y | 7.3 (5.3) | … |
| Time practicing in a health discipline, % | ||
| 0‐5 y | 4.4 | 16.7 |
| 6‐10 y | 7.7 | 9.5 |
| 11‐20 y | 34.1 | 23.8 |
| 21‐30 y | 26.4 | 23.8 |
| 30+ y | 26.4 | 21.4 |
| Currently practicing in arthritis or MSK care, % | 97.8 | 95.2 |
| Professional designation, % | ||
| Physical therapist | 65.9 | 57.1 |
| Occupational therapist | 18.7 | 28.6 |
| Registered nurse | 8.8 | 4.8 |
| Other | 6.6 | 9.5 |
| ERP characteristics | ||
| Working as an ERP; shared‐care model, % | 95.6 | 23.8b |
| ERP‐advanced training or knowledge, % | 97.8 | 47.6b |
| Act under medical directives to perform advanced tasks, % | 83.5 | 4.8b |
| Funding for clinical time, % | ||
| Fee for service | 6.6 | 7.1 |
| Physician | 5.5 | 2.4 |
| Hospital | 70.3 | 35.7 |
| The Arthritis Society | 17.6 | 40.5 |
| Retirement plans, % | ||
| 5 y | 24.2 | 19.1 |
| 10 y | 16.5 | 11.9 |
| Uncertain | 16.5 | 16.7 |
| No retirement plans | 42.7 | 47.6 |
| Language used for patients, % | ||
| English | 100.0 | 95.2 |
| French | 12.1 | 7.1 |
| Other (Cantonese, Spanish, Arabic) | 5.5 | 0.0 |
| Age of patients, % | ||
| <15 y | 34.1 | 33.3 |
| 16‐18 y | 49.5 | 40.5 |
| 19‐65 y | 87.9 | 81.0 |
| 65+ y | 86.8 | 81.0 |
| Clinical practice settings, % | ||
| Acute hospital inpatient | 8.8 | … |
| Acute hospital outpatient | 49.5 | … |
| Private | 7.7 | … |
| Community | 22.0 | … |
| Community home care | 6.6 | … |
| Geography | ||
| Urban academic | 46.2 | … |
| Urban community/suburban | 38.5 | … |
| Rural | 13.2 | … |
| Participation in traveling clinics | 13.2 | … |
| Participation in telehealth/ECHO® | 20.9 | … |
| Types of patients seen, % | ||
| General rheumatology | 36.3 | … |
| General pediatric rheumatology | 13.2 | … |
| JIA | 25.3 | … |
| IA | 49.5 | … |
| Spondyloarthropathy | 45.1 | … |
| Connective tissue disorders | 39.6 | … |
| Crystalline arthropathy | 40.7 | … |
| Degenerative spinal disorders | 34.1 | … |
| Osteoporosis | 29.7 | … |
| Nonarticular disorders | 19.8 | … |
| Osteoarthritis | 58.2 | … |
| Geriatric musculoskeletal | 18.7 | … |
| Orthopedic (eg, fracture or arthroplasty assessment clinics) | 24.2 | … |
Abbreviation: ECHO®, Extension for Community Healthcare Outcomes; ERP, extended role practitioner; IA, inflammatory arthritis; JIA, juvenile idiopathic arthritis; MSK, musculoskeletal.
Administrators/researchers not included.
Wilcoxon rank‐sum P value < 0.0001 between ERP and non‐ERP groups.
Training characteristics
The engagement in arthritis care training undertaken by ERPs and non‐ERPs is shown in Figure 1. Overall, of those reporting institutional/apprenticeship and other training (n = 25), 84.0% were classified as ERPs; however, those reporting institutional training alone were a minority (n = 7: ERPs = 2, non‐ERPs = 5). Specific post‐licensure training undertaken by ERPs, further denoted by their health discipline, is shown in Table 3.
Figure 1.
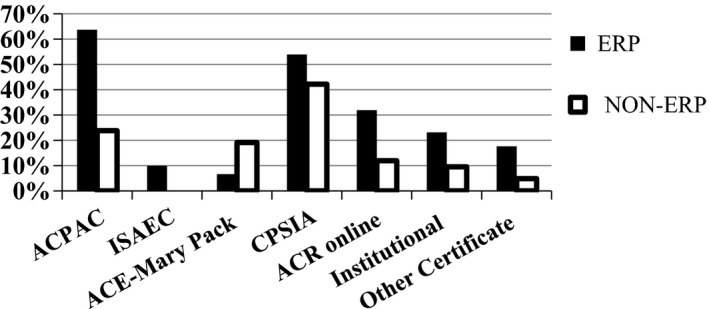
ERP vs. non‐ERP participation in post‐licensure training
Table 3.
Post‐licensure arthritis care training undertaken by ERPs
| Training | ERP Health Disciplines (n = 91) | |||
|---|---|---|---|---|
| PT (n = 60), % | OT (n = 17), % | RN (n = 8), % | Other (n = 6), % | |
| ACPAC | 68.3 | 70.6 | 62.5 | 0.0 |
| ISAEC | 10.0 | 0.0 | 0.0 | 50.0 |
| Mary Pack ACE | 6.7 | 5.9 | 12.5 | 0.0 |
| CPSIA | 53.3 | 70.6 | 50.0 | 16.7 |
| ACR online | 33.3 | 29.4 | 50.0 | 0.0 |
| Institutional | 28.3 | 11.8 | 25.0 | 0.0 |
| Other | 18.3 | 11.8 | 12.5 | 33.3 |
Abbreviation: ACPAC, Advanced Clinician Practitioner in Arthritis Care; ACR, American College of Rheumatology; CPSIA, Clinical Practice Skills for Inflammatory Arthritis; ERP, extended role practitioner; ISAEC, Interprofessional Spine Assessment and Education Clinics; Mary Pack ACE; OT, occupational therapist; PT, physical therapist; RN, registered nurse.
Clinical practice setting and funding
Most ERP roles were funded either by hospitals (70.3%) or The Arthritis Society (17.6%), reflective of global budget allocation. Half (49.5%) of hospital positions served acute outpatients. Most ERPs reported working in urban academic institutions (46.2%) or urban community/suburban settings (38.2%). However, 13.2% reported working in rural settings, which included those participating in traveling (visiting rheumatologist and/or ERP) clinics. Additionally, 20.9% of ERPs reported participating in telehealth/Extension for Community Healthcare Outcomes (ECHO®), which serves rural/ remote patients.
Clinical tasks
Clinical tasks performed by ERPs and non‐ERPs are summarized in Table 4. Many ERPs operate under physician delegation or medical directives, enabling them to work in an extended practice capacity. It was noted that ERPs and non‐ERPs continue to perform tasks aligned with their defining health discipline.
Table 4.
Clinical tasks performed by profession
| Task | ERPa | Non‐ERPa | |||
|---|---|---|---|---|---|
| Physiotherapy (n = 60), % | Occupational Therapy (n = 17), % | Registered Nurse (n = 8), % | Physiotherapy (n = 24), % | Occupational Therapy (n = 12), % | |
| Paper triage | 8.3 | 35.3 | 12.5 | 37.9 | 41.7 |
| Physical triageb | 60.0 | 58.8 | 12.5 | 29.2 | 41.7 |
| Review patients in clinicb | 61.7 | 64.7 | 37.5 | 37.5 | 66.7 |
| Order laboratory testsb | 46.7 | 35.3 | 25.0 | 4.2 | 8.3 |
| Order diagnostic testsb | 41.7 | 11.8 | 25.0 | 0.0 | 8.3 |
| Order x‐raysb | 61.7 | 47.1 | 25.0 | 4.2 | 8.3 |
| Recommend dosage changesb | 36.7 | 58.8 | 50.0 | 12.5 | 8.3 |
| Recommend joint injectionsb | 70.0 | 76.5 | 50.0 | 33.3 | 16.7 |
| Perform joint injectionsb | 10.0 | 17.7 | 25.0 | 0.0 | 0.0 |
| IM medications in clinic | 0.0 | 11.8 | 50.0 | 0.0 | 0.0 |
| Vaccination/TB education | 20.0 | 41.2 | 37.5 | 16.7 | 16.7 |
| Patient education | 78.3 | 88.2 | 50.0 | 66.7 | 83.3 |
| School letters | 26.7 | 47.1 | 0.0 | 37.5 | 58.3 |
| Insurance letters | 25.0 | 41.2 | 0.0 | 41.7 | 75.0 |
| Refer to specialist | 66.7 | 88.2 | 50.0 | 70.8 | 50.0 |
| Refer to allied health | 80.0 | 88.2 | 37.5 | 83.3 | 83.3 |
| Dictateb | 60.0 | 58.8 | 25.0 | 50.0 | 41.7 |
| Inpatient or outpatient consultations | 58.3 | 64.7 | 12.5 | 58.3 | 58.3 |
Abbreviation: IM, intramuscular; TB, tuberculosis.
Only those professions with >5 respondents are included in the table.
Wilcoxon rank‐sum P < 0.05 between ERP and non‐ERP groups.
Qualitative results
Training to support ERP roles
More than 90% of participants supported formal clinical/academic training for ERP roles for patient‐centered, provider‐centered, and systems‐centered reasons.
Participants highlighted that formal training ensures patient safety and an improved, different approach to care via an “understanding of a differential diagnosis and approaching the patient from a multi‐systems perspective” (respondent No. 84, PT/ERP).
As providers, participants recognized that they would gain knowledge and clinical skills through training. Academic programs were seen as filling a gap in their standard professional training: “It is impossible for entry level degree requirements to prepare clinicians for independent practice in specialized areas” (respondent No. 95, OT/non‐ERP).
Participants noted a growing need in the health system for experts in arthritis care, referencing long wait times to see specialists. Individuals occupying ERP roles contribute to the system of care, with one respondent writing that they “should and will become increasingly important in the triage and monitoring of the growing number of individuals with MSK conditions” (respondent No. 37, administrator).
Formal training helps build trust or credibility among the health care provider community, and an additional credential was seen as a signal of competence to others: “It is the only way to ensure that there is a basic documented level of knowledge, skills and judgment to act in an advanced role” (respondent No. 51, OT/ERP).
Barriers
Ninety percent of all respondents agreed that barriers to training exist. Although they identified barriers to training such as geography, personal needs, and patient‐care needs, administrative, post‐program recognition, and remuneration barriers were emphasized.
Administrative barriers were identified by one‐third of participants, protected time to pursue training opportunities being the most common: “The cost of formal training programs may be prohibitive as well as having to take time off work to attend the programs if your employer does not provide paid days for attending” (respondent No. 70, OT/ERP).
Other administrative barriers included managerial or administrative support to pursue training or the ERP role itself in practice. Notably, the administrator group rarely described administrative barriers.
Close to half of all respondents (47.5%) identified post‐program recognition barriers. The lack of role and credential recognition after completing existing training programs is a strong barrier to pursuing training. This sentiment was often compared to the recognition received by other professional groups:
Recognition of training once completed by organizations is often lacking…the [Ministry of Health]‐ for example, they recognize nurse practitioners as a unique health human resource; but there is no similar recognition of extended role practitioners from other professions who have successfully completed competency‐based programs. (respondent No. 110, PT/ERP)
There is also little incentive to pursue formal training when the role is misunderstood, when there are policy barriers restricting opportunities to practice as an ERP, or when there is no perceived financial benefit of a credential: “Policy limits the ability of advanced practitioners (eg, PT, OT) to refer directly to specialists. This could potentially save time and money by eliminating unnecessary visits to Primary Care Physicians for referral. Lastly, there needs to be review of the remuneration model in health care” (respondent No. 84, PT/ERP).
The most common barriers to training were financial, recognized by almost two‐thirds of the participants, including support for training by institutions and compensation once in practice: “Unless clinicians are financially supported by their institutions, it is very costly to enroll in formal training programs” (respondent No. 27, PT/ERP).
Support required
When asked what support was needed for ERP roles, respondents identified funding, policy change, and education.
ERPs and non‐ERPS recommended changes to policy, roles, and scopes of practice to allow for the augmented clinical practice of ERPs. Recommendations included promotion of the ERP designation through professional associations and regulatory bodies and standardization of existing roles, with titles harmonized to decrease the existing heterogeneity of these roles. Respondents also recommended larger policy changes, such as the ability to independently bill, grant ERPs broader capacity in the ordering and viewing of images and reports of relevant MSK imaging modalities, and directly refer to specialists: “[R]emove barrier to allow direct specialist (rheumatologist, orthopaedic surgeon) referrals from trained arthritis/MSK providers…access to appropriate diagnostic imaging modalities and laboratory evaluation to support preparing the patient for specialist consultation” (respondent No. 37, PT/non‐ERP). Participants articulated a desire to be heard and better included in health care practices, including taking part in strategy building, growth, and expansion planning.
Respondents suggested changes to the education/credentialing programs. Instead of ERP training being considered a continuing professional development program, ERP training could be recognized as a specialty focus of the individual professions, “similar to medical students who pursue specializations” (respondent No. 81, PT/ERP).
Although some seemed satisfied with entry‐to‐practice degrees in their disciplines and additional certification, others suggested that existing programs (eg, ACPAC with some additions such as a research component) could be better served via a recognized post‐graduate pathway: “Masters of Rehabilitation Science ‐ similar to the Orthopedic Manipulative Masters offered through McMaster and Western [Universities]” (respondent No. 79, PT/non‐ERP). Participants also suggested changes in the actual credential level. Some believed the training should be recognized as an interprofessional post‐licensure residency, similar to nurse practitioners, or equivalent to a masters or doctorate, which “may help to elevate the profile of the program” (respondent No. 2, OT/ERP).
DISCUSSION
This study identified the characteristics of 141 non‐physician allied health professionals in arthritis care and their general distribution across Canada. Two‐thirds of the respondents to the survey (n = 91) worked in an ERP capacity, as defined by our criteria, with most reporting Ontario as their primary practice setting. This is not surprising because most specialist post‐licensure programs in arthritis care are offered in Ontario (eg, ACPAC, TAS‐CPSIA), and most of their graduates continue to practice in this region (36).
The results of this exploratory study are important from a workforce management perspective to better understand attributes of ERPs who can augment capacity by supporting a known and growing shortage of rheumatologists (7, 15, 20). Differences in practice patterns were noted between ERPs and non‐ERPs, with more ERPs working in advanced practice capacities (while retaining activities reflective of their professional backgrounds); thus, potential for augmenting shared‐care practices exists. Much of the rheumatology workforce shrinkage is attributed to their imminent retirement plans in Canada (2); however, the present study reveals that almost half of the specialist ERP workforce also plan to retire within 10 years. There is clearly a need to support existing (and devise new) service‐demand management strategies to address the growing gap in care for an expanding population living with arthritis.
The majority of respondents identified the need for specialized training to fulfill an ERP role, yet half (non‐ERPs) expressed the opinion that insufficient opportunities exist for them to accomplish that end. We were not surprised by the heavy emphasis in our data on the need for individual training opportunities, but we were encouraged by the responses centered around patient‐care needs and systems, indicating that ERPs and non‐ERPs do see themselves as part of the health system and not only as individuals providing care.
Respondents conveyed that there is not a “one size fits all” approach for formal academic/clinical training to support interprofessional ERP roles in arthritis/MSK care. Participants expressed a desire for continued professional development opportunities that would be convenient and of high quality, with the potential to build on the individual professional licensure training and “scale up” existing training offered in programs such as ACPAC, ISAEC, TAS‐CPSIA, and Mary Pack ACE. It was largely represented that funding and institutional/administrative support are needed for practitioners to pursue continued professional development.
Barriers to the pursuit of training are various, from personal, geographic, and patient care/needs–related concerns to administrative, post‐program recognition, and financial/remuneration concerns. Some of the solutions to these are systems based, requiring changes in legislation and funding models. At every level, we suggest that participants, institutions, and regulatory, professional, and governmental partners work collectively to remove barriers to optimize the scope of formally trained arthritis/MSK ERPs, with a continued focus on providing high‐quality and safe patient care.
To that end, we were surprised by the absence of participants’ references to their regulatory bodies. Our participants come under the leadership of multiple professional organizations, and there was no mention of regulatory bodies’ impetus to mandate the pursuit of advanced training to support ERP roles. When regulators were mentioned, they appeared in questions about barriers to the scope of practice. Because regulators have an interest in ensuring the competency of their constituents, it was puzzling that we failed to identify a drive requiring the pursuit of standardized formal post‐licensure training to assume ERP roles in practice. Establishing standards of competency is known to be vital within the context of interprofessional education and practice (37).
ERPs themselves do need to have the necessary leadership skills to make these roles work once they enact these positions in their organizations. Given the current barriers, these leadership skills need to be built or deeply engrained because the lack thereof may contribute to some trained individuals not being able to develop a role in their organization.
Limitations of the study include the small number of pharmacists, chiropractors, and social workers who participated in the survey. Their numbers were so small we risked identifying them in our description and could not represent them as individual groups. The survey was circulated via electronic distribution of the AAC newsletter, although it was not issued in French, which may have limited its reach in Quebec. Because this study also used snowball sampling, in which initial survey respondents could send the survey to other practitioners perceived as working in advanced/extended practice roles, it is possible that an element of selection bias was introduced. This study was designed to capture descriptive information on the current workforce of ERPs working in arthritis care in Canada. No sample size justification was warranted because this was an exploratory study, with one of the objectives being to estimate the size of this workforce.
Future research considerations include sustaining and renewing this important group of arthritis care professionals and acknowledging that their roles in developing new models of care need to be included in broader arthritis workforce conversations addressing the impending shortage of rheumatologists in Canada. This study's intent was to add a unique data set to the literature for those who develop, provide, support, or finance advanced/extended care training models. As such, the results should be of interest to target groups, including clinicians, researchers, and users of the results of clinical research (academia, insurers, industry sponsors, policy makers, ministries of health and long‐term care, particularly those charged with overseeing health and human resources and access to specialist care portfolios). Although securing stable funding for continuing education is often a challenge (38, 39), understanding learning needs and expectations of ERPs to support such roles requires ongoing consideration.
In conclusion, no studies to date have assessed advanced practice workforce characteristics or the perceived need for the training of ERPs working in arthritis care. ERPs work in advanced practice capacities and can augment shared‐care practice with arthritis/MSK specialists. It is important to continue to support formal standardized training and measure workforce capacity of ERPs as they evolve and integrate into the Canadian health care system.
AUTHOR CONTRIBUTIONS
All authors drafted the article, revised it critically for important intellectual content, approved the final version to be published, and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design
Lundon, Inrig, Paton, Shupak, Kennedy, McGlynn, Barber.
Acquisition of data
Lundon, Inrig, Paton.
Analysis and Interpretation of data
Lundon, Inrig, Paton, Shupak, Kennedy, Barber.
ACKNOWLEDGMENTS
The authors wish to acknowledge the funding support of the Canadian Rheumatology Association in conducting this project.
APPENDIX 1. QUALITATIVE QUESTIONS
In your opinion, do you agree that formal clinical/academic training is necessary to work in an advanced/extended practice role in arthritis and musculoskeletal care?
Do you feel that adequate opportunities currently exist to pursue formal academic/clinical training to support advanced or extended practice roles in arthritis and musculoskeletal care?
Are there or do you perceive there to be any barriers in the pursuit/enrollment in any formal academic/clinical training programs to further support your advanced or extended practice role in arthritis and musculoskeletal care?
What more do you need to support advanced or extended practice roles in arthritis and musculoskeletal care?
In your opinion, what credential level should support the training of non‐physician advanced or extended role practitioners in arthritis care?
Supported by funding from the Canadian Rheumatology Association.
Katie Lundon, BScPT, MSc, PhD, Morag Paton, MEd: University of Toronto, Toronto, Ontario, Canada; 2Taucha Inrig, BScN, MDiv, Carol Kennedy, BScPT, MSc: St. Michael's Hospital, Toronto, Ontario, Canada; 3Rachel Shupak, MD, FRCP(C): St. Michael's Hospital and University of Toronto, Toronto, Ontario, Canada; 4Mandy McGlynn, MSc, BScPT: Toronto Rehabilitation Institute, University Health Network, Toronto, Ontario, Canada; 5Claire Barber, MD, PhD, FRCP(C): Cumming School of Medicine, University of Calgary, Calgary, Alberta, Canada.
Some of the leadership for this research study was provided by the Advanced Clinical Practitioner in Arthritis Care (ACPAC) Program/Continuing Professional Development at the University of Toronto. No other disclosures relevant to this article were reported.
REFERENCES
- 1. Barber CE, Marshall DA, Mosher DP, Akhavan P, Tucker L, Houghton K, et al. Development of system‐level performance measures for evaluation of models of care for inflammatory arthritis in Canada. J Rheumatol 2016;43:530–40. [DOI] [PubMed] [Google Scholar]
- 2. Barber CE, Jewett L, Badley EM, Lacaille D, Cividino A, Ahluwalia V, et al. Stand up and be counted: measuring and mapping the rheumatology workforce in Canada. J Rheumatol 2017;44:248–57. [DOI] [PubMed] [Google Scholar]
- 3. Barber C, Lundon K, Shupak R, Marshall D. So we stood up and got counted… Now what? The Journal of the Canadian Rheumatology Association 2016;26:7–8. [Google Scholar]
- 4. Arthritis Alliance of Canada . The impact of arthritis in Canada: today and over the next 30 years. Toronto: Arthritis Alliance of Canada; 2011. [Google Scholar]
- 5. Widdifield J, Paterson JM, Bernatsky S, Tu K, Thorne JC, Ahluwalia V, et al. The rising burden of rheumatoid arthritis surpasses rheumatology supply in Ontario. Can J Public Health 2013;104:e450–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Westby MD, Hassett AL. The ARHP promotes interdisciplinary approach to rheumatology patient care. The Rheumatologist. 2017; 1–3. [Google Scholar]
- 7. Ahluwalia V, Larsen TL, Kennedy CA, Inrig T, Lundon K. An advanced clinician practitioner in arthritis care can improve access to rheumatology care in community‐based practice. J Multidiscip Healthc 2019;12:63–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lundon K, Shupak R, Schneider R, Herold McIlroy J. Development and early evaluation of an inter‐professional post‐licensure education programme for extended practice roles in arthritis care. Physiother Can 2011;63:94–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lundon K, Shupak R, Canzian S, Ziesmann E, Schneider R. Don't let up: implementing and sustaining change in a new post‐licensure education model for developing extended role practitioners involved in arthritis care. J Multidiscip Healthc 2015;8:389–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Robarts S, Kennedy D, MacLeod AM, Findlay H, Gollish J. A framework for the development and implementation of an advanced practice role for physiotherapists that improves access and quality of care for patients. Healthc Q 2008;11:67–75. [DOI] [PubMed] [Google Scholar]
- 11. Aiken AB, McColl MA. Diagnostic and treatment concordance between a physiotherapist and an orthopedic surgeon: a pilot study. J Interprof Care 2008;22:253–61. [DOI] [PubMed] [Google Scholar]
- 12. Napier C, McCormack RG, Hunt MA, Brooks‐Hill A. A physiotherapy triage service for orthopaedic surgery: an effective strategy for reducing wait times. Physiother Can 2013;65:358–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rampersaud RY, Bidos A, Fanti CL, Young BW, Drew BM, Puskas DA. Preliminary report from the Ontario Interprofessional Spine Assessment and Education Clinics (ISAEC) [abstract]. The Spine Journal 2014;14 Suppl:S40. [Google Scholar]
- 14. Suter E, Birney A, Charland P, Misfeldt R, Weiss S, Howden JS, et al. Optimizing the interprofessional workforce for centralized intake of patients with osteoarthritis and rheumatoid disease: case study. Hum Resour Health 2015;13:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ahluwalia V, Lineker S, Sweezie R, Bell MJ, Kendzerska T, Widdifield J, et al. The effect of triage assessments on identifying inflammatory arthritis and reducing rheumatology wait times in Ontario. J Rheumatol 2020;47:461–7. [DOI] [PubMed] [Google Scholar]
- 16. Federation of Health Regulatory Colleges of Ontario . An interprofessional guide on the use of orders, directives and delegation for regulated health professionals in Ontario. 2020. URL: http://www.regulatedhealthprofessions.on.ca/orders,-directives,-delegation.html
- 17. Passalent LA, Kennedy C, Warmington K, Soever LJ, Lundon K, Shupak R, et al. System integration and clinical utilization of the Advanced Clinician Practitioner in Arthritis Care (ACPAC) program‐trained extended role practitioners in Ontario: a two‐year, system‐level evaluation. Healthc Policy 2013;8:56–70. [PMC free article] [PubMed] [Google Scholar]
- 18. Lineker SC, Lundon K, Shupak R, Schneider R, Mackay C, Varatharasan N. Arthritis extended‐role practitioners: impact on community practice (an exploratory study). Physiother Can 2011;63:434–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Warmington K, Kennedy CA, Lundon K, Soever LJ, Brooks SC, Passalent LA, et al. The patient perspective: arthritis care provided by Advanced Clinician Practitioner in Arthritis Care program‐trained clinicians. Open Access Rheumatol 2015;7:45–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Farrer C, Abraham L, Jerome D, Hochman J, Gakhal N. Triage of rheumatology referrals facilitates wait time benchmarks [published erratum appears in J Rheumatol 2017;44:263]. J Rheumatol 2016;43:2064–7. [DOI] [PubMed] [Google Scholar]
- 21. University of Toronto Faculty of Medicine . ACPAC program. URL: https://acpacprogram.ca.
- 22. Arthritis Society . Clinical practice skills for inflammatory arthritis. 2019. URL: https://arthritis.ca/healthcare-professionals/professional-education/clinical-practice-skills-for-inflammatory-arthriti.
- 23. Inter‐professional Spine Assessment and Education Clinics. URL: http://www.isaec.org/.
- 24. American College of Rheumatology . Educational activities. 2019. URL: https://www.rheumatology.org/Learning-Center/Educational-Activities.
- 25. Schultz K, Griffiths J. Implementing competency‐based medical education in a postgraduate family medicine residency training program: a stepwise approach, facilitating factors, and processes or steps that would have been helpful. Acad Med 2016;91:685–9. [DOI] [PubMed] [Google Scholar]
- 26. Lundon K, Kennedy C, Rozmovits L, Sinclair L, Shupak R, Warmington K, et al. Evaluation of perceived collaborative behaviour amongst stakeholders and clinicians of a continuing education programme in arthritis care. J Interprof Care 2013;27:401–7. [DOI] [PubMed] [Google Scholar]
- 27. Lundon K, Shupak R, Sunstrum‐Mann L, Galet D, Schneider R. Leading change in the transformation of arthritis care: development of an inter‐professional academic‐clinical education training model. Healthc Q 2008;11:62–8. [DOI] [PubMed] [Google Scholar]
- 28. Health Quality Ontario . Rapid access clinics for musculoskeletal care. 2019. URL: https://www.hqontario.ca/Quality-Improvement/Quality-Improvement-in-Action/Rapid-Access-Clinics-for-Musculoskeletal-Care.
- 29. Razmjou H, Robarts S, Kennedy D, McKnight C, MacLeod A, Holtby R. Evaluation of an advanced‐practice physical therapist in a specialty shoulder clinic: diagnostic agreement and effect on wait times. Physiother Can 2013;65:46–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. University of Toronto Faculty of Medicine . ACPAC program publications. 2019. URL: https://acpacprogram.ca/publications/.
- 31. SAS software: release 9.4. Cary (NC): SAS Institute; 2016. [Google Scholar]
- 32. NVivo qualitative data analysis software: release 12. Doncaster (Australia): QSR International; 2018. [Google Scholar]
- 33. Charmaz K. Grounded theory: objectivist and constructivist methods In: Denzin N, Lincoln Y, editors. Strategies of qualitative inquiry. 2nd ed London: SAGE Publications; 2003. p. 249–91. [Google Scholar]
- 34. Charmaz K. Constructing grounded theory: a practical guide through qualitative analysis. London: SAGE Publications; 2006. [Google Scholar]
- 35. Sandelowski M. Whatever happened to qualitative description?. Res Nurs Health 2000;23:334–40. [DOI] [PubMed] [Google Scholar]
- 36. Lundon K, Shupak R, Pullan A. Measuring the Advanced Clinician Practitioner in Arthritis Care (ACPAC) program trained extended role practitioner (ERP) workforce in Canada: a profile of practice settings, roles and participation in models of arthritis care in Canada [abstract]. Arthritis Rheumatol 2018;70 Suppl 10 URL: https://acrabstracts.org/abstract/measuring-the-advanced-clinician-practitioner-in-arthritis-care-acpac-program-trained-extended-role-practitioner-erp-workforce-in-canada-a-profile-of-practice-settings-roles-and-participation-in/. [Google Scholar]
- 37. Paradis E, Pipher M, Cartmill C, Rangel JC, Whitehead CR. Articulating the ideal: 50 years of interprofessional collaboration in Medical Education. Med Educ 2017;51:861–72. [DOI] [PubMed] [Google Scholar]
- 38. Campbell C, Sisler J. Supporting learning and continuous practice improvement for physicians in Canada: a new way forward. Summary report of the future of medical education in Canada (FMEC) CPD project. 2019. URL: https://www.fmec-cpd.ca/wp-content/uploads/2019/04/FMEC-CPD_Synthesized_EN.pdf.
- 39. Institute of Medicine . Redesigning continuing education in the health professions. Washington (DC): National Academic Press; 2010. [Google Scholar]


