Abstract
Introduction:
Laparoscopic cholecystectomy has been known as one of the most important prevalent and minimally invasive surgeries in medicine.
Aim:
The aim here was to investigate the changes in liver enzymes and bilirubin levels after laparoscopic cholecystectomy in patients diagnosed with chronic cholecystitis.
Methods:
This cross-sectional study was conducted at Poursina Hospital (Rasht, Iran) and 128 patients who met both inclusion and exclusion criteria were enrolled for further investigations. After collecting the patients’ bio-demographic information, levels of serum alkaline phosphatase, lactate dehydrogenase, alanine aminotransferase, aspartate aminotransferase, and bilirubin were checked before laparoscopic cholecystectomy and 24 (post-op 1) and 48 (post-op 2) h after laparoscopic cholecystectomy.
Results:
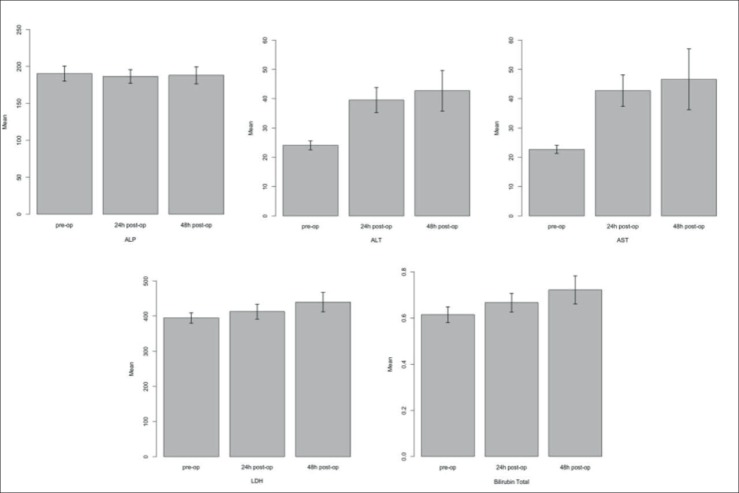
No significant difference was found in the serum levels of ALP in post-op 1 and 2 compared both to each other and to the baseline (P>0.05). Regarding AST and ALT, there was a significant increase in post-op 1 and 2 compared to their baseline values (P<0.05). However, the difference between post-op 1 and post-op 2 was not significant for these outcomes. Compared to baseline levels, LDH had a significant increase after post-op 2 (P=0.001); but not after post-op 1 (P >0.05). Moreover, total bilirubin levels showed significant increases at post-op 1 and post-op 2 from the baseline and also in comparison with each other (P < 0.05).
Conclusion:
Our results demonstrated a transient increase in liver function tests and bilirubin after laparoscopic cholecystectomy.
Keywords: Liver Function Tests, Bilirubin, Laparoscopic Cholecystectomy, Cholelithiasis
1. INTRODUCTION
Since 1882, cholecystectomy has been used as the most common treatment for gallstones, a prevalent gastrointestinal disease (1, 2). Nowadays, however, the laparoscopic cholecystectomy (LC) has replaced the mentioned conventional method
The main advantages of this method include lower hospitalization duration, small incisions made during the surgery, fewer complications, and shorter recovery periods for the patients (1-3). According to the studies, the incidence of complications after laparotomic cholecystectomy is reported 5-17% (3, 4, 5), while it is decreased to 2-10% in the laparoscopic approach (1, 2). Considering the mentioned advantages, laparotomic cholecystectomy is now approved as the gold standard treatment for symptomatic gallstone (1).
Any alterations in the liver enzymes following abdominal surgeries, especially cholecystectomy, could lead to a challenge after the surgery. So far, different results from various studies have been presented among which some seem to be contradictory. While in some studies it has been shown that laparoscopic cholecystectomy does no affect on liver function tests (6, 7), others believe in transient alterations following this procedure (8, 9); even 72 h after the intervention (4, 10). Although the exact mechanism behind the changes in these enzymes and bilirubin is still unclear, it has been hypothesized that anesthetics medications and impaired blood supply through the surgery (3, 4) could play roles. Impaired blood supply due to cardiovascular issues could also be resulted in increased intra-abdominal pressure after carbon-dioxide (CO2) injection or its absorption. The mentioned condition might be a possible etiology as well as reverse Trendelenburg position (11, 2, 12).
2. AIM
According to the facts stated above, the aim of the current study was to investigate the possible changes in the liver enzymes levels following laparoscopic cholecystectomy in patients diagnosed with chronic cholecystitis.
3. METHODS
This cross-sectional study was conducted in Poursina Hospital (Guilan University of Medical Sciences, Rasht, Iran) between April 2017 and April 2018. Our protocols and methods were approved by the Medical Ethics Committee of the affiliated hospital. All patients were asked to sign a paper printed consent form freely after being explained all the aims and methods according to their knowledge. The study was also in accordance with the 1975 Declaration of Helsinki and its next revisions. The inclusion criteria were adopted to include any patient diagnosed with gallstone and a candidate for laparoscopic cholecystectomy. The exclusion criteria were defined as iatrogenic biliary injuries, common bile duct diameter greater than 12 mm, preoperative abnormal liver function tests, hypotension, pregnancy, pancreatitis, previous major abdominal surgery, and diabetes mellitus.
The demographic data including age, gender, height, weight, body mass index (BMI), and duration of operation were recorded in patients’ files. The patients underwent laparoscopic cholecystectomy under general anesthesia with CO 2 pressure between 15 to 20 mmHg. The blood samples were collected before the operation, and also 24 h (post-op 1) and 48 h (post-op 2) after the surgery and analyzed for alkaline phosphatase (ALP), alanine aminotransferase (ALT), aspartate aminotransferase (AST), lactate dehydrogenase (LDH), and bilirubin levels.
Data from each collection step were saved into an Excel file and re-checked by another author. Then, the appropriate statistical analyses were performed. Repeated-measure analysis of variance and Bonferroni tests were used to investigate the difference between pre and post-surgical levels of laboratory parameters as well as their possible associations with demographic characteristics. Any P-values less than 0.05 were considered statistically significant. Analyses were performed using Statistical Package for Social Sciences version 20.0 (SPSS, Inc. Chicago, IL, USA).
4. RESULTS
Based on the inclusion criteria, 140 patients were enrolled among whom a final number of 128 patients were selected for further analysis after meeting the exclusion criteria. Table 1 demonstrates the demographic data of our study population. As data shows, 85.16% (N=109) and 14.84% (N=19) of the patients were female and male, respectively, with the mean age of 65.1±14.6 years. Also, the mean calculated BMI was 19.43±2.19 (kg/m2). Table 2 represents mean, standard deviation and 95% confidence interval of laboratory parameters.
The differences between outcome measurements of baseline values and post-op 1 and 2 and also between post-op 1 and post-op 2 were also assessed and shown in Table 3. According to these data, no statistically significant difference was found between baseline and post-op 1 and 2 values for ALP (p=0.20 and 0.99, respectively). A comparison between post-op 1 and 2 values showed the same result (p=0.99). On the other hand, AST and ALT values were significantly different in post-op 1 and 2 measurements compared to their preoperative level (P<0.05). However, the difference between post-op 1 and 2 values was not statistically significant (p=0.57 for AST and 0.33 for ALT). In comparison to the baseline level, LDH had a significant increase in post-op 2 samples (P<0.05), but not in post-op 1; although, it was close to significance. (P=0.06). There was also a significant rise in LDH in post-op 2 samples compared to post-op 1 levels (P<0.05). Total bilirubin measurements demonstrated a significant increase compared to their baseline values in both post-op 1 and 2 evaluations (P<0.05). There was also a significant increase in total bilirubin from post-op1 to post-op 2 measurements.
In sub-group analysis, age, gender and, BMI showed no significant association with the postoperative changes of the evaluated enzymes (P>0.05).
5. DISCUSSION
In the current study, we found significant increases in AST, ALT, and bilirubin, 24 h and 48 h after laparoscopic cholecystectomy. Moreover, a delayed significant increase of LDH and a non-significant change of ALP were observed 48 h after the surgery. Moreover, the results showed no evidence on the role of age, sex, and BMI on the mentioned parameters.
Nowadays, the laparoscopic cholecystectomy has replaced open surgery and is considered as the gold standard treatment for gallstone disease. However, some studies have shown that alterations in liver enzymes, bilirubin, and LDH are commonly expected after laparoscopic surgeries with different etiologies being hypothesized. In a study by Guven and Oral, liver enzymes, as well as LDH, were investigated in two groups of patients who had undergone laparoscopic and open cholecystectomy. According to their results, AST, ALT, and LDH (but not ALP) were significantly increased following laparoscopic cholecystectomy (13). Hasukic et al. showed that 48-hour post-intervention levels of AST and ALT were significantly higher in patients undergone laparoscopic cholecystectomy in comparison to open surgery. However, they mentioned that LDH and ALP were remained unchanged after 48 h. Considering another similar study by Halevy et al., it has been shown that after laparoscopic cholecystectomy, AST, ALT, ALP, and bilirubin levels were increased by 73%, 82%, 53%, and 14%, respectively (10). Enzymes returned to normal values 72 hours after surgery in this study. Their result was almost in line with our results, except for ALP levels and the duration of follow up. In our study, there was a trend toward normal values for AST and ALT, 48 hours after surgery which could be confirmed in a longer period of follow up. There are controversies regarding the effect of issues such as gender and age of the patient and the post-operation time that enzymes increase after surgery on the enzyme alterations (14, 7, 1, 15, 10). We found that there is no significant correlation between age, gender and, BMI on the post-operative enzyme alterations.
Hajnasrollah et al. demonstrated that nearly four percent of patients undergoing laparoscopic cholecystectomy had bile duct injuries in further need of surgical repairs. Accordingly, they recommended assessing the liver enzymes for the detection of potential biliary injuries (12). However, in our study, it was observed that an increase in liver enzymes was common among the majority of patients undergoing laparoscopic cholecystectomy regardless of bile duct injury, and therefore this alteration could not be an appropriate tool for monitoring iatrogenic bile duct injuries.
Neri et al. demonstrated that the mean levels of AST and ALT were significantly increased 24 h after laparoscopic cholecystectomy which is compatible with our results. They also detected no significant changes in bilirubin levels which are in contrast to our finding of a significant increase in. bilirubin levels after surgery.
Furthermore, they showed that BMI>28 is a risk factor for alteration in the liver enzymes which seems not to agree with the results from our study. they also revealed that three days after surgery, the liver function tests regained their normal range (16). We followed our patients for 48 h after surgery and although the final values for AST and ALT were still significantly different from pre-operative measures, the difference between post-op 2 and post-op 1 was not significant which reflects the level of enzymes shifting towards their normal values. This outcome could be further confirmed through a longer follow-up course.
Studies are stating that increased abdominal pressure during laparoscopy could result in hepatocellular ischemia which in turn elevates serum level of ALT (17, 18). Mohindra et al. (17) reported an alteration in liver function test, especially ALT, in the patients undergoing laparoscopic cholecystectomy. However, we did not consider the effect of abdominal pressure as a factor of influence on the enzyme increase, although the same pattern of enzyme increase was observed in our study.
6. CONCLUSION
Our study demonstrated significant increases in the bilirubin and liver enzymes levels after LC, except for ALP. Considering that no side effect was observed after the surgery, this increase seems to be due to the laparoscopic surgery itself and not a serious complication. However, further studies with larger sample size and multi-center trials would yield more definite results, along with meta-analyses. Authors strongly suggest the consideration of confounding factors such as duration of surgery, background diseases, CO2 pressure, utilized anesthetic agents and longer follow-ups.
Figure 1. Comparing changes in liver enzymes, bilirubin, and lactate dehydrogenase levels before and after laparoscopic cholecystectomy. Pre-op; Pre-operation; Post-op; Post operation; AST: Aspartate aminotransferase; ALT: Alanine aminotransferase; ALP: Alkaline phosphatase; LDH: lactate dehydrogenase.
Table 1. demographic characteristics in patients.
| Frequency | Percent | ||
|---|---|---|---|
| < 60 | 37 | 28.91% | |
| Age Groups (years) | [60-70) | 28 | 21.88% |
| ≤70 | 63 | 49.22% | |
| Gender | Female | 109 | 85.16% |
| Male | 19 | 14.84% | |
| BMI (kg/m2) | Normal | 5 | 3.91% |
| Overweight | 65 | 50.78% | |
| Obese | 58 | 45.31% |
Table 2. Alterations in evaluated laboratory parameters. Post-op 1: 24 h after surgery and Post-op 2: 48 h after surgery.
| Parameter | Time | Mean±SD | 95% Confidence | |
|---|---|---|---|---|
| interval | ||||
| Total Bilirubin | Preoperative | 0.61±0.19 | [0.58 | -0.64] |
| Post-op 1 | 0.66±0.22 | [0.62-0.7] | ||
| Post-op 2 | 0.72±0.33 | [0.66 | -0.78] | |
| Alkaline Phosphatase (ALP) | Preoperative | 190.2±57.8 | [180.1 | -200.3] |
| Post-op 1 | 186.4±52.3 | [177.2 | -195.5] | |
| Post-op 2 | 187.9±63.9 | [176.73-199.1] | ||
| Alanine Aminotransferase (ALT) | Preoperative | 24.0±8.7 | [22.5 | -25.6] |
| Post-op 1 | 39.5±24.1 | [35.3 | -43.7] | |
| Post-op 2 | 42.6±39.0 | [35.8 | -49.5] | |
| Aspartate Aminotransferase (AST) | Preoperative | 22.6±7.7 | [21.3 | -24.0] |
| Post-op 1 | 42.7±30.2 | [37.4 | -48.0] | |
| Post-op 2 | 46.6±58.1 | [36.4 | -56.8] | |
| Lactate Dehydrogenase (LDH) | Preoperative | 394.5±84.2 | [379.8 | -409.3] |
| Post-op 1 | 412.4±116.6 | [392.0 | -432.8] | |
| Post-op 2 | 439.5±154.3 | [412.5 | -466.5] | |
Table 3. Comparison of evaluated laboratory parameters across the time.
| Parameter | Primary time | Secondary time | Mean | P Value* | 95% Confidence |
|---|---|---|---|---|---|
| Difference±SD | interval | ||||
| Post-op 1 | 3.82±2.06 | 0.200 | [-1.19-8.84] | ||
| Preoperative | |||||
| ALP | Post-op 2 | 2.30±3.00 | 0.99 | [-4.98-9.59] | |
| Post-op 1 | Post-op 2 | -1.51±2.37 | 0.99 | [-7.28-4.24] | |
| Post-op 1 | -20.04±2.63 | 0.001 | [-26.44-(-13.64)] | ||
| Preoperative | |||||
| AST | Post-op 2 | -23.93±5.05 | 0.001 | [-36.19-(-11.67)] | |
| Post-op 1 | Post-op 2 | -3.88±2.96 | 0.577 | [-11.08-3.31] | |
| Post-op 1 | -15.44±1.98 | 0.001 | [-20.27-(-10.62)] | ||
| Preoperative | |||||
| ALT | Post-op 2 | -18.62±3.37 | 0.001 | [-26.81-(-10.43)] | |
| Post-op 1 | Post-op 2 | -3.17±1.97 | 0.334 | [-7.97-1.62] | |
| Post-op 1 | -17.86±7.67 | 0.065 | [-36.48-0.76] | ||
| Preoperative | |||||
| LDH | Post-op 2 | -44.93±11.93 | 0.001 | [-73.89-(-15.98)] | |
| Post-op 1 | Post-op 2 | -27.07±6.68 | <0.001 | [-43.29-(-10.86)] | |
| Post-op 1 | -0.052±0.016 | 0.005 | [-0.091-(-0.013)] | ||
| Total | Preoperative | ||||
| Post-op 2 | -0.107±0.25 | 0.001 | [-0.168-(-.047)] | ||
| bilirubin | |||||
| Post-op 1 | Post-op 2 | -0.055±0.20 | 0.018 | [-0.103-(-.007)] | |
| ALP: Alkaline phosphatase; ALT: Alanine aminotransferase; AST: aspartate aminotransferase; LDH: | |||||
| lactate | dehydrogenase (LDH); Post-op 1: 24 hours after surgery and Post-op 2: 48 hours after surgery. | ||||
Adjustment for multiple comparisons: Bonferroni test
Author’s contribution
SAM and NE gave substantial contributions to the conception or design of the work in acquisition, analysis, or interpretation of data for the work. SAM and NE had a part in article preparing for drafting or revising it critically for important intellectual content, and SAM and NE gave final approval of the version to be published and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Financial support and sponsorship
None.
Conflict of interests
There are no conflicts of interest.
REFERENCES
- 1.Hasukic S, Kosuta D, Muminhodzic K. Comparison of postoperative hepatic function between laparoscopic and open cholecystectomy. Medical Principles and Practice. 2005;14(3):147–150. doi: 10.1159/000084630. [DOI] [PubMed] [Google Scholar]
- 2.Kotake Y, Takeda J, Matsumoto M, Tagawa M, Kikuchi H. Subclinical hepatic dysfunction in laparoscopic cholecystectomy and laparoscopic colectomy. British journal of anaesthesia. 2001;87(5):774–777. doi: 10.1093/bja/87.5.774. [DOI] [PubMed] [Google Scholar]
- 3.Bostanci EB, Yol S, Teke Z, Kayaalp C, Sakaogullari Z, Turkcu UO, et al. Effects of carbon dioxide pneumoperitoneum on hepatic function in obstructive jaundice: an experimental study in a rat model. Langenbeck’s archives of surgery. 2010;395(6):667–676. doi: 10.1007/s00423-009-0577-6. [DOI] [PubMed] [Google Scholar]
- 4.Giraudo G, Contul RB, Caccetta M, Morino M. Gasless laparoscopy could avoid alterations in hepatic function. Surgical endoscopy. 2001;15(7):741–746. doi: 10.1007/s004640090020. [DOI] [PubMed] [Google Scholar]
- 5.Meierhenrich R, Gauss A, Vandenesch P, Georgieff M, Poch B, Schutz W. The effects of intraabdominally insufflated carbon dioxide on hepatic blood flow during laparoscopic surgery assessed by transesophageal echocardiography. Anesthesia & Analgesia. 2005;100(2):340–347. doi: 10.1213/01.ANE.0000143566.60213.0A. [DOI] [PubMed] [Google Scholar]
- 6.Mujicić E, Durić A, Radovanovioć J. Influence of CO2 pneumoperitoneum on liver function. Med Arch. 2006;60(2):87–89. [PubMed] [Google Scholar]
- 7.Sakorafas G, Anagnostopoulos G, Stafyla V, Koletis T, Kotsifopoulos N, Tsiakos S, et al. Elevation of serum liver enzymes after laparoscopic cholecystectomy. NZ Med J. 2005;118(1210):U1317. [PubMed] [Google Scholar]
- 8.Curro G, Iapichino G, Melita G, Lorenzini C, Cucinotta E. Laparoscopic cholecystectomy in Child-Pugh class C cirrhotic patients. JSLS: Journal of the Society of Laparoendoscopic Surgeons. 2005;9(3):311. [PMC free article] [PubMed] [Google Scholar]
- 9.Neudecker J, Sauerland S, Neugebauer E, Bergamaschi R, Bonjer H, Cuschieri A, et al. The European Association for Endoscopic Surgery clinical practice guideline on the pneumoperitoneum for laparoscopic surgery. Surgical endoscopy. 2002;16(7):1121–1143. doi: 10.1007/s00464-001-9166-7. [DOI] [PubMed] [Google Scholar]
- 10.Halevy A, Gold-Deutch R, Negri M, Lin G, Shlamkovich N, Evans S, et al. Are elevated liver enzymes and bilirubin levels significant after laparoscopic cholecystectomy in the absence of bile duct injury? Annals of surgery. 1994;219(4):362. doi: 10.1097/00000658-199404000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tan M, Xu FF, Peng JS, Li D-M, Chen LH, Lv BJ, et al. Changes in the level of serum liver enzymes after laparoscopic surgery. World Journal of Gastroenterology: WJG. 2003;9(2):364. doi: 10.3748/wjg.v9.i2.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rademaker B, Odoom J, Kalkman C, Ringers J. Haemodynamic effects of pneumoperitoneum for laparoscopic surgery: a comparison of CO2 with N2O insufflation. European journal of anaesthesiology. 1994;11(4):301–306. [PubMed] [Google Scholar]
- 13.Guven H, Oral S. Liver enzyme alterations after laparoscopic cholecystectomy. Journal of Gastroenterological and Liver Diseases. 2007;16(4):391. [PubMed] [Google Scholar]
- 14.Saber AA, Laraja RD, Nalbandian HI, Pablos-Mendez A, Hanna K. Changes in liver function tests after laparoscopic cholecystectomy: not so rare, not always ominous. The American surgeon. 2000;66(7):699. [PubMed] [Google Scholar]
- 15.Hasukić Š. Postoperative changes in liver function tests: randomized comparison of low-and high-pressure laparoscopiccholecystectomy. Surgical Endoscopy and Other Interventional Techniques. 2005;19(11):1451–1455. doi: 10.1007/s00464-005-0061-5. [DOI] [PubMed] [Google Scholar]
- 16.Neri V, Ambrosi A, Fersini A, Tartaglia N, Cianci P, Lapolla F, et al. Laparoscopic cholecystectomy: evaluation of liver function tests. Annali italiani di chirurgia. 2014;85(5):431–437. [PubMed] [Google Scholar]
- 17.Mohindra M, Singh MP, Arora D. Incidence of Alteration in Liver Functional Tests in Patients Undergoing Laparoscopic Cholecystectomy. Journal of Advanced Medical and Dental Sciences Research. 2017;5(10):62–64. [Google Scholar]
- 18.Rizvi ZA, Hafeez MA, Majeed S, Aslam F, Ahmad SH, Bhatti HW, et al. Effects of Laparoscopic Cholecystectomy on Serum Alt Levels. Journal of Rawalpindi Medical College. 2018;22(S-1):15–18. [Google Scholar]