Summary
Background
The Middle East respiratory syndrome coronavirus (MERS-CoV) is an emerging virus involved in cases and case clusters of severe acute respiratory infection in the Arabian Peninsula, Tunisia, Morocco, France, Italy, Germany, and the UK. We provide a full description of a fatal case of MERS-CoV infection and associated phylogenetic analyses.
Methods
We report data for a patient who was admitted to the Klinikum Schwabing (Munich, Germany) for severe acute respiratory infection. We did diagnostic RT-PCR and indirect immunofluorescence. From time of diagnosis, respiratory, faecal, and urine samples were obtained for virus quantification. We constructed a maximum likelihood tree of the five available complete MERS-CoV genomes.
Findings
A 73-year-old man from Abu Dhabi, United Arab Emirates, was transferred to Klinikum Schwabing on March 19, 2013, on day 11 of illness. He had been diagnosed with multiple myeloma in 2008, and had received several lines of treatment. The patient died on day 18, due to septic shock. MERS-CoV was detected in two samples of bronchoalveolar fluid. Viral loads were highest in samples from the lower respiratory tract (up to 1·2 × 106 copies per mL). Maximum virus concentration in urine samples was 2691 RNA copies per mL on day 13; the virus was not present in the urine after renal failure on day 14. Stool samples obtained on days 12 and 16 contained the virus, with up to 1031 RNA copies per g (close to the lowest detection limit of the assay). One of two oronasal swabs obtained on day 16 were positive, but yielded little viral RNA (5370 copies per mL). No virus was detected in blood. The full virus genome was combined with four other available full genome sequences in a maximum likelihood phylogeny, correlating branch lengths with dates of isolation. The time of the common ancestor was halfway through 2011. Addition of novel genome data from an unlinked case treated 6 months previously in Essen, Germany, showed a clustering of viruses derived from Qatar and the United Arab Emirates.
Interpretation
We have provided the first complete viral load profile in a case of MERS-CoV infection. MERS-CoV might have shedding patterns that are different from those of severe acute respiratory syndrome and so might need alternative diagnostic approaches.
Funding
European Union; German Centre for Infection Research; German Research Council; and German Ministry for Education and Research.
Introduction
In June, 2012, a coronavirus belonging to a group of viruses that had previously only been detected in bats was cultured from respiratory secretions of a patient who had died from severe acute respiratory infection.1 The same agent was retrospectively detected in clinical samples from a hospital outbreak of severe acute respiratory infection that occurred in Jordan in April, 2012, marking the first known occurrence of the virus in people.2 The agent has been named Middle East respiratory syndrome coronavirus (MERS-CoV).3 As of June 10, 2013, 55 laboratory-confirmed cases had been reported in Jordan, Saudi Arabia, the UK, France, Italy, Germany, and Tunisia.3 31 individuals with laboratory-confirmed infection had died. Few virological data have become available for MERS-CoV cases, and there is no information about the viral genome sequence, which could identify important epidemiological characteristics.4, 5, 6
Here, we provide a full description of a fatal case of MERS-CoV infection imported to Munich, Germany, from Abu Dhabi, including a chronological profile of virus concentrations in diverse body compartments. We fully sequenced the MERS-CoV genome, and therefore could do a chronologically calibrated phylogenetic analysis with all available MERS-CoV genome sequences. These data were complemented by novel sequence data from an unlinked case treated in Germany in 2012.7, 8
Methods
Patient and procedures
We report data for a patient who was admitted to the Klinikum Schwabing (Munich, Germany) in March, 2013. Investigation was done as part of a public health intervention according to the German Infection Protection Act. Written consent for scientific assessment was obtained from the patient's spouse as part of the patient treatment contract.
We did diagnostic RT-PCR and indirect immunofluorescence, following WHO recommendations.7, 9 For serum neutralisation tests, we grew Vero B4 cells to subconfluence in 24-well plates. Pre-incubation reactions contained 25 plaque-forming units of MERS-CoV (EMC strain) in 100 μL of medium, mixed one-to-one with serum samples from the patient prediluted in medium. The starting dilution was a tenth. After 1 h incubation at 37°C, each well was infected for 1 h at 37°C with the total 200 μL pre-incubation reaction. Supernatants were removed and overlaid with Avicell resin as described by Herzog and colleagues.10 Assays were terminated and stained after 3 days. We defined neutralisation titres as the serum dilution reducing the number of plaques in four parallel wells in summary by greater than 90%. Antibodies were tested by immunofluorescence assay.7
All clinical materials stored in the ward and laboratories were gathered and submitted for virological diagnostic tests. From the time of laboratory diagnosis, respiratory, faecal, and urine samples were obtained. We designed two different sets of primers generating overlapping amplicons (available on request). The first set consisted of 70 amplicons, 386–800 bp in length, with all primers containing two strong Watson-Crick bps at their 3′ ends, so as to bind the template with high affinity. The second set consisted of 68 amplicons, 415–761 bp in length, with primers that had no more than two strong bps in their five 3′ terminal nucleotides and no strong pairings in the two 3′ positions. This method of primer design can decrease sensitivity, but it prevents mispriming within the product, which can improve the success of amplification. After RT-PCR, we sequenced all fragments on a Roche 454 Junior instrument (Roche, Penzberg, Germany) and assembled in Geneious (version 6.1.2). Virus quantification was done with standard calibration curves that were based on quantified in-vitro transcribed RNA for the upE target gene.9
We constructed a maximum likelihood tree of the five available complete MERS-CoV genomes with PhyML11 and the GTR+Gamma model of molecular evolution; we assessed phylogenetic support with 1000 bootstrap replicates. We inferred a timescale by linear regression of genetic divergence from the root against time of collection of the samples. The root was placed such that the correlation coefficient was maximised. A phylogenetic tree based on all available MERS-CoV sequences was calculated with PhyML11 on a concatenated 4012 bp dataset with the HKY substitution model. Reduction of the dataset was determined by the small number of sequence fragments that could be retrieved from a stored clinical sample containing a small amount of the virus, derived from a patient treated in Essen, Germany.
Role of the funding source
The sponsors of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding authors had full access to all the data in the study and final responsibility to submit for publication.
Results
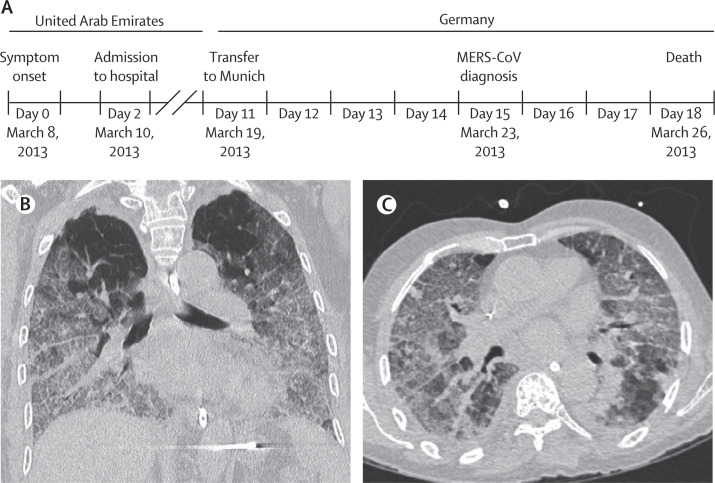
On March 8 (day 0), the patient—a 73-year-old man from Abu Dhabi, United Arab Emirates—abruptly developed flu-like symptoms, with fever and non-productive cough. He was admitted to Mafraq hospital (Abu Dhabi) on day 2 (figure 1 ), and was diagnosed with pneumonia. He was intubated on day 9 because of progressive hypoxia and acute respiratory distress syndrome (fraction of inspired oxygen 60%; positive end-expiratory pressure 10 cm H2O). The patient had received intensive antimicrobial treatment with meropenem, levofloxacin, vancomycin, caspofungin, aciclovir, and oseltamivir during his stay in an intensive care unit in Abu Dhabi, without major improvement in his pulmonary function. The patient was transferred to Klinikum Schwabing (Munich, Germany) on March 19, 2013 (figure 1).
Figure 1.
Disease and treatment
(A) Chronology. Frontal (B) and horizontal (C) CT scans done on day 12 of disease, showing intense basally-pronounced congestions indicative of atypical pneumonia and acute respiratory distress syndrome. MERS-CoV=Middle East respiratory syndrome coronavirus.
The patient had been diagnosed with multiple myeloma in 2008, and had received several lines of treatment in the previous few years, such as high-dose chemotherapy with autologous stem-cell transplantation in 2009. At relapse of his multiple myeloma in November, 2012, he was given lenalidomide plus dexamethasone. Relatives reported that the patient owned camels, and had taken care of a diseased animal shortly before onset of symptoms. No animal samples, or further details about potential sources or exposures could be retrieved.
During his stay in Munich, we recorded thrombocytopenia (table 1 ). Thrombocytopenia was also reported in the first described case of MERS-CoV infection,1 in two of four patients from a family cluster in Saudi Arabia,12 and in the two cases reported from France.5
Table 1.
Laboratory measurements
| Day 11 | Day 12 | Day 14 | Day 16 | Day 17 | Day 18 (death) | Normal range | |
|---|---|---|---|---|---|---|---|
| Blood count | |||||||
| Leucocyte count (cells×109 per L) | 4·7 | 3·8 | 7·2 | 7·6 | 6·7 | 4·8 | 3·5–9·8 |
| Lymphocytes (proportion of 1·0) | ND | 0·08 | ND | ND | ND | 0·05 | 0·16–0·45 |
| Platelet count (cells×109 per L) | 36 | 18 | 11 | <5 | 8 | <5 | 140–360 |
| Haematocrit (proportion of 1·0) | 0·299 | 0·310 | 0·219 | 0·246 | 0·265 | 0·152 | 0·40–0·53 |
| Haemoglobin (g/L) | 100 | 103 | 74 | 85 | 92 | 51 | 135–175 |
| Coagulation variables | |||||||
| Prothrombin time (international normalised ratio) | 1·3 | 1·4 | 1·5 | 1·5 | 1·7 | 2·5 | .. |
| Partial thromboplastin time (s) | 46 | 50 | 57 | 40 | 46 | 58 | 26–37 |
| Serological variables | |||||||
| Creatine kinase (μkat/L) | 2·4 | ND | ND | 13·8 | 28·1 | 26·5 | 0·5–3·4 |
| C-reactive protein (nmol/L) | 652·4 | 800·9 | 2247·7 | 473·3 | 285·7 | 167·6 | <47·6 |
| Procalcitonin (μg/L) | 0·24 | ND | ND | ND | 1·01 | 1·61 | <0·5 |
| Serum creatinine (μmol/L) | 70·7 | 70·7 | 221·0 | 194·5 | 247·5 | 327·1 | 61·9–106·1 |
| Urea (mmol/L) | 15·3 | 18·3 | 39·8 | 25·3 | 34·6 | 38·5 | 3·0–9·0 |
| Lactate dehydrogenase (μkat/L) | 9·5 | 9·2 | ND | ND | 21·9 | 34·8 | 2·0–3·7 |
| Gamma-glutamyltransferase (U/L) | 47 | ND | 57 | 40 | ND | 27 | 12–64 |
| Alanine transaminase (μkat/L) | 0·48 | ND | 0·45 | 0·40 | ND | 1·80 | <0·75 |
| Total bilirubin (μmol/L) | 5·3 | ND | 20·5 | 17·1 | ND | 18·8 | 3·4–20·5 |
ND=not determined.
The patient developed renal insufficiency on day 14, and required dialysis. Despite continuous invasive ventilation and antibiotic treatment, the patient's health status deteriorated. Death occurred on day 18 and was due to septic shock, with signs of haemolysis and acute coagulation disorder (figure 1, table 1).
After hospital admission in Munich, infection with MERS-CoV was suspected on the basis of treatment-refractory acute respiratory distress syndrome, combined with the geographical origin of the patient. Bronchoalveolar fluid was obtained on March 20 and 22 (days 12 and 14). MERS-CoV was detected in both samples by RT-PCR. We also detected herpes simplex virus type 1 DNA13 (6·4 × 104 to 1·9 × 107 copies per mL) and rhinovirus RNA14 (3·7 × 105 to 2·1 × 109 copies per mL) by (RT-)PCR in both samples.
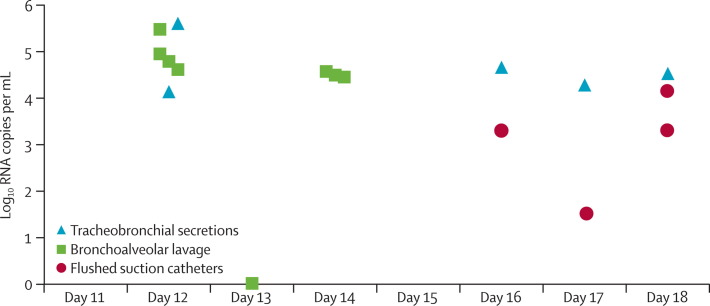
MERS-CoV RNA concentrations in respiratory samples ranged from 933 to 1·2 × 106 genome copies per mL. Virus concentrations seemed to be higher in samples taken earlier in the course than in those obtained later (figure 2 ). Concentrations were more variable in tracheobronchial samples than in bronchoalveolar lavage samples (figure 2), which was ascribed to variation in volumes of saline solution applied during removal of tracheobronchial samples. Notably, suction catheters without opening at point of care and stored for as long as 5 days at 8°C in a refrigerator in the intensive care unit tested consistently positive but yielded up to roughly 3·5log10 lower RNA concentrations than did those in fresh tracheobronchial aspirates taken on the same days (figure 2).
Figure 2.
Absolute virus concentrations in respiratory secretions and bronchoalveolar lavage samples
Immunofluorescence assays yielded endpoint titres on day 16 of infection (table 2 ). An IgM-specific immunofluorescence assay confirmed recent infection in the same serum sample (table 2). Plaque-reduction neutralisation test confirmed MERS-CoV specificity of detected antibody titres (table 2). These titres were somewhat lower than those recorded for serum samples from an unlinked non-fatal case of MERS-CoV treated in Germany in 2012.8 Serum samples from this patient had been taken later than they were for our patient (table 2).
Table 2.
Comparison of serological results in two patients with Middle East respiratory syndrome coronavirus infection treated in Germany
|
Indirect Immunofluorescence assay |
Virus neutralisation assay: 90% plaque reduction at titre | ||
|---|---|---|---|
| IgG | IgM | ||
| Munich case; day 16 | 1/2560 | 1/80 | 1/320 |
| Essen case; week 3 | 1/10 000 | 1/1000 | 1/640 |
| Essen case; week 8 | 1/10 000 | 1/100 | 1/640 |
We tested two urine samples on day 12, one on day 13, and one on day 16. One of the two samples on day 12, and the sample from day 13 were positive, meaning that the virus was not present in urine after renal failure (day 14), with a maximum virus concentration of 2691 RNA copies per mL on day 13. Both stool samples obtained on day 12 and the five on day 16 were positive, with up to 1031 RNA copies per g, which is a concentration close to the lowest detection limit of the assay. We recorded a low virus concentration in one of two oronasal aspirate samples taken from the intubated patient on day 16 (5370 copies per mL). One dialysate sample and two serum samples on day 16, and one serum sample on day 18 were negative.
Although we obtained several isolates for the herpes simplex virus type 1, repeated attempts to isolate MERS-CoV were unsuccessful. Herpes simplex virus is a frequent bystander infection in intubated patients, and is known to not affect the cardiorespiratory prognosis and outcome.15
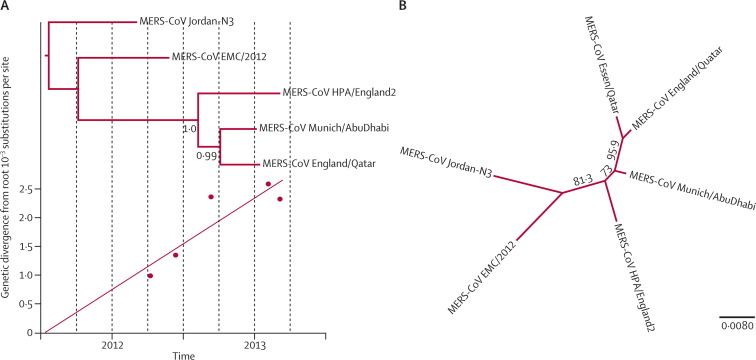
We sequenced the full MERS-CoV genome directly from respiratory samples (GenBank accession number KF192507). We subjected all available MERS-CoV genome sequences to phylogenetic analysis, including a correlation and regression analysis of known dates of virus isolation versus tree branch lengths (figure 3 ). We estimated the rate of evolution as 1·6 × 10−3 substitutions per site per year. The time of the common ancestor of all five viruses for which genomes are available was halfway through 2011 (figure 3). The virus in our patient clustered with a sequence from a virus imported into the UK from Qatar.16 To compare this sequence with that of another virus from the same region, we reanalysed a stored clinical sample from another case of MERS-CoV infection imported into Germany in October, 2012. This sample contained low concentrations of RNA, so the genome of the virus had not been successfully sequenced previously.8 After many attempts to recover RT-PCR fragments from the available bronchoalveolar lavage sample, we could sequence 12 fragments, covering 4012 nucleotides of the MERS-CoV genome (GenBank accession number KC875821). A concatenated alignment of homologous sequence portions of all available MERS-CoV sequences was subjected to phylogenetic analyses, confirming a clustering of sequences from Qatar and the United Arab Emirates (figure 3). A sequence from a patient with a history of travel to Pakistan and Saudi Arabia branched next to this cluster.
Figure 3.
Maximum likelihood phylogenetic analysis
(A) Tree with linear regression of genetic divergence from the root against time of collection of samples. (B) Tree based on all available MERS-CoV sequences (concatenated 4012 bp dataset). Full genomes for other viruses available. MERS-CoV=Middle East respiratory syndrome coronavirus.
During and up to 10 days after the course of treatment, 14 health-care workers who had direct contact with our patient or patient-derived materials reported mild respiratory symptoms. Samples were taken from the upper respiratory tract and tested by two different RT-PCR assays for MERS-CoV. None yielded positive results. By contrast, one patient who had had direct contact with the patient with MERS-CoV was infected with HCoV-NL63, a common human coronavirus, and four patients were infected with rhinoviruses. These rhinoviruses were not all mutually related, and none was related to the rhinovirus detected in the patient with MERS-CoV (appendix). Follow-up of all contact patients, including investigation for subclinical infections, is in progress.
Discussion
We have outlined the chronological follow-up of a patient with MERS-CoV, in which we used quantitative virological diagnostic tests (panel ). Viral loads were highest in the lower-respiratory tract. The viral sequence from this patient clustered with sequences from nearby Qatar.
Panel. Research in context.
Systematic review
We searched PubMed for reports published in English at any time before June 7, 2013. We used the search term “MERS-CoV OR HCoV-EMC”. We identified 29 reports linked to Middle East respiratory syndrome coronavirus (MERS-CoV), starting with Zaki and colleagues' initial report,1 in which a previously unknown coronavirus isolated from the sputum of a 60-year-old man is described. When we used the search term “MERS-CoV”, we identified four reports,2, 5, 12, 17 none of which provided quantitative viral load profiles of infected patients.
Interpretation
Our report provides the first complete viral load profile in a case of MERS-CoV infection. The distribution of viral loads in the respiratory tract suggests lower-respiratory-tract samples should be taken preferentially. Low concentrations of the virus in stool, urine, and blood samples suggests little virus excretion—at least in our patient—from body compartments other than the respiratory tract.
Laboratory data are crucial for diagnostic recommendations, to make projections about prognosis, and to estimate infection risks. Without quantitative laboratory data from well documented cases of MERS-CoV infection, most considerations had been made on the basis of an assumed analogy to severe acute respiratory syndrome (SARS).12, 18, 19, 20 However, elementary traits of the virus, such as its receptor usage and sensitivity to type I and type III interferon, differ substantially from that of the SARS coronavirus, suggesting that differences in disease patterns (eg, in organ tropism or in virus shedding) might exist.21, 22, 23, 24, 25 We focused on these aspects with quantitative virus testing in all relevant body compartments, including viral loads in non-respiratory samples.5, 12 However, our patient—like most other cases anecdotally reported so far—had an underlying disease that could affect virus shedding patterns. Only analysis of a large number of patients can yield general figures about qualitative virus data.
Faecal shedding was of particular interest, because patients with SARS regularly showed high virus concentrations and prolonged virus excretion in stools that led to the use of stool samples, even for routine SARS diagnostic tests.18, 20, 26 Diarrhoea was reported in two descriptions of MERS-CoV clusters, and it was speculated that faecal virus shedding might have occurred.5, 12 However, no laboratory data for virus in stool samples were provided. Our patient had low faecal virus concentrations that were close to the lowest detection limit on days 12 and 16 of illness. In the only other description so far, one stool sample from a patient with MERS-CoV had a negative result.16 Stool samples from many patients, including those with early stages of disease, should be tested to assess whether faecal sources could have a role in transmission, or whether MERS-CoV differs from SARS in this aspect.
Another important finding was that we recorded low concentrations of virus in urine samples. This finding is surprising, because early kidney failure during the course of MERS-CoV infection has been reported, and kidney cells in laboratory models are highly permissive for MERS-CoV replication.5, 12, 23 The fact that the virus was present in urine but not in the blood suggests autonomous virus replication in the kidneys, potentially without active secretion of virus into the urine. However, renal failure due to specific viral infection or immunopathogenesis is not necessarily indicated, because the patient had received several doses of potentially nephrotoxic antimicrobial agents in a setting of underlying multiple myeloma. Post-mortem examinations are urgently needed to clarify whether kidney failure in MERS-CoV infection is a primary and preventable result of viral infection, or a secondary complication of severe systemic disease.27, 28
Quantitative virus data are needed to orient diagnostics and hospital infection control measures. The recorded viral load profile, with highest RNA concentrations in bronchoalveolar lavage and tracheobronchial aspirates, confirms suggestions made in another report about the preferential use of lower-respiratory-tract samples for virus diagnostic tests.5 Notably, the reported overall stability of detectable virus RNA in closed suction catheters indicates a straightforward and non-contagious way to collect diagnostic samples even from non-intubated patients. Oronasal swabs should not be preferentially submitted for testing, especially in patients presenting late in their disease course with substantial lower respiratory involvement.5
Our data for stool, urine, and blood samples suggest a fairly low infection risk during non-respiratory care procedures. The absence of detectable virus in blood matches reports made in an earlier case of MERS-CoV infection.16 However, Guery and colleagues5 reported low semi-quantitative virus measurements in the blood of one of their patients. Moreover, initial experimental studies suggested that MERS-CoV infected vascular endothelial cells.25 However, quantitative data suggest a low risk from general laboratory procedures involving blood.
By contrast, the low virus concentrations and failure to isolate infectious virus from respiratory secretions should not be taken as a general indication of airway-associated infection risks. Virological monitoring of the patient started only late in the disease course, at a time when the infectiousness of the virus could already have been reduced (as suggested by the occurrence of neutralising antibodies). The fact that we could not isolate MERS-CoV could have been due to the concomitant presence of herpes simplex virus type 1, which overgrew some of the diagnostic cell cultures. Furthermore, coronaviruses that infect people are generally difficult to isolate, particularly in late phases of disease. Only two successful isolations of MERS-CoV have been reported worldwide so far.1, 5 These isolations were done on day 4 of disease,5 and day 7 of disease.1 Our samples were taken on days 12 and 14, and the sample from day 12 was stored for 3 days before cell culture. Isolation success cannot provide any information about infectiousness of the patient. Even a highly concentrated rhinovirus does not seem to have been transmitted from the patient, suggesting that effective protective measures were in place during treatment of the intubated patient in the intensive care unit.
The sequence data from this and another patient treated in Germany enable an extended analysis of phylogeny, hinting at a geographical structure of the MERS-CoV tree. Specifically, viral sequences from the eastern part of the Arabian Peninsula cluster together and stem from one common ancestor whose date of existence is projected to be after that of viruses from Jeddah and Jordan. Date estimates will probably be refined when more sequences become available. Moreover, whether the reported geographical structure represents repeated transfer from a geographically structured viral reservoir population and limiting chains of person-to-person transmission or multiple sustained lineages of human infections is unclear. With only five complete genome sequences available as yet, genetic data are urgently needed to establish the spatial and temporal distribution of cases, estimate the number of independent human chains of transmission, and thus better assess the threat that MERS-CoV poses to world health. Four sequences from a continuing hospital outbreak in Al-Hasa, Saudi Arabia, have now been deposited in GenBank. Preliminary phylogenetic analyses confirm the clustering of viruses from the eastern part of the Arabian Peninsula (Qatar: strains England2 and Essen; Abu Dhabi: strain Munich; Al-Hasa: GenBank Accession numbers KF186564-KF186567).
For more on EMPERIE see http://www.emperie.eu/emp/
Acknowledgments
Acknowledgments
This work was supported by a European research project on emerging diseases detection and response (EMPERIE; contract No 223498). CD has received infrastructural support from the German Centre for Infection Research, which included full funding of the position of VC. Virological analyses were partly support by the German Ministry for Research and Education and the German research council (grants 01KIO701 and DR 772/3-1). We thank Tobias Bleicker, Sebastian Brünink, Monika Eschbach-Bludau, Stephan Kallies, Heike Kirberg, Tobias Klant, Ingrid Kröning, and Astrid Schneider (Institute of Virology, Bonn, Germany) for excellent technical assistance.
Contributors
CD designed the virological studies, phylogenetic analysis, and virological data analysis. MS, WHar, GS, SS, WG, HGu, TR, MS-W, FB, and C-MW contributed to clinical data generation and analysis. MS, VMC, RK, DM, SJ, and AR contributed to figures. VMC, RK, DM, SJ, MAM, SA, and UD generated and analysed virological data. AR did phylogenetic analysis. CD, WHaa, HGo, and C-MW interpreted data. CD, MS, VMC, FB, AR, and C-MW wrote the report. WHaa advised the public health intervention. HGo and PG coordinated the public health intervention.
Conflicts of interest
We declare that we have no conflicts of interest.
Contributor Information
Christian Drosten, Email: drosten@virology-bonn.de.
Clemens-Martin Wendtner, Email: clemens.wendtner@klinikum-muenchen.de.
Supplementary Material
References
- 1.Zaki AM, van Boheemen S, Bestebroer TM, Osterhaus AD, Fouchier RA. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N Engl J Med. 2012;367:1814–1820. doi: 10.1056/NEJMoa1211721. [DOI] [PubMed] [Google Scholar]
- 2.de Groot RJ, Baker SC, Baric RS. Middle East Respiratory Syndrome coronavirus (MERS-CoV); announcement of the Coronavirus Study Group. J Virol. 2013 doi: 10.1128/JVI.01244-13. published online May 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO Middle East respiratory syndrome coronavirus (MERS-CoV)—update. June 7, 2013. http://www.who.int/csr/don/2013_06_07/en/index.html (accessed June 12, 2013). [DOI] [PMC free article] [PubMed]
- 4.Bermingham A, Chand M, Brown C. Severe respiratory illness caused by a novel coronavirus, in a patient transferred to the United Kingdom from the Middle East, September 2012. Euro Surveill. 2012;17:20290. [PubMed] [Google Scholar]
- 5.Guery B, Poissy J, el Mansouf L. Clinical features and viral diagnosis of two cases of infection with Middle East Respiratory Syndrome coronavirus: a report of nosocomial transmission. Lancet. 2013 doi: 10.1016/S0140-6736(13)60982-4. published online May 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cotten M, Lam TT, Watson SJ. Full-genome deep sequencing and phylogenetic analysis of novel human betacoronavirus. Emerg Infect Dis. 2013;19:736–742. doi: 10.3201/eid1905.130057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Corman V, Muller M, Costabel U. Assays for laboratory confirmation of novel human coronavirus (hCoV-EMC) infections. Euro Surveill. 2012;17:20334. doi: 10.2807/ese.17.49.20334-en. [DOI] [PubMed] [Google Scholar]
- 8.Buchholz U, Muller MA, Nitsche A. Contact investigation of a case of human novel coronavirus infection treated in a German hospital, October–November 2012. Euro Surveill. 2013;18:20406. [PubMed] [Google Scholar]
- 9.Corman V, Eckerle I, Bleicker T. Detection of a novel human coronavirus by real-time reverse-transcription polymerase chain reaction. Euro Surveill. 2012;17:20285. doi: 10.2807/ese.17.39.20285-en. [DOI] [PubMed] [Google Scholar]
- 10.Herzog P, Drosten C, Muller MA. Plaque assay for human coronavirus NL63 using human colon carcinoma cells. Virol J. 2008;5:138. doi: 10.1186/1743-422X-5-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guindon S, Gascuel O. A simple, fast, and accurate algorithm to estimate large phylogenies by maximum likelihood. Syst Biol. 2003;52:696–704. doi: 10.1080/10635150390235520. [DOI] [PubMed] [Google Scholar]
- 12.Memish ZA, Zumla AI, Al-Hakeem RF, Al-Rabeeah AA, Stephens GM. Family cluster of Middle East Respiratory Syndrome coronavirus infections. N Engl J Med. 2013 doi: 10.1056/NEJMoa1303729. published online May 29. [DOI] [PubMed] [Google Scholar]
- 13.Kessler HH, Muhlbauer G, Rinner B. Detection of herpes simplex virus DNA by real-time PCR. J Clin Microbiol. 2000;38:2638–2642. doi: 10.1128/jcm.38.7.2638-2642.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lu X, Holloway B, Dare RK. Real-time reverse transcription-PCR assay for comprehensive detection of human rhinoviruses. J Clin Microbiol. 2008;46:533–539. doi: 10.1128/JCM.01739-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van den Brink JW, Simoons-Smit AM, Beishuizen A, Girbes AR, Strack van Schijndel RJ, Groeneveld AB. Respiratory herpes simplex virus type 1 infection/colonisation in the critically ill: marker or mediator? J Clin Virol. 2004;30:68–72. doi: 10.1016/j.jcv.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 16.Bermingham A, Chand MA, Brown CS. Severe respiratory illness caused by a novel coronavirus, in a patient transferred to the United Kingdom from the Middle East, September 2012. Euro Surveill. 2012;17:20290. [PubMed] [Google Scholar]
- 17.Lau SK, Li KS, Tsang AK. Genetic characterization of Betacoronavirus lineage C viruses in bats revealed marked sequence divergence in the spike protein of Pipistrellus bat coronavirus HKU5 in Japanese pipistrelle: implications on the origin of the novel Middle East Respiratory Syndrome Coronavirus. J Virol. 2013 doi: 10.1128/JVI.01055-13. published online May 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Peiris JS, Yuen KY, Osterhaus AD, Stohr K. The severe acute respiratory syndrome. N Engl J Med. 2003;349:2431–2441. doi: 10.1056/NEJMra032498. [DOI] [PubMed] [Google Scholar]
- 19.Poon LL, Guan Y, Nicholls JM, Yuen KY, Peiris JS. The aetiology, origins, and diagnosis of severe acute respiratory syndrome. Lancet Infect Dis. 2004;4:663–671. doi: 10.1016/S1473-3099(04)01172-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Drosten C, Gunther S, Preiser W. Identification of a novel coronavirus in patients with severe acute respiratory syndrome. N Engl J Med. 2003;348:1967–1976. doi: 10.1056/NEJMoa030747. [DOI] [PubMed] [Google Scholar]
- 21.Kindler E, Jonsdottir HR, Muth D. Efficient replication of the novel human betacoronavirus EMC on primary human epithelium highlights its zoonotic potential. MBio. 2013;4:e00611–e00612. doi: 10.1128/mBio.00611-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Raj VS, Mou H, Smits SL. Dipeptidyl peptidase 4 is a functional receptor for the emerging human coronavirus-EMC. Nature. 2013;495:251–254. doi: 10.1038/nature12005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Muller MA, Raj VS, Muth D. Human coronavirus EMC does not require the SARS-coronavirus receptor and maintains broad replicative capability in mammalian cell lines. MBio. 2012;3:00515. doi: 10.1128/mBio.00515-12. 00512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zielecki F, Weber M, Eickmann M. Human cell tropism and innate immune system interactions of human respiratory coronavirus EMC compared to those of severe acute respiratory syndrome coronavirus. J Virol. 2013;87:5300–5304. doi: 10.1128/JVI.03496-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chan RW, Chan MC, Agnihothram S. Tropism of and innate immune responses to the novel human betacoronavirus lineage C virus in human ex vivo respiratory organ cultures. J Virol. 2013;87:6604–6614. doi: 10.1128/JVI.00009-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Peiris JS, Guan Y, Yuen KY. Severe acute respiratory syndrome. Nat Med. 2004;10(suppl):S88–S97. doi: 10.1038/nm1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gu J, Gong E, Zhang B. Multiple organ infection and the pathogenesis of SARS. J Exp Med. 2005;202:415–424. doi: 10.1084/jem.20050828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chu KH, Tsang WK, Tang CS. Acute renal impairment in coronavirus-associated severe acute respiratory syndrome. Kidney Int. 2005;67:698–705. doi: 10.1111/j.1523-1755.2005.67130.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.